Abstract
Radiotherapy is the major treatment of non-small cell lung cancer (NSCLC). The radioresistance and toxicity are the main obstacles that leading to therapeutic failure and poor prognosis. Oncogenic mutation, cancer stem cells (CSCs), tumor hypoxia, DNA damage repair, epithelial-mesenchymal transition (EMT), and tumor microenvironment (TME) may dominate the occurrence of radioresistance at different stages of radiotherapy. Chemotherapy drugs, targeted drugs, and immune checkpoint inhibitors are combined with radiotherapy to treat NSCLC to improve the efficacy. This article reviews the potential mechanism of radioresistance in NSCLC, and discusses the current drug research to overcome radioresistance and the advantages of Traditional Chinese medicine (TCM) in improving the efficacy and reducing the toxicity of radiotherapy.
Keywords: non-small cell lung cancer, radiotherapy, radioresistance mechanisms, toxicity, Traditional Chinese Medicine
1. Introduction
Radiotherapy is the mainstay of treatment for patients with non-small cell lung cancer (NSCLC), and usually combined with surgery, chemotherapy, immunotherapy, and targeted therapy (1–6). The radiation commonly used in radiotherapy mainly includes photo radiation, such as X-ray and γ-ray and particle rays such as neutrons, electrons, protons and heavy ions (2, 7–10). However, no matter what radiation and dose segmentation methods are used, radioresistance will inevitably occur, leading to radiotherapy failure and local recurrence. Simply increasing the radiation dose does not improve survival benefits but leads to adverse reactions and poor prognosis (11).
Radioresistance of NSCLC can be classified as inherent radioresistance and acquired radioresistance, of which acquired radioresistance plays a major role. Various mechanisms that cause radioresistance run through the whole process of radiotherapy. Whether they cause inherent radioresistance or acquired radioresistance is relative. We have simply classified them according to their leading role in different stages of radiotherapy. Acquired radioresistance is mainly related to DNA damage repair, tumor microenvironment (TME) remodeling by inflammation, immune response, tumor metabolic reprogramming, tumor microbiota and senescence cells, and epithelial-mesenchymal transition (EMT) (12–20). Inherent radioresistance is mainly associated with oncogenic mutation, cancer stem cells (CSCs), and tumor hypoxia (21–29).
Targeted drugs or small molecule drugs combined with radiotherapy are used in the treatment of NSCLC. However, there is no systematic review on the mechanism of radioresistance and radiosensitizers of NSCLC. Therefore, we will discuss the radioresistance mechanisms of NSCLC and the study of drugs that can enhance the efficacy and reduce the toxicity of radiotherapy, especially TCM. So as to provide a theoretical basis for clinical development of anti-tumor drugs in combination with radiotherapy.
2. Mechanisms of acquired radioresistance
Acquired radioresistance occurs mainly with radiation induction, the underlying mechanisms involve DNA damage repair and EMT in cancer cell itself, as well as changes in TME such as inflammation, immune response, tumor metabolic reprogramming etc. (15, 16, 19, 30–32). Acquired radioresistance may enhance invasion and metastasis of surviving cancer cells after primary radiotherapy and affect the prognosis and life quality of patients.
2.1. DNA damage repair and radioresistance
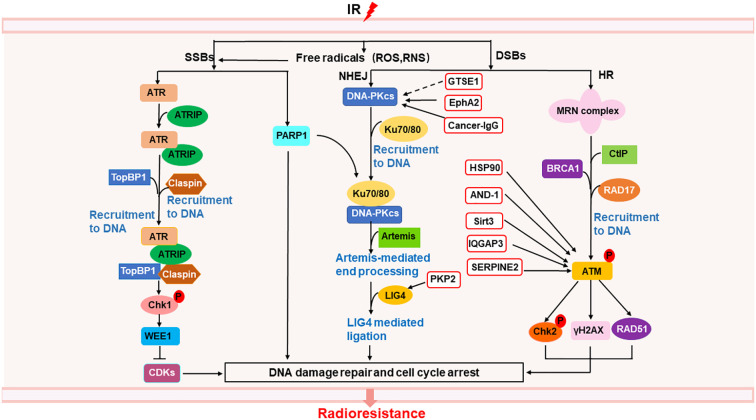
Radiation causes direct DNA single-strand breaks (SSBs) and double-strand breaks (DSBs), as well as indirect DNA damage from oxidative stress such as ROS and reactive nitrogen species (RNS) (30)( Figure 1 ). SSBs is repaired by poly (ADP-ribose) polymerase (PARP) (33), as well as ATR/Chk1 pathway (34). ATR can be activated by recruitment to its partner protein ATRIP, binding to topoisomerase (DNA) II binding protein 1 (TopBP1) and claspin, phosphorylated Chk1 (34), activated Chk1 phosphorylated WEE1, leading to cell cycle arrest and DNA repair (35), resulting in radioresistance of NSCLC (36, 37). DSBs are repaired by homologous recombination (HR) and non-homologous ending joining (NHEJ) (33). In HR, the MRN complex comprising meiotic recombination 11 homolog1 (MRE11), ATP-binding cassette-ATPase (RAD50), and Nijmegen breakage syndrome protein 1 (NBS1), binds to C-terminal binding protein (CtBP)-interacting protein (CtIP) and BRCA1, was recruited by RAD17 to DSB sites, activated ATM, inducing the phosphorylation Chk2 and H2AX, as well as accumulation of RAD51, thus leading to cell cycle arrest and DNA repair (34, 35, 38, 39). Radiation delayed tumor growth and increased local control in Atm deletion tumor model of lung adenocarcinoma (40). In NHEJ, DNA-dependent protein kinase catalytic subunit (DNA-PKcs) is directly recruited to DNA damage sites via Ku heterodimers (Ku70/80), inducing Artemis-mediated end processing and DNA ligase 4 (LIG4) mediated ligation, leading to DNA repair (35). Besides, heat shock protein 90 (HSP90) (41), acidic nucleoplasmic DNA binding protein1 (AND-1) (42), sirtuin 3 (Sirt 3) (43), IQ motif containing GTPase-activating protein 3 (IQGAP3) (44), and serine proteinase inhibitor clade E member 2 (SERPINE2) (45) can enhance radioresistance via activating ATM to activate the HR pathway in NSCLC. G2 and S phase-expressed 1(GTSE1) (46), plakophilin2 (PKP2) (47), ephrin type-A receptor 2 (EphA2) (48, 49), and cancer-derived IgG (cancer-IgG) (50) can participate in NHEJ pathway, leading to radioresistance in NSCLC. AAA ATPases RUVBL1/2 can activate both HR and NHEJ pathway, inducing radioresistance in NSCLC (51). In addition to Chk1 and Chk2, WEE1 can also regulate cell cycle arrest by inhibiting the phosphorylation of cyclin-dependent kinases (CDKs) (52, 53), inducing radioresistance (54). Thus, targeting DNA repair proteins or cell cycle regulator may overcome radiation-induced radioresistance in NSCLC.
Figure 1.
Mechanisms of radioresistance caused by DNA damage repair in NSCLC. Radiation induced DNA damage response can activate the DNA repair pathway, of which SSBs can be repaired through ATR/Chk1 pathway and PARP1, DSBs can be repaired through NHEJ and HR. In the red box are proteins related to the repair of DSBs that may become new targets for radiosensitization. The solid line represents a clear target, and the dotted line represents a possible action through this target.
It can be seen from the above that tumor cells have multiple ways to repair radiation-induced DNA damage. Drugs targeting a single target may not have obvious effect on overcoming radioresistance, and are prone to drug resistance. Therefore, the combination of multiple targets for DNA repair will be the direction of tumor treatment in the future, but how to effectively combine the targets still needs more research.
2.2. Tumor microenvironment remodeling and radioresistance
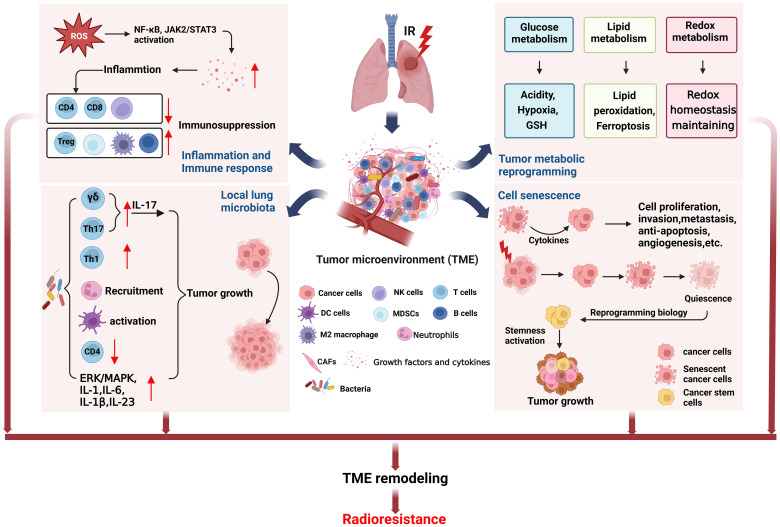
Tumor microenvironment (TME) is closely related to tumor progression, and the remodeling of TME after radiotherapy can lead to radioresistance (18). Here, we focus on the effects of inflammation and immune response, tumor microbiota, tumor metabolic reprogramming, and cell senescence on TME to clarify the role of radiation-induced TME remodeling in the radioresistance of NSCLC ( Figure 2 ).
Figure 2.
TME remodeling may lead to radioresistance of NSCLC. The TME changed in NSCLC cells surviving after radiotherapy. Radiation induced inflammation and immune response can cause immunosuppression. The local lung microbiota can induce tumor growth by regulating the immune cells. Tumor metabolic reprogramming after radiation will lead to increase of acidity, hypoxia, and GSH production, unbalance of ferroptosis, and redox homeostasis maintaining, being conductive to tumor growth. Cell senescence after radiotherapy can also induce cell proliferation and tumor growth. The above factors together form TME remodeling that promotes tumor growth, metastasis and recurrence after radiotherapy. (This figure is adapted from an image created from BioRender.com).
2.2.1. Inflammation and immune response
Radiation generated ROS and RNS can activate NF-κB, Janus-associated kinase (JAK)2/signal transducer and activator of transcription (STAT)3 pathway to increase the release of growth factors and cytokines, such as VEGF, TGF-β, IL-1, IL-8, TNF-α and IL-6 etc. (15, 31, 55, 56), which are involved in inflammation and immune response (18, 57–60). TGFβ and TNFα in TME are very important in the formation and development of tumor (61). Our previous study found that irradiation of NSCLC cell lines A549 and H1299 can cause overexpression of TGFβ and TNFα, resulting in HIF1α activation and cause genomic instability of BMSCs and may promote tumor progression (62). We also found that TGFβ mainly causes short-term side effects, while TNFα mainly causes long-term side effects. This may provide a guideline for clinical use of combined drugs at different stages of radiotherapy for NSCLC. In addition, radiation-induced inflammation reduces tumor-suppressing immune cells such as CD4+T cells, CD8+T cells, and natural killer (NK) cells, while tumor-promoting immune cells such as regulatory T cells (Treg), myeloid-derived suppressor cells (MDSC), and M2 tumor-associated macrophages (TAMs) increase, eventually forming an immunosuppressive environment, and high level of TGFβ (19, 63). Moreover, M2 macrophages and B cells infiltrate into TME also participate in the radioresistance of NSCLC (64, 65). Thus targeting inflammation not only enhance the tumor killing effects of radiotherapy, but also protect the normal cells and tissues from radiation-induced bystander effects.
2.2.2. Tumor microbiota
It is well known that intestinal microbiome can regulate host physiological and pathological processes through metabolism, inflammation and immune response (66, 67). On the one hand, tumor microbiota can enhance anti-tumor immunity through STING signal activation, T and NK cell activation. On the other hand, it can upregulate ROS, induce anti-inflammatory environment, and inactivate T cell to promote immunosuppression and cancer progression (68). Moreover, tumor microbiota stimulates γδT cells to produce IL-17 that triggering inflammation and cancer progression (69), and increases Th17 cells that enhancing lung cancer proliferation and angiogenesis (70). It is found that the dysbiosis of local lung microbiota in patients with advanced lung cancer can lead to Th1, Th17, γδT cells and PD-1 positive T cells increase, neutrophils recruitment, dendritic cells (DCs) activation, CD4+T cells decrease, cytokines IL-1, IL-1b, IL-6, IL-17, IL-23 upregulation, as well as upregulation of ERK/MAPK and inflammation pathways, all these above alterations promoted tumor progression (71). Although there is no research report on the correlation between tumor microbiota and radioresistance, there is no doubt that tumor microbiota will participate in tumor response to radiotherapy through inflammation and immune response and affect the final efficacy. The microbiome may serve as an indicator for cancer diagnosis or prognostic assessment and could be used as potential targets to develop new cancer therapies.
2.2.3. Tumor metabolic reprogramming
Tumor metabolic reprogramming after radiotherapy, such as glucose metabolism, lipid metabolism, and redox metabolism, contributes to TME remodeling and acquired radioresistance (19). The increased expression of glucose transporter1 (GLUT1), pyruvate kinase M2 isoform (PKM2), and lactate dehydrogenase (LDHA) after irradiation promoted glycolysis (19, 72, 73), while the expression of glycogen synthetase 1 (GYS1) was also up-regulated, leading to glycogen accumulation (74). These changes enable cancer cells to survive, proliferate and resist radiation. In addition, pentose phosphate pathway (PPP) after radiation induced more NADPH production, which promoted the production of reduced glutathione (GSH) (19), may lead to radioresistance of NSCLC.
IR can induce the expression of ACSL4, which is a lipid metabolizing enzyme in cancer cells, to increase lipid peroxidation and ferroptosis (75). Intriguingly, IR can also induce the expression of ferroptosis inhibitors SLC7A11 and GPX4, causing radioresistance (75). Perhaps, radioresistant cells have formed a balance between promoting ferroptosis and inhibiting ferroptosis, enabling cells to survive. In radioresistant lung cancer cells, the expression of lipid Droplet (LD) and ferritin heavy chain (FTH1) increased and correlated with each other, which can be targeted and synergistically inhibit tumor radioresistance (76). In addition, the activation of sPLA2-PKCδ-MAPKs-cPLA2α pathway promoted tumor progression and radioresistance in NSCLC (77).
