Abstract
A systematic review and meta-analysis of microsurgical vasoepididymostomy (MVE) for treating epididymal obstructive azoospermia (EOA) with different intussusception techniques. We conducted a comprehensive literature search using PubMed, Embase, and the Cochrane Central Register of Controlled Trials, retained literature related to obstructive azoospermia or male infertility and vasoepididymostomy, proactively reviewed other relevant literature, supplemented valuable references, and excluded studies that did not use intussusception and where valuable statistical data were difficult to obtain. Event rate and risk ratio (RR) were estimated. Patency rates were investigated. The influence of motile sperms found in the epididymal fluid, anastomotic sides and sites on patency was evaluated. 273 articles were comprised in this analysis, and 25 observational studies were eventually included, with a total patient sample of 1400. The overall mean patency rate was 69.3% (95% confidence interval [CI] 64.6–73.6%; I2 = 63.735%). We conducted a meta-analysis of the factors affecting patency after microsurgical IVE, finding that the presence of motile sperms in epididymal fluid (RR = 1.52; 95% CI 1.18–1.97%; P = 0.001), anastomosing bilaterally (RR = 1.32; 95% CI 1.15–1.50%; P < 0.0001) and distally (RR = 1.42; 95% CI 1.09–1.85%; P = 0.009) lead to higher patency rates. IVE is an effective treatment for EOA. The presence of motile sperms found in the epididymal fluid, anastomosing bilaterally and distally are significantly correlated with higher patency rates.
Subject terms: Male factor infertility, Urogenital diseases
Introduction
Microsurgical vasoepididymostomy (MVE) is an effective technique for epididymal obstructive azoospermia (EOA) to improve male fertility. Since the new century, intussusception vasoepididymostomy (IVE) has become the mainstream mode of MVE, which has a higher surgical patency rate1,2. Microsurgical longitudinal intussusception vasoepididymostomy (LIVE) has been the preferred operation for EOA treatment since 20043, and this procedure requires superior surgical skills and meticulous surgical technique4.
Evaluating the differences in surgical results with different techniques and finding out the factors affecting surgical results will provide the basis for the decision-making of surgical methods and obtain better surgical results.
This analysis aims to systematically review the evidence for IVE treatment of EOA, explore differences in outcomes among different IVE techniques, and provide a meta-analysis of their effectiveness.
Methods
Literature search
This systematic review and meta-analysis were reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and MOOSE Guidelines for Meta-analyses and Systematic Reviews of Observational studies.
Databases searched included PubMed, Embase, and the Cochrane Central Register of Controlled Trials from inception to March 20, 2022. Exhaustive electronic search was conducted by two independent authors (Wang S. and Fang Y.) using the subject terms ((“azoospermia” [All Fields]) OR (“epididymal obstructive azoospermia [All Fields]”) OR (“epididymal obstruction” [All Fields]) OR (“epididymis obstruction” [All Fields]) OR (“vasoepididymal obstruction” [All Fields]) OR (“infertility” [All Fields]) OR (“fertility” [All Fields])) AND ((“vasoepididymostomy” [All Fields]) OR (“epididymovasostomy” [All Fields])). The two independent authors evaluated the searching results. The senior author (Hong K.) reviewed these articles to ensure their relevance to our study and determined the articles included. The search strategy was initially developed for PubMed and subsequently adapted for the other databases. Event rate and risk ratio (RR) were estimated using a random‑effects model. Heterogeneity was investigated using the Q statistic and I2 values.
Inclusion and exclusion criteria and outcome measures
During the screening, we included articles evaluating the effect of vasoepididymostomy on EOA patency rate and those comparing the effect of different factors on patency. We excluded review articles, animal studies, < 10 case series, and a previous meta-analysis. We excluded articles in which IVE was not carried out in treating EOA. There are no language or publication date restrictions for this analysis.
We extracted the following data from the retrieved studies: author names and years of publication, methods of study design, surgical techniques, sample sizes, patients’ and partners’ ages, patency rates, pregnancy rates and follow-up. We also extracted intraoperative information, including the presence or absence of motile sperms in epididymal fluid, anastomotic sides and sites of epididymal.
