INTRODUCTION
Infertility affects 15% of Canadian couples trying to conceive.1,2 Male factor infertility is a contributing cause in 50% of cases — 30% of which are the sole cause.3 Non-obstructive azoospermia (NO A) is the most severe form of male factor infertility and it accounts for 10–15% of men seeking treatment for infertility.4 NO A is defined by the absence of sperm in ejaculate secondary to a failure in spermatogenesis.4
Treatment of NO A currently lacks coverage for surgical intervention within the Canadian healthcare system, with costs borne exclusively by patients. The current gold standard management for NO A includes microdissection testicular sperm extraction (mTESE ) to retrieve sperm, which is then processed for intra-cytoplasmic sperm injection (ICSI ). The average success of sperm retrieval using mTESE is approximately 50%, with pregnancy rates of approximately 30% and a live birth rate of up to 25%.1,5–7
While advances in assisted reproductive technologies have dramatically changed the management of NO A, there is a knowledge gap in our understanding of the patient experience. A need exists for further research into patient perspectives, expectations, and satisfaction of treatment to frame both current and future potential therapies. Recognizing the threshold of clinically significant difference in sperm retrieval or pregnancy rates is critical to appreciating the potential interest in future technologies.
As novel treatments for NO A are developed, it is important to understand the thresholds of costs and benefit associated with treatment paradigms deemed acceptable to patients. To our knowledge, there is no literature around urologists’ understanding of patients’ preferences regarding NO A treatment. Here, we describe the results of a survey ascertaining NO A patients’ and their providers’ expectations surrounding their treatment.
METHODS
This was a prospective, survey-based study approved by the University of British Columbia’s clinical research ethics board. This center is a high-volume, Canadian tertiary care hospital with one fellowship-trained urologist who specializes in male infertility, and this group performs approximately 10–15 mTESE s per year.
Two discrete surveys were created using the Checkbox™ online survey software and links were emailed to participants. We emailed one survey to all patients who had undergone treatment for NO A at our center between July 2018 and January 2022, who had valid emails on file (40 patients), and their partners. The survey included questions on previous treatment for NO A, the maximum cost patients would be willing to pay out-of-pocket for a new treatment for NO A, and what minimum benefit to sperm retrieval rate, pregnancy rate, and live birth rate they would tolerate for an additional NO A treatment (Appendix A; available at cuaj.ca).
A second survey was developed and emailed to all Canadian urologists and fellowship trainees who routinely treat NO A. This list of 23 urologists was collated by our research team based on knowledge of surgeons’ practices. This survey included questions on surgical experience with NO A, the maximum costs urologists believed patients would be willing to pay out-of-pocket for a new treatment for NO A, and what minimum benefit urologists believed patients would tolerate to sperm retrieval rate, pregnancy rate, and live birth rate for an additional NO A treatment (Appendix B; available at cuaj.ca).
The surveys remained open for eight weeks and all responses were anonymous. When surveys were not completed in their entirety, partial responses were still included in the data analysis. Descriptive analyses of the survey results were performed using Microsoft Excel©, including demographics analysis and a comparative analysis between the two surveyed populations, and between those who had undergone sperm retrieval and those who had not, using the Mann-Whitney U test. Statistical significance was set at p<0.05.
RESULTS
Forty patients were identified to have been seen for NO A since July 2018; 22 patients (55%) responded and 19 (48%) elicited complete responses. Patient demographics are summarized in Table 1.
Table 1.