ROS levels are elevated in lung cancer radioresistant cells, which exhibit radioresistance by maintaining oxidative stress and NRF2-dependent metabolic adaptation (78). The expression of TP53-regulated inhibitor of apoptosis 1 (TRIAP1) in NSCLC cell lines A549 and H460 increased after irradiation, and caused upregulation of antioxidant proteins such as thioredoxin-related transmembrane protein (TMX) 1, TMX2, thioredoxin (TXN), glutaredoxin (GLRX) 2, GLRX3, peroxiredoxin (PRDX) 3, PRDX4 and PRDX6, participated in redox metabolism and enhanced the ROS scavenging, leading to radioresistance in NSCLC (79).
In conclusion, NSCLC cells that survived after radiation have altered metabolism that favors cell proliferation and tumor progression. Therefore, targeting tumor metabolism will be an effective measure to improve the radiotherapy prognosis and survival rate of NSCLC patients.
2.2.4. Cell senescence
Studies have shown that induction of premature senescence can radiosensitize NSCLC cells (80). On the contrary, the cytokines secreted by senescent cells which not killed by radiation will affect the adjacent surviving cancer cells in TME, stimulate tumor cell proliferation, invasion and metastasis, escape apoptosis, induce angiogenesis, and promote tumor phenotype (20). In addition, lung cancer cells survived from radiotherapy experienced senescence and entered a dormant state, reprogrammed their biology months or years after irradiation, reactivated stemness, and produced tumors with enhanced growth and metastasis (81).
To sum up, the TME itself is inflammatory, radiation further promotes the release of inflammatory factors, aggravates inflammatory reaction, causes immunosuppression, and hinders anti-tumor immunity. In addition, tumor microbiota can activate inflammatory pathways to promote tumor progression. Moreover, the oxidative stress reaction induced by radiation promotes the occurrence of tumor metabolism reprogramming, causes the depletion of T cells, and makes tumor cells resistant to radiation. The senescent cells in TME can promote tumor proliferation, invasion and metastasis by secreting cytokines. The interaction of the above factors leads to TME remodeling and radioresistance. In addition to these above, tumor hypoxia also play a key role in TME. It is a challenge to overcome radioresistance by targeting TME, because any single targeting action may not achieve the desired therapeutic effect.
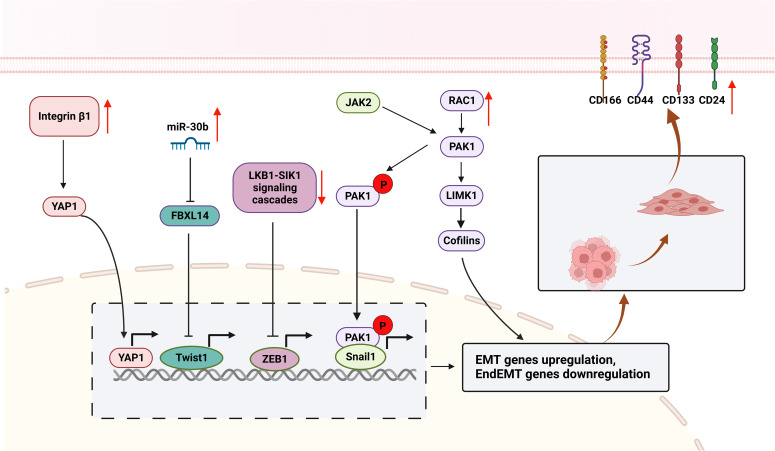
2.3. Epithelial-mesenchymal transition and radioresistance
Radiotherapy induced EMT and CSCs characteristics, enhanced the invasion and metastasis of cancer cells surviving after primary radiotherapy, leading to acquired resistance of NSCLC, which in turn weakened the radiation-induced tumor killing effect (16, 17, 82). TWIST1 (83, 84) increased after radiation in NSCLC, resulting in downregulation of E-cadherin, overexpression of Snail1, Vimentin, N-cadherin, and PDGFR (85), which promotes cell proliferation, invasion and vascular regeneration, leading to tumor metastasis and radioresistance. PDGF secretion also increased after radiation and resulted in radiation-induced pneumonitis and fibrosis (86), PDGF binds to PDGFR to induce proliferation and vascular regeneration. In addition, Yes-associated protein 1 (YAP1) (87), Snail1 (88), PAK1-LIM domain kinase 1 (LIMK1)-cofilins signaling (89), and zinc-finger E-box-binding homeobox factor 1 (ZEB1) (90)were upregulated after radiotherapy, leading to EMT ( Figure 3 ). Radiation survived NSCLC cells also show cancer stemness properties, such as highly expressed CD166, CD24, CD44, Sox-2, CD133, etc. (76, 85, 91). EMT are critical targets and biomarkers for radiotherapy, radiosensitizers targeting EMT are promising treatment for NSCLC in clinical.
Figure 3.
Mechanisms of EMT contributes to radioresistance in NSCLC. The surviving cells included enriched CSCs subpopulations that highly expressed CSCs markers (CD24, CD44, CD133, and CD166). miR-30b was upregulated and targeted to FBXL14, activating the transcription factor Twist1, resulting in increased expression of Vimentin, N-cadherin and Fibronectin, and decreased E-cadherin expression. Integrin β1 is overexpressed after radiotherapy and targets YAP1 to activate ATM/Chk2 signaling, leading to EMT. Furthermore, RAC1 is upregulated in radioresistant NSCLCs, activates the RAC1/PAK1/LIMK1/Cofilins pathway and the PAK1/Snail pathway, causes EMT and promotes tumor metastasis and invasion. LKB1/SIK1 signaling is downregulated after radiotherapy, prompting activation of the transcription factor ZEB1, leading to EMT and tumor metastasis and invasion. (This figure is adapted from an image created from BioRender.com).
3. Mechanisms of inherent radioresistance
Inherent radioresistance is an important factor leading to radiotherapy failure, which is mainly related to the gene mutation status of tumor cells, hypoxia status, distribution of CSCs (28, 92, 93), etc.
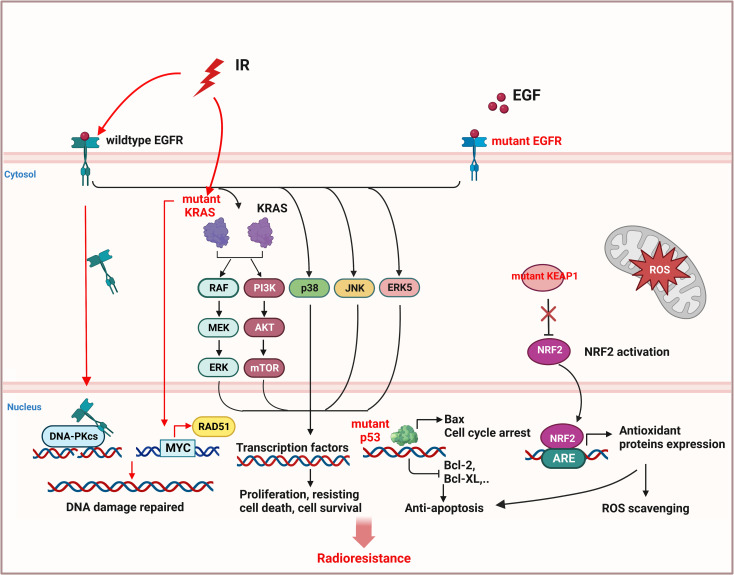
3.1. Mutation status of oncogenes and radioresistance
Mutations of oncogenes, such as epidermal growth factor receptor (EGFR) (94, 95) and kirsten rat sarcoma viral oncogene (KRAS) (96), or tumor suppressor genes such as Kelch-like ECH-associated protein 1 (KEAP1) (97, 98) and tumor protein P53 (TP53) (99, 100), can cause activation of cell proliferation and resisting cell death signals in NSCLC, leading to radioresistance ( Figure 4 ).
Figure 4.
Inherent radioresistance is related to the mutation status of oncogene or tumor suppressor gene in NSCLC. Wildtype EGFR and mutant EGFR both caused cell proliferation and resisting cell death by activation of downstream pathway. In addition, wildtype EGFR can be stimulated by radiation and translocate to nucleus to activate DNA-PKcs, leading to DNA repair. Mutant KRAS can also promote the expression of DNA repair protein RAD51 by activating MYC and improving DNA repair. Mutant p53 will induce anti-apoptosis of NSCLC cells. Mutant KEAP1 cannot inhibit activation of NRF2, leading to the expression of antioxidant proteins to eliminate ROS. (This figure is adapted from an image created from BioRender.com).
EGFR is overexpressed in 40% to 80% of patients with NSCLC and is associated with poor prognosis (101, 102). Radiation can stimulate wild-type EGFR to enter nucleus and bind with DNA-PK catalytic subunit (DNA-PKcs) to promote DNA repair, thus leading to radioresistance of NSCLC (103, 104). However, the NSCLC with mutant EGFR is not necessarily more sensitive to radiation (94), since the mutant EGFR can trigger the downstream pathways, including extracellular signal-regulated kinase (RAS/ERK), p38MAPK, c-Jun N-terminal kinase (JNK), and ERK5, and also activate PI3K/AKT/mTOR signaling pathway, leading to cell proliferation and anti-apoptosis, migration, DNA repair, cell cycle arrest, etc., which in turn increases the radioresistance of NSCLC (22, 23, 103, 105–108).
KRAS can regulate cell growth, differentiation and apoptosis, its mutations mainly occur at codons 12 and 13, and have been found approximately in 20-30% of NSCLC tumor samples (109). KRAS-mutant NSCLC cells are more radioresistant than KRAS wild-type cells (96, 110) or EGFR-mutant cells (21), because mutant KRAS can upregulate RAD51 expression through oncogene MYC, thereby enhancing DNA damage repair and cell survival (111). In addition, EGFR-dependent chromatin condensation, namely mitotic-like concentrated chromatin (MLCC), can protect KRAS-mutant NSCLC cells from ionizing radiation (IR)-induced DSBs and premature senescence (110), and enhance the expression of CSC marker protein CD133 via osteopontin/EGFR pathway, promoting tumor invasion and radioresistance (112).
KEAP1/nuclear factor E2-related factor (NRF2) mutation happens approximately 30% of NSCLC (92), and 7% of patients have co-mutations of KEAP1/NRF2 and EGFR (113). Mutant KEAP1 lost its inhibitory effect on NRF2 in cytoplasm, the activated NRF2 translocated to the nucleus and activated the expression of antioxidant proteins by binding to antioxidant-responsive elements (AREs), resulting in the scavenging of ROS and anti-apoptosis of tumor cells, leading to unlimited proliferation, metastasis and radioresistance of NSCLC (114–116).
TP53 mutation occurs in more than half of human cancers, including NSCLC (92). p53 can not only induce cell cycle arrest, senescence, and apoptosis, but also regulate tumor metabolism, promote ferroptosis, and inhibit tumor development (117). Mutant p53 can neither induce the expression of pro-apoptotic protein Bax, nor inhibit the expression of anti-apoptotic proteins (Bcl-2, Bcl-xl) (118), which makes cancer cells survive in radiotherapy (119). Compared with single mutations in TP53, NSCLC with co-mutation in KRAS and TP53, or co-mutation in TP53 and KEAP1 are more resistance to IR-induced cell death (100, 114).
In addition to the oncogenic mutation, high levels of inhibitor of apoptosis proteins, such as cIAP1/2, XIAP, and survivin, participate in cell death and survival by binding and inhibiting caspases, leading to radioresistance of NSCLC (120–123). In addition, microRNAs can also affect the radiosensitivity of NSCLC by regulating the cell proliferation and apoptosis. miR-99a and miR-770-5p can induce apoptosis and improve radiosensitivity (124, 125). On the contrary, miR-410 and miR-208a promote radioresistance by inducing EMT and increasing cell proliferation respectively in NSCLC (126, 127).
According to the potential mechanism of inherent radioresistance mentioned above, genome sequencing can be carried out before treatment to determine the mutation type and formulate effective treatment strategies, so as to improve the tumor-killing rate and reduce the tumor recurrence rate after primary radiotherapy of NSCLC.
3.2. Cancer stem cells and radioresistance
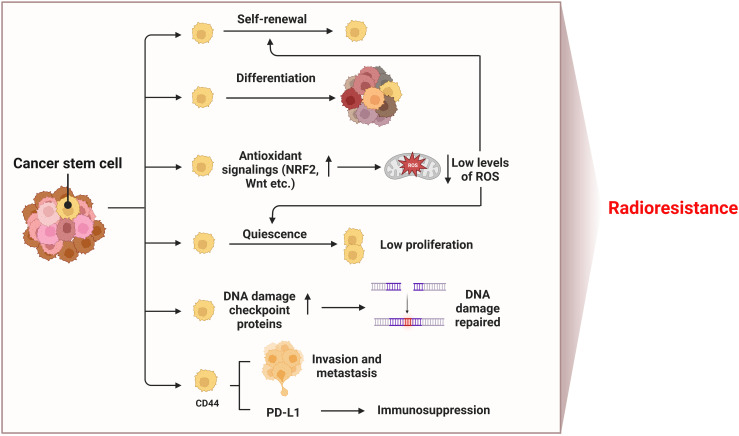
Cancer stem cells (CSCs) are subpopulations of tumor cells with the ability to self-renew and differentiate into heterogeneous tumor cells, promote tumor growth and metastasis through unlimited proliferation and migration, leading to tumor recurrence and treatment failure (128–131). Antioxidant signaling pathways (NRF2, Wnt, etc.) in CSCs are activated, and more antioxidant proteins are expressed to clear ROS, so as to maintain a low level of ROS in cells, which contributes to the quiescence and self-renewal of CSCs (130, 132–134) ( Figure 5 ). In addition, CSCs have a strong ability to repair DNA damage (135). CD133 is one of the markers of CSCs. As early as 2006, Bao et al. reported that CD133-positive glioma cells showed higher expression of DNA damage checkpoint proteins (i.e. ATM, Rad17, Chk1 and Chk2) than CD133-negative cells (136). In 2014, Desai et al. clarified that CD133-positive NSCLC cells highly express DNA damage repair proteins RAD51 and Exo1, which can promote radioresistance, but had cell type specificity (137). Therefore, low levels of ROS and enhanced DNA damage repair make CSCs insensitive to radiotherapy, leading to tumor relapse (138). CD44 is another CSCs marker, which is related to tumor recurrence and metastasis, as well as prediction of the outcome after radiotherapy (139, 140). The overexpression of CD44 promotes the proliferation of NSCLC, and up-regulates the expression of PD-L1 to promote tumorigenesis, immunosuppression and chemotherapy resistance (141, 142). It is worth noting that due to the low sensitivity of CSCs to IR, the CSCs not killed by radiation will be enriched, which leads to acquired radioresistance. Therefore, the treatment efficiency of NSCLC can be improved by inducing CSCs to differentiate to reduce their proportion in tumor tissues, or by combining drugs targeting key proteins of CSCs antioxidant pathways or surface marker proteins with radiotherapy.