Quality assessment
The NIH “Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group”, which can be achieved at https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools, was used for uncontrolled before-after studies. This tool is composed of 12 items that could be answered as “Yes”, “No”, “Not Reported” or “Not applicable”, and the overall quality of each study could be classified as “Good”, “Fair” or “Poor”. In this analysis, however, the 12th item should always be answered as “Not applicable”, thus the highest quality score theoretically is 11.
Statistical analyses
RevMan 5.3 (Cochrane Community) and Comprehensive Meta-Analysis V3 (CMA; Biostat) were used for the meta-analysis. SPSS 24.0 (IBM) was used for statistical analysis of quality assessment. Event rates or RR and 95% confidence interval (CI) for dichotomous variables were investigated. Due to the heterogeneity of the included studies, the Mantel–Haenszel random-effects model was used. All P values are two-tailed, and P < 0.05 was considered statistically significant.
Q statistics were used to test homogeneity between studies. Homogeneity is rejected when the Q statistic P value is < 0.10.
The effects of IVE on patency, in total and in different techniques respectively, were shown by the forest plots, which contain a pooled estimate of the effect (event rate or RR) as a dashed vertical line with a diamond at the bottom representing the 95% CI. Individual studies are represented as squares with their CIs, and the weight of each study is represented by the proportion of its corresponding square.
Results
Eligible studies
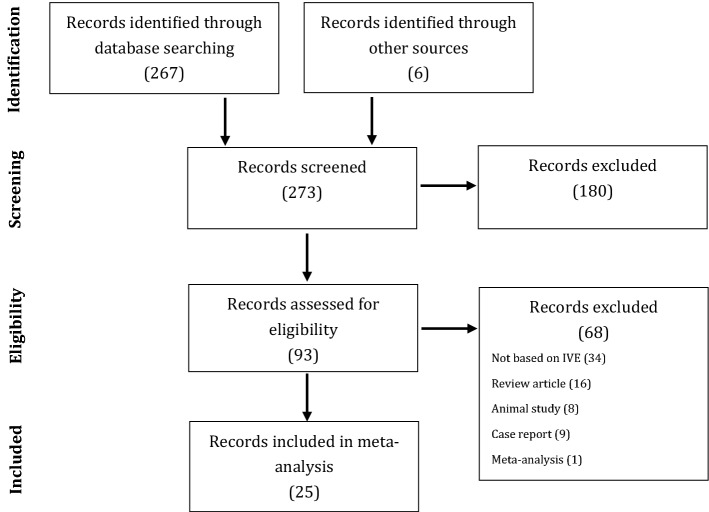
Among 273 retrieved articles, 25 met the eligibility criteria and were included in the system review2,5–28. A PRISM flow chart describing the results of study identification and selection is shown in Fig. 1.
Figure 1.
Flow chart depicting the study selection process (PRISMA flow diagram).
Among these 25 studies (9 prospective cohort studies and 16 retrospective cohort studies), 1400 patients in the meta-analysis were aggregated qualitatively and quantitatively (Table 1).
Table 1.
Study and patient characteristics among included studies.
