Abstract
Purpose
To develop a standardized method to improve readability of orthopaedic patient education materials (PEMs) without diluting their critical content by reducing the use of complex words (≥3 syllables) and shortening sentence length to ≤15 words.
Methods
OrthoInfo, a patient education website developed by the Academy of American Orthopedic Surgeons, was queried for PEMs relevant to the care of athletic injuries of the knee. Inclusion criteria were PEMs that were unique, pertained to topics of knee pathology in sports medicine, and written in a prose format. Exclusion criteria were information presented in video or slideshow format, or topics not pertaining to knee pathology in sports medicine. Readability of PEMs was evaluated using 7 unique readability formulas before and after applying a standardized method to improve readability while preserving critical content (reducing the use of ≥3 syllable words and ensuring sentence length is ≤15 words). Paired samples t-tests were conducted to assess the relationship between reading levels of the original PEMs and reading level of edited PEMs.
Results
Reading levels differed significantly between the 22 original PEMs and edited PEMs across all 7 readability formulas (P < .01). Mean Flesch Kincaid Grade Level of original PEMs (9.8 ± 1.4) was significantly increased compared to that of edited PEMs (6.4 ± 1.1) (P = 1.9 × 10–13). 4.0% of original PEMs met National Institutes of Health recommendations of a sixth-grade reading level compared with 48.0% of modified PEMs.
Conclusions
A standardized method that reduces the use of ≥3 syllable words and ensures sentence length is ≤15 words significantly reduces the reading-grade level of PEMs for sports-related knee injuries. Orthopaedic organizations and institutions should apply this simple standardized method when creating PEMs to enhance health literacy.
Clinical Relevance
The readability of PEMs is important when communicating technical material to patients. While many studies have suggested strategies to improve the readability of PEMs, literature describing the benefit of these proposed changes is scarce. The information from this study details a simple standardized method to use when creating PEMs that may enhance health literacy and improve patient outcomes.
The internet has become a vast resource for medical information. Approximately one-half of adult internet users have reported using the internet to learn more information about a specific medical treatment or procedure.1 In response to this current trend, the American Academy of Orthopaedic Surgeons (AAOS) has developed online patient education materials (PEMs) to enhance patient–doctor communication and improve patient health literacy in the treatment of orthopaedic conditions.2,3 However, although the internet can be a vast source of information, its usefulness in patient care is dependent not only on the content available to patients but also the health literacy of the patient consuming the information.
Health literacy is the capacity to obtain, process, and understand basic health concepts needed to make appropriate health decisions.3, 4, 5 Health literacy is considered to be the single best predictor of a patient’s health status, with poor health literacy leading to worse patient outcomes.3,6,7 Poor health literacy has been associated with more frequent hospital admissions, longer hospital stays, increased risk for seeking emergency care, increased complications, reduced compliance, and more frequent missed appointments.3,6,8, 9, 10, 11, 12, 13 Not only does poor health literacy bring worse outcomes for the patient, but it also contributes an estimated $73 billion of additional cost burden to the U.S. health care system.3 To be effective, PEMs must be written at a level that the target population can comprehend.
There is clearly a disparity with regards to health literacy in the United States. It is estimated that approximately 21% of U.S. adults read at, or below a fifth-grade reading level, described as “functionally illiterate.”1,3,14 An additional 30% of U.S. adults read between a sixth-grade and eighth-grade reading level, termed “marginally literate.” 1,3,14 Furthermore, nearly one-half of the Hispanic and African American US population is functionally illiterate.3,15,16 Therefore, the American Medical Association and National Institutes of Health recommend that all PEMs be written at or below a sixth-grade reading level.1, 2, 3, 4,17,18
Sports-related knee injuries such as anterior cruciate ligament or meniscus tears are very common, and there are ample resources for knee injury-related PEMs. However, anatomy, pathology, and treatment plans of knee injuries often are described in terms that are obscure to patients. Complex, multisyllable terminology, including “anterior cruciate ligament,” “articular cartilage,” “meniscectomy,” or “arthroscopy,” can be foreign and confusing terms for patients. Therefore, the field of sports medicine, specifically involving knee pathology, is rife with the possibility for misunderstanding, leading to low patient health literacy. Improving the readability of orthopaedic PEMs is a realistic and important goal to improve the health literacy and overall health of patients. While many studies have suggested simple strategies to improve readability scores of PEMs such as reducing complex words, literature describing the benefit of these proposed changes is scarce.2,17 The purpose of this study is to develop a standardized method that can be applied to orthopaedic knee injury–related PEMs for the purpose of improving their readability without diluting their critical content. We hypothesized that reducing the use of complex words (≥3 syllables) and shortening sentence length to ≤15 words would improve the readability of orthopaedic PEMs.
