Abstract
Background
The phenomenon of antibiotic resistance shows no sign of stopping, despite global policies to combat it that have been in place for several years. The risk of forms of pathogenic microorganisms that are increasingly resistant to common antibiotics has led health authorities around the world to pay greater attention to the phenomenon. The worrying situation, has led to further recommendations from the World Health Organization (WHO) and national recommendations in Italy through the new National Plan against Antibiotic Resistance 2022–2025 (PNCAR 2022–2025).
Aim
This manuscript aims to raise the awareness of all health professionals to follow what is suggested by regulatory agencies and scientific societies.
Method
We conducted a retrospective study of antibiotic pharmacoutilization in Italy, in the Campania region at the Azienda Sanitaria Locale (ASL) Napoli 3 Sud, on consumption in the first half of 2022 in a population of more than 1 million people.
Result
The results indicate that consumption, based on defined daily doses (DDDs), is above the national average. Probably the COVID-19 pandemic has influenced this growth in prescriptions.
Conclusions
Our study suggests an informed and appropriate use of antibiotics, so as to embark on a virtuous path in the fight against antibiotic resistance.
Keywords: Antibiotic resistance, Antibiotics, Appropriateness, Governance, Telemedicine
Résumé
Fond
Le phénomène de la résistance aux antibiotiques ne semble pas vouloir s’arrêter, malgré les politiques mondiales de lutte mises en place depuis plusieurs années. Le risque de formes de micro-organismes pathogènes de plus en plus résistants aux antibiotiques courants a conduit les autorités sanitaires du monde entier à porter une plus grande attention au phénomène. La situation préoccupante a conduit à de nouvelles recommandations de l’Organisation mondiale de la santé (OMS) et à des recommandations nationales en Italie à travers le nouveau Plan national de lutte contre la résistance aux antibiotiques 2022–2025 (PNCAR 2022–2025).
Avoir pour but
Ce manuscrit vise à sensibiliser tous les professionnels de santé à suivre ce qui est suggéré par les agences réglementaires et les sociétés savantes.
Méthode
Nous avons mené une étude rétrospective de la pharmacoutilisation des antibiotiques en Italie, dans la région de Campanie à l’Azienda Sanitaria Locale (ASL) Napoli 3 Sud, sur la consommation au premier semestre 2022 dans une population de plus de 1 million de personnes.
Résultat
Les résultats indiquent que la consommation, basée sur des doses journalières définies (DDD), est supérieure à la moyenne nationale. La pandémie de COVID-19 a probablement influencé cette croissance des prescriptions.
Conclusions
Notre étude suggère une utilisation informée et appropriée des antibiotiques, afin de s’engager sur une voie vertueuse dans la lutte contre la résistance aux antibiotiques.
Mots clés: Résistance aux antibiotiques, Antibiotiques, Pertinence, Gouvernance, Télémédecine
Abbreviations
- AIFA
Italian Medicines Agency
- AMR
Antimicrobial Resistance
- ATC
Anatomical Therapeutic Chemical
- DDD
Defined Daily Dose
- GAP
Global Action Plan
- GP
General Practitioner
- HAI
Healthcare-associated infections
- IOC
Indian Ocean Commission
- LHC
Local Health Company
- NAP
national action plans
- NPCAR
National Plan to Combat Antibiotic Resistence
- PFC
Pediatricians of free choice
- PNRR
Plan National Recovery and Resilience
- SNPC
Territorial Functional Aggregation
- WHO
World Health Organization
- WG
Working Group
Introduction
The phenomenon of Antimicrobial Resistance (AMR according to the Anglo-Saxon acronym) is a global human and veterinary public health emergency which has a strong impact on morbidity and mortality, and which can generate an increase in expenditure following the higher use of health care resources (length of stay, diagnostic tests, drugs). Several antibiotics become partially or completely ineffective, making advanced medical procedures risky (e.g., cancer chemotherapies, organ transplants, hip replacements). The National Plan to Combat Antimicrobial Resistance (NPCAR), drafted from a One Health perspective, has as its aims to decrease the rate of care-related infections (HAI) and promote the rational and informed use of antibiotics in human and veterinary settings. The year 2025 will mark 10 years since the adoption of the World Health Organization (WHO) Global Plan of Action (GAP) against AMR, and although progress has been made to date, concrete and effective actions still need to be initiated to halt this phenomenon [1], [2]. Today, this issue results in clinical and economic harm to the health care world, and if the measures to be put in place are insufficient by 2050, up to 10 million deaths per year could be estimated (a number higher than deaths caused by malignancies) [3], [4]. This is followed by the World Bank's alarming analysis of the economics: impact on health care costs with global increases by 2050 between $300 billion and over $1 trillion per year [5]. In addition, to this growing trend, it should be considered that the recent COVID-19 pandemic has further exacerbated the data on increasing resistance to antibiotic overuse [6], [7]. After all, in the early pandemic period, many classes of drugs, such as azithromycin, were used with the hope of quickly obtaining a cure for COVID-19 infection, before the emergence of mRNA vaccines and direct antivirals [8], [9], [10]. Antibiotic resistance is one of the biggest and most troubling global health challenges; a “hidden pandemic” that is almost never talked about, but reportedly causes hundreds of thousands of deaths each year. The Global Database for Tracking Antimicrobial Resistance Country Self Assessment Survey (TrACSS) is an estimate of data that is based precisely on the self-assessment of individual countries [11]. COVID-19 reminded again how, in a global context, the health of humans and animals and the ecosystems in which they live are closely interconnected. Animals and people share the same environment, often live in close contact with