Abstract
The present study investigated the influence of parent and child-driven effects on body image dissatisfaction during the COVID-19 pandemic. The moderating effect of parents’ acceptance of the COVID-19 pandemic and child gender were also investigated. The participants were 175 Canadian parents (mothers = 87.4%, fathers = 12%, unspecified = 0.6%) of children aged between 7 and 12 years old (M = 9.2; boys = 48.9%, girls = 51.1%). Two cohorts of parents were asked to complete a questionnaire in June 2020 and January 2021, respectively, followed by a second questionnaire approximately five months later. At both time points, the questionnaires addressed the parents’ body image dissatisfaction and acceptance of the COVID-19 pandemic. In addition, parents reported on their child’s body image dissatisfaction at both time points. Path analysis models were used to examine parent-driven and child-driven effects. Parents’ acceptance of the pandemic significantly moderated both parent and child-driven effects such that parents with low levels of acceptance were more likely to negatively influence, and be negatively influenced by, their perception of their child’s body image dissatisfaction. Child gender significantly moderated child-driven effects, as mothers’ perception of their son’s body image dissatisfaction predicted their own dissatisfaction over time. Our findings suggest that child-driven effects should be considered in future studies on body image dissatisfaction.
Keywords: Body image dissatisfaction, Acceptance, Parent-driven effects, Child-driven effects, COVID-19 pandemic
1. Introduction
Body image consists of the way in which we perceive our body, and the attitudes, beliefs, and thoughts we have towards it (Cuzzolaro, 2018). It varies from one individual to the next and is being composed of perceptual, cognitive, affective, and behavioural dimensions (Cash, 2004). Body image dissatisfaction, generally viewed as belonging to the affective dimension, is characterized by the discrepancy between how one perceives their body and their ideal body. Researchers have highlighted the early age at which children’s body image development begins by suggesting that children as young as four years old exhibit signs of weight biases and begin to show signs of body dissatisfaction a year later (Liechty, 2010, Worobey and Worobey, 2014).
Parents, as primary socializing agents in young children’s lives, play a pivotal role in children’s body image development. As suggested in Rodgers and Chabrol’s (2009) review, parents may place emphasis on, and become preoccupied with, their children’s body size and weight, which can bring children to place greater value upon their appearance. Parents may also model their own dissatisfaction through their behaviors (e.g., restricting food and making negative comments about their own body), which can subsequently be internalized by their children (Haines et al., 2008; Hart & Chow, 2020). For instance, Perez et al., 2018 conducted an experiment with mother-daughter dyads during which participants stood in front of a mirror and described what they liked and disliked about their body. The researchers found that the mothers’ comments about their own bodies predicted their daughters’ body-related comments, suggesting that young girls are likely to emulate how their mothers talk about their bodies. Therefore, by modeling specific behaviours and sharing thoughts and beliefs regarding their own and their children’s bodies, parents can influence children’s body image development both implicitly and explicitly.
1.1. Parent-child influences
Despite the consistent findings suggesting that parents have a strong influence on their children’s body image development, few studies have examined this relationship longitudinally or considered its dyadic nature, that is, the presence of both parent and child-driven effects. Parent-driven effects encompass parents’ characteristics and behaviors that are assumed to predict children’s development and are commonly found in the scientific literature (e.g., Solano-Pinto et al., 2021). However, researchers have begun emphasizing the importance of investigating child-driven effects as well, which suggest that children’s characteristics, or the parents’ perception of such, might influence parents’ outcomes (e.g., Barbot et al., 2014; Guimond et al., 2016).
Child-driven effects have rarely been considered when studying body image, and when they have, researchers have focused on adolescents. For instance, Hart and colleagues (2021) investigated whether mothers’ and daughters’ anti-fat attitudes influenced both their own and each other’s dietary restriction. Several maternal attitudes were found to influence the daughters’ dietary restriction and yet daughters’ dislike and negative attitudes towards fatness also influenced the mothers’ dietary restriction. These findings suggest the presence of a bidirectional relationship between parents’ and adolescents’ body image-related behaviours and attitudes and, therefore, the existence of both parent and child-driven effects.
Researchers have concluded that peak body image dissatisfaction is often reached during adolescence. It is expressed in a way that closely resembles that of an adult, which could make parents more easily aware of, and therefore impacted by, their adolescent’s body image dissatisfaction (Grogan, 2021). However, a similar bidirectional influence may be present in parent-child dyads with school-aged children. Indeed, although school-aged children’s body image dissatisfaction is less common and less known to parents (Hart et al., 2015), parents’ perception of this dissatisfaction could influence how parents feel about their own bodies. Similarly, a parent’s own body image dissatisfaction may predict how they perceive their child’s body image dissatisfaction. Hence, a parent’s perception of their child’s body image dissatisfaction, and whether it can impact or be impacted by a parent’s own body image dissatisfaction, is important to explore. This perception can not only impact the way a parent feels about themself, but also their dietary and body image-related parental practices, as well as their interactions with their child (Pedroso et al., 2018, Webb and Haycraft, 2019). Given that parents play such an important role in children’s body image development (Rodgers & Chabrol, 2009), dyadic effects could inform future research on the impact of child-driven influences on parental practices, subsequently informing parent-focused interventions aimed at improving body image dissatisfaction in families.
1.2. Gender differences
The influence of parental factors has also been found to vary based on both parent and child gender. At times, research has suggested that a parent’s body image dissatisfaction has the greatest impact on the body image development of their same-gendered children (Damiano et al., 2015). However, these findings are not always consistent. For instance, Solano-Pinto et al. (2021) found that mothers’ drive for thinness, body mass index (BMI), approach to change, and body image dissatisfaction significantly predicted sons’ body image dissatisfaction but not daughter’s dissatisfaction. These findings suggest that maternal variables were more impactful for sons than daughters. By contrast, none of the fathers’ variables significantly predicted sons’ nor daughters’ body image dissatisfaction. These results are inconsistent with another study that found that only perceived fathers’ value of thinness related to sons’ and daughters’ dieting behaviours (Field et al., 2001). However, there is still a lack of research closely investigating parental influences on boys, making it difficult to draw firm conclusions from this area of research. Hence, the role of parent and child gender in children’s body image development remains unclear.
Researchers have also found that girls tend to have greater body image dissatisfaction and weight concerns, as well as lower levels of self-esteem than boys, and may also receive more comments regarding their appearance within the family environment (Jongenelis et al., 2014, Phares et al., 2004). Gender differences have also been found in how girls and boys present their body image-related difficulties. For example, girls typically indicate wanting a thinner body, whereas boys are more likely to want to gain muscle and look fit (Sánchez et al., 2018, Ricciardelli and Williams, 2016). In addition, Ata et al., 2007 found differences regarding associated behaviors, as girls displayed more high-risk eating behaviors than boys (e.g., restrictive attitudes towards food). Given these different profiles, boys and girls may also be impacted differently by their parents’ behaviors and attitudes. In addition, parents may perceive their child’s body image dissatisfaction differently based on their child’s gender.
