Abstract
Purpose
People released from incarceration are at increased risk of suicide compared to the general population. We aimed to synthesise evidence on the incidence of and sex differences in suicide, suicidal ideation, and self-harm after release from incarceration.
Methods
We searched MEDLINE, EMBASE, PsycINFO, Web of Science and PubMed between 1 January 1970 and 14 October 2021 for suicide, suicidal ideation, and self-harm after release from incarceration (PROSPERO registration: CRD42020208885). We calculated pooled crude mortality rates (CMRs) and standardised mortality ratios (SMRs) for suicide, overall and by sex, using random-effects models. We calculated a pooled incidence rate ratio (IRR) comparing rates of suicide by sex.
Results
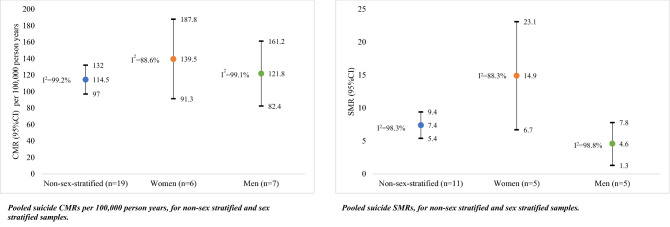
Twenty-nine studies were included. The pooled suicide CMR per 100,000 person years was 114.5 (95%CI 97.0, 132.0, I2 = 99.2%) for non-sex stratified samples, 139.5 (95% CI 91.3, 187.8, I2 = 88.6%) for women, and 121.8 (95% CI 82.4, 161.2, I2 = 99.1%) for men. The suicide SMR was 7.4 (95% CI 5.4, 9.4, I2 = 98.3%) for non-sex stratified samples, 14.9 for women (95% CI 6.7, 23.1, I2 = 88.3%), and 4.6 for men (95% CI 1.3, 7.8, I2 = 98.8%). The pooled suicide IRR comparing women to men was 1.1 (95% CI 0.9, 1.4, I2 = 82.2%). No studies reporting self-harm or suicidal ideation after incarceration reported sex differences.
Conclusion
People released from incarceration are greater than seven times more likely to die by suicide than the general population. The rate of suicide is higher after release than during incarceration, with the elevation in suicide risk (compared with the general population) three times higher for women than for men. Greater effort to prevent suicide after incarceration, particularly among women, is urgently needed.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-022-02390-z.
Keywords: Self-harm, Suicide, Suicidal ideation, Sex differences, Incarceration, Systematic review
Introduction
People in custody experience elevated rates of suicide, suicidal ideation, and self-harm compared to the general population [1–3]. Although suicide is more common among men than women in the general population, self-harm and suicidal ideation are more common among women [4, 5]. Research on suicide, suicidal ideation, and self-harm among people involved in the criminal justice system typically focuses on time during incarceration [1]. There is some evidence that rates of suicide [6], self-harm [7], and suicidal ideation [8] during incarceration are similar between sexes, in contrast with general population trends [4, 9].
People with a history of incarceration often experience major social challenges upon return to the community, including homelessness [10], substance use [11], and unemployment [12]. People with a history of incarceration also experience elevated rates of poor health and preventable death compared to the general population [13], including by suicide [14]. Women with a history of incarceration experience poorer health and social circumstances than both their male counterparts and women in the general population [15–17]. Exposure to trauma and abuse, and the consequences of poor mental health, substance use and homelessness, are all common among justice-involved women [18–20], and contribute to their markedly poor health profiles after release from incarceration.
A previous systematic review conducted in 2012 [21] that examined all-cause and external-cause deaths among people released from incarceration reported crude mortality rates (CMRs) for suicide ranging from 41 to 204 deaths per 100,000 person years among people released from incarceration [21]. This is substantially higher than the rate of 11 per 100,000 person years reported in the global general population [4]. However, this review did not calculate a pooled CMR or standardised mortality ratios (SMRs) for suicide. A meta-analysis conducted in 2013 and including five studies found that people released from incarceration were roughly seven times more likely to die by suicide than the general population (pooled risk ratio = 6.8, 95% CI 6.1, 7.5) [22]. Neither review examined differences in suicide between women and men after release from incarceration. To date, no reviews have looked at self-harm and/or suicidal ideation in women or men after release from incarceration.
As the number of people who experience incarceration continues to increase globally [23], robust and reliable estimates of suicide, self-harm, and suicidal ideation in people released from incarceration are needed to support and inform effective prevention strategies. Given the disproportionate growth in the number of women incarcerated globally [24], and their unique health and social needs [25], developing evidence-based and targeted interventions to reduce suicide, self-harm, and suicidal ideation among people released from incarceration requires an understanding of differences between women and men in this population. As such, we aimed to (1) calculate the incidence and risk relative to the general population of suicide, self-harm, and suicidal ideation among people released from incarceration, overall and stratified by sex; and (2) examine the association between sex and suicide, self-harm, and suicidal ideation.
Methods
Search strategy and selection criteria
Our review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (Table S1) [26, 27]. The review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO; CRD42020208885), and was updated on 14 December 2021.
We searched five key health and social science databases (MEDLINE, EMBASE, PsycINFO, Web of Science, and PubMed) using search terms relating to incarceration and release, suicide, self-harm, and suicidal ideation for literature published from 1 January 1970 to 8 September 2020. The search strategy (Table S2) was developed in consultation with a trained research librarian. Reference lists of included studies were checked to identify any additional relevant studies not captured by the search. As done previously [28], and as described in PRISMA guidelines [26], we updated our search by receiving email alerts from the Web of Science Core Collection for records published between 9 September 2020 and 14 October 2021.
Studies were eligible for inclusion if they were published in peer-reviewed journals, reported on suicide, self-harm, and/or suicidal ideation occurring in the community following release from incarceration (including youth justice detention, prison, and jail), and reported at least one measure of interest or sufficient data for calculation (CMR, SMR, and/or an association between sex and any outcome). We contacted authors if the total number of participants (overall and/or sex-stratified) could not be determined from the study. Studies that reported CMRs and SMRs overall and/or stratified by sex were eligible for inclusion. The definitions of suicide, self-harm, and suicidal ideation used in this review are presented in Table S3.
Studies published in languages other than English were excluded. We included studies from all geographic locations. Previous literature reviews were excluded; however, the reference lists of these reviews were checked for additional relevant studies. Consistent with previous literature [21], studies reporting on selected samples (e.g., people who use drugs) were excluded.
After the removal of duplicates, titles and abstracts of potentially eligible studies were screened by EJ with MW also screening a random 10% sample. There was moderate inter-rater agreement between the two reviewers (kappa value 0.79) [29]. Any uncertainty related to study inclusion was resolved through discussion between the authors. Full-text articles were independently screened once by EJ and then again by MW, CK, or SoK. Any conflicts were resolved through discussion. We included studies that used the same study data where articles reported different findings of interest. In the case that multiple studies reported the same findings, both studies were included in the review, but only the study with the longest follow-up period was included in meta-analysis.
Data analysis
Data were independently extracted by EJ (a summary of the information extracted is provided in Table S4). If not directly reported, we calculated CMRs and SMRs (and 95% CI) for suicide in a manner consistent with previous research [21]. Using standard formulae [30], for each study that reported a CMR for both women and men, we calculated incidence rate ratios (IRRs, and 95% CI) for suicide using men as the reference group.
Study quality was assessed using the Methodological Standard for Epidemiological Research (MASTER) scale [31]. The MASTER scale ranks studies based on the number of safeguards against bias present in the study, with a higher number of safeguards indicating a lower probability of bias (score range 0, 40) [31]. Risk of bias of each study was assessed by EJ and any uncertainty was resolved through discussion and consensus with CK (scores for each study are presented in Table 1).
Table 1.
