Abstract
目的
总结股前外侧嵌合穿支肌皮瓣制备方式及优化策略。
方法
回顾分析2015年6月—2021年12月收治的359例口腔肿瘤患者临床资料。男338例,女21例;年龄28~59岁,平均35.7岁。舌癌161例,牙龈癌132例,口颊癌66例。按照国际抗癌联盟(UICC)TNM 分期:T4N0M0 137例,T4N1M0 166例,T3N1M0 43例,T3N2M0 13例。病程1~12个月,平均6.3个月。肿瘤根治术后遗留软组织缺损范围为5.0 cm×4.0 cm~10.0 cm×7.5 cm,均采用游离股前外侧嵌合穿支肌皮瓣移植修复。肌皮瓣制备包括4个步骤:步骤1显露并分离穿支血管,穿支血管主要来自斜支和降支外侧支;步骤2分离穿支血管蒂主干并确定肌瓣血管蒂来源,包括斜支、降支外侧支和降支内侧支3个来源;步骤3确定制备肌瓣的来源,包括股外侧肌和股直肌2个来源;步骤4确定肌瓣制备形式,包括主干肌支型、主干远端型和主干侧边型3种形式。
结果
术中共切取359块游离股前外侧嵌合穿支肌皮瓣,股前外侧穿支均恒定存在。其中,皮瓣穿支血管来自斜支127例、降支外侧支232例,肌瓣血管蒂来自斜支94例、降支外侧支187例、降支内侧支78例,肌瓣来源于股外侧肌308例、股直肌51例,制备形式包括主干肌支型154例、主干远端型78例、主干侧边型127例。皮瓣切取范围为6.0 cm×4.0 cm~16.0 cm×8.0 cm,肌瓣范围5.0 cm×4.0 cm~9.0 cm×6.0 cm。316例穿支血管蒂动脉与甲状腺上动脉吻合,伴行静脉与甲状腺上静脉吻合;43例穿支血管蒂动脉与面动脉吻合,伴行静脉与面静脉吻合。术后6例发生血肿、4例发生血管危象,经急诊探查后7例成功挽救,1例皮瓣部分坏死(经换药后愈合),2例皮瓣完全坏死(采用胸大肌皮瓣补救)。患者均获随访,随访时间10~56个月,平均22.5个月。皮瓣外观满意,患者吞咽、语言功能恢复满意。供区仅遗留线性瘢痕,大腿功能未见明显影响。随访期间23例发生肿瘤局部复发,16例发生颈部淋巴结转移。患者3年生存率为38.2%(137/359)。
结论
在股前外侧嵌合穿支肌皮瓣制备关键环节做出灵活而有明确分类的选择,可以最大程度优化手术流程,增加手术安全性,降低手术难度。
Keywords: 股前外侧皮瓣, 肌皮瓣, 穿支皮瓣, 嵌合瓣, 口腔肿瘤
Abstract
Objective
To summarize the combination methods and optimization strategies of the harvest procedure of anterolateral thigh chimeric perforator myocutaneous flap.
Methods
A clinical data of 359 cases of oral cancer admitted between June 2015 and December 2021 was retrospectively analyzed. There were 338 males and 21 females with an average age of 35.7 years (range, 28-59 years). There were 161 cases of tongue cancer, 132 cases of gingival cancer, and 66 cases of buccal and oral cancer. According to the Union International Center of Cancer (UICC) TNM staging, there were 137 cases of T4N0M0, 166 cases of T4N1M0, 43 cases of T3N1M0, 13 cases of T3N2M0. The disease duration was 1-12 months (mean, 6.3 months). The soft tissue defects in size of 5.0 cm×4.0 cm to 10.0 cm×7.5 cm remained after radical resection were repaired with the free anterolateral thigh chimeric perforator myocutaneous flaps. The process of harvesting the myocutaneous flap was mainly divided into 4 steps. Step 1: exposing and separating the perforator vessels, which mainly came from the oblique branch and the lateral branch of the descending branch. Step 2: isolating the main trunk of the perforator vessel pedicle and determining the origin of the vascular pedicle of muscle flap, which was came from oblique branch, lateral branch of the descending branch, or medial branch of the descending branch. Step 3: determining the source of muscle flap, including lateral thigh muscle and rectus femoris muscle. Step 4: determining the harvest form of muscle flap, which included muscle branch type, main trunk distal type, and main trunk lateral type.
