Abstract
The capability to monitor gait stability during everyday life could provide key information to guide clinical intervention to patients with lower limb disabilities. Whole body angular momentum (Lbody) is a convenient stability indicator for wearable motion capture systems. However, Lbody is costly to estimate, because it requires monitoring all major body segment using expensive sensor elements. In this study, we developed a simplified rigid body model by merging connected body segments to reduce the number of body segments, which need to be monitored. We demonstrated that the Lbody could be estimated by a seven-segment model accurately for both people with and without lower extremity amputation.
Keywords: angular momentum, gait stability, wearable system, rigid body model
Introduction
Gait stability is referred to as the capacity of continuous locomotion tasks in the presence of disturbances, such as new terrains, additional cognitive tasks, and contacts with the environment [1, 2]. Impaired gait stability is regarded as a contributor to life quality degradation and associated with underlying disease development, increased fall risk, and mobility loss [3]. Evaluation of gait stability is critical to track the impact of disease and quantify the effectiveness of rehabilitation [4, 5]. Although various clinical approaches [6] are available to evaluate gait stability through motor performance tests or specially designed questionnaires, these clinic-based assessments cannot represent the actual observed gait stability in daily life; as an example these stability indicators are not well correlated with the number of falls.[1]. One of the major speculations is that the clinical evaluation does not represent the everyday tasks well enough, so both clinicians and researchers are seeking gait stability metrics that are feasible to be monitored beyond clinics. However, making a gait stability monitor requires careful selection of stability indicators and effective system integration.
Wearable biomechanics sensors
The development of wearable sensors enables measurements of gait variables at a relatively low cost in a variety of environments. The most commonly adopted mechanical sensors include, accelerometers, inertial measurement units (IMU), force sensors, and pressure sensors [7]. Some wearable sensors are commercially available and used for daily step counting and fall detection, such as the Apple watch (Apple Inc., CA, US) and MOBILITY LAB (APDM wearable technologies Inc. OR, US).
IMU (often includes accelerometers, gyroscopes, and magnetometers) is the most adopted wearable sensor [8]. Despite its popularity, IMUs have their own limitations: 1) IMU only generates orientation, acceleration, angular velocity of a body segment. Repeated calibration is necessary for accurate position measurements to compensate sensor drifts or integration errors [9]; 2) IMUs have difficulty in detecting gait events accurately. Despite extensive efforts, there is still no reliable solution for detecting both heel strike and toe-off [10] for all populations; 3) although trivial compared with camera-based systems, the cost of each IMU block is still around $1,000 for gait analysis based on authors’ current knowledge; and 4) IMU sensors have to be calibrated at a known reference posture to avoid orientation bias between the IMU’s coordinates and the coordinates of human body.
Gait stability indicators
Existing gait stability indicators [1] are based on 1) practical measurements, 2) dynamic system theories, and 3) margin to unstable gait status. Practical measurements, such as walking speed, step length, and cadence, are easy to calculate and their correlation to gait stability are well documented [11, 12]. These practical gait measures, however, are evaluated on a step-by-step basis and therefore rely on accurate gait event detection. Furthermore, because these indicators do not reflect gait stability directly, it is not reliable to infer stability solely based on these measures.
Indicators from dynamic system theories quantify the capability of human to maintain stable status (continuous walking in most cases) under disturbances. Although these indicators, such as maximum Lyapunov exponent [13] and maximum Floquet multiplier [14], are theoretically sound, they can only be estimated reliably based on data collected from a continuous-consistent locomotion (often over 100 steps, seldom seen outside a lab) [14].
Another way to define stability is to find the minimum margin between the current status and an unstable status. By defining the event, when the centre of mass (COM) is out of the base of support (BOS), as unstable, margin of stability (MOS) is measured as the distance between the velocity adjusted COM and the boundary of the BOS [15]. MOS also relies on accurate gait event detection and foot location measurements.