Characteristics of included studies
| First author, year | City/state, country | Study type | Years of observation | Median follow up (years) | Outcome | Sex | Detention type | Age at baseline (years) | Participants n (%) | Reference population for SMR | QAS | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Men | Women | |||||||||||
| Barnert, 2019 [66] | US (national) | R | 1994–2008 | NR | Suicidal ideation | Women & men | Youth detention | Range: 7–24 | 1727 | 1344 (77.8) | 383 (22.2) | NA | 18 |
| Binswanger, 2007 [51] | Washington, US | R | 1999–2003 | NR | Suicide | Women & men | Prison | Mean: 33.4 ± 9.8 (Range: 18–84) | 30,237 | 26,270 (87.0) | 3697 (13.0) | Washington State residents of the same age, sex, and race | 24 |
| Binswanger, 2013 [52] | Washington, US | R | 1999–2009 | NR | Suicide | Women & men | Prison | Range: 18–84 | 76,208 | 63,979 (84.0) | 12,229 (16.0) | Washington State residents of the same age, sex, and race | 25 |
| Bird, 2003 [39]a | Scotland | R | 1996–1999 | NR | Suicide | Men only | Prison | Range: 15–35 | 19,486 | 19,486 (100) | NA | 15–35-year-old men in Scotland | 22 |
| Borschmann, 2017a [64] | Queensland, Australia | P | 2007–2013 | 2.6 | Self-harm | Women & men | Prison | Range: 18–40 + | 1307 | 1030 (78.8) | 277 (21.2) | NA | 28 |
| Borschmann, 2017b [65] | Queensland, Australia | P | 2007–2014 | 3.9 | Self-harm | Women & men | Prison | Range: 18–40 + | 1309 | 976 (74.6) | 260 (19.9) | NA | 28 |
| Brinkley-Rubinstein, 2019 [7] | North Carolina, US | R | 2000–2015 | NR | Suicide | Women & men | Prison | Median: 32 (IQR: 26–42) | 229,274 | 197,656 (86.2) | 31,618 (13.8) | NA | 24 |
| Bukten, 2017 [41]b | Norway (national) | P | 2000–2014 | NR | Suicide | Women & men | Prison | NR | 92,663 | (Range: 90.0–92.0) | (Range: 8.0–10.0) | NA | 23 |
| Bukten, 2021 [61] | Norway (national) | R | 2000–2016 | NR | Suicide | Women & men | Prison | Median: 31 (IQR: 23–41) | 96,735c | 86,761 (89.7) | 9957 (10.3) | NA | 26 |
| Chang, 2015 [50] | Sweden (national) | R | 2000–2009 | 5.1 | Suicide | Women & men | Prison | NR | 47,326 | 43,840 (92.6) | 3486 (8.0) | NA | 28 |
| Coffey, 2003 [53] | Victoria, Australia | R | 1988–1999 | 3.3 (men) 1.4 (women) | Suicide | Women & men | Youth detention | NR | 2849 | 2621 (92.0) | 228 (8.0) | Calendar year, sex, age stratified Victoria residents | 22 |
| Coffey, 2004 [54] | Victoria, Australia | R | 1988–2003 | 6.3 (men) 4.6 (women) | Suicide | Women & men | Youth detention | NR | 2849 | 2625 (92.0) | 228 (8.0) | NA | 23 |
| Dirkzwager, 2012 [55] | Netherlands | R | 1977–2003 | NR | Suicide | Women & men | Prison | Range: 12–40 + | 597 | 578 (96.8) | 19 (3.2) | Age and gender adjusted 1977 Dutch population | 22 |
| Farrell, 2008 [62] | England and Wales (national) | R | 1998–2003 | NR | Suicide | Women & men | Prison | 15 + | 48,771 | 36,513 (74.9) | 12,258 (25.1) | NA | 19 |
| Graham, 2003 [56] | Victoria, Australia | R | 1990–2000 | NR | Suicide | Women & men | Prison | NR | 25,469 | 22,978 (90.2) | 2490 (9.8) | Age, sex stratified Victorian residents | 18 |
| Haglund, 2014 [49] | Sweden (national) | P | 2005–2009 | 1.2 | Suicide | Women & men | Prison | Mean: 37.8 (SD: 12.1, range: 18–84) | 38,995 | 36,146 (92.7) | 2849 (7.3) | Gender and age matched Swedish people from general population (without incarceration history) | 26 |
| Harding-Pink, 1990 [63]a | Geneva, Switzerland | R | 1982–1986 | NR | Suicide | Women & men | Prison | NR | NR | NR | NR | NA | 16 |
| Jones, 2017 [58] | North Carolina, US | R | 2008–2012 | NR | Suicide | Women & men | Prison | Range: 20–60 + | 41,495 | 37,053 (89.3) | 4442 (10.7) | NA | 19 |
| Kariminia, 2007a, b [14, 42] | New South Wales, Australia | R | 1988–2003 | 7.7 | Suicide | Women & men | Prison | NR | 85,203 | 76,383 (89.6) | 8820 (10.4) | Age, sex stratified New South Wales population | 22 |
| Kouyoumdjian, 2016 [43] | Ontario, Canada | R | 2000–2012 | NR | Suicide | Women & men | Prison | NR | 48,166 | 43,419 (90.1) | 4747 (9.9) | General Canadian population | 24 |
| Lim, 2012 [44] | New York City, US | R | 2001–2005 | NR | Suicide | Women & men | Jail | Range: 16–89 | 155,272 | 137,161 (88.3) | 18,111 (12.7) | Age matched New York City residents | 21 |
| Pratt, 2006 [48] | England and Wales | R | 2000–2002 | NR | Suicide | NR | Prison | Range: 18–50 + | 244,988 | NR | NR | Age, sex stratified “general populations” | 21 |
| Rosen, 2008 [59] | North Carolina, US | R | 1980–2005 | 10.3 | Suicide | Men only | Prison | Median: 32 (IQR:25–40, range: 20–69) | 168,001 | 168,001 (100.0) | NA | Mid-years from 2008 to 2012 North Carolina population in residents matched on County, sex, race, and age | 22 |
| Rosen, 2020 [60] | North Carolina, US | R | 2008–2016 | NR | Suicide | Women & men | Prison | Range: 18–88 | 111,479 | 96,367 (86.4) | 15,112 (13.6) | NA | 20 |
| Sailas, 2006 [57] | Finland (national) | R | 1984–2002 | 11.7 | Suicide | Women & men | Youth detention | Range: 15–21 | 3832 | 3743 (97.7) | 89 (2.3) | NA | 20 |
| Spittal, 2014 [47] | Queensland, Australia | R | 1994–2007 | 7.5 | Suicide | Women & men | Prison | Range: 17–40 + | 41,970 | 36,994 (88.1) | 4976 (12.9) | Age and sex matched general population | 22 |
| Stewart, 2004 [45] | Western Australia, Australia | R | 1994–1999 | 3.4 | Suicide | Women & men | Prison | Mean: 31, median: 29, mode: 21 (range: 16–82) | 9381 | 8199 (87.4) | 1182 (13.6) | Age, sex, race matched Western Australian population | 25 |
| van Dooren, 2013 [46] | Queensland, Australia | R | 1994–2007 | NR | Suicide | Women & men | Prison | NR | 42,015 | 37,039 (88.2) | 4976 (11.8) | Age and sex matched Queensland general population | 22 |
NA not applicable, NR not reported, P prospective, R retrospective, US United States, QAS Quality Assessment Score
aIncluded in the review but excluded from primary meta-analyses because there was either less than 6 months follow up time and/or fewer than 20 suicides
bIncluded in the review but excluded from primary meta-analyses because another study from the same cohort reported findings with a longer follow-up time (i.e., Bukten 2021)
cRefers to gender, and not sex. Gender was unknown for 17 participants
We calculated pooled estimates of CMRs and SMRs for death by suicide, overall and stratified by sex. Using the IRRs for suicide, with men as the reference group, we calculated a pooled estimate of the IRR for suicide according to sex. Estimates were pooled using the DerSimonian Laird method [32]. A random-effects method was used because we did not expect the assumptions of a fixed-effects model to be met (i.e., the assumption of a common effect size) [33]. Heterogeneity between studies was assessed using the I2 statistic [34].
We extracted data from studies reporting other measures of association (e.g., odds ratios or hazard ratios) between sex and suicide. Due to the small number of studies reporting other measures of association between sex and suicide, and the diversity of measures reported, it was not possible to pool other measures of associations between sex and suicide.
Given the limited number of studies, it was not possible to calculate pooled estimates for self-harm or suicidal ideation (overall or sex-stratified). The results for these outcomes are narratively described [35].
To examine the effect of study quality on the outcomes, we conducted a sensitivity analysis in which we restricted the analysis to studies scoring above the median on the MASTER scale. Due to the small number of studies that reported SMRs, we were only able to conduct this sensitivity analysis on the CMR and SMR meta-analyses that did not stratify by sex.
Where data were available, we conducted univariable meta-regression to identify factors which influenced the heterogeneity of effect measures. We did this using restricted maximum likelihood (REML) estimation with the Knapp–Hartung modification [36]. Values less than zero were rounded to zero. Consistent with previous research [37], the following factors were considered: type of incarceration facility (i.e., prison, jail, or youth detention), prospective/retrospective design, length of follow-up, geographic location of the study, single-sex samples, and whether subsequent periods of incarceration during follow-up were removed from analysis (i.e., interval censoring).
All analyses were conducted using Stata/BE Release 17 [38].
Deviations from protocol
Consistent with previous reviews [21, 37], we modified our eligibility criteria by excluding studies from the primary analysis that had fewer than 20 total deaths from suicide or less than 6 months of follow-up. To test the effect of excluding these studies, we conducted a sensitivity analysis that included studies that did not meet these criteria but were otherwise eligible to be included in the review. As the studies that did not meet these criteria only reported non-sex stratified CMRs, we were only able to conduct this sensitivity analysis for the CMR not stratified by sex.
Role of the funding source
There was no funding source for this study.
Results
Our search retrieved 3284 records, 1711 of which remained after duplicates were removed (Figure S1). During title and abstract screening, 1556 records were excluded, leaving 155 full texts to be assessed. Of these, 27 met the eligibility criteria, along with an additional two records identified through citation searching. A total of 29 records were assessed for quality and included in this review.
The characteristics of included studies and characteristics of included participants are outlined in Table 1. The number of suicide deaths, person-years, CMRs, and SMRs for each study are presented in Table 2. Of the 29 included studies, there were 26 studies on suicide from 22 cohorts [14, 39–63], two studies on self-harm from one cohort [64, 65], and one study on suicidal ideation [66]. Data from 23 studies were included in meta-analyses for suicide. Two studies were only included in sensitivity analyses for suicide because they reported less than six months follow up time and/or fewer than 20 suicides. One study was not included in meta-analyses for suicide because it reported on a cohort for which longer follow-up time was available in another included study.
Table 2.