Results
The 359 free anterolateral thigh chimeric perforator myocutaneous flaps were harvested. In all cases, the anterolateral femoral perforator vessels existed. The perforator vascular pedicle of the flap came from the oblique branch in 127 cases and the lateral branch of the descending branch in 232 cases. The vascular pedicle of muscle flap originated from the oblique branch in 94 cases, the lateral branch of the descending branch in 187 cases, and the medial branch of the descending branch in 78 cases. The muscle flaps harvested from the lateral thigh muscle in 308 cases and the rectus femoris muscle in 51 cases. The harvest forms of muscle flaps included 154 cases of muscle branch type, 78 cases of main trunk distal type, and 127 cases of main trunk lateral type. The size of skin flaps ranged from 6.0 cm×4.0 cm to 16.0 cm×8.0 cm, and the size of muscle flaps range from 5.0 cm×4.0 cm to 9.0 cm×6.0 cm. In 316 cases, the perforating artery anastomosed with the superior thyroid artery, and the accompanying vein anastomosed with the superior thyroid vein. In 43 cases, the perforating artery anastomosed with the facial artery, and the accompanying vein anastomosed with the facial vein. After operation, the hematoma occurred in 6 cases and vascular crisis in 4 cases. Among them, 7 cases were successfully saved after emergency exploration, 1 case had partial necrosis of skin flap, which was healed after conservative dressing change, and 2 cases had complete necrosis of skin flap, which was repaired by pectoralis major myocutaneous flap. All patients were followed up 10-56 months (mean, 22.5 months). The appearance of the flap was satisfactory, and the swallowing and language functions were restored satisfactorily. Only linear scar left in the donor site with no significant effect on thigh function. During follow-up, 23 patients had local tumor recurrence and 16 patients had cervical lymph node metastasis. The 3-year survival rate was 38.2% (137/359).
Conclusion
The flexible and clear classification of the key points in the harvest process of anterolateral thigh chimeric perforator myocutaneous flap can optimize the protocol to the greatest extent, increase the safety of the operation, and reduce the difficulty of the operation.
Keywords: Anterolateral thigh flap, myocutaneous flap, perforator flap, chimeric flap, oral tumor
口腔肿瘤综合治疗中最重要的一环是肿瘤病灶扩大根治性切除,但往往会遗留较复杂缺损,包括软组织缺损以及口底深部腔隙残留[1]。此类缺损修复时,不仅要考虑覆盖软组织缺损,还需要填塞深部腔隙,以减少术后并发症的发生,降低手术失败风险[2-3]。随着显微外科技术的进步和肿瘤整形外科的发展,游离皮瓣移植修复已成为口腔肿瘤综合治疗中的重要内容,其中最常用股前外侧肌皮瓣修复[4]。传统股前外侧肌皮瓣切取形式为复合组织瓣,肌瓣与皮瓣紧密相连,调整灵活度低,容易卡压并出现坏死等并发症。与之相比,股前外侧嵌合穿支肌皮瓣最大优势是皮瓣与肌瓣相对独立且共用血管蒂,可减少供区损伤,尤其是可减少血管吻合数量,缩短手术时间,临床应用越来越广泛[5-6]。然而,嵌合穿支肌皮瓣制备相对困难,对术者技术要求较高,制定嵌合穿支肌皮瓣的规范制备流程,探讨不同组合方式及其适应证,对进一步优化治疗策略、提高疗效具有重要临床意义[7-9]。为此,我们回顾了2015年6月—2021年12月于湖南省肿瘤医院采用游离股前外侧嵌合穿支肌皮瓣治疗的359例口腔肿瘤患者临床资料,总结该肌皮瓣制备流程,分析不同组合方式疗效及适应证,以期优化手术策略。报告如下。
1. 临床资料
1.1. 一般资料
本组男338例,女21例;年龄28~59岁,平均35.7岁。舌癌161例,牙龈癌132例,口颊癌66例。按照国际抗癌联盟(UICC)TNM 分期:T4N0M0 137例,T4N1M0 166例,T3N1M0 43例,T3N2M0 13例。病程1~12个月,平均6.3个月。肿瘤根治术后遗留复杂软组织缺损,缺损范围为5.0 cm×4.0 cm~10.0 cm×7.5 cm,均合并口底深部腔隙缺损;同期行颈部淋巴结清扫术。
1.2. 皮瓣修复手术方案设计及方法
1.2.1. 股前外侧嵌合穿支肌皮瓣制备流程
股前外侧嵌合穿支肌皮瓣制备主要分为4个步骤。步骤1:显露并分离穿支血管,穿支血管主要来自斜支和降支外侧支。步骤2:分离穿支血管蒂主干并确定肌瓣血管蒂来源,包括斜支、降支外侧支和降支内侧支3个来源。步骤3:确定制备肌瓣的来源,包括股外侧肌和股直肌2个来源。步骤4:确定肌瓣制备形式,包括主干肌支型、主干远端型和主干侧边型3种形式。
1.2.2. 股前外侧嵌合穿支肌皮瓣制备方法
① 皮瓣设计及显露分离穿支血管:术前以髂髌线为轴线设计股前外侧嵌合穿支肌皮瓣。具体方法:常规触诊大腿前外侧区域,采用夹捏试验决定在组织量最丰富且松弛区域切取皮瓣,皮岛设计形式包括斜形和纵形。术中先按照皮瓣内侧设计线切开皮肤及皮下组织,从内向外在阔筋膜表面探查穿支血管,可来自斜支或降支外侧支。见图1a、b。
图 1.