Based on the observation that Lbody is well regulated during locomotion, whole-body angular momentum (Lbody) is also used as a practical measurement of stability; and its deviation from the usual/nominal values indicates unstable [16]. The Lbody has following advantages: 1) it does not rely on accurate gait event detection or foot position measurements, and 2) it can provide continuous information and has been used to a) extract information about behaviour of people with/without disability [17, 18] in walking and more challenging tasks, such as stair ambulating [19], turning [20], sloped walking [21], and coping with perturbation [22, 23], and b) guide the development of assistive devices to restore efficient walking behaviour during daily life [24, 25]. All these features make Lbody a good option for IMU based stability monitoring.
Challenges
Despite advantages of Lbody, the cost to measurement is relatively high. To calculate the Lbody, we need to estimate the angular momentum (Ls) for each major body segment. Because one IMU can only track one segment, a lot of IMU sensors are needed (for an example, the MVN Awinda system from Xsens includes 17 sensors). It is still too costly for a home device. Additionally, more sensors also mean higher demands on data transfer, processing, and storage, which increases the required computational resources. A high number of sensors can also be cumbersome to don and doff.
A straightforward way to reduce the number of IMU sensors is to reduce the number of monitored segments. However, removing segments from Lbody may reduce accuracy. One practical approach is to generate a simplified body model, which 1) includes fewer segments, and 2) reserve the inertial properties needed for Lbody calculation. However, no related studies are available.
Our solution
Here we developed a simplified model to calculate Lbody through segment merging. We estimated the key merging parameters on kinematic data collected from 10 able-bodied subjects through optimization. The merged model was also validated on data collected from three transfemoral amputees. The results demonstrate that a simplified model can be used to calculate the Lbody reliably on various subjects.
Methods
Merging of body segments
Because motions of adjacent segments are often correlated, it is reasonable to assume that some of the segments can be represented by a dominant one. A straightforward solution is to 1) merge a proximal segment and a distal segment, which are physically connected and 2) define the orientation of the merged segment in the reference posture. We expect that the LS of the merged segment equal the sum of LS of the two segments before merging.
A 12-segment rigid body model was used as the standard model, which includes: head, torso, right/left upper arms, right/left front arms, right/left thighs, right/left shanks, and right/left feet. The model is calibrated using the anatomical position as the reference posture.
Some rational assumptions were made to simplify the merging procedure. 1) the merged segment is connected to the adjacent body using the same joint as the original proximal segment, 2) angular velocity of the merged segment is the same as the original proximal segment, and 3) the merging procedure does not affect the mass distribution of the two merged segments. Based on these assumptions, we can claim that there is a constant bias between the merged segment and the original proximal segment (BMO); and we can use an IMU attached on the original proximal segment to track the merged segment after we remove the bias by adjusting the adopted reference posture.
To calculate LS of the merged segment, following information is needed: 1) COM of the merged segment (a 3X1 vector) and 2) the moment of inertia of the merged segment, Im (a 3X3 matrix). Because it is impractical to get and Im through optimization directly, further simplifications are needed. Here, we assumed that 1) the merging is conducted by fixing the joint angle, which connects the two segments; and 2) the orientation BMO is limited in the sagittal plane. These assumptions 1) made it easy to calculate and Im using known properties of the body segments, and 2) permitted the model to be optimized for the sagittal plane component of Lbody, which has the largest amplitude among its three dimensions.
