Abstract
Background:
Chemotherapy resistance is caused by a multiplicity of reasons; some of which can be avoided and others that are beyond the scope of current treatment methods. Since chemotherapy is administered under the supervision of health personnel, the role of oncologists cannot be undermined, and yet none is known about their knowledge and perspective. This research is the first-ever study aiming to develop a valid and reliable tool to determine oncologists’ knowledge, attitude, and practice (KAP) toward chemotherapy resistance.
Methods:
Based on information gathered from literature searches, in-depth interviews with oncologists, and discussions with experts, an English-language questionnaire was developed. The questionnaire was tested for validity and reliability. A final version of the questionnaire (63 items) was piloted among 64 practicing oncologists and oncology trainees via convenient sampling. Data analysis was done using SPSS.
Results:
Correlation coefficients for each of the questionnaire’s domains were more than 0.7 (P<0.001), which suggests that the questionnaire had strong test-retest reliability. The overall internal consistency (Cronbach’s alpha) for knowledge (0.728), attitude (0.722), and practice (0.716) were greater than 0.7 indicating good internal consistency. Participants demonstrated a low level of knowledge and a positive attitude toward chemotherapy resistance. A statistically significant difference was noted between the knowledge score and education level, years of experience in the medical and oncology field, and experiencing resistance cases.
Conclusion:
The developed questionnaire was found to be valid and reliable and can be used as an assessment tool for assessing oncologists’ knowledge, attitude, and practice toward chemotherapy resistance in future studies. This study also reported that the oncologists have low knowledge on chemotherapy resistance and a predominantly positive attitude towards fighting chemotherapy resistance. Thus, it is essential for current practices in chemotherapy to be optimized to reduce the risk of chemotherapy resistance.
Key Words: Chemotherapy resistance, knowledge, attitude, practice, oncologists
Introduction
Chemotherapy resistance happens when cancers suddenly begin to grow despite having previously responded to therapy (Van der Jeught et al., 2018). This means that the drugs which are used in the therapy would be no longer effective in attacking the cancer cells. For both the patients and oncologists, chemotherapy resistance is a disheartening issue because it nullifies the efforts which have been made towards the treatment (Phi et al., 2018). Therefore, once the oncologists note that the cancers are no longer responding to the current therapy which they are administering, it is recommended for the drugs to be changed. Before changing the therapy and drugs being given to the patient; it is essential for the oncologists to be aware of the causes for drug resistance in cancer patients and rectify these causes in the next phase of treatment (Lim & Ma, 2019). Therefore, this brings growing attention to the role of oncologists in monitoring chemotherapy resistance. The knowledge which the oncologists have on chemotherapy resistance would determine the extent to which they would monitor it among their patients. The attitudes which oncologists have towards chemotherapy resistance would steer their actions in incidents where they are treating patients and there is a high risk of drug resistance occurring.
For patients who have been undergoing chemotherapy for a while, the remaining cancer cells mutate, and they become resistant to the therapy (Vasan et al., 2019). This indicates that the cancer cells are no longer responsive to that type of treatment and a change of treatment is required. The danger, however, of chemotherapy resistance, is that there might be a lack of any alternative treatment to cancer, and thus the patient would eventually die. When cancer patients become resistant to drugs, cancer would continue to grow and multiply leading to fatality. In some instances, the cancer cells may amplify and replicate themselves, and the gene would nullify the effects of an anti-cancer drug which has been administered (Wang et al., 2019). Another danger which is posed by chemotherapy resistance is that the cancer cells would repeal the drug, repair themselves from anti-cancer drugs or even inactivate the drug. This compromises the patient because they would be unable to benefit from any treatment which is being administered to them (Nikolaou et al., 2018). Despite the cause, it is essential for oncologists to be able to aptly identify any signs of potential cancer resistance, quickly cure it and prevent it from recurring in the patients.
Chemotherapy resistance has been explored by different scholars and they have resulted in a wide range of findings that have been implemented in cancer treatment (Bahar et al., 2019; Christie & Bowtell, 2017; Kalal et al., 2017). However, most of the studies have been focused on drug administration, the composition of drugs, and the variables of the patient’s medical history and response to drugs. There are limited studies that have focused on oncologists and their knowledge, attitude, and practice toward chemotherapy resistance (Kim, 2016; Pokhriyal et al., 2019). As of date, there is limited evidence of any tool which has been designed to achieve this objective; thus, there is limited evidence of how the oncologists perceive chemotherapy resistance. Developing a questionnaire in this field is essential because it would kick-start the process of engaging oncologists and their varied experiences with chemotherapy resistance (Nedeljković & Damjanović, 2019). Additionally, the development of the questionnaire is a landmark step that can drive the improvement of oncology. Improving the quality of oncologists through equipping them with the relevant resources and support would result in better outcomes in the treatment of cancer. The questionnaire probes into the various elements of treatment, revealing the areas in which the oncologists would need additional support and which practices would probably be outdated and need new solutions (Price et al., 2018). By collecting the responses from the oncologists and analysing the data, the main trends and patterns in chemotherapy resistance would be noted. This evidence can be used in formulating strategies that are targeted at curbing chemotherapy resistance and other novel ways of treatment. Thus, the current study is going to be the first international study that mainly aims to develop a valid and reliable assessment tool to assess the level of knowledge, attitude, and practice (KAP) of oncologists toward chemotherapy resistance.
Materials and Methods
Questionnaire development
A qualitative study involving 15 oncologists was initially conducted to investigate their knowledge, attitudes, and practices regarding chemotherapy resistance. A questionnaire in the English language was prepared based on the findings of the qualitative and literature review studies (Bahar et al., 2019; Nedeljković & Damjanović, 2019; Nuhn et al., 2019; Oh et al., 2018; Pokhriyal et al., 2019; Wang & Zhong, 2018). The first draft of the questionnaire using five Likert-scale comprised of forty-one items to assess knowledge, 14 items to evaluate attitude, and thirty-one to assess the practice of oncologists and oncology trainees regarding chemotherapy resistance.