1.3. Acceptance of the COVID-19 pandemic
Given that family members in Canada have been spending a significant amount of time together in the last two years due to the strict social restrictions instated during the COVID-19 pandemic (e.g., stay-at-home order, social distancing, social gathering restrictions), and the greater prevalence of online schooling and working from home, it is likely that familial factors were very influential on children’s well-being during this period, including body image (e.g., Guimond et al., 2021). Liu and Doan (2020) mentioned the potential for stress contagion within families during the COVID-19 pandemic, that is, the spreading of pandemic-related stress into other spheres of family life. Through this process, parents and children alike may pass on their stressors to other family members, impacting the family’s well-being and functioning. It is therefore plausible that body image-related difficulties may be passed on similarly within families during this time.
The COVID-19 pandemic has also greatly impacted body image-related thoughts and behaviors (e.g., Flaudias et al., 2020). In general, researchers have found that individuals have become more concerned with their weight and less satisfied with their bodies (Vall-Roqué et al., 2021). Given that body image disturbances can lead to several adverse consequences, it is essential to investigate factors influencing body image development within the context of the COVID-19 pandemic, as both adults and children alike are experiencing this current rise in body image-related difficulties (Radhakrishnan et al., 2022, Robertson et al., 2021).
During the COVID-19 pandemic, researchers have also highlighted ways in which individuals have coped and exhibited resilience. Acceptance-based coping has been defined as adapting and accommodating to a life stressor that cannot be changed easily or that one has no control over (Carver et al., 1989). For example, an individual has accepted their circumstances when they no longer attempt to change the situation or avoid it, but rather choose to live with it (Polizzi et al., 2020). Learning to live with uncontrollable situations is considered an essential component of acceptance-based coping (Carver, 1997) and has been linked to children’s and parents’ positive mental health outcomes during the COVID-19 pandemic (Guimond et al., 2021, Gurvich et al., 2021). Acceptance has also been studied in the context of body acceptance, that is, accepting one’s body as it is, rather than trying to change it, despite any dissatisfaction toward it (Tylka, 2011). Body acceptance has been shown to lead to various positive body image outcomes (Prefit et al., 2020). Given the benefits of practicing acceptance on both psychological difficulties and negative body image-related thoughts and behaviors, parents who are more apt to adopt an accepting view of the COVID-19 pandemic may similarly experience improved well-being and body image outcomes within their family.
1.4. The current study
Although research has focused on parent-adolescent relationships given the more egalitarian relationship between parents and their children at that age, child-driven effects warrant investigation in children as well. Many school-aged children engage in body comparison and experience body image-related difficulties (Damiano et al., 2015, Dion et al., 2016). Children are also less likely to have experienced other major sources of body image influence such as social media and romantic relationships (Rodgers & Chabrol, 2009), making parents an important factor in their life. It is therefore crucial that we investigate parent-child effects on body image dissatisfaction at a younger age to further understand body image development within the familial context. Moreover, families have been spending more time together since the beginning of the COVID-19 pandemic due to the social restrictions put in place (Liu et al., 2021). In consequence, parents may be more perceptive of their child’s body image dissatisfaction and related behaviors and may be more influenced by such, though this may also vary based on how they are adapting to the pandemic (Aznar et al., 2021) and their child’s gender.
Therefore, the present study had three objectives. First, we sought to investigate the longitudinal impact of parent’s body image dissatisfaction on their perception of their child’s body image dissatisfaction (i.e., parent-driven effects) while investigating the impact of their perception on their own body image dissatisfaction (i.e., child-driven effects) during the COVID-19 pandemic. Given that past literature on the subject has mostly focused on parent effects on children’s body image, we hypothesized that parents’ body image dissatisfaction would negatively impact their perception of their child’s body image dissatisfaction over time (i.e., parent-driven effects). However, given preliminary evidence of child-driven effects in adolescence (Hart et al., 2021), we also believe that parents’ perception of their child’s body image dissatisfaction will negatively impact their own body image dissatisfaction over time (i.e., child-driven effects). Our second objective was to examine the moderating influence of parents’ acceptance of the COVID-19 pandemic. We hypothesized that parents who were less accepting of the pandemic would be more likely to perceive more body image concerns in their child (i.e., parent-driven effects). These parents’ body image dissatisfaction may also be negatively impacted by their perception of their child’s body image dissatisfaction (i.e., child-driven effects). Our final objective was to investigate child gender differences in the previous associations. Given the small proportion of fathers within our sample, we were unable to investigate the influence of parent gender and, thus, only examined the influence of child gender on mothers’ perception. Despite the mixed findings in the literature, we hypothesized that mothers would be more likely to influence, and be influenced by, their daughters’, rather than sons’, body image dissatisfaction.
2. Method
2.1. Participants
We collected data from two cohorts of parents (n = 175 parents of 247 children) over the course of a year during the COVID-19 pandemic. Throughout the year, restrictive measures and COVID-19 case numbers varied regularly, with each time point experiencing states of emergency and lockdown measures such as stay-at-home orders, indoor and outdoor social gathering restrictions, and sporadic business and school closures.
The first cohort (n = 99 parents) was recruited between June and July 2020, and the second (n = 76 parents) was recruited between January and February 2021. Parents completed a survey on behalf of themselves and their children at this initial time point and a follow-up survey at a second time point, approximately five months later. Children ranged from 7- to 12-years-old. For parents with several children (range = 2–4 children, n = 62), one child per family was randomly selected in order to address the interdependence within our sample. Therefore, our final sample at Time 1 comprised 175 Canadian parents (mothers = 87.4%, fathers = 12%, unspecified = 0.6%; of boys = 48.9%, of girls = 51.1%, M age = 9.2 years). At Time 2, 103 parents completed the survey (mothers = 86.4%, fathers = 12.6%, unspecified = 1%; of boys = 46.6%, of girls = 52.4%, unspecified = 1%, M age = 9 years). Of the 175 parents, 46.3% lived in Ontario, 43.4% lived in Quebec, 6.8% lived in another Canadian province or territory, and 3.4% did not respond. Although some parent respondents had shared custody of their children (14.9%), many lived with their children full-time (84.6%). Additional sociodemographic characteristics can be found in Table 1.
Table 1.
Sociodemographic Characteristics of the Sample.
| Characteristic | N | % |
|---|---|---|
| Child Gender Female Male No response |
89 85 1 |
51.1 48.9 0.6 |
| Child Age (in years) 7 8 9 10 11 12 No response |
43 32 20 24 26 28 2 |
24.6 18.3 11.4 13.7 14.9 16.0 1.1 |
| Child Ethnicity White Mixed race Asian Black Latino/a Other |
140 15 11 3 4 2 |
80 8.6 6.3 2.3 1.7 1.1 |
| Marital Status Married Common-law Separated/Divorced Single Other |
92 47 16 10 4 |
52.6 26.9 9.1 5.7 2.3 |
| Annual Income (CAD) Over 120,000 80,000–119,999 60,000–79,000 40,000–59,999 Less than 39,000 No response |
51 48 18 10 12 36 |
29.2 27.4 10.3 5.7 6.9 20.6 |
| Level of Education Elementary school High School Diploma College diploma University certificate Bachelor’s degree Master’s degree Doctoral degree Other No response |
2 14 49 9 48 29 14 3 7 |
1.7 5.1 27.4 1.1 16.6 8 8 1.7 4 |
Independent sample t-tests were conducted to ensure the equivalence of our two cohorts of participants. The cohorts did not differ in terms of child age, t(171) = −0.76, p = 0.45, child BMI, t(154) = −0.39, p = 0.70, parent’s perception of child body image dissatisfaction at Time 1, t(173) = −0.66, p = 0.51, and at Time 2, t(173) = −0.20, p = 0.84, and parent body image dissatisfaction at Time 1, t(173) = 0.97, p = 0.34, and Time 2, t(173) = 0.65, p = 0.54. However, parents in the first cohort reported significantly lower levels of acceptance of the COVID-19 pandemic (M = 2.7, SD = 1.2) than in the second cohort (M = 3.1, SD = 0.8, t(173) = −2.27, p = 0.02). Given this minor difference, we combined the cohorts into one sample. However, the models were compared between cohorts when examining parent’s acceptance of the COVID-19 pandemic.