Preparation of anterolateral thigh chimeric perforator myocutaneous flap
股前外侧嵌合穿支肌皮瓣制备示意图
a、b. 皮瓣穿支血管分别来自斜支及降支外侧支;c、d. 肌瓣血管蒂分别来自降支内侧支、降支外侧支;e、f. 制备股外侧肌嵌合穿支肌皮瓣、股直肌嵌合穿支肌皮瓣;g~i. 制备主干肌支型、主干远端型、主干侧边型肌瓣
a, b. The perforating branches of the flap were from the oblique branch and the lateral branch of the descending branch, respectively; c, d. The vascular pedicle of the muscle flap came from the medial branch and the lateral branch of the descending branch, respectively; e, f. The lateral thigh muscle chimeric perforator myocutaneous flap and the rectus femoris muscle chimeric perforator myocutaneous flap were prepared; g-i. Preparation of muscle branch type, main trunk distal type, and main trunk lateral type muscle flaps, respectively

② 分离穿支血管蒂主干并确定肌瓣血管蒂来源:确定目标穿支血管后,在股外侧肌内逆行分离穿支血管至旋股外侧动脉斜支或降支主干,进一步在血管蒂主干上显露分离适合的肌支制备肌瓣。肌瓣血管蒂来源基本与穿支血管蒂一致,可来自斜支、降支外侧支及降支内侧支。见图1c、d。
③ 确定肌瓣供区及制备形式:根据优势肌支进入的肌肉确定肌瓣供区,包括股外侧肌及股直肌。根据血管蒂主干发出的肌支大小、数量和位置灵活调整肌瓣制备形式,包括主干肌支型、主干远端型、主干侧边型。见图1e~i。
1.2.3. 股前外侧嵌合穿支肌皮瓣修复
将切取的股前外侧嵌合穿支肌皮瓣转移至口腔缺损区域,肌瓣填塞口底腔隙缺损。根据受区实际皮肤缺损范围和受区血管位置调整皮瓣摆放方向,首先将皮瓣皮缘与缺损边缘间断缝合固定,再完成皮瓣血管蒂与受区血管的吻合。确认皮瓣血运良好后留置2~3根负压引流管,创缘分层缝合。供区彻底止血后,留置1根负压引流管,逐层缝合皮下、皮肤,无菌敷料覆盖。
1.3. 术后处理