Methods
Data Collection
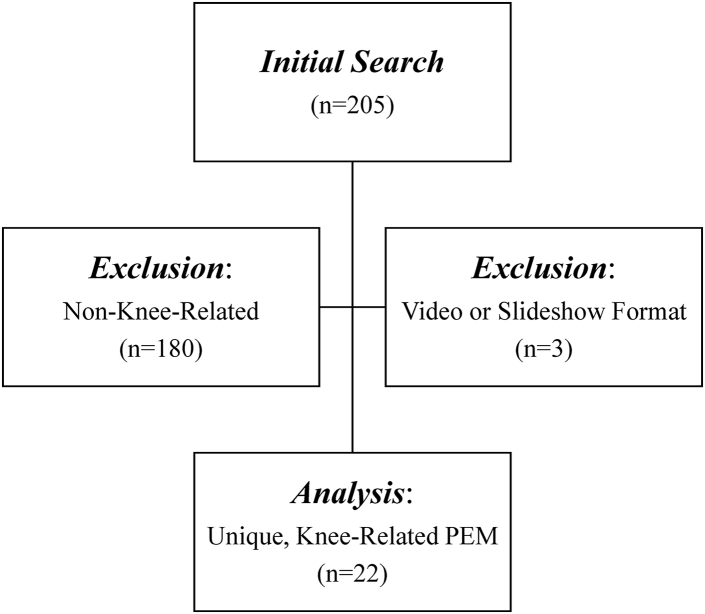
OrthoInfo, a patient education website developed and reviewed by the AAOS, was queried for PEMs relevant to the care of athletic injuries of the knee.19 All PEMs were collected by a single author from OrthoInfo (S.H.). Inclusion criteria were PEMs that were unique articles, pertained to topics of knee pathology in sports medicine, and written in a prose format. Exclusion criteria were information presented in video or slideshow format or topics not pertaining to knee pathology in sports medicine. A total of 205 PEMs were available for review for the study. After application of inclusion and exclusion criteria, 22 PEMs were included in the study (Table 1).
Table 1.
Readability Formula Scores of Seven Independent Readability Formulas for Original Versus Edited PEMs Included in the Present Study
| PEM: Article Title | Flesch Reading Ease Score |
Gunning Fog |
Flesch–Kincaid Grade Level |
The Coleman-Liau Index |
The SMOG Index |
Automated Readability Index |
Linsear Write Formula |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Original | Edited | Original | Edited | Original | Edited | Original | Edited | Original | Edited | Original | Edited | Original | Edited | |
| Adolescent Anterior Knee Pain | 48.8 | 63.5 | 13.5 | 9.2 | 11.2 | 7.5 | 12.0 | 11.0 | 10.3 | 7.4 | 11.8 | 7.5 | 12.7 | 6.8 |
| Anterior Cruciate Ligament (ACL) Injuries | 49.4 | 65.6 | 12.9 | 8.5 | 10.0 | 6.6 | 12.0 | 11.0 | 10.1 | 7.1 | 9.9 | 6.3 | 9.4 | 5.5 |
| Collateral Ligament Injuries | 61.3 | 75.6 | 11.4 | 7.5 | 8.1 | 4.9 | 10.0 | 9.0 | 8.8 | 6.0 | 7.8 | 4.5 | 8.2 | 4.4 |
| Combined Knee Ligament Injuries | 52.5 | 69.7 | 13.3 | 8.3 | 9.5 | 5.6 | 11.0 | 10.0 | 10.0 | 6.5 | 9.0 | 5.0 | 9.0 | 4.4 |
| Common Knee Injuries | 52.9 | 69.7 | 11.6 | 8.3 | 9.6 | 5.6 | 12.0 | 10.0 | 9.8 | 6.5 | 9.4 | 5.0 | 9.2 | 4.4 |
| Meniscus Tears | 55.3 | 69.9 | 11.7 | 7.7 | 8.7 | 5.7 | 11.0 | 10.0 | 8.9 | 6.3 | 8.4 | 5.3 | 7.7 | 4.5 |
| Osgood–Schlatter Disease (Knee Pain) | 55.5 | 73.2 | 12.6 | 8.2 | 9.7 | 6.0 | 12.0 | 10.0 | 9.2 | 6.2 | 10.8 | 6.7 | 11.0 | 6.1 |
| Patellar Dislocation and Instability in Children (Unstable Kneecap) | 52.5 | 68.6 | 13.0 | 9.2 | 10.1 | 6.6 | 12.0 | 10.0 | 9.9 | 7.3 | 10.3 | 6.3 | 11.2 | 6.3 |
| Patellar Tendon Tear | 56.5 | 70.7 | 11.6 | 8.7 | 9.1 | 6.3 | 11.0 | 9.0 | 8.8 | 6.7 | 9.1 | 6.2 | 8.7 | 6.2 |
| Patellofemoral Pain Syndrome | 51.9 | 70.7 | 12.9 | 8.6 | 10.4 | 6.3 | 12.0 | 9.0 | 9.8 | 6.7 | 10.8 | 6.3 | 11.6 | 6.1 |
| Pes Anserine (Knee Tendon) Bursitis | 42.9 | 63.0 | 14.4 | 10.0 | 11.6 | 7.6 | 13.0 | 10.0 | 11.1 | 7.9 | 11.6 | 7.5 | 12.4 | 7.2 |
| Posterior Cruciate Ligament (PCL) Injuries | 46.2 | 66.4 | 15.1 | 10.2 | 10.9 | 6.7 | 12.0 | 9.0 | 11.1 | 7.6 | 10.4 | 5.6 | 12.0 | 6.1 |
| Shin Splints | 57.5 | 63.1 | 11.5 | 9.8 | 8.4 | 7.0 | 12.0 | 11.0 | 8.4 | 7.3 | 8.6 | 7.0 | 7.4 | 5.7 |
| Unstable Kneecap | 64.4 | 73.9 | 11.4 | 8.3 | 8.6 | 5.9 | 9.0 | 9.0 | 8.3 | 6.3 | 9.2 | 5.9 | 10.8 | 6.1 |
| ACL Injury: Does It Require Surgery? | 37.7 | 53.0 | 16.9 | 12.5 | 13.3 | 9.6 | 13.0 | 12.0 | 12.4 | 9.4 | 13.8 | 9.5 | 15.4 | 9.0 |