each other, can be infected by the same pathogens and not infrequently even treated with the same drugs, affecting each other's health. It is clear that there is a need to approach the concept of health with a new, comprehensive, multidisciplinary and holistic vision capable of integrating the resources and expertise present in the human, veterinary and environmental spheres. This vision is called One Health. The One Health approach is now an indispensable element in addressing what is now internationally recognized as one of the most serious threats to global health and development, namely the issue of antimicrobial resistance [12], [13]. For these reasons, coordinated global action is needed to effectively mitigate the threat and contain the phenomenon [14], [15], [16], [17], [18], [19]. In addition, the uncontrolled spread of AMR threatens global sustainable development goals of health, food security, environmental well-being, and socioeconomic development [20]. Therefore, in September 2013, the WHO recommended the development of a GAP on antimicrobial resistance. The recommendation was subsequently adopted in May 2014 as a World Health Assembly resolution, and WHO began drafting the GAP together with the Food and Agriculture Organization of the United Nations. The GAP was endorsed as early as May 2015 by the 194 WHO member states, which were asked to develop and implement national action plans (NAPs) on AMR by the new deadline of 2025, modeled after the GAP guidelines. In particular, the GAP identifies five areas for collective action to address AMR effectively [21], [22]:
-
•
effective communication, education, and training in order to improve awareness and understanding of microbial resistance;
-
•
effective antimicrobial surveillance to strengthen the knowledge and evidence base and research;
-
•
improve infection prevention and control measures to reduce incidence of infections;
-
•
optimize the use of antimicrobial drugs in human and animal health;
-
•
develop an economic case for sustainable investments that take into account the needs of all countries, and increase investments in new drugs, diagnostic tools, vaccines and other interventions.
Therefore, the 194 member states of the WHO have committed to integrate the five goals and corresponding actions of the GAP into a globally coordinated effort. To monitor national progress, the Tripartite relies on member states’ self-reports and antimicrobial resistance policies made available in the Global Antimicrobial Resistance Self-Assessment Database [23]. The database is based on surveys submitted annually to all member states. The United Nations General Assembly reaffirmed the GAP as a program to address AMR by identifying the roles of national governments, tripartite organizations, and other national and international partners. Tailoring the response in this way is essential to ensure that action addresses the priorities and contexts of individual countries [20], [24].
Aim
Italy is one of the European countries with the highest levels of AMR, associated with a high consumption of antibiotics (ranked 5th, ESAC-Net data). The objectives of this study concern aiming to raise awareness among all health care personnel toward decreasing the proportion of HAI and fostering rational and informed use of antibiotics in human and veterinary settings.
Methods
Asl Naples 3 Sud has a high population density of 1737 inhabitants/km2, with a population of approximately 1,077,000 inhabitants which is distributed between 57 municipalities, covering an area of 620 km2. This is one of the highest in the region and it is far higher compared with the national average. An analysis of antibiotic use in Italy in the first half of 2022 has been carried out, then a comparison has been made with data obtained from the “Tessera Sanitaria portal,” which reports all territorial pharmaceutical prescriptions. Cross-referencing this information made it possible to extrapolate the territorial incidence of the number of prescriptions carried out at the LHC Naples 3 Sud and in the Campania region. Mainly, consumption data expressed in defined daily dose (DDD) and gross expenditure have been extracted. A retrospective study on pharmacoutilization has been conducted to compare Italian national data with regional (Campania Region) and local (LHC Naples 3 Sud) data. The consumption data have been extrapolated on the basis of two main indicators: DDD × 1000 inhabitant/day, which standardizes the dose taken in the population taken into consideration, and the Gross expenditure × 1000 inhabitant/day, which it quantifies also the expenditure incurred in relation to the increased use of anti-infective drugs. DDD and Gross expenditure are the main indicators to perform a retrospective analysis of pharmacutilisation and thus arriving at a useful monitoring, in order to implement any corrective pharmaceutical governance actions. The “New Guarantee System for Health Monitoring”, published in the Official Journal on 14 June 2019 and in force since 1 January 2020, introduces a new indicator to monitor the consumption of antimicrobial drugs (ATC II: J01) at the population level pertaining to the Healthcare Company; the value is expressed in terms of DDD, with a threshold value referring to the entire year and equal to 7263. In addition, as part of the rationalization of antibiotic consumption and of the fight against the antibiotic resistance issue, the Campania Region, with Executive Decree No. 138/2018 and subsequent Executive Decree No. 213/2021, established that the consumption of antibiotics, expressed in DDD per 1000 population per day, should not exceed more than 10% of the value of antibiotic consumption reported in the national annual report on pharmaceutical assistance published by the Italian Medicine Agency (AIFA). Therefore, following the provisions of the Campania Region, the following tables have been generated, in order to provide a comparison of the trends of antimicrobial drugs consumption data between Italy, Campania and LHC Naples 3 Sud, over the period between January and June 2022.