Questionnaire validation
Ten experts from the Department of Medical Oncology at oncology Teaching Hospital Baghdad were chosen based on their research experience to evaluate the questionnaire’s face validity. They were given the questionnaire and the research’s specific objectives. The experts were asked for their feedback on the questionnaire designed to accomplish these study aims. Expert feedback on the questionnaire was accepted and included to bolster its face validity. Additionally, to improve content validity, the experts were picked based on their experience in epidemiological research in the oncology sector, as determined by their number of peer-reviewed publications. Totally approximately 10 experts were approached however only 6 accepted the invitation and reviewed the questionnaire with their knowledge. Their recommendations to remove some items and viewpoints were considered and included in the questionnaire, so helping to establish the content validity of the questionnaire.
The final version of the questionnaire contains information about the knowledge, attitude, and practice (KAPs) related to chemotherapy resistance. Knowledge, in this study, refers to the accurate knowledge and facts among the oncologist about chemotherapy resistance, whereas attitude represents the perceptions of oncologists regarding chemotherapy resistance. Practices denote the existing management and current practice that the oncologists follow when handling chemotherapy resistance cases. The final version of the questionnaire comprises four sections. Section one consists of eight questions on collecting various socio-demographic information from the oncologists; section two consists of thirty-two questions for determining the knowledge level among the oncologists about chemotherapy resistance; section three consists of thirteen items describing the attitude of oncologists about chemotherapy resistance; and section four consists of eighteen questions for evaluating the current practices of oncologists related to chemotherapy resistance cases (supplementary file 1).
Test-retest reliability
Test-retest reliability was used to determine the consistency of the test in a period of time. The questionnaire was provided to ten practicing oncologists, and after two weeks, the same questionnaire was presented to the same participants. Then, a Spearman rank correlation analysis was done to verify the questionnaire’s consistency. The correlation coefficients for each of the questionnaire’s domains, knowledge, attitude, and practice, were 0.753 (p = 0.003), 0.749 (p= 0.005) and 0.721 (p = 0.009) indicating the questionnaire had strong test-retest reliability.
Data collection
A cross-sectional study design was employed to assess oncologists’ knowledge, attitude, and practice toward chemotherapy resistance. This pilot test was conducted in Baghdad, the capital city of Iraq, in multi-oncology centers including Oncology Teaching Hospital Baghdad and Alamal National Hospital for Cancer Treatment. Specialist oncologists and oncology trainees from the chosen public and private primary health care oncology centers were recruited using the convenience sampling technique. The Ministry of Health gave its formal approval for this study on primary health care center to be carried out.
The participants for this pilot test were selected based on the following criteria: specialist oncologists and oncology trainees who are currently practicing and working in the oncology field. A total of 75 specialist oncologists and oncology trainees were invited to participate; however, 64 of them were successfully recruited as participants in this study. Participants were approached by well-trained researchers, and the study was explained to them. Interested participants were asked to answer all of the questions in the questionnaire. On average, the participants were able to complete the questionnaire within 10 min. All of the participants in the study were asked to read a cover letter describing the study objectives and the time needed to fill in the questionnaire, and the researchers received written informed consent from the participants before involving them in the research.
Data analysis
The data collected in this study were tabulated and analyzed using SPSS version 26. A scoring system was adapted and modified from a previous literature study (Persaud et al., 2021) and applied to measure the respondents’ knowledge and attitudes towards chemotherapy resistance. The chemotherapy resistance knowledge score was calculated as a continuous variable by summing the participant’s number of correct responses to 32 statements. One point was awarded for each correct response (strongly agree or agree for correct statement and strongly disagree or disagree for incorrect statement), and zero for each wrong or uncertain response, with a maximum obtainable correct score of 32 for each respondent. Correct statements in the knowledge section of the questionnaire are items 1-6, 9,11, 15-22, 24-26, and 29 while the rest of the items are incorrect statements. The knowledge score was categorized into three levels indicated low (score 0–16), moderate (score 17–26), and high (score 27–32). On the other hand, the attitude score was calculated as a continuous variable by summing the participant’s number of appropriate responses to 13 statements. One point was awarded for each appropriate response (strongly agree or agree for positive statement and strongly disagree or disagree for negative statement) and zero for each inappropriate or uncertain response, with a maximum obtainable correct score of 13 for each respondent. Positive statements in the attitude sections of the questionnaire are items 3-6, and 8-13. The attitude score was categorized into two levels indicated by negative (0–6) and positive (7–13).
Descriptive statistics such as frequency, mean, and standard deviation were used to describe participants’ characteristics. Spearman’s rank correlation was used to assess test-retest reliability, and Cronbach’s alpha was utilized to assess internal consistency for the scores on knowledge, attitude, and practice. In addition, the Mann–Whitney U-test and the Kruskal–Wallis test were used to examine any differences between participants’ knowledge, attitude, and practice scores, and demographic factors.
Results
Demographic characteristics
The respondents of the study are oncologists and oncology trainees who are already working in the medical field at different levels and departments. The mean age of participants was 36.9 ± 9.2, and the majority of them were female. The mean years of practice in the medical field were 11.39 ± 8.09, and almost half of it was spent in the oncology field (6.72 ± 4.57). Only 17% of the respondents have their Doctorate, while about half of them are Medical Doctors (50%). Of note, some of the respondents (20%) are chemotherapy oncologists and over half of them are medical oncologists. Nearly all of the oncologists (70%) have experienced chemotherapy resistance before while only 30% have not experienced it before (Table 1).
Table 1.
Characteristics of Participants (N=64)
| Characteristics | N (%) |
|---|---|
| Age (Mean ± SD = 36.92 ± 9.235) | |
| 26-35 | 37 (57.8) |
| 36-45 | 16 (25) |
| 46-55 | 6 (9.4) |
| ≥ 56 | 5 (7.8) |
| Gender | |
| Male | 30 (46.9) |
| Female | 34 (53.1) |
| Educational Level | |
| Med Bachelor | 18 (28.1) |
| Med Master | 2 (3.1) |
| Medical Doctor | 32 (50) |
| Post Doctorate | 12 (18.8) |
| Clinical Specialisation | |
| Medical oncologist | 32 (50) |
| Surgical oncologist | 5 (7.8) |
| Radiation oncologist | 12 (18.8) |
| Chemotherapy oncologist | 15 (23.4) |
| Total years in practice (Mean ± SD = 11.39 ± 8.09) | |
| 0-9 | 32 (50) |
| 10-19 | 24 (37.5) |
| ≥ 20 | 8 (12.5) |
| Years in cancer field (Mean ± SD = 6.72 ± 4.57) | |
| 0-4 | 26 (40.9) |
| 6-9 | 18 (28.1) |
| ≥ 10 | 20 (31) |
| Title of position | |
| Professor | 3 (4.7) |
| Assistant Professor | 17 (26.6) |
| Resident | 38 (59.4) |
| Fellow | 6 (9.4) |
| Experienced chemotherapy resistance cases before | |
| Yes | 45 (70) |
| No | 19 (30) |
Internal consistency and validity of the questionnaire
In order to ensure that the questionnaire is reliable and valid, it is subjected to a validity test, where a minimum Cronbach’s Alpha of 0.7 indicates that the research assessment tool is internally valid and consistent (Mallah et al., 2020) . For knowledge, attitude and practice; Table 2 indicated that the questionnaire is valid, understandable by the respondents, and therefore deemed to be fit for mass data collection. The item-total correlations of each section are presented in Supplementary file 1.