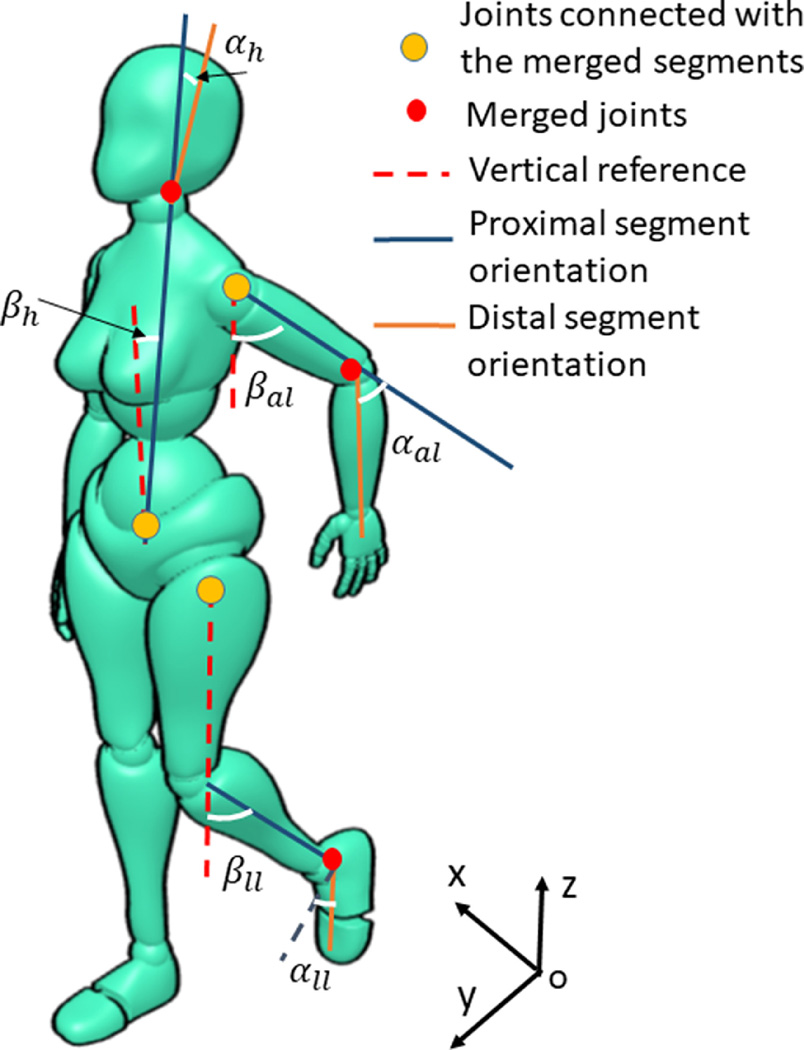
The Fig. 1 provided an illustrative example of the merging. The segments on the right side of the body remained in its anatomical position, and the segments on the left side were merged, as were the head and torso. Following the above discussion, the merging procedure was conducted using two steps. Step 1: defining a merged segment by fixing the joint between the two segments (a distal one and a proximal one) at a fixed angle, which is defined as the merging angle. Step 2: selecting an incline angle, , which can represent the BMO. This incline angle was materialized by rotating the merged segment on the reference posture around its proximal joint in the sagittal plane. Although two angles are both defined in the sagittal plane, compared with the, which is defined between two segments, the is defined between the proximal-distal axis of the proximal segment and the z axis. The coordinate system is also shown in Fig. 1.
Figure 1:
the merging procedure and definition of the merging parameters on the left side of the body and on the trunk and head.
Here, we developed the simplified model by merging forearms and upper arms, feet and shanks, and head and torso. The list of merging angles, incline angles, and their related segments are shown in Table 1. We will address the potential of further merging in the discussion.
Table 1:
the list of merging angles and incline angles used in the merging procedure.
| Merging Angle | Incline Angle | Proximal Segment | Distal Segment |
|---|---|---|---|
| Left upper arm | Left forearm | ||
| Right upper arm | Right forearm | ||
| Left shank | Left foot | ||
| Right shank | Right foot | ||
| Trunk | Head |
Calculate variables related to the merged segment
To adopt the simplified model, we 1) calculated the COM location and moments of inertia of the merged segments in the reference posture using the defined and; 2) calculated the Ls of the merged segments. Merging of forearm and upper arm is detailed in the supplementary file as an example.
