Abstract
Background:
The optimal timing of surgery for pectus excavatum (PE) is controversial. A large proportion of children will not undergo surgery before puberty. However, untimely surgery may lead to a decline in the children’s social adaptation and competitiveness because the children have already developed psychological and physiological impairments due to PE at an early age. The study retrospectively compared the academic performance in PE children undergoing the Nuss procedure versus nonsurgical observation.
Methods:
This retrospective real-world research study included 480 PE patients with definite surgical indications, in whom it was first recommended that they undergo surgery between the ages of 6 and 12 years old. Academic performance was collected at baseline and 6 years later. A generalized linear regression was calculated to screen the factors affecting the performance. A propensity score matching (PSM) analysis was conducted to reduce the potential for confounding factors between surgical and nonsurgical PE patients.
Results:
Haller index (HI) and pulmonary function were recognized as factors affecting baseline performance according to the generalized linear regression. For PE children with surgical indications, their academic performance significantly declined after 6 years of nonsurgical observation (52.1% ± 17.1% versus 58.3% ± 16.7%, p = 0.042). The academic performance in the surgery group was better than that in the nonsurgery group 6 years after PSM (60.7% ± 17.7% versus 52.1% ± 17.1%, p = 0.008).
Conclusions:
The severity of PE will affect the academic performance of children.
For PE children with definite surgical indications between the ages of 6 and 12 years old, surgical intervention rather than nonsurgical observation is more conducive to the development of children’s academic performance.
Keywords: academic performance, Nuss procedure, pectus excavatum
Graphical abstract

Introduction
Pectus excavatum (PE), characterized by obvious anterior chest wall depression, is the most common congenital chest wall deformity leading to compression of the lungs and heart.1 The Nuss procedure is recognized as an effective therapeutic option for the majority of children with PE.2 Several optimal ages of surgery have been reported but are still controversial.3 A considerable proportion of PE patients choose surgical intervention in adulthood or even lifelong follow-up without surgery.4,5
Psychological and physiological impairments brought by PE and the progress of these impairments directly determine the timing of surgical intervention and the use of other adjuvant treatments outside of surgery.6 Previously conducted studies have shown that persons with PE suffer from psychosocial distress due to the deformity; commonly reported issues are poor body image, low self-esteem and feelings of shame because of how the chest looks.6–8
Considering that there is definite evidence that PE will damage children’s cardiopulmonary function,9,10 cause psychological and behavioural discords,11,12 and affect children’s sleep quality at night,13,14 we speculate that the social adaptation and competitiveness of children with PE will be abnormal. Academic performance is a relatively objective and possibly the most concerning competitiveness evaluation index of parents and children in China.15 Therefore, we conducted this cohort study to explore the impact of PE on children’s academic performance (i.e. school gradings). In this study, we will focus on whether different surgical ages will cause differences in the academic performance of children with PE over a long period of follow-up.
Methods
Data and patients
This study was approved by the Ethics Committee of our hospital (approval number: 2019-211) and was registered in the Chinese Clinical Trail registry (registry number: ChiCTR1900028575). This study involving human participants was in accordance with the 1964 Helsinki Declaration and its later amendments and comparable ethical standards,16 and all of the children’s guardians signed a consent form authorizing the authors to collect the clinical data and academic performance ranking (i.e. school gradings) of the children. This study was reported according to the strengthening the reporting of cohort studies (STROCSS) criteria17 and reporting of observational studies in epidemiology (STROBE) statement.18 Retrospective data were collected from the Clinical Database of Children’s Hospital of Chongqing Medical University from January 1997 to May 2019. The data were extracted and integrated by two groups of independent authors, and the inconsistent data were discussed and analysed by all of the authors. Since there is no relevant similar study, the sample size cannot be accurately calculated.