Number of suicide deaths, time at risk following release (person-years), CMRs and SMRs for suicide deaths after release from prison, overall and stratified by sex
| First author, year | N of suicide deaths | Person-years | Suicide death CMR (95% CI) per 100,000 person years | Suicide death SMR (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Women | Men | Total | Women | Men | Total | Women | Men | Total | Women | Men | |
| Binswanger, 2007 [51] | 40 | NR | NR | 57,049 | NR | NR | 18.0 (9.0–33.0) | NR | NR | 3.4 (2.5–4.7) | NR | NR |
| Binswanger, 2013 [52] | 212 | 21 | 191 | 334,238 | NR | NR | 63.0 (55.0–72.0) | 68.0 (58.0–77.0) | 41.0 (23.0–58.0) | 3.2 (2.9–3.6) | NR | NR |
| Bird, 2003 [39] | 10 | NA | 10 | 3797 | NA | 3797 | 263.4 (100.1–426.6)a | NA | NR | NR | NA | NR |
| Brinkley-Rubinstein, 2019 [40] | 635 | NR | NR | 1,974,823 | NR | NR | 32.2 (29.7–34.7)a | NR | NR | NR | NR | NR |
| Bukten, 2017 [41] | 74 | NR | NR | NR | NR | NR | 100.0 (80.0–130.0) | NR | NR | NR | NR | NR |
| Bukten, 2021 [61] | 749 | NR | NR | 904,331 | NR | NR | 82.8 (76.9–88.8) | NR | NR | NR | NR | NR |
| Chang, 2015 [50] | 471 | 36 | 435 | 238,457 | 16,935 | 221,522 | 198.0 (180.0–215.0) | 213.0 (143.0–282.0) | 196.0 (178.0–215.0) | NR | NR | NR |
| Coffey, 2003 [53] | 23 | 1 | 22 | 11,333 | 619 | 10,714 | NR | NR | NR | 9.2 (5.8, 14.7) | NR | NR |
| Coffey, 2004 [54] | 34 | NR | NR | 19,949 | NR | NR | 170.0 (120.0–240.0) | NR | NR | NR | NR | NR |
| Dirkzwager, 2012 [55] | 12 | NR | NR | NR | NR | NR | NR | NR | NR | 6.7 (2.9–10.5) | NR | NR |
| Farrell, 2008 [62]c | 36 | NR | NR | 48,578 | NR | NR | 74.0 (50.0–98.0) | NR | NR | NR | NR | NR |
| Graham, 2003 [56] | 279 | NR | NR | 25,469 | NR | NR | 181.4 (160.1–202.7)a | NR | NR | NR | NR | NR |
| Haglund, 2014 [49] | 127 | 12 | 115 | NR | NR | NR | 204.0 (168.5–239.5)b | NR | NR | 18.4 (13.9–23.8) | NR | NR |
| Harding-Pink, 1990 [63] | 5 | NR | NR | 8200 | NR | NR | 61.0 (7.5–114.4)a | NR | NR | NR | NR | NR |
| Jones, 2017 [58] | 39 | NR | NR | 147,782 | NR | NR | 26.4 (18.1–34.7)a | NR | NR | 14.5 (10.3–19.8) | NR | NR |
| Kariminia, 2007a, b [14, 52]d | 724 | 46 | 678 | 557,352 | 56,354 | 500,998 | 129.9 (120.4–139.4)a | 135 (96.0–174.0)b | 82 (75.8, 88.2)b | 4.2 (0.2–8.2)a,d | 11.5 (4.9–18.2)a,d | 4.0 (0.1–8.0)a,d |
| Kouyoumdjian, 2016 [43] | 340 | NR | NR | 580,003 | 57,261 | 522,742 | 58.6 (52.4–64.9)a | NR | NR | 4.3 (3.9–4.8) | NR | NR |
| Lim, 2012 [44] | 35 | 5 | 30 | 379,363 | NR | NR | 9.2 (6.2–12.3)a | NR | NR | 1.0 (0.7–1.4) | 3.5 (1.2–8.3) | 0.9 (0.6–1.2) |
| Pratt et al. 2006 [48] | 382 | 34 | 348 | 244,988 | 18,942 | 226,046 | 156.0 (140.4–171.6)b | 180.0 (119.5–240.5)b | 154.0 (137.8–170.1)a | 13.5 (12.2–14.9) | 35.8 (25.4–50.2) | 8.3 (7.5–9.3) |
| Rosen et al. 2008 [59] | 746 | NA | 746 | 1,822,869 | NA | 1,822,869 | 40.9 (38.0–43.9)a | NA | 40.9 (38.0–43.9)a | NR | NA | NR |
| Rosen et al. 2020 [60] | 179 | NR | NR | 471,282 | NR | NR | 38.0 (32.4–43.6)b | NR | NR | NR | NR | NR |
| Sailas et al. 2006 [57] | 148 | NR | NR | 43,411 | NR | NR | 340.9 (286.0–395.9)a | NR | NR | NR | NR | NR |
| Spittal et al. 2014 [47] | 371 | 30 | 341 | 270,394 | 31,134 | 239,260 | 137.0 (123.1–151.0)b | 96.0 (6.6–130.4)b | 143.0 (127.8–158.2)b | 7.6 (6.8–8.4) | 14.2 (9.6–20.3) | 4.8 (4.3–5.4) |
| Stewart et al. 2004 [45] | 64 | 4 | 60 | NR | NR | NR | 203.7 (153.8–253.5) | NR | NR | 5.0 (0.7–9.3) | 16.1 (8.3–24.0) | 4.7 (0.4–8.9) |
| van Dooren et al. 2013 [46] | 84 | 11 | 73 | 38,769 | 4717 | 34,052 | 216.7 (170.3–263.0)a | 233.2 (95.4–371.0)a | 214.4 (165.2–263.6)a | NR | NR | NR |
CMR crude mortality rate, SMR standardised mortality ratio, NA not applicable, NR not reported
aPoint estimate and confidence interval calculated from available data
bConfidence interval calculated from available data
cFigures reported are those from Zlodre & Fazel (2012)
dTwo studies from one cohort were included. We used data from Kariminia 2007b to calculate CMRs overall and by sex. For SMR calculations, we used the number of expected deaths for the general population from Kariminia 2007a and the number of observed deaths in the study cohort from Kariminia 2007b to calculate SMRs excluding time in prison
The data sources and outcome definitions used in each included study are summarised in Table S5. Of the 26 studies reporting on suicide, most (n = 23) reported using the International Classification of Diseases (ICD) to define death by suicide. Of the 26 suicide studies, 11 examined confirmed deaths by suicide exclusively (e.g., ICD9: E950, E959, ICD10: X60, X84) [14, 39–47, 61], three included both suicide and unnatural deaths with undetermined intent (e.g., ICD10: X60, X84, Y10, Y34) [48–50], and 12 did not provide detailed information about suicide definitions [51–60, 62, 63].
The 26 included studies that reported on suicide were published between 1990 and 2021, and had a median follow-up of 10 years (IQR: 6, 16 years). The median MASTER scale score was 21 (range 16, 26). Sources of bias included short follow up periods, and limitations regarding sampling (e.g., only including people who were incarcerated for their first offence). Most of the 26 suicide studies reported on non-sex stratified samples (n = 24), with all samples either mostly, or exclusively, comprising men. Two of the 26 suicide studies reported on male-only cohorts, and no studies reported on female-only cohorts. All 26 suicide studies reported on cohort studies, with 24 using a retrospective and two using a prospective design. Twenty-three studies reported on adult samples released from jail or prison, and three studies (with two from one cohort) reported on people released from youth detention. All studies included in this review (n = 29) were from high-income countries, most frequently Australia (n = 10). Reported sociodemographic characteristics of study participants are presented in Table S6.
Suicide
Suicide CMRs for non-sex stratified samples were available in 19 studies. Suicide CMRs for women were reported in six studies, and for men in seven studies (including one male-only cohort). CMRs for suicide per 100,000 person years ranged from 9.2 to 340.9 for non-sex stratified samples, 68.0 to 233.2 for women, and from 40.9 to 214.4 for men. The pooled suicide CMR per 100,000 person years was 114.5 (95%CI 97.0, 132.0, I2 = 99.2%) for non-sex stratified samples, 139.5 (95% CI 91.3, 187.8, I2 = 88.6%) for women, and 121.8 (95%CI 82.4, 161.2, I2 = 99.1%) for men (Fig. 1). Forest plots for each estimate are presented in Figures S2–4. For all three pooled estimates, between-study heterogeneity was high (i.e., I2 > 75.0%), and Cochran’s Q tests were significant (i.e., p < 0.001).
Fig. 1.
Pooled suicide CMRs per 100,000 person years, and pooled suicide SMRs, for non-sex stratified samples and stratified by sex. n = number of studies. This figure presents two stock plots. The first stock plot presents pooled suicide CMRs per 100,000 person years, for non-sex stratified samples, and stratified by sex. The pooled CMR for non-sex stratified samples was 114.5 per 100,000 person years (95% CI 97, 132, I2 = 99.2%). The pooled CMR for females was 139.5 per 100,000 person years (95% CI 91.3, 187.8, I2 = 88.6%). The pooled CMR for males was 121.8 per 100,000 person years (95% CI 82.4, 161.2, I2 = 99.1%). The suicide SMR was 7.4 (95% CI 5.4, 9.4, I2 = 98.3%) for non-sex stratified samples, 14.9 for women (95% CI 6.7, 23.1, I2 = 88.3%), and 4.6 for men (95% CI 1.3, 7.8, I2 = 98.8%)
We used univariable meta-regression to identify possible sources of heterogeneity in the pooled suicide CMR for non-sex stratified samples (Table 3). The pooled suicide CMR was higher for studies examining people released from youth detention compared to prison or jail (p = 0.03; I2 = 99.0%). Pooled suicide CMRs also varied significantly by country (p < 0.001; I2 = 96.7%; Table 3). We were not able to perform meta-regression for studies reporting female-only or male-only findings, due to the small number of studies that reported suicide CMRs by sex (n = 6 and n = 7 for women and men, respectively).
Table 3.