Figure 5.
Mechanisms of radioresistance caused by CSCs in NSCLC. Hallmarks of CSCs such as self-renewal and differentiation, low levels of ROS, quiescence, DNA damage repair, invasion and metastasis ability, and immunosuppression induced by upregulated PD-L1 all contribute to radioresistance of NSCLC. (This figure is adapted from an image created from BioRender.com).
3.3. Tumor hypoxia and radioresistance
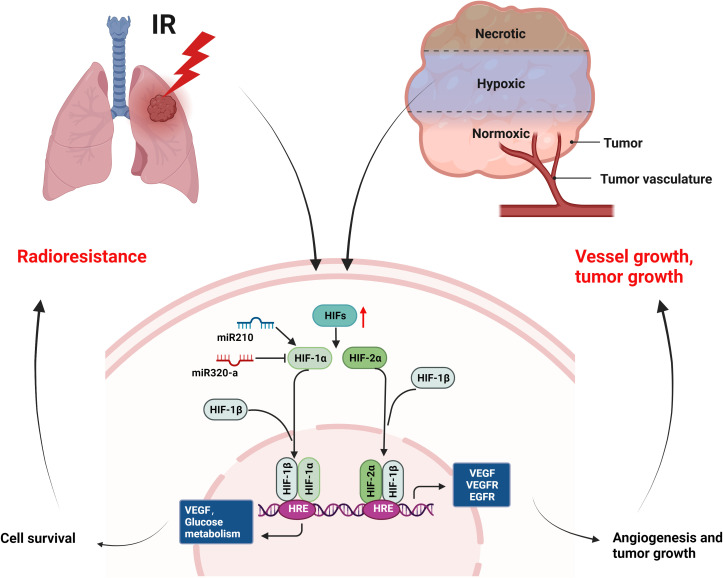
As one of the cancer hallmarks, hypoxia induces angiogenesis, tumor invasion, metastasis, and treatment resistance (27, 28). Hypoxic tumor cells are very insensitive to radiation (143). In this article, we mainly introduce the research on HIFs and radioresistance in NSCLC ( Figure 6 ). Hypoxia environment and radiation activate HIFs (144, 145), activated HIF-1α and its partner subunits HIF-1β enter nucleus and bind to hypoxia-responsive element (HRE) to trigger gene transcription regulating VEGF and glucose metabolism etc., leading to cell survival (146–148). HIF-2α mainly induces angiogenic factors, such as VEGF, VEGFR, EGFR etc., promoting angiogenesis and tumor growth (149–151). Research showed that the upregulation of HIF-1α enhanced the radioresistance of NSCLC (152). Conversely, the decrease of HIF-1α in acidic environment caused radioresistance in NSCLC cells and blocking simultaneously of both HIF-1α and HIF-2α radiosensitized NSCLC, suggesting the role of HIF-2α in radioresistance (153). In addition, miR-210 promoted the hypoxic phenotype of NSCLC cells and increased radioresistance by inducing and stabilizing HIF-1α (154). By contrast, another microRNA, miR-320a targeted HIF-1α to promote methylation of PTEN, thereby reducing the radioresistance of NSCLC in vitro and in vivo (155). In conclusion, targeting HIFs may enhance radiosensitivity of NSCLC in clinical, but the pH value should be considered when targeting HIF-1α.
Figure 6.
Mechanisms of radioresistance caused by hypoxia in NSCLC. Hypoxia environment of tumor and radiation can activate the expression of HIFs, which will induce the expression of growth factors (VEGF, VEGFR, EGFR etc.) and improved glucose metabolism, leading to cell survival, angiogenesis, and tumor growth of NSCLC. (This figure is adapted from an image created from BioRender.com).
4. Radiosensitizing non-small cell lung cancer
As we discussed above, the mechanisms of radioresistance of NSCLC are complex and not isolated from each other. Whether surgery, chemotherapy, targeted therapy, or immunotherapy, the goal of their combination with radiotherapy is to kill tumor cells, but what cannot be avoided is limited effect, tumor recurrence and metastasis, as well as side effects.
At present, chemotherapy drugs, targeted drugs, immune checkpoint inhibitors, etc. can be used as radiosensizitizers in NSCLC, but these drugs are prone to drug resistance and toxic side effects (11, 30, 156, 157). In addition, most of the current studies about radiosensitizers used in NSCLC is still limited to experimental research, and only a few drugs have been used in clinical. We summarized the drugs or agents for NSCLC radiosensitization in Table 1 , including antibody drugs and small molecule inhibitors from non-natural sources. In addition to drug toxicity, radiotherapy itself can also cause lung toxicity in patients, manifesting as different grades of pneumonia, pulmonary fibrosis (32, 183). In addition, the mechanisms of radioresistance are complex, and the efficacy of these single targeted drugs is limited. Therefore, it is an urgent need to develop drugs targeting multiple targets, with synergistic effects and low toxicity in NSCLC radiotherapy.
Table 1.
Non-natural products radiosensitize NSCLC by targeting key proteins.
| Mechanism of action | Targets | Radiosensitizing modulators | Experimental models/(in vitro or in vivo or clinical) | Conclusion | Reference |
|---|---|---|---|---|---|
| Targeting DNA repair | PARP | Olaparib+ML216 | In vitro and in vivo | PARP inhibitors and BLM helicase inhibitors synergistically radiosensitized NSCLC. | (158) |
| PARP | niraparib | In vitro and in vivo | Niraparib activated anti-tumor CD8+T cells in the tumor microenvironment through the STING/TBK1/IRF3 pathway in EGFR-mutant NSCLC. | (159) | |
| ATM | KU55933 | In vitro | ATM inhibitors radiosensitized NSCLC by inhibiting IR-induced EGFR activation and can be used in EGFR-resistant tumor cells for radiotherapy. | (160) | |
| DNA-PK | AZD7648 | In vitro and in vivo | DNA-PK inhibitors are promising radiosensitizers for treatment of NSCLC. | (161) | |
| Telomerase | BIBR1532 | In vitro and in vivo | Inhibiting telomerase function can radiosensitize NSCLC. | (162) | |
| AND-1 | CH-3 compound | In vitro and in vivo | Inhibition of AND-1 will be a promising strategy for enhancing radiosensitivity in NSCLC. | (42) | |
| RUVBL1/2 | Compound B | In vitro and in vivo | RUVBL1/2 inhibition combined with radiotherapy may be effective treatment for NSCLC. | (51) | |
| Targeting cell cycle | BET | JQ1 | In vitro and in vivo | BET inhibition may be a potential treatment for radiosensitizing NSCLC. | (163) |
| CDK4/6 | Palbociclib/ | In vitro | Combining inhibition of CDK4/6 and radiotherapy will be promising strategy for patients with p53-wild type NSCLC. | (164) | |
| CDK4/6 | Abemaciclib | In vitro and in vivo | Abemacilcib combined with radiotherapy radiosensitized NSCLC in preclinical models. | (165) | |
| Targeting inflammation | IKKβ | IMD03544 | In vitro and/or in vivo | Blockade of IKK-NF-κB signaling will be benefit for radiotherapy in NSCLC. | (60, 166) |
| TGF-β | LY364947 | In vitro and in vivo | TGF-β inhibition combined with radiotherapy enhanced therapeutic efficacy in NSCLC. | (167) | |
| STAT3 | Niclosamide | In vitro and in vivo | Inhibition of STAT3 signaling will be effective treatment for NSCLC to radiotherapy. | (59) | |
| JAK2 | TG101209 | In vitro and in vivo | Targeting JAK2 may enhance radiotherapy response in KRAS-mutant NSCLC. | (168) | |
| Targeting immune suppression | PD-L1 | anti-PD-L1 antibody | In vitro and in vivo | Anti-PD-L1 antibody combined with radiotherapy synergistically enhanced anti-tumor immunity in NSCLC. | (169) |
| PD-1 | Nivolumab | Clinical phase II (Enrollment: 65) |
No published results to date | (170) | |
| PD-1 | pembrolizumab | Clinical phase I/II (Enrollment: 104) |
Pembrolizumab combined with radiotherapy may be effective in certain subgroups of NSCLC patients with low PD-L1 expression | (171) | |
| CTLA-4 | Ipilimumab | Clinical phase I/II (Enrollment: 39) | CTLA-4 blockade and radiotherapy synergistically induced robust antitumor T cell responses | (172) | |
| Targeting glutamine metabolism | Glutaminase | CB-839 | Clinical phase I/II (Enrollment: unknown) | KEAP1/NFE2L2 mutations is associated with radioresistance and local recurrence, and glutaminase inhibition enhanced radiotherapeutic effects in NSCLC. | (97) |
| Targeting cell proliferation | EGFR | Erlotinib, gefitinib | Clinical phase II (Enrollment: 10) | EGFR-TKI combined with radiotherapy achieves long-term control of stage IV NSCLC with EGFR mutations. | (173) |
| EGFR/HER2/HER3 | Pan-HER | In vitro and in vivo | Pan-HER exerted anti-proliferation and tumor growth-delay effect by inhibiting multiple HER members to enhance radiation response in NSCLC. | (174) | |
| ERK5 | XMD8-92/ERK5 knockdown | In vitro and in vivo | ERK5 contributes to lung cancer development and radioresistance and can be a novel target for radiotherapy in NSCLC. | (23) | |
| EGFR and Norch | Anti-EGFR/Notch CrossMab (CT16) | In vitro and in vivo | Combined blocking of EGFR and Notch signaling enhanced radiation response in NSCLC. | (175) | |
| EGFR and COX2 | Afatinib+celecoxib | In vitro | Combined inhibition of EGFR and COX-2 radiosensitized NSCLC. | (176) | |
| Targeting cell apoptosis | mTOR | miR-99a | In vitro and in vivo | MiR-99a enhanced radiosensitivity via targeting mTOR in NSCLC. | (124) |
| miR-410 | In vitro and in vivo | MiR-410 increased radioresistance via targeting PTEN/PI3K/mTOR pathway in NSCLC. | (126) | ||
| Bcl-XL | BXI-61, BXI-72 | In vitro and in vivo | Small molecules targeting Bcl-XL conquered acquired radioresistance in NSCLC. | (177) | |
| Anti-apoptotic Bcl-2 family | ABT-737 | In vitro and in vivo | ABT-737 radiosensitized K-ras mutant NSCLC by inhibiting the activity of Bcl-2 family proteins. | (178) | |
| Bak | BKA-073 | In vitro and in vivo | Bak activators may be promising anticancer drugs in NSCLC treatment. | (179) | |
| Bcl-2/Bcl-xL | ABT-263 | In vitro and in vivo | Inhibiting anti-apoptotic Bcl-2 family proteins may enhance radiosensitivity by reducing hypoxia-mediated anti-apoptosis in NSCLC. | (180) | |
| cIAP1/2 | Birinapant | In vitro | cIAP1/2 will be promising targets for enhancing radiosensitivity of NSCLC. | (123) | |
| Targeting angiogenesis | VEGFR2 | Apatinib | In vivo | Apatinib can radiosensitize lung cancer through vascular normalization and hypoxia reduction in the xenograft model | (181) |
| VEGF | Endostar | Clinical phage II (Enrollment: 67) | Continuous intravenous endurance combined with concurrent etoposide and radiation prolongs OS in patients with unresectable stage III NSCLC. | (182) |
5. Application and advantages of TCM in radiotherapy for NSCLC
As an auxiliary means of radiotherapy for NSCLC, TCM can increase the apoptosis of cancer cells, inhibit tumor metastasis, enhance the anti-tumor immunity of patients, regulate the TME homeostasis, thus improving the efficacy of radiotherapy and reducing the recurrence rate (184, 185), which reflecting the basic principles of treating tumor by reinforcing healthy qi to eliminate pathogenic factors of TCM. Some single herbs are frequently used in the treatment of NSCLC (186). Commonly used TCM for reinforcing healthy qi to eliminate pathogenic factors include Ginseng, Codonopsis pilosula, Astragalus, Angelica, and Polygonatum, etc. Astraglus has immunoregulatory, antioxidant, anti-inflammatory, and anti-cancer activities and combined with chemotherapy to increase the efficacy and reduce the toxicity in patients with advanced NSCLC (187, 188). Our previous research found that Astragalus polysaccharides can reduce the radiation induced bystander effects (RIBE) of bone marrow mesenchymal stem cells (BMSCs) caused by X-rays and heavy ions, and reduce the toxicity of normal cells and tissues in lung cancer radiotherapy (189–191). In addition, our research also found that Guiqi Baizhu Decoction, which composed of Astragalus, Angelica, Atractylodes, Paeonia lactiflora, Tangerine peel, Rhubarb, and Licorice, can significantly reduce the radiation inflammatory reaction and immune damage, and prevent intestinal microbial imbalance and metabolic disorders caused by radiation (192). We further found that Guiqi Baizhu Decoction can regulate HIF-1α, AQP4 and Na+/K+-ATPase to reduce hypoxia and oxidative stress, thus treating radiation-induced intestinal edema (193). Moreover, in the study of gastric cancer, we used chemical informatics and cell experiments to verify that Guiqi Baizhu decoction plays a dual role of anti-tumor and immunoregulation by targeting HER2 and PD-L1 through its active components quercetin and isorhamnetin respectively, reflecting the mechanism of multi-point and synergistic effect of TCM in tumor treatment (194).