Results
The illustrated results highlight differences in consumption and spending on antibiotic drugs between Italy, Campania region and LHC Naples 3 Sud. The analysis has been carried out focusing on a macroscopic reality such the Italian Nation and on a microscopic local reality (LHC Naples 3 Sud), going through the Campania Region, an area with an average population, to compare regional and national data. This monitoring analysis has been necessary in the aftermath of the COVID-19 pandemic, since health care attention to AMR problems declined dramatically, both due to the commitment of health care workers and since many antibiotics were used inappropriately to counteract the virus in the first steps. At LHC Naples 3 Sud, there has been an increase in the prescription of antimicrobial drugs and this retrospective analysis sought to highlight the issue and also to frame it against national and regional data, thus implementing urgent measures to contain and prevent the spread of AMR. Monitoring analyzes carried out before the COVID-19 pandemic showed steadily declining data on the consumption and expenditure of antibiotic drugs, whereas it was only after the pandemic that such consumption increased, in 2021 and 2022 respectively, when the COVID-19 pandemic was spread worldwide. The consumption of antibiotic drugs, expressed in DDD/1000 inhabitant/die, in H1 2022 is 22.8 DDD 1000 inhabitant/die for LHC Naples 3 Sud, with an increase of 18.8% compared to the regional value, and with an increase of 67.6%, compared to the national value (Table 1 ). These data confirm an increased prescription of microbial drugs in the area surveyed, with a high consumption compared to the national average. Moreover, data regarding gross expenditure on antibiotic drugs expressed as gross expenditure per 1000 inhabitant/die, in the first half of 2022 is € 51.8 DDD 1000 inhabitant/die for LHC Naples 3 Sud, with an increase respectively of 24.8% compared to the regional value, and 118.6% compared to the national value (Table 2 ) [25]. These data show how urgent measures are needed at the Campania Region and even more so at LHC Naples 3 Sud, with the aim to curb the consumption not only to limit AMR, but also to reduce the health care spending which increased in the pandemic years. In Table 3 , increase in Gross Expenditure × 1000 inhabitant/die (+14.6 percent) and consumption expressed in terms of DDD/1000 inhabitant/die (+22.8 percent) compared to H1 2021, is evident. Therefore, the expenditure and consumption values of individual antibiotic molecules have been compared in detail to identify to which antibiotics should be attributed the reason of the recorded deviation for LHC Naples 3 Sud, illustrated in Table 1, Table 2. Analyzing these data, it is necessary to understand which active ingredients are responsible for the higher consumption and expenditure. Table 4 shows the comparison of the 20 antibiotics active ingredients most used at the LHC Naples 3 Sud, in relation to the use in Campania region and Italy. It is illustrated that Amoxicillin + beta-lactamase inhibitor, with a value of 7.02 DDD/1000 inhabitant/die, diverts by +15.5% from the Campania value and by +46.1 percent from the Italy reference value. It is followed by Azithromycin, with a value of 3.81 DDD/1000 inhabitant/die which deviates by +25% from the Campania value and +11.6% from the Italy reference value. Clarithromycin, with a value of 3.31 DDD/1000 inhabitant/die, deviates respectively +23.4% from the Campania value and +92.8% from the Italy reference value. Eventually, Table 5 illustrates the analysis of the consumption of antibiotics by active ingredient by comparing what has been recorded in the same period the previous year. In LHC Naples 3 Sud, the antibiotic with the greatest impact in terms of consumption is Amoxicillin + beta-lactamase inhibitor, with a value of 7.02 DDD/1000 inhabitants/day, followed by Azithromycin with a value of 3.81 DDD/1000 inhabitant/die, and Clarithromycin with a value of 3.31 DDD/1000 inhabitant/die. The change from the previous year shows a generalized trend of increasing consumption for almost all active ingredients under analysis.
Table 1.
Antibiotic drug consumption-Comparison Italy, Campania Region, LHC Naples 3 Sud.