2.2. Procedure and ethical considerations
The study was approved by [university masked for review]. Prior to parents’ completion of the surveys at both time points, informed written consent was obtained. Parents were recruited via social media platforms, email threads, and advertisements in Canadian newspapers. One parent from each family completed a survey regarding their own and their children’s body image dissatisfaction. The survey could be completed in French or English, based on the parent’s preference. Parents were contacted approximately five months later, requesting that they complete a similar survey at that second time point. The surveys took an average of 25 min to complete at both time points, and parents received a $5 gift card to a Canadian bookstore upon completion of each survey.
2.3. Measures
2.3.1. Parent body image dissatisfaction
Parents’ body image dissatisfaction was measured using eight items (e.g., “Have you been afraid that you might become fat (or fatter)?”; “Has feeling full (e.g., after eating a large meal) made you feel fat?”) from the Body Shape Questionnaire Short-Version (BSQ-8 C; Welch et al., 2012). Each item was scored on a four-point Likert scale ranging from 1 (never) to 4 (always). Good test-retest reliability (r = 0.95) was found in a sample of undergraduate students, and high convergent validity has been reported (Welch et al., 2012). In the current sample, internal consistency was high at both time points (α = 0.92, 0.89). The item responses were averaged to obtain a total score of body image dissatisfaction in parents at Time 1 (M = 1.95, SD = 0.8) and at Time 2 (M = 2.02, SD = 0.7), where higher scores represent greater body image dissatisfaction.
2.3.2. Child body image dissatisfaction
The parent’s perception of their child’s body image dissatisfaction was measured with five items (e.g., “My child likes his/her body”; “My child would like to be thinner”) from the Child Body Esteem Scale (Coyne et al., 2016), a parent-reported questionnaire. Responses were on a four-point Likert scale ranging from 1 (never) to 4 (always). Previous researchers have found that the scale has good internal consistency (α = 0.79; Coyne et al., 2016), and similar results were obtained in our sample at both time points (α = 0.77, 0.81). Certain items were reverse coded, and all item responses were averaged to create a total score of perceived child body image dissatisfaction at Time 1 (M = 1.6, SD = 0.5) and at Time 2 (M = 1.7, SD = 0.4), where higher scores represent greater perceived body image dissatisfaction.
2.3.3. Parent’s acceptance of the COVID-19 pandemic
The parent’s acceptance of the COVID-19 pandemic was measured using a single item (“I’ve been learning to live with it”) taken from the Brief COPE Inventory (Carver, 1997), a validated measure of various coping strategies. This item was chosen given its high loading on the acceptance-based coping factor of the original scale, its clear understanding by a wide variety of populations, and its adequacy to account for the long-lasting nature of the COVID-19 pandemic and the need to learn to live with the situation (Carver, 1997, Carver et al., 1989). This item was scored on a four-point Likert scale ranging from 1 (never) to 4 (always), which provided us with the parent’s score of acceptance of the COVID-19 pandemic at Time 1 (M = 2.9, SD = 1).
2.4. Control variables
Parents reported on their children’s gender, age, weight, and height. Child BMI was calculated using the estimation of the child’s weight and height.
2.5. Plan of analysis
As preliminary analyses, we conducted correlations to examine bivariate associations between study variables and repeated-measure ANOVAs to assess children’s age and gender differences in perceived body image dissatisfaction, as well as changes in parents’ perception of their own and their child’s body image dissatisfaction over time. Next, we performed path analysis models within a structural equation modeling framework to investigate our hypotheses using Mplus v8 (Muthén & Muthén, 2017). Longitudinal path analyses allowed us to investigate the stability of parents’ perception of their own and their child’s body image dissatisfaction from Time 1 to Time 2. It also permits us to examine the bidirectional influence between parents’ own body image dissatisfaction and their perception of their child’s body image dissatisfaction.
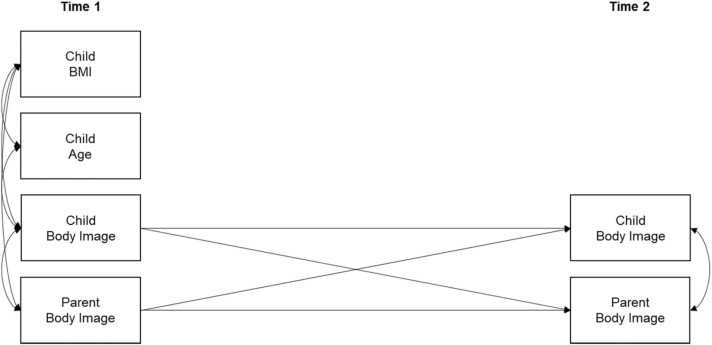
To assess our first study objective, we conducted a path analysis model to examine child-driven and parent-driven effects (see Fig. 1). Parents’ perception of their own and their child’s body image dissatisfaction were entered as independent variables at Time 1 and as outcome variables at Time 2, with the child’s BMI and age as covariates at Time 1. A significant association between parents’ body image dissatisfaction at Time 1 and their perception of their child’s body image dissatisfaction at Time 2 would represent a parent-driven effect whereas the opposite would suggest a child-driven effect.
Fig. 1.
Measurement Model of Path Analysis Model Between Parent’s Perception of Parent-Child Body Image Dissatisfaction, Note. N = 175.
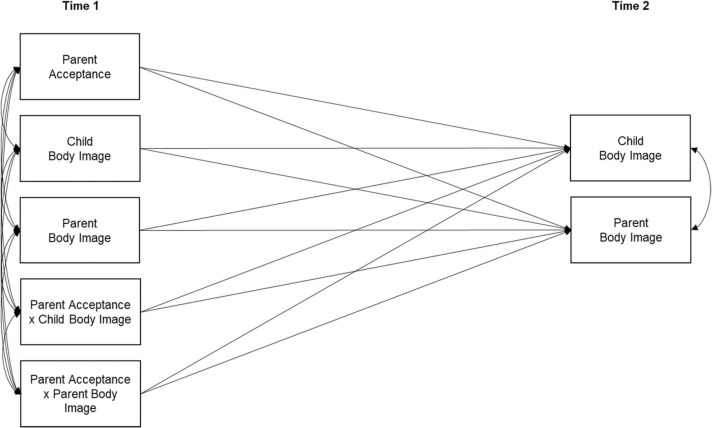
To assess our second objective, we created two interaction terms: one between parent’s acceptance of the pandemic and parent’s body image dissatisfaction and one between parent’s acceptance of the pandemic and perceived child’s body image dissatisfaction. We then included parent’s acceptance of the pandemic and both interaction terms in a path analysis model to test the hypothesis that parent’s acceptance of the pandemic moderates the associations between parent’s perception of their own and their child’s body image dissatisfaction over time (see Fig. 2).