PE was diagnosed by visual evaluation and computed tomography (CT) scans. Patient sex, Haller index (HI), resting pulmonary function test results and echocardiography (UCG) and electrocardiogram (ECG) results were collected as demographic and baseline characteristics. The indications for surgical treatment included at least two of the following19: (1) HI greater than 3.20 or deformity had progressed by visual assessment of parents; (2) cardiac or pulmonary compression by visual assessment on CT or reduced cardiac diastolic function parameters such as E peak/A peak ratio and ventricular end diastolic volume index ratio on echocardiogram; (3) abnormal lung function by resting pulmonary function test; (4) mitral valve prolapse or arrhythmia; (5) symptoms such as repeated episodes of respiratory infections were present; (6) patients had a severe psychosocial disorder; (7) patients or their parents had a strong desire for deformity correction.
Patients who underwent the Nuss procedure within 6 years in our institution after the initial recommendation of surgery and according to the above indications were included in the surgery group. Otherwise, they were included in the nonsurgical group. The baseline time of the patients in the surgery group was the first hospitalization time. The baseline time of the nonsurgical group was when they first received a recommendation for surgery. Academic performance rankings of the patients at baseline and at the endpoint were collected.
The endpoint time was set to 6 years after the baseline time. Children aged 6–12 years at baseline were included in the study. Only participants with complete demographic data and complete class rankings of final examinations at baseline and endpoint were included in the final analysis.
During the study period, the children who have experienced parents’ divorce, relatives’ demise, leaving the city, or a diagnosis of a major disease that interrupted their schooling were excluded.20,21 Healthy children who underwent routine physical examination in our hospital were selected as the control group. We randomized matched healthy children with PE children at a ratio of 1:1 using our hospital data management system according to age, gender and city. The academic performance rankings at baseline were collected to explore whether the academic performance ranking of the children with PE was abnormal.
Variables and outcome measures
Patient sex, HI, resting pulmonary function test results, cardiac function and academic performance ranking in class at baseline were collected as demographic and baseline characteristics. HI was calculated by the CT scans. Abnormal lung function was defined as forced expiratory volume in 1 second (FEV1) that was less than 80% of the predicted value, forced vital capacity (FVC) that was less than 80% of the predicted value, or FEV1/FVC less than 92% of the predicted value.22 Abnormal cardiac function was defined as mitral valve prolapse or arrhythmia.
Total academic performance ranking (i.e. school gradings) in class at endpoint was set as the outcome of the study. The scores of arts, music and sports are usually not included in these rankings. According to our national policy, we cannot report a specific ranking for children’s grades or what percentage of the children’s grades are ranked in the class. Therefore, we can only report what percentage of the students in his or her class did his or her score exceed. For example, if the score is marked as 45%, this shows that his or her final grade is better than 45% of the children in the class. The improvement rate of academic performance was estimated with the following equation:
Statistical analysis
Continuous data are displayed as the means with standard deviations (SDs) or the medians with interquartile ranges (IQRs). The Kolmogorov–Smirnov test was calculated to assess the normal distribution. The differences in the continuous variables between the two groups were compared by an unpaired t test if the variables were normally distributed. Otherwise, the Mann–Whitney U test was performed. Data from categorical variables were compared by a chi-square test. A generalized linear regression model screened the factors affecting the performance. Pearson correlation was calculated to measure the relevance between two continuous variables. Subgroup analysis and restricted cubic spline (RCS) were used to observe specific relationships between the variables in detail. The p values and standardized differences were used to assess the differences between the groups. Standardized differences less than 0.10 indicated absolute balance.
Propensity score matching (PSM) was used to reduce the potential for confounding by the baseline factors.23 The nearest neighbour matching method was employed, and the calliper was set as 0.02. In matching, maximization of execution performance and randomization of case order were performed.
SPSS version 24 (IBM, Armonk, NY, USA), Stata version 14.0 (Stata Corp, College Station, TX, USA) and R (http://www.R-project.org) were used for statistical analysis.
