Abstract
Introduction:
Breast cancer is the most diagnosed cancer worldwide. With an estimated 685,000 deaths, female breast cancer was the fifth leading cause of cancer mortality worldwide, accounting for 6.9% of all cancer deaths. Previous studies have shown that late detection and delayed diagnosis are associated with advanced-stage breast cancer and poor survival. Factors contributing to non-adherence to breast cancer screening among women were elicited from previous studies. However, few studies have focused on the Muslim community, particularly Muslim women. As such, this systematic review aims to fill this gap by collecting information from studies conducted globally over the past ten years that examined cultural, religious and socio-ethical misconceptions about breast cancer screening among Muslim women.
Methods:
Following the PRISMA guidelines, literature searches were conducted systematically through various databases including PubMed, Science Direct, Scopus, Cochrane Library and Oxford Academic Journals. Article identification, screening steps and eligibility measures were meticulously performed throughout the review.
Results:
A total of 22 papers were appraised and included in this review. Five main themes were generated which were socio-ethical misconceptions, cultural and religious beliefs, cultural and religious barriers, stigmatization and fear of breast cancer impact. Eight sub-themes and 14 sub sub-themes were further elicited from the main themes.
Conclusion:
Muslim women have socio-ethical, cultural and religious misconceptions on what constitutes health and practices as well as on the nature and etiology of BC. Cultural barriers and religious values of Muslim women were indicated to influence their health behaviors such as upholding their modesty when choosing health interventions. BC stigma and fear were also found to be key sources of psychological distress that discouraged Muslim women from undergoing BC screening. The study suggests the implementation of holistic effort in educating Muslim women to increase BC screening rate.
Key Words: Breast cancer, breast cancer screening, Muslim women, systematic review
Introduction
Female breast cancer (BC) was the most prevalent cancer globally in 2020, surpassing its predecessor, lung cancer. The estimated new cases of female BC were 2.3 million cases, accounting for 11.7% of all global cancer incidence. With an estimated number of 685,000 deaths, female BC was the fifth leading cause of cancer death worldwide accounting for 6.9% of the overall deaths from cancer (Sung et al., 2021). Previous studies have demonstrated that late detection and delayed diagnosis of BC are associated with advanced BC stage and low survival rate (Caplan, 2014; Maghous et al., 2016). Besides, presuming a post-diagnosis disease management, early detection is a cornerstone to improve BC prognosis and increase the chance of survival. Advances in BC management and screening approaches have been shown to reduce the mortality rate of BC by early detection of the disease (Plevritis et al., 2018; Duffy et al., 2020; Maroni et al., 2021).
Numerous studies have evaluated the rate of BC screening participation and factors influencing women across various regions, countries, ethnicities and from different racial, religious and socio-cultural backgrounds. For instance, Satoh and Sato (2021) reported that economic factor was a major contributing factor leading to a low rate of BC screening participation among Japanese women. Factors such as accessibility to healthcare facilities (Alexandraki and Mooradian, 2010), emotional barriers (O’Hara et al., 2018) and educational levels (Özkan and Taylan, 2021) were found to influence BC screening participation among women of various socio-cultural backgrounds.
While there are many studies examining BC screening rate and factors affecting participation in BC screening among women, there are limited studies that have identified factors to BC screening participation among Muslim women. Few studies have identified several factors affecting BC screening participation among Muslim women including the cultural and religious factors, and the influence of patient characteristics on the uptake of population-based mammographic screening (Ferreira et al., 2021; Mottram et al., 2021). Although there is a growing body of literature that identifies factors affecting women’s participation in BC screening, there is a lack of systematic review that specifically examine misconceptions about BC screening among the Muslim community in order for Muslim women to participate in BC screening. In this context, the objective of this study was to examine the cultural, religious and socio-ethical misconceptions about BC screening among Muslim women in encouraging early BC screening practices. The findings of this study may pave the way for the development of effective interventions and educational programs aimed at the misconceptions and or barriers identified for BC screening.
Materials and Methods
Systematic searching strategies
This systematic review was guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Liberati et al., 2009; Moher et al., 2009; Moher et al., 2015). Relevant papers were retrieved using the systematic processes of identification, screening and eligibility (Shaffril et al., 2021). Based on the formulated research question, several keywords were used to search for papers in five databases namely, PubMed, Science Direct, Scopus, Cochrane Library and Oxford Academic Journals. Complete search strategies tailored to each database are as listed in Table 1. Article screening was carried out to include or exclude the articles based on pre-determined criteria. Refer to Table 2.
Table 1.
Keywords Used for the Search Strategy in the Identification Process
| Database | Keywords |
|---|---|
| MEDLINE (Through PubMed) |
#1 Search "Breast Neoplasms"[Mesh] |
| #2 Search breast[Title] AND (neoplasm[Title] OR neoplasms[Title] OR cancer[Title] OR cancers[Title] OR tumor[Title] OR tumors[Title] OR carcinoma[Title] OR carcinomas[Title]) | |
| #3 Search #1 OR #2 | |
| #4 Search ("Mass Screening"[Mesh] OR "Early Detection of Cancer"[Mesh]) | |
| #5 Search (screen*[Title] OR mammogra*[Title] OR “self-examin*”[Title] OR examin*[Title] OR "early diagnosis"[Title] OR "early detection"[Title]) | |
| #6 Search #4 OR #5 | |
| #7 Search muslim[Title/Abstract] | |
| #8 Search (cultur*[Title/Abstract] OR religio*[Title/Abstract] OR soci*[Title/Abstract] OR ethic* [Title/Abstract]) |
|
| #9 Search #3 AND #6 AND #7 AND #8 | |
| #10 Search #9, Filters applied: 10 years, English. | |
| The Cochrane Library | #1 MeSH descriptor: [Breast Neoplasms] explode all trees |
| #2 breast:ti | |
| #3 cancer or cancers or neoplasm or neoplasms or tumor or tumors or carcinoma or carcinomas:ti | |
| #4 #1 or (#2 and #3) 32478 | |
| #5 MeSH descriptor: [Mass Screening] explode all trees | |
| #6 MeSH descriptor: [Early Detection of Cancer] explode all tree | |
| #7 screen*:ti or mammogra*:ti “self-examin*” or examin* "early diagnosis" or "early detection": | |
| #8 #5 or #6 or #7 13757 | |
| #9 #4 and #8 1091 | |
| #10 (muslim):ti,ab,kw | |
| #11 #9 and #10 2 | |
| #12 cultur*:ti,ab,kw or religio*:ti,ab,kw or soci*:ti,ab,kw or ethic*:ti,ab,kw | |
| #13 #11 and #12 with Publication Year from 2011 to 2021, with Cochrane Library publication date Between Jan 2011 and Dec 2021, in Trials 1 | |
| Scopus | TITLE-ABS-KEY ((breast AND cancer OR cancers OR neoplasm OR neoplasms OR tumor OR tumors OR carcinoma OR carcinomas) AND (screen* OR mammogra* OR "self-examin*" OR examin* OR "early diagnosis" OR "early detection" OR "Mass Screening" OR "Early Detection of Cancer") AND muslim AND (cultur* OR religio* OR soci* OR ethic*)), Filtered by language (English) |
| Science Direct | #1 “breast cancer” |
| #2 #1 | |
| #3 “Early Detection of Cancer” | |
| #4 “Mass Screening” | |
| #5 screening | |
| #6 examine | |
| #7 mammogram | |
| #8 #3 or #4 or #5 or #6 or #7 | |
| #9 muslim | |
| #11 #2 AND #8 AND #9, Year: 2011–2021, Refine by: Article Type (“Review articles” and “Research articles”) |
Table 3.