Optimize the merging procedure based on experimental data
To decide the five merging and five incline angles, which are key parameters, we conducted an optimization based on data collected from able-bodied subjects using a brutal force optimization (see supplementary materials for details). The root mean square of the error compared with the reference Lbody, which was averaged for each stride, was used as the cost function. To reduce calculation burden, we made a further simplification that merging was conducted symmetrically by forcing:
| Eq. (1) |
To understand the influence of inter-subject variation, we also calculate subject-specific optimal merging parameters. The impact of inter-subject variation was quantified by the ratio of the increased cost function, which is defined as:, where Cj is the cost function for the subject j using that subject’s optimal merging parameters, and the as the cost function for the subject j using the merging parameters in Table 1. A model, which yields low fi for all participants, can be treated as a genetic model.
Human subjects and the experimental procedure
Following approved IRB protocols, the simplified model is constructed based on data collected from ten subjects without disabilities, who walked through a 15-meter walkway in three self-selected walking speeds, normal, slow, and fast. The simplified model was also validated using data collected from three transfemoral amputees, who wore a powered knee prosthesis. These participants underwent a similar protocol although they walked 1) on a 7m long walkway, 2) only at self-selected normal speed, and 3) with fall protection from an overhead rail. The demographic information about the participants and experimental procedure can be found in the supplementary materials.
Results
The optimal merging parameters were identified from data collected from all subjects without disabilities and shown in Table 2. For all the subjects without disabilities, fj is 0.07(mean) ± 0.06(standard diviation), which indicated that inter-subject variation had a limited impact.
Table 2:
optimized merging parameters based on data collected from able-body subjects.
| Merge Parameter | ||||||
|---|---|---|---|---|---|---|
| Optimal Value (°) | 50 | 0 | 10 | 0 | 170 | 9 |
The Lbody was also calculated for three transfemoral amputees. Although these participants wore a powered prosthetic knee, which was much heavier than their everyday prosthetic legs, the simplified model performed well with both subject-specific optimized merging parameter sets, and the merging parameters represented in Table 2. The ratio of the increased cost function was 0.04, 0.08, and 0.03 for the TF01, TF02, and TF03, respectively. The subject specific optimized parameters are included in the supplementary materials.
Discussion and Conclusion
This work focused on developing a simplified model, so fewer IMU sensors would be needed to measure whole-body angular momentum, Lbody, a gait stability indicator. The concept stemmed from the observation that the motion of adjacent segments is correlated, suggesting that a proxy of their combined contribution could accurately provide Lbody from the merged segments. Indeed, we demonstrated that Lbody could be calculated using a 7-segment model incorporating optimal merging parameters.
Although Eq. 1 puts additional limitation on the merging procedure, its impacts on the Ls are expected to be limited, due to the facts 1) the asymmetry inertial properties of the segments are considered when the rigid mode was defined before merging; and 2) the two thighs and shanks contribute a large portion of the Lbody and their kinematics are represented accurately in the simplified model. Because amputees’ uses a fixed ankle prosthesis, the amputees’ merging angles at the ankle shows a large variation (see the supplementary material), however, this variation’s impact is limited due to 1) inertia of the foot is much lower compared with the shank and 2) the foot motion follows the shank in most of the gait cycle. Good merging results on amputees, who showed an asymmetry gait, is aligned with our expectation.
We assessed the feasibility of further simplifying the model by considering: 1) merging the two arms with the torso/head 2) merging the feet, shanks, and thighs. Although the torso/head have a much larger inertial, the quick movement of the arms generates a significant Ls along the z-axis. This component could not be preserved after merging, so merging of the arm and torso/head should only be considered when the Lbody along the z-axis can be ignored.