In recent decades, the advantages of natural products in anti-tumor have become more and more obvious, such as paclitaxel (195) and vinorelbine (196) has been used in clinical for decades. Here we listed the application of TCM compound prescription, single herb, herbal extracts, and small molecules from TCM in the preclinical and clinical research of radiotherapy toxicity reduction and efficiency enhancement for NSCLC ( Table 2 ). The various factors that cause radioresistance are not independent, nor only appear in a certain period of time. Moreover, at different stages of radiotherapy, the mechanism that dominates radioresistance is variable and complex. However, TCM can adjust the radiation anti-tumor effect in different ways with the advantage of multi-component and multi-target, improve the efficacy of radiotherapy, reduce the toxicity of radiotherapy and improve the quality of life of patients.
Table 2.
Natural compound/traditional Chinese medicine used in radiotherapy of NSCLC.
| Natural compound/Traditional Chinese medicine | Type of drug | Experimental models /(in vitro or in vivo or clinical) | Function | Reference |
|---|---|---|---|---|
| Aidi injection | Compound prescription, composed of extracts from Mylabri, Ginseng Astragalus, and Acanthopanacis senticosi. | Clinical | Heat-clearing and toxin-removing, eliminating stasis and resolve masses. Aidi injection improved PSF and immune function in lung cancer patients and alleviated the myelosuppression, radiation pneumonitis, radiation esophagitis. | (197, 198) |
| Shengqi Fuzheng injection | Compound prescription, composed of extracts from Codonopsis and Astragalus. | Clinical | Supplement and tonify lung qi. Reduced the inflammatory response and improved immune function by regulating the expression of TNF-α and TGF-β. | (199) |
| Compound kushen injection | Compound prescription, composed of extracts from Sophorae and Rhizoma Smilacis Glabrae. | Clinical | Clear heat and drain dampness, resolve masses and alleviate pain. Improved efficacy and reduced radiation pneumonitis, radiation esophagitis, and myelosuppression. | (200) |
| Kangai injection | Compound prescription, composed of extracts from Astragalus, Ginseng, and Oxymatrine. | In vitro | Increased FOXO3a-mediated apoptosis and autophagic cell death in cisplatin-resistance A549 cells. | (201) |
| Astragalus | Monomer herb | Meta-analysis | Reduced the toxicity and increased the efficacy of radiotherapy. | (202) |
| Elemene injection | Herbal extractions from Curcuma | Meta-analysis | Reduce adverse reactions, relieve symptoms. | (203) |
| Ganoderma lucidum polysaccharide | Herbal extractions from Ganoderm | In vitro and in vivo | Decreased the tumor immune suppression. | (204) |
| Kanglaite injection (KLTi) | Herbal extractions from Coix agrestis Lour | Clinical | KLTi in combination with radiotherapy improved patient survival but can induce adverse effects such as leukopenia, nausea and vomiting. | (205) |
| Astragalus polysaccharide | Herbal extractions from Astragalus. | In vitro | Reduced the radiation-induced bystander effects through regulation of MAPK/NF-κB signaling pathway, or TGF-βR/MAPK/ROS pathway. | (189–191) |
| Micheliolide | Small molecule derived from Michelia. | In vitro | Micheliolide enhanced radiosensitivity via inducing the ubiquitination degradation of HIF-1α in p53-null NSCLC. | (206) |
| Quercetin | Small molecule, derived from a variety of TCM such as Bupleurum, Hypericum, Astragalus, etc. | In vitro | Inhibited WEE1 signaling | (54) |
| Daurinol | Small molecule, derived from Haplophyllum. | In vitro | Suppressed serine/threonine family of aurora kinases A/B(AURKA/AURKB) can radiosensitize NSCLC. | (207) |
| Isorhamnetin | Small molecule, derived from a variety of TCM such as Folium Ginkgo, Astragalus, etc. | In vitro | Upregulated IL-13, suppressed NF-κB signaling and increased cell apoptosis. | (208) |
| Cucurbitacin I | Small molecule, mainly distributed in Cucurbitaceae. | In vitro and in vivo | Inhibition of STAT3 signaling in CD133- positive NSCLC may enhance radiotherapy effect. | (209) |
| Phoyunnanin E | Small molecule, isolated from Dendrobium venustum. | In vitro | Induce lung cancer cell apoptosis via inhibiting survivin. | (210) |
| Celastrol | Small molecule, derived from Celeastrus. | In vitro | Celastrol radiosensitized NSCLC by suppressing the ATP-binding activity of Hsp90. | (211) |
| Curcumin | Small molecule, isolated from Curcuma longa L. | In vitro and in vivo | Increasing cell apoptosis via activating the p53-miR-192-5p/215-XIAP pathway. | (212) |
| Scutellarin | Small molecule, isolated from Scutellaria altissima L. or S.baicalensis Georgi. | In vitro and in vivo | Promoted cell apoptosis via down-regulating AKT/mTOR pathway. | (213) |
6. Conclusions
In conclusion, the radioresistance mechanisms of NSCLC are complex. Therefore, prior to radiotherapy gene sequencing should be performed for NSCLC patients to determine the type of mutation, or abnormally expressed genes, proteins, and signaling pathways, thus to develop more effective treatment strategies. In the early stage of radiotherapy, it is suggested to combine EGFR, KRAS and other mutant targeted drugs, drugs to improve DNA damage, immune checkpoint drugs or drugs to target hypoxia. In the middle and late stage of radiotherapy, it is suggested that the combination of drugs targeting EMT or regulating TME can improve the curative effect. TCM can run through the whole radiotherapy process. However, the specific mechanism of TCM in the sensitization of NSCLC radiotherapy needs to be further explored. The combination of effective small molecules extracted from TCM and radiotherapy may provide a new application prospect for the future clinical treatment of NSCLC.
Author contributions
TZ is responsible for literature review and article writing. LZ and JH are responsible for revising articles. ZM, YYL, YZ, and ZL are responsible for collecting and sorting materials. SZ, YC, and GZ are responsible for sorting charts. YQL provides ideas and guidance for the article. All authors contributed to the article and approved the submitted version.
Funding Statement
This work was supported by the National Natural Science Foundation of China (No.81973595), The basic research Innovation Group in Gansu (No.20JR10RA332), Provincial University industry support project in Gansu (No.2020C-15), and National Natural Science Foundation of China (No.82260882).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Koh PK, Faivre-Finn C, Blackhall FH, De Ruysscher D. Targeted agents in non-small cell lung cancer (NSCLC): Clinical developments and rationale for the combination with thoracic radiotherapy. Cancer Treat Rev (2012) 38(6):626–40. doi: 10.1016/j.ctrv.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 2. Wirsdörfer F, de Leve S, Jendrossek V. Combining radiotherapy and immunotherapy in lung cancer: Can we expect limitations due to altered normal tissue toxicity? Int J Mol Sci (2019) 20(1):24. doi: 10.3390/ijms20010024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sears CR, Cooney SA, Chin-Sinex H, Mendonca MS, Turchi JJ. DNA Damage response (DDR) pathway engagement in cisplatin radiosensitization of non-small cell lung cancer. DNA Repair (Amst). (2016) 40:35–46. doi: 10.1016/j.dnarep.2016.02.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Provencio M, Sánchez A. Therapeutic integration of new molecule-targeted therapies with radiotherapy in lung cancer. Transl Lung Cancer Res (2014) 3(2):89–94. doi: 10.3978/j.issn.2218-6751.2014.03.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hirsch FR, Scagliotti GV, Mulshine JL, Kwon R, Curran WJ, Wu YL, et al. Lung cancer: current therapies and new targeted treatments. Lancet. (2017) 389(10066):299–311. doi: 10.1016/S0140-6736(16)30958-8 [DOI] [PubMed] [Google Scholar]
- 6. Trakul N, Harris JP, Quynh-Thu Le, WY H, PG M, BW L, et al. Stereotactic ablative radiotherapy for reirradiation of locally recurrent lung tumors. J Thorac Oncol (2012) 7(9):1462–5. doi: 10.1097/JTO.0b013e31825f22ce [DOI] [PubMed] [Google Scholar]
- 7. Iyengar P, Zhang VE, Court L, Westover K, Yan YL, Lin MH, et al. Accelerated hypofractionated image-guided vs conventional radiotherapy for patients with stage II/III non-small cell lung cancer and poor performance status: A randomized clinical trial. JAMA Oncol (2021) 7(10):1497–505. doi: 10.1001/jamaoncol.2021.3186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Senthi S, Lagerwaard FJ, Haasbeek Cornelis JA, Slotman BJ, Senan S. Patterns of disease recurrence after stereotactic ablative radiotherapy for early stage non-small-cell lung cancer: a retrospective analysis. Lancet Oncol (2012) 13(8):802–9. doi: 10.1016/S1470-2045(12)70242-5 [DOI] [PubMed] [Google Scholar]
- 9. Sato K, Shimokawa T, Imai T. Difference in acquired radioresistance induction between repeated photon and particle irradiation. Front Oncol (2019) 9:1213. doi: 10.3389/fonc.2019.01213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Catton CN, Shultz DB. Should we expand the carbon ion footprint of prostate cancer? Lancet Oncol (2019) 20(5):608–9. doi: 10.1016/S1470-2045(19)30094-4 [DOI] [PubMed] [Google Scholar]
- 11. Bradley JD, Hu C, Komaki RR, Masters GA, Blumenschein GR, Schild SE, et al. Long-term results of NRG oncology RTOG 0617: Standard- versus high-dose chemoradiotherapy with or without cetuximab for unresectable stage III non-small-cell lung cancer. J Clin Oncol (2020) 38(7):706–14. doi: 10.1200/JCO.19.01162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Buckley AM, Lynam-Lennon N, O'Neill H, O'Sullivan J. Targeting hallmarks of cancer to enhance radiosensitivity in gastrointestinal cancers. Nat Rev Gastroenterol Hepatol (2020) 17(5):298–313. [DOI] [PubMed] [Google Scholar]
- 13. Lee SY, Jeong EK, Ju MK, Jeon HM, Kim MY, Kim CH, et al. Induction of metastasis, cancer stem cell phenotype, and oncogenic metabolism in cancer cells by ionizing radiation. Mol Cance. (2017) 16(1):10. doi: 10.1186/s12943-016-0577-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alhaddad L, Pustovalova M, Blokhina T, Chuprov-Netochin R, Osipov AN, Leonov S. IR-surviving NSCLC cells exhibit different patterns ofmolecular and cellular reactions relating to the multifraction irradiation regimen and p53-family proteins expression. Cancers (Basel) (2021) 13(11):2669. doi: 10.3390/cancers13112669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McKelvey KJ, Hudson AL, Back M, Eade T, Diakos CI. Radiation, inflammation and the immune response in cancer. Mamm Genome. (2018) 29(11-12):843–65. doi: 10.1007/s00335-018-9777-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nantajit D, Dong L, Jian JL. The network of epithelial–mesenchymal transition: potential new targets for tumor resistance. J Cancer Res Clin (2015) 141(10):1697–713. doi: 10.1007/s00432-014-1840-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Marie-Egyptienne DT, Lohse I, Hill RP. Cancer stem cells, the epithelial to mesenchymal transition (EMT) and radioresistance: Potential role of hypoxia. Cancer Lett (2013) 341(1):63–72. doi: 10.1016/j.canlet.2012.11.019 [DOI] [PubMed] [Google Scholar]
- 18. Barker HE, Paget JT, Khan AA, Harrington KJ. The tumour microenvironment after radiotherapy: Mechanisms of resistance and recurrence. Nat Rev Cancer. (2015) 15(7):409–25. doi: 10.1038/nrc3958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mittal A, Nenwani M, Sarangi I, Achreja A, Lawrence TS, Nagrath D. Radiotherapy-induced metabolic hallmarks in the tumor microenvironment. Trends Cancer. (2022) 8(10):1–15. doi: 10.1016/j.trecan.2022.05.005 [DOI] [PubMed] [Google Scholar]
- 20. Hanahan D. Hallmarks of cancer: New dimensions. Cancer Discovery (2022) 12(1):31–46. doi: 10.1158/2159-8290.CD-21-1059 [DOI] [PubMed] [Google Scholar]
- 21. Johung KL, Yao XP, Li FY, Yu JB, Gettinger SN, Goldberg S, et al. A clinical model for identifying radiosensitive tumor genotypes in non-small cell lung cancer. Clin Cancer Res (2013) 19(19):5523–32. [DOI] [PubMed] [Google Scholar]
- 22. Sad K, Parashar P, Tripathi P, Hungyo H, Sistla R, Soni R, et al. Prochlorperazine enhances radiosensitivity of non-small cell lung carcinoma by stabilizing GDP-bound mutant KRAS conformation. Free Radic Biol Med (2021) 177:299–312. doi: 10.1016/j.freeradbiomed.2021.11.001 [DOI] [PubMed] [Google Scholar]
- 23. Jiang WW, Jin GH, Cai FF, Chen X, Cao NN, Zhang XY, et al. Extracellular signal-regulated kinase 5 increases radioresistance of lung cancer cells by enhancing the DNA damage response. Exp Mol Med (2019) 51(2):1–20. doi: 10.1038/s12276-019-0209-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hanahan D, Weinberg RA. Hallmarks of cancer: The next generation. Cell. (2011) 144(5):646–74. doi: 10.1016/j.cell.2011.02.013 [DOI] [PubMed] [Google Scholar]