Table 2.
Cronbach's alpha Value for Awareness, Perception and Attitude Score
| Scale | No.items | Cronbach’s alpha |
|---|---|---|
| Knowledge | 32 | 0.728 |
| Attitude | 13 | 0.722 |
| Practice | 18 | 0.716 |
| Overall | 63 | 0.849 |
Knowledge, attitude and practice of oncologists toward chemotherapy resistance
Almost all of the participants indicate that they are aware what chemotherapy resistance is, its incidence among patients and how it can occur at any stage of treatment. The oncologists indicate that they have uncertainty of the various tests which should be taken prior to chemotherapy treatment and the measures which should be taken when Extreme Resistance is indicated.On the factors which cause chemotherapy resistance, the responses indicate that the majority of the oncologists are in agreement with the proposed factors, with only a small percentage disagreeing with the generally agreed causes of chemotherapy resistance. The oncologists also indicate that as the cycle of chemotherapy treatment increases; the incidence of chemotherapy also increases. Overall, the majority of the oncologists indicate low knowledge (71.9%) and the rest of them have moderate knowledge (28.1%) (Table 3).
Table 3.
Knowledge of Oncologists Toward Chemotherapy Resistance
| Items | Strongly Disagree |
Disagree | Uncertain | Agree | Strongly Agree |
|---|---|---|---|---|---|
| 1. I know what chemotherapy resistance is | 0 (0) | 1 (1.6) | 9 (14.1) | 40 (62.5) | 14 (21.8) |
| 2. I am aware that chemotherapy resistance can exist among cancer patients. | 0 (0) | 2 (3.2) | 5 (7.8) | 43 (67.2) | 14 (21.8) |
| 3. I am aware that chemotherapy resistance can happen at any stage of cancer disease | 0 (0) | 2 (3.2) | 14 (21.8) | 35 (54.7) | 13 (20.3) |
| 4. I have sufficient knowledge about how to use chemotherapy appropriately for my current practice | 0 (0) | 10 (15.7) | 14 (21.8) | 25 (39.1) | 15 (23.4) |
| 5. I am aware of the activities and lifestyle habits that should be avoided to counter chemotherapy resistance. | 2 (3.2) | 12 (18.8) | 16 (25) | 22 (34.4) | 12 (18.8) |
| 6. I have sufficient knowledge about Chemotherapy-Resistance-Test (CRT-test) |
1 (1.6) | 10 (15.6) | 25 (39.1) | 21 (32.8) | 7 (10.9) |
| 7.I used to ask for CTR-test prior to chemotherapy administration | 3 (4.8) | 20 (31.3) | 21 (32.8) | 15 (23.4) | 5 (8) |
| 8. When CTR-test result showed slight resistance (SR), this means the treatment plan most likely would not lead to an effective chemotherapy |
0 (0) | 13 (20.3) | 30 (46.9) | 18 (28.1) | 3 (4.8) |
| 9. When CTR-test result showed extreme resistance (ER), a new chemotherapy treatment should be planned |
0 (0) | 4 (6.3) | 15 (23.4) | 37 (57.8) | 8 (12.5) |
| 10. When CTR-test result showed medium resistance (MR), this means the probability of therapeutic failure is low |
0 (0) | 10 (15.6) | 36 (56.3) | 17 (26.6) | 1 (1.6) |
| 11. Chemotherapy resistance is a critical health issue worldwide | 3 (4.7) | 6 (9.4) | 16 (25) | 29 (45.3) | 10 (15.6) |
| 12. Chemotherapy resistance can be transmitted from one cancer patient to another | 20 (31.3) | 27 (42.2) | 12 (18.8) | 5 (7.8) | 0 (0) |
| 13. Every cancer patient treated with chemotherapy is at high risk of chemotherapy resistance |
3 (4.7) | 25 (39.1) | 16 (25) | 16 (25) | 4 (6.3) |
| 14. Misuse of chemotherapy can lead to chemotherapy resistance | 1 (1.6) | 14 (21.9) | 20 (31.3) | 23 (35.9) | 4 (6.3) |
| 15. Chemotherapy resistance occurs when cancer cells become resistant to chemotherapy, and they no longer work as well | 2 (3.2) | 13 (20.3) | 24 (37.5) | 24 (37.5) | 1 (1.6) |
| 16. Chemotherapy resistance occurs because of a gene-mutation happened in the cancer tissue | 2 (3.2) | 2 (3.2) | 22 (34.3) | 35 (54.7) | 3 (4.7) |
| 17. Chemotherapy resistance occurs because of cancer cells may pump the drug out of the cell as fast as it is going in using a molecule called p-glycoprotein |
0 (0) | 12 (18.8) | 37 (57.8) | 13 (20.3) | 2 (3.2) |
| 18. Chemotherapy resistance occurs because of cancer cells may stop taking in the drugs because the protein that transports the drug across the cell wall stops working |
0 (0) | 5 (7.8) | 33 (51.6) | 23 (35.9) | 3 (4.7) |
| 19. Chemotherapy resistance occurs because of the cancer cells may learn how to repair the DNA breaks caused by some anti-cancer drugs. | 0 (0) | 4 (6.3) | 35 (54.7) | 17 (26.6) | 8 (12.5) |
| 20. Chemotherapy resistance occurs because of cancer cells may develop a mechanism that inactivates the drug |
2 (3.2) | 6 (9.4) | 28 (43.8) | 24 (37.5) | 4 (6.3) |
| 21. Chemotherapy resistance occurs because of some of the cancer cells that are not killed by the chemotherapy mutate (change) and become resistant to the drug. | 0 (0) | 2 (3.2) | 17 (26.6) | 34 (53.1) | 11 (17.2) |
| 22. Delaying chemotherapy plays a major role in incidence of chemotherapy resistance. | 2 (3.2) | 15 (23.4) | 23 (35.9) | 22 (34.4) | 2 (3.2) |
| 23. Reducing chemotherapy dose plays a major role in incidence of chemotherapy resistance. |
1 (1.6) | 12 (18.8) | 25 (39.1) | 26 (40.6) | 0 (0) |
| 24. Using of mono-chemotherapy rather than combination-chemotherapy plays a major role in incidence of chemotherapy resistance | 0 (0) | 23 (35.9) | 23 (35.9) | 17 (26.6) | 1 (1.6) |