| Knee Arthroscopy Exercise Guide | 71.1 | 77.7 | 8.0 | 6.3 | 6.0 | 4.7 | 10.0 | 9.0 | 6.3 | 5.2 | 5.9 | 4.4 | 5.5 | 4.4 |
| Knee Arthroscopy | 49.8 | 60.4 | 13.4 | 10.7 | 10.4 | 8.1 | 12.0 | 11.0 | 10.2 | 8.3 | 10.8 | 8.1 | 11.4 | 7.6 |
| Meniscal Transplant Surgery | 49.8 | 69.8 | 13.2 | 8.1 | 10.2 | 6.7 | 12.0 | 10.0 | 10.0 | 6.4 | 10.1 | 6.9 | 10.7 | 6.5 |
| Discoid Meniscus | 53.9 | 67.9 | 12.4 | 8.5 | 9.4 | 6.5 | 12.0 | 10.0 | 9.4 | 6.6 | 9.5 | 6.4 | 9.0 | 5.7 |
| Arthritis of the Knee | 48.6 | 73.3 | 13.7 | 7.5 | 10.6 | 5.7 | 13.0 | 10.0 | 10.3 | 6.0 | 11.1 | 5.8 | 11.4 | 5.3 |
| Osteonecrosis of the Knee | 49.9 | 72.8 | 12.5 | 6.7 | 10.4 | 6.0 | 12.0 | 9.0 | 9.7 | 5.4 | 10.4 | 6.0 | 11.0 | 5.6 |
| Patellofemoral Arthritis | 55.6 | 75.6 | 11.4 | 6.5 | 8.8 | 5.3 | 12.0 | 10.0 | 8.8 | 5.4 | 9.2 | 5.8 | 8.0 | 5.0 |
| Mean values | 52.9 | 68.8 | 12.7 | 8.6 | 9.8 | 6.4 | 11.7 | 10.0 | 9.6 | 6.8 | 9.9 | 6.3 | 10.2 | 5.9 |
| Standard deviation | 6.9 | 5.6 | 1.7 | 1.4 | 1.4 | 1.1 | 1.0 | 0.8 | 1.2 | 1.0 | 1.6 | 1.2 | 2.1 | 1.1 |
PEMs, patient education materials; SMOG, Simple Measure of Gobbledygook.
Determination of Readability
The reading level of each PEM was calculated using an online tool.20 Reading level was evaluated by 7 readability formulas, including Flesch Reading Ease score, Gunning-Fog, Flesch–Kincaid Grade Level, The Coleman–Liau Index, The Simple Measure of Gobbledygook Index, Automated Readability Index, and Linsear Write Formula (Table 2). Additional data recorded for each PEM included total number of words, mean number of words per sentence, mean number of syllables per word, and percentage of complex words.
Table 2.
Descriptions of the Seven Independent Readability Formulas Used to Evaluate Handouts in the Current Study
| Readability Assessment | Formula | Description |
|---|---|---|
| Flesch–Kincaid grade level | (0.39 × B) + (11.8 × W) – 15.59 | B = mean number of syllables per word W = mean number of words per sentence |
| Flesch Reading Ease | 206.835 – (1.015 × W) – (84.6 × B) | B = mean number of syllables per word W = mean number of words per sentence |
| Simple Measure of Gobbledygook (SMOG) Index | 1.043 × √(P × 30) + 3.1291 | P = number of words with ≥3 syllables S = number of sentences |
| Coleman–Liau | (0.0588 × L) – (0.296 × T) – 15.8 | L = mean number of letters/word T = mean number of sentences/100 words |
| Gunning Fog | 0.4 × (W/S + 100 – P/W) | S = mean number of sentences W = mean number of words/sentence P = mean number of words with ≥3 syllables |
| Automated Readability Index | 4.71 (characters/words) + 0.5 (words/sentences) – 21.43 | |
| Linsear Write | No formula—calculates the U.S. grade level of a text sample based on sentence length and the number of words with 3 or more syllables. | |
Assessing Readability
Each PEM was accessed on and downloaded from OrthoInfo.com. The content of each PEM was copy and pasted into a new Microsoft Word document. This content was then copy and pasted into the text box of the Automatic Readability Checker on www.readabilityformulas.com/. The option to “Check Text Readability” was selected and the readability data for each PEM was recorded.