Consommation d’antibiotiques. Comparaison entre l’Italie, la région de Campanie, le LHC Naples 3 Sud.
| ATC2/antibacterial (J01) | DDD 1000 inhabitant/die | Comparison | Change % |
|---|---|---|---|
| Italy | 13.6 | Campany VS ITaly | 41.20% |
| Campany | 19.2 | LHC Naples 3 Sud VS Italy | 67.60% |
| LHC Naples 3 Sud | 22.8 | LHC Naples 3 Sud VS Campany | 18.80% |
Table 2.
Gross expenditure on antibiotic drugs-comparison Italy, Campania Region, LHC Naples 3 Sud.
Dépenses brutes en antibiotiques. Comparaison entre l’Italie, la région de Campanie, le LHC Naples 3 Sud.
| ATC/Antibacterial/J01 | Gross expenditure x 1000 inhabitant/die | Comparison | Change % |
|---|---|---|---|
| Italy | 23.7 | Campany VS Italy | 75.10% |
| Campany | 41.5 | LHC Naples 3 Sud VS Italy | 118.60% |
| LHC Naples 3 Sud | 51.8 | LHC Naples 3 Sud VS Campany | 24.80% |
Table 3.
ATC J01 Spending and Consumption Data in January/June 2022 LHC Naples 3 Sud.
ATC J01 - Données sur les dépenses et la consommation entre janvier et juin 2022 au LHC Naples 3 Sud.
| ATC2 | Gross expediture | Gross expenditure × 1000 inhabitant/die | Change % first semester 2022 VS first semester 2021, % | Number of packages | DDD 1000 inhabitant/die | Change % first semester 2022 VS first semester 2021, % |
|---|---|---|---|---|---|---|
| J01 | 8,930,153.15 | 51.8 | 14.60 | 1,090,767 | 22.8 | 24.00 |
Table 4.
Top 20 active ingredients in descending order of consumption, comparison Italy, Campania Region, LHC Naples 3 sud - January/June 2022.
Top 20 des ingrédients actifs par ordre décroissant de consommation. Comparaison Italie, Région Campanie, LHC Naples 3 sud entre janvier/juin 2022.
| Description | Italy |
Campany |
LHC Naples 3 Sud |
Change % |
||||
|---|---|---|---|---|---|---|---|---|
| DDD × 1000 inhabitant/die | Gross expenditure × 1000 inhabitant/die | DDD × 1000 inhabitant/die | Gross expenditure × 1000 inhabitant/die | DDD × 1000 inhabitant/die | Gross expenditure × 1000 inhabitant/die | LHC Naples 3 Sud VS Italy, % | LHC Naples 3 Sud VS Campany, % | |
| Amoxicillin and beta lactamase inhibitor | 4.80 | 6.54 | 6.07 | 9.20 | 7.02 | 10.95 | 46.10 | 15.50 |
| Azithromycin | 1.78 | 2.52 | 3.05 | 4.67 | 3.81 | 5.93 | 113.60 | 25.00 |
| Clarithromycin | 1.72 | 1.54 | 2.69 | 2.69 | 3.31 | 3.41 | 92.80 | 23.40 |
| Cefixime | 1.07 | 2.50 | 1.37 | 3.53 | 1.62 | 4.26 | 51.60 | 18.20 |
| Ciprofloxacin | 0.64 | 1.64 | 1.13 | 3.18 | 1.41 | 4.02 | 120.30 | 24.00 |
| Levofloxacin | 0.70 | 1.04 | 1.05 | 1.74 | 1.16 | 1.93 | 65.90 | 9.70 |
| Amoxicillin | 0.78 | 0.45 | 0.85 | 0.51 | 0.86 | 0.54 | 9.50 | 1.30 |
| Ceftriaxone | 0.20 | 2.40 | 0.50 | 6.64 | 0.64 | 8.68 | 219.10 | 27.20 |
| Cefditoren | 0.22 | 0.80 | 0.37 | 1.42 | 0.56 | 2.20 | 151.10 | 52.10 |
| Fosfomycin | 0.36 | 1.66 | 0.45 | 2.29 | 0.52 | 2.68 | 44.20 | 15.20 |
| Sulfamethoxazole and trimethoprim | 0.33 | 0.16 | 0.38 | 0.20 | 0.39 | 0.21 | 17.10 | 1.90 |
| Nitrofurantoin | 0.14 | 0.14 | 0.20 | 0.20 | 0.27 | 0.27 | 83.90 | 32.20 |
| Doxycycline | 0.19 | 0.07 | 0.17 | 0.07 | 0.19 | 0.08 | 0.30 | 9.40 |
| Roxithromycin | 0.04 | 0.09 | 0.12 | 0.30 | 0.16 | 0.42 | 347.10 | 34.50 |
| Limecycline | 0.12 | 0.11 | 0.16 | 0.15 | 0.15 | 0.14 | 20.10 | −6.70 |
| Prulifloxacin | 0.07 | 0.28 | 0.08 | 0.34 | 0.12 | 0.53 | 75.70 | 52.40 |
| Minocycline | 0.05 | 0.06 | 0.06 | 0.09 | 0.07 | 0.10 | 60.10 | 14.90 |
| Cefuroxime | 0.08 | 0.09 | 0.07 | 0.09 | 0.06 | 0.08 | −18.90 | −12.10 |
| Ceftazidime | 0.01 | 0.21 | 0.04 | 0.78 | 0.06 | 1.15 | 415.40 | 45.80 |
| Cefaclor | 0.04 | 0.07 | 0.05 | 0.10 | 0.05 | 0.11 | 37.70 | 12.70 |
Table 5.
