Sir,
India was abruptly affected during the second wave of Coronavirus Disease (COVID-19) and dramatically several different oral lesions were observed in these patients. In March and April 2021, a total of 120 COVID-positive patients reported to us through teleconsultation for different oral symptoms. Out of 120 patients, 71 patients were in the age group of 41 to 80 years, while 49 patients were between 20 and 40 years. A thorough video consultation was done and all the patients were provided pharmacological treatment for their oral lesions. All the results were carefully evaluated and statistically analyzed.
We observed that out of 120 patients, 21 patients were hospitalized and were under oxygen support, while the remaining 99 patients were home isolated. All patients were tested positive for COVID-19 and most of them were on medicinal treatment. All 120 patients were suffering from stress and high-grade anxiety.
On examination, candidiasis alone (26.7%) or with fissured tongue (10%) was the most common oral lesion observed followed by herpes labialis (16.7%), aphthous stomatitis (14.2%), oral mucositis (13.3%), atrophy of tongue papillae (10.8%), erosive lichen planus (5.8%) and Herpes Zoster infection (2.5%). Candidiasis, erosive lichen planus and herpes zoster infection were more in patients who were above 40 years of age, whereas herpes labialis, aphthous stomatitis and oral mucositis were more common among patients who were less than 40 years of age (x2 = 52.129; df = 7; P < 0.001; Highly significant) [Table 1, Figure 1].
Table 1.
Prevalence of oral lesions according to type and age
| Type of oral lesion | Age <=40 yrs | Age >40 yrs | Total | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | % | n | % | n | % | |
| Aphthous Stomatitis | 16 | 32.7 | 1 | 1.4 | 17 | 14.2 |
| Atrophy of tongue papillae | 2 | 4.1 | 11 | 15.5 | 13 | 10.8 |
| Candidiasis on tongue | 3 | 6.1 | 29 | 40.8 | 32 | 26.7 |
| Candidiasis with fissured tongue | 2 | 4.1 | 10 | 14.1 | 12 | 10.0 |
| Erosive lichen planus | 2 | 4.1 | 5 | 7.0 | 7 | 5.8 |
| Herpes labialis | 14 | 28.6 | 6 | 8.5 | 20 | 16.7 |
| Herpes zoster | - | - | 3 | 4.2 | 3 | 2.5 |
| Mucositis | 10 | 20.4 | 6 | 8.5 | 16 | 13.3 |
| Total | 49 | 100.0 | 71 | 100.0 | 120 | 100.0 |
x2=52.129; df=7; P<0.001; Highly significant
Figure 1.
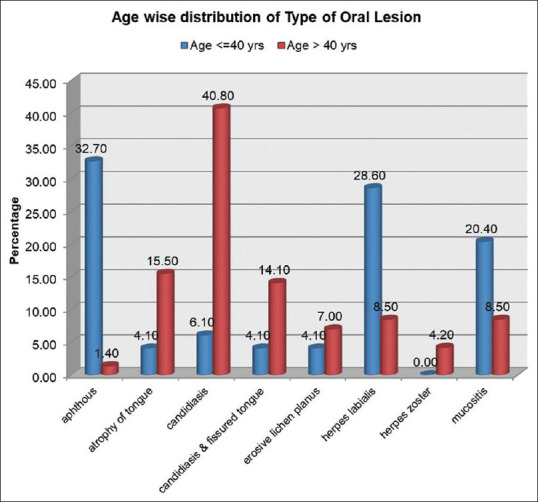
Showing the prevalence of oral lesions according to type and age
Tongue lesions were in the form of candidiasis, fissures and atrophy of papillae, while buccal mucosa involvement was more in patients with aphthous stomatitis, oral mucositis and erosive lichen planus. Lip involvement was mainly due to herpes labialis. Two patients with Herpes zoster had unilateral intraoral lesions on the palate while one patient had right-side face involvement (x2 = 28.017; df = 5; P < 0.001; Highly significant) [Table 2, Figure 2].
Table 2.