Criteria Used for Quality Appraisal Procedure Based on MMAT 2018
| Research design | Assessment criteria |
|---|---|
| Qualitative | QA1—Is the qualitative approach appropriate to answer the research question? |
| QA2—Are the qualitative data collection methods adequate to address the research question? | |
| QA3- Are the findings adequately derived from the data? | |
| QA4- Is the interpretation of results sufficiently substantiated by data? | |
| QA5—Is there coherence between qualitative data sources, collection, analysis and interpretation? | |
| Quantitative (descriptive) |
QA1—Is the sampling strategy relevant to address the research question? |
| QA2- Is the sample representative of the target population? | |
| QA3- Are the measurements appropriate? | |
| QA4- Is the risk of nonresponse bias low? | |
| QA5- Is the statistical analysis appropriate to answer the research question? | |
| Quantitative (non- randomised) |
QA1- Are the participants representative of the target population? |
| QA2- Are measurements appropriate regarding both the outcome and intervention (or exposure)? | |
| QA3- Are there complete outcome data? | |
| QA4- Are the confounders accounted for in the design and analysis? | |
| QA5- During the study period, is the intervention administered (or exposure occurred) as intended? | |
| Mixed methods | QA1- Is there an adequate rationale for using a mixed methods design to address the research question? |
| QA2- Are the different components of the study effectively integrated to answer the research question? | |
| QA3- Are the outputs of the integration of qualitative and quantitative components adequately interpreted? | |
| QA4- Are divergences and inconsistencies between quantitative and qualitative results adequately addressed? | |
| QA5- Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? |
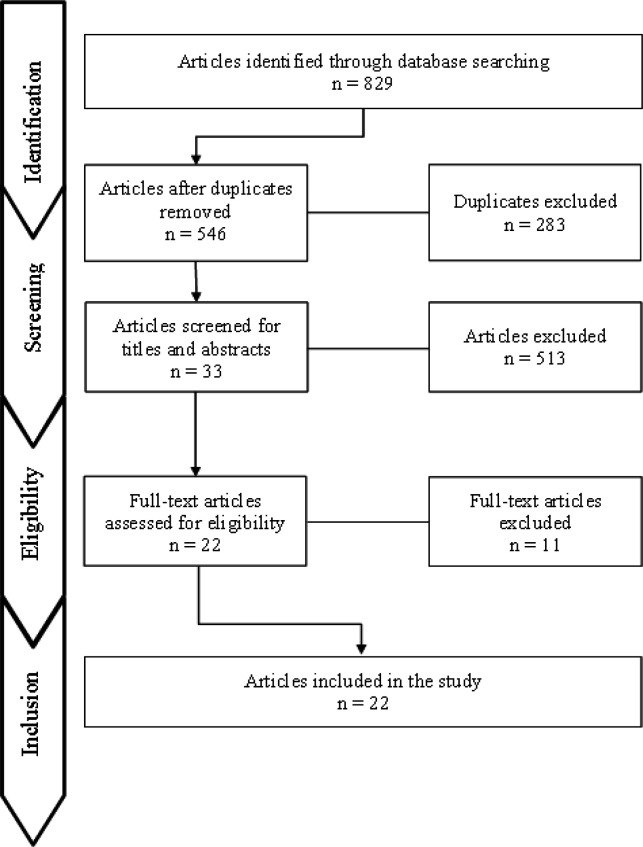
The article search was confined by language, which is English, and the date of publication, from 2011 to 2021. This process yielded 829 papers. For the article eligibility process, a researcher manually screened the articles by reading either the title or abstract or the entire paper to determine if the papers met the established inclusion criteria. A second researcher reviewed the outcome of this process. Thirty-three papers were obtained from the quality appraisal process. Refer to Figure 1.
Figure 1.
Flow of Paper Selection Process According to PRISMA 2009 Guidelines
Quality appraisal
A quality appraisal procedure was carried out by three researchers to affirm the validity and reliability of the selected papers. This appraisal procedure was conducted using the Mixed-Method Appraisal Tool (MMAT) (Hong et al., 2018). Referring to the five criteria defined in the research designs, the quality of each article selected was assessed. Refer to Table 3. if the article passed at least three criteria, it will be included in the review. Mutual concentual decisions were made on the appraised articles. This process yielded 22 articles. Refer to Table 4 and Table 5.
Table 4.