Results
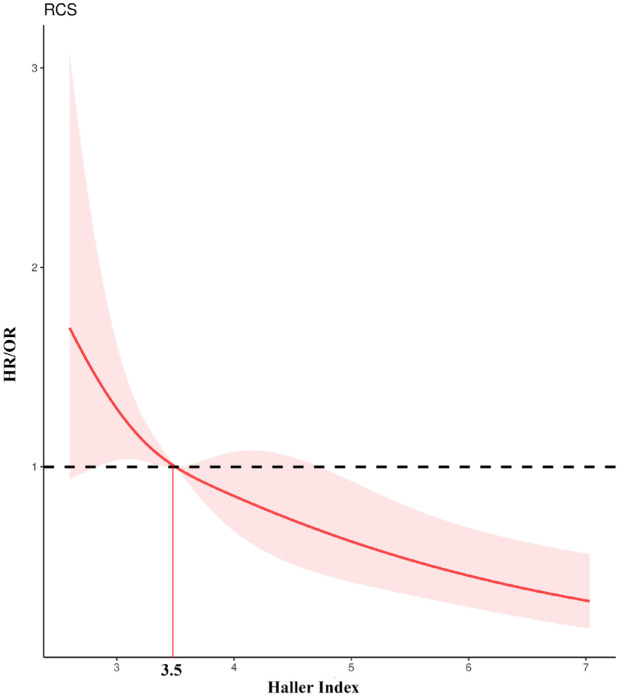
The flow chart of the study is shown in Figure 1. Four hundred and twenty-one patients in the surgery group and 59 patients in the nonsurgery group were analysed in the cohort study (Table 1). The HI of the surgery group (mean = 3.60, IQR = 3.18–4.17) was sufficiently higher than that of the nonsurgery group (mean = 3.28, IQR = 2.84–3.87, p < .001). Differences in age, sex, pulmonary function and cardiac function were not observed. The distribution of sex was the only well-balanced clinical characteristic. HI and pulmonary function were recognized as factors affecting the baseline performance according to the generalized linear regression model (Table 2). HI was confirmed as a risk factor for the baseline performance by the trend analysis (Figure 2) (p for trend <0.001). The reference point (HR/OR = 1) of HI was 3.5 (RCS) (Figure 3). If a patient has an HI higher than 3.5, the risk that his academic performance will be worse than the average level of children with PE will be significantly increased.
Figure 1.
Flow chart of the study.
PE, pectus excavatum; PSM, propensity score matching.
Table 1.
Demographic and preoperative clinical characteristics.
| Variable | Surgery (n = 421) |
Nonsurgery (n = 59) |
p value | Standardized differences |
|---|---|---|---|---|
| Gender | Male/Female (340/81) | Male/Female (48/11) | 0.91 | 0.02a |
| Age | 10.0(7.0–11.0) | 10.0(8.0–11.0) | 0.21 | 0.17 |
| Haller index | 3.6(3.18–4.17) | 3.28(2.84–3.87) | <0.001* | 0.56 |
| Pulmonary function | Normal/Abnormal (302/119) |
Normal/Abnormal (47/12) |
0.20 | 0.18 |
| Cardiac function | Normal/Abnormal (293/128) |
Normal/Abnormal (45/14) |
0.29 | 0.16 |
| Baseline performance (%) | 57.6 ± 16.4 | 58.3 ± 16.7 | 0.743 | 0.04a |
| Endpoint performance (%) | 59.2 ± 17.0 | 52.1 ± 17.1 | 0.003* | 0.41 |
Abnormal lung function is defined as (FEV1) less than 80% predicted value or FVC less than 80% predicted value or FEV1/FVC less than 92% predicted value.
Abnormal cardiac function is defined as mitral valve prolapse or arrhythmia.
The academic performance is reported as what percentage of the students in his or her class did his or her score exceed.
Standardized differences less than 0.10 indicated absolute balance.
p < 0.05.
Table 2.
Generalized linear regression model of baseline performance.
| Variables | R | 95% CI low | 95% CI up | p value |
|---|---|---|---|---|
| Age | 0.001 | −0.006 | 0.007 | 0.841 |
| Haller index | −0.033 | −0.046 | −0.02 | <0.001* |
| Gender (male) | 0.001 | −0.035 | 0.038 | 0.938 |
| Cardiac function (Normal) |
−0.005 | −0.05 | 0.04 | 0.835 |
| Pulmonary function (Normal) |
0.054 | 0.009 | 0.1 | 0.02* |
CI, confidence interval.
Abnormal lung function is defined as (FEV1) less than 80% predicted value or FVC less than 80% predicted value or FEV1/FVC less than 92% predicted value.