Showing the commonly involved intraoral and facial sites
| Site | Age <=40 yrs | Age >40 yrs | Total | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | % | n | % | n | % | |
| Buccal mucosa | 18 | 36.7 | 8 | 11.3 | 26 | 21.7 |
| Lips | 14 | 28.6 | 6 | 8.5 | 20 | 16.7 |
| Face | - | - | 1 | 1.4 | 1 | 0.8 |
| Gingiva | - | - | 3 | 4.2 | 3 | 2.5 |
| Palate | - | - | 6 | 8.5 | 6 | 5.0 |
| Tongue | 17 | 34.7 | 47 | 66.2 | 64 | 53.3 |
| Total | 49 | 100.0 | 71 | 100.0 | 120 | 100.0 |
x2=28.017; df=5; P<0.001; Highly significant
Figure 2.
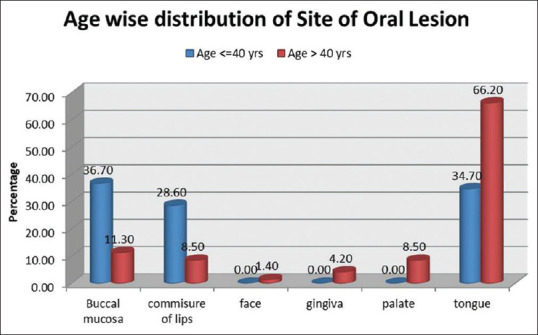
Showing the commonly involved intraoral and facial sites
There is a low certainty of evidence regarding oral mucosal lesions in patients with COVID-19 and their etiopathogenesis. The multiple clinical aspects suggest co-infections, immunity impairment, and adverse reactions rather than a genuine oral mucosal infection primarily caused by SARS-CoV-2. Therefore, the range of COVID-19 manifestations in the oral cavity has a broad and current interest.
The “COVID tongue” term was recently highlighted in literature for white appearing tongue and emphasised as one of the most common oral manifestations.[1] We suggest that in the initial stages of the disease, tongue appears coated, while as the disease progresses, superadded candida infection occurs making the tongue creamy white [Figure 3]. Candidal involvement was more common in older age groups as seen in the present study and hospitalized patients.
Figure 3.

Showing candidiasis on the tongue
COVID patients already have compromised immunity and the presence of comorbidities, stress and anxiety lead to further immune suppression resulting in reactivation of Herpes Simplex Virus 1 or Herpes Zoster virus [Figure 4], as seen in our study. The development of anxiety and stress associated with this pandemic disease triggers the formation of aphthous stomatitis and Lichen planus in patients with a strong autoimmune component.
Figure 4.

Showing intraoral Herpes Zoster infection on the palate
Other miscellaneous oral manifestations mentioned in the literature include the presence of petechiae, diffuse ulcers as seen in erythema multiforme, geographic tongue, irregular macules, increased melanin pigmentation and angina bullosa-like lesions.[1,2,3,4,5] Opportunistic fungal infection, mucormycosis, was later added to the list taxing the lives of the COVID-19 patients.
Awareness of the various oral lesions in COVID-19 is important as these may be the only sign in asymptomatic patients. To the best of our knowledge, this is one of the first studies in India highlighting oral lesions in COVID patients in a large population sample.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Corchuelo J, Ulloa FC. Oral manifestations in a patient with a history of asymptomatic COVID-19: Case report. Int J Infect Dis. 2020;100:154–7. doi: 10.1016/j.ijid.2020.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh G, Priya H, Mishra D, Kumar H, Monga N, Kumari K. Oral manifestations and dental practice recommendations during COVID-19 pandemic. J Family Med Prim Care. 2021;10:102–9. doi: 10.4103/jfmpc.jfmpc_1605_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iranmanesh B, Khalili M, Amiri R, Zartab H, Aflatoonian M. Oral manifestations of COVID-19 disease: A review article. Dermatol Ther. 2020;31:e14578. doi: 10.1111/dth.14578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dos Santos JA, Normando AGC, Da Silva RLC, Acevedo AC, De Luca Canto G, Sugaya N, et al. Oral manifestations in patients with COVID-19: A living systematic review. J Dent Res. 2021;100:141–54. doi: 10.1177/0022034520957289. [DOI] [PubMed] [Google Scholar]
- 5.Finsterer J, Stollberger C. Causes of hypogeusia/hyposmia in SARSCoV2 infected patients. J Med Virol. 2020;92:1793–4. doi: 10.1002/jmv.25903. [DOI] [PMC free article] [PubMed] [Google Scholar]