Univariable meta-regressions of (1) the crude mortality rate (CMR) for suicide and of (2) the standarised mortality ratio (SMR) for suicide, by study factors
| Factor | Meta-regression (1) Crude mortality rate (CMR) of suicide by study factors | Meta-regression (2) Standardised mortality ratio (SMR) of suicide by study factors | ||||||
|---|---|---|---|---|---|---|---|---|
| Number of studies (n = 19) | CMR (95% CI) per 100,000 person years | p value | I2 | Number of studies (n = 11) | SMR (95% CI) | p value | I2 | |
| Type of incarceration facility | ||||||||
| Jail | 1 | 9.2 (0.0, 163.2) | 0.033 | 99.0% | 1 | 1.0 (0.0, 12.7) | 0.416 | 97.5% |
| Prison | 16 | 113.5 (74.5, 152.4) | 9 | 8.4 (4.3, 12.5) | ||||
| Youth detention | 2 | 256.5 (139.0, 374.0) | 1 | 9.2 (0.0, 22.1) | ||||
| Study design | ||||||||
| Prospective | 1 | 204.0 (19.2, 388.8) | 0.350 | 99.2% | 1 | 6.7 (3.6, 9.9) | 0.047 | 98.0% |
| Retrospective | 18 | 117.5 (73.4, 160.7) | 10 | 18.4 (7.4, 29.4) | ||||
| Interval censoring | ||||||||
| No | 7 | 140.7 (70.2, 211.1) | 0.494 | 99.2% | 4 | 11.0 (5.4, 16.7) | 0.131 | 97.3% |
| Yes | 12 | 111.4 (58.0, 164.8) | 7 | 5.9 (1.8, 10.0) | ||||
| Total length of follow-up (years)a | ||||||||
| ≤ 10 years | 9 | 123.4 (60.6, 186.1) | 0.955 | 99.2% | 6 | 10.1 (4.9, 15.3) | 0.195 | 98.1% |
| > 10 years | 10 | 121.0 (61.6, 180.5) | 5 | 5.8 (1.14, 11.9) | ||||
| Countryb | ||||||||
| Australia | 6 | 166.5 (137.8, 195.1) | < 0.001 | 96.7% | 4 | 6.6 (0.3, 12.8) | 0.337 | 95.1% |
| Canada | 1 | 58.6 (0.0, 118.6) | 1 | 4.3 (0.0, 15.8) | ||||
| Finland | 1 | 340.9 (255.4, 426.5) | – | – | ||||
| Netherlands | – | – | – | – | 1 | 6.7 (0.0, 19.3) | ||
| Norway | 1 | 82.8 (22.9, 142.8) | – | – | ||||
| Sweden | 2 | 200.6 (153.4, 247.8) | 1 | 18.4 (5.1, 31.7) | ||||
| England and Wales | 2 | 117.0 (72.1, 162.1) | 1 | 13.5 (1.9, 25.1) | ||||
| US | 6 | 34.9 (10.4, 59.3) | 3 | 5.5 (0.0, 12.5) | ||||
| Male only samplesb | ||||||||
| No | 18 | 126.6 (83.5, 169.8) | 0.344 | 99.24% | – | – | – | – |
| Yes | 1 | 40.9 (0.0, 221.6) | – | – | ||||
CMR crude mortality rate, SMR standardised mortality ratio, 95% CI 95% confidence interval
aIncluded studies for meta-analysis 1 had a median follow up length of 10 years, range 0–25 years. Included studies for meta-analysis 2 had a median follow-up length of 10.8 years, range 0–25 years
bAs no studies included in the primary analysis reported SMRs for men only, the “Male only samples” variable was not included in meta-regression 2
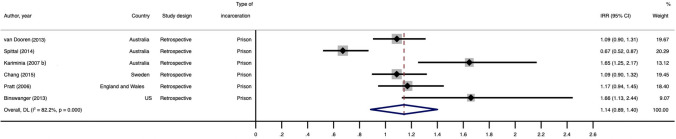
Six studies provided sufficient data to calculate suicide IRRs after release from incarceration by sex, using men as the reference group (Fig. 2). Suicide IRRs ranged from 0.7 to 1.8. The pooled suicide IRR estimate for the association between sex and suicide provided no indication of a difference in suicide risk between women and men (1.1, 95% CI 0.9, 1.4) The estimate of heterogeneity was high (I2 = 82.2%) and the Cochran’s Q test was significant (p < 0.001). Due to the small number of studies reporting suicide IRRs, we were unable to perform a meta-regression for this estimate.
Fig. 2.
Forest plot for pooled IRR for suicide after release from prison comparing women and men. IRRs greater than 1.0 indicate a greater risk of suicide for women than men. This figure presents a forest plot for the pooled IRR for suicide after release from prison, comparing women and men. Six figures were included in this meta-analysis. The authors, figures and study characteristics are as follows: van Dooren [2013] (IRR = 1.09, 95% CI 0.90, 1.31; Australia); Spittal [2014] (IRR = 0.67, 95% CI 0.52, 0.87; Australia); Kariminia [2007b] (IRR = 1.65, 95% CI 1.25, 2.17; Australia); Chang (IRR = 1.09, 95% CI 0.90, 1.32; Sweden); Pratt [2006] (IRR = 1.17, 95% CI 0.94, 1.45; England and Wales); and Binswanger [2013] (IRR = 1.66, 95% CI 1.13, 2.44; US). All included studies used a retrospective design. The pooled IRR was 1.14 (95% CI 0.89, 1.40), and the I2 estimate was 82.2%
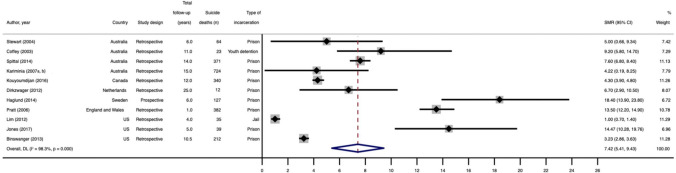
Eleven studies reported suicide SMRs for non-sex stratified samples. Five studies reported suicide SMRs for women only and men only, respectively. The reference populations for suicide SMRs were usually the general population of the geographic location of the study matched on age, sex and/or ethnicity (Table 1). Suicide SMRs ranged from 1.0 to 18.4 for non-sex stratified samples, from 3.5 to 35.8 for women, and from 0.9 to 8.3 for men. The pooled suicide SMR for non-sex stratified samples was 7.4 (95% CI 5.4, 9.4, I2 = 98.3%). The pooled suicide SMR for women (14.9, 95% CI 6.7, 23.1, I2 = 88.3%) was more than three times greater than the pooled suicide SMR for men (4.6, 95% CI 1.3, 7.8, I2 = 98.8%). Forest plots for each estimate are presented in Fig. 3, and Figures S5 and 6. The pooled estimates are presented in Fig. 1. For all three pooled estimates, between-study heterogeneity was high (I2 > 75.0%), and the Cochran’s Q tests were significant (i.e., p < 0.001).
Fig. 3.
Forest plot for pooled suicide SMR for non-sex stratified samples. This figure presents a forest plot for the pooled SMR for suicide after release from prison, not stratified by sex. Eleven studies were included in this meta-analysis. The authors, and figures are as follows: Stewart [2004] (SMR = 5.00, 95% CI 0.66, 9.34; Australia); Coffey [2003] (SMR = 9.20, 95% CI 5.80, 14.70; Australia); Spittal [2014] (SMR = 7.60, 95% CI 6.80, 8.40); Kariminia [2007 a, b]; (SMR = 4.22, 95% CI 0.19, 8.25; Australia); Kouyoumdijan [2016] (SMR = 4.30, 95% CI 4.20, 95% CI 3.90, 4.80; Canada); Dirkzwager [2012] (SMR = 6.70, 95% CI 2.90, 10.50; Netherlands); Haglund [2014] (SMR = 18.40, 95% CI 13.90, 23.80; Sweden); Pratt [2006] (SMR = 13.50, 95% CI 12.20, 14.90; England and Wales); Lim [2012] (SMR = 1.00, 95% CI 0.70, 1.40; US); Jones [2017] (SMR = 14.47, 95% CI 10.28, 19.76; US); Binswanger [2013] (SMR = 3.23, 95% CI 2.86, 3.63; US). The pooled SMR was 7.42 (95% CI 5.41, 9.43), and the I2 estimate was 98.3%
We used univariable meta-regression to identify possible sources of heterogeneity in the pooled suicide SMR for non-sex stratified samples (Table 3). The pooled suicide SMR was higher for studies with a retrospective compared to a prospective design (p < 0.05; I2 = 98.4%). We were not able perform meta-regressions for studies reporting female-only or male-only findings, due to the small number of studies that reported suicide SMRs by sex (n = 5 for women and n = 5 for men, respectively).
Six studies examined sex as a risk factor for suicide as part of their analyses (Table S7). No studies observed sex differences in the risk of suicide after release from incarceration.
The results of sensitivity analyses including studies that reported the measures of interest but did not meet the criteria to be included in the primary analysis (i.e., reporting fewer than 20 suicide deaths or less than six months of follow-up), were consistent with the results of the primary analysis (Tables S8–9; Figures S7, 9). The results of sensitivity analyses that restricted the analysis to studies with a score above the median on the MASTER scale were also consistent with the results of the primary analysis (Table S8, 10–11; Figures S8, 10) except that type of incarceration facility was no longer significant in the meta-regression for non-sex stratified CMRs (Table S10).
Suicidal ideation and self-harm
The one study that reported on suicidal ideation after release from incarceration used data from 1727 participants of the US National Longitudinal Study of Adolescent to Adult Health. Data on incarceration history were collected during Wave I of the study (in 1994) and self-reported data on suicidal ideation were collected during Wave IV (in 2008). This study examined sex as a risk factor for adult suicidal ideation and found no difference between women and men (adjusted odds ratio 1.2, 95% CI 0.7, 2.2; male reference group).