术后患者仰卧位卧床休息,避免颈部过度牵拉,常规对症支持治疗。术后第1天每小时观察皮瓣血运1次,第2天起每4小时观察1次。术后第1天即鼓励患者开始床上双下肢抬腿以及髋、膝、踝关节屈伸活动,预防下肢深静脉血栓形成;第3天开始指导患者下床活动。根据引流液情况,颈部引流管于术后7~14 d拔除,皮瓣供区引流管于术后5~8 d拔除。
2. 结果
2.1. 皮瓣制备情况
本组共切取359块游离股前外侧嵌合穿支肌皮瓣,股前外侧穿支均恒定存在。其中,皮瓣穿支血管来自斜支127例,斜支血管蒂平均长度7.4 cm(6.8~9.0 cm),动脉平均管径2.1 mm(1.8~3.2 mm),伴行静脉平均管径2.2 mm(1.7~3.0 mm);来自降支外侧支232例,降支血管蒂平均长度9.8 cm(8.7~11.3 cm),动脉平均管径2.4 mm(1.9~3.5 mm),伴行静脉平均管径2.5 mm(2.1~3.9 mm)。肌瓣血管蒂来自斜支94例、降支外侧支187例、降支内侧支78例,肌瓣来源于股外侧肌308例、股直肌51例,制备形式包括主干肌支型154例、主干远端型78例、主干侧边型127例。本组皮瓣切取范围为6.0 cm×4.0 cm~16.0 cm×8.0 cm,肌瓣范围5.0 cm×4.0 cm~9.0 cm×6.0 cm。316例穿支血管蒂动脉与甲状腺上动脉吻合,伴行静脉与甲状腺上静脉吻合;43例穿支血管蒂动脉与面动脉吻合,伴行静脉与面静脉吻合。
2.2. 临床疗效观察
术后6例发生血肿、4例发生血管危象。其中,7例经急诊探查后皮瓣顺利成活;1例皮瓣部分坏死,采用换药治疗后愈合;2例皮瓣完全坏死,采用胸大肌皮瓣补救。本组患者均获随访,随访时间10~56个月,平均22.5个月。皮瓣外观满意,患者吞咽、语言功能恢复满意。供区仅遗留线性瘢痕,大腿功能未见明显影响。
随访期间23例发生肿瘤局部复发,再次行肿瘤根治术并以带蒂胸大肌皮瓣移位修复。16例发生颈部淋巴结转移,其中同侧4例、对侧12例,再次行颈部淋巴结清扫术。本组患者3年生存率为38.2%(137/359)。死亡患者共222例,其中183例死于肿瘤复发,24例死于脑转移,15例死于肺转移。
3. 典型病例
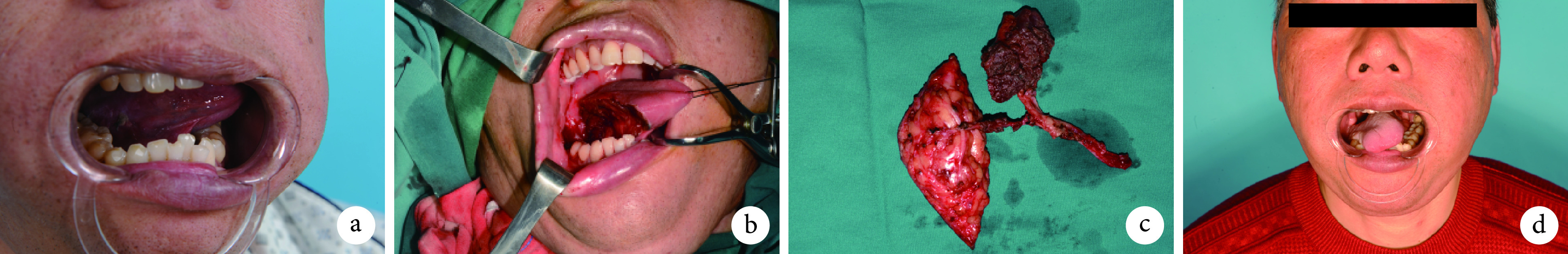
患者 男,47岁,因“右侧舌缘鳞状细胞癌(T3N1M0)”入院。入院后行颈部淋巴结清扫术+舌癌根治性切除术,术中设计切取右侧游离股前外侧嵌合穿支肌皮瓣修复遗留缺损。皮瓣穿支血管来自斜支,血管蒂长度为7.9 cm,动脉管径2.0 mm,伴行静脉平均管径2.5 mm(1.7~3.0 mm);肌瓣血管蒂来自斜支,肌瓣来源于股外侧肌,制备形式为主干远端型。皮瓣切取面积为10.0 cm×6.0 cm,肌瓣切取面积为7.0 cm×4.0 cm。穿支血管蒂动脉与甲状腺上动脉吻合,伴行静脉与甲状腺上静脉吻合。皮瓣供区直接拉拢缝合。术后皮瓣成活良好,24个月随访时未见明显并发症,口颊外形功能满意。见图2。
图 2.