| Study | Design | Technique | N | Age (range) | Age of partner (range) | Time for patency, months (range) | Patency (rate, %) | Pregnant rate, % | Follow-up, months (range) | Quality score* |
|---|---|---|---|---|---|---|---|---|---|---|
| Chan, P. T. et al.5 | P | 3-suture double-armed triangulation | 63 | 39.8 (22–57) | 31.8 (24–41) | 2.1 | 53 (84) | 40 | 15.2 (1–36) | 8 |
| Schiff, J. et al.2 | R | 3-suture double-armed triangulation | 19 | N/A | 30.7 | 2.8 (1–11) | 16 (84) | 46 | 70.8 | 9 |
| 2-suture double-armed longitudinal | 15 | 30.4 | 2.9 (1–6) | 12 (80) | 44 | 17.2 | ||||
| Kumar, R. et al.6 | P | 2-suture double-armed longitudinal | 23 | 30.7 (24–38) | N/A | 3.2 (1.5–7) | 11 (48) | N/A | 7.6 (1.5–30) | 5 |
| Ho, K. L. et al.7 | R | 3-suture double-armed triangulation | 6 | 36 | 30 | 4 (1–20) | 4 (67) | 32 | 15 (4–32) | 8 |
| 2-suture double-armed longitudinal | 17 | 9 (53) | ||||||||
| Zhang, G. X. et al.8 | R | 2-suture double-armed longitudinal | 42 | 37 | N/A | N/A | 30 (71.4) | 26.3 | > 6–12 | 7 |
| Kumar, R. et al.9 | P | 2-suture double-armed longitudinal | 23 | 31 (23–40) | N/A | 6.6 (3–15) | 11 (48) | N/A | 11.47 (3–26) | 7 |
| Smrkolj, T. et al.10 | P | 3-suture double-armed triangulation | 34 | 34.5 (21–49) | 30.4 (19–40) | N/A | 21 (63.6) | 38.2 | N/A | 8 |
| Peng, J. et al.11 | R | 2-suture double-armed longitudinal | 72 | 30.4 (21–57) | N/A | N/A | 46 (63.9) | N/A | 24 (11–45) | 6 |
| Peng, J. et al. 12 | P | 2-suture double-armed longitudinal | 53 | 30.9 (22–48) | N/A | 4.3 (3–9) | 38 (71.7) | 33.3 | 13.5 (4–22) | 9 |
| Zhang, H. et al.13 | R | 2-suture double-armed transverse | 16 | 33.0 (21–52) | N/A | N/A | 11 (68.8) | 37.5 | 46–63 | 8 |
| Zhao, L. et al.14 | R | 2-suture single-armed longitudinal | 17 | 30.4 | N/A | N/A | 10 (58.8) | N/A | N/A | 7 |
| Binsaleh, S. et al.15 | R | 2-suture single-armed longitudinal | 22 | 31 (23–47) | 25 (21–36) | 3 (1–24) | 13 (59) | 36 | 18 (6–30) | 7 |
| Jiang, H. T. et al.16 | P | 2-suture double-armed transverse | 33 | 31.6 (22–45) | 28.5 (20–42) | N/A | 29 (87.9) | 44.8 | 22 (9–52) | 6 |
| Peng, J. et al.17 | R | 2-suture double-armed longitudinal | 53 | 30.4 (22–48) | 27.3 (21–35) | 3.6 (3–7) | 42 (79.2) | 35.8 | 19.8 (6–43) | 9 |
| Zhao, L. et al.18 2015 | R | 2-suture single-armed longitudinal | 39 | 31.4 | 29.2 | 6.2 (1.5–12) | 24 (61.5) | 38.5 | 10.3 (2.5–12) | 7 |
| Chen, X. F. et al.19 | P | 2-suture single-armed longitudinal | 150 | 28.5 (22–38) | N/A | N/A | 108 (72) | 38.7 | 16.5 (4–28) | 8 |
| Hong, K. et al.20 | R | 2-suture single-armed longitudinal | 62 | 31 (23–45) | N/A | N/A | 41 (66.1) | 34.1 | 8.8 (2–17) | 8 |
| Peng, J. et al.21 | R | 2-suture double-armed longitudinal | 198 | 31.0 (20–51) | 28.4 (18–42) | 3.8 (2–10) | 151 (76.3) | 40.9 | 25.3 (12–48) | 9 |
| Lyu, K. L. et al.22 | R | 2-suture single-armed longitudinal | 59 | 31.1 (18–42) | N/A | N/A | 49 (83.1) | 40.7 | 15.6 (3–33) | 8 |
| Wang, S. Y. et al.23 | R | 2-suture single-armed longitudinal | 82 | 30.7 | N/A | N/A | 59 (72.0) | 32.8 | 19 (12–33) | 7 |
| Tang, S. X. et al.24 | R | 2-suture single-armed longitudinal | 69 | 25 (21–42) | N/A | N/A | 50 (72.5) | 34.0 | 12.0 (3–29) | 7 |
| Shimpi, R. K. et al.25 | P | 2-suture double-armed longitudinal | 40 | 30.2 (24–37) | N/A | N/A | 25 (62.5) | 15 | N/A | 7 |
| Tiwari, D. P. et al.26 | P | 2-suture double-armed longitudinal | 19 | 30.1 (22–38) | N/A | N/A | 6 (31.6) | 5.2 | 14 | 6 |
| Liu, N. et al.27 | R | 2-suture single-armed longitudinal | 134 | 32.1 (23–50) | 27.2 (20–43) | 4.1 | 74 (55.2) | 40.9 | 17 (3–36) | 8 |
| Li, P. et al.28 | R | 2-suture single-armed longitudinal | 40 | 30.4 | 28.9 | 3.6 | 33 (82.5) | 51.5 | 16.9 (12– 23) | 9 |
*R retrospective cohort, P prospective cohort, N/A not available.