Quality Appraisal Assessment Results
| Study | Research Design | QA1 | QA2 | QA3 | QA4 | QA5 | Number of criteria fulfilled | Inclusion in the review |
|---|---|---|---|---|---|---|---|---|
| Alatrash (2020) | QN (DC) | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Shirazi et al. (2013) | QL | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Yeasmeen (2020) | QN (DC) | × | × | ✓ | × | ✓ | 2/5 | û |
| Madkhali et al. (2019) | QL | ✓ | × | ✓ | ✓ | C | 3/5 | ü |
| Vahabi et al. (2017) | QN (DC) | × | × | ✓ | ✓ | ✓ | 3/5 | ü |
| Hasnain et al. (2014) | QN (DC) | ✓ | ✓ | × | × | × | 2/5 | û |
| Pratt et al. (2020) | QN (DC) | C | ✓ | ✓ | ✓ | ✓ | 4/5 | ü |
| Al-Amoudi et al. (2015) | QL | ✓ | × | ✓ | × | ✓ | 3/5 | ü |
| Padela et al. (2015) | QN (DC) | C | ✓ | ✓ | ✓ | C | 3/5 | ü |
| Mukem et al. (2015) | QN (NR) | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Padela et al. (2018) | QN (NR) | ✓ | ✓ | C | C | ✓ | 3/5 | ü |
| Salman (2012) | QN (DC) | ✓ | × | ✓ | × | ✓ | 3/5 | ü |
| Zorogastua et al. (2017) | MX | ✓ | ✓ | × | ✓ | × | 3/5 | ü |
| Islam et al. (2017) | QL | ✓ | ✓ | × | ✓ | C | 3/5 | ü |
| Racine et al. (2021) | MX | ✓ | C | × | × | C | 1/5 | û |
| Alatrash (2021) | QN (DC) | ✓ | × | ✓ | × | ✓ | 3/5 | û |
| Soffer et al. (2020) | QN (DC) | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Padela et al. (2019) | QN (DC) | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Kissal et al. (2018) | QN (DC) | ✓ | ✓ | ✓ | × | ✓ | 4/5 | ü |
| Shaw et al. (2018) | QL | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Travado et al. (2017) | x | × | × | × | × | × | 0/5 | û |
| Padela et al. (2016) | QL | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Alkhasawneh et al. (2016) | MX | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Kawar (2013) | QL | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| Saadi et al. (2015) | QL | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
| McKeever and McDermott-Levy (2012) | x | × | × | × | × | × | 0/5 | û |
| Shaheen et al. (2011) | QN (DC) | × | × | × | × | × | 0/5 | û |
| Bowser et al. (2017) | x | × | × | × | × | × | 0/5 | û |
| Miller et al. (2019) | x | × | × | × | × | × | 0/5 | û |
| Raza et al. (2012) | QN (DC) | C | ✓ | ✓ | ✓ | ✓ | 4/5 | ü |
| Virani et al. (2018) | x | × | × | × | × | × | 0/5 | û |
| Elobaid et al. (2016) | QL | ✓ | ✓ | ✓ | ✓ | ✓ | 5/5 | ü |
QA, Quality assessment; QN (DC), Quantitative descriptive; QN (NR), Quantitative non-randomised; QL, Qualitative; MX, Mixed-Method; C, Can’t tell
Table 5.
Appraised Articles Based on Mutual Consensus among the Researchers for which the Data were Extracted
| No | Authors and publication year | Country | Sample size (n) | Proportion of Muslim women (%) | Age range of participants (years) | Methodology and instruments | Outcome | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Alatrash, 2020 | USA | 316 | 67.4 | 40 and older | Quantitative/ Questionnaire | Screening rates among Muslim women were lower than Christian women attributable to how benefits and barriers regarding screening practices were perceived and the modesty of Muslim women and their religion that bans exposing the body to a male physician. | ||||||||
| 2 | Shirazi et al., 2013 | USA | 53 | 100 | 40–87 | Qualitative/ Interview | The study showed that Muslim women have low rates of BC screening due to husbands’ influence on screening decisions, being more concerned about the well-being of children and family than their own health, prevailing tradition of cultural privacy and modesty, and lack of knowledge. | ||||||||
| 3 | Madkhali et al., 2019 | SA | 64 | 100 | 18 and older | Qualitative/ Interview | Religion, cultural background and healthcare services were found to influence the participation of Muslim women in BC screening. No differences were found between female nurses and females from the general population in terms of their knowledge of BC and awareness of breast health. | ||||||||
| 4 | Vahabi et al., 2017 | Canada | 238,218 | 17.9 | 50–74 | Quantitative/ Questionnaire | Screening rates were significantly lower among immigrant women from Muslim-majority countries. The decision to undergo BC screening may be influenced by women’s religious beliefs, a confluence of cultural beliefs and practices, socio-demographic, and immigration trajectories. | ||||||||
| 5 | Pratt et al., 2020 | USA | 30 | 100 | 30–70 | Quantitative/ Questionnaire | Some of the Muslim women's religiously attributed barrier beliefs may be combined with other cultural factors that affected the screening decisions. | ||||||||
| 6 | Al-Amoudi et al., 2015 | USA | 14 | 100 | 30–69 | Qualitative/ Focus groups interview | Barriers to participating in BC screening were reported to include fear of pain, lack of knowledge about where to seek services, preference for female or Muslim doctors, lack of doctor advice, reluctance to discuss breast health, difficulty with transport and perceiving religion as a coping mechanism for illness. | ||||||||
| 7 | Padela et al., 2015 | USA | 240 | 100 | 40 or older | Quantitative/ Questionnaire | Mammography screening rates were found to be varied based on Islam-related factors in which Muslim women with positive religious coping mechanisms and those who perceived religious discrimination in healthcare were less likely to have had a mammogram in the past two years. | ||||||||
| 8 | Mukem et al., 2015 | Thailand | 24,194,750 | 4.7 | 30–70 | Quantitative/ Questionnaire | Reasons for non-uptake of the screening included the perception that screening is not necessary and feeling nothing wrong with the breast. Muslim women were reported to have lower levels of knowledge about mammogram than Buddhist and Christian women. | ||||||||
| 9 | Padela et al., 2018 | USA | 58 | 100 | ND | Quantitative/ Questionnaire | Barrier beliefs impeding mammography screening among Muslim American women were addressed through reframing, reprioritizing, or reforming such beliefs. Findings showed nearly 40% of women obtained a mammogram within 12 months of the intervention. | ||||||||
| 10 | Salman, 2012 | USA | 50 | 100 | 18 or older | Quantitative/ Questionnaire | Participation in mammography screening was hampered by lack of time, insurance coverage and embarrassment or modest about exposing their breasts in front of strangers. | ||||||||
| 11 | Zorogastua et al., 2017 | USA | 140 | 100 | 18 and older | Mixed-methods/ Questionnaire and focus groups interview | Barriers to screening adherence revealed include negative perceptions that BC is a serious and deadly disease, misconceptions such as BC is contagious, BC is caused by mammogram, and BC screening is only necessary when women take oral contraceptives. | ||||||||
| 12 | Islam et al., 2017 | USA | 12 | 75 | ND | Qualitative/ Interview | Structural and socio-cultural barriers emerged as barriers to BC screening. Among them were language, insurance, immigration status, the feeling of fatalism, doctor’s gender, embarrassment, perceiving screening as unnecessary, prioritizing their family's health over their own and lack of knowledge about preventive care/ cancer. | ||||||||
| 13 | Soffer et al., 2020 | Israel | 433 | 85.9 | 26–70 | Quantitative/ Questionnaire | Laywomen held more cultural beliefs and more fatalistic beliefs than physicians. Laywomen also were reported to have greater social barriers to BC screening such as fear of being pitied, fear of being detachment and resentment from husbands, fear of being disrespected by family, fear of losing the place of work and friends and fear of neglecting family). | ||||||||