The two included studies on self-harm after release from incarceration were from the same cohort, comprising 277 women and 1030 men released from prisons in Queensland, Australia. This cohort was followed prospectively using linked administrative health records. The first study reported a higher incidence of self-harm-related emergency department presentations for women released from incarceration (IR = 60.5 per 1000 person-years) compared to their male counterparts (IR = 49.2 per 1000 person-years). The second study used ambulance records to determine the incidence of ambulance attendances due to self-harm in the cohort. Rates of ambulance attendance for self-harm were similar for women (IR = 25.6 per 1000 person-years, 95% CI 20.7, 31.4) and men (IR = 25.5 per 1000 person-years, 95% CI 16.8, 37.1). There was no significant sex difference in the rate of ambulance attendance for self-harm (IRR = 1.1, 95% CI 0.52, 2.2; adjusted IRR = 0.67, 95% CI 0.3, 1.4).
Discussion
We synthesised evidence on suicide, self-harm, and suicidal ideation among adults and youth after release from incarceration, and examined sex differences in these outcomes. Twenty-nine studies on suicide, two studies on self-harm, and one study on suicidal ideation met our inclusion criteria. Rates of suicide between women and men released from incarceration were similar, which contrasts with evidence from general population studies in which rates of suicide are typically higher among men than women [4]. We found that women released from incarceration have a risk of suicide that is almost 15 times greater than that of their general population counterparts. These findings have important implications for evidence-based suicide prevention efforts and transitional support for people released from incarceration, including services for both women and men that address their specific needs. Although evidence on self-harm and suicidal ideation among people released from incarceration is limited, the available findings indicate that high rates of these outcomes exist among this group. There is an urgent need for more high-quality research in these outcomes among people released from incarceration.
Although a high level of heterogeneity in a meta-analysis of observational studies is not unexpected [67], the amount of unexplained variance between studies in our findings means that they should be interpreted with some caution. The variance in our review may be due to a range of measured and unmeasured factors, such as underlying suicide risk across countries, the age of release from incarceration, access to various suicide methods across settings (e.g., firearm availability) and methodological factors (e.g., prospective or retrospective designs). Additionally, heterogeneity has been recognised as an issue in this area in a previous review of data linkage studies on mortality after release from incarceration [68]. This review recommended that to reduce avoidable heterogeneity, data linkage studies should ascertain deaths from a national death registry (rather than using state-based or coronial records) and exclude or adjust for subsequent periods of imprisonment [68]. Despite these recommendations having been made almost a decade ago, our study has found that these are ongoing methodological issues in this literature that potentially reduce study quality. Future research using linked data to examine suicide deaths after release from incarceration should consider such recommendations, to increase study quality, the utility of findings, and potential for evidence synthesis.
Our finding that people released from incarceration are more than seven times more likely than people in the general population to die by suicide is similar to findings from a previous meta-analysis on suicide after release from incarceration (RR = 6.8) [22]. Established predictors of suicide in the general population include, but are not limited to, unemployment [69], mental illness [70], homelessness [71], low socioeconomic status [72], and acute psychosocial stress [73]. These factors are common among people with a history of incarceration, and may be particularly pronounced in the weeks and months following release [13, 74, 75]. Further, a lack of continuity of care, including gaining or regaining access to mental health services in the community, is a common experience for people released from incarceration [76–78], and may contribute to their elevated suicide risk. A study from England and Wales found that increasing age over 25 years, release from a local prison, a history of alcohol misuse or self-harm, a psychiatric diagnosis, and requiring Community Mental Health Services (CMHS) follow-up after release from prison were all risk factors for suicide among people released from prison, while non-white ethnicity and a history of previous imprisonment were protective factors [79]. Similarly, a Swedish study found that a previous diagnosis of substance use disorder, previous suicide attempt and being born in Sweden (compared to being born abroad) were risk factors for suicide after release from incarceration [49]. Incarceration-level risk factors for suicide explored in previous research includes prison security level, with people released from high-security prisons experiencing an elevated risk of suicide compared to those released from low-security prisons [80]. Previous research on suicide risk during incarceration indicates that an interaction of social and incarceration-level factors (e.g., isolation) contribute to the risk of suicide during incarceration, rather than incarceration-level factors alone [1].
We found that suicide rates were similar between women and men released from incarceration. This is in contrast with the general population, where men have higher suicide rates than women [5]. Taken together, our findings may indicate that women released from incarceration are particularly vulnerable to suicide, because their rates of suicide are so high that they reach the same level as men released from incarceration. Consistent with this, we found that women released from incarceration are almost 15 times more likely than women in the general population to die by suicide. We found that, although both women and men released from incarceration are at increased risk of suicide relative to the same-sex general population, this elevation in risk is more than three times greater for women than for men (i.e., SMR of 14.9 and 4.6 for women and men, respectively).
Understanding the markedly elevated suicide risk among women released from incarceration compared to the general population requires examination of the potentially gender-specific risk factors for suicide to which women released from incarceration are exposed. Compared to both women in the general population and men released from incarceration, women released from incarceration experience substantially higher rates of homelessness [81, 82], substance use [19, 81], and mental illness [15, 83], which are established predictors of suicide [70, 71, 84]. Women released from incarceration may experience additional ‘gendered’ risk factors for suicide such as a history of childhood sexual abuse, trauma, and exposure to intimate partner violence [18]. These risk factors are more common among justice-involved women compared to both women in the general population [85–87] and justice-involved men [82, 88–90], and are also key drivers of female incarceration [88, 91]. These are also established risk factors for suicide [92–95]. Removal of one’s children is another risk factor for suicide that is more common among women with a history of incarceration compared to women in the general population [96–98]. There is evidence from the general population that exposure to more than one the aforementioned suicide risk factors compounds risk [99, 100]. Given that women released from incarceration typically experience a range of suicide risk factors [101, 102], the compounded and interacting effects of these exposures might explain, in part, their high suicide rates compared to women in the general population, and their similar rates to men released from incarceration. Targeted research, involving large and representative cohorts of women released from incarceration, are urgently required to explicate these pathways and inform prevention efforts tailored to women.
Our finding that suicide rates between women and men released from incarceration are similar does not necessarily mean that the same suicide prevention efforts will be effective for women and men in this population. The unique challenges women experience after release from incarceration [25, 101] must be considered as part of policy and planning. Existing transitional services are typically based on men’s needs and then applied to women [101] and, given the elevated risk of suicide among men and women released from incarceration, are evidently failing to adequately address both women’s and men’s suicide risk. A recent review of suicide prevention interventions among justice-involved people found limited evidence on interventions to address suicide risk, particularly for justice-involved women [103]. Another systematic review examining suicide prevention interventions among incarcerated people did not examine sex or gender differences at all [104]. More research is needed to inform gender-sensitive suicide prevention interventions to address both women’s and men’s unique needs, particularly among people in contact with the criminal justice system. Addressing the risk factors for why women enter incarceration, which overlap with risk factors for women’s suicide after release from incarceration (e.g., intimate partner violence, exposure to trauma, and removal of children) may be an effective way of reducing both women’s incarceration and suicide risk post-release.
Research on non-fatal suicidal outcomes after release from incarceration remains a critical gap in the literature. Our review identified just two studies on self-harm [64, 65] and one study on suicidal ideation [66] in people released from incarceration. The available findings indicate that people released from incarceration experience high rates of self-harm, with no difference by sex [64, 65]. This contrasts with the higher rates of self-harm and suicidal ideation among women in the general population compared to men. Although self-harm and suicidal ideation have been relatively well examined among incarcerated populations [3, 105], our study highlights the dearth of studies examining self-harm and suicidal ideation after incarceration. Further, although self-harm is often monitored in police custody or during incarceration [106], there does not appear to be monitoring of self-harm after release from incarceration, by health or justice agencies. This is despite evidence that the rates of these outcomes are an order of magnitude higher after incarceration than in custody [42]. Robust data on the incidence of self-harm and suicidal ideation after release from incarceration, including sex differences, are necessary to inform upstream transitional supports (e.g., addressing housing, supporting prosocial relationships, and early contact with mental health services), so that service providers can intervene as quickly as possible among both women and men at risk of suicide.
Our review is the most comprehensive to date to examine suicide, self-harm, and suicidal ideation after release from incarceration. We followed best-practice reporting guidelines [26] and excluded studies with small numbers of suicide deaths and short follow-up times; a conservative approach consistent with previous work [21]. The heterogeneity of estimates examined in our meta-analysis was high, and this was not accounted for by the factors examined in meta-regression. Due to the uneven distribution of covariates among studies, our meta-regression may lack sufficient statistical power to identify other sources of heterogeneity. All included studies reported on cohort studies, which is likely the strongest study design to examine the effect measures of interest in this population. However, there is considerable scope for methodological heterogeneity in cohort studies [68]. Our review was limited to studies published in peer-reviewed journals. However, there is some evidence that the inclusion of grey literature has a meaningful impact on meta-analyses in only a minority of reviews [107]. It is possible that including only English-language studies may have introduced some bias to our review, although there is evidence that excluding non-English studies does not have a meaningful impact on systematic review findings [108, 109]. All included studies were from high-income countries, which arguably precludes generalizing our findings to low- and middle-income countries (LMICs). High-quality evidence on suicide among people released from incarceration in LMICs is urgently needed.