Abnormal cardiac function is defined as mitral valve prolapse or arrhythmia.
p < 0.05.
Figure 2.
Trend analysis between HI and academic performance at baseline.
HI, Haller index.
*p < 0.05.
Figure 3.
RCS between HI and academic performance at baseline.
The reference point (HR/OR = 1) was 3.5. HI, Haller index.
Although the average academic performance of the children in the healthy group was higher than that of the children with PE, the difference did not reach statistical significance (58.9% ± 21.1% versus 57.6% ± 16.4%, p = 0.27) (Figure S1). Similar results were observed (58.4% ± 20.1% versus 55.3% ± 17.0%, p = 0.079) in the PE patients with a higher HI of the reference point (higher than 3.5). We performed a subgroup analysis of the two groups according to their age at baseline. No differences in academic performance were found in any age group (Figure 4). At the same time, we did not find a stable trend with age. The p for trend in the PE group was 0.647 and was 0.219 in the control group (Table S1).
Figure 4.
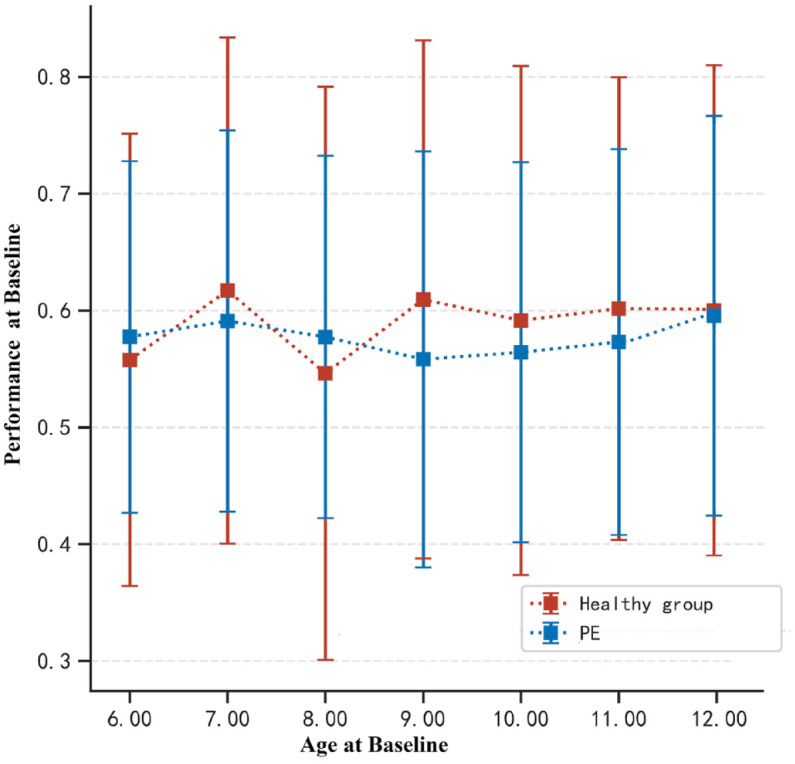
Subgroup analysis between age at baseline and academic performance at baseline in PE and healthy group.
PE, pectus excavatum.
Then, we focused on the impact of surgery on the academic performance of children with PE. However, the academic performance at the endpoint was not significantly better than that at baseline in the surgery group (59.2% ± 17.0% versus 57.6% ± 16.4%, p = 0.212). The academic performance at the endpoint of the children in the nonsurgical group decreased significantly from the baseline (52.1% ± 17.1% versus 58.3% ± 16.7%, p = 0.042) (Figure 5). We evaluated the improvement rate of academic performance in the PE children and found that HI was a factor in the change in academic performance [R = 0.115, 95% confidence interval (CI): 0.037–0.193, p = 0.041] (Table S2). No other significant variables were observed.
Figure 5.
Comparisons of performance ranking at baseline and endpoint in surgery and nonsurgery group.