Demographics of patients surveyed (N=22)
| Response rate | 55% | |
|
| ||
| Number of complete responses | 19 | 86.4% |
|
| ||
| Years trying to conceive | ||
| <1 | 1 | 4.5% |
| 1 | 1 | 4.5% |
| 2 | 8 | 36.4% |
| 3 | 5 | 22.7% |
| 4 | 1 | 4.5% |
| 5+ | 3 | 13.6% |
| Missing | 3 | 13.6% |
|
| ||
| Ideal no of children | ||
| 1 | 6 | 27.3% |
| 2 | 11 | 50.0% |
| 3 | 1 | 4.5% |
| 4+ | 1 | 4.5% |
| Missing | 3 | 13.6% |
|
| ||
| Infertility treatments | ||
| Sperm retrieval (IVF, ICSI) | 15 | 68.2% |
| Donor sperm | 13 | 59.1% |
| Adoption | 4 | 18.2% |
| No further treatment | 2 | 9.1% |
|
| ||
| Highest level of education | ||
| Did not complete high school | 0 | 0.0% |
| High school | 0 | 0.0% |
| Apprenticeship/trades diploma | 3 | 13.6% |
| CEGEP, college, or other non-university certificate/ diploma | 5 | 22.7% |
| University undergraduate degree | 12 | 54.5% |
| Post graduate degree | 1 | 4.5% |
| Professional degree | 1 | 4.5% |
|
| ||
| Household income | ||
| <$50 000 | 1 | 4.5% |
| $51 000–75 000 | 1 | 4.5% |
| $76 000–100 000 | 5 | 22.7% |
| $101 000–150 000 | 2 | 9.1% |
| $151 000–200 000 | 6 | 27.3% |
| $201 000–300 000 | 4 | 18.2% |
| >$300 000 | 3 | 13.6% |
ICSI: intracytoplasmic sperm injection; IVF: in-vitro fertilization.
To consider pursuing medical/non-surgical treatment, participants indicated that they would expect a median increase in the success rates of sperm retrieval by a minimum of 7.5% (standard deviation [SD ] 11.62%), successful pregnancy by 17.5% (SD 15.05%), and obtaining a live birth by 10% (SD 17.60%). To pursue surgical interventions, participants had greater expectations for the increased success rate of sperm retrieval, pregnancy, and live birth rate (Figure 1). Patients who did not have sperm retrieval had greater expectations for success rates of all surgical interventions compared to patients who had undergone sperm retrieval (Table 2).
Figure 1.
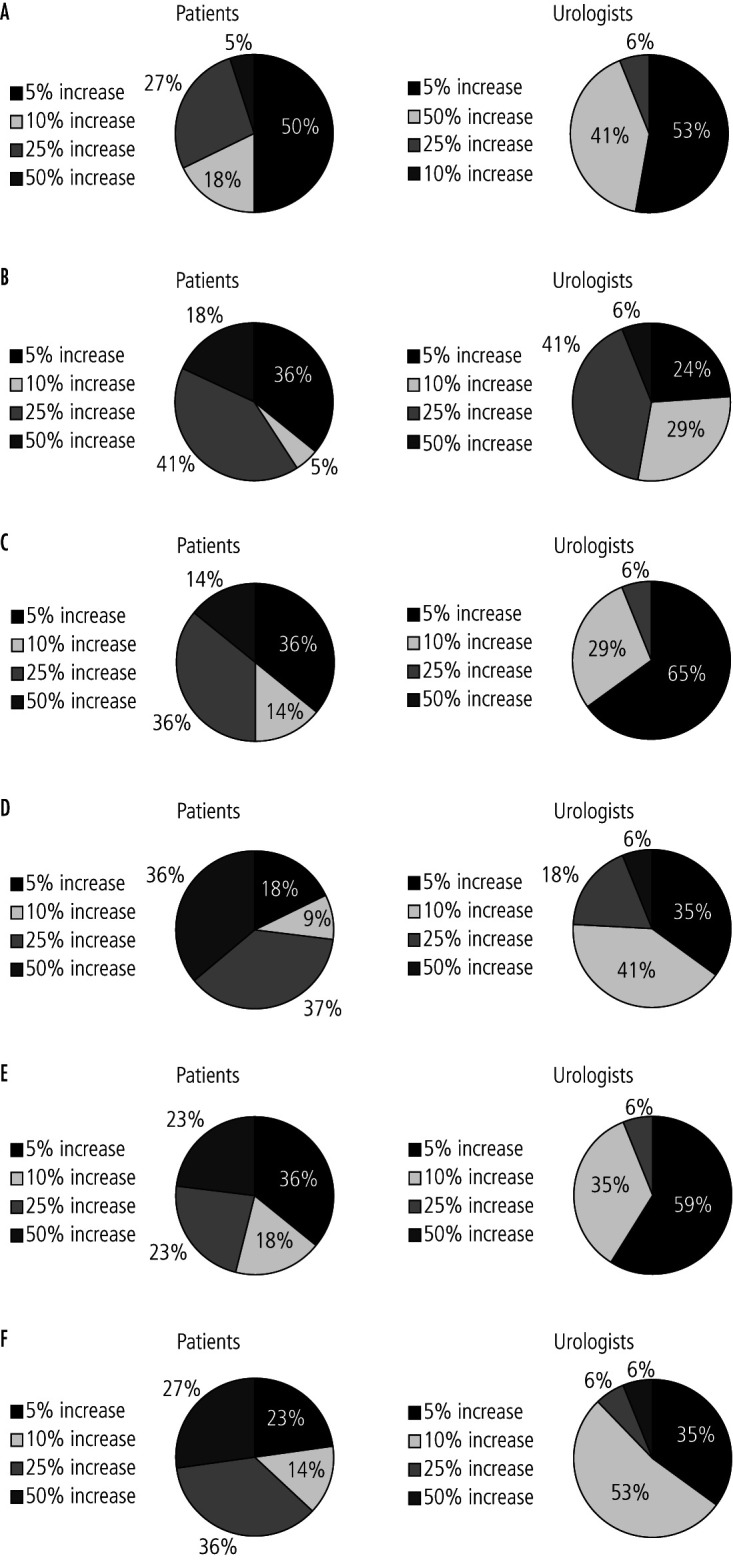