| 14 | Padela et al., 2019 | USA | 58 | 100 | 40–74 | Quantitative/ Questionnaire | Religiously-tailored messages to modify mammography-related beliefs among Muslim Americans were made possible as the percentage of those who agreed that BC screening is unimportant because God decides who gets the disease significantly decreased. Additionally, knowledge of mammography among participants improved after the intervention. | ||||||||
| 15 | Kissal et al., 2018 | Turkey | 339 | 100 | 40–50 | Quantitative/ Questionnaire | The findings revealed poor participation rates for women in BC screening due to high levels of perceived barriers. The women’s fear of BC was determined to be at a high level, while their fatalism was at a moderate level. | ||||||||
| 16 | Shaw et al., 2018 | Singapore | 27 | 92.6 | 40–69 | Qualitative/ Focus groups interview | Low BC screening uptake rates were attributable to barriers such as spiritual and religious beliefs, preference for traditional medicine over Western medical recommendations, family and community influence on health-related decisions, and differences in intergenerational beliefs that created different attitudes toward screening and prevention. | ||||||||
| 17 | Padela et al., 2016 | USA | 69 | 100 | 40–75 | Qualitative/ Focus groups and individual interview | Muslim women reported religion-related salient beliefs to influence their screening behaviours which included perceived responsibility for body and health care, religious practices as methods of disease prevention, fatalistic views about health, and preference for female healthcare providers due to modesty norms. | ||||||||
| 18 | Alkhasawneh et al., 2016 | Oman | 1391 | 100 | 20 and older | Mixed-methods/ Questionnaire, interviews and focus group discussions | The level of early detection screening practice was reported to be influenced by age, education and marital status. Additionally, the factors also included the perception of BC such as BC as a cursed word, “taboo” and ill-fated disease, and superstitious beliefs especially the belief in the “evil eye” or envy as a risk factor for BC. | ||||||||
| 19 | Kawar, 2013 | USA | 107 | 52.3 | 20–80 | Qualitative/ Interview | Findings revealed numerous barriers to BC screening which include embarrassment, fear of getting BC, ignorance, lack of motivation, stigmatization of cancer, family relationships, fatalistic beliefs, consultation of traditional healers, affordability, availability of services, citizenship and language issues. | ||||||||
| 20 | Saadi et al., 2015 | USA | 57 | 96.5 | 18–75 | Qualitative/ Interview | Among the barriers to BC screening among refugee women were fear of pain and diagnosis, modesty, work and childcare commitments, outreach efforts, appointment reminders, personal contact from health providers, varying degrees of medical exposure to doctors in home countries and the impact of war on health systems. | ||||||||
| 21 | Raza et al., 2012 | Pakistan | 300 | 81 | 23–63 | Quantitative/ Questionnaire | The embarrassment, painful procedures, fear of bringing disgrace to their families and fear of being rejected or divorced by husbands from the diagnosis of BC, lack of transportation and expense of travel were cited as barriers to screening. | ||||||||
| 22 | Elobaid et al., 2016 | UAE | 19 | 100 | 35–68 | Qualitative/ Interview | The themes that emerged with regards to barriers in health seeking behavior were symptom recognition and appraisal, fear of societal stigmatization, fear of being abandoned by the husband because of BC, lack of awareness of the nature of BC and routine screening, and healthcare system such as male doctors and errors in diagnosis. | ||||||||
ND, no data
Table 6.
Results of the Thematic Analysis of the 22 Selected Articles
| Main Themes | Sub-themes | Sub sub-themes | Statement |
|---|---|---|---|
| Socio-ethical misconception |
Barriers for BC screening | Conception of health | Health is regarded as the absence of disease/ conception of health (Shirazi et al., 2013; Salman, 2012; Saadi et al., 2015; Padela et al., 2016), perceived to be healthy as they don’t have to see a doctor (Islam et al., 2017). |
| Healthcare practices | No need to seek medical advice if no symptom(s)/ symptom recognition (Saadi et al., 2015; Elobaid et al., 2016; Kissal et al., 2018; Madkhali et al., 2019), sought care only when necessary (Zorogastua et al., 2017). | ||
| Misconception of BC | Cause of BC | BC is contagious (Al-Amoudi, 2015; Elobaid et al., 2016; Zorogastua et al., 2017), injury to breast cause BC (Al-Amoudi, 2015), etiology of BC (Raza et al., 2012; Al-Amoudi, 2015; Elobaid et al., 2016; Alkhasawneh et al., 2016; Madkhali et al., 2019; Soffer et al., 2020), evil eye (Kawar, 2013; Elobaid et al., 2016; Alkhasawneh et al., 2016; Shaw et al., 2018). | |
| Cultural/ religious belief | Cultural belief | Alternative treatment | Alternative treatment - holy water, superstitious belief, black magic (Kawar, 2013; Shaw et al., 2018; Madkhali et al., 2019). |
| Religious belief | Fatalism | Construed cultural and religious beliefs discourage screening (Padela et al., 2019; Pratt et al., 2020), developing cancer is viewed as inevitable, women would not get screened and believed it’s fated (Islam et al., 2017), view illness as divinely ordained (Shirazi et al., 2013; Padela et al., 2015; Saadi et al., 2015; Padela et al., 2016; Alkhasawneh et al., 2016; Shaw et al., 2018; Kissal et al., 2018; Pratt et al., 2020; Soffer et al., 2020). | |
| Role of religion | Dying from BC as a test of faith in Allah (God) (Madkhali et al., 2019; Pratt et al., 2020), worship practices and faith protect/diminish disease risk (Padela et al., 2016), God’s retribution or curse (Vahabi et al., 2017), punishment from God (Elobaid et al., 2016; Vahabi et al., 2017; Islam et al., 2017; Padela et al., 2019; Soffer et al., 2020), God gave the disease and God can take away the disease (Al-Amoudi, 2015), chances of getting cancer is in the hands of Allah (Zorogastua et al., 2017; Padela et al., 2019). | ||
| Cultural/ religious barrier | Cultural barrier | Reluctance to discuss breast health/ screening | Feeling shy with healthcare personnel (Salman et al., 2012; Shirazi et al., 2013; Kawar, 2013), uncomfortable/ reluctance of discussing health matters with healthcare provider (Al-Amoudi, 2015; Elobaid et al., 2016; Padela et al., 2018), embarrassed talking or engaging in screening (Islam et al., 2017), talking about the breast or the body is shameful (Islam et al., 2017). |
| Family relationship | Influence of family (Raza et al., 2012; Kawar, 2013; Shaw et al., 2018), negative perceptions of BC screening (Zorogastua et al., 2017), Muslim men against breast screening by male providers (Zorogastua et al., 2017), prioritizing the well-being of family members over own (Shirazi et al., 2013; Islam et al., 2017), work and/or childcare commitments (Saadi et al., 2015; Zorogastua et al., 2017). | ||