- 25. Haura EB, Cress WD, Chellappan S, Zheng Z, Bepler G. Antiapoptotic signaling pathways in non-small-cell lung cancer: Biology and therapeutic strategies. Clin Lung Cancer. (2004) 6(2):113–22. doi: 10.3816/CLC.2004.n.025 [DOI] [PubMed] [Google Scholar]
- 26. Olivares-Urbano MA, Griñán-Lisón C, Marchal JA, Núñez MI. CSC radioresistance: A therapeutic challenge to improve radiotherapy effectiveness in cancer. Cells. (2020) 9(7):1651. doi: 10.3390/cells9071651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Walsh JC, Lebedev A, Aten E, Madsen K, Marciano L, Kolb HC. The clinical importance of assessing tumor hypoxia: Relationship of tumor hypoxia to prognosis and therapeutic opportunities. Antioxid Redox Signal (2014) 21(10):1516–54. doi: 10.1089/ars.2013.5378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Salem A, Asselin MC, Reymen B, Jackson A, Lambin P, West CML, et al. Targeting hypoxia to improvenon-small cell lung cancer outcome. J Natl Cancer Inst (2018) 110(1):djx160. doi: 10.1093/jnci/djx160 [DOI] [PubMed] [Google Scholar]
- 29. Jansen J, Vieten P, Pagliari F, Hanley R, Marafioti MG, Tirinato L, et al. A novel analysis method for evaluating the interplay of oxygen and ionizing radiation at the gene level. Front Genet (2021) 12:597635. doi: 10.3389/fgene.2021.597635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang H, Mu XY, He H, Zhang XD. Cancer radiosensitizers. Trends Pharmacol Sci (2018) 39(1):24–48. doi: 10.1016/j.tips.2017.11.003 [DOI] [PubMed] [Google Scholar]
- 31. Havaki S, Kotsinas A, Chronopoulos E, Kletsas D, Georgakilas A, Gorgoulis VG. The role of oxidative DNA damage in radiation induced bystander effect. Cancer Lett (2015) 356(1):43–51. doi: 10.1016/j.canlet.2014.01.023 [DOI] [PubMed] [Google Scholar]
- 32. Barker HE, Paget JT, Khan AA, Harrington KJ. The tumour microenvironment after radiotherapy: Mechanisms of resistance and recurrence. Nat Rev Cancer. (2015) 15(7):409–25. doi: 10.1038/nrc3958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stingele J, Bellelli R, Boulton SJ. Mechanisms of DNA-protein crosslink repair. Nat Rev Mol Cell Biol (2017) 18(9):563–73. doi: 10.1038/nrm.2017.56 [DOI] [PubMed] [Google Scholar]
- 34. Smith J, Tho LM, Xu N, Gillespie DA. The ATM-Chk2 and ATR-Chk1 pathways in DNA damage signaling and cancer. Adv Cancer Res (2010) 108:73–112. doi: 10.1016/B978-0-12-380888-2.00003-0 [DOI] [PubMed] [Google Scholar]
- 35. Syed A, Tainer JA. The MRE11-RAD50-NBS1 complex conducts the orchestration of damage signaling and outcomes to stress in DNA replication and repair. Annu Rev Biochem (2018) 87:263–94. doi: 10.1146/annurev-biochem-062917-012415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zou N, Xie GZ, Cui TT, Srivastava AK, Qu MH, Yang LL, et al. DDB2 increases radioresistance of NSCLC cells by enhancing DNA damage responses. Tumor Biol (2016) 37(10):14183–91. doi: 10.1007/s13277-016-5203-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Choi SH, Yang H, Lee SH, Ki JH, Nam DH, Yoo HY. TopBP1 and claspin contribute to the radioresistance of lung cancer brain metastases. Mol Cancer. (2014) 13:211. doi: 10.1186/1476-4598-13-211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Burma S, Chen BP, Murphy M, Kurimasa A, Chen DJ. ATM Phosphorylates histone H2AX in response to DNA double-strand breaks. J Biol Chem (2001) 276:42462–7. doi: 10.1074/jbc.C100466200 [DOI] [PubMed] [Google Scholar]
- 39. Paull TT. Mechanisms of ATM activation. Annu Rev Biochem (2015) 84:711–38. doi: 10.1146/annurev-biochem-060614-034335 [DOI] [PubMed] [Google Scholar]
- 40. Torok JA, Oh P, Castle KD, Reinsvold M, Ma Y, Luo LX, et al. Deletion of atm in tumor but not endothelial cells improves radiation response in a primary mouse model of lung adenocarcinoma. Cancer Res (2019) 79(4):773–82. doi: 10.1158/0008-5472.CAN-17-3103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Koll TT, Feis SS, Wright MH, Teniola MM, Richardson MM, Robles AI, et al. HSP90 inhibitor, DMAG, synergizes with radiation of lung cancer cells by interfering with base excision and ATM-mediated DNA repair. Mol Cancer Ther (2008) 7(7):1985–92. doi: 10.1158/1535-7163.MCT-07-2104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gou W, Yu X, Wu S, Wu H, Chang H, Chen L, et al. Targeted inhibition of acidic nucleoplasmic DNA-binding protein 1 enhances radiosensitivity of non-small cell lung cancer. Cancer Lett (2022) 530:100–9. doi: 10.1016/j.canlet.2022.01.020 [DOI] [PubMed] [Google Scholar]
- 43. Cao K, Chen Y, Zhao S, Huang Y, Liu T, Liu H, et al. Sirt3 promoted DNA damage repair and radioresistance through ATM-Chk2 in non-small cell lung cancer cells. J Cancer. (2021) 12(18):5464–72. doi: 10.7150/jca.53173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zeng Y, Jie X, Wu B, Wu G, Liu L, Xu S. IQGAP3 interacts with Rad17 to recruit the Mre11-Rad50-Nbs1 complex and contributes to radioresistance in lung cancer. Cancer Lett (2020) 493:254–65. doi: 10.1016/j.canlet.2020.08.042 [DOI] [PubMed] [Google Scholar]
- 45. Zhang J, Wu Q, Zhu L, Xie S, Tu L, Yang Y, et al. SERPINE2/PN-1 regulates the DNA damage response and radioresistance by activating ATM in lung cancer. Cancer Lett (2022) 524:268–83. doi: 10.1016/j.canlet.2021.10.001 [DOI] [PubMed] [Google Scholar]
- 46. Lei X, Du L, Zhang P, Ma N, Liang Y, Han Y, et al. Knockdown GTSE1 enhances radiosensitivity in non-small-cell lung cancer through DNA damage repair pathway. J Cell Mol Med (2020) 24(9):5162–7. doi: 10.1111/jcmm.15165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cheng C, Pei X, Li SW, Yang J, Li C, Tang J, et al. CRISPR/Cas9 library screening uncovered methylated PKP2 as a critical driver of lung cancer radioresistance by stabilizing β-catenin. Oncogene. (2021) 40(16):2842–57. doi: 10.1038/s41388-021-01692-x [DOI] [PubMed] [Google Scholar]
- 48. Kaminskyy VO, Hååg P, Novak M, Végvári Á, Arapi V, Lewensohn R, et al. EPHA2 interacts with DNA-PK in cell nucleus and controls ionizing radiation responses in non-small cell lung cancer cells. Cancers (Basel). (2021) 13(5):1010. doi: 10.3390/cancers13051010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gong S, Li Y, Lv L, Men W. Restored microRNA-519a enhances the radiosensitivity of non-small cell lung cancer via suppressing EphA2. Gene Ther (2021) 29:1–13. doi: 10.1038/s41434-020-00213-x [DOI] [PubMed] [Google Scholar]
- 50. Yang X, Wang G, You J, Gu R, Xu X, Xu C, et al. High expression of cancer-IgG is associated with poor prognosis and radioresistance via PI3K/AKT/DNA-PKcs pathway regulation in lung adenocarcinoma. Front Oncol (2021) 11:675397. doi: 10.3389/fonc.2021.675397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yenerall P, Das AK, Wang S, Kollipara RK, Li LS, Villalobos P, et al. RUVBL1/RUVBL2 ATPase activity drives PAQosome maturation, DNA replication and radioresistance in lung cancer. Cell Chem Biol (2020) 27(1):105–121.e14. doi: 10.1016/j.chembiol.2019.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Aarts M, Sharpe R, Garcia-Murillas I, Gevensleben H, Hurd MS, Shumway SD, et al. Forced mitotic entry of s-phase cells as a therapeutic strategy induced by inhibition of WEE1. Cancer Discovery (2012) 2(6):524–39. doi: 10.1158/2159-8290.CD-11-0320 [DOI] [PubMed] [Google Scholar]
- 53. McCarthy N. Cell cycle: A WEE pointer. Nat Rev Cancer. (2012) 12(6):378–9. doi: 10.1038/nrc3286 [DOI] [PubMed] [Google Scholar]
- 54. Wang Q, Chen Y, Lu H, Wang H, Feng H, Xu J, et al. Quercetin radiosensitizes non-small cell lung cancer cells through the regulation of miR-16-5p/WEE1 axis. IUBMB Life (2020) 72(5):1012–22. doi: 10.1002/iub.2242 [DOI] [PubMed] [Google Scholar]
- 55. Aggarwal BB, Sung B. NF-κB in cancer: a matter of life and death. Cancer Discovery (2011) 1(6):469–71. doi: 10.1158/2159-8290.cd-11-0260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sergei IG, Florian R, Michael K. Immunity, inflammation, and cancer. Cell. (2010) 140(6):883–99. doi: 10.1016/j.cell.2010.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bai M, Ma X, Li X, Wang X, Mei Q, Li X, et al. The accomplices of NF-κB lead to radioresistance. Curr Protein Pept Sci (2015) 16:279–94. doi: 10.2174/138920371604150429152328 [DOI] [PubMed] [Google Scholar]
- 58. Harada D, Takigawa N, Kiura K. The role of STAT3 in non-small cell lung cancer. Cancers (Basel) (2014) 6(2):708–22. doi: 10.3390/cancers6020708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. You S, Li R, Park D, Xie M, Sica GL, Cao Y, et al. Disruption of STAT3 by niclosamide reverses radioresistance of human lung cancer. Mol Cancer Ther (2014) 13(3):606–16. doi: 10.1158/1535-7163.MCT-13-0608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Tsolou A, Liousia M, Kalamida D, Pouliliou S, Giatromanolaki A, Koukourakis M. Inhibition of IKK-NFκB pathway sensitizes lung cancer cell lines to radiation. Cancer Biol Med (2017) 14(3):293–301. doi: 10.20892/j.issn.2095-3941.2017.0049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Zhi-Wei. L, Yi-Ming. Z, Li-Ying. Z, Ting. Z, Yang-Yang. Li, Gu-Cheng. Z, et al. Duality of interactions between TGF-β and TNF-α during tumor formation. Front Immunol (2021) 12:810286(undefined). doi: 10.3389/fimmu.2021.810286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Yi-Ming. Z, Li-Ying. Z, Yang-Yang. Li, Heng. Z, Zhi-Ming. M, Zhi-Wei. L, et al. Radiation-induced bystander effect on the genome of bone marrow mesenchymal stem cells in lung cancer. Antioxid Redox Signal (2022). doi: 10.1089/ars.2022.0072. undefined(undefined), undefined. doi: 10.1089/ars.2022.0072 [DOI] [PubMed] [Google Scholar]
- 63. He K, Barsoumian HB, Hu Y, Sezen D, MD W, et al. Inhibition of STAT6 with antisense oligonucleotides enhances the systemic antitumor effects of radiotherapy and anti-PD1 in metastatic non-small cell lung cancer. Cancer Immunol Res (2023). undefined(undefined), undefined. doi: 10.1158/2326-6066.CIR-22-0547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Wang J, Han Q, Liu H, Luo H, Li L, Liu A, et al. Identification of radiotherapy-associated genes in lung adenocarcinoma by an integrated bioinformatics analysis approach. Front Mol Biosci (2021) 8:624575. doi: 10.3389/fmolb.2021.624575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Zhang F, Sang Y, Chen D, Wu X, Wang X, Yang W, et al. M2 macrophage-derived exosomal long non-coding RNA AGAP2-AS1 enhances radiotherapy immunity in lung cancer by reducing microRNA-296 and elevating NOTCH2. Cell Death Dis (2021) 12(5):467. doi: 10.1038/s41419-021-03700-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Zitvogel L, Kroemer G. Lower airway dysbiosis exacerbates lung cancer. Cancer Discovery (2021) 11(2):224–6. doi: 10.1158/2159-8290.CD-20-1641 [DOI] [PubMed] [Google Scholar]
- 67. Pinato DJ, Howlett S, Ottaviani D, Urus H, Patel A, Mineo T, et al. Association of prior antibiotic treatment with survival and response to immune checkpoint inhibitor therapy in patients with cancer. JAMA Oncol (2020) 6(2):302. doi: 10.1001/jamaoncol.2019.6921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Li. Y, Aitian. Li, Ying. W, Yi. Z. Intratumoral microbiota: roles in cancer initiation, development and therapeutic efficacy. Signal Transduct Target Ther (2023) 8(1):35. doi: 10.1038/s41392-022-01304-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Jin C, Lagoudas GK, Zhao C, Bullman S, Bhutkar A, Hu B, et al. Commensal microbiota promote lung cancer development via γδ T cells. Cell. (2019) 176(5):998–1013. doi: 10.1016/j.cell.2018.12.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Xiang L, Meng X. Emerging cellular and molecular interactions between the lung microbiota and lung diseases. Crit Rev Microbiol (2022) 48(5):577–610. doi: 10.1080/1040841X.2021.1992345 [DOI] [PubMed] [Google Scholar]
- 71. Tsay JC, Wu BG, Sulaiman I, Gershner K, Schluger R, Li Y, et al. Lower airway dysbiosis affects lung cancer progression. Cancer Discovery (2021) 11(2):293–307. doi: 10.1158/2159-8290.CD-20-0263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Yang Y, Chong Y, Chen M, Dai W, Zhou X, Ji Y, et al. Targeting lactate dehydrogenase a improves radiotherapy efficacy in non-small cell lung cancer: From bedside to bench. J Transl Med (2021) 19(1):170. doi: 10.1186/s12967-021-02825-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Meng MB, Wang HH, Guo WH, Wu ZQ, Zeng XL, Zaorsky NG, et al. Targeting pyruvate kinase M2 contributes to radiosensitivity of non-small cell lung cancer cells in vitro and in vivo . Cancer Lett (2015) 356:985–93. doi: 10.1016/j.canlet.2014.11.016 [DOI] [PubMed] [Google Scholar]
- 74. Tsolou A, Koparanis D, Lamprou I, Giatromanolaki A, Koukourakis MI. Increased glucose influx and glycogenesis in lung cancer cells surviving after irradiation. Int J Radiat Biol (2022) 1-10. doi: 10.1080/09553002.2022.2113837 [DOI] [PubMed] [Google Scholar]