LHC Naples 3 Sud - Top 20 active ingredients in descending order of consumption - January June 2022 vs January June 2021.
LHC Naples 3 Sud. Top 20 des actifs par ordre décroissant de consommation à janvier juin 2022 vs janvier juin 2021.
| Description | LHC Naples 3 Sud |
Change % 1st semester 2022 Vs 1st semester 2021 |
||
|---|---|---|---|---|
| DDD × 1000 inhabitant/die | Gross expenditure × 1000 inhabitant/die | DDD × 1000 inhabitant/die, % | Gross expenditure × 1000 inhabitant/die, % | |
| Amoxicillin and beta lactamase inhibitor | 7.02 | 10.95 | 25.00 | 26.00% |
| Azithromycin | 3.81 | 5.93 | 9.00 | 1.00 |
| Clarithromycin | 3.31 | 3.41 | 42.00 | 44.00 |
| Cefixime | 1.62 | 4.26 | 42.00 | 42.00 |
| Ciprofloxacin | 1.41 | 4.02 | 5.00 | 5.00 |
| Levofloxacin | 1.16 | 1.93 | 5.00 | 4.00 |
| Amoxicillin | 0.86 | 0.54 | 11.00 | 14.00 |
| Ceftriaxone | 0.64 | 8.68 | 5.00 | 4.00 |
| Cefditoren | 0.56 | 2.20 | 12.00 | 12.00 |
| Fosfomycin | 0.52 | 2.68 | −1.00 | −2.00 |
| Sulfamethoxazole and trimethoprim | 0.39 | 0.21 | 2.00 | 3.00 |
| Nitrofurantoin | 0.27 | 0.27 | −3.00 | −5.00 |
| Doxycycline | 0.19 | 0.08 | −3.00 | −3.00 |
| Roxithromycin | 0.16 | 0.42 | 40.00 | 40.00 |
| Limecycline | 0.15 | 0.14 | −24.00 | −24.00 |
| Prulifloxacin | 0.12 | 0.53 | −13.00 | −19.00 |
| Minocycline | 0.07 | 0.10 | −4.00 | −5.00 |
| Cefuroxime | 0.06 | 0.08 | −4.00 | −5.00 |
| Ceftazidime | 0.06 | 1.15 | 4.00 | 6.00 |
| Cefaclor | 0.05 | 0.11 | 50.00 | 46.00 |
Discussion
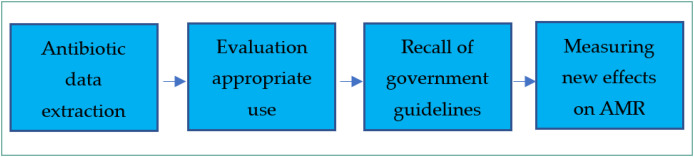
As shown in the five tables, the trend of antibiotic consumption in the first half of 2021 rose steadily, leading to an increase in pharmaceutical spending with potential repercussions on the phenomena of antibiotic resistance. In recent years, continuous worldwide awareness campaigns aimed at decreasing consumption and safeguarding the effectiveness of antimicrobials available on the market today have not had the desired results. WHO's new global action plan aims precisely to establish a tighter grip on regulations governing disproportionate prescribing of antibiotics by prescribers. Some studies in the literature show that the only way to combat antibiotic resistance is to limit their consumption to only clinical cases that require precise anti-infective intervention, thus reducing their prescription [26], [27], [28], [29]. In order to empower prescribers and patients on the antibiotics issue, it is necessary for each Health Authority to carry out more information campaigns so that all stakeholders concerned are informed of the effects to which extensive antibiotic resistance can lead. Large-scale projections show that deaths from infectious diseases, in the absence of viable therapeutic alternatives, will increase with no possibility of counteracting them with effective drugs. To counteract this critical issue, in the Campania Region and in particular at LHC Naples 3 Sud, multiple actions have been carried out, including new territorial organizations of physicians. The presence of Territorial Functional Aggregation (TFA) has precisely the purpose of create a territorial network among physicians, in order to create therapeutic continuity for patients, but especially to provide ongoing training for participants (General Practitioner GPs and Pediatricians of free choice PFCs). TFAs are the first health access sites where the problem of antibiotic overprescribing and future effects may occur by primary care physicians (GPs and PFCs). This allows continuous monitoring of prescriptions to assess the appropriateness of care and the status of microbial drug use. In addition, as the pandemic progresses, at LHC Naples 3 Sud it has been necessary to promote numerous educational events, such as mandatory conferences and conventions, specifically to help disseminating and raising awareness of the issue between all health care personnel. Moreover, distance learning events, such as webinars and online courses, have already been scheduled in the years 2023–2024. The issue of preventive health and socio-health needs a particular attention. In fact, not often health care professionals are familiar with the subject regarding sanitary disinfection, therefore it is necessary to reiterate the appropriate products for disinfecting and sterilizing people, environments, and health care equipment. Special courses of prevention are crucial to support caregivers and patients, to work safely. Furthermore, there are several strategic actions, which have