Applying the Standardized Method to Improve Readability
After evaluating the readability of the original PEMs provided by OrthoInfo, the original documents were edited using a standardized method for improvement of readability while preserving critical content of the PEM (S.H., N.C., S.G., J.B.). The standardized method involved reducing the use of complex words (≥3 syllables) and ensuring sentence length was ≤15 words. The application of these editing techniques reflects the most often cited techniques for improving readability, which include replacing complex medical jargon with simpler terms and shortening sentence length to 10-15 words per sentnces.2,3,8,17,18,21,22 Critical content was described as medical information necessary for patient understanding of the described knee pathology and determined by the author who originally collected the PEMs (S.H.). Individuals determining critical content are preferably practicing orthopaedic surgeons; however, critical content also can be determined by individuals training within the field of orthopaedic surgery. Investigators were limited to a single round of editing in further attempts to preserve critical content. After editing, the reading level of each PEM was evaluated for a second time using the aforementioned criteria. The same readability formulas and same additional datapoints were recorded for the edited documents as for the original documents.
Statistical Analysis
Mean reading level, percentage of PEMs above a sixth-grade reading level, and percentage of PEMs at-or-below sixth-grade reading level were calculated for both original and edited PEMs. In addition, the mean change in reading level after editing was calculated for original and edited PEMs. Extracted data were analyzed through SPSS software version 19.0. Categorical variables are reported in frequencies and percentages. In addition, statistical analysis was conducted using paired-sample t-test to determine differences in reading level between original PEMs and edited PEMs. Paired samples t-tests were conducted to assess the relationship between reading levels of the original PEMs and reading level of edited PEMs. A P-value of .05 was deemed statistically significant.
Results
A total of 205 PEMs were available for review. Of these, 22 met the inclusion criteria and were included in the study (Fig 1). Reading levels differed significantly between the 22 original PEMs and edited PEMs across all 7 readability formulas (P < .01) (Table 1). Using the Flesch–Kincaid Grade Level readability formula, we found that the mean reading level for original PEMs was 9.77 ± 1.42 compared before modification with 6.40 ± 1.08 for edited PEMS (P = 1.9 × 10–13). Per the Flesch–Kincaid Grade level readability formula, one original PEM (4.0%) versus 12 edited PEMs (48.0%) met National Institutes of Health recommendations of a sixth-grade reading level before and after changes respectively. Readability formula scores and numerical data for each PEM evaluated is displayed in Tables 1 and 3. Readability scores across these 7 readability formulas are summarized in Table 4.
Fig 1.
Application of inclusion and exclusion criteria to patient education materials (PEMs) collected from a query of OrthoInfo.com for PEMs relevant to the care of athletic injuries of the knee.
Table 3.
Numerical Descriptive Statistics for Original Versus Edited PEMs Included in the Present Study
| Patient Education Material: Article Title | Number of Words (Total) |
Words per Sentence |
Mean Characters per Word |
Mean Syllables per Word |
% of 3+ Syllable Words |
No. of 3+ Syllable Words |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Original | Edited | Original | Edited | Original | Edited | Original | Edited | Original | Edited | Original | Edited | |
| Adolescent Anterior Knee Pain | 1,469 | 1,408 | 19 | 12 | 5 | 4.8 | 2 | 2 | 17% | 13% | 244 | 176 |