Quality assessment and publication bias
Table 1 shows the quality score for each article measured by the “Quality Assessment Tool for Before-After (Pre-Post) Studies with No Control Group”. In Statistical analysis by SPSS, the median quality score was 8 (interquartile range 7–8).
The publication bias in this analysis was shown in funnel plots (Fig. 2). There was no publication bias in the overall patency rate (P = 0.99, Egger’s test).
Figure 2.
Publishing bias: funnel plots for patency.
Patency
The definition of patency after IVE varied among all the 25 studies. 9 studies defined patency in different sperm concentrations: > 104 sperms/ml (8) and > 106 sperms/ml (1). In other studies, intact sperm (2), motile sperm (1), or any sperm (9) seen in the ejaculates were considered patency. The definition of patency was not clear in the remaining 4 studies. Natural pregnancy observed is always considered patency.
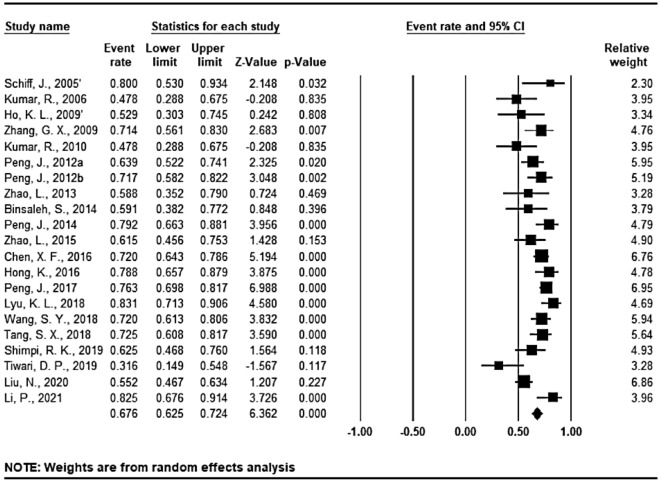
Patency was analyzed according to different surgical techniques in all the 25 studies (27 sequences) (Figs. 3, 4 and 5). The overall mean patency rate was 69.3% (95% CI 64.6–73.6%; I2 = 63.735%), 3-suture double-armed triangulation and 2-suture double-armed transverse IVE mean patency rate was 77.2% (95% CI 66.9–85.5%; I2 = 48.155%) (75.9 and 80.0% respectively). LIVE mean patency rate was 67.6% (95% CI 62.5–72.4%; I2 = 65.258%).
Figure 3.
Forest plots of overall patency rate; CI confidence interval. Annotation: 2 IVE techniques were reported by Schiff, J. et al.2 and Ho, K. L. et al.7 respectively, and were statistically analyzed separately in this analysis.
Figure 4.
Forest plots of patency rate under 3-suture double-armed triangulation and 2-suture double-armed transverse IVE technique.
Figure 5.
Forest plots of patency rate under LIVE technique.
Pregnancy
Although “pregnancy rates” were reported in 20 studies (Table 1), the definition of “pregnancy rates” and methods of computation were different, and the duration of follow-up varied widely from study to study: “Natural pregnancy & Pregnancy/All” in 9 studies, “Natural pregnancy & Pregnancy/Patency” in 7 studies, “Natural pregnancy or ART & Pregnancy/All” in 5 studies, “Natural pregnancy or ART & Pregnancy/Patency” in 2 studies, and "Pregnancy method unspecified” in 1 study. Moreover, most studies did not specify the method of determining pregnancy. So, “pregnancy rates” based on these 20 studies were not the same variable and had no statistical value indeed.