been, activate, and one additional thing which can be improved is reporting by clinical and microbiology laboratories. Periodic reporting by public laboratories could be helpful to highlight and to immediately inform those affected by any definite bacterial infections detected, thus enabling the rapid adoption of appropriate measures with the right clinical therapy. For instance, the antibiotics prescription carried out on the basis of oropharyngeal swabs, antibiogram etc., it would always allow greater therapeutic appropriateness which would ensure not only the safety and efficacy of treatments, but also it would reduce the antibiotic resistance. With new European and global policies aimed at greater computerization of National Health Systems, telemedicine can take on a crucial role so that rapid communication between all health care personnel occurs. With a regional informatics platform available, even in an anonymous form, it would be a rapid dissemination of information, other than the integration of the results obtained by prevention and by the treatment measures shared by all providers. Certainly, a rapid identification of the source of bacterial infection would lead to targeted intervention on the transmission focus with high precision and accuracy, based on the spectrum of action and on the characteristics of the most appropriate antibiotic. With reference to the latter topic, many infections are contracted especially in hospital and care settings, demonstrating that the measures in place and already present are not always sufficient to eliminate or at least reduce them. Infections contracted in the care setting involve a patient who is already immunocompromised and thus more fragile and vulnerable to possible bacterial infections and superinfections. Most antibiotics are already ineffective for this type of patient, therefore the need for urgent intervention is higher. In addition, this same trend of overuse of antibiotics and development of antibiotic resistance is unfortunately also occurring in the veterinary field. A further suggestion could be the introduction of national recommendations aimed precisely at limiting this growing phenomenon. Observing official recommendations is certainly a way for all health care professionals to feel obliged to comply with precise regulations in both hospital and territorial settings (Fig. 1 ). The issue of antibiotic resistance is real in the Campania Region, and adequate information support is provided to raise awareness among all health care professionals, to pay the utmost prescriptive attention by increasing the appropriateness of treatments [30]. Many reports on antibiotic resistance are issued at the regional level, and there is always evidence of an increase that probably diminished due to pandemic emergencies [31].
Figure 1.
Process for evaluating the use of antibiotics to combat AMR.
Processus d’évaluation de l’utilisation des antibiotiques pour lutter contre la RAM.
In order to stop the antimicrobial resistance, in addition to all these regional and local Italian actions there are the directives issued by the WHO, which can be summarized in three main points [22]. Surveillance of multidrug-resistant microbes such as carbapenemase-resistant Enterobacteria should be developed in such centres, as well as the production of an annual report on healthcare-associated infections in HAI monitoring committees. The release of the annual regional report (in line with the NPCAR) and the growth of homogeneous regional procedures for intersectoral investigations in case of detection of resistant pathogenic bacteria in humans, animals and food products, should be issued continuously. The second aspect concerns the prevention of care-related infections: all hospitals and health care facilities must have a Committee for the Control of Care-Related Infections, a regional system for monitoring the consumption of hydroalcoholic hand hygiene products, and a training system for all health care professionals on the correct use of antibiotics. The third WHO's recommendation is about the promotion of the appropriate use of antibiotics in human and veterinary settings. In fact, the existence of a multidisciplinary team responsible for human Antimicrobial stewardship programs in all Health Authorities/Hospitals can help make a provision and implementation of initiatives aimed at verifying the adoption by farmers of the appropriate use of antibiotics, according to national guidelines.