| Anterior Cruciate Ligament (ACL) Injuries | 1,333 | 1,247 | 15 | 10 | 5.1 | 4.8 | 2 | 2 | 21% | 14% | 277 | 178 |
| Collateral Ligament Injuries | 1,048 | 926 | 14 | 9 | 4.7 | 4.6 | 2 | 1 | 16% | 11% | 172 | 106 |
| Combined Knee Ligament Injuries | 752 | 641 | 14 | 8 | 4.9 | 4.7 | 2 | 2 | 21% | 14% | 156 | 91 |
| Common Knee Injuries | 1,316 | 641 | 15 | 8 | 5 | 4.7 | 2 | 2 | 19% | 14% | 252 | 91 |
| Meniscus Tears | 1,239 | 1,099 | 13 | 9 | 5 | 4.7 | 2 | 2 | 18% | 12% | 226 | 137 |
| Osgood-Schlatter Disease (Knee Pain) | 626 | 590 | 17 | 12 | 5 | 4.7 | 2 | 1 | 15% | 9% | 93 | 52 |
| Patellar Dislocation and Instability in Children (Unstable Kneecap) | 996 | 1,032 | 17 | 12 | 5 | 4.7 | 2 | 1 | 18% | 13% | 175 | 135 |
| Patellar Tendon Tear | 1,890 | 1,819 | 15 | 12 | 4.9 | 4.6 | 2 | 1 | 15% | 11% | 287 | 199 |
| Patellofemoral Pain Syndrome | 1,844 | 1,769 | 18 | 12 | 5 | 4.6 | 2 | 1 | 16% | 11% | 298 | 191 |
| Pes Anserine (Knee Tendon) Bursitis | 439 | 446 | 18 | 13 | 5.2 | 4.8 | 2 | 2 | 21% | 14% | 91 | 63 |
| Posterior Cruciate Ligament (PCL) Injuries | 1,195 | 1,131 | 17 | 11 | 5 | 4.6 | 2 | 2 | 22% | 15% | 263 | 172 |
| Shin Splints | 1,165 | 1,040 | 13 | 10 | 5 | 4.9 | 2 | 2 | 16% | 15% | 191 | 153 |
| Unstable Kneecap | 473 | 457 | 18 | 12 | 4.6 | 4.5 | 1 | 1 | 11% | 9% | 54 | 42 |
| ACL Injury: Does It Require Surgery? | 3,143 | 3,145 | 22 | 15 | 5.2 | 5 | 2 | 2 | 22% | 17% | 678 | 548 |
| Knee Arthroscopy Exercise Guide | 1,106 | 1,074 | 11 | 9 | 4.7 | 4.5 | 1 | 1 | 10% | 8% | 114 | 83 |
| Knee Arthroscopy | 1,708 | 1,402 | 17 | 13 | 5.1 | 4.9 | 2 | 2 | 19% | 15% | 317 | 214 |
| Meniscal Transplant Surgery | 1,175 | 1,037 | 15 | 13 | 5.1 | 4.7 | 2 | 1 | 19% | 9% | 226 | 92 |
| Discoid Meniscus | 1,266 | 1,165 | 15 | 11 | 5 | 4.7 | 2 | 2 | 17% | 11% | 221 | 132 |
| Arthritis of the Knee | 2,340 | 1,920 | 16 | 11 | 5.2 | 4.8 | 2 | 1 | 19% | 9% | 451 | 176 |
| Osteonecrosis of the Knee | 1,774 | 1,543 | 16 | 12 | 5 | 4.6 | 2 | 1 | 17% | 7% | 300 | 104 |
| Patellofemoral Arthritis | 1,440 | 1,208 | 13 | 11 | 5.1 | 4.7 | 2 | 1 | 17% | 7% | 242 | 90 |
| Mean values | 1,351.7 | 1,215.5 | 15.8 | 11.1 | 5.0 | 4.7 | 1.9 | 1.5 | 17.5% | 11.7% | 242.2 | 146.6 |
| Standard deviation | 600.3 | 584.4 | 2.4 | 1.7 | 0.2 | 0.1 | 0.3 | 0.5 | 3% | 3% | 129.1 | 100.2 |
PEMs, patient education materials.
Table 4.
Readability Scores of Seven Independent Readability Formulas for Original Versus Edited PEMs Included in the Present Study
| Readability Formula | Original PEMs |
Edited PEMs |
Change in Mean | P Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Flesch Reading Ease Score | 52.9 | 6.9 | 68.8 | 5.6 | 15.9 | P = 5.5E-13 |
| Gunning Fog | 12.7 | 1.7 | 8.6 | 1.4 | –4.1 | P = 1.5E-13 |
| Flesch–Kincaid Grade Level | 9.8 | 1.4 | 6.4 | 1.1 | –3.4 | P = 1.9E-13 |
| The Coleman-Liau Index | 11.7 | 1.0 | 10.0 | 0.8 | –1.7 | P = 5.2E-09 |
| The SMOG Index | 9.6 | 1.2 | 6.8 | 1.0 | –2.9 | P = 1.0E-12 |
| Automated Readability Index | 9.9 | 1.6 | 6.3 | 1.2 | –3.6 | P = 1.5E-13 |
| Linsear Write Formula | 10.2 | 2.1 | 5.9 | 1.1 | –4.3 | P = 2.0E-12 |
PEMs, patient education materials; SMOG, Simple Measure of Gobbledygook; SD, standard deviation.
The relationship between additional numerical data describing the original PEMs and edited PEMs, including mean number of words, mean words per sentence, mean characters per word, mean syllables per word, mean percentage of complex words, and mean number of complex words differed significantly. The mean number of words per sentence was measured to be 15.8 ± 2.4 for original PEMs versus 11.1 ± 1.7 for edited PEMs (P = 5.8 × 10–13). Percentage of complex words was measured to be 17.6% ± 3.1% for original PEMs compared to 11.7% ± 2.8% for edited PEMs (P = 7.2 × 10–10). Numerical data regarding these variables are summarized in Table 5. All numerical data compared between original PEMs and edited PEMs differed significantly (P < .01).
Table 5.