- 75. Lei G, Zhang Y, Koppula P, Liu X, Zhang J, Lin SH, et al. The role of ferroptosis in ionizing radiation-induced cell death and tumor suppression. Cell Res (2020) 30(2):146–62. doi: 10.1038/s41422-019-0263-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Tirinato L, Marafioti MG, Pagliari F, Jansen J, Aversa I, Hanley R, et al. Lipid droplets and ferritin heavy chain: A devilish liaison in human cancer cell radioresistance. Elife. (2021) 10:e72943. doi: 10.7554/eLife.72943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lee S, Kim D, Kang J, Kim E, Kim W, Youn H, et al. Surfactant protein b suppresses lung cancer progression by inhibiting secretory phospholipase A2 activity and arachidonic acid production. Cell Physiol Biochem (2017) 42(4):1684–700. doi: 10.1159/000479418 [DOI] [PubMed] [Google Scholar]
- 78. Singh B, Patwardhan RS, Jayakumar S, Sharma D, Sandur SK. Oxidative stress associated metabolic adaptations regulate radioresistance in human lung cancer cells. J Photochem Photobiol B (2020) 213:112080. doi: 10.1016/j.jphotobiol.2020.112080 [DOI] [PubMed] [Google Scholar]
- 79. Hao CC, Luo JN, Xu CY, Zhao XY, Zhong ZB, Hu XN, et al. TRIAP1 knockdown sensitizes non-small cell lung cancer to ionizing radiation by disrupting redox homeostasis. Thorac Cancer. (2020) 11(4):1015–25. doi: 10.1111/1759-7714.13358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Luo H, Wang L, Schulte BA, Yang A, Tang S, Wang GY. Resveratrol enhances ionizing radiation-induced premature senescence in lung cancer cells. Int J Oncol (2013) 43(6):1999–2006. doi: 10.3892/ijo.2013.2141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Tsolou A, Lamprou I, Fortosi AO, Liousia M, Giatromanolaki A, Koukourakis MI. 'Stemness' and 'senescence' related escape pathways are dose dependent in lung cancer cells surviving post irradiation. Life Sci (2019) 232:116562. doi: 10.1016/j.lfs.2019.116562 [DOI] [PubMed] [Google Scholar]
- 82. Qiao L, Chen Y, Liang N, Xie J, Deng G, Chen F, et al. Targeting epithelial-to-mesenchymal transition in radioresistance: crosslinked mechanisms and strategies. Front Oncol (2022) 12:775238. doi: 10.3389/fonc.2022.775238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Eckert MA, Lwin TM, Chang AT, Kim J, Danis E, Ohno-Machado L, et al. Twist1-induced invadopodia formation promotes tumor metastasis. Cancer Cell (2011) 19(3):372–86. doi: 10.1016/j.ccr.2011.01.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Cui YH, Kang JH, Suh Y, Zhao Y, Yi JM, Bae IH, et al. Loss of FBXL14 promotes mesenchymal shift and radioresistance of non-small cell lung cancer by TWIST1 stabilization. Signal Transduct Target Ther (2021) 6(1):272. doi: 10.1038/s41392-021-00599-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Gomez-Casal R, Bhattacharya C, Ganesh N, Bailey L, Basse P, Gibson M, et al. Non-small cell lung cancer cells survived ionizing radiation treatment display cancer stem cell and epithelial-mesenchymal transition phenotypes. Mol Cancer. (2013) 12(1):94. doi: 10.1186/1476-4598-12-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Dadrich M, Nicolay NH, Flechsig P, Bickelhaupt S, Hoeltgen L, Roeder F, et al. Combined inhibition of TGFβ and PDGF signaling attenuates radiation-induced pulmonary fibrosis. Oncoimmunology. (2016) 5(5):e1123366. doi: 10.1080/2162402X.2015.1123366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Li Y, Sun C, Tan Y, Zhang H, Li Y, Zou H. ITGB1 enhances the radioresistance of human non-small celllung cancer cells by modulating the DNA damage response and YAP1-induced epithelial-mesenchymal transition. Int J Biol Sci (2021) 17(2):635–50. doi: 10.7150/ijbs.52319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Kim E, Youn H, Kwon T, Son B, Kang J, Yang HJ, et al. PAK1 tyrosine phosphorylation is required to induce epithelial-mesenchymal transition and radioresistance in lung cancer cells. Cancer Res (2014) 74(19):5520–31. doi: 10.1158/0008-5472.CAN-14-0735 [DOI] [PubMed] [Google Scholar]
- 89. Tan S, Yi P, Wang H, Xia L, Han Y, Wang H, et al. RAC1 involves in the radioresistance by mediating epithelial-mesenchymal transition in lung cancer. Front Oncol (2020) 10:649. doi: 10.3389/fonc.2020.00649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Yao YH, Cui Y, Qiu XN, Zhang LZ, Zhang W, Li H, et al. Attenuated lkb1-sik1 signaling promotes epithelial-mesenchymal transition and radioresistance of non–small cell lung cancer cells. Chin J Cancer. (2016) 35(10):9. doi: 10.1186/s40880-016-0113-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Fu W, Zhao J, Hu W, Dai L, Jiang Z, Zhong S, et al. LINC01224/ZNF91 promote stem cell-like properties and drive radioresistance in non-small cell lung cancer. Cancer Manag Res (2021) 13:5671–81. doi: 10.2147/CMAR.S313744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Cancer Genome Atlas Research Network . Comprehensive molecular profiling of lung adenocarcinoma. Nature (2014) 511(7511):543–50. doi: 10.1038/nature13385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Yang LQ, Shi PF, Zhao GC, Xu J, Peng W, Zhang JY, et al. Targeting cancer stem cell pathways for cancer therapy. Signal Transduct Target Ther (2020) 5(1):8. doi: 10.1038/s41392-020-0110-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Hsu F, Sit D, Pastuch A, Dingler A, Atwal P. Lung cancer epidermal growth factor receptor mutations and radiotherapy response: A multicentre clinical study. Clin Transl Radiat Oncol (2021) 30:15–8. doi: 10.1016/j.ctro.2021.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Butkiewicz D, Krześniak M, Gdowicz-Kłosok A, Giglok M, Marszałek-Zeńczak M, Suwiński R. EGFR polymorphisms in gene predict clinical outcome in unresectable non-small cell lung cancer treated with radiotherapy and platinum-based chemoradiotherapy. Int J Mol Sci (2021) 22(11):5605. doi: 10.3390/ijms22115605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Zhu DQ, Liu Y, Yu ZJ, Zhang RH, Li AW, Gong FY, et al. The diverse analysis identifies mutated KRAS associated with radioresistance in non-small cell lung cancer. World J Oncol (2022) 13(2):84–95. doi: 10.14740/wjon1465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Binkley MS, Jeon YJ, Nesselbush M, Moding EJ, Nabet BY, Almanza D, et al. KEAP1/NFE2L2 mutations predict lung cancer radiation resistance that can be targeted by glutaminase inhibition. Cancer Discovery (2020) 10(12):1826–41. doi: 10.1158/2159-8290.CD-20-0282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Kinslow CJ, Kumar P, Cai LL, Sun RC, Chaudhary KR, Cheng SK. NRF2-pathway mutations predict radioresistance in non-small cell lung cancer. Transl Lung Cancer Res (2022) 11(7):1510–3. doi: 10.21037/tlcr-22-292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Pustovalova M, Alhaddad L, Smetanina N, Chigasova A, Blokhina T, Chuprov-Netochin R, et al. The p53-53BP1-related survival of A549 and H1299 human lung cancer cells after multifractionated radiotherapy demonstrated different response to additional acute X-ray exposure. Int J Mol Sci (2020) 21(9):3342. doi: 10.3390/ijms21093342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Gurtner K, Kryzmien Z, Koi L, Wang M, Benes CH, Hering S, et al. Radioresistance of kras/tp53-mutated lung cancer can be overcome by radiation dose escalation or egfr tyrosine kinase inhibition. vivo. Int J Cancer. (2020) 147(2):472–7. doi: 10.1002/ijc.32598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc (2008) 83(5):584–94. doi: 10.4065/83.5.584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Mendelsohn J, Baselga J. Status of epidermal growth factor receptor antagonists in the biology and treatment of cancer. J Clin Oncol (2003) 21(14):2787–99. doi: 10.1200/JCO.2003.01.504 [DOI] [PubMed] [Google Scholar]
- 103. Das AK, Chen BP, Story MD, Sato M, Minna JD, Chen DJ, et al. Somatic mutations in the tyrosine kinase domain of epidermal growth factor receptor (EGFR) abrogate EGFR-mediated radioprotection in non-small cell lung carcinoma. Cancer Res (2007) 67(11):5267–74. doi: 10.1158/0008-5472.CAN-07-0242 [DOI] [PubMed] [Google Scholar]
- 104. Chen GD, Kong PZ, Yang MM, Hu WL, Prise KM, Yu KN, et al. Golgi phosphoprotein 3 confers radioresistance via stabilizing EGFR in lung adenocarcinoma. Int J Radiat Oncol Biol Phys (2022) 112(5):1216–28. doi: 10.1016/j.ijrobp.2021.11.023 [DOI] [PubMed] [Google Scholar]
- 105. Liang K, Ang KK, Milas L, Hunter N, Fan Z. The epidermal growth factor receptor mediates radioresistance. Int J Radiat Oncol Biol Phys (2003) 57(1):246–54. doi: 10.1016/s0360-3016(03)00511-x [DOI] [PubMed] [Google Scholar]
- 106. LoRusso PM. Inhibition of the PI3K/AKT/mTOR pathway in solid tumors. J Clin Oncol (2016) 34(31):3803–15. doi: 10.1200/JCO.2014.59.0018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Schuurbiers OC, Kaanders JH, van der Heijden H, Dekhuijzen RP, Oyen WJ, Bussink J. The PI3-K/AKT-pathway and radiation resistance mechanisms in non-small cell lung cancer. J Thorac Oncol (2009) 4(6):761–7. doi: 10.1097/JTO.0b013e3181a1084f [DOI] [PubMed] [Google Scholar]
- 108. Raghav KP, Gonzalez-Angulo AM, Blumenschein GR. Role of HGF/MET axis in resistance of lung cancer to contemporary management. Transl Lung Cancer Res (2012) 1(3):179–93. doi: 10.3978/j.issn.2218-6751.2012.09.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Califano R, Landi L, Cappuzzo F. Prognostic and predictive value of K-RAS mutations in non-small cell lung cancer. Drugs. (2012) 72(1):28–36. doi: 10.2165/1163012-S0-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 110. Wang M, Kern AM, Hülskötter M, Greninger P, Singh A, Pan YF, et al. EGFR-mediated chromatin condensation protects KRAS-mutant cancer cells against ionizing radiation. Cancer Res (2014) 74(10):2825–34. doi: 10.1158/0008-5472.CAN-13-3157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Hu JF, Zhang ZG, Zhao L, Li L, Zuo W, Han L. High expression of RAD51 promotes DNA damage repair and survival in KRAS-mutant lung cancer cells. BMB Rep (2019) 52(2):151–6. doi: 10.5483/BMBRep.2019.52.2.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wang M, Han J, Marcar L, Black J, Liu Q, Li XY, et al. Radiation resistance in KRAS-mutated lung cancer is enabled by stem-like properties mediated by an osteopontin-EGFR pathway. Cancer Res (2017) 77(8):2018–28. doi: 10.1158/0008-5472.CAN-16-0808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Dempke WC, Reck M. KEAP1/NRF2 (NFE2L2) mutations in NSCLC-fuel for a superresistant phenotype? Lung Cancer. (2021) 159(2021):10–7. doi: 10.1016/j.lungcan.2021.07.006 [DOI] [PubMed] [Google Scholar]
- 114. Jeong Y, Hoang NT, Lovejoy A, Stehr H, Newman AM, Gentles AJ, et al. Role of KEAP1/NRF2 and TP53 mutations in lung squamous cell carcinoma development and radiotherapy rresponse prediction. Cancer Discovery. (2017) 7(1):86–101. doi: 10.1158/2159-8290.CD-16-0127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Pillai R, Hayashi M, Zavitsanou AM, Papagiannakopoulos T. NRF2: KEAPing tumors protected. Cancer Discovery (2022) 12(3):625–43. doi: 10.1158/2159-8290.CD-21-0922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Lee SL, Ryu H, Son AR, Seo B, Kim J, Jung SY, et al. TGF-β and hypoxia/reoxygenation promote radioresistance of A549 lung cancer cells through activation of Nrf2 and EGFR. Oxid Med Cell Longev (2016) 2016:6823471. doi: 10.1155/2016/6823471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Liu YQ, Gu W. p53 in ferroptosis regulation: The new weapon for the old guardian. Cell Death Differ (2022) 29(5):895–910. doi: 10.1038/s41418-022-00943-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Bieging K, Mello S, Attardi L. Unravelling mechanisms of p53-mediated tumour suppression. Nat Rev Cancer. (2014) 14(5):359–70. doi: 10.1038/nrc3711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Moretti L, Li B, Kim KW, Chen HD, Lu B. AT-101, a pan-Bcl-2 inhibitor, leads to radiosensitization of non-small cell lung cancer. J Thorac Oncol (2010) 5(5):680–7. doi: 10.1097/JTO.0b013e3181d6e08e [DOI] [PubMed] [Google Scholar]
- 120. Tu H, Costa M. XIAP's profile in human cancer. Biomolecules. (2020) 10(11):1493. doi: 10.3390/biom10111493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Sato Y, Yoshino H, Kazama Y, Kashiwakura I. Involvement of caspase-8 in apoptosis enhancement by cotreatment with retinoic acid-inducible gene-i-like receptor agonist and ionizing radiation in human non-small cell lung cancer. Mol Med Rep (2018) 18(6):5286–94. doi: 10.3892/mmr.2018.9536 [DOI] [PubMed] [Google Scholar]
- 122. Lu B, Mu Y, Cao C, Zeng FH, Schneider S, Tan JH, et al. Survivin as a therapeutic target for radiation sensitization in lung cancer. Cancer Res (2004) 64(8):2840–5. doi: 10.1158/0008-5472.can-03-3547 [DOI] [PubMed] [Google Scholar]