Given the structure of the criminal justice system in most jurisdictions (i.e., incarcerating people by sex and not gender) and the scope of the available evidence, our review focused on sex differences and did not examine gender differences. There is some evidence that incarcerated transgender people have higher rates of suicide and self-harm compared to the general incarcerated population [110]. Future primary data collection studies on suicide, self-harm, and/or suicidal ideation in these settings should consider the experiences of transgender and gender diverse people.
People released from incarceration are more than seven times more likely than the general population to die by suicide. Women released from incarceration experience a particularly elevated risk of suicide compared to women in the general population. However, little is known about self-harm and suicidal ideation among this population, including differences between women and men. Our findings illustrate that suicide is not a ‘male problem’ only, particularly among people released from incarceration. Population-level suicide prevention policies must consider the needs of high-risk, marginalised groups, such as people released from incarceration, including the differences that exist between women and men.
These findings have important implications for the design and delivery of evidence-based transitional services for people released from incarceration that meet the needs of both women and men. Attention to the specific needs of women to reduce suicide risk is needed as part of these services. Along with robust, primary data collection about suicidal ideation and self-harm, more research is needed about people released from incarceration in LMICs, and about people who do not identify with their sex assigned at birth, to inform inclusive and effective suicide prevention policies and practices for these people who are marginalised.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
MW is supported by a National Health and Medical Research Council (NHMRC) Postgraduate Scholarship (GNT1151103). RB is supported by an NHMRC Emerging Leader Investigator Grant (EL2; GNT2008073). MW, RB, and SAK are researchers in the NHMRC-funded Centre of Research Excellence in Driving Global Investment in Adolescent Health (GNT1171981). We would like to thank Kathryn Snow for her assistance designing the study. We would also like to thank Poh Chua from the Murdoch Children’s Research Institute library for her assistance with designing the database searches.
Author contributions
EJ, RB and SAK conceived the idea for the study. EJ, CK, RB, GS, and SAK designed the study. EJ designed and conducted the search. EJ, MW, CK and SoK screened and identified eligible studies, and EJ conducted the data extraction. EJ conducted the analysis, created the figures and wrote the first draft. All authors contributed to interpretation of data and critical revision of the article. EJ and CK verified the data reported in the study. All authors had access to the data, approved the final version of the manuscript and had final responsibility for the decision to submit for publication.
Data availability
Study data are available on request to the authors. The protocol for this review is available online via PROSPERO (CRD42020208885).
Declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article. No funding was received for conducting this study.
References
- 1.Fazel S, Ramesh T, Hawton K. Suicide in prisons: an international study of prevalence and contributory factors. Lancet Psychiatry. 2017;4(12):946–952. doi: 10.1016/S2215-0366(17)30430-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hawton K, Linsell L, Adeniji T, Sariaslan A, Fazel S (2014) Self-harm in prisons in England and Wales: an epidemiological study of prevalence, risk factors, clustering, and subsequent suicide. Elsevier Science B.V., Amsterdam., Great Britain [DOI] [PMC free article] [PubMed]
- 3.Favril L, Vander Laenen F, Vandeviver C, Audenaert K. Suicidal ideation while incarcerated: prevalence and correlates in a large sample of male prisoners in Flanders, Belgium. Int J Law Psychiatry. 2017;55:19–28. doi: 10.1016/j.ijlp.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Naghavi M (2019) Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. bmj 364 [DOI] [PMC free article] [PubMed]
- 5.Hawton K. Sex and suicide: Gender differences in suicidal behaviour. Br J Psychiatry. 2000;177(6):484–485. doi: 10.1192/bjp.177.6.484. [DOI] [PubMed] [Google Scholar]
- 6.Dye MH. The gender paradox in prison suicide rates. Women Crim Just. 2011;21(4):290–307. doi: 10.1080/08974454.2011.609400. [DOI] [Google Scholar]
- 7.Favril L, Yu R, Hawton K, Fazel S. Risk factors for self-harm in prison: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(8):682–691. doi: 10.1016/S2215-0366(20)30190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Larney S, Topp L, Indig D, Odriscoll C, Greenberg D. A cross-sectional survey of prevalence and correlates of suicidal ideation and suicide attempts among prisoners in New South Wales, Australia. BMC Public Health. 2012;12(1):1–7. doi: 10.1186/1471-2458-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Australian Institute of Health and Welfare (2018) Deaths in Australia, 2017
- 10.Kushel MB, Hahn JA, Evans JL, Bangsberg DR, Moss AR. Revolving doors: imprisonment among the homeless and marginally housed population. Am J Public Health. 2005;95(10):1747–1752. doi: 10.2105/AJPH.2005.065094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Winter R, Young J, Stoove M, Agius P, Hellard M, Kinner S. Resumption of injecting drug use following release from prison in Australia. Drug Alcohol Depend. 2016;168:104–111. doi: 10.1016/j.drugalcdep.2016.08.640. [DOI] [PubMed] [Google Scholar]
- 12.Visher CA, Debus-Sherrill SA, Yahner J. Employment after prison: a longitudinal study of former prisoners. Justice Q. 2011;28(5):698–718. doi: 10.1080/07418825.2010.535553. [DOI] [Google Scholar]
- 13.Kinner SA, Young JT. Understanding and improving the health of people who experience incarceration: an overview and synthesis. Epidemiol Rev. 2018;40(1):4–11. doi: 10.1093/epirev/mxx018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kariminia A, Butler TG, Corben SP, Levy MH, Grant L, Kaldor JM, Law MG. Extreme cause-specific mortality in a cohort of adult prisoners–1988 to 2002: a data-linkage study. Int J Epidemiol. 2007;36(2):310–316. doi: 10.1093/ije/dyl225. [DOI] [PubMed] [Google Scholar]
- 15.Stanton AE, Kako P, Sawin KJ. Mental health issues of women after release from jail and prison: a systematic review. Issues Ment Health Nurs. 2016;37(5):299–331. doi: 10.3109/01612840.2016.1154629. [DOI] [PubMed] [Google Scholar]
- 16.Freudenberg N, Daniels J, Crum M, Perkins T, Richie BE. Coming home from jail: the social and health consequences of community reentry for women, male adolescents, and their families and communities. Am J Public Health. 2008;9:191. doi: 10.2105/AJPH.98.Supplement_1.S191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, Altice FL. Gender disparities in HIV treatment outcomes following release from jail: results from a multicenter study. Am J Public Health. 2014;104(3):434–441. doi: 10.2105/AJPH.2013.301553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simpson SS, Yahner JL, Dugan L. Understanding women’s pathways to jail: analysing the lives of incarcerated women. Australian and New Zealand J Criminol. 2008;1:84. doi: 10.1375/acri.41.1.84. [DOI] [Google Scholar]
- 19.Tripodi SJ, Pettus-Davis C. Histories of childhood victimization and subsequent mental health problems, substance use, and sexual victimization for a sample of incarcerated women in the US. Int J Law Psychiatry. 2013;36(1):30–40. doi: 10.1016/j.ijlp.2012.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spjeldnes S, Jung H, Yamatani H. Gender differences in jail populations: factors to consider in reentry strategies. J Offender Rehabil. 2014;53(2):75–94. doi: 10.1080/10509674.2013.868387. [DOI] [Google Scholar]
- 21.Zlodre J, Fazel S. All-cause and external mortality in released prisoners: systematic review and meta-analysis. Am J Public Health. 2012;102(12):e67–e75. doi: 10.2105/AJPH.2012.300764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones D, Maynard A. Suicide in recently released prisoners: a systematic review. Ment Health Pract. 2013;17(3):20–27. doi: 10.7748/mhp2013.11.17.3.20.e846. [DOI] [Google Scholar]
- 23.World Prison Brief . World prison population list. London: Institute for Crime and Justice Policy Research; 2018. [Google Scholar]
- 24.Walmsley R. World female imprisonment list, fourth edition: women and girls in penal institutions, including pre-trial detainees/remand prisoners. London: Institute for Criminal Policy Research; 2017. [Google Scholar]
- 25.Sheehan R. Women exiting prison: supporting successful reintegration in a changing penal climate. Br J Commun Justice. 2014;12(2):57–66. [Google Scholar]
- 26.Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, Koffel JB, Blunt H, Brigham T, Chang S, Clark J, Conway A, Couban R, de Kock S, Farrah K, Fehrmann P, Foster M, Fowler SA, Glanville J, Harris E, Hoffecker L, Isojarvi J, Kaunelis D, Ket H, Levay P, Lyon J, McGowan J, Murad MH, Nicholson J, Pannabecker V, Paynter R, Pinotti R, Ross-White A, Sampson M, Shields T, Stevens A, Sutton A, Weinfurter E, Wright K, Young S, Group P-S PRISMA-S: an extension to the PRISMA Statement for reporting literature searches in systematic reviews. Systematic Rev. 2021;10(1):39. doi: 10.1186/s13643-020-01542-z. [DOI] [Google Scholar]
