Sir,
Herpes zoster (HZ) is a common disease caused by reactivation of varicella-zoster virus (VZV).[1] Besides the classical vesicular rash on the skin, VZV is known to cause extra-cutaneous manifestations, including vasculopathy of different sized vessels.[2,3] VZV vasculopathy is a well-recognised entity in central nervous system (CNS); however, only few data have been published on cutaneous small-vessel vasculitis (CSVV) in HZ. Herein, we present a case of HZ with CSVV and a review of the literature.
A 53-year-old woman with a history of acute myeloid leukaemia and allogeneic stem cell transplantation was admitted to our department with complaints of painful lesions in left gluteal region and upper leg for 2 days. On examination, purpuric papules/plaques with central necrohaemorrhagic crusts were seen in dermatomal distribution [Figure 1]. Punch biopsy showed intraepidermal bulla with viral nuclear inclusions and giant cell formations, as well as perivascular mononuclear inflammation, leukocytoclasia and fibrinoid necrosis around superficial dermal capillaries [Figure 2]. To exclude the presence of herpes simplex virus (HSV), an immunohistochemical staining for HSV and plasma HSV-1/HSV-2 PCR were performed and resulted in negative. After routine laboratory screenings, systemic involvement of vasculitis was excluded. Based on these findings, the patient was diagnosed with HZ with CSVV. She was started on valacyclovir 3 × 1000 mg/day and analgesics. After 7 days, complete resolution of the cutaneous lesions was observed without sequelae and no additional systemic therapy was required for CSVV. She did not develop postherpetic neuralgia (PHN) or vasculopathy of CNS during 2 months of follow-up.
Figure 1.

Purpuric papules and plaques on an erythematous base with occasional central black haemorrhagic and necrotic crusts on (a) left gluteal region and (b) left upper leg
Figure 2.
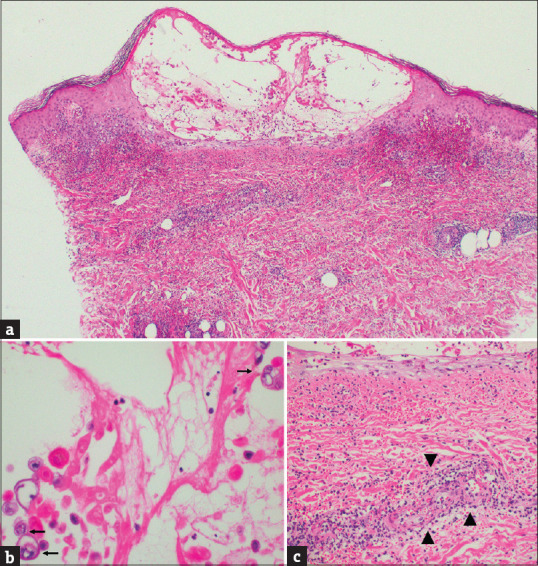
Skin biopsy, haematoxylin-eosin stain, (a) intraepidermal bulla formation, erythrocyte extravasation and perivascular inflammation in the superficial dermis (×40 original magnification), (b) viral nuclear inclusions and giant cell formations in the cells within the bulla (arrows) (×400 original magnification) and (c) superficial dermal vessel with leukocytoclastic vasculitis (arrows) (×200 original magnification)
Vascular changes associated with VZV are vessel wall thickening, stenosis and inflammatory infiltrate with abundant neutrophils. VZV is suggested to spread transaxonally from neural ganglia to vessel walls.[4] It can infect endothelial cells directly from adjacent nerves and cause vascular damage including microthrombi formation and haemorrhage.[3,5] In 1984, Cohen and Trapuckd[6] described the first case of CSVV associated with HZ. After a detailed literature review, we found 10 published cases.[6,7,8,9,10,11,12,13,14,15] Clinicopathological features of present and reported cases are summarised in Table 1. The mean age was 57.18 ± 17.74 years, which can be explained by the fact that advanced age is a major risk factor for HZ.[1] Most cases, including ours, were immunocompromised individuals. Cutaneous findings were characterised by vesicles, palpable purpura and ulcerated nodules/plaques. The lesions were mostly on the lower extremities. Histopathological findings included intraepidermal blisters, multinucleated giant cells and leukocytoclastic vasculitis. In most cases, complete recovery was achieved with anti-viral agents and no patient required further systemic therapy for CSVV. It is estimated that PHN occurs in 5%–20% of patients with HZ; the absence of postherpetic neuralgia (PHN) in our patient can be explained by early treatment with valacyclovir.[16]
Table 1.