Factors affecting patency
Factors affecting patency after IVE were analyzed and presented by forest plots (Fig. 6).
Figure 6.
Forest plots of comparison of different factors affecting patency rate: the presence of motile vs. non-motile sperms found in epididymal fluid, anastomosis bilateral vs. unilateral, and anastomosing distal vs. proximal respectively.
In 10 studies involving 626 patients, those with the presence of motile sperms found in epididymal fluid showed higher patency rate (RR = 1.52; 95% CI 1.18–1.97%; P = 0.001).
13 studies involving 839 patients analyzed the patency rate according to anastomosis sides (unilateral or bilateral). Compared with the unilateral group, patients in the bilateral group exhibited higher patency rate (RR = 1.32; 95% CI 1.15–1.50%; P < 0.0001).
The effect of anastomotic sites on patency rate was analyzed in 11 studies involving 796 patients. Distal anastomosis leads to a higher patency rate than proximal one (RR = 1.42; 95% CI 1.09–1.85%; P = 0.009).
Discussion
Several systematic evaluations have preliminarily confirmed the safety and efficacy of MVE in the treatment of EOA1,29. IVE has gradually replaced other surgical techniques for EOA treatment since the beginning of this century, and remains to be one of the most technically challenging urological surgery. In this analysis, including 25 studies (9 prospective cohort studies and 16 retrospective cohort studies) involving 1400 patients, the efficacy of IVE was analyzed, and the total patency rate was 69.3%, which confirmed that this surgical technique had good efficacy in treating patients with EOA, and was proved to have a higher patency rate than previous MVE surgical techniques1.
Currently, LIVE is considered to be the preferred operation for treating EOA3.Contrary to common belief, we found that other IVE techniques (3-suture double-armed triangulation and 2-suture double-armed transverse IVE) can achieve a higher patency rate than LIVE (77.2 vs. 67.3%). We tried to explain this result as follows. The triangulation technique, which is not a mainstream technique nowadays, was reported in earlier studies. As was described in the earlier studies, in the cases where the epididymal tubule was too small to accommodate three micro sutures, the 2-suture technique, especially the longitudinal technique, should be used. Therefore, the triangulation technique showed a higher patency rate because of the bias of its patient population with a relatively wider epididymal tubule. It is similar to the 2-suture transverse technique.
Several studies have suggested that motile sperm detected in epididymal fluid, bilateral, and distal epididymal anastomosis can improve the patency rate. In this analysis, we confirmed that motile sperms found in epididymal fluid (80.8% [291/360] vs. 56.8% [151/266]), bilateral anastomosis (74.3% [746/641] vs. 53.55% [106/198]) and distal anastomosis (73.9% [465/629] vs. 48.5% [81/167]) lead to obvious higher patency rate. According to this conclusion, urologists can make more appropriate surgical decisions under certain objective conditions, to improve the patency rate and promote the rehabilitation of male fertility. Bilateral IVE should be considered in all circumstances that are possible in EOA. Moreover, IVE may lead to natural pregnancy, avoiding the risks of assisted reproductive technology (ART) to both female partners and fetuses30.
At the same time, we recognize several limitations of this analysis. First of all, we found differences or ambiguities in the definitions of “patency rate” and “pregnancy rate” in previous studies. Especially for “pregnancy rate”, the same name means different parameters indeed. Then, this analysis only included observational studies and most of the studies (16) were retrospective. In addition, several included studies were performed in same centers (Peng, J. et al.11,12,17,21; Zhao, L. et al.14,18) which may cause unpredictability bias. Increasing the sample size can further eliminate the influence of bias. Combined with the result that “different IVE techniques obtain different patency rates” found in this analysis, which is contrary to popular belief, it is feasible to design randomized controlled trial (RCT) studies of different surgical techniques on the patency rate of IVE. Finally, other factors which may affect patency rates were not systematically reviewed and analyzed limited by the number of studies.
Conclusions
Microsurgical vasoepididymostomy using intussusception technique proved to have good patency rates. Thus, IVE is effective in improving the fertility of men from EOA. The presence of motile sperms in perioperative epididymal fluid, and anastomosing bilaterally and distally are significantly correlated with higher patency rates in IVE.