| 25. Chemotherapy resistance is associated with the use of specific types of chemotherapy | 0 (0) | 13 (20.3) | 23 (35.9) | 25 (39.1) | 3 (4.7) |
| 26. The use oradministration of multiple types of chemotherapy treatments can cause chemotherapy resistance | 1 (1.6) | 20 (39.3) | 26 (40.6) | 15 (23.4) | 2 (3.2) |
| 27. Long duration (i.e., number of cycles) of chemotherapy can cause chemotherapy resistance | 1 (1.6) | 30 (46.9) | 16 (25) | 13 (20.3) | 4 (6.3) |
| 28. High dose of chemotherapy can cause chemotherapy resistance | 2 (3.2) | 35 (54.7) | 13 (20.3) | 10 (15.6) | 4 (6.3) |
| 29. Route of chemotherapy administration can play role in incidence of chemotherapy resistance | 1 (1.6) | 29 (45.3) | 21 (32.8) | 10 (15.6) | 3 (4.7) |
| 30. Anemia plays a major role in incidence of chemotherapy resistance. | 3 (4.7) | 21 (32.8) | 24 (37.5) | 15 (23.4) | 1 (1.6) |
| 31. Hormonal factors contribute to chemotherapy resistance in breast cancer. | 0 (0) | 10 (15.6) | 21 (32.8) | 31 (48.4) | 2 (3.2) |
| 32. Age is a determinant of chemotherapy resistance. | 0 (0) | 23 (35.9) | 23 (35.9) | 17 (26.6) | 1 (1.6) |
| Knowledge level (N=64) | Low knowledge: 46 (71.9%) Moderate knowledge: 18 (28.1%) High: 0 (0%) |
||||
The questionnaire addresses the attitude of the oncologists toward chemotherapy resistance (Table 4). There is a relatively small portion of the oncologists who believe that chemotherapy resistance is the patient’s fault, while others believe that it is the oncologist’s fault. Additionally, a smaller population of the oncologists believe that if the proper steps are taken; chemotherapy resistance can be curbed. Despite the incidence of chemotherapy resistance, majority of the oncologists believe that cancer patients can still beat the disease. The oncologists perceive that the national policies are not supportive of curbing chemotherapy resistance. Overall, the majority of the oncologists (59.4%) have a positive attitude and a smaller fraction (40.6%) has a negative attitude towards chemotherapy resistance.
Table 4.
Attitude of Oncologists Toward Chemotherapy Resistance
| Items | Strongly Disagree |
Disagree | Uncertain | Agree | Strongly Agree |
|---|---|---|---|---|---|
| 1. Chemotherapy resistance is the patient's fault. | 8 (12.5) | 39 (60.9) | 11 (17.2) | 4 (6.3) | 2 (3.2) |
| 2. Chemotherapy resistance is the oncologist's fault. | 6 (9.6) | 38 (59.4) | 11 (17.2) | 5 (7.8) | 4 (6.3) |
| 3. If proper steps are taken, chemotherapy resistance can be combated. | 0 (0) | 12 (18.8) | 29 (45.3) | 18 (28.1) | 5 (7.8) |
| 4. I am confident that we can still beat cancer disease successfully after incidence of chemotherapy resistance. |
0 (0) | 3 (4.7) | 16 (25) | 41 (64.1) | 4 (6.3) |
| 5. If a patient receives proper information about the risk of chemotherapy resistance, it can be avoided |
2 (3.2) | 18 (28.1) | 21 (32.8) | 21 (32.8) | 2 (3.2) |
| 6. Oncologists should fully assess factors that cause chemotherapy resistance in patients before commencing chemotherapy treatment | 1 (1) | 2 (3.2) | 12 (18.8) | 46 (71.9) | 3 (4.7) |
| 7. I am satisfied with the current treatment guideline to treat chemotherapy resistance | 1 (1.6) | 5 (7.8) | 20 (31.3) | 32 (50) | 6 (9.4) |
| 8. Rapid and effective diagnostic techniques are required for diagnosis of chemotherapy resistance | 0 (0) | 2 (3.2) | 10 (15.6) | 51 (79.7) | 1 (1.6) |
| 9. Personalizing chemotherapy treatment will help to prevent and/or overcome chemotherapy resistance problem |
0 (0) | 11 (17.2) | 24 (37.5) | 28 (43.8) | 1 (1.6) |
| 10. National and healthcare policies are impractical against chemotherapy resistance | 0 (0) | 10 (15.6) | 37 (57.8) | 14 (21.9) | 3 (4.7) |
| 11. Some chemotherapy resistance stems from genetic factors and it cannot be rectified. | 0 (0) | 4 (6.3) | 26 (40.6) | 32 (50) | 2 (3.2) |
| 12. The patients’ coping mechanisms have a bearing on their ability to overcome drug resistance. |
0 (0) | 10 (15.6) | 35 (54.7) | 17 (26.6) | 2 (3.2) |
| 13. Chemotherapy resistance decreases the chance of survival | 0 (0) | 5 (7.8) | 15 (23.4) | 38 (59.4) | 6 (9.4) |
| Attitude level (N=64) | Negative attitude: 26 (40.6%) | ||||
| Positive attitude: 38 (59.4%) | |||||
The questionnaire addressed the various practices which the oncologists incorporate in chemotherapy treatment and their response to cases of resistance (Table 5). There is a general consensus that the chemotherapy protocols should be improved. The oncologists also indicate that they have relatively easy access to the materials which they need to give advice on chemotherapy treatment to their patients. However, slightly smaller proportions of the respondents indicate that they have adequate support for dealing with current developments in the treatment of cancer. The oncologists indicate high levels of collaboration through sharing of information and dissemination of information in the field. Through practice, the oncologists have noted that chemotherapy resistance is more common in other types of cancers than others. Due to chemotherapy resistance, some of the oncologists concur that there are alternative treatments to cancer which are just as effective as chemotherapy.