Fig. 2.
Measurement Model of Path Analysis with Parent Acceptance as a Moderator of Parent Perceptions of Parent-Child Body Image Dissatisfaction, Note. N = 175.
To interpret significant interaction effects, we followed the procedure recommended by Holmbeck (2002). A statistically significant association between parents’ own body image dissatisfaction at Time 1 and their perception of their child’s body image dissatisfaction at Time 2 (i.e., parent-driven effects) was examined when the moderator (i.e., parent’s acceptance of the pandemic) was at 1 standard deviation (SD) above the mean and when the moderator was at 1 SD below the mean. The same procedure was used for child-driven effects (i.e., a statistically significant association between parents’ perception of their child’s body image dissatisfaction at Time 1 and their own body image dissatisfaction at Time 2). This allowed us to understand in which context the moderator influenced parent and child-driven effects. Since parents’ acceptance of the pandemic varied significantly between cohorts, we specified equality constraints and performed a chi-square difference test to make sure that results would generalize to both cohorts.
To assess our third objective, we selected mothers only (n = 153), we specified equality constraints, and we used a chi-square difference test to examine child gender differences between constrained and unconstrained path analysis models (mothers-sons: n = 73, mothers-daughters: n = 79). Within all our models, child’s age and BMI were included as covariates, and all variables, including the interaction terms, were grand mean centered, except for child gender.
We had a range of.03–55% of data missing amongst our variables (M = 29.6%). Little’s MCAR test indicated that data were missing completely at random, χ 2(5) = 8.36, p = .14. We used multiple imputations to address our item- and wave-level missing data using the Statistical Package for Social Sciences, v. 28 (SPSS) to impute 25 independent datasets. As this study is part of a larger longitudinal study, variables that were included within our imputation model are known predictors of body image dissatisfaction, including participants’ sociodemographic characteristics (i.e., ethnicity, socio-economic status), mental health variables (i.e., parent’s and child’s depression and social anxiety) and parent’s perception of their own and their child’s body image dissatisfaction. To account for the potential impact of multiple time points of data collection, we included data collected at both time points for variables likely to have variability over time. Next, we used the imputed datasets to test our models using maximum likelihood estimation and averaged all parameter estimates over them. Multiple imputations have been shown to produce accurate and unbiased estimates in cases with up to 80% of data missing completely at random (Lee & Huber, 2021).
3. Results
3.1. Preliminary analyses
A 2 (gender) by 6 (age) repeated measures ANOVA was conducted with parent’s perception of child body image dissatisfaction as the dependent variable and time as the repeated measure. We included child’s age in the preliminary analyses given its known influence on children’s body image development (e.g., O'Dea & Caputi, 2001). A separate repeated measures ANOVA was performed to investigate changes in parent’s body image dissatisfaction over time. For parents’ perception of their child’s body image dissatisfaction, there was a statistically significant main effect for age, F(6, 340) = 2.56, p = 0.02, where perceived child’s body image dissatisfaction increased with age (d = 0.34). There was no significant effect of child gender, F(2, 340) = 0.69, p = 0.50, nor a significant change in parents’ perception of their own and their child’s body image dissatisfaction over time (respectively, F(1, 340) = 0.53, p = 0.47; F(1, 340) = 0.48, p = 0.27). Hence, perceived child’s body dissatisfaction was similar between boys and girls, and both parents’ perception of their own and their child’s body dissatisfaction were stable from Time 1 to Time 2.
Bivariate correlations, means, and standard deviations for the study variables are present in Table 2. At both time points, there was a significant positive correlation between parent’s body image dissatisfaction and perceived child’s body image dissatisfaction. Child’s BMI was also positively correlated with perceived child body image dissatisfaction at both time points. Age was correlated with perceived child’s body image dissatisfaction at Time 2. Hence, heavier, and older children were less likely to be perceived as satisfied with their bodies. Parent’s acceptance of the COVID-19 pandemic was negatively correlated with parent’s body image dissatisfaction. Hence, parents who had greater levels of acceptance of the COVID-19 pandemic were more likely to be satisfied with their bodies.
Table 2.
Correlations, Means, and Standard Deviations.
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Child Age | − | ||||||
| 2. Child BMI Time 1 |
.20** | − | |||||
| [.04,.34] | |||||||
| 3. Child Body Image Time 1 | .15 | .41** | − | ||||
| [− .00,.29] | [.27,.53] | ||||||
| 4. Child Body Image Time 2 | .17* | .36** | .61** | − | |||
| [.02,.31] | [.22,.49] | [.51,.70] | |||||
| 5. Parent Body Image Time 1 | -.04 | .14 | .17* | .11 | − | ||
| [− .19,.11] | [− .02,.29] | [.02,.31] | [− .04,.25] | ||||
| 6. Parent Body Image Time 2 | -.12 | .08 | .17* | .16* | .27** | − | |
| [− .26,.03] | [− .08,.23] | [.02,.31] | [.01,.30] | [.12,.40] | |||
| 7. Parent Acceptance Time 1 |
.06 | -.01 | -.06 | -.10 | -.13 | -.20** | |
| [− .09,.21] | [− .16,.15] | [− .20,.09] | [− .25,.05] | [− .27,.02] | [− .34, − .05] | − | |
| M (SD) | 9.2 (1.8) | 18.4 (4.4) | 1.6 (0.5) | 1.7 (0.4) | 2 (0.5) | 2 (0.5) | 2.9 (1) |
Note. N = 175. 95% Confidence intervals are presented in brackets. Child and parent body image dissatisfaction and parent acceptance were rated on a scale from 1 (never) to 4 (always). * p < .05, * * p < .01, two-tailed.
3.2. Main analyses
In the first path analysis model, as can be seen in Table 3, parent’s perception of their own and their child’s body image dissatisfaction were stable from Time 1 to Time 2 (respectively, B =.61, SE =.05, p < .001; B =.25, SE =.07, p < .001). Parent’s perception of their child’s body image dissatisfaction was correlated with child BMI (B =.42, SE =.07, p < .001) and age (B =.15, SE =.07, p = .05) at Time 1, where heavier and older children seem to be perceived as less satisfied with their appearance by their parent. Parent’s perception of their own and their child’s body image dissatisfaction were also correlated at Time 1 (B =.17, SE =.07, p = .03). However, the child-driven and parent-driven effects were not statistically significant (B =.13, SE =.07, p = .08; B =.01, SE =.06, p = .88).
Table 3.