| Religious barrier | Modesty | Modesty/ privacy - exposing breast/ body (Salman, 2012; Kawar, 2013; Mukem et al., 2015; Saadi et al., 2015; Padela et al., 2016; Vahabi et al., 2017; Padela et al., 2018; Shaw et al., 2018; Alatrash, 2020), embarrassment of exposing body to the male healthcare providers (Salman, 2012; Kawar, 2013; Shirazi et al., 2013; Mukem et al., 2015; Elobaid et al., 2016; Padela et al., 2016; Padela et al, 2018; Alatrash, 2020), mistrust with male healthcare providers (Zorogastua et al., 2017), modesty of how women should interact with males (Islam et al., 2017), refuse treatment by male healthcare provider (Salman, 2012; Elobaid et al., 2016), adherence practice of religious faith - aurah, close physical contact (Salman, 2012). | |
| Stigma | BC | Stigma with diagnosis of BC (Raza et al., 2012; Kawar, 2013; Elobaid et al., 2016; Soffer et al., 2020; Alatrash, 2020), concerns of healthcare providers living in the same village (Mukem et al., 2015), shame seen by neighbours when attending screening (Mukem et al., 2015; Alatrash, 2020). | |
| Self-image | Altered image of losing breast(s) - less attractive, feminine (Madkhali et al., 2019), shame to admit if suffer from cancer (Zorogastua et al., 2017). | ||
| Fear | BC | Diagnosis | BC diagnosis, abnormalities (Kawar, 2013; Saadi et al., 2015; Kissal et al., 2018; Padela et al., 2018; Alatrash, 2020). |
| Screening procedure | Discomfort from the screening procedure (Alatrash, 2020), fear of BC screening (Zorogastua et al., 2017). | ||
| Pain | Fear of pain (Saadi et al., 2015; Al-Amoudi, 2015; Mukem et al., 2015; Padela et al., 2018). | ||
| Rejection | Rejection from family, friends and husband (Raza et al., 2012; Kawar, 2013; Elobaid et al., 2016; Islam et al., 2017; Soffer et al., 2020). |
Data extraction and analysis
The 22 articles were further analysed thematically by three researchers. The steps of thematic synthesis proposed by Kiger and Varpio (2020) were adopted for this process. The first step involved familiarization with the overall dataset through repeated and active readings. This step allowed valuable raw data orientation and was vital to subsequent steps. Initial codes were generated by organizing data at the granular and specific levels during the second step. At this stage, all the selected articles were read and any data relevant to the research question was extracted. Inductive coding framework was utilized and any connections and similarities between the extracted data were noted during the final step of the data extraction and analysis. Through these processes, five main themes were generated followed by subsequent sub-themes and sub sub-themes. All the themes, sub-themes and sub sub-themes were reviewed and validated by two researchers.
Results
Background of selected studies
A final 22 articles from 2012 to 2020 were included in this systematic review (Raza et al., 2012; Salman, 2012; Kawar, 2013; Shirazi et al., 2013; Al-Amoudi et al., 2015; Padela et al., 2015; Saadi et al., 2015; Mukem et al., 2015; Padela et al., 2016; Elobaid et al., 2016; Alkhasawneh et al., 2016; Zorogastua et al., 2017; Vahabi et al., 2017; Islam et al., 2017; Padela et al., 2018; Kissal et al., 2018; Shaw et al., 2018; Padela, 2019; Madkhali et al., 2019; Alatrash, 2020; Pratt et al., 2020; Soffer et al., 2020). Out of the 22 articles, fourteen studies were carried out in the United States of America (USA) while one study was carried out in Saudi Arabia, Canada, Thailand, Israel, Turkey, Singapore, Oman and United Arab Emirates (UAE). Eleven studies were carried out quantitatively whilst nine studies were conducted qualitatively. The remaining two studies employed a mixed-method study design. The breakdown of the articles used in this review is as shown in Figure 2.
Themes and sub-themes generated
Following the thematic analysis of the 22 selected papers, five main themes were generated: (1) socio-ethical misconception, (2) cultural and religious belief, (3) cultural and religious barrier, (4) stigmatization and (5) fear of BC impact. Eight sub-themes and 14 sub sub-themes were further elicited from the five main themes. Refer to Table 6.
Table 2.
Inclusion and Exclusion Criteria for Article Selection
| Criterion | Inclusion | Exclusion |
|---|---|---|
| Time/period | 10 years (2011–2021) | Before 2011 |
| Language | English | Other than English |
| Type of article | Quantitative, Qualitative, Mixed Method | Review, Clinical Studies, Laboratory Studies, Case Studies, Opinion Paper, Policy Paper, Predatory Paper |
| Population | Muslim community, Muslim women, Muslim female healthcare professionals | Other than Muslim community and Muslim women |
Discussion
The five main themes were generated from the thematic analysis to answer the research question on cultural, religious and socio-ethical misconceptions leading to poor adoption of BC screening practices among the Muslim community will be discussed below.
Socio-ethical misconception of BC screening
The adoption of BC screening practices among Muslim women appears to be influenced by multiple factors and is extremely complex. Health-related concept was one of the factors elicited from the findings of this review. For some people, health is considered as the absence of disease (Shirazi et al., 2013) while for others, an individual is considered healthy if he/she has no signs and symptoms of the disease leading to the perception that they are in good health if they do not have to see a doctor (Islam et al., 2017). This concept can then lead to the underlying disease to be masked and hence prevents early detection (Salman, 2012). Additionally, it would prevent the individual from not going for BC screening (Salman, 2012; Shirazi et al., 2013; Saadi et al., 2015; Padela et al., 2016; Zorogastua et al., 2017; Madkhali et al., 2019). In the included studies, Salman (2012) reported that women from Middle Eastern cultures perceive themselves to be in good health so long as they are capable to carry out daily activities. In another study conducted by Shirazi et al. (2013), health is perceived as the ability to perform duties and responsibilities towards family and is not considered as the absence of disease. These misconceptions of health in turn cause health practice misconceptions among women in undertaking BC screening as a preventive measure against BC.
Misconceptions about BC also affects women’s decision to participate in BC screening. While the decision to be screened for BC as a whole is in the hands of the individual, socio-cultural factors such as health beliefs and perceptions, cultural psychological status, urgency of care, enabling factors towards seeking care, barrier-free health care facilities and family social support have a significant impact on a person’s decision-making in health-seeking behavior (Ma et al., 2013). In the included study conducted by Elobaid et al. (2016), it was reported that some women in UAE were afraid to undergo BC screening for fear of being isolated from society as the community viewed BC as being a contagious disease. On the contrary, Al-Amoudi et al. (2015) reported that although some people knew that BC was not contagious, the prevalence of cultural beliefs led them to have misconceptions about the disease. Further, an included study conducted on Omani women found that the belief in the “evil eye” or envy as the cause of BC is prevalent among young and unmarried women. It was further reported in the study that most of the participants from all education levels tended to agree with this belief of the “evil eye” and was highest among those with low education (Alkhasawneh et al., 2016).