A typical case
典型病例
a. 术前外观; b. 术中右侧舌癌肿瘤根治性切除后遗留缺损;c. 术中股前外侧嵌合穿支肌皮瓣制备完毕;d. 术后24个月外观
a. Preoperative appearance; b. The defects after radical resection of the right tongue tumor; c. The anterolateral thigh chimeric perforator musculocutaneous flap was prepared; d. The appearance at 24 months after operation
4. 讨论
口腔肿瘤根治性切除后往往会遗留广泛软组织缺损以及深部腔隙,而且位置不固定,涉及区域较广泛[10-11]。与传统复合肌皮瓣相比,嵌合穿支肌皮瓣有其独特优势,皮瓣和肌瓣拥有共同血管蒂,但未紧密固定在一起,彼此独立,从而具有理想的灵活性,方便组织瓣位置调整并修复不同区域缺损,安全性更高,效果更满意[12-13]。然而手术操作难度较大,对于术者临床经验和技术要求非常高[14-15]。我们基于359例临床应用经验,总结了股前外侧嵌合穿支肌皮瓣修复手术流程,最终确定该嵌合穿支肌皮瓣制备的4个关键步骤,每个步骤操作过程中可根据具体情况选择不同选项,以达到最优化组合方式,在增加手术安全性同时优化手术流程,缩短手术时间,降低手术难度。
股前外侧嵌合穿支肌皮瓣制备的第1个步骤是显露并分离穿支血管。术中发现穿支后切开阔筋膜,逆行分离穿支血管,通常只有两种解剖情况,来自斜支或者降支外侧支,目前尚无降支内侧支发出的股前外侧穿支血管报道[9]。皮瓣穿支血管选择需根据实际情况灵活应变[16],本组359例患者中优势股前外侧穿支血管有127例来自旋股外侧动脉斜支、232例来自降支外侧支。如果有较多穿支血管可供选择时,我们会优先选择来自降支的穿支血管,因为降支血管本身比斜支长,血管相对更粗。与穿支血管相比,肌瓣血管蒂来源血管选择较为灵活,如有较粗大肌支血管发自血管蒂主干,就可以选择其制备肌瓣;如没有显露较明显的肌支血管,也可以采用血管蒂主干远端或者血管蒂主干侧边制备肌瓣,同样可以确保肌瓣血运。同时,肌瓣摆放于腔隙中,很少会发生血管扭转、卡压情况,肌瓣本身抗感染能力强,发生坏死可能性非常小。虽然术后难以直接评估肌瓣血运,但是本组术后未发生明显肌瓣感染坏死和口底瘘情况,间接证明肌瓣血运良好。
进一步根据穿支血管蒂来源确定肌瓣的血管蒂来源,因此第2个步骤分离穿支血管蒂主干并确定肌瓣血管蒂来源过程中,要密切联系第1个步骤的实际情况,确定制备肌瓣血管蒂来源。如果穿支血管来自斜支,则优先制备斜支血管蒂主干为蒂的肌瓣;如果穿支血管来自于降支外侧支主干,肌瓣选择则较为灵活,既可以制备外侧支来源肌瓣,也可以制备内侧支来源肌瓣。相对来说,内侧支来源的肌瓣其血管蒂更长,肌瓣与皮瓣之间的灵活性大大增加。
制备嵌合穿支肌皮瓣的第3个步骤中需要确定肌瓣来源,一部分肌支会进入股直肌。虽然大部分情况下制备股外侧肌瓣,当有合适的粗大股直肌肌支存在时,直接制备中小组织量股直肌瓣操作更简单,而且股直肌瓣调整更灵活。在第4个步骤确定肌瓣具体形式过程中,尤为重要的是确保肌瓣血运可靠。大多数情况下会采用粗大主干肌支或者直接以主干远端制备肌瓣,血运较可靠。但在一些情况下,穿支血管发出之后血管蒂主干会逐渐变得非常细小,难以分辨粗大的肌支以及血管蒂主干远端分支,此时要尽量制备主干侧边型肌瓣。但主干侧边型肌瓣血管蒂较短,肌瓣摆放调整位置较困难,因此要谨慎选择该型肌瓣。
综上述,本课题组明确了股前外侧嵌合穿支肌皮瓣制备的流程和步骤,并且针对每一个步骤总结了手术方法的选择分类,有助于术者更好地判断和选择手术方式,降低手术难度,优化手术流程。
利益冲突 在课题研究和文章撰写过程中不存在利益冲突
伦理声明 研究方案经湖南省肿瘤医院伦理委员会批准[2022年科研快审(60)号]
作者贡献声明 宋达疆:论文撰写、数据整理及统计学分析;李赞:研究指导;章一新:论文修改
References
- 1.Hanasono MM, Matros E, Disa JJ Important aspects of head and neck reconstruction. Plast Reconstr Surg. 2014;134(6):968e–980e. doi: 10.1097/PRS.0000000000000722. [DOI] [PubMed] [Google Scholar]
- 2.宋达疆, 李赞, 周晓, 等 分叶股前外侧穿支皮瓣修复口腔复杂洞穿缺损. 中华整形外科杂志. 2019;35(10):978–985. doi: 10.3760/cma.j.issn.1009-4598.2019.10.006. [DOI] [Google Scholar]
- 3.Lyons A Current concepts in the management of oral cancer. Dent Update. 2006;33(9):538–539. doi: 10.12968/denu.2006.33.9.538. [DOI] [PubMed] [Google Scholar]
- 4.Bokhari WA, Wang SJ Tongue reconstruction: recent advances. Curr Opin Otolaryngol Head Neck Surg. 2007;15(4):202–207. doi: 10.1097/MOO.0b013e3281fbd406. [DOI] [PubMed] [Google Scholar]
- 5.Wei FC, Jain V, Celik N, et al Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg. 2002;109(7):2219–2226. doi: 10.1097/00006534-200206000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Wong CH, Wei FC Anterolateral thigh flap. Head Neck. 2010;32(4):529–540. doi: 10.1002/hed.21204. [DOI] [PubMed] [Google Scholar]