Path Analyses Results of Parent and Child-Driven Effects of Body Image Dissatisfaction.
| Parameters | Estimate (SE) | p |
|---|---|---|
| Stability Effects | ||
| C1→C2 | .61 (.05) | < .001 |
| P1→P2 | .25 (.07) | < .001 |
| Parent and Child-Driven Effects | ||
| C1→P2 | .13 (.07) | .08 |
| P1→C2 | .01 (.06) | .88 |
Note. N = 175. The estimates are standardized regression coefficients. C1 = Perceived child’s body image dissatisfaction at Time 1; C2 = Perceived child’s body image dissatisfaction at Time 2; P1 = Parent’s body image dissatisfaction at Time 1; P2 = Parent’s body image dissatisfaction at Time 2. Child’s gender and BMI were included as covariates at Time 1.
In the second path analysis model, as can be seen in Table 4, when examining the moderating role of parent’s acceptance of the COVID-19 pandemic on the child-driven effect, the interaction term was statistically significant (B = −.16, SE =.07, p = .02). Hence, in families where the parent was displaying low levels of acceptance of the pandemic, parent’s perception of their child’s body dissatisfaction was more likely to influence the parent’s own body image dissatisfaction over time. When examining the moderating role of parent’s acceptance of the pandemic on the parent-driven effect, the interaction term was also statistically significant (B = −.13, SE =.06, p = .03). Hence, parents that were displaying low levels of acceptance of the COVID-19 pandemic were more likely to report on their child’s body image dissatisfaction in accordance with their own body image dissatisfaction. The results did not significantly differ between cohorts, χ 2(23) = 32.32, p = 0.09.
Table 4.
Path Analysis Results of Parent and Child-Driven Effects of Body Image Dissatisfaction with Parent Acceptance of the COVID-19 Pandemic as a Moderator.
| Parameters | Estimate (SE) | p |
|---|---|---|
| Stability Effects | ||
| C1→C2 | .61 (.05) | < .001 |
| P1→P2 | .25 (.07) | < .001 |
| Parent and Child-Driven Effects | ||
| C1→P2 | .13 (.07) | .08 |
| P1→C2 | .01 (.06) | .88 |
| Interaction effects | ||
| Parent acceptance Parent acceptance × C1→P2 |
-.15 (.07) -.16 (.07) |
.04 .02 |
| Parent acceptance × P1→C2 | -.13 (.06) | .03 |
Note. N = 175. The estimates are standardized regression coefficients. C1 = Perceived child’s body image dissatisfaction at Time 1; C2 = Perceived child’s body image dissatisfaction at Time 2; P1 = Parent’s body image dissatisfaction at Time 1; P2 = Parent’s body image dissatisfaction at Time 2. Interaction effects were tested within a model that included all the main effects.
In the third path analysis model, gender differences were investigated. When examining mothers’ perception of their daughter, both parent-driven and child-driven effects were not statistically significant (respectively, B = −.02, SE =.10, p = .87; B = −.12, SE =.11, p = .28). However, when considering mothers’ perception of their sons, the child-driven effect was statistically significant (B =.25, SE =.11, p = .02). Hence, mothers’ perception of their child’s body image dissatisfaction is more likely to influence mothers’ own body image dissatisfaction over time when that child is a boy, rather than a girl, χ 2(1) = 5.56, p = 0.02.
4. Discussion
We sought to investigate the longitudinal and bidirectional influence between parents’ perception of their own and their child’s body image dissatisfaction during the COVID-19 pandemic. In addition, this study examined the moderating influence of parents’ acceptance of the pandemic, as well as child gender differences, on parent and child-driven effects.
In terms of stability effects, parents’ perception of their own and their child’s body image dissatisfaction remained stable over time. These findings are in line with previous longitudinal research indicating that both adults’ and adolescents’ body image satisfaction typically remains stable over several years (Archibald et al., 1999, Rozin et al., 2001). Although fewer studies have followed children’s body image dissatisfaction longitudinally, existing research suggests that children’s body image satisfaction and related thoughts and behaviors may vary throughout development, but that changes generally occur over several years (e.g., McCabe & Ricciardelli, 2005). Therefore, it is plausible that parents’ reports of their child’s body image dissatisfaction would remain relatively stable over time.
Neither parent-driven nor child-driven effects emerged as statistically significant in our first model. These findings were not in line with our hypotheses, as we expected both parent-driven and child-driven effects to emerge. Generally, researchers have investigated and found significant parent-driven effects, in which parents’ body image-related attitudes and behaviors impact children’s body image dissatisfaction (e.g., Ventura & Birch, 2008). However, when examining the moderating role of parent’s acceptance of the COVID-19 pandemic, both child-driven and parent-driven effects were significant. The findings confirmed our hypotheses as we posited that acceptance of the pandemic would impact parent and child-driven effects and may serve as a protective factor against intra-familial transmission of body image dissatisfaction.
Parent’s acceptance of the COVID-19 pandemic was found to be positive and helpful for children’s well-being in previous studies (e.g., Guimond et al., 2021). In the context of our findings, acceptance of the pandemic may have prevented parents’ body image from deteriorating during the pandemic. We also found that parents with greater acceptance of the pandemic had lower levels of body image dissatisfaction. These parents may adopt an accepting attitude in other spheres of their life, potentially leaving them more satisfied with their bodies. Consequently, these parents may have been less likely to manifest body image dissatisfaction, which positively impacted their perception of their child’s body image as well. They also may have been less influenced by their perception of their child, having psychological safeguards in place to support their child without being impacted.
We also note that there was a significant main effect of parent acceptance of the COVID-19 pandemic. Therefore, it is possible that the effect of the pandemic on family well-being was so important that parent-driven and child-driven effects in the first model were nonsignificant consequently. It could be worth investigating these main effects to see whether they would be significant in another context, as the pandemic likely played an important role in families’ adjustment, especially for parents with low levels of acceptance.
Interestingly, when considering child gender within our model, mothers’ perception of their sons’, but not daughters’, body image dissatisfaction significantly predicted their own body image dissatisfaction over time. These results contradicted our hypothesis, given that past research has suggested that parents might have the greatest influence on their gender-matched child (e.g., McCabe & Ricciardelli, 2005). However, research on the subject remains inconclusive, given that many studies have provided mixed findings. In fact, several studies have emphasized that boys’ body image may be most influenced by their mothers (e.g., Rodgers et al., 2019). Indeed, mothers’ body image dissatisfaction may have been influenced by their perception of their sons for several reasons. Mothers who perceived their daughters to have greater body image dissatisfaction, which is a widespread phenomenon (Phares et al., 2004), may have implicitly or explicitly compensated by putting protective practices in place such as avoiding body-related comments (Carbonneau et al., 2021). These measures may have inadvertently improved mothers’ own body image dissatisfaction over time. However, given that society has often neglected body image disturbances in males (Strother et al., 2012), when mothers were aware of their son’s body image-related difficulties, they may have given these unexpected struggles more thought, consequently making them more aware of their own body image-related difficulties. That being said, this is one of the first studies, to our knowledge, to investigate body image-related gender differences within parent and child-driven effects, and, therefore, further research is necessary to replicate our findings.