Table 5.
Practice of Oncologists Toward Chemotherapy Resistance
| Items | Strongly Disagree |
Disagree | Uncertain | Agree | Strongly Agree |
|---|---|---|---|---|---|
| 1. Chemotherapy protocols should be improved. | 1 (1.6) | 1 (1.6) | 11 (17.2) | 46 (71.9) | 5 (7.8) |
| 2. I have easy access to guidelines I need on managing chemotherapy resistance |
0 (0) | 8 (12.5) | 20 (31.3) | 36 (56.3) | 0 (0) |
| 3. I have easy access to the materials I need to give advice on prudent chemotherapy use and chemotherapy resistance |
0 (0) | 14 (21.9) | 24 (37.5) | 24 (37.5) | 2 (3.2) |
| 4. In the last 12 months, Ireceivedsufficient information about chemotherapy resistance | 3 (4.7) | 28 (43.8) | 20 (31.3) | 13 (20.3) | 0 (0) |
| 5. On the basis of information I receive, I change my practice on prescribing and/or administering of chemotherapy | 1 (1.6) | 10 (15.6) | 26 (40.6) | 25 (39.1) | 2 (3.2) |
| 6. My country has a national action plan on chemotherapy resistance | 2 (3.2) | 27 (42.2) | 22 (34.4) | 13 (20.3) | 0 (0) |
| 7. Chemotherapy resistance is very common in my practical settings | 0 (0) | 13 (20.3) | 30 (46.9) | 19 (29.7) | 2 (3.2) |
| 8. Iusually consult my colleagues about any case of chemotherapy resistance | 3 (4.7) | 6 (9.4) | 8 (12.5) | 45 (70.3) | 2 (3.2) |
| 9. When there is chemotherapy resistance, alternative treatments, which are equally effective to chemotherapy, should be used |
0 (0) | 3 (4.7) | 15 (23.4) | 39 (60.9) | 7 (10.9) |
| 10. The sharing of information with patients on how to self-monitor and self-manage during chemotherapy resistance could be improved. |
0 (0) | 5 (7.8) | 15 (23.4) | 39 (60.9) | 5 (7.8) |
| 11. I treat a patient with chemotherapy resistance similarly to those who do not have chemotherapy resistance |
4 (6.3) | 39 (60.9) | 14 (21.9) | 7 (10.9) | 0 (0) |
| 12. Incidence of chemotherapy resistance is more common in specific types of cancers than others. |
0 (0) | 9 (14.1) | 13 (20.3) | 39 (60.9) | 3 (4.7) |
| 13. Cross-resistance in chemotherapy can be detected and rectified in patients. | 3 (4.7) | 2 (3.2) | 41 (64.1) | 8 (12.5) | 0 (0) |
| 14. Chemotherapy should be stopped immediately when it shows no signs of efficacy. | 2 (3.2) | 6 (9.6) | 19 (29.7) | 33 (51.6) | 4 (26.4) |
| 15. Physicians, nurses, and healthcare personnel should be trained in detecting chemotherapy resistance. |
0 (0) | 4 (6.3) | 7 (10.9) | 40 (62.5) | 13 (20.3) |
| 16. Oncologists should clearly explain to their patients about the consequences of chemotherapy resistance |
1 (1.6) | 3 (4.7) | 2 (3.2) | 48 (75) | 10 (15.6) |
| 17. Therapeutic privilege among oncologists should be revised to allow more transparency. | 1 (1.6) | 2 (3.2) | 12 (18.8) | 38 (59.4) | 11 (17.2) |
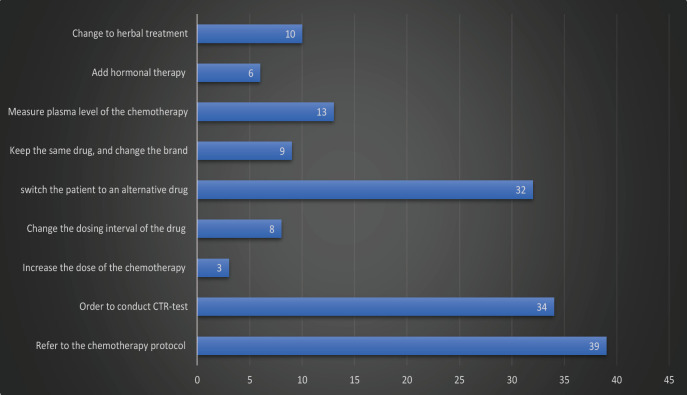
Moreover, when the participants were asked about their intervention plan to deal with chemotherapy resistance case, the majority of them indicated that they would refer back to the local chemotherapy protocol regarding chemotherapy resistance, order to conduct chemotherapy resistance (CTR) test, and switch the patient to an alternative drug, respectively (Figure 1).
Figure 1.
Oncologist Intervention with Chemotherapy Resistance Cases
Association between the demographic characteristics and knowledge and attitude score
Statistical tests showed that age and gender do not have an association with the knowledge and attitude score of the participants. However, the participants’ education level and previous experience with chemotherapy cases have a statistically significant effect on the participant’s knowledge score (p<0.05), yet it does not affect the attitude score. Table 6 also reported that the mean score of knowledge significantly increases as the number of years in the medical field, particularly in the oncology field, increases (p<0.05).
Table 6.