- 7.Ulas Bali Z, Keçeci Y, Pabuşcu Y, et al Anterolateral thigh flap design by using suprafascial course of the perforator. Ann Plast Surg. 2020;84(5):550–553. doi: 10.1097/SAP.0000000000002066. [DOI] [PubMed] [Google Scholar]
- 8.Zapata-Ospina A, Chen J, Tee R, et al Harvesting the anterolateral thigh flap with non-sizable perforators. J Plast Reconstr Aesthet Surg. 2021;74(5):1022–1030. doi: 10.1016/j.bjps.2020.10.063. [DOI] [PubMed] [Google Scholar]
- 9.Hsieh F, Leow OQY, Cheong CF, et al Musculoseptocutaneous perforator of anterolateral thigh flap: A clinical study. Plast Reconstr Surg. 2021;147(1):103e–110e. doi: 10.1097/PRS.0000000000007471. [DOI] [PubMed] [Google Scholar]
- 10.Chen SH, Kuo YL, Chang TY, et al. Use of anterolateral thigh flap and fibula flap in oncologic maxillary reconstruction: An algorithm approach. Ann Plast Surg, 2020, 84(1S Suppl 1): S17-S25.
- 11.Blackwell KE, Buchbinder D, Biller HF, et al Reconstruction of massive defects in the head and neck: the role of simultaneous distant and regional flaps. Head Neck. 1997;19(7):620–628. doi: 10.1002/(SICI)1097-0347(199710)19:7<620::AID-HED10>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 12.Koshima I Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast Reconstr Surg. 2000;105(7):2358–2360. doi: 10.1097/00006534-200006000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Koshima I, Yamamoto H, Hosoda M, et al Free combined composite flaps using the lateral circumflex femoral system for repair of massive defects of the head and neck regions: an introduction to the chimeric flap principle. Plast Reconstr Surg. 1993;92(3):411–420. doi: 10.1097/00006534-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Chong LSH, Tjahjono R, Eviston TJ, et al Dual chimeric innervated vastus lateralis free flap for single stage blink and midface reanimation. Head Neck. 2017;39(9):1894–1896. doi: 10.1002/hed.24795. [DOI] [PubMed] [Google Scholar]
- 15.Hasmat S, Low TH, Krishnan A, et al Chimeric vastus lateralis and anterolateral thigh flap for restoring facial defects and dynamic function following radical parotidectomy. Plast Reconstr Surg. 2019;144(5):853e–863e. doi: 10.1097/PRS.0000000000006183. [DOI] [PubMed] [Google Scholar]
- 16.Lu JC, Zelken J, Hsu CC, et al Algorithmic approach to anterolateral thigh flaps lacking suitable perforators in lower extremity reconstruction. Plast Reconstr Surg. 2015;135(5):1476–1485. doi: 10.1097/PRS.0000000000001168. [DOI] [PubMed] [Google Scholar]