Conclusions
In Europe, about 25,000 deaths per year come from infections due to antibiotic-resistant bacteria, and it is estimated that by 2050 deaths could attain 10 million worldwide (WHO source). The new Italian document “National Strategy and Plan to Combat Antibiotic Resistance 2022–2025” has been created with the aim of providing the country with strategic guidelines and operational directions, to try to stop the problem of antibiotic resistance, according to a multidisciplinary approach and a One Health vision. The Competent Italian Authority strengthened the Working Group (WG) aimed at struggling antimicrobial resistance, identifying scientific societies as the interlocutor capable of providing a synergistic and functional contribution to structuring the new vision of the NPCAR 2022–2025. In this context, the figure of the Hospital and Territorial Pharmacist, who has always been involved in the hospital setting within the committees of the Indian Ocean Commission (IOC) and in the territorial pharmaceutical monitoring of the appropriate use of antimicrobials (about 90% of the consumption takes place at a territorial level), has been identified as a key figure to provide a decisive contribution. The new document, the result of the contribution of numerous institutional interlocutors and scientific societies, will be divided into three macro-areas: the first to identify the national strategy, describing the areas that make it up, the actors who can intervene for its implementation and the general objectives; the second indicating, for each area, the specific objectives and actions; the third to focus on resistance to antibiotics, fungi, viruses and parasites, also aimed primarily at professionals. In this scenario, among the most effective interventions, there is the development of multidisciplinary antimicrobial stewardship programs. Also, as a result of the territorial strengthening of Proximity Networks (NRP funding), organizational and training interventions will be necessary in many specialist fields, such as home antibiotic therapy, which will see the Territorial Pharmaceutical Service playing a central role in the promotion of qualified information, in monitoring efficacy, appropriateness of use and prescription of medicinal products and in monitoring adherence through the interoperability of health data flows, also in light of the development of new distribution models such as home delivery of home therapy or telemonitoring. The assessment of these results will certainly involve decisive actions aimed at adherence to the directions dictated by international, national and regional guidelines. Probably, with the decrease of the COVID-19 pandemic waves, antibiotic resistance activities can also be fully resumed. Actions to monitor the proper use and prescription of antibiotics are essential to try to arrest a steadily growing phenomenon, and to prevent the spread of multidrug-resistant pathogens.
Ethical approval
Not applicable.
Authors contributions
F.F.: Conceptualization, Writing - original draft, Writing - review & editing, Validation; A.Z.: Conceptualization, Writing - original draft, Methodology; E.N.: Writing - review & editing, Validation; U.T.: Supervision, Validation; A.V.: Conceptualization, Writing - original draft, Validation.
Funding
No funding was received to conduct this study.
Disclosure of interest
The authors declare that they have no competing interest. The authors declare that the opinions expressed are of a personal nature and do not in any way commit the responsibility of the Administrations to which they belong.
Acknowledgments
None.
References
- 1.Munkholm L., Rubin O. The global governance of antimicrobial resistance: a cross-country study of alignment between the global action plan and national action plans. Global Health. 2020;16(1):109. doi: 10.1186/s12992-020-00639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Neill J [Internet]. Tackling drug-resistant infections globally: final report and recommendations. https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf.[updated 2016, May].
- 3.Naylor N.R., Atun R., Zhu N., Kulasabanathan K., Silva S., Chatterjee A., et al. Estimating the burden of antimicrobial resistance: a systematic literature review. Antimicrob Resist Infect Control. 2018;7:58. doi: 10.1186/s13756-018-0336-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Report to the Secretary-General of the United Nations [Internet]. UN Interagency Coordination Group on Antimicrobial Resistance: No Time to Wait: Securing the future from drug-resistant infections. https://www.who.int/publications/i/item/no-time-to-wait-securing-the-future-from-drug-resistant-infections.[updated 2019, April, 29].
- 5.World Bank. World Bank. License: Creative Commons Attribution CC BY 3.0 IGO; Washington, DC: 2017. Drug-Resistant Infections: A Threat to Our Economic Future.https://openknowledge.worldbank.org/handle/10986/26707 [Internet; updated 2017] [Google Scholar]
- 6.Patel J., Sridhar D. The pandemic legacy of antimicrobial resistance in the USA. Lancet. 2022;3(10):e726–e727. doi: 10.1016/S2666-5247(22)00227-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vitiello A., Ferrara F. A short focus, azithromycin in the treatment of respiratory viral infection COVID-19: efficacy or inefficacy? Immunol Res. 2022;70(1):129–133. doi: 10.1007/s12026-021-09244-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrara F., Mancaniello C., Varriale A., et al. COVID-19 mRNA Vaccines: A Retrospective Observational Pharmacovigilance Study. Clin Drug Investig. 2022;42(12):1065–1074. doi: 10.1007/s40261-022-01216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vitiello A., Porta R., Pianesi L., Ferrara F. COVID-19 pandemic: vaccine and new monoclonal antibodies, point of view. Ir J Med Sci. 2022;191(1):487–488. doi: 10.1007/s11845-021-02584-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ferrara F., Zovi A., Trama U., Vitiello A. Nirmatrelvir–remdesivir association for non-hospitalized adults with COVID-19, point of view. Inflammopharmacology. 2022;30(5):1927–1931. doi: 10.1007/s10787-022-01055-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization (WHO). https://www.who.int/publications/m/item/tripartite-amr-country-self-assessment-survey-(tracss)-2020-2021. [Accessed November 2022].