Patients’ and urologists’ perceptions of patients’ minimal threshold for additive efficacy for a novel non-obstructive azoospermia treatment. (A) Minimal increase in sperm retrieval ate with a medication. (B) Minimal increase in sperm retrieval ate with a surgery. (C) Minimum increase in pregnancy with a medication. (D) Minimum increase in pregnancy with a surgery. (E) Minimum increase in live birth rate with a medication. (F) Minimum increase in live birth rate with a surgery.
Table 2.
Comparison between patients’ minimal threshold for additive efficacy for a novel NOA treatment for those who had sperm retrieval and those who had not
| History of sperm retrieval | No history of sperm retrieval | p | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| n | % total | Median | n | % total | Median | ||
|
| |||||||
| Minimum increase in sperm retrieval rate with a medication | 5% | 10% | 0.230 | ||||
| 5% | 9 | 60.0% | 2 | 28.6% | |||
| 10% | 2 | 13.3% | 2 | 28.6% | |||
| 25% | 4 | 26.7% | 2 | 28.6% | |||
| 50% | 0 | 0% | 1 | 14.3% | |||
|
| |||||||
| Minimum increase in sperm retrieval rate with a surgery | 5% | 25% | 0.035 | ||||
| 5% | 8 | 53.3% | 0 | 0.0% | |||
| 10% | 1 | 6.7% | 0 | 0.0% | |||
| 25% | 4 | 26.7% | 5 | 71.4% | |||
| 50% | 2 | 13.3% | 2 | 28.6% | |||
|
| |||||||
| Minimum increase in pregnancy with a medication | 10% | 17.5% | 0.435 | ||||
| 5% | 6 | 40.0% | 2 | 28.6% | |||
| 10% | 2 | 13.3% | 1 | 14.3% | |||
| 25% | 6 | 40.0% | 2 | 28.6% | |||
| 50% | 1 | 6.7% | 2 | 28.6% | |||
|
| |||||||
| Minimum increase in pregnancy with a surgery | 25% | 50% | 0.022 | ||||
| 5% | 4 | 26.7% | 0 | 0.0% | |||
| 10% | 2 | 13.3% | 0 | 0.0% | |||
| 25% | 6 | 40.0% | 2 | 28.6% | |||
| 50% | 3 | 20.0% | 5 | 71.4% | |||
|
| |||||||
| Minimum increase in live birth rate with a medication | 10% | 10% | 0.529 | ||||
| 5% | 6 | 40.0% | 2 | 28.6% | |||
| 10% | 2 | 13.3% | 2 | 28.6% | |||
| 25% | 5 | 33.3% | 0 | 0.0% | |||
| 50% | 2 | 13.3% | 3 | 42.9% | |||
|
| |||||||
| Minimum increase in live birth rate with a surgery | 10% | 37.5% | 0.015 | ||||
| 5% | 5 | 27.3% | 0 | 0.0% | |||
| 10% | 3 | 13.6% | 0 | 0.0% | |||
| 25% | 5 | 36.4% | 3 | 42.9% | |||
| 50% | 2 | 27.3% | 4 | 57.1% | |||
NOA: non-obstructive azoospermia.