Within this study, child and parent-driven effects emerged when considering parents’ acceptance of the pandemic, whereas solely child-driven effects were significant when mothers reported on their sons. This was surprising as existing research on the subject has suggested that parent-driven effects prevail in parent-adolescent dyads (Hart and Chow, 2020, Hart et al., 2021). In the current study, our child-driven effects might be explained by our use of parents’ perception of their child’s body image dissatisfaction, which may have biased our findings. However, our findings suggest that, in certain contexts, parents’ body image dissatisfaction may be influenced by their perception of their child’s body image dissatisfaction, offering preliminary evidence of child-driven transmission of body image dissatisfaction. These findings also highlight that parents’ perception of their child’s body image dissatisfaction might be important to consider in future research investigating the intra-familial transmission of body image dissatisfaction.
Child-driven effects may emerge through a variety of mechanisms present in the household. With the rise in body image-related disturbances and children’s lack of extra-familial social contact during the early periods of the COVID-19 pandemic, children may have begun to disclose their body image-related difficulties more often to their parents. Existing research suggests that exposure to, or involvement in, negative appearance-related communication (e.g., discussions about fear of weight gain and body comparison) is significantly related to body image dissatisfaction and disordered eating (Cruwys et al., 2016, Sharpe et al., 2013). Therefore, if children confided in their parents regarding their struggles with their body image, parents in specific contexts (i.e., mothers of sons and parents with low levels of acceptance of the pandemic) would have not only been more aware of their child’s body image dissatisfaction, but potentially of their own insecurities as well. They may also have subsequently participated in appearance-related communication with their children, impacting their own body image dissatisfaction over time. Alternatively, parents may have had greater opportunities to observe body image concerns in their children due to the increased time spent together.
Parents may also have engaged in body comparison with their child, whether consciously or not, by comparing their own body to their child’s body. Thus, based on their perception, parents may have felt worse about their own body after comparing themselves. Alternatively, parents who felt that their child, with whom they likely share physical traits, was dissatisfied with parts of their bodies, may have reflected this dissatisfaction onto their own bodies, believing that they should have those insecurities as well. Similarly, in the presence of low levels of acceptance of the pandemic, parents may project their own biases onto their children, making their perception of their child’s body image dissatisfaction a reflection of their own assumptions. A similar mechanism may occur for mothers of sons. For instance, parents may have been more likely to perceive their older children, with higher BMIs, as experiencing higher levels of body image dissatisfaction due to their own personal biases or concerns towards their child’s body, rather than how the child behaves. Ultimately, our findings suggest that parents’ own body image dissatisfaction might be impacted by their perception of their child’s body image dissatisfaction over time, in specific contexts, during the COVID-19 pandemic. However, further research is necessary outside the context of the pandemic, and with child reports of body image dissatisfaction, to further understand child-driven effects and their modes of transmission within families.
4.1. Strengths and limitations
This study provides a novel perspective on how parents might influence, and be influenced by, their perception of their child’s body image dissatisfaction during the COVID-19 pandemic and how parental acceptance of the pandemic might serve as a protective factor. Our longitudinal design and consideration of both parent and child-driven effects are important strengths of this study. However, there are several limitations to consider. First, as mentioned above, we used parent reports of child’s body image dissatisfaction, which may have biased our findings. In the future, it would be helpful to collect data from both children’s and parents’ perspective. Second, our measures of body image dissatisfaction were limited to the whole body, rather than addressing one’s body composition and specific phenotypic characteristics (e.g., hair color, lips shape). These components would be important to consider, given that they are an integral part of one’s body image (Grogan, 2021). Third, the lack of diversity within our sample prevented us from comparing different sociodemographic groups. This would be a valuable avenue for future research to understand how family members belonging to different sociodemographic backgrounds (e.g., socioeconomic status, ethnicity) may experience body image dissatisfaction and influence each other.
A fourth limitation is our considerable amount of missing data, which was accounted for with multiple imputations. Fifth, we were also unable to investigate fathers’ perception of their child’s body image because of an insufficient number of father-respondents, which would be valuable in furthering our understanding of the role of parent gender in perceived body image dissatisfaction. In addition, it could be worthwhile to investigate whether gender-related parent-driven and child-driven effects might vary based on whether children live in a dual-parent or single-parent household. Next, we used a single-item measure of acceptance of the COVID-19 pandemic, which prevented us from investigating the use of acceptance more broadly during the pandemic. Acceptance-based coping and body acceptance have both been considered helpful strategies for improving body image satisfaction (Pearson et al., 2012, Prefit et al., 2020). Future research would benefit from using more elaborate measures of acceptance to investigate the role of different forms of acceptance in the intra-familial transmission of body image dissatisfaction. Investigating additional coping strategies could also be of future interest. Sixth, we also had a relatively high attrition rate (i.e., 26%), which may have been due to pandemic stressors that families were facing. However, our attrition rates were consistent between cohorts. Finally, although we collected data over the course of an entire year, these results can only draw short-term conclusions. Future research might consider following families as the COVID-19 pandemic evolves (e.g., when uncertainty and stressors are still present, but families are spending more time apart) and post-pandemic.
4.2. Conclusions
This study was a first step in understanding how parents’ perception of their child’s body image dissatisfaction might impact their own body image dissatisfaction over time during the COVID-19 pandemic. It appears that parents’ body image dissatisfaction may be influenced by their perception of their child’s body image dissatisfaction. More specifically, when parents perceive their child to be struggling with their body image satisfaction, they seem more likely themselves to develop struggles in specific contexts over time (i.e., when parents display low levels of acceptance of the pandemic and mothers of sons). The acceptance of the COVID-19 pandemic may serve as a protective factor against child-driven effects, but also against parents’ potential transmission of body image issues to their children through their perception of their child’s body image dissatisfaction. These findings can help inform future prevention and intervention programs aimed at optimizing families’ body image during health-related crises. Encouraging parents to accept difficult extraneous circumstances may be a helpful first step. Future research would be required to extend this finding to the implementation of coping strategies, such as acceptance-based coping, into family-oriented programs. In addition, it may be necessary to address different familial mechanisms depending on the parent and the child gender.
CRediT authorship contribution statement
Olivia Gardam: Conceptualization, Data curation, Supervision, Writing – original draft, Writing – review & editing. Laila Kokenberg-Gallant: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. Sahej Kaur: Formal analysis, Writing – original draft, Writing – review & editing. Elizabeth St. John: Data curation, Methodology, Project administration, Writing – original draft, Writing – review & editing. Noémie Carbonneau: Validation, Writing – original draft, Writing – review & editing. Fanny-Alexandra Guimond: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Writing - original draft, Writing – review & editing.
Conflicts of interest
The authors have no relevant financial or non-financial interests to disclose.
Acknowledgements
We would like to thank the participating families.
Data Availability
Data will be made available on request.