Cultural and religious belief
Widespread cultural beliefs on alternative treatments to BC were found to inhibit the adoption of BC screening among Muslim women. This includes the belief in healing through herbal medications, incantation or holy water (Shaw et al., 2018; Madkhali et al., 2019) as well as the belief in black magic (Kawar, 2013; Alkhasawneh et al., 2016; Elobaid et al., 2016; Shaw et al., 2018). The findings of this review indicated that in the Malay culture, low participation in BC screening uptake was associated with distrust in modern medicine and the inclination towards traditional medicine (Shaw et al., 2018). This finding is consistent with another study conducted by Citrin et al., (2012) in which BC patients refused chemotherapy and radiotherapy even though it is proven to be safe and efficacious. This is because they perceived that alternative therapies are safer and can fulfil their psychological needs (Moschèn et al., (2001).
In the included studies, some Muslim women believe that BC was fated and therefore could or should not be prevented. Hence, participating in BC screening was futile and interference with God’s will. Most of the included studies reported a high degree of fatalistic beliefs had led to a lower BC screening participation (Kawar, 2013; Saadi et al., 2015; Padela et al., 2016; Islam et al., 2017; Kissal et al., 2018; Shaw et al., 2018; Padela et al., 2019; Soffer et al., 2020). The finding is also in line with a study carried out by Shirazi et al., (2013) that reported fatalism was a barrier to BC screening among Muslim women. This is because women who strongly believe that BC is the will of God will regard BC as a divine punishment or test and treatment of BC is only effective if God allows it. Hence, they surrendered their fate completely to their destiny (Hajian et al., 2017). In the included study carried out by Kissal et al., (2018), it was reported that women with low education have high perceived level of fatalism. They believed that illnesses were divinely ordained and tragic events happened because of God and cannot be avoided. As such, Muslim women with fatalism beliefs may feel powerless as they perceived BC was fated (Shirazi et al., (2013).
Cultural and religious barrier
The findings of this review also found that some Muslim women were reluctant to discuss their breast health and screening. This then could influence their decision on BC screening uptake. Further, patriarchal marital beliefs and gender roles were also found to influence the support for Muslim women to undergo BC screening. It was reported in the included studies that some Muslim women were shy and uncomfortable to discuss their health matters and breast health with healthcare personnel (Salman et al., 2012; Kawar, 2013; Shirazi et al., 2013; Al-Amoudi et al., 2015; Elobaid et al., 2016; Padela et al., 2018). This is because they perceived it as shameful to talk about their breast or body (Islam et al., 2017). This finding correlated to an included study that found the influence of cultural beliefs of Muslim women which regarded their breast as an intimate and personal organ that should not be openly discussed. As such, they felt embarrassed to talk or get involved in BC screening (Islam et al., 2017). The review also found that culturally, Muslim women were taught to keep their breasts for their spouse’s satisfaction and as such this perception prevented women from undergoing screening administered by male providers (Zorogastua et al., 2017). Key informants from the included studies reported that Muslim women are expected to prioritize the health of their families before their own health (Padela et al., 2012; Islam et al., 2017). Due to this, many Muslim women delay or do not seek preventive BC screening (Islam et al., 2017). Further, an included study indicated that work and childcare commitments were common barriers for adopting BC screening practices particularly if they do not have a flexible work schedule (Saadi et al., 2015).
The religious views and values of Muslim women also influence their health behaviors such as upholding their modesty when choosing health interventions (Padela et al., 2014; Amir et al., 2022). In this respect, it was reported in almost all the included studies that Muslim women were embarrassed to expose their breasts or bodies to healthcare providers especially to male healthcare providers (Salman, 2012; Kawar, 2013; Shirazi, 2013; Mukem et al., 2015; Saadi et al., 2015; Elobaid et al., 2016; Padela et al., 2016; Islam et al., 2017; Vahabi et al., 2017; Padela et al., 2018; Shaw et al., 2018; Alatrash, 2020). Modesty appeared to significantly influence Muslim women’s health decision-making. Since modesty is often viewed in the context of gender dissonant care, there were concerns about how women should interact with male healthcare providers which then could cause refusal of treatment of Muslim women mainly due to the medical mistrust of male healthcare providers (Salman, 2012; Elobaid et al., 2016; Islam et al., 2017; Zorogastua et al., 2017). Additionally, adherence to religious teaching in covering the aurah caused some Muslim women to have a particular concern about having close physical contact and exposing their body parts to others of the opposite gender (Salman, 2012).
BC stigma
BC stigma was indicated to significantly influence BC screening practices among Muslim women with BC (Raza et al., 2012; Kawar, 2013; Elobaid et al., 2016; Alatrash, 2020; Soffer et al., 2020). Inclusive studies indicated that there was a concern of healthcare providers living in the same village (Mukem et al., 2015) as well as fear of being seen by neighbours and acquaintances while attending BC screenings (Alatrash, 2020). This could be due to their worries about screening privacy and embarrassment (Mukem et al., 2015; Alatrash, 2020). This review also discovered that some Muslim women felt ashamed to admit if they are diagnosed with BC (Zorogastua et al., 2017). It was further reported that some Muslim women were concerned with an altered image of losing their breast and becoming less attractive and feminine if diagnosed with BC (Madkhali et al., 2019). This is because culturally, the women’s breasts is associated with motherhood, feminity, security and sexual desire. Hence, it will impact the women’s coping role if they were to lose one or both breasts or the risk of having misaligned breasts (Madkhali et al., 2019). As such, BC stigma is a major source of psychological distress mediated through body image among Muslim women (Amini-Tehrani et al., 2021).
Fear of BC
Poor BC screening uptake among Muslim women was found to be attributed to fear of BC diagnosis (Kawar, 2013; Saadi et al., 2015; Kissal et al., 2018; Padela et al., 2018; Alatrash, 2020). Fear of BC diagnosis was so significant amongst Muslim women almost at a paralyzing level to an extent of even hearing or talking about it. Fear of BC treatment and visible body image changes such as hair loss and breast deformity that take place after treatment were reported as fear of BC diagnosis. Hence, they prefer not to know which then obstructed them from pursuing BC screening (Kawar, 2013; Saadi et al., 2015; Kissal et al., 2018; Padela et al., 2018; Alatrash, 2020). Further, it was indicated that some Muslim women fear of mammographic screening procedures (Zorogastua et al., 2017; Alatrash, 2020) due to fear of pain (Al-Amoudi et al., 2015; Mukem et al., 2015; Saadi et al., 2015; Padela et al., 2018) and would rather avoid undergoing the procedure. Additionally, fear of finding breast abnormalities even if it is benign could evoke fear of death and as such, they prefer not to know (Madkhali et al., 2019; Alatrash, 2020). Furthermore, an inclusive study suggested that some Muslim women who were diagnosed with BC perceived that they had done something “bad” and fear of rejection by family, friends and husbands and hence will delay screening until it is at an advanced stage (Islam et al., 2017).