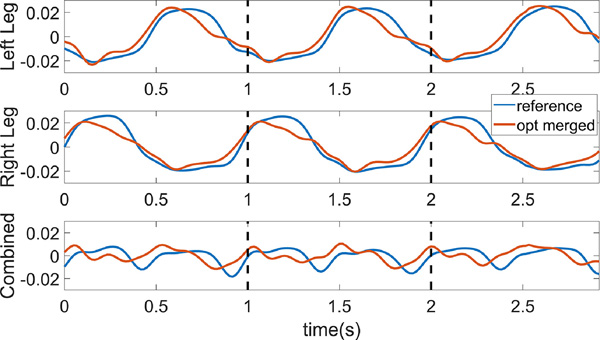
Finally, we merged segments within the legs (e.g., thigh, shank, and foot) as shown in Fig. 3. Although the Ls of the full leg segments, merged at the knee and ankle, still shared the general trends, the sum of the two legs deviated substantially from the reference. We were unable to overcome this problem, even with eliminating the symmetry limitation at the knee and hip, as posed in Eq. 1. Considering that the legs contribute about 70% of the Lbody, the current merging approach failed to generate a merged leg segment.
Figure 3:
The angular momentum of the left leg, right leg, and both legs in the sagittal plane. The blue line is from the reference model, the red line is from the optimized model with the thigh, shank, and foot merged together for each leg. The optimization is conducted for each leg separately.
The limitations of this research include a limited number of subjects and relies on an existing motion capture system to calculate all kinematic variables. In our future study, we plan to build a customized IMU system for Lbody calculation and test on more subjects with various age and level of disabilities.
In summary, our findings suggest that we were able to accurately calculate Lbody from a reduced number of segments. Through careful merging of adjacent segments, with optimized genetic parameters (i.e., merging and incline angles), we were able to accurately calculate Lbody with only a 7-segment model.
Supplementary Material
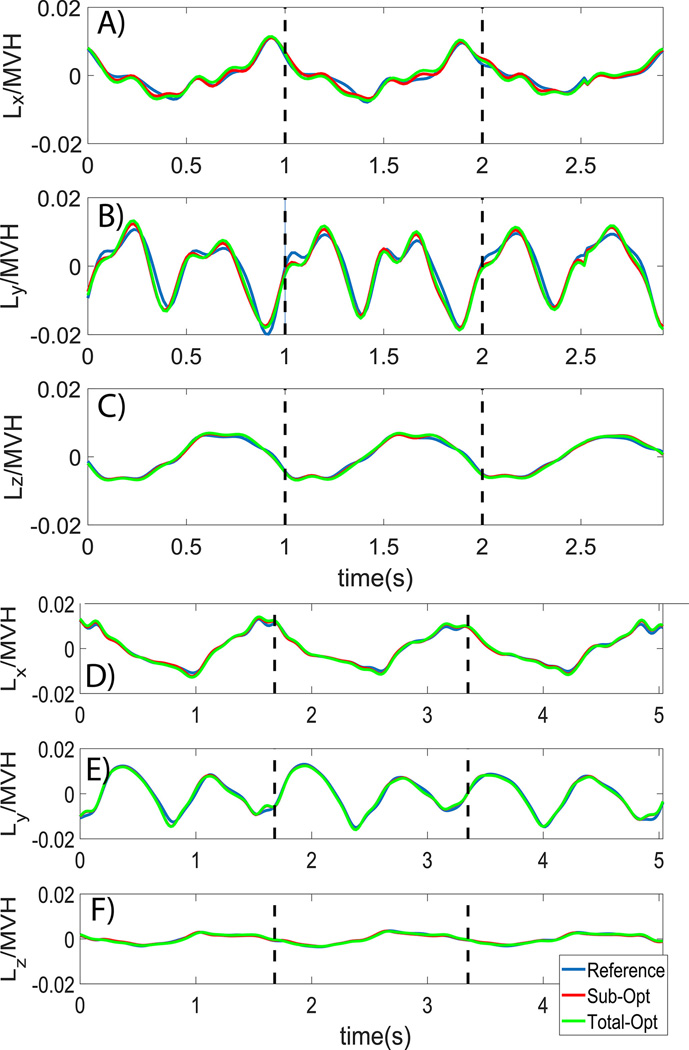
Figure 2.