Composite Descriptive Statistics Comparing Original Versus Edited PEMs Included in the Present Study
| Measurement | Original PEMs |
Edited PEMs |
Change in Mean | P Value | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Number of words (total) | 1351.7 | 600.3 | 1215.5 | 584.4 | –136.2 | P = .00042 |
| Number of words per sentence | 15.8 | 2.4 | 11.1 | 1.7 | –4.7 | P = 5.8E-12 |
| Mean characters per word | 5.0 | 0.2 | 4.7 | 0.1 | –0.3 | P = 3.3E-11 |
| Mean syllables per word | 1.9 | 0.3 | 1.5 | 0.5 | –0.4 | P = .23 |
| % of 3+ syllable words | 17.60% | 3.10% | 11.70% | 2.80% | 5.9% | P = 7.2E-10 |
| No. of 3+ syllable words | 242.2 | 129.1 | 146.6 | 100.2 | –95.6 | P = 1.3E-7 |
PEMs, patient education materials; SD, standard deviation.
Discussion
The primary findings of this study support our hypothesis and illustrate that a standardized method focused on reducing the usage of complex words and reducing sentence length to ≤15 words per sentence improves readability of PEMs across all 7 readability formulas. This current study not only shows that PEMs for knee pathology in orthopaedic sports medicine are written at a level well above the recommended reading level, but also, more importantly, proposes a simple standardized method that effectively improves readability of PEMs while preserving critical content. The standardized method for improving readability used in this study significantly improved the readability of all PEMs across all 7 independent readability formulas and significantly reduced numbers of words, number of words per sentence, characters per word, syllables per word, percentage of complex words, and number of complex words. This is a clinically impactful finding as improving the readability of PEMs directly translates to enhanced patient health literacy which can lead to better patient outcomes.23, 24, 25 Furthermore, the simplicity of the standardized method allows for it to easily be applied to other fields within orthopaedics, as well as other specialties within medicine, to improve health literacy on a wider scale.
Recommendations for improving readability of PEMs have existed for several decades. The prevailing sentiment of these suggestions is that it is essential to consider the reading skills of the target audience when creating PEMs. The most often cited technique for improving readability includes replacing complex medical jargon with simpler terms (Fig 2).2,3,8,17,18,21,22 An example of simplifying word choice would be the replacement of the 4-syllable term “arthroscopy” with the 1-syllable word “scope.”8 Although both terms convey the same message, the latter is easier to understand and thus more accessible to the reader. In improving word choice, it has been recommended to use shorter words with fewer syllables.1,8,18 Another often-suggested technique includes simplifying sentences to be more succinct and easier to understand. 1,3,8,17,18,21,22 Reducing length of sentences to 10 to 15 words was shown by one study to improve the reading level of 8 PEMs by an average of 1.41 grade levels.2 This parallels the finding in the current study that limiting use of complex words and reducing sentence length to fewer than 15 words can effectively improve the reading level of PEMs by 3.13 grade levels according to the Flesch–Kincaid Grade Level readability formula. Other recommended strategies for improving readability of PEMs include writing in active versus passive voice, using bulleted lists when appropriate, supplementing with visual illustrations, using traditional 12- to 14-point font size, and maintaining consistency in word choice (e.g., using only “surgery,” “operation,” or “procedure” instead of interchanging them).1, 2, 3,8,22 Pitfalls that decrease readability, and should be avoided, include using all capital letters, italics, and nontraditional fonts and sans-serif fonts.3,26 While many studies analyzing readability of orthopaedic PEMs suggest these improvements, few, if any, have investigate the ability for these strategies to effectively improve readability of PEMs.
Fig 2.
List of complex words, often containing medical jargon, and their suggested alternatives that can function to improve readability of patient education materials (PEMs).17
Although the availability of PEMs has increased in past decades, there exists a remarkable discrepancy between the readability of the documents and the reading skills of target audience. Current literature has consistently demonstrated the readability of orthopaedic PEMs to be inappropriately high and well above the recommended sixth-grade reading level.1, 2, 3, 4,8,17,18 For many patients, this creates a barrier to understanding medical information and their own diagnoses. There exists ample literature describing the inappropriately high reading level of PEMs across many fields within orthopaedic surgery.1, 2, 3, 4,8,17,18 A 2008 study showed that PEMs published on the AAOS website had an average reading grade level of 10.4, and only 2% of the articles were written below the recommended sixth-grade reading level.3,4 A re-evaluation of AAOS PEMs in 2015 still showed that only 3% of these articles were written at or below the sixth-grade reading level.4,27 Recommendations for improving readability of PEMs have existed for several decades. The most often cited techniques include replacing complex medical jargon with simpler terms and shortening sentence length to 10-15 words per sentence.2,3,8,17,18,21,22 These measures are supposed to create PEMs that are more accessible to the reader without sacrificing the critical content of the article.