References
- Archibald A.B., Graber J.A., Brooks-Gunn J. Associations among parent-adolescent relationships, pubertal growth, dieting, and body image in young adolescent girls: A short-term longitudinal study. Journal of Research on Adolescence. 1999;9(4):395–415. doi: 10.1207/s15327795jra0904_2. [DOI] [Google Scholar]
- Ata R.N., Ludden A.B., Lally M.M. The effects of gender and family, friend, and media influences on eating behaviors and body image during adolescence. Journal of Youth and Adolescence. 2007;36:1024–1037. doi: 10.1007/s10964-006-9159-x. [DOI] [Google Scholar]
- Aznar A., Sowden P.T., Bayless S., Ross K.M., Warhurst A., Pachi D. Home-schooling during COVID-19 lockdown: Effects of coping style, home space, and everyday creativity on stress and home-schooling outcomes. Couple and Family Psychology: Research and Practice. 2021;10(4):294–312. doi: 10.31234/osf.io/dzh8m. [DOI] [Google Scholar]
- Barbot B., Crossman E., Hunter S.R., Grigorenko E.L., Luthar S.S. Reciprocal influences between maternal parenting and child adjustment in a high-risk population: A 5-year cross-lagged analysis of bidirectional effects. American Journal of Orthopsychiatry. 2014;84(5):567–580. doi: 10.1037/ort0000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbonneau N., Hamilton L., Musher-Eizenman D.R. From dieting to delight: Parenting strategies to promote children’s positive body image and healthy relationship with food. Canadian Psychology/Psychologie Canadienne. 2021;62(2):204–212. doi: 10.1037/cap0000274. [DOI] [Google Scholar]
- Carver C.S. You want to measure coping but your protocol’ too long: Consider the brief cope. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Cash T.F. Body image: Past, present, and future. Body Image. 2004;1:1–5. doi: 10.1016/S1740-1445(03)00011-1. [DOI] [PubMed] [Google Scholar]
- Coyne S.M., Linder J.R., Rasmussen E.E., Nelson D.A., Birkbeck V. Pretty as a princess: Longitudinal effects of engagement with Disney princesses on gender stereotypes, body esteem, and prosocial behavior in children. Child Development. 2016;87(6):1909–1925. doi: 10.1111/cdev.12569. [DOI] [PubMed] [Google Scholar]
- Cruwys T., Leverington C.T., Sheldon A.M. An experimental investigation of the consequences and social functions of fat talk in friendship groups. International Journal of Eating Disorders. 2016;49(1):84–91. doi: 10.1002/eat.22446. [DOI] [PubMed] [Google Scholar]
- Cuzzolaro M. In: Body image, eating, and weight: A guide to assessment, treatment, and prevention. Cuzzolaro M., Fassino S., editors. Springer; 2018. Body schema and body image: History and controversies; pp. 1–24. [Google Scholar]
- Damiano S.R., Gregg K.J., Spiel E.C., McLean S.A., Wertheim E.H., Paxton S.J. Relationships between body size attitudes and body image of 4-year-old boys and girls, and attitudes of their fathers and mothers. Journal of Eating Disorders. 2015;3(16):1–10. doi: 10.1186/s40337-015-0048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dion J., Haines J., Vachon P., Plouffe J., Laberge L., Perron M., McDuff P., Kalinova E., Leone M. Correlates of body dissatisfaction in children. The Journal of Pediatrics. 2016;171:202–207. doi: 10.1016/j.jpeds.2015.12.045. [DOI] [PubMed] [Google Scholar]
- Field A.E., Camargo C.A., Taylor C.B., Berkey C.S., Roberts S.B., Colditz G.A. Peer, parent, and media influences on the development of weight concerns and frequent dieting among preadolescent and adolescent girls and boys. Pediatrics. 2001;107(1):54–60. doi: 10.1542/peds.107.1.54. [DOI] [PubMed] [Google Scholar]
- Flaudias V., Iceta S., Zerhouni O., Rodgers R.F., Billieux J., Llorca P., Boudesseul J., De Chazeron I., Romo L., Maurage P., Samalin L., Bègue L., Naassila M., Brousse G., Guillaume S. COVID-19 pandemic lockdown and problematic eating behaviors in a student population. Journal of Behavioral Addictions. 2020;9(3):826–835. doi: 10.1556/2006.2020.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grogan S. Body image: Understanding body dissatisfaction in men, women and children. Fourth ed. Routledge; 2021. [Google Scholar]
- Guimond F., Laursen B., Vitaro F., Brendgen M., Dionne G., Boivin M. Associations between mother–child relationship quality and adolescent adjustment. International Journal of Behavioral Development. 2016;40(3):196–204. doi: 10.1177/0165025415620059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guimond F., Smith J., Vitoroulis I., Aucoin P., St. John E., Gardam O., MacLachlan M. The role of online schooling, screen-based activities, and parent coping in Canadian children’s COVID-19-Related trauma and anxiety symptoms. Psychiatry International. 2021;2:180–190. doi: 10.3390/psychiatryint2020014. [DOI] [Google Scholar]
- Gurvich C., Thomas N., Thomas E.H., Hudaib A., Sood L., Fabiatos K., Sutton K., Isaacs A., Arunogiri S., Sharp G., Kulkarni J. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. International Journal of Social Psychiatry. 2021;67(5):540–549. doi: 10.1177/0020764020961790. [DOI] [PubMed] [Google Scholar]
- Haines J., Neumark-Sztainer D., Hannan P., Robinson-O′Brien R. Child versus parent report of parental influences on children's weight-related attitudes and behaviors. Journal of Pediatric Psychology. 2008;33(7):783–788. doi: 10.1093/jpepsy/jsn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart E., Chow C.M. “I just don’t want to be fat!”: Body talk, body dissatisfaction, and eating disorder symptoms in mother–adolescent girl dyads. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2020;25(5):1235–1242. doi: 10.1007/s40519-019-00756-y. [DOI] [PubMed] [Google Scholar]
- Hart E., Tan C.C., Chow C.M. Anti-fat attitudes and dietary restraint within mother-daughter dyads: An actor-partner interdependence model (APIM) analysis. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2021;26(5):1417–1426. doi: 10.1007/s40519-020-00949-w. [DOI] [PubMed] [Google Scholar]
- Hart L.M., Damiano S.R., Cornell C., Paxton S.J. What parents know and want to learn about healthy eating and body image in preschool children: A triangulated qualitative study with parents and early childhood professionals. BMC Public Health. 2015;15(1) doi: 10.1186/s12889-015-1865-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck G.N. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27(1):87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Jongenelis M.I., Byrne S.M., Pettigrew S. Self-objectification, body image disturbance, and eating disorder symptoms in young Australian children. Body Image. 2014;11(3):290–302. doi: 10.1016/j.bodyim.2014.04.002. [DOI] [PubMed] [Google Scholar]
- Lee J.H., Huber J.C., Jr. Evaluation of multiple imputation with large proportions of missing data: How much is too much? Iranian Journal of Public Health. 2021;50(7):1372–1380. doi: 10.18502/ijph.v50i7.6626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liechty J.M. Body image distortion and three types of weight loss behaviors among Nonoverweight girls in the United States. Journal of Adolescent Health. 2010;47(2):176–182. doi: 10.1016/j.jadohealth.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Liu C.H., Doan S.N. Psychosocial stress contagion in children and families during the COVID-19 pandemic. Clinical Pediatrics. 2020;59(9–10):853–855. doi: 10.1177/0009922820927044. [DOI] [PubMed] [Google Scholar]
- Liu C.Y., Berlin J., Kiti M.C., Fava E.D., Grow A., Zagheni E., Melegaro A., Jenness S.M., Omer S., Lopman B., Nelson K. Rapid review of social contact patterns during the COVID-19 pandemic. Epidemiology. 2021;32(6):781–791. doi: 10.1101/2021.03.12.21253410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe M., Ricciardelli L. A longitudinal study of body image and strategies to lose weight and increase muscles among children. Journal of Applied Developmental Psychology. 2005;26(5):559–577. doi: 10.1016/j.appdev.2005.06.007. [DOI] [Google Scholar]
- Muthén, L.K. , Muthén, B.O. (2017) Mplus version 8 user's guide.