Clinical and histopathological features of the present and reported cases in the literature
| Authors, year of publication | Age | Sex | Comorbidities | Clinical presentation | Localisation | Histopathology | Immunohistochemistry, PCR or viral culture for VZV | Therapy/Outcome |
|---|---|---|---|---|---|---|---|---|
| Cohen et al., 1984[6] | 67 | M | Valvular heart disease, abdominal aortic aneurysm, streptococcal endocarditis and petechial rash treated with prednisone | Haemorrhagic vesicles | Right hypothenar eminence, face, abdomen, right hip and buttock | Intraepidermal vesiculation with ballooning and reticular degeneration, multinucleated giant epithelial cells, eosinophilic intranuclear inclusions and leukocytoclastic vasculitis of dermal venules | Viral culture for VZV was positive | Spontaneous resolution |
| Erhard et al., 1995[7] | 62 | M | Mycosis fungoides under methotrexate 17.5 mg twice a week | Sharply demarcated, indurated erythematous nodules and confluent necrotic plaques with central, shallow ulcerations | Right cheek and medial chin | Dermal necrosis surrounded by a perivascular and periadnexal lymphohistiocytic infiltrate, severe obliterative vasculitis of the dermal vessels, nuclear inclusion bodies of Cowdry type A in endothelial cells without ballooning degeneration, giant cells, and vesicles in the epidermis. | Viral culture for VZV was positive and VZV-specific IgG was detected in low titre by indirect immunofluorescence | Systemic acyclovir/Healing with moderate scarring |
| Uhoda et al., 2000[8] | 22 | M | Primary mediastinal large B cell lymphoma under cyclophosphamide, vincristine, doxorubicin, prednisone, bleomycin and methotrexate | Reddish nodules | Right axilla and right hand | Superficial and deep perivascular lymphoid infiltrate, swollen endothelial cells and dense nuclear chromatin, red blood cell extravasation without epidermal alterations mediated by viruses | Immunochemical stains for VZV were positive. | Iv acyclovir/Complete resolution |
| Wollina and Schönlebe, 2012[9] | 58 | M | Pulmonary sarcoidosis under prednisolone 7.5 mg/day | Initially palpable purpura and later on typical grouped vesicles of herpes zoster | Right upper and lower leg | Intraepithelial vesiculation with acantholysis and formation of ghost cells, lympho- monocytic perivascular infiltrate with leukocytoclasia in dermis | VZV-specific IgG was detected in low titre by direct immunofluorescence | Oral brivudine/Complete resolution |
| Wong et al., 2013[10] | 57 | M | Ulcerative colitis under methylprednisolone 80 mg/day mesalamine 2400 mg/day | Purpuric rash | Left lower trunk and left lower extremity | Focal epidermal erosions with acantholytic squamous cells, multinucleation, nuclear molding and chromatin margination along with lymphocytic vasculitis with red blood cell extravasation, endothelial cell swelling and frequent nuclear dust in the dermal venules | NA | Iv acyclovir/gradual improvement over 2 weeks |
| Tanaka et al., 2014[11] | 72 | M | Rheumatoid arthritis under methotrexate 8 mg/week, prednisolone 5 mg/day and bucillamine 200 mg/day | Ulcer with surrounding small erythematous, bullous lesions and scattered necrosis | Left fifth toe and the dorsum of the left foot | Leukocytoclastic vasculitis with fibrinoid degeneration in the reticular dermis and subcutaneous tissue without the epidermal involvement typical of VZV | Immunochemical stains for VZV were positive. | Iv acyclovir/Significant improvement |
| Burgard et al., 2018[12] | 72 | M | Not mentioned/immunocompetent patient | Multiple patchy lesions, orange-red in colour with dusky foci and a peripheral rim of pallor | Left upper leg | Dense perivascular and patchy lichenoid infiltrate with extravasated erythrocytes, leukocytoclasia and papillary oedema without the epidermis changes, acantholysis or ghost cells | Swab VZV PCR and immunochemical stains for VZV were positive. | NA |
| Clark et al., 2018[13] | 66 | M | Hypertension, chronic kidney disease and multisystem sarcoidosis under methotrexate 15 mg/week and prednisolone 5–40 mg/day | Multiple well- demarcated 1–3 cm ulcers with multiple scattered violaceous papules | Left lower leg | Epidermal necrosis with sparse perivascular and interstitial inflammatory infiltrate, leukocytoclasis, sebaceous gland necrosis, fibrin exudation and thrombosis of small vessels in superficial dermis | Plasma VZV PCR and immunochemical stains for VZV were positive. | Iv acyclovir and oral valacyclovir/Significant improvement |
| Cury-Martins et al., 2019[14] | 26 | M | Acute lymphoid leukaemia under POMP regimen (prednisone, vincristine, methotrexate, mercaptopurine) | Deep infiltrated and ulcerated nodules with tense blisters | Bilateral upper and lower legs | Intraepidermal blister with ballooning, acantholytic keratinocytes, multinucleated cells and fibrinoid necrosis and thrombosis of vessels of the hypodermis | NA | Iv and oral acyclovir/Complete healing with residual atrophic scars |