Differences between Knowledge and Attitude Score with Participants’ Demographic Characteristics
| Characteristic | Knowledge score Mean | P | Attitude score Mean | P |
|---|---|---|---|---|
| Gender | 0.969 | |||
| Male | 14.4 | 6.9 | 0.579 | |
| Female | 14.5 | 6.5 | ||
| Age | 0.075 | |||
| 26-35 | 13.5 | 6.2 | 0.229 | |
| 36-45 | 14.8 | 7.3 | ||
| 46-55 | 17 | 7.6 | ||
| ≥ 56 | 17.4 | 7.8 | ||
| Educational Level | 0.029* | 0.293 | ||
| Med Bachelor | 12.1 | 5.9 | ||
| Med Master | 13.5 | 5.5 | ||
| Medical Doctor | 15.1 | 7 | ||
| Post Doctorate | 16.3 | 7.4 | ||
| Clinical Specialisation | 0.077 | 0.607 | ||
| Medical oncologist | 15.3 | 7 | ||
| Surgical oncologist | 16.2 | 7.2 | ||
| Radiation oncologist | 12 | 5.9 | ||
| Chemotherapy oncologist | 13 | 6.7 | ||
| Years in practice (Mean ± SD = 11.39 ± 8.09) | 0.02* | 0.51 | ||
| 0-9 | 13.1 | 6.4 | ||
| 10-19 | 15.4 | 6.9 | ||
| ≥ 20 | 17 | 7.5 | ||
| Years in cancer (Mean ± SD = 6.72 ± 4.57) | 0.035* | 0.086 | ||
| 0-4 | 12.9 | 6.2 | ||
| 6-9 | 14.6 | 6.3 | ||
| ≥ 10 | 16.2 | 7.8 | ||
| Title of position | 0.356 | 0.418 | ||
| Professor | 16.3 | 7 | ||
| Assistant Professor | 15.1 | 7.1 | ||
| Resident | 13.7 | 6.3 | ||
| Fellow | 16.1 | 8 | ||
| Experienced chemotherapy resistance cases before | 0.015* | 0.307 | ||
| Yes | 15.2 | 6.9 | ||
| No | 12.4 | 6.3 |
*statistically significant (p<0.05)
Discussion
The questionnaire developed in this study has been proven to be a valid and reliable research assessment tool. Cumulatively, the questionnaire has 63 questions, with 32 questions on knowledge, 13 questions on attitude, and 18 questions of practice of chemotherapy resistance. To the best of the researcher’s knowledge, this kind of questionnaire is the first international tool ever to be developed in the field of chemotherapy resistance aiming to explore the level of the knowledge, attitude, and practice of oncologists regarding chemotherapy resistance. The study probes into the various perceptions that the oncologists might have towards chemotherapy resistance; ranging from general questions which pertain to general information to specific questions which pertain to the medical practice of cancer treatment. Based on Cronbach’s Alpha, the questionnaire is considered valid and internally consistent. It is reliable as a tool for mass data collection; thus, it can be used as a basis for future studies.
The majority of the respondents are between 26 and 35 years, with less than 9 years of experience in the medical field and up to 4 years in the cancer field. This indicates that most of the respondents are still in the early days of working in the medical field, thus some of their responses would be due to their limited exposure. The respondents have advanced their education as medical doctors, with some of them advancing to doctoral studies. This suggests that for oncologists to be well equipped in dealing with chemotherapy resistance it is essential for them to be advancing their education and improving their knowledge of their field (Chen et al., 2017). Despite their less number of years in the field, the majority of the respondents have experienced a chemotherapy case before, which might suggest the high rate of incidence in chemotherapy resistance. Chemotherapy resistance is a common phenomenon in the medical field, with up to 90% of chemotherapy treatments failing (Kischel et al., 2019). This alarming rate of failure in chemotherapy indicates the need to probe further into how chemotherapy can be improved to lead to higher success rates. It calls for continuous research and development; with collaboration from the oncologists currently in practice contributing through their skill and experience (Lohitesh et al., 2018).
The participants indicate a high level of awareness of what chemotherapy resistance is, however, they also indicate lower levels of the intricacies of chemotherapy resistance. The oncologists acknowledge that once a patient has cancer, they also have a chance of having chemotherapy resistance during treatment. Based on their own perspective, the participants believe that they have sufficient information which can help them in practice for specifically in chemotherapy treatments. However, this is contrasted to the responses of the participants to questions on the actual knowledge which they possess on chemotherapy treatments. The respondents indicate that they have low knowledge of the tests which should be run prior to beginning chemotherapy treatment, and the steps which should be taken once the patients indicate extreme resistance (ER). Therefore, the questionnaire exposes the disparity between the perceived skills and the actual skills which the respondents possess. This is a common concern in the medical field because it compromises the overall performance of the personnel and impedes their capacity to successfully perform the chemotherapy treatment (Bukowski et al., 2020). Ideally, the skills and knowledge which the medical personnel perceive they possess should be symmetrical to increase the success of chemotherapy treatments (Choudhury et al., 2019).
The knowledge which oncologists have on the chemotherapy-resistance-test (CRT-test) which should be taken prior to chemotherapy treatment is essential. This knowledge is valuable, because it helps the oncologists in formulating the best possible treatment protocol for the patients. More importantly, the interpretation of the results of the CTR is crucial as it would guide the oncologist on the best course of action given the particular patients circumstances (Van der Jeught et al., 2018). However, the responses from this study show that the participants are mostly uncertain of how to handle the next step of treatment when the patient’s results have shown extreme resistance to chemotherapy. Overall, the oncologists show low to moderate levels of knowledge on chemotherapy resistance. This is alarming and calls for corrective action as it can be inferred that they would be contributors to chemotherapy resistance and failure. Therefore, this brings attention to the role of oncologists in formulating the best treatment protocol for cancer patients. Based on the findings of this study, it could be inferred that chemotherapy resistance could be triggered by inadequate protocol preparation after CTR has been conducted. This is consistent with the findings of Liegise et al., (2022) which place part of chemotherapy failure on the inadequate preparation of treatment protocols by oncologists (Liegise et al., 2022; Nathanson et al., 2014).
From the findings of this study, it is noted that there are varied reasons which oncologists believe to be the cause of chemotherapy resistance. This study specifically probes into the elements of chemotherapy itself which lead to chemotherapy resistance. For example, the participants indicate that improper administration of chemotherapy, its prolonged use and either delaying or reducing the dosage can lead to chemotherapy would increase the incidence of chemotherapy resistance. This suggests that there is need for reform in the methods in which this treatment is administered, and the potential inclusion of alternative treatments which would ensure the efficacy of the treatment (Abotaleb et al., 2018). This is consistent with the findings of Islam (2018) which asserts that for chemotherapy treatment to be fully effective it can be incorporated with other holistic treatments (Islam, 2018). Holistic treatments for the treatment of cancer have been explored for a while but this has yielded divergent views. Some oncologists believe that it can be effectively included in the treatment of cancer to curb chemotherapy resistance, while others assert that the deviation from chemotherapy to include other forms of treatments is a driver for chemotherapy resistance (Mashouri et al., 2019; Si et al., 2019).