- 123. Sun H, Du Y, Yao M, Wang Q, Ji K, Du L, et al. cIAP1/2 are involved in the radiosensitizing effect of birinapant on NSCLC cell line in vitro . J Cell Mol Med (2021) 25(13):6125–36. doi: 10.1111/jcmm.16526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Yin H, Ma JQ, Chen L, Piao SQ, Zhang Y, Zhang SL, et al. MiR-99a enhances the radiation sensitivity of non-small cell lung cancer by targeting mTOR. Cell Physiol Biochem (2018) 46(2):471–81. doi: 10.1159/000488615 [DOI] [PubMed] [Google Scholar]
- 125. Lee HC, Her NG, Kang D, Jung SH, Shin J, Lee M, et al. Radiation-inducible miR-770-5p sensitizes tumors to radiation through direct targeting of PDZ-binding kinase. Cell Death Dis (2017) 8(3):e2693. doi: 10.1038/cddis.2017.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Yuan Y, Liao H, Pu Q, Ke XX, Hu XT, Ma YF, et al. miR-410 induces both epithelial-mesenchymal transition and radioresistance through activation of the PI3K/mTOR pathway in non-small cell lung cancer. Signal Transduct Target Ther (2020) 5(1):85. doi: 10.1038/s41392-020-0182-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Tang YT, Cui YY, Li ZP, Jiao ZQ, Zhang Y, He Y, et al. Radiation-induced miR-208a increases the proliferation and radioresistance by targeting p21 in human lung cancer cells. J Exp Clin Cancer Res (2016) 35:7. doi: 10.1186/s13046-016-0285-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Clarke MF, Fuller M. Stem cells and cancer: Two faces of eve. Cell. (2006) 124(6):1111–5. doi: 10.1016/j.cell.2006.03.011 [DOI] [PubMed] [Google Scholar]
- 129. Schulz A, Meyer F, Dubrovska A, Borgmann K. Cancer stem cells and radioresistance: DNA repair and beyond. Cancers (Basel). (2019) 11(6):862. doi: 10.3390/cancers11060862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Geng YY, Amante JJ, Goel HL, Zhang XZ, Walker MR, Luther DC, et al. Differentiation of cancer stem cells through nanoparticle surface engineering. ACS Nano. (2020) 14(11):15276–85. doi: 10.1021/acsnano.0c05589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Paul R, Dorsey JF, Fan Y. Cell plasticity, senescence, and quiescence in cancer stem cells: Biological and therapeutic implications. Pharmacol Ther (2022) 231:107985. doi: 10.1016/j.pharmthera.2021.107985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Jang YY, Sharkis SJ. A low level of reactive oxygen species selects for primitive hematopoietic stem cells that may reside in the low-oxygenic niche. Blood. (2007) 110(8):3056–63. doi: 10.1182/blood-2007-05-087759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Lendeckel U, Wolke C. Redox-regulation in cancer stem cells. Biomedicines (2022) 10(10):2413. doi: 10.3390/biomedicines10102413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Ryoo I, Lee S, Kwak MK. Redox modulating NRF2: A potential mediator of cancer stem cell resistance. Oxid Med Cell Longev (2016) 2016:2428153. doi: 10.1155/2016/2428153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Chang L, Graham P, Hao JL, Ni J, Deng JL, Bucci J, et al. Cancer stem cells and signaling pathways in radioresistance. Oncotarget. (2016) 7(10):11002–17. doi: 10.18632/oncotarget.6760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Bao SD, Wu QL, McLendon RE, Hao YL, Shi Q, Hjelmeland AB, et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. (2006) 444(7120):756–60. doi: 10.1038/nature05236 [DOI] [PubMed] [Google Scholar]
- 137. Desai A, Webb B, Gerson SL. CD133+ cells contribute to radioresistance via altered regulation of DNA repair genes in human lung cancer cells. Radiother Oncol (2014) 110(3):538–45. doi: 10.1016/j.radonc.2013.10.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Moore N, Lyle S. Quiescent, slow-cycling stem cell populations in cancer: a review of the evidence and discussion of significance. J Oncol (2011) 2011:396076. doi: 10.1155/2011/396076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Krause M, Yaromina A, Eicheler W, Koch U, Baumann M. Cancer stem cells: targets and potential biomarkers for radiotherapy. Clin Cancer Res (2011) 17(23):7224–9. doi: 10.1158/1078-0432.CCR-10-2639 [DOI] [PubMed] [Google Scholar]
- 140. Baumann M, Krause M. CD44: a cancer stem cell-related biomarker with predictive potential for radiotherapy. Clin Cancer Res (2010) 16(21):5091–3. doi: 10.1158/1078-0432.CCR-10-2244 [DOI] [PubMed] [Google Scholar]
- 141. Hu B, Ma YY, Yang Y, Zhang LJ, Han HB, Chen JF. CD44 promotes cell proliferation in non-small cell lung cancer. Oncol Lett (2018) 15(4):5627–33. doi: 10.3892/ol.2018.8051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Kong T, Ahn R, Yang KN, Zhu XB, Fu Z, Morin G, et al. CD44 promotes PD-L1 expression and its tumor-intrinsic function in breast and lung cancers. Cancer Res (2020) 80(3):444–57. doi: 10.1158/0008-5472.CAN-19-1108 [DOI] [PubMed] [Google Scholar]
- 143. Bayer C, Shi K, Astner ST, Maftei CA, Vaupel P. Acute versus chronic hypoxia: why a simplified classification is simply not enough. Int J Radiat Oncol Biol Phys (2011) 80(4):965–8. doi: 10.1016/j.ijrobp.2011.02.049 [DOI] [PubMed] [Google Scholar]
- 144. Telarovic I, Wenger RH, Pruschy M. Interfering with tumor hypoxia for radiotherapy optimization. J Exp Clin Cancer Res (2021) 40(1):197. doi: 10.1186/s13046-021-02000-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Sun JC, He F, Yi W, Wan MH, Li R, Wei X, et al. High expression of hif-2α and its anti-radiotherapy effect in lung cancer stem cells. Genet Mol Res (2015) 14(4):18110–20. doi: 10.4238/2015.December.22.37 [DOI] [PubMed] [Google Scholar]
- 146. Wang Y, Roche O, Yan MS, Finak G, Evans AJ, Metcalf JL, et al. Regulation of endocytosis via the oxygen-sensing pathway. Nat Med (2009) 15(3):319–24. doi: 10.1038/nm.1922 [DOI] [PubMed] [Google Scholar]
- 147. Downes NL, Laham-Karam N, Kaikkonen MU, Ylä-Herttuala S. Differential but complementary HIF1α and HIF2α transcriptional regulation. Mol Ther (2018) 26(7):1735–45. doi: 10.1016/j.ymthe.2018.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Gonzalez FJ, Xie C, Jiang CT. The role of hypoxia-inducible factors in metabolic diseases. Nat Rev Endocrinol (2018) 15(1):21–32. doi: 10.1038/s41574-018-0096-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Semenza GL. Targeting HIF-1 for cancer therapy. Nat Rev Cancer. (2003) 3(10):721–32. doi: 10.1038/nrc1187 [DOI] [PubMed] [Google Scholar]
- 150. Uniacke J, Holterman CE, Lachance G, Franovic A, Jacob MD, Fabian MR, et al. An oxygen-regulated switch in the protein synthesis machinery. Nature. (2012) 486(7401):126–9. doi: 10.1038/nature11055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Choueiri TK, Kaelin WG. Targeting the HIF2-VEGF axis in renal cell carcinoma. Nat Med (2020) 26(10):1519–30. doi: 10.1038/s41591-020-1093-z [DOI] [PubMed] [Google Scholar]
- 152. Moeller BJ, Cao YT, Li CY, Dewhirst MW. Radiation activates HIF-1 to regulate vascular radiosensitivity in tumors: Role of reoxygenation, free radicals, and stress granules. Cancer Cell (2004) 5(5):429–41. doi: 10.1016/s1535-6108(04)00115-1 [DOI] [PubMed] [Google Scholar]
- 153. Moreno RE, Groot AJ, Yaromina A, Hendrickx TC, Barbeau LM, Giuranno L, et al. HIF-1α and HIF-2α differently regulate the radiation sensitivity of NSCLC cells. Cells. (2019) 8(1):45. doi: 10.3390/cells8010045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Grosso S, Doyen J, Parks SK, Bertero T, Paye A, Cardinaud B, et al. MiR-210 promotes a hypoxic phenotype and increases radioresistance in human lung cancer cell lines. Cell Death Dis (2013) 4(3):e544. doi: 10.1038/cddis.2013.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Xu LM, Yu H, Yuan YJ, Zhang J, Ma Y, Cao XC, et al. Overcoming of radioresistance in non-small cell lung cancer by microRNA-320a through HIF1α-suppression mediated methylation of PTEN. Front Cell Dev Biol (2020) 8:553733. doi: 10.3389/fcell.2020.553733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Isla D, De Las PR, Insa A, Marsé R, Martínez-Banaclocha N, Mut P, et al. Oral vinorelbine versus etoposide with cisplatin and chemo-radiation as treatment in patients with stage III non-small cell lung cancer: A randomized phase II (RENO study). Lung Cancer. (2019) 135:161–8:135. doi: 10.1016/j.lungcan.2018.11.041 [DOI] [PubMed] [Google Scholar]
- 157. Shaverdian N, Lisberg AE, Bornazyan K, Veruttipong D, Goldman JW, Formenti SC, et al. Previous radiotherapy and the clinical activity and toxicity of pembrolizumab in the treatment of non-small-cell lung cancer: A secondary analysis of the KEYNOTE-001 phase 1 trial. Lancet Oncol (2017) 18(7):895–903. doi: 10.1016/S1470-2045(17)30380-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Kong Y, Xu C, Sun X, Sun H, Zhao X, He N, et al. BLM helicase inhibition synergizes with PARP inhibition to improve the radiosensitivity of olaparib resistant non-small cell lung cancer cells by inhibiting homologous recombination repair. Cancer Biol Med (2021) 19(8):1150–71. doi: 10.20892/j.issn.2095-3941.2021.0178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Zhang N, Gao Y, Zeng Z, Luo Y, Xie C. PARP inhibitor niraparib as a radiosensitizer promotes antitumor immunity of radiotherapy in EGFR-mutated non-small cell lung cancer. Clin Transl Oncol (2021) 23(9):1827–37. doi: 10.1007/s12094-021-02591-z [DOI] [PubMed] [Google Scholar]
- 160. Tang S, Li Z, Yang L, Shen L, Wang Y. A potential new role of ATM inhibitor in radiotherapy: Suppressing ionizing radiation-activated EGFR. Int J Radiat Biol (2020) 96(4):461–8. doi: 10.1080/09553002.2020.1707325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Fok JHL, Ramos-Montoya A, Vazquez-Chantada M, Wijnhoven PWG, Follia V, James N, et al. AZD7648 is a potent and selective DNA-PK inhibitor that enhances radiation, chemotherapy and olaparib activity. Nat Commun (2019) 10(1):5065. doi: 10.1038/s41467-019-12836-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Ding X, Cheng J, Pang Q, Wei X, Zhang X, Wang P, et al. BIBR1532, a selective telomerase inhibitor, enhances radiosensitivity of non-small cell lung cancer through increasing telomere dysfunction and ATM/CHK1 inhibition. Int J Radiat Oncol Biol Phys (2019) 105(4):861–74. doi: 10.1016/j.ijrobp.2019.08.009 [DOI] [PubMed] [Google Scholar]
- 163. Wang J, Wang Y, Mei H, Yin Z, Geng Y, Zhang T, et al. The BET bromodomain inhibitor JQ1 radiosensitizes non-small cell lung cancer cells by upregulating p21. Cancer Lett (2017) 391:141–51. doi: 10.1016/j.canlet.2017.01.031 [DOI] [PubMed] [Google Scholar]
- 164. Fernández-Aroca DM, Roche O, Sabater S, Pascual-Serra R, Ortega-Muelas M, Sánchez Pérez I, et al. P53 pathway is a major determinant in the radiosensitizing effect of palbociclib: Implication in cancer therapy. Cancer Lett (2019) 451:23–33. doi: 10.1016/j.canlet.2019.02.049 [DOI] [PubMed] [Google Scholar]
- 165. Naz S, Sowers A, Choudhuri R, Wissler M, Gamson J, Mathias A, et al. Abemaciclib, a selective CDK4/6 inhibitor enhances the radiosensitivity of non-small cell lung cancer in vitro and in vivo . Clin Cancer Res (2018) 24(16):3994–4005. doi: 10.1158/1078-0432.CCR-17-3575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Wang R, Peng S, Zhang X, Wu Z, Duan H, Yuan Y, et al. Inhibition of NF-κB improves sensitivity to irradiation and EGFR-TKIs and decreases irradiation-induced lung toxicity. Int J Cancer. (2019) 144:200–9. doi: 10.1002/ijc.31907 [DOI] [PubMed] [Google Scholar]
- 167. Du S, Bouquet S, Lo CH, Pellicciotta I, Bolourchi S, Parry R, et al. Attenuation of the DNA damage response by transforming growth factor-β inhibitors enhances radiation sensitivity of non–small-cell lung cancer cells in vitro and in vivo . Int J Radiat Oncol (2015) 91(1):91–9. doi: 10.1016/j.ijrobp.2014.09.026 [DOI] [PubMed] [Google Scholar]
- 168. Sun Y, Moretti L, Giacalone NJ, Schleicher S, Speirs CK, Carbone DP, et al. Inhibition of JAK2 signaling by TG101209 enhances radiotherapy in lung cancer models. J Thorac Oncol (2011) 6(4):699–706. doi: 10.1097/JTO.0b013e31820d9d11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Gong X, Li X, Jiang T, Xie H, Zhu Z, Zhou F, et al. Combined radiotherapy and anti-PD-L1 antibody synergistically enhances antitumor effect in non-small cell lung cancer. J Thorac Oncol (2017) 12(7):1085–97. doi: 10.1016/j.jtho.2017.04.014 [DOI] [PubMed] [Google Scholar]