More recent literature consistently displays that readability of PEMs continues to be a barrier for patients. An analysis of the readability of PEMs provided by the American Orthopaedic Society for Sports Medicine in 2018 found that all PEMs were written above the recommended sixth-grade reading level with 36% written above a twelfth-grade reading level.17 In addition, a 2018 investigation of PEMs for hip arthroscopy found an average reading level of grade 12.79, with no individual websites containing information below an eighth-grade reading level.1 Furthermore, a 2015 analysis of online foot and ankle PEMs produced by the AAOS, the American Orthopaedic Foot and Ankle Society, Medline Plus, and 11 academic centers found an average reading level of grade 10.1, with no organization or institution producing a reading level within the recommended range.2 Thus, as these studies show, online PEMs currently require some degree of secondary education to properly understand the presented information. This limits the potential for improvement in health literacy and is a disservice to patients at large.
Inappropriately high reading levels of PEMs reduce both the accessibility and potential utility of these important opportunities for improving health literacy. Health literacy is vital for orthopaedic patients. Multiple studies have demonstrated an association between health literacy and patient expectation and outcomes and also have highlighted the importance of setting realistic expectations.17,28,29 When patients do not have a complete understanding of their health information, they have been shown to ask fewer questions when meeting with physicians and express understanding when they are actually unsure.17,30,31 Investigators have shown that, when health literacy is low, and patients lack a thorough understanding of their diagnosis and treatment plan, patients experience worse outcomes.3,8, 9, 10, 11 Poor health literacy has been associated with more frequent hospital admissions, with longer stays in the hospital, greater risks for seeking emergency care, increased complications, reduced compliance, and more frequent missed appointments.3,6,8, 9, 10, 11, 12, 13 Not only does poor health literacy bring worse outcomes for the patient, but also it creates financial burden. Poor health literacy contributes an estimated $73 billion of additional burden to the U.S. health care system.3 Estimates show that the health care cost of Medicaid for those with limited health literacy is approximately 4 times greater than those with adequate health literacy.3,7 Poor health literacy is a pervasive issue in orthopaedics that results in worse patient outcomes but has the potential to be fixed with better patient education.
Limitations
There are several limitations of this study. The first is the lack of patient perception of improvement of readability. As objective, evidence-based equations were used to determine readability, individual patients were not recruited to evaluate subjective readability of PEMs. In addition, the PEMs were only taken from a single informational website. While this was done to improve consistency with regards to the writing style and content, there is the possibility that other sources of literature may present information in a more readable form. Since this website is endorsed by the AAOS and is used by a large number or patients and providers alike, it was determined that this would be a valuable resource to assess. A third limitation was that the readability of the original and edited PEMs used in this study was not tested by actual patients. This represents an area of focus of future studies in which actual patient comprehension can be measured before and after reading the PEMs.
Conclusions
A standardized method that reduces the use of ≥3 syllable words and ensures that sentence length is ≤15 words significantly reduces the reading-grade level of PEMs for sports-related knee injuries. Orthopaedic organizations and institutions should apply this simple standardized method when creating PEMs to enhance health literacy.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.D. receives research support from Arthrex and travel support from Arthrex and Stryker. He is an editorial board member for Arthroscopy. He is a speaker for AO North America. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Mehta M.P., Swindell H.W., Westermann R.W., Rosneck J.T., Lynch T.S. Assessing the readability of online information about hip arthroscopy. Arthroscopy. 2018;34:2142–2149. doi: 10.1016/j.arthro.2018.02.039. [DOI] [PubMed] [Google Scholar]
- 2.Sheppard E.D., Hyde Z., Florence M.N., McGwin G., Kirchner J.S., Ponce B.A. Improving the readability of online foot and ankle patient education materials. Foot Ankle Int. 2014;35:1282–1286. doi: 10.1177/1071100714550650. [DOI] [PubMed] [Google Scholar]
- 3.Badarudeen S., Sabharwal S. Assessing readability of patient education materials: Current role in orthopaedics. Clin Orthop Rel Res. 2010;468:2572–2580. doi: 10.1007/s11999-010-1380-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts H., Zhang D., Dyer G.S.M. The readability of AAOS patient education materials: Evaluating the progress since 2008. J Bone Joint Surg Am. 2016;98:e70. doi: 10.2106/JBJS.15.00658. [DOI] [PubMed] [Google Scholar]
- 5.Friedman D.B., Hoffman-Goetz L. A systematic review of readability and comprehension instruments used for print and web-based cancer information. Health Educ Behav. 2006;33:352–373. doi: 10.1177/1090198105277329. [DOI] [PubMed] [Google Scholar]
- 6.Baker D.W., Parker R.M., Williams M.v., Clark W.S., Nurss J. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87:1027–1030. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson K., Weiss B.D. How long does it take to assess literacy skills in clinical practice? J Am Board Fam Med. 2008;21:211–214. doi: 10.3122/jabfm.2008.03.070217. [DOI] [PubMed] [Google Scholar]
- 8.Yi M.M., Yi P.H., Hussein K.I., Cross M.B., della Valle C.J. Readability of patient education materials from the web sites of orthopedic implant manufacturers. J Arthroplasty. 2017;32:3568–3572. doi: 10.1016/j.arth.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: An updated systematic review. Ann Intern Med. 2011;155:97. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 10.DeWalt D.A., Berkman N.D., Sheridan S., Lohr K.N., Pignone M.P. Literacy and health outcomes. J Gen Intern Med. 2004;19:1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Serper M., Patzer R.E., Curtis L.M., et al. Health literacy, cognitive ability, and functional health status among older adults. Health Serv Res. 2014;49:1249–1267. doi: 10.1111/1475-6773.12154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedland R. Congress of the United States. U.S. Congress; Washington, DC: 1998. Understanding health literacy: new estimates of the high costs of inadequate health literacy; pp. 57–91. The price we pay for illiteracy. [Google Scholar]
- 13.Murero M., D’Ancona G., Karamanoukian H. Use of the internet by patients before and after cardiac surgery: An interdisciplinary telephone survey. J Med Internet Res. 2001;3:e27. doi: 10.2196/jmir.3.3.e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ley P., Florio T. The use of readability formulas in health care. Psychol Health Med. 1996;1:7–28. [Google Scholar]
- 15.National Center for Education Statistics. A First Look at the Literacy of America’s Adults in the 21st Century. 2006. https://nces.ed.gov/naal/pdf/2006470.pdf Accessed March 14, 2022.