- 12.Ghosh S., Bornman C., Zafer M.M. Antimicrobial Resistance Threats in the emerging COVID-19 pandemic: where do we stand? J Infect Public Health. 2021;14(5):555–560. doi: 10.1016/j.jiph.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohmagari N. National Action Plan on Antimicrobial Resistance (AMR) 2016–2020 and relevant activities in Japan. Glob Health Med. 2019;1(2):71–77. doi: 10.35772/ghm.2019.01017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoffman S.J., Outterson K. What Will It Take to Address the Global Threat of Antibiotic Resistance? J Law Med Ethics. 2015;43(2):363–368. doi: 10.1111/jlme.12253. [DOI] [PubMed] [Google Scholar]
- 15.Padiyara P., Inoue H., Sprenger M. Global Governance Mechanisms to Address Antimicrobial Resistance. Infect Dis (Auckl) 2018;11 doi: 10.1177/1178633718767887. [1178633718767887] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rochford C., Sridhar D., Woods N., Saleh Z., Hartenstein L., et al. Global governance of antimicrobial resistance. Lancet. 2018;391(10134):1976–1978. doi: 10.1016/S0140-6736(18)31117-6. [DOI] [PubMed] [Google Scholar]
- 17.Rubin O. The glocalization of antimicrobial stewardship. Global Health. 2019;15:54. doi: 10.1186/s12992-019-0498-2. [Accessed December 2022] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rogers Van Katwyk S., Giubilini A., Kirchhelle C., Weldon I., Harrison M., et al. Exploring Models for an International Legal Agreement on the Global Antimicrobial Commons: Lessons from Climate Agreements. Health Care Anal. 2020 doi: 10.1007/s10728-019-00389-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lomazzi M., Moore M., Johnson A., Balasegaram M., Borisch B. Antimicrobial resistance - moving forward? BMC Public Health. 2019;19(1):858. doi: 10.1186/s12889-019-7173-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization (WHO), Food and Agriculture Organization of the United Nations (FAO), World Organization for Animal Health (OIE) 2019. Monitoring and evaluation of the global action plan on antimicrobial resistance Framework and recommended indicators.https://www.who.int/publications/i/item/monitoring-and-evaluation-of-the-global-action-plan-on-antimicrobial-resistance [Accessed December 2022] [Google Scholar]
- 21.Ruckert A., Fafard P., Hindmarch S., Morris A., Packer C., et al. Governing antimicrobial resistance: a narrative review of global governance mechanisms. J Public Health Policy. 2020;41(4):515–528. doi: 10.1057/s41271-020-00248-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO), Food and Agriculture Organization of the United Nations (FAO), World Organization for Animal Health (OIE) 2015. Global action plan on antimicrobial resistance.https://www.who.int/publications/i/item/9789241509763 [Accessed December 2022] [Google Scholar]
- 23.WHO, FAO, OIE . 2020. Global Database for Antimicrobial Resistance Country Self-Assessment.https://amrcountryprogress.org/ [Accessed December 2022] [Google Scholar]
- 24.Tsai F.J., Tipayamongkholgul M. Are countries’ self-reported assessments of their capacity for infectious disease control reliable? Associations among countries’ self-reported international health regulation 2005 capacity assessments and infectious disease control outcomes. BMC Public Health. 2020;20(1):282. doi: 10.1186/s12889-020-8359-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Italian Medicines Agency–AIFA. https://www.aifa.gov.it/web/guest/uso-dei-farmaci-in-italia. [Accessed Dicember 2022].
- 26.Zovi A., Musazzi U.M., D’Angelo C., Piacenza M.G., Vimercati S., et al. Medicines shortages and the perception of healthcare professionals working in hospitals: an Italian case study. J Interprofessional Educ Pract. 2021 doi: 10.1016/j.xjep.2021.100472. [DOI] [Google Scholar]
- 27.Crofts T.S., Gasparrini A.J., Dantas G. Next-generation approaches to understand and combat the antibiotic resistome. Nat Rev Microbiol. 2017;15(7):422–434. doi: 10.1038/nrmicro.2017.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wan F., Draz M.S., Gu M., Yu W., Ruan Z., et al. Novel strategy to combat antibiotic resistance: a sight into the combination of CRISPR/Cas9 and nanoparticles. Pharmaceutics. 2021;13(3):352. doi: 10.3390/pharmaceutics13030352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garvey M. Bacteriophages and the one health approach to combat multidrug resistance: is this the way? Antibiotics (Basel) 2020;9(7):414. doi: 10.3390/antibiotics9070414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Campania Region. Antibiotic Resistance and Care-Related Infections - Antibiotic Resistance and Care-Related Infections. https://regione.campania.it. [Accessed December 2022].
- 31.Vitiello A., La Porta R., Trama U., Ferrara F., Zovi A., et al. Pandemic COVID-19, an update of current status and new therapeutic strategies. Naunyn Schmiedebergs Arch Pharmacol. 2022;395(10):1159–1165. doi: 10.1007/s00210-022-02265-9. [DOI] [PubMed] [Google Scholar]