The attitude of the oncologists towards chemotherapy resistance is also significant as it forms the basis upon which they administer the treatment. There are oncologists, though few, which indicate that chemotherapy resistance is the patient’s fault. While it might be true that some of the patient’s lifestyle habits, adherence to treatment and coping mechanisms result in the cancer drugs losing their efficacy; it should not be accounted to the patient per se as they would be in a distressed state. The relationship between the patients and the oncologists should be more collaborative rather than competitive, thus oncologists would need to be more empathetic towards the patients (Settleman, 2016). However, the present study also finds that the majority of the oncologists are positive that there will be solutions to curb chemotherapy resistance and despite its occurrence; the patients can still fully recover and beat cancer. Therefore, the positive attitude is indicative that there would be ongoing studies and trials targeted at identifying how chemotherapy resistance can be accurately detected and prevented in the patients.
From present study, the attitudes of the oncologists towards treatment are mainly driven by the amount of knowledge which is shared among the patients and among the oncologists. This suggests that there is need for review on how information is shared with the patients; calling for comprehensive education on the treatment which they will get its adverse side effects and the recommended coping mechanisms which lead to successful chemotherapy.
Additionally, the current study probes into the instances where chemotherapy resistance can be avoided. Chemotherapy resistance can be avoided when the patient’s lifestyle is assessed, and the risk factors are eliminated. While this does not guarantee the efficacy of chemotherapy, it eliminates the foreseeable circumstances which might result in the incidents of drug resistance among patients. However, this is equally impacted by the factors which cause chemotherapy resistance which are beyond the scope of the patient’s lifestyle. For example, the incidents where the cancer cells mutate; replicate exponentially or repair themselves from the effect of the anticancer drugs (Nathanson et al., 2014). Therefore, with this view in mind it is essential to note that chemotherapy resistance is to be curbed using various strategies to look out for both the foreseeable and non-foreseeable factors which trigger drug resistance, as noted in a previous literature study (Junttila & De Sauvage, 2013).
In terms of the practice, there is a general consensus among the oncologists that there should be amendments to the protocols of chemotherapy treatment. This is reasonable, given the high rate of chemotherapy resistance and failure. From current study, it is noted that there is need for progressive information to be shred on developments in chemotherapy. National policy should also be accommodative of the improvements in the treatment of cancer, to ensure that the oncologists are provided with the tools and resources to improve their practice. The nurses and doctors should be trained on rigorous methods of detecting chemotherapy resistance, and detection tools should be availed with top priority in a bid to reduce the fatality of cancer (Nishikimi et al., 2020).
Additionally, the questionnaire formulated in this study probes into the issue of oncologists being transparent with their patients on the progress of their chemotherapy treatment. However, this could be deemed controversial, as it might be stated that the lack of transparency is for the benefit of the patient. When the patient is informed of the full scope of their illness, they would probably be disheartened and further derail the course of chemotherapy. On the other hand, being transparent with the patient on the state of their health can result in the patient making improved lifestyle choices and being more cautious with drug adherence to help in curbing chemotherapy resistance. This issue of transparency with chemotherapy patients remains an inconclusive area. Therefore, it can be noted that oncologists still have several areas in their practice where they need improvement and reform for them to be able to have higher rates of success in chemotherapy and reduce the incidence of chemotherapy resistance.
Limitation and future studies
This study has some limitations. The sample size was small as the main objective of this study was to develop and confirm the validity and reliability of the developed assessment tool. Thus, findings should be generalised with caution and larger sample is required in the future studies. Besides that, the participants were only oncologists and oncology trainees so that future studies might consider to include other healthcare professionals in the oncology field such as nurses and oncology pharmacists.
In conclusion, this study has enabled the formulation of a questionnaire that can be used to measure the interaction of oncologists and chemotherapy. This tool would be useful in incidents where there is a need to revisit the chemotherapy resistance strategies, with the focus on the role of oncologists in the treatment process. It is essential for such a tool to be availed to oncologists in clinical practice so that the healthcare management can identify their staff’s current knowledge and attitudes and identify how they can be amended. Continuous research is underway on how strategies can be formulated to curb chemotherapy resistance. The role of oncologists is of paramount importance since they are in close proximity to patients, and they would be able to monitor how several patients respond to treatment and how future incidents of drug resistance can be curbed. Therefore, chemotherapy resistance is an ongoing research area where the methods of treatment are being continuously treated.
Author Contribution Statement
BARH and AHM did the conception and design of the study, acquisition of data, analysis and interpretation of the data, drafting the manuscript and revising the manuscript critically for important intellectual content; AMW,AZAA, AAA, and MKA were involved in data collection and checked the content of the developed questionnaire; AS helped in keying in the data for data analysis.
Acknowledgments
Funding
The authors declare that there is no funding for this study.
Ethics approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Research Ethics Committee of Ministry of Health in Iraq granted the ethical approval for this study (EC-6833).