Based on this review, Muslim women have socio-ethical misconceptions about what constitutes health and what determines good health practices as well as on the nature and etiology of BC. Further, the review suggested that Muslim women have construed cultural and religious beliefs on BC fatality and were inclined to adopt alternative treatments such as holy water and black magic. Cultural barriers such as reluctance to discuss on breast health issues as well as the influence of family relationship were also found to impact the uptake of BC screening. Religious views and values of Muslim women were also indicated to influence their health behaviors such as upholding their modesty when choosing health interventions. BC stigma was also found to be a key source of psychological distress mediated through body image among Muslim women. Fear of BC impact such as BC screening and diagnosis as well as rejection from spouse were among the factors that discouraged Muslim women from undergoing BC screening. Therefore, this study suggests the implementation of efforts in a comprehensive and holistic manner using numerous approaches to ensure efficiency and effectiveness in educating Muslim women to increase the rate of BC screening in reducing morbidity and mortality caused by the disease.
Author Contribution Statement
MSF designed the study. MSF, SNS and NSMA were involved in the journal appraising, peer checking and developing the first draft. NSMA searched the databases. MSF, SNS and NSMA performed the study quality assessments. AAH and MFMI performed peer checking of the content. NCM prepared the manuscript and MSF performed critical revision of the manuscript. MSF, SNS and NCM finalized the manuscript.
Acknowledgements
Funding Statement
This study is made possible through a research grant provided by the Islamic Advisory Group (IAG). The authors extend their gratitude and appreciation to the IAG for funding this project (SPI22-121-0121). This study was not conducted as part of a student’s thesis or dissertation.
Ethical Approval
This study did not involve the use of human or animal participants, therefore, ethical approval does not apply. This study was approved by the IIUM Research Ethics Committee (IREC).
Availability of Data
Data are available by request to the corresponding author.
Study Registration
This systematic review was conducted according to PRISMA guidelines; however, the review was not registered in any data set.
Conflict of Interest
The authors declare no potential conflicts of interest.
References
- Al-Amoudi S, Cañas J, Hohl SD, Distelhorst SR, Thompson B. Breaking the silence: Breast cancer knowledge and beliefs among Somali Muslim women in Seattle, Washington. Health Care Women Int. 2015;36:608–16. doi: 10.1080/07399332.2013.857323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alatrash M. Prevalence, perceived benefits, and perceived barriers regarding breast cancer screening among three Arab American women subgroups. J Transcult Nurs. 2020;31:242–9. doi: 10.1177/1043659619859058. [DOI] [PubMed] [Google Scholar]
- Alexandraki I, Mooradian AD. Barriers related to mammography use for breast cancer screening among minority women. J Natl Med Assoc. 2010;102:206–18. doi: 10.1016/s0027-9684(15)30527-7. [DOI] [PubMed] [Google Scholar]
- Alkhasawneh E, Siddiqui ST, Leocadio M, et al. I do not even say ‘It’—A mixed methods study on breast cancer awareness of Omani Women. Asian Pac J Cancer Prev. 2016;17:2247–54. doi: 10.7314/apjcp.2016.17.4.2247. [DOI] [PubMed] [Google Scholar]
- Amini-Tehrani M, Zamanian H, Daryaafzoon M, et al. Body image, internalized stigma and enacted stigma predict psychological distress in women with breast cancer: A serial mediation model. J Adv Nurs. 2021;77:3412–23. doi: 10.1111/jan.14881. [DOI] [PubMed] [Google Scholar]
- Caplan L. Delay in breast cancer: Implications for stage at diagnosis and survival. Front Public Health. 2014;2:1–5. doi: 10.3389/fpubh.2014.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Citrin DL, Bloom DL, Grutsch JF, Mortensen SJ, Lis CG. Beliefs and perceptions of women with newly diagnosed breast cancer who refused conventional treatment in favor of alternative therapies. Oncologist. 2012;17:607–12. doi: 10.1634/theoncologist.2011-0468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffy S, Vulkan D, Cuckle H, et al. Annual mammographic screening to reduce breast cancer mortality in women from age 40 years: Long-term follow-up of the UK Age RCT. Health Technol Assess. 2020;24:1–24. doi: 10.3310/hta24550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira C, Rodrigues J, Moreira S, Ribeiro F, Longatto filho A. Breast cancer screening adherence rates and barriers of implementation in ethnic, cultural and religious minorities: A systematic review. Mol Clin Oncol. 2021;15:1–9. doi: 10.3892/mco.2021.2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elobaid Y, Aw TC, Lim JNW, Hamid S, Grivna M. Breast cancer presentation delays among Arab and national women in the UAE: A qualitative study. SSM Popul Health. 2016;2:155–63. doi: 10.1016/j.ssmph.2016.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajian S, Mehrabi E, Simbar M, Houshyari M. Coping strategies and experiences in women with a primary breast cancer diagnosis. Asian Pac J Cancer Prev. 2017;18:215–24. doi: 10.22034/APJCP.2017.18.1.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong QN, Pluye P, Fàbregues S, et al. The Mixed Methods Appraisal Tool (MMAT) Version 2018 for Information Professionals and Researchers. Educ Inf. 2018;34:285–91. [Google Scholar]
- Islam N, Patel S, Brooks-Griffin Q, et al. Understanding barriers and facilitators to breast and cervical cancer screening among Muslim women in New York City: Perspectives from key informants. SM J Community Med. 2017;3:1–14. [PMC free article] [PubMed] [Google Scholar]
- Kawar LN. Barriers to breast cancer screening participation among Jordanian and Palestinian American women. Eur J Oncol Nurs. 2013;17:88–94. doi: 10.1016/j.ejon.2012.02.004. [DOI] [PubMed] [Google Scholar]
- Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE Guide No 131. Med Teach. 2020;42:846–54. doi: 10.1080/0142159X.2020.1755030. [DOI] [PubMed] [Google Scholar]
- Kissal A, Ersin F, Koç M, Vural B, Çetin Ö. Determination of women’s health beliefs, breast cancer fears, and fatalism associated with behaviors regarding the early diagnosis of breast cancer. Int J Cancer Manag. 2018;11:1–9. [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Wang MQ, Ma XS, et al. The sociocultural health behavioral model and disparities in colorectal cancer screening among Chinese Americans. J Nurs Educ Pract. 2013;3:129–39. doi: 10.5430/jnep.v3n7p129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madkhali NA, Santin O, Noble H, Reid J. Breast health awareness in an Arabic culture: A qualitative exploration. J Adv Nurs. 2019;75:1713–22. doi: 10.1111/jan.14003. [DOI] [PubMed] [Google Scholar]