- 16.National Center for Education Statistics . National Center for Education Statistics; Washington, DC: 1993. Adult literacy in America: A first look at the results of the National Adult Literacy Survey. [Google Scholar]
- 17.Kakazu R., Schumaier A., Minoughan C., Grawe B. Poor readability of AOSSM patient education resources and opportunities for improvement. Orthop J Sports Med. 2018;6 doi: 10.1177/2325967118805386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stelzer J.W., Wellington I.J., Trudeau M.T., et al. Readability assessment of patient educational materials for shoulder arthroplasty from top academic orthopedic institutions. JSES Int. 2022;6:44–48. doi: 10.1016/j.jseint.2021.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Academy of Orthopaedic Surgeons OrthoInfo. https://orthoinfo.org
- 20.My Byline Media Readability Formulas. www.readabilityformulas.com
- 21.Jackson R.H., Davis T.C., Bairnsfather L.E., George R.B., Crouch M.A., Gault H. Patient reading ability: An overlooked problem in health care. South Med J. 1991;84:1172–1175. doi: 10.1097/00007611-199110000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Flesch R. A new readability yardstick. J Appl Psychol. 1948;32:221–233. doi: 10.1037/h0057532. [DOI] [PubMed] [Google Scholar]
- 23.Rooney M.K., Santiago G., Perni S., et al. Readability of patient education materials from high-impact medical journals: A 20-year analysis. J Patient Exp. 2021;8 doi: 10.1177/2374373521998847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Friedman A.J., Cosby R., Boyko S., Hatton-Bauer J., Turnbull G. Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. J Cancer Educ. 2011;26:12–21. doi: 10.1007/s13187-010-0183-x. [DOI] [PubMed] [Google Scholar]
- 25.Wilson E.A.H., Park D.C., Curtis L.M., et al. Media and memory: The efficacy of video and print materials for promoting patient education about asthma. Patient Educ Couns. 2010;80:393–398. doi: 10.1016/j.pec.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Albright J., de Guzman C., Acebo P., Paiva D., Faulkner M., Swanson J. Readability of patient education materials: Implications for clinical practice. Appl Nursing Res. 1996;9:139–143. doi: 10.1016/s0897-1897(96)80254-0. [DOI] [PubMed] [Google Scholar]
- 27.Eltorai A.E.M., Thomas N.P., Yang H., Daniels A.H., Born C.T. Readability of trauma-related patient education materials from the American Academy of Orthopaedic Surgeons. Trauma Mon. 2016;21 doi: 10.5812/traumamon.20141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rossi M.J., Brand J.C., Provencher M.T., Lubowitz J.H. The expectation game: Patient comprehension is a determinant of outcome. Arthroscopy. 2015;31:2283–2284. doi: 10.1016/j.arthro.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Wu J.R., Moser D.K., DeWalt D.A., Rayens M.K., Dracup K. Health literacy mediates the relationship between age and health outcomes in patients with heart failure. Circ Heart Fail. 2016;9 doi: 10.1161/CIRCHEARTFAILURE.115.002250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Katz M.G., Jacobson T.A., Veledar E., Kripalani S. Patient literacy and question-asking behavior during the medical encounter: A mixed-methods analysis. J Gen Intern Med. 2007;22:782–786. doi: 10.1007/s11606-007-0184-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Menendez M.E., van Hoorn B.T., Mackert M., Donovan E.E., Chen N.C., Ring D. Patients with limited health literacy ask fewer questions during office visits with hand surgeons. Clin Orthop Relat Res. 2017;475:1291–1297. doi: 10.1007/s11999-016-5140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.