Availability of data and Material
Data and other materials are available upon request from the corresponding author.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Abotaleb M, Kubatka P, Caprnda M, et al. Chemotherapeutic agents for the treatment of metastatic breast cancer: An update. Biomed Pharmacother. 2018;101:458–77. doi: 10.1016/j.biopha.2018.02.108. [DOI] [PubMed] [Google Scholar]
- Bahar E, Kim J-Y, Yoon H. Chemotherapy resistance explained through endoplasmic reticulum stress-dependent signaling. Cancers. 2019;11:338–58. doi: 10.3390/cancers11030338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukowski K, Kciuk M, Kontek R. Mechanisms of multidrug resistance in cancer chemotherapy. Int J Mol Sci. 2020;21:3233–57. doi: 10.3390/ijms21093233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen D, Liu D, Chen Z. Potential therapeutic implications of miRNAs in osteosarcoma chemotherapy. Tumor Biol. 2017:39. doi: 10.1177/1010428317705762. [DOI] [PubMed] [Google Scholar]
- Choudhury H, Pandey M, Yin T H, et al. Rising horizon in circumventing multidrug resistance in chemotherapy with nanotechnology. Mater Sci Eng C. 2019;101:596–613. doi: 10.1016/j.msec.2019.04.005. [DOI] [PubMed] [Google Scholar]
- Christie E, Bowtell D. Acquired chemotherapy resistance in ovarian cancer. Annal Oncol. 2017;28:13–5. doi: 10.1093/annonc/mdx446. [DOI] [PubMed] [Google Scholar]
- Islam MS. Treat patient, not just the disease: holistic needs assessment for haematological cancer patients. Oncol Rev. 2018:12. doi: 10.4081/oncol.2018.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junttila MR, De Sauvage FJ. Influence of tumour micro-environment heterogeneity on therapeutic response. Nature. 2013;501:346–54. doi: 10.1038/nature12626. [DOI] [PubMed] [Google Scholar]
- Kalal BS, Upadhya D, Pai VR. Chemotherapy resistance mechanisms in advanced skin cancer. Oncol Rev. 2017:11. doi: 10.4081/oncol.2017.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim E S. Chemotherapy resistance in lung cancer. Lung Cancer Personalized Med. 2016;2016:189–09. doi: 10.1007/978-3-319-24223-1_10. [DOI] [PubMed] [Google Scholar]
- Kischel P, Girault A, Rodat-Despoix L, et al. Ion channels: New actors playing in chemotherapeutic resistance. Cancers. 2019;11:376. doi: 10.3390/cancers11030376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liegise H, Barmon D, Baruah U, et al. Reason for improper simple hysterectomy in invasive cervical cancer in Northeast India. J Can Res Ther. 2022;17:241–68. doi: 10.4103/jcrt.JCRT_1005_20. [DOI] [PubMed] [Google Scholar]
- Lim Z-F, Ma PC. Emerging insights of tumor heterogeneity and drug resistance mechanisms in lung cancer targeted therapy. J Hematol. Oncol. 2019;12:1–18. doi: 10.1186/s13045-019-0818-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohitesh K, Chowdhury R, Mukherjee S. Resistance a major hindrance to chemotherapy in hepatocellular carcinoma: an insight. Cancer Cell Int. 2018;18:1–15. doi: 10.1186/s12935-018-0538-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallah N, Rodriguez-Cano R, Figueiras A, Takkouche B. Design, reliability and construct validity of a knowledge, attitude and practice questionnaire on personal use of antibiotics in Spain. Sci Rep. 2020;10:1–10. doi: 10.1038/s41598-020-77769-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mashouri L, Yousefi H, Aref AR, Molaei F, Alahari SK. Exosomes: composition, biogenesis, and mechanisms in cancer metastasis and drug resistance. Mol Cancer. 2019;18:1–14. doi: 10.1186/s12943-019-0991-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathanson D A, Gini B, Mottahedeh J, et al. Targeted therapy resistance mediated by dynamic regulation of extrachromosomal mutant EGFR DNA. Science. 2014;343:72–6. doi: 10.1126/science.1241328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nedeljković M, Damjanović A. Mechanisms of chemotherapy resistance in triple-negative breast cancer—how we can rise to the challenge. Cells. 2019;8:957. doi: 10.3390/cells8090957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaou M, Pavlopoulou A, Georgakilas AG, Kyrodimos E. The challenge of drug resistance in cancer treatment: a current overview. Clin Exp Metastasis. 2018;35:309–18. doi: 10.1007/s10585-018-9903-0. [DOI] [PubMed] [Google Scholar]
- Nishikimi K, Tate S, Kato K, Matsuoka A, Shozu M. Well-trained gynecologic oncologists can perform bowel resection and upper abdominal surgery safely. J Gynecol Oncol. 2020:31. doi: 10.3802/jgo.2020.31.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuhn P, De Bono J S, Fizazi K, et al. Update on systemic prostate cancer therapies: management of metastatic castration-resistant prostate cancer in the era of precision oncology. Eur Urol. 2019;75:88–99. doi: 10.1016/j.eururo.2018.03.028. [DOI] [PubMed] [Google Scholar]
- Oh W K, Cheng W Y, Miao R, et al. Real-world outcomes in patients with metastatic castration-resistant prostate cancer receiving second-line chemotherapy versus an alternative androgen receptor-targeted agent (ARTA) following early progression on a first-line ARTA in a US community oncology setting. Urol Oncol Semin ORI. 2018;36:501–9. doi: 10.1016/j.urolonc.2018.08.002. [DOI] [PubMed] [Google Scholar]
- Persaud S, Sukhraj R, Goetz L. Knowledge, attitude and practices towards antibiotic use among patients at a tertiary urology centre in trinidad and Tobago. Caribb Med J. 2021:83. [Google Scholar]
- Phi L TH, Sari IN, Yang Y-G, et al. Cancer stem cells (CSCs) in drug resistance and their therapeutic implications in cancer treatment. Stem Cells Int. 2018;2018:1–16. doi: 10.1155/2018/5416923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokhriyal R, Hariprasad R, Kumar L, Hariprasad G. Chemotherapy resistance in advanced ovarian cancer patients. Biomark Cancer. 2019:11. doi: 10.1177/1179299X19860815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price L, Gozdzielewska L, Young M, et al. Effectiveness of interventions to improve the public’s antimicrobial resistance awareness and behaviours associated with prudent use of antimicrobials: a systematic review. J Antimicrob Chemother. 2018;73:1464–78. doi: 10.1093/jac/dky076. [DOI] [PubMed] [Google Scholar]
- Settleman J. Bet on drug resistance. Nature. 2016;529:289–90. doi: 10.1038/nature16863. [DOI] [PubMed] [Google Scholar]
- Si W, Shen J, Zheng H, Fan W. The role and mechanisms of action of microRNAs in cancer drug resistance. Clin Epigenetics. 2019;11:1–24. doi: 10.1186/s13148-018-0587-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Jeught K, Xu H-C, Li Y-J, Lu X-B, Ji G. Drug resistance and new therapies in colorectal cancer. World J Gastroenterol. 2018;24:3834. doi: 10.3748/wjg.v24.i34.3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasan N, Baselga J, Hyman DM. A view on drug resistance in cancer. Nature. 2019;575:299–09. doi: 10.1038/s41586-019-1730-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang A, Zhong H. Roles of the bone marrow niche in hematopoiesis, leukemogenesis, and chemotherapy resistance in acute myeloid leukemia. Hematol. 2018;23:729–39. doi: 10.1080/10245332.2018.1486064. [DOI] [PubMed] [Google Scholar]
- Wang X, Zhang H, Chen X. Drug resistance and combating drug resistance in cancer. Cancer Drug Resist. 2019;2:141. doi: 10.20517/cdr.2019.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data and other materials are available upon request from the corresponding author.