With regards to the maximal acceptable cost to pursue further fertility treatments for a given percentage increase in live birth rate, there was a trend towards a higher acceptable cost for an increased rate of successful live births (Figure 2). The median acceptable costs for a 10% and 50% increase in live birth rate were $5000 and $15 000, respectively.
Figure 2.
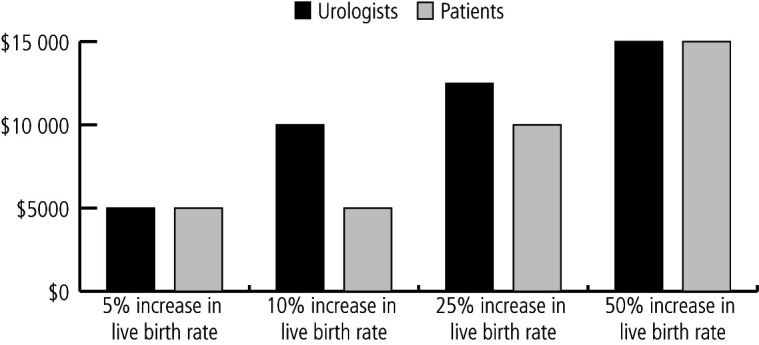
Patients’ and urologists’ perceptions of patients’ maximal acceptable cost of new fertility treatments.
Of the 22 Canadian urologists surveyed, 17 (77%) responded and 16 (73%) completed the survey in its entirety. Most practiced in an academic center and nearly half estimated treating more than 50 NO A patients per year (Table 3).
Table 3.
Demographics of urologists surveyed (N=17)
| Response rate | 77% | |
|
| ||
| Number of complete responses | 16 | 94.1% |
|
| ||
| Years in practice | ||
| <5 years | 7 | 41.2% |
| 5–10 years | 1 | 5.9% |
| 10–15 years | 3 | 17.6% |
| >15 years | 6 | 35.3% |
|
| ||
| Fellowship trained | 16 | 94.1% |
|
| ||
| Practice type | ||
| Academic | 13 | 76.5% |
| Community | 1 | 5.9% |
| Both | 3 | 17.6% |
|
| ||
| NOA patients treated per year | ||
| <10 | 2 | 11.8% |
| 10–50 | 7 | 41.2% |
| >50 | 8 | 47.1% |
NOA: non-obstructive azoospermia.
Looking broadly, practitioners underestimated the threshold at which patients would consider further fertility treatment. To consider a new medical or surgical management, urologists had assumed a median minimum 5% and 10% respective increase (SD 4.8%, 11.7%) in sperm retrieval would be acceptable, and similarly a median minimum 5% and 10% respective increase (SD 4.9%, 10.7%) in live birth rates (Figure 1). Their opinion on the median maximal acceptable costs for patients for a 10% and 50% increase in live birth rate were $10 000 and $15 000, respectively (Figure 2).
DISCUSSION
Treatment of NO A has limited success with respect to outcomes and is financially burdensome to Canadian patients; however, to our knowledge, there have been no studies exploring the acceptability and willingness of patients to engage in treatment, nor their cost threshold.