A), B), and C) The normalized Lbody of AB05. Fig. D), E), and F) The normalized Lbody of TF01. The Lbody calculated from the reference model (blue line), simplified model with the subject-specific optimal merging parameters (red line), and simplified model with the merging parameters shown in Table 2. The steps started from the right heel strike and the dash black lines show the second and the third right heel strike. MVH is an abbreviation of body mass, walking velocity, and body height.
Highlights:
A simplified rigid body model to calculation of full body angular momentum
Only 7 IMU sensors are needed to calculate the full body angular momentum using this simplified model
The model was validated on both able-bodied subjects and transfemoral amputees
Funding
This work was supported by the National Institutes of Health [R01EB024570].
Footnotes
Ethical approval
This work was approved by the IRB at the University of North Carolina, Chapel Hill, with protocol number 13–2689.
Competing interests
None declared.
Declarations
The following additional information is required for submission. Please note that this form runs over two pages and failure to respond to these questions/statements will mean your submission will be returned to you. If you have nothing to declare in any of these categories then this should be stated.
Conflict of interest
All authors must disclose any financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work. Examples of potential conflicts of interest include employment, consultancies, stock ownership, honoraria, paid expert testimony, patent applications/registrations, and grants or other funding.
Conflicts of Interest
No conflicts for all authors.
Ethical Approval
Work on human beings that is submitted to Medical Engineering & Physics should comply with the principles laid down in the Declaration of Helsinki; Recommendations guiding physicians in biomedical research involving human subjects. Adopted by the 18th World Medical Assembly, Helsinki, Finland, June 1964, amended by the 29th World Medical Assembly, Tokyo, Japan, October 1975, the 35th World Medical Assembly, Venice, Italy, October 1983, and the 41st World Medical Assembly, Hong Kong, September 1989. You should include information as to whether the work has been approved by the appropriate ethical committees related to the institution(s) in which it was performed and that subjects gave informed consent to the work.
DOES YOUR STUDY INVOLVE HUMAN SUBJECTS? Please cross out whichever is not applicable.
Yes
If your study involves human subjects you MUST have obtained ethical approval.
Please state whether Ethical Approval was given, by whom and the relevant Judgement’s reference number
This work was approved by the IRB at the University of North Carolina, Chapel Hill, with protocol number 13–2689.
DOES YOUR STUDY INVOLVE ANIMAL SUBJECTS? Please cross out whichever is not applicable.
No
If your study involves animals you must declare that the work was carried out in accordance with your institution guidelines and, as appropriate, in accordance with the EU Directive 2010/63/EU. http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32010L0063
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference:
- 1.Hamacher D, et al. , Kinematic measures for assessing gait stability in elderly individuals: a systematic review. Journal of The Royal Society Interface, 2011. 8(65): p. 1682–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perera S, et al. , Gait speed predicts incident disability: a pooled analysis. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 2016. 71(1): p. 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salzman B, Gait and balance disorders in older adults. American family physician, 2010. 82(1): p. 61–68. [PubMed] [Google Scholar]
- 4.Williams SB, et al. , Feasibility and outcomes of a home-based exercise program on improving balance and gait stability in women with lower-limb osteoarthritis or rheumatoid arthritis: a pilot study. Archives of physical medicine and rehabilitation, 2010. 91(1): p. 106–114. [DOI] [PubMed] [Google Scholar]