- 27.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE (2021) PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. bmj 372 [DOI] [PMC free article] [PubMed]
- 28.Spurling GK, Del Mar CB, Dooley L, Foxlee R, Farley R (2017) Delayed antibiotic prescriptions for respiratory infections. Cochrane Database of Systematic Reviews (9) [DOI] [PMC free article] [PubMed]
- 29.McHugh ML. Interrater reliability: the kappa statistic. Biochemia medica. 2012;22(3):276–282. doi: 10.11613/BM.2012.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 31.Stone JC, Glass K, Clark J, Munn Z, Tugwell P, Doi SA. A unified framework for bias assessment in clinical research. Int J Evid Based Health. 2019;17(2):106–120. doi: 10.1097/XEB.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 32.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 33.Riley RD, Higgins JP, Deeks JJ (2011) Interpretation of random effects meta-analyses. Bmj 342 [DOI] [PubMed]
- 34.Cochrane Training (2019) Cochrane Handbook for Systematic Reviews of Interventions. Cochrane. https://training.cochrane.org/handbook/current. Accessed 8 Sep 2020
- 35.Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S (2006) Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version 1:b92
- 36.Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22(17):2693–2710. doi: 10.1002/sim.1482. [DOI] [PubMed] [Google Scholar]
- 37.Willoughby M, Young JT, Spittal MJ, Borschmann R, Janca E, Kinner PSA. Violence-related deaths among people released from incarceration: systematic review and meta-analysis of cohort studies. EClinicalMedicine. 2021;41:101162. doi: 10.1016/j.eclinm.2021.101162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Corporation S. Stata 17. Texas, US: Stata Corporation; 2021. [Google Scholar]
- 39.Bird SH, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996–99. Addiction. 2003;98(2):185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- 40.Brinkley-Rubinstein L, Sivaraman J, Rosen DL, Cloud DH, Junker G, Proescholdbell S, Shanahan ME, Ranapurwala SI. Association of restrictive housing during incarceration with mortality after release. JAMA Netw Open. 2019 doi: 10.1001/jamanetworkopen.2019.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bukten A, Stavseth MR, Skurtveit S, Tverdal A, Strang J, Clausen T. High risk of overdose death following release from prison: variations in mortality during a 15-year observation period. Addiction. 2017;112(8):1432–1439. doi: 10.1111/add.13803. [DOI] [PubMed] [Google Scholar]
- 42.Kariminia A, Law MG, Butler TG, Levy MH, Corben SP, Kaldor JM, Grant L (2007) Suicide risk among recently released prisoners in New South Wales, Australia. Australia [DOI] [PubMed]
- 43.Kouyoumdjian FG, Kiefer L, Wobeser W, Gonzalez A, Hwang SW. Mortality over 12 years of follow-up in people admitted to provincial custody in Ontario: a retrospective cohort study. CMAJ Open. 2016;4(2):E153–161. doi: 10.9778/cmajo.20150098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lim S, Seligson AL, Parvez FM, Luther CW, Mavinkurve MP, Binswanger IA, Kerker BD. Risks of drug-related death, suicide, and homicide during the immediate post-release period among people released from New York city jails, 2001–2005. Am J Epidemiol. 2012;175(6):519–526. doi: 10.1093/aje/kwr327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stewart LM, Henderson CJ, Hobbs MST, Ridout SC, Knuiman MW. Risk of death in prisoners after release from jail. Australian & New Zealand J Public Health. 2004;28(1):32–36. doi: 10.1111/j.1467-842X.2004.tb00629.x. [DOI] [PubMed] [Google Scholar]
- 46.van Dooren K, Kinner SA, Forsyth S. Risk of death for young ex-prisoners in the year following release from adult prison. Aust N Z J Public Health. 2013;37(4):377–382. doi: 10.1111/1753-6405.12087. [DOI] [PubMed] [Google Scholar]
- 47.Spittal MJ, Forsyth S, Pirkis J, Alati R, Kinner SA. Suicide in adults released from prison in Queensland, Australia: a cohort study. J Epidemiol Commun Health. 2014;68(10):993–998. doi: 10.1136/jech-2014-204295. [DOI] [PubMed] [Google Scholar]
- 48.Pratt D, Piper M, Appleby L, Webb R, Shaw J. Suicide in recently released prisoners: a population-based cohort study. Lancet. 2006;368(9530):119–123. doi: 10.1016/S0140-6736(06)69002-8. [DOI] [PubMed] [Google Scholar]
- 49.Haglund A, Tidemalm D, Jokinen J, Långström N, Liechtenstein P, Fazel S, Runeson B. Suicide after release from prison-a population-based cohort study from Sweden. J Clin Psychiatry. 2014;75(10):1047. doi: 10.4088/JCP.13m08967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chang Z, Lichtenstein P, Larsson H, Fazel S. Substance use disorders, psychiatric disorders, and mortality after release from prison: a nationwide longitudinal cohort study. Lancet Psychiatry. 2015;2(5):422–430. doi: 10.1016/S2215-0366(15)00088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison—a high risk of death for former inmates. N Engl J Med. 2007;356(2):157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Binswanger IA, Blatchford PJ, Mueller SR, Stern MF. Mortality after prison release: opioid overdose and other causes of death, risk factors, and time trends from 1999 to 2009. Ann Intern Med. 2013;159(9):592–600. doi: 10.7326/0003-4819-159-9-201311050-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coffey C, Veit F, Wolfe R, Cini E, Patton GC. Mortality in young offenders: retrospective cohort study. BMJ. 2003;326(7398):1064–1066. doi: 10.1136/bmj.326.7398.1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coffey C, Wolfe R, Lovett AW, Moran P, Cini E, Patton GC. Predicting death in young offenders: a retrospective cohort study. Med J Aust. 2004;181(9):473–477. doi: 10.5694/j.1326-5377.2004.tb06402.x. [DOI] [PubMed] [Google Scholar]
- 55.Dirkzwager A, Nieuwbeerta P, Blokland A. Effects of first-time imprisonment on postprison mortality: a 25-year follow-up study with a matched control group. J Res Crime Delinq. 2012;49(3):383–419. doi: 10.1177/0022427811415534. [DOI] [Google Scholar]
- 56.Graham A. Post-prison mortality: unnatural death among people released from Victorian prisons between January 1990 and December 1999. Aust N Z J Criminol. 2003;36(1):94–108. doi: 10.1375/acri.36.1.94. [DOI] [Google Scholar]
- 57.Sailas ES, Feodoroff B, Lindberg NC, Virkkunen ME, Sund R, Wahlbeck K. The mortality of young offenders sentenced to prison and its association with psychiatric disorders: a register study. Eur J Public Health. 2006;16(2):193–197. doi: 10.1093/eurpub/cki169. [DOI] [PubMed] [Google Scholar]
- 58.Jones M, Kearney GD, Xu X, Norwood T, Proescholdbell SK. Mortality rates and cause of death among former prison inmates in North Carolina. North Carolina Med J. 2017;78(4):223–229. doi: 10.18043/ncm.78.4.223. [DOI] [PubMed] [Google Scholar]
- 59.Rosen DL, Schoenbach VJ, Wohl DA. All-cause and cause-specific mortality among men released from state prison, 1980–2005. Am J Public Health. 2008;98(12):2278–2284. doi: 10.2105/AJPH.2007.121855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosen DL, Kavee AL, Brinkley-Rubinstein L. Postrelease mortality among persons hospitalized during their incarceration. Ann Epidemiol. 2020;45:54–60. doi: 10.1016/j.annepidem.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bukten A, Stavseth MR (2021) Suicide in Prison and After Release: A 17-Year National Cohort Study [DOI] [PMC free article] [PubMed]
- 62.Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction. 2008;103(2):251–255. doi: 10.1111/j.1360-0443.2007.02081.x. [DOI] [PubMed] [Google Scholar]
- 63.Harding-Pink D. Mortality following release from prison. Med Sci Law. 1990;30(1):12–16. doi: 10.1177/002580249003000104. [DOI] [PubMed] [Google Scholar]
- 64.Borschmann R, Thomas E, Moran P, Carroll M, Heffernan E, Spittal MJ, Sutherland G, Alati R, Kinner SA. Self-harm following release from prison: a prospective data linkage study. Aust N Z J Psychiatry. 2017;51(3):250–259. doi: 10.1177/0004867416640090. [DOI] [PubMed] [Google Scholar]
- 65.Borschmann R, Young JT, Moran P, Carroll M, Heffernan E, Spittal M, Mok K, Kinner SA. Ambulance attendances resulting from self-harm after release from prison: a prospective data linkage study. Soc Psychiatry Psychiatr Epidemiol. 2017;52(10):1295–1305. doi: 10.1007/s00127-017-1383-z. [DOI] [PubMed] [Google Scholar]
- 66.Barnert ES, Abrams LS, Dudovitz R, Coker TR, Bath E, Tesema L, Nelson BB, Biely C, Chung PJ. What is the relationship between incarceration of children and adult health outcomes? Acad Pediatr. 2019;19(3):342–350. doi: 10.1016/j.acap.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Imrey PB. Limitations of meta-analyses of studies with high heterogeneity. JAMA Netw Open. 2020;3(1):e1919325–e1919325. doi: 10.1001/jamanetworkopen.2019.19325. [DOI] [PubMed] [Google Scholar]
- 68.Kinner SA, Forsyth S, Williams G. Systematic review of record linkage studies of mortality in ex-prisoners: why (good) methods matter. Addiction. 2013;108(1):38–49. doi: 10.1111/add.12010. [DOI] [PubMed] [Google Scholar]
- 69.Blakely TA, Collings SC, Atkinson J. Unemployment and suicide: evidence for a causal association? J Epidemiol Commun Health. 2003;57(8):594–600. doi: 10.1136/jech.57.8.594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mortensen PB, Agerbo E, Erikson T, Qin P, Westergaard-Nielsen N. Psychiatric illness and risk factors for suicide in Denmark. The Lancet. 2000;355(9197):9–12. doi: 10.1016/S0140-6736(99)06376-X. [DOI] [PubMed] [Google Scholar]