| Alvarez- Salafranca et al.,2020[15] | 74 | M | Chronic kidney disease, type 2 diabetes mellitus, and chronic obstructive pulmonary disease | Purpuric non-confluent papules and vesicles | Bilateral lower legs and dorsum of the feet | Intraepidermal vesicle with acantholytic keratinocytes, multinucleation, intranuclear inclusion bodies and superficial dermis with perivascular inflammatory infiltrate with vasculitic changes | Swab VZV PCR was positive | Oral acyclovir/Complete resolution |
| Present report | 53 | F | Acute myeloid leukaemia under sorafenib 400 mg/day | Purpuric papules and plaques on an erythematous base with central haemorrhagic and necrotic crusts | Left gluteal area and upper leg | Intraepidermal bulla formation with nuclear inclusions, giant cell formations and superficial dermal vessels with leukocytoclastic vasculitis | NA | Oral valacyclovir/Complete resolution |
F, female; M, male; NA, not available
In conclusion, all previously reported cases and our case had a clinically distinctive appearance that prompted dermatologists to obtain a biopsy. Nevertheless, given the well-known vasculopathic effects of VZV, it is possible that this phenomenon is more common than reported. Although the clinical picture is alarming, this association appears quite benign and has no further complications. However, future studies are needed to elucidate the clinical implications of HZ with CSSV.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kennedy PG, Gershon AA. Clinical features of varicella-zoster virus infection. Viruses. 2018;10:609. doi: 10.3390/v10110609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mueller NH, Gilden DH, Cohrs RJ, Mahalingam R, Nagel MA. Varicella zoster virus ınfection: Clinical features, molecular pathogenesis of disease, and latency. Neurol Clin. 2008;26:675–97. doi: 10.1016/j.ncl.2008.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu X, Yun SJ, Erickson L, Chen L. Diseases caused by viruses. In: Elder DE, Elenitsas R, Rosenbach M, Murphy GF, Rubin AI, Xu X, editors. Lever's Histopathology of the Skin. Philadelphia, PA: Wolters Kluwer; 2015. pp. 1692–710. [Google Scholar]
- 4.Nagel MA, Gilden D. Update on varicella zoster virus vasculopathy. Curr İnfect Dis Rep. 2014;16:407. doi: 10.1007/s11908-014-0407-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keller TT, Mairuhu AT, de Kruif MD, Klein SK, Gerdes VE, ten Cate H, et al. Infections and endothelial cells. Cardiovasc Res. 2003;60:40–8. doi: 10.1016/s0008-6363(03)00354-7. [DOI] [PubMed] [Google Scholar]
- 6.Cohen C, Trapuckd S. Leukocytoclastic vasculitis associated with cutaneous infection by herpesvirus. Am J Dermatopathol. 1984;6:561–5. doi: 10.1097/00000372-198412000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Erhard H, Rünger TM, Kreienkamp M, Müller J, Müller-Hermelink HK, Bröcker EB. Atypical varicella-zoster virus infection in an immunocompromised patient: Result of a virus-induced vasculitis. J Am Acad Dermatol. 1995;32:908–11. doi: 10.1016/0190-9622(95)91560-5. [DOI] [PubMed] [Google Scholar]
- 8.Uhoda I, Piérard-Franchimont C, Piérard GE. Varicella-zoster virus vasculitis: A case of recurrent varicella without epidermal involvement. Dermatology. 2000;200:173–5. doi: 10.1159/000018359. [DOI] [PubMed] [Google Scholar]
- 9.Wollina U, Schönlebe J. Segmental leukocytoclastic vasculitis in herpes zoster. Int J Dermatol. 2012;51:1351–2. doi: 10.1111/j.1365-4632.2011.05167.x. [DOI] [PubMed] [Google Scholar]
- 10.Wong J-M, Huang P-H, Wei S-C. Gastrointestinal: Herpes vasculitis in an ulcerative colitis patient. J Gastroenterol Hepatol. 2013;28:586. doi: 10.1111/jgh.12093. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka A, Hayaishi N, Kondo Y, Kurachi K, Tanemura A, Katayama I. Severe gangrene accompanied by varicella zoster virus-related vasculitis mimicking rheumatoid vasculitis. Case Rep Dermatol. 2014;6:103–7. doi: 10.1159/000360979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burgard B, Smola S, Vogt T, Müller CS. Small vessel vasculitis in herpes zoster-Discussion of current aspects of varicella zoster virus vasculopathy. Am J Dermatopathol. 2018;40:602–4. doi: 10.1097/DAD.0000000000001134. [DOI] [PubMed] [Google Scholar]
- 13.Clark AK, Dhossche J, Korcheva VB, Keller JJ. Herpes zoster presenting as unilateral vasculitis. Dermatol Online J. 2018;24 13030/qt5dd717sw. [PubMed] [Google Scholar]
- 14.Cury-Martins J, Bellesso M, Sotto MN, Sanches JA. Atypical herpes vasculitis in a leukemic patient: An unusual presentation. Hematol Transfus Cell Ther. 2019;41:95–8. doi: 10.1016/j.htct.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alvarez-Salafranca M, Garcés-Horna V, García-García M, Ara-Martin M. Atypical vasculopathic varicella-zoster infection mimicking cutaneous small-vessel vasculitis. Int J Dermatol. 2020;59:e214–6. doi: 10.1111/ijd.14816. [DOI] [PubMed] [Google Scholar]
- 16.Mallick-Searle T, Snodgrass B, Brant JM. Postherpetic neuralgia: Epidemiology, pathophysiology, and pain management pharmacology. J Multidiscip Healthc. 2016;9:447–54. doi: 10.2147/JMDH.S106340. [DOI] [PMC free article] [PubMed] [Google Scholar]