Acknowledgements
Thanks to Kai Hong for his suggestions on this study.
Author contributions
S.W. designed the research. S.W. and Y.F. conducted the search. S.W. and Y.F. had full access to the study data and carried out all analysis. S.W. and Y.F. wrote the draft of this paper. S.W. and Y.F. contributed to the manuscript writing, read and approved the final manuscript.
Data availability
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Shou-yang Wang and Yang-yi Fang.
References
- 1.Yoon YE, et al. The role of vasoepididymostomy for treatment of obstructive azoospermia in the era of in vitro fertilization: A systematic review and meta-Analysis. Asian J. Andros. 2019;21:67–73. doi: 10.4103/aja.aja_59_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schiff J, Chan P, Li PS, Finkelberg S, Goldstein M. Outcome and late failures compared in 4 techniques of microsurgical vasoepididymostomy in 153 consecutive men. J. Urol. 2005;174:651–655. doi: 10.1097/01.ju.0000165573.53109.92. [DOI] [PubMed] [Google Scholar]
- 3.Chan PT. The evolution and refinement of vasoepididymostomy techniques. Asian J. Androl. 2013;15:49–55. doi: 10.1038/aja.2012.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Namekawa T, Imamoto T, Kato M, Komiya A, Ichikawa T. Vasovasostomy and vasoepididymostomy: Review of the procedures, outcomes, and predictors of patency and pregnancy over the last decade. Reprod. Med. Biol. 2018;17:343–355. doi: 10.1002/rmb2.12207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chan PT, Brandell RA, Goldstein M. Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. BJU Int. 2005;96:598–601. doi: 10.1111/j.1464-410X.2005.05691.x. [DOI] [PubMed] [Google Scholar]
- 6.Kumar R, Gautam G, Gupta NP. Early patency rates after the two-suture invagination technique of vaso-epididymal anastomosis for idiopathic obstruction. BJU Int. 2006;97:575–577. doi: 10.1111/j.1464-410X.2006.05952.x. [DOI] [PubMed] [Google Scholar]
- 7.Ho KL, Wong MH, Tam PC. Microsurgical vasoepididymostomy for obstructive azoospermia. Hong Kong Med. J. 2009;15:452–457. [PubMed] [Google Scholar]
- 8.Zhang GX, Bai WJ, Xu KX, Wang XF, Zhu JC. Clinical observation of loupe-assisted intussusception vasoepididymostomy in the treatment of obstructive azoospermia (analysis of 49 case reports) Asian J. Androl. 2009;11:193–199. doi: 10.1038/aja.2008.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kumar R, Mukherjee S, Gupta NP. Intussusception vasoepididymostomy with longitudinal suture placement for idiopathic obstructive azoospermia. J. Urol. 2010;183:1489–1492. doi: 10.1016/j.juro.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 10.Smrkolj T, Virant-Klun I, Sinkovec J, Oblak C, Zorn B. Epididymovasostomy as the first-line treatment of obstructive azoospermia in young couples with normal spermatogenesis. Reprod. Biomed. Online. 2010;20:594–601. doi: 10.1016/j.rbmo.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 11.Peng J, et al. Causes of suspected epididymal obstruction in Chinese men. Urology. 2012;80:1258–1261. doi: 10.1016/j.urology.2012.08.057. [DOI] [PubMed] [Google Scholar]
- 12.Peng J, et al. Patency rates of microsurgical vasoepididymostomy for patients with idiopathic obstructive azoospermia: A prospective analysis of factors associated with patency–single-center experience. Urology. 2012;79:119–122. doi: 10.1016/j.urology.2011.09.034. [DOI] [PubMed] [Google Scholar]
- 13.Zhang H, et al. Microsurgical transverse 2-suture intussusception vasoepididymostomy: Effectiveness and rationality. Chin. Med. J. (Engl.) 2013;126:4670–4673. [PubMed] [Google Scholar]
- 14.Zhao L, et al. A modified single-armed technique for microsurgical vasoepididymostomy. Asian J. Androl. 2013;15:79–82. doi: 10.1038/aja.2012.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Binsaleh S. Two-suture single-armed longitudinal intussusception vasoepididymostomy for obstructive azoospermia: report of patients characteristics and outcome. Int. Urol. Nephrol. 2014;46:2271–2277. doi: 10.1007/s11255-014-0835-6. [DOI] [PubMed] [Google Scholar]