- 71.Votta E, Manion I. Suicide, high-risk behaviors, and coping style in homeless adolescent males' adjustment. J Adolesc Health. 2004;34(3):237–243. doi: 10.1016/S1054-139X(03)00271-4. [DOI] [PubMed] [Google Scholar]
- 72.Lorant V, Kunst AE, Huisman M, Costa G, Mackenbach J. Socio-economic inequalities in suicide: a European comparative study. Br J Psychiatry. 2005;187(1):49–54. doi: 10.1192/bjp.187.1.49. [DOI] [PubMed] [Google Scholar]
- 73.van Heeringen K. Stress-diathesis model of suicidal behavior. Neurobiol Basis Suicide. 2012;51:113. [Google Scholar]
- 74.Baldry E, McDonnell D, Maplestone P, Peeters M. Ex-prisoners, homelessness and the state in Australia. Aust N Z J Criminol. 2006;39(1):20–33. doi: 10.1375/acri.39.1.20. [DOI] [Google Scholar]
- 75.Thomas E, Spittal M, Heffernan E, Taxman F, Alati R, Kinner S. Trajectories of psychological distress after prison release: implications for mental health service need in ex-prisoners. Psychol Med. 2016;46(3):611. doi: 10.1017/S0033291715002123. [DOI] [PubMed] [Google Scholar]
- 76.Kinner SA, Wang EA. The case for improving the health of Ex-prisoners. Am J Public Health. 2014;104(8):1352–1355. doi: 10.2105/AJPH.2014.301883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Quinn C, Byng R, Shenton D, Smart C, Michie S, Stewart A, Taylor R, Maguire M, Harris T, Shaw J. The feasibility of following up prisoners, with mental health problems, after release: a pilot trial employing an innovative system, for engagement and retention in research, with a harder-to-engage population. Trials. 2018;19(1):1–11. doi: 10.1186/s13063-018-2911-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hopkin G, Evans-Lacko S, Forrester A, Shaw J, Thornicroft G. Interventions at the transition from prison to the community for prisoners with mental illness: a systematic review. Administration Policy Mental Health Mental Health Services Res. 2018;45(4):623–634. doi: 10.1007/s10488-018-0848-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pratt D, Appleby L, Piper M, Webb R, Shaw J. Suicide in recently released prisoners: a case-control study. Psychol Med. 2010;40(5):827. doi: 10.1017/S0033291709991048. [DOI] [PubMed] [Google Scholar]
- 80.Bukten A, Skjærvø I, Stavseth MR. The association of prison security level with mortality after release from prison: a retrospective national cohort study (2000–16) Lancet Public Health. 2022;7(7):e583–e592. doi: 10.1016/S2468-2667(22)00107-4. [DOI] [PubMed] [Google Scholar]
- 81.Fries L, Fedock G, Kubiak SP. Role of gender, substance use, and serious mental illness in anticipated postjail homelessness. Social Work Res. 2014;38(2):107–116. doi: 10.1093/swr/svu014. [DOI] [Google Scholar]
- 82.AIHW (2018) The health of Australia’s prisoners. Canberra
- 83.King EA, Tripodi SJ, Veeh CA. The relationship between severe mental disorders and recidivism in a sample of women released from prison. Psychiatr Q. 2018 doi: 10.1007/s11126-018-9572-9. [DOI] [PubMed] [Google Scholar]
- 84.Borges G, Walters EE, Kessler RC. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. Am J Epidemiol. 2000;151(8):781–789. doi: 10.1093/oxfordjournals.aje.a010278. [DOI] [PubMed] [Google Scholar]
- 85.Australian Institute of Health and Welfare (2019) The health of Australia’s females. AIHW, Canberra
- 86.Grella CE, Lovinger K, Warda US. Relationships among trauma exposure, familial characteristics, and PTSD: a case-control study of women in prison and in the general population. Women Crim Just. 2013;23(1):63–79. doi: 10.1080/08974454.2013.743376. [DOI] [Google Scholar]
- 87.Bloom B, Owen B, Covington S. Women offenders and the gendered effects of public policy. Rev Policy Res. 2004;21(1):31–48. doi: 10.1111/j.1541-1338.2004.00056.x. [DOI] [Google Scholar]
- 88.Moloney KP, van den Bergh BJ, Moller LF. Women in prison: the central issues of gender characteristics and trauma history. Public Health. 2009;123(6):426–430. doi: 10.1016/j.puhe.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 89.Wakefield S, Wildeman C (2013) Children of the prison boom: Mass incarceration and the future of American inequality. Oxford University Press
- 90.US Department of Justice (2008) Parents in Prison and Their Minor Children. Office of Justice Programs, Bureau of Justice Statistics
- 91.Saxena P, Messina NP, Grella CE. Who benefits from gender-responsive treatment? Accounting for abuse history on longitudinal outcomes for women in prison. Crim Justice Behav. 2014;41(4):417–432. doi: 10.1177/0093854813514405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gulliver P, Fanslow J. Exploring risk factors for suicidal ideation in a population-based sample of New Zealand women who have experienced intimate partner violence. Aust N Z J Public Health. 2013;37(6):527–533. doi: 10.1111/1753-6405.12110. [DOI] [PubMed] [Google Scholar]
- 93.Brown S, Seals J. Intimate partner problems and suicide: are we missing the violence? J Injury Violence Res. 2019;11(1):53. doi: 10.5249/jivr.v11i1.997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. J Pers Disord. 2002;16(3):201–214. doi: 10.1521/pedi.16.3.201.22542. [DOI] [PubMed] [Google Scholar]
- 95.Evans E, Hawton K, Rodham K. Suicidal phenomena and abuse in adolescents: a review of epidemiological studies. Child Abuse Negl. 2005;29(1):45–58. doi: 10.1016/j.chiabu.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 96.Stone U, Liddell M, Martinovic M. Incarcerated mothers: Issues and barriers for regaining custody of children. Prison J. 2017;97(3):296–317. doi: 10.1177/0032885517703957. [DOI] [Google Scholar]
- 97.Wall-Wieler E, Roos LL, Nickel NC, Chateau D, Brownell M. Mortality among mothers whose children were taken into care by child protection services: a discordant sibling analysis. Am J Epidemiol. 2018;187(6):1182–1188. doi: 10.1093/aje/kwy062. [DOI] [PubMed] [Google Scholar]
- 98.Dowell CM, Mejia GC, Preen DB, Segal L. Maternal incarceration, child protection, and infant mortality: a descriptive study of infant children of women prisoners in Western Australia. Health & justice. 2018;6(1):1–12. doi: 10.1186/s40352-018-0060-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Thompson MP, Kaslow NJ, Kingree JB. Risk factors for suicide attempts among African American women experiencing recent intimate partner violence. Violence Vict. 2002;17(3):283–295. doi: 10.1891/vivi.17.3.283.33658. [DOI] [PubMed] [Google Scholar]
- 100.Clapperton A, Newstead S, Bugeja L, Pirkis J. Relative risk of suicide following exposure to recent stressors, Victoria, Australia. Aust N Z J Public Health. 2019;43(3):254–260. doi: 10.1111/1753-6405.12886. [DOI] [PubMed] [Google Scholar]
- 101.Baldry E. Women in transition: from prison to. Curr Issues Crim Just. 2011;3:253. [Google Scholar]
- 102.Trotter C, Sheehan R (2017) Women’s transitions from prison: the post-release experience. Routledge
- 103.Carter A, Butler A, Willoughby M, Janca E, Kinner SA, Southalan L, Fazel S, Borschmann R. Interventions to reduce suicidal thoughts and behaviours among people in contact with the criminal justice system: A global systematic review. EClinicalMedicine. 2022;44:101266. doi: 10.1016/j.eclinm.2021.101266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Winicov N. A systematic review of behavioral health interventions for suicidal and self-harming individuals in prisons and jails. Heliyon. 2019;5(9):e02379. doi: 10.1016/j.heliyon.2019.e02379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Borschmann R, Janca E, Carter A, Willoughby M, Hughes N, Snow K, Stockings E, Hill NT, Hocking J, Love A. The health of adolescents in detention: a global scoping review. Lancet Public Health. 2020;5(2):e114–e126. doi: 10.1016/S2468-2667(19)30217-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Humber N, Hayes A, Senior J, Fahy T, Shaw J. Identifying, monitoring and managing prisoners at risk of self-harm/suicide in England and Wales. J Forensic Psychiatry Psychol. 2011;22(1):22–51. doi: 10.1080/14789949.2010.518245. [DOI] [Google Scholar]
- 107.Schmucker CM, Blümle A, Schell LK, Schwarzer G, Oeller P, Cabrera L, von Elm E, Briel M, Meerpohl JJ, Consortium O (2017) Systematic review finds that study data not published in full text articles have unclear impact on meta-analyses results in medical research. PloS One 12 (4):e0176210 [DOI] [PMC free article] [PubMed]
- 108.Nussbaumer-Streit B, Klerings I, Dobrescu A, Persad E, Stevens A, Garritty C, Kamel C, Affengruber L, King V, Gartlehner G. Excluding non-English publications from evidence-syntheses did not change conclusions: a meta-epidemiological study. J Clin Epidemiol. 2020;118:42–54. doi: 10.1016/j.jclinepi.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 109.Morrison A, Polisena J, Husereau D, Moulton K, Clark M, Fiander M, Mierzwinski-Urban M, Clifford T, Hutton B, Rabb D. The effect of English-language restriction on systematic review-based meta-analyses: a systematic review of empirical studies. Int J Technol Assess Health Care. 2012;28(2):138. doi: 10.1017/S0266462312000086. [DOI] [PubMed] [Google Scholar]
- 110.Brömdal A, Clark KA, Hughto JM, Debattista J, Phillips TM, Mullens AB, Gow J, Daken K. Whole-incarceration-setting approaches to supporting and upholding the rights and health of incarcerated transgender people. Taylor & Francis; 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Study data are available on request to the authors. The protocol for this review is available online via PROSPERO (CRD42020208885).