This study is significant in that it is the first to report patient and physician thresholds for treatment successes and associated costs. Furthermore, it garnered a Canada-wide response from urologists who treat NO A. Patients indicated that to pursue medical or surgical treatment, they would expect a 7–25% median increase in fertility outcomes, ranging from sperm retrieval to live birth, respectively. Patients who had undergone sperm retrieval had a lower threshold of acceptable increase in fertility outcomes for surgical procedures compared to those who had not. Notably, this was divergent from urologists’ perceptions of patient expectations, whereby the minimal threshold to engage in treatment was estimated from 5–10%. There was a statistically significant difference between thresholds of patients and urologists in the domains of achieving pregnancy with a new medication (p=0.023) or surgery (p=0.010) and increasing live birth rate with a new medication (p=0.041) or surgery (p=0.020). There were no statistically significant differences in financial expectations between practitioners and patients.
Limitations of this study include small sample size due to the nature of a single-center study. The study did not look at how potential side effects could affect patients’ willingness for treatment.
CONCLUSIONS
Given the differential acceptability in fertility outcomes between patient and provider, this study highlights the importance of providing patients with clear information about the expected outcome and the impact it may have on their quality of life, self-esteem, and overall relationship.8,9 As new best practice guidelines place a greater emphasis on personalized, patient-centered care, this study is a first step towards understanding the expectations of medical and surgical management for NO A.
KEY MESSAGES.
■ This is the first prospective, survey-based study comparing patient and physician thresholds for NO A treatment successes and associated costs.
■ Urologists underestimate the minimum acceptable increase in outcomes of pregnancy and live birth patients would tolerate for additional NO A treatment.
■ Urologists’ estimates of financial thresholds for additional NO A treatment were concurrent with patients’ reported values.
Supplementary Information
Footnotes
Appendix available at cuaj.ca
COMPETING INTERESTS: The authors do not report any competing personal or financial interests related to this work.
This paper has been peer-reviewed.
REFERENCES
- 1.Jarvi K, Lo K, Grober E, et al. CUA guideline: The workup and management of azoospermic males. Can Urol Assoc J. 2015;9:229–35. doi: 10.5489/cuaj.3209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eisenberg ML, Lathi RB, Baker VL, et al. Frequency of the male infertility evaluation: Data from the national survey of family growth. J Urol. 2013;189:1030–4. doi: 10.1016/j.juro.2012.08.239. [DOI] [PubMed] [Google Scholar]
- 3.Leaver RB. Male infertility: An overview of causes and treatment options. Br J Nurs. 2016;25:S35–40. doi: 10.12968/bjon.2016.25.18.S35. [DOI] [PubMed] [Google Scholar]
- 4.Tournaye H, Krausz C, Oates RD. Concepts in diagnosis and therapy for male reproductive impairment. Lancet Diabetes Endocrinol. 2017;5:554–64. doi: 10.1016/S2213-8587(16)30043-2. [DOI] [PubMed] [Google Scholar]
- 5.Corona G, Minhas S, Giwercman A, et al. Sperm recovery and ICSI outcomes in men with non-obstructive azoospermia: A systematic review and meta-analysis. Hum Reprod Update. 2019;25:733–57. doi: 10.1093/humupd/dmz028. [DOI] [PubMed] [Google Scholar]
- 6.Schiff JD, Palermo GD, Veeck LL, et al. Success of testicular sperm injection and intracytoplasmic sperm injection in men with Klinefelter syndrome. J Clin Endocrinol Metab. 2005;90:6263–7. doi: 10.1210/jc.2004-2322. [DOI] [PubMed] [Google Scholar]
- 7.Raman JD, Schlegel PN. Testicular sperm extraction with intracytoplasmic sperm injection is successful for the treatment of nonobstructive azoospermia associated with cryptorchidism. J Urol. 2003;170:1287–90. doi: 10.1097/01.ju.0000080707.75753.ec. [DOI] [PubMed] [Google Scholar]
- 8.Dancet EAF, Van Empel IWH, Rober P, et al. Patient-centered infertility care: A qualitative study to listen to the patients’ voice. Hum Reprod. 2011;26:827–33. doi: 10.1093/humrep/der022. [DOI] [PubMed] [Google Scholar]
- 9.Bendayan M, Sais E, Alter L, et al. For patients with non-obstructive azoospermia, the outcome of testicular sperm extraction correlates with self-esteem, sexual health, and the quality of the couple’s relationship. Basic Clin Androl. 2022;32:3. doi: 10.1186/s12610-022-00153-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