- 16.Jiang HT, et al. Multiple advanced surgical techniques to treat acquired seminal duct obstruction. Asian J. Androl. 2014;16:912–916. doi: 10.4103/1008-682x.139256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Peng J, et al. Microsurgical vasoepididymostomy is an effective treatment for azoospermic patients with epididymal obstruction and prior failure to achieve pregnancy by sperm retrieval with intracytoplasmic sperm injection. Hum. Reprod. 2014;29:1–7. doi: 10.1093/humrep/det385. [DOI] [PubMed] [Google Scholar]
- 18.Zhao L, et al. Retrospective analysis of early outcomes after a single-armed suture technique for microsurgical intussusception vasoepididymostomy. Andrology. 2015;3:1150–1153. doi: 10.1111/andr.12111. [DOI] [PubMed] [Google Scholar]
- 19.Chen XF, et al. Microsurgical vasoepididymostomy for patients with infectious obstructive azoospermia: Cause, outcome, and associated factors. Asian J. Androl. 2016;18:759–762. doi: 10.4103/1008-682x.175095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hong K, et al. Multiple factors affecting surgical outcomes and patency rates in use of single-armed two-suture microsurgical vasoepididymostomy: A single surgeon's experience with 81 patients. Asian J. Androl. 2016;18:129–133. doi: 10.4103/1008-682x.159718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peng J, Zhang Z, Yuan Y, Cui W, Song W. Pregnancy and live birth rates after microsurgical vasoepididymostomy for azoospermic patients with epididymal obstruction. Hum. Reprod. 2017;32:284–289. doi: 10.1093/humrep/dew331. [DOI] [PubMed] [Google Scholar]
- 22.Lyu KL, et al. A novel experience of deferential vessel-sparing microsurgical vasoepididymostomy. Asian J. Androl. 2018;20:576–580. doi: 10.4103/aja.aja_46_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang SY, et al. Multifactor analysis of postoperative patency of microsurgical vasoepididymostomy. J. Chin. J. Urol. 2018;39:441–445. [Google Scholar]
- 24.Tang SX, et al. Retrospective analysis of factors affecting patency rates and causes of failure in use of single-armed two-suture microsurgical vasoepididymostomy. Zhonghua Yi Xue Za Zhi. 2018;98:3741–3745. doi: 10.3760/cma.j.issn.0376-2491.2018.46.004. [DOI] [PubMed] [Google Scholar]
- 25.Shimpi RK, Raval KV, Patel DN. Modification of microsurgical longitudinal intussusception technique of vaso-epididymal anastomosis: A single-center experience. Urol. Ann. 2019;11:374–379. doi: 10.4103/ua.Ua_90_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tiwari DP, Razik A, Das CJ, Kumar R. Prospective analysis of factors predicting feasibility & success of longitudinal intussusception vasoepididymostomy in men with idiopathic obstructive azoospermia. Indian J. Med. Res. 2019;149:51–56. doi: 10.4103/ijmr.IJMR_1192_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu N, et al. A modified single-armed microsurgical vasoepididymostomy for epididymal obstructive azoospermia: Intraoperative choice and postoperative consideration. BMC Urol. 2020;20:121. doi: 10.1186/s12894-020-00692-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li P, et al. Vasal vessel-sparing microsurgical single-armed vasoepididymostomy to epididymal obstructive azoospermia: A retrospective control study. Andrologia. 2021;53:e14133. doi: 10.1111/and.14133. [DOI] [PubMed] [Google Scholar]
- 29.Wan B, et al. Current progress on the curative effects of vasoepididymostomy for patients with obstructive azoospermia: An updated systematic review and meta-analysis of human studies. Andrology. 2023;11:103–111. doi: 10.1111/andr.13300. [DOI] [PubMed] [Google Scholar]
- 30.Sutcliffe AG, Ludwig M. Outcome of assisted reproduction. Lancet. 2007;370:351–359. doi: 10.1016/s0140-6736(07)60456-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.