- Maghous A, Rais F, Ahid S. Factors influencing diagnosis delay of advanced breast cancer in Moroccan women. BMC Cancer. 2016;16:1–8. doi: 10.1186/s12885-016-2394-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maroni R, Massat NJ, Parmar D, et al. A case-control study to evaluate the impact of the breast screening programme on mortality in England. Br J Cancer. 2021;124:736–43. doi: 10.1038/s41416-020-01163-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6:1–6. [PMC free article] [PubMed] [Google Scholar]
- Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mottram R, Knerr WL, Gallacher D, et al. Factors associated with attendance at screening for breast cancer: A systematic review and meta-analysis. BMJ Open. 2021;11:1–12. doi: 10.1136/bmjopen-2020-046660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moschèn R, Kemmler G, Schweigkofler H, et al. Use of alternative/ complementary therapy in breast cancer patients—A psychological perspective. Supportive Care Cancer. 2001;9:267–74. doi: 10.1007/s005200000208. [DOI] [PubMed] [Google Scholar]
- Mukem S, Meng Q, Sriplung H, Tangcharoensathien V. Low coverage and disparities of breast and cervical cancer screening in Thai women: Analysis of national representative household surveys. Asian Pac J Cancer Prev. 2015;16:8541–51. doi: 10.7314/apjcp.2015.16.18.8541. [DOI] [PubMed] [Google Scholar]
- O’Hara J, McPhee C, Dodson S, et al. Barriers to breast cancer screening among diverse cultural groups in Melbourne, Australia. Int J Environ Res Public Health. 2018;15:1–13. doi: 10.3390/ijerph15081677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özkan İ, Taylan S. Barriers to women’s breast cancer screening behaviors in several countries: A meta-synthesis study. Health Care Women Int. 2021;42:1013–43. doi: 10.1080/07399332.2020.1814777. [DOI] [PubMed] [Google Scholar]
- Padela AI, Peek M, Johnson-Agbakwu CE, Hosseinian Z, Curlin F. Associations between religion-related factors and cervical cancer screening among Muslims in greater Chicago. J Low Genit Tract Dis. 2014;18:326–32. doi: 10.1097/LGT.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padela AI, Murrar S, Adviento B, et al. Associations between religion-related factors and breast cancer screening among American Muslims. J Immigr Minor Health. 2015;17:660–9. doi: 10.1007/s10903-014-0014-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padela AI, Vu M, Muhammad H, et al. Religious beliefs and mammography intention: Findings from a qualitative study of a diverse group of American Muslim women: Islam and mammography intention. Psychooncology. 2016;25:1175–82. doi: 10.1002/pon.4216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padela AI, Malik S, Ally SA, et al. Reducing Muslim mammography disparities: Outcomes from a religiously tailored mosque-based intervention. Health Educ Behav. 2018;45:1025–35. doi: 10.1177/1090198118769371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Padela AI, Malik S, Din H, Hall S, Quinn M. Changing mammography-related beliefs among American Muslim women: Findings from a religiously-tailored mosque-based intervention. J Immigr Minor Health. 2019;21:1325–33. doi: 10.1007/s10903-018-00851-9. [DOI] [PubMed] [Google Scholar]
- Plevritis SK, Munoz D, Kurian AW, et al. Association of screening and treatment with breast cancer mortality by molecular subtype in US women, 2000-2012. JAMA. 2018;319:154–64. doi: 10.1001/jama.2017.19130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt R, Mohamed S, Dirie W, et al. Testing a religiously tailored intervention with Somali American Muslim women and Somali American imams to increase participation in breast and cervical cancer screening. J Immigr Minor Health. 2020;22:87–95. doi: 10.1007/s10903-019-00881-x. [DOI] [PubMed] [Google Scholar]
- Raza S, Sajun SZ, Selhorst CC. Breast cancer in Pakistan: Identifying local beliefs and knowledge. J Am Coll Radiol. 2012;9:571–7. doi: 10.1016/j.jacr.2012.02.020. [DOI] [PubMed] [Google Scholar]
- Saadi A, Bond BE, Percac-Lima S. Bosnian, Iraqi, and Somali Refugee women Speak: A comparative qualitative study of refugee health beliefs on preventive health and breast cancer screening. Womens Health Issues. 2015;25:501–8. doi: 10.1016/j.whi.2015.06.005. [DOI] [PubMed] [Google Scholar]
- Salman KF. Health beliefs and practices related to cancer screening among Arab Muslim women in an Urban community. Health Care Women Int. 2012;33:45–74. doi: 10.1080/07399332.2011.610536. [DOI] [PubMed] [Google Scholar]
- Satoh M, Sato N. Relationship of attitudes toward uncertainty and preventive health behaviors with breast cancer screening participation. BMC Womens Health. 2021;21:1–11. doi: 10.1186/s12905-021-01317-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffril HAM, Samah AA, Kamarudin S. Speaking of the devil: A systematic literature review on community preparedness for earthquakes. Nat Hazards. 2021;108:2393–419. [Google Scholar]
- Shaw T, Ishak D, Lie D, et al. The influence of Malay cultural beliefs on breast cancer screening and genetic testing: A focus group study. Psychooncology. 2018;27:2855–61. doi: 10.1002/pon.4902. [DOI] [PubMed] [Google Scholar]
- Shirazi M, Bloom J, Shirazi A, Popal R. Afghan immigrant women’s knowledge and behaviors around breast cancer screening. Psycooncology. 2013;22:1705–17. doi: 10.1002/pon.3216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soffer M, Cohen M, Azaiza F. The role of explanatory models of breast cancer in breast cancer prevention behaviors among Arab-Israeli physicians and laywomen. Prim Health Care Res Dev. 2020;21:1–7. doi: 10.1017/S1463423620000237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- Vahabi M, Lofters A, Kim E, et al. Breast cancer screening utilization among women from Muslim majority countries in Ontario, Canada. Prev Med. 2017;105:176–83. doi: 10.1016/j.ypmed.2017.09.008. [DOI] [PubMed] [Google Scholar]
- Zorogastua K, Sriphanlop P, Reich A, et al. Breast and cervical cancer screening among US and non-US born African American Muslim women in New York City. AIMS Public Health. 2017;4:78–93. doi: 10.3934/publichealth.2017.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available by request to the corresponding author.