- 5.Rochester L, et al. , A roadmap to inform development, validation and approval of digital mobility outcomes: the Mobilise-D approach. Digital Biomarkers, 2020. 4(1): p. 13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siragy T. and Nantel J, Quantifying Dynamic Balance in Young, Elderly and Parkinson’s Individuals: A Systematic Review. Front Aging Neurosci, 2018. 10: p. 387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang G, et al. , Review wearable sensing system for gait recognition. Cluster Computing, 2019. 22(2): p. 3021–3029. [Google Scholar]
- 8.Fong DT-P and Chan Y-Y, The use of wearable inertial motion sensors in human lower limb biomechanics studies: a systematic review. Sensors, 2010. 10(12): p. 11556–11565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teufl W, et al. , Towards inertial sensor based mobile gait analysis: Event-detection and spatio-temporal parameters. Sensors, 2019. 19(1): p. 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Panebianco GP, et al. , Analysis of the performance of 17 algorithms from a systematic review: Influence of sensor position, analysed variable and computational approach in gait timing estimation from IMU measurements. Gait & posture, 2018. 66: p. 76–82. [DOI] [PubMed] [Google Scholar]
- 11.Espy DD, et al. , Independent influence of gait speed and step length on stability and fall risk. Gait & posture, 2010. 32(3): p. 378–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young PMM and Dingwell JB, Voluntary changes in step width and step length during human walking affect dynamic margins of stability. Gait & posture, 2012. 36(2): p. 219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dingwell JB, et al. , Slower speeds in patients with diabetic neuropathy lead to improved local dynamic stability of continuous overground walking. J Biomech, 2000. 33(10): p. 1269–77. [DOI] [PubMed] [Google Scholar]
- 14.Bruijn SM, et al. , Statistical precision and sensitivity of measures of dynamic gait stability. Journal of neuroscience methods, 2009. 178(2): p. 327–333. [DOI] [PubMed] [Google Scholar]
- 15.Sivakumaran S, et al. , Relationship between margin of stability and deviations in spatiotemporal gait features in healthy young adults. Hum Mov Sci, 2018. 57: p. 366–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herr H. and Popovic M, Angular momentum in human walking. Journal of experimental biology, 2008. 211(4): p. 467–481. [DOI] [PubMed] [Google Scholar]
- 17.Kim D, Lewis CL, and Gill SV, The Effect of Obesity on Whole-body Angular Momentum During Steady-state Walking. Gait & Posture, 2022. [DOI] [PubMed] [Google Scholar]
- 18.Owaki D, et al. , Two-Week Rehabilitation with Auditory Biofeedback Prosthesis Reduces Whole Body Angular Momentum Range during Walking in Stroke Patients with Hemiplegia: A Randomized Controlled Trial. Brain sciences, 2021. 11(11): p. 1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Silverman AK, et al. , Whole-body angular momentum during stair ascent and descent. Gait & Posture, 2014. 39(4): p. 1109–1114. [DOI] [PubMed] [Google Scholar]
- 20.Nolasco LA, Silverman AK, and Gates DH, Whole-body and segment angular momentum during 90-degree turns. Gait & posture, 2019. 70: p. 12–19. [DOI] [PubMed] [Google Scholar]
- 21.Silverman AK, et al. , Whole-body angular momentum in incline and decline walking. Journal of biomechanics, 2012. 45(6): p. 965–971. [DOI] [PubMed] [Google Scholar]
- 22.Sheehan RC, et al. , Mediolateral angular momentum changes in persons with amputation during perturbed walking. Gait & posture, 2015. 41(3): p. 795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martelli D, et al. , Angular momentum during unexpected multidirectional perturbations delivered while walking. IEEE Transactions on Biomedical Engineering, 2013. 60(7): p. 1785–1795. [DOI] [PubMed] [Google Scholar]
- 24.D’Andrea S, et al. , Does use of a powered ankle-foot prosthesis restore whole-body angular momentum during walking at different speeds? Clinical Orthopaedics and Related Research®, 2014. 472(10): p. 3044–3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pickle NT, et al. , Whole-body angular momentum during sloped walking using passive and powered lower-limb prostheses. Journal of biomechanics, 2016. 49(14): p. 3397–3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.