- 170. Bozorgmehr F, Hommertgen A, Krisam J, Lasitschka F, Kuon J, Maenz M, et al. Fostering efficacy of anti-PD-1-treatment: Nivolumab plus radiotherapy in advanced non-small cell lung cancer - study protocol of the FORCE trial. BMC Cancer. (2019) 19(1):1074. doi: 10.1186/s12885-019-6205-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Welsh J, Menon H, Chen D, Verma V, Heymach JV. Pembrolizumab with or without radiation therapy for metastatic non-small cell lung cancer: A randomized phase I/II trial. J Immunother Cancer. (2020) 8(2):e001001. doi: 10.1136/jitc-2020-001001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Formenti SC, Rudqvist NP, Golden E, Cooper B, Wennerberg E, Lhuillier C, et al. Radiotherapy induces responses of lung cancer to CTLA-4 blockade. Nat Med (2018) 24(12):1845–51. doi: 10.1038/s41591-018-0232-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Zheng LP, Wang Y, Xu Z, Yang Q, Zhu G, Liao XY, et al. Concurrent EGFR-TKI and thoracic radiotherapy as first-line treatment for stage IV non-small cell lung cancer harboring EGFR active mutations. Oncologist. (2019) 24(8):1031–e612. doi: 10.1634/theoncologist.2019-0285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Francis DM, Huang S, Armstrong EA, Werner LR, Hullett C, Li C, et al. Pan-HER inhibitor augments radiation response in human lung and head and neck cancer models. Clin Cancer Res (2016) 22(3):633–43. doi: 10.1158/1078-0432.CCR-15-1664 [DOI] [PubMed] [Google Scholar]
- 175. Hu S, Fu W, Li T, Yuan Q, Wang F, Lv G, et al. Antagonism of EGFR and notch limits resistance to EGFR inhibitors and radiation by decreasing tumor-initiating cell frequency. Sci Transl Med (2017) 9(380):1–15. doi: 10.1126/scitranslmed.aag0339 [DOI] [PubMed] [Google Scholar]
- 176. Zhang P, Song E, Jiang M, Song Y. Celecoxib and afatinib synergistic enhance radiotherapy sensitivity on human non-small cell lung cancer A549 cells. Int J Radiat Biol (2021) 97(2):170–8. doi: 10.1080/09553002.2021.1846817 [DOI] [PubMed] [Google Scholar]
- 177. Park D, Magis AT, Li R, Owonikoko TK, Sica GL, Sun SY, et al. Novel small-molecule inhibitors of bcl-XL to treat lung cancer. Cancer Res (2013) 73:5485–96. doi: 10.1158/0008-5472.CAN-12-2272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Lee JM, Kim HS, Kim A, Chang YS, Lee JG, Cho J, et al. ABT-737, a BH3 mimetic, enhances the therapeutic effects of ionizing radiation in K-ras mutant non-small cell lung cancer preclinical model. Yonsei Med J (2022) 63(1):16–25. doi: 10.3349/ymj.2022.63.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Park D, Anisuzzaman AS, Magis AT, Chen G, Xie M, Zhang G, et al. Discovery of small molecule bak activator for lung cancer therapy. Theranostics. (2021) 11:8500–16. doi: 10.7150/thno.60349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Ritter V, Krautter F, Klein D, Jendrossek V, Rudner J. Bcl-2/Bcl-xL inhibitor ABT-263 overcomes hypoxia-driven radioresistence and improves radiotherapy. Cell Death Dis (2021) 12(7):694. doi: 10.1038/s41419-021-03971-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Jiang S, Zhou Y, Zou L, Chu L, Chu X, Ni J, et al. Low- dose apatinib promotes vascular normalization and hypoxia reduction and sensitizes radiotherapy in lung cancer. Cancer Med (2022) 00:1–12. doi: 10.1002/cam4.5113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Zhai Y, Ma H, Hui Z, Zhao L, Li D, Liang J, et al. HELPER study: A phase II trial of continuous infusion of endostar combined with concurrent etoposide plus cisplatin and radiotherapy for treatment of unresectable stage III non-small-cell lung cancer. Radiother Oncol (2019) 131:27–34. doi: 10.1016/j.radonc.2018.10.032 [DOI] [PubMed] [Google Scholar]
- 183. Kong FM, Hayman JA, Griffith KA, Kalemkerian GP, Arenberg D, Lyons S, et al. Final toxicity results of a radiation-dose escalation study in patients with non-small-cell lung cancer (NSCLC): predictors for radiation pneumonitis and fibrosis. Int J Radiat Oncol Biol Phys (2006) 65(4):1075–86. doi: 10.1016/j.ijrobp.2006.01.051 [DOI] [PubMed] [Google Scholar]
- 184. Liu W, Yang BB, Yang L, Kaur J, Jessop C, Fadhil R, et al. Therapeutic effects of ten commonly used Chinese herbs and their bioactive compounds on cancers. Evid Based Complement Alternat Med (2019) 2019:6057837. doi: 10.1155/2019/6057837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Yang Y, Li N, Wang TM, Di L. Natural products with activity against lung cancer: A review focusing on the tumor microenvironment. Int J Mol Sci (2021) 22(19):10827. doi: 10.3390/ijms221910827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Li SG, Chen HY, Ou-Yang CS, Wang XX, Yang ZJ, Tong Y, et al. The efficacy of Chinese herbal medicine as an adjunctive therapy for advanced non-small cell lung cancer: a systematic review and meta-analysis. PloS One (2013) 8(2):e57604. doi: 10.1371/journal.pone.0057604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Balakrishnan B, Liang Q, Fenix K, Tamang B, Hauben E, Ma L, et al. Combining the anticancer and immunomodulatory effects of Astragalus and shiitake as an integrated therapeutic approach. Nutrients. (2021) 13(8):2564. doi: 10.3390/nu13082564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Cao A, He H, Wang Q, Li L, An Y, Zhou X. Evidence of astragalus injection combined platinum-based chemotherapy in advanced nonsmall cell lung cancer patients: A systematic review and meta-analysis. Medicine. (2019) 98(11):e14798. doi: 10.1097/MD.0000000000014798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Zhang YM, Zhang LY, Zhou H, Li YY, Wei KX, Li CH, et al. Astragalus polysaccharide inhibits radiation-induced bystander effects by regulating apoptosis in bone mesenchymal stem cells (BMSCs). Cell Cycle (2020) 19(22):3195–207. doi: 10.1080/15384101.2020.1838793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Zhang L, Luo Y, Lu Z, He J, Wang L, Zhang L, et al. Astragalus polysaccharide inhibits ionizing radiation-induced bystander effects by regulating MAPK/NF-kB signaling pathway in bone mesenchymal stem cells (BMSCs). Med Sci Monit (2018) 24:4649–58. doi: 10.12659/MSM.909153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Zhang L, Yong W, Wang L, Zhang L, Yongqi L. Astragalus polysaccharide eases g1 phase-correlative bystander effects through mediation of TGF-βR/MAPK/ROS signal pathway after carbon ion irradiation in BMSCs. Am J Chin Med (2019) 47(3):595–612. doi: 10.1142/S0192415X19500319 [DOI] [PubMed] [Google Scholar]
- 192. Zhang LY, Zhou T, Zhang YM, Xu XM, Li YY, Wei KX, et al. Guiqi baizhu decoction alleviates radiation inflammation in rats by modulating the composition of the gut microbiota. Evid Based Complement Alternat Med (2020) 2020(undefined):9017854. doi: 10.1155/2020/9017854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Li YY, Zhang LY, Zhang YM, Miao ZM, Liu ZW, Zhou GC, et al. Potential molecular mechanism of guiqi baizhu decoction in radiation-induced intestinal edema by regulating HIF-1a, AQP4 and Na/K-ATPase. Phytomedicine (2022) 107(undefined):154445. doi: 10.1016/j.phymed.2022.154445 [DOI] [PubMed] [Google Scholar]
- 194. Li L, Jin XJ, Li JW, Li CH, Zhou SY, Li JJ, et al. Systematic insight into the active constituents and mechanism of guiqi baizhu for the treatment of gastric cancer. Cancer Sci (2021) 112(5):1772–84. doi: 10.1111/cas.14851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Jabbour SK, Berman AT, Decker RH, Lin Y, Feigenberg SJ, Gettinger SN, et al. Phase 1 trial of pembrolizumab administered concurrently with chemoradiotherapy for locally advanced non-small cell lung cancer: A nonrandomized controlled trial. JAMA Oncol (2020) 6(6):848–55. doi: 10.1001/jamaoncol.2019.6731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Descourt R, Vergnenegre A, Barlesi F, Lena H, Fournel P, Falchero L, et al. Oral vinorelbine and cisplatin with concurrent radiotherapy after induction chemotherapy with cisplatin and docetaxel for patients with locally advanced non-small cell lung cancer: the GFPC 05-03 study. J Thorac Oncol (2011) 6(2):351–7. doi: 10.1097/JTO.0b013e318200f47e [DOI] [PubMed] [Google Scholar]
- 197. Xiao Z, Liang R, Wang CQ, Xu S, Li N, He Y, et al. Can aidi injection alleviate the toxicity and improve the clinical efficacy of radiotherapy in lung cancer: A meta-analysis of 16 randomized controlled trials following the PRISMA guidelines. Med (Baltimore). (2016) 95(35):e4517. doi: 10.1097/MD.0000000000004517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Zhang H, Jiang H, Hu X, Jia Z. Aidi injection combined with radiation in the treatment of non-small cell lung cancer: A meta-analysis evaluation the efficacy and side effects. J Cancer Res Ther (2015) 00:C118–21. doi: 10.4103/0973-1482.163864 [DOI] [PubMed] [Google Scholar]
- 199. Dong XR, Wang JN, Liu L, Chen X, Chen MS, Chen J, et al. Modulation of radiation-induced tumour necrosis factor-α and transforming growth factor β1 expression in the lung tissue by shengqi fuzheng injection. Mol Med Rep (2010) 3(4):621–7. doi: 10.3892/mmr_00000306 [DOI] [PubMed] [Google Scholar]
- 200. Wang S, Lian X, Sun M, Luo L, Guo L. Efficacy of compound kushen injection plus radiotherapy on nonsmall-cell lungcancer: A systematic review and meta-analysis. J Cancer Res Ther (2016) 12(4):1298–306. doi: 10.4103/0973-1482.199538 [DOI] [PubMed] [Google Scholar]
- 201. Zhou H, Pan P, Zhao Q, Liu W, Sun Y, Wang J, et al. Overcoming basal autophagy, kangai injection enhances cisplatin cytotoxicity by regulating FOXO3a-dependent autophagic cell death and apoptosis in human lung adenocarcinoma A549/DDP cells. BioMed Res Int (2022) 2022:6022981. doi: 10.1155/2022/6022981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. He H, Zhou X, Wang Q, Zhao Y. Does the couse of astragalus-containing chinese herbal prescriptions and radiotherapy benefit to non-small-cell lung cancer treatment: a meta-analysis of randomized trials. Evid Based Complement Alternat Med (2013) 2013:426207. doi: 10.1155/2013/426207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Jiang X, Hidru TH, Zhang Z, Bai Y, Kong L, Li X. Evidence of elemene injection combined radiotherapy in lung cancer treatment among patients with brain metastases: A systematic review and meta-analysis. Med (Baltimore). (2017) 96(21):e6963. doi: 10.1097/MD.0000000000006963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Yu H, Yang Y, Jiang T, Zhang X, Zhao Y, Pang G, et al. Ganoderma lucidum effective radiotherapy in tumor assisted by polysaccharide-conjugated bismuth sulfide nanoparticles through radiosensitization and dendritic cell activation. ACS Appl Mater Interfaces. (2019) 11(31):27536–47. doi: 10.1021/acsami.9b07804 [DOI] [PubMed] [Google Scholar]
- 205. Lu T, Yu J, Gao R, Wang J, Wang H, Wang X, et al. Chinese Patent medicine kanglaite injection for non-small-cell lung cancer: An overview of systematic reviews. J Ethnopharmacol (2022) 302:115814. doi: 10.1016/j.jep.2022.115814 [DOI] [PubMed] [Google Scholar]
- 206. Kong P, Yu KN, Yang M, Almahi WA, Nie L, Chen G, et al. Micheliolide enhances radiosensitivities of p53-deficient non-small-cell lung cancer via promoting HIF-1α degradation. Int J Mol Sci (2020) 21(9):3392. doi: 10.3390/ijms21093392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Woo JK, Kang JH, Shin DY, Park SH, Kang K, Nho CW, et al. Daurinol enhances the efficacy of radiotherapy in lung cancer via suppression of aurora kinase A/B expression. Mol Cancer Ther (2015) 14(7):1693–704. doi: 10.1158/1535-7163.MCT-14-0960 [DOI] [PubMed] [Google Scholar]
- 208. Du Y, Jia C, Liu Y, Li Y, Wang J, Sun K. Isorhamnetin enhances the radiosensitivity of A549 cells through interleukin-13 and the NF-κB signaling pathway. Front Pharmacol (2020) 11:610772. doi: 10.3389/fphar.2020.610772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Hsu HS, Huang PI, Chang YL, Tzao C, Chen YW, Shih HC, et al. CucurbitacinI inhibits tumorigenic ability and enhances radiochemosensitivity in nonsmall cell lung cancer-derived CD133-positive cells. Cancer. (2011) 117(13):2970–85. doi: 10.1002/cncr.25869 [DOI] [PubMed] [Google Scholar]
- 210. Phiboonchaiyanan PP, Petpiroon N, Sritularak B, Chanvorachote P. Phoyunnanin e induces apoptosis of non-small cell lung cancer cells via p53 activation and down-regulation of survivin. Anticancer Res (2018) 38(11):6281–90. doi: 10.21873/anticanres.12984 [DOI] [PubMed] [Google Scholar]
- 211. JiH L, KJ C, WD S, SY J, Kim M, BW L, et al. Enhancement of radiation sensitivity in lung cancer cells by celastrol is mediated by inhibition of Hsp90. Int J Mol Med (2011) 27(3):441–6. doi: 10.3892/ijmm.2011.601 [DOI] [PubMed] [Google Scholar]
- 212. Ye M, Zhang J, Zhang J, Miao Q, Yao L, Zhang J. Curcumin promotes apoptosis by activating the p53-miR-192-5p/215-XIAP pathway in non-small cell lung cancer. Cancer Lett (2015) 357(1):196–205. doi: 10.1016/j.canlet.2014.11.028 [DOI] [PubMed] [Google Scholar]
- 213. He GH, Xing DJ, Jin D, Lu Y, Guo L, Li YL, et al. Scutellarin improves the radiosensitivity of non-small cell lung cancer cells to iodine-125 seeds via downregulating the AKT/mTOR pathway. Thorac Cancer. (2021) 12(17):2352–9. doi: 10.1111/1759-7714.14077 [DOI] [PMC free article] [PubMed] [Google Scholar]