- O'Dea J.A., Caputi P. Association between socioeconomic status, weight, age and gender, and the body image and weight control practices of 6- to 19-year-old children and adolescents. Health Education Research. 2001;16(5):521–532. doi: 10.1093/her/16.5.521. [DOI] [PubMed] [Google Scholar]
- Pearson A.N., Follette V.M., Hayes S.C. A pilot study of acceptance and commitment therapy as a workshop intervention for body dissatisfaction and disordered eating attitudes. Cognitive and Behavioral Practice. 2012;19(1):181–197. doi: 10.1016/j.cbpra.2011.03.001. [DOI] [Google Scholar]
- Pedroso J., Toral N., Bauermann Gubert M. Maternal dissatisfaction with their children's body size in private schools in the Federal District, Brazil. PLoS One. 2018;13(10) doi: 10.1371/journal.pone.0204848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez M., Kroon Van Diest A.M., Smith H., Sladek M.R. Body dissatisfaction and its correlates in 5- to 7-Year-Old girls: A social learning experiment. Journal of Clinical Child & Adolescent Psychology. 2018;47(5):757–769. doi: 10.1080/15374416.2016.1157758. [DOI] [PubMed] [Google Scholar]
- Phares V., Steinberg A.R., Thompson J.K. Gender differences in peer and parental influences: Body image disturbance, self-worth, and psychological functioning in preadolescent children. Journal of Youth and Adolescence. 2004;33(5):421–429. doi: 10.1023/b:joyo.0000037634.18749.20. [DOI] [Google Scholar]
- Polizzi C., Lynn S.J., Perry A. Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clinical Neuropsychiatry. 2020;17(2):59–62. doi: 10.36131/CN20200204. https://doi.org/10.36131/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prefit A.B., Cândea D., Szentagotai-Tătar A. Effects of acceptance and reappraisal on body dissatisfaction: An experimental comparison of two adaptive emotion regulation strategies. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 2020;25:803–809. doi: 10.1007/s40519-019-00691-y. [DOI] [PubMed] [Google Scholar]
- Radhakrishnan L., Leeb R.T., Bitsko R.H., Carey K., Gates A., Holland K.M., Hartnett K.P., Kite-Powell A., DeVies J., Smith A.R., Van Santen K.L., Crossen S., Sheppard M., Wotiz S., Lane R.I., Njai R., Johnson A.G., Winn A., Kirking H.L., Anderson K.N. Pediatric emergency department visits associated with mental health conditions before and during the COVID-19 pandemic — United States, January 2019–January 2022. Morbidity and Mortality Weekly Report. 2022;71(8):319–324. doi: 10.15585/mmwr.mm7108e2. [DOI] [PubMed] [Google Scholar]
- Ricciardelli L.A., Williams R.J. In: Chemically modified bodies: The use of diverse substances for appearance enhancement. Hall M., Grogan S., Gough B., editors. Palgrave Macmillan; 2016. Use of supplements and drugs to change body image and appearance among boys and male adolescents; pp. 13–30. [Google Scholar]
- Robertson M., Duffy F., Newman E., Prieto Bravo C., Ates H.H., Sharpe H. Exploring changes in body image, eating and exercise during the COVID-19 lockdown: A UK survey. Appetite. 2021;159(105062) doi: 10.1016/j.appet.2020.105062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers R., Chabrol H. Parental attitudes, body image disturbance and disordered eating amongst adolescents and young adults: A review. European Eating Disorders Review. 2009;17(2):137–151. doi: 10.1002/erv.907. [DOI] [PubMed] [Google Scholar]
- Rodgers R.F., Wertheim E.H., Damiano S.R., Paxton S.J. Maternal influences on body image and eating concerns among 7– and 8–year‐old boys and girls: Cross‐sectional and prospective relations. International Journal of Eating Disorders. 2019;53(1):79–84. doi: 10.1002/eat.23166. [DOI] [PubMed] [Google Scholar]
- Rozin P., Trachtenberg S., Cohen A.B. Stability of body image and body image dissatisfaction in American College students over about the last 15 years. Appetite. 2001;37(3):245–248. doi: 10.1006/appe.2001.0426. [DOI] [PubMed] [Google Scholar]
- Sharpe H., Naumann U., Treasure J., Schmidt U. Is fat talking a causal risk factor for body dissatisfaction? A systematic review and meta-analysis. International Journal of Eating Disorders. 2013;46(7):643–652. doi: 10.1002/eat.22151. [DOI] [PubMed] [Google Scholar]
- Solano-Pinto N., Sevilla-Vera Y., Fernández-Cézar R., Garrido D. Can parental body dissatisfaction predict that of children? A study on body dissatisfaction, body mass index, and desire to diet in children aged 9–11 and their families. Frontiers in Psychology. 2021;12:10–12. doi: 10.3389/fpsyg.2021.650744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strother E., Lemberg R., Stanford S.C., Turberville D. Eating disorders in men: Underdiagnosed, Undertreated, and misunderstood. Eating Disorders. 2012;20(5):346–355. doi: 10.1080/10640266.2012.715512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez G.F., Suárez A.D., Smith L. Analysis of body image and obesity by Stunkard's silhouettes in 3- to 18-year-old Spanish children and adolescents. Anales Délelőtt Psicología. 2018;34(1):167–172. doi: 10.6018/analesps.34.1.294781. [DOI] [Google Scholar]
- Tylka T.L. In: Body image: A handbook of science, practice, and prevention. Cash T.F., Smolak L., editors. Guilford Press; 2011. Positive psychology perspectives on body image; pp. 56–64. [Google Scholar]
- Vall-Roqué H., Andrés A., Saldaña C. The impact of COVID-19 lockdown on social network sites use, body image disturbances and self-esteem among adolescent and young women. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2021;110(110293) doi: 10.1016/j.pnpbp.2021.110293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura A.K., Birch L.L. Does parenting affect children's eating and weight status. International Journal of Behavioral Nutrition and Physical Activity. 2008;5(1):15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb H.J., Haycraft E. Parental body dissatisfaction and controlling child feeding practices: A prospective study of Australian parent-child dyads. Eating Behaviours. 2019;32:1–6. doi: 10.1016/j.eatbeh.2018.10.002. [DOI] [PubMed] [Google Scholar]
- Welch E., Lagerström M., Ghaderi A. Body shape questionnaire: Psychometric properties of the short version (BSQ-8C) and norms from the general Swedish population. Body Image. 2012;9:547–550. doi: 10.1016/j.bodyim.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Worobey J., Worobey H.S. Body-size stigmatization by preschool girls: In a doll's world, it is good to be “Barbie”. Body Image. 2014;11(2):171–174. doi: 10.1016/j.bodyim.2013.12.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.