We performed PSM to reduce the potential for confounding by baseline factors to analyse the impact of surgery on academic performance more scientifically. Fifty-six patients in the surgery group and 59 patients in the nonsurgery group were included in the analysis after PSM. The imbalance of variables was obviously reduced, but the variables of age were not well balanced (Figure S2). The academic performance at the endpoint in the surgery group was better than that in the nonsurgery group after PSM (60.7%±17.7% versus 52.1%±17.1%, p = 0.008) (Table 3).
Table 3.
Demographic and preoperative clinical characteristics after PSM.
| Variable | Surgery (n = 56) |
Nonsurgery (n = 59) |
p value | Standardized differences |
|---|---|---|---|---|
| Gender | Male/Female (45/11) | Male/Female (48/11) | 0.89 | 0.02a |
| Age | 10.0(8.0–11.0) | 10.0(8.0–11.0) | 0.27 | 0.13 |
| Haller index | 3.26(3.01–3.60) | 3.28(2.84–3.87) | 0.79 | 0.07a |
| Pulmonary Function | Normal/Abnormal (46/10) |
Normal/Abnormal (47/12) |
0.73 | 0.06a |
| Cardiac Abnormality | Normal/Abnormal (45/11) |
Normal/Abnormal (45/14) |
0.60 | 0.09a |
| Baseline Performance (%) | 57.7.±16.5 | 58.3 ± 16.7 | 0.741 | 0.04a |
| Endpoint Performance (%) | 60.7 ± 17.7 | 52.1 ± 17.1 | 0.008* | 0.48 |
Abnormal lung function is defined as (FEV1) less than 80% predicted value or FVC less than 80% predicted value or FEV1/FVC less than 92% predicted value; Abnormal cardiac function is defined as mitral valve prolapse or arrhythmia; The academic performance is reported as what percentage of the students in his/her class did his or her score exceed.
Standardized differences less than 0.10 indicated absolute balance.
p < 0.05
Discussion
The damage caused by PE in children may be beyond conventional imagination.24 Traditionally, the damage caused by PE is mainly concentrated in the compression of the heart and lung.25 Previous studies have confirmed that because of the depression of the sternum, the lungs, especially the small airways, will be widely affected, and the heart movement will be limited.10 The above results will lead to a decline in resting and exercise lung function and abnormal exercise cardiac function in children.9,10 This may make children more prone to fatigue during high-intensity mental and physical activities. In addition, long-term cardiopulmonary compression may be closely related to the occurrence and progression of other diseases, such as sleep-related breathing disorder (SRBD).13,14 The occurrence of PE and scoliosis seems to have a similar genetic background, and the progression of PE may also aggravate scoliosis.26
Moreover, the appearance of the deformity of PE is very obvious. With the development of social media, children, parents and their peers are more likely to recognize this deformity than in the past. A previous study indicated that the majority of patients first perceived their chest wall deformity between the ages of 6 years.12 This makes children have obstacles in psychological and behavioural development. Children may feel inferior because of this appearance and be discriminated against by their peers. Finally, they are afflicted by social withdrawal, depression and aggressive behaviour. Their behavioural disorders may not readily resolve after surgery once they occur.6 The fear of abnormal psychological behaviour has been the most important factor for deciding to undergo surgery for more than half of the parents of the children.27
Due to the comprehensive impact of PE on children as described above, some researchers speculated that the quality of life of children with PE would decline and conducted questionnaire surveys. Most of the questionnaire results confirmed that the quality of life of children with PE will decline.28 However, these questionnaires are rather subjective. More objective criteria are needed to evaluate the impact of PE on children in society. We look forward to selecting an appropriate outcome to analyse whether PE will cause a decline in children’s social competitiveness. It is difficult to evaluate the social competitiveness of children, and academic performance is a relatively objective indicator. Academic performance seems to be the most important social evaluation index of minors for parents and students in our country. In clinical work, many parents will choose to complete PE surgery in winter and summer vacation because of the worry about surgery affecting their children’s studies. The children in our country place great pressure on their academic performance, which provides us with an opportunity to observe their competitiveness under high intensity. Therefore, we conducted this research with academic performance as the primary outcome.
There are many factors affecting academic performance. To minimize potential bias, we have made attempts in three aspects. First, we standardized the academic performance of children by the rank of class to avoid the potential bias caused by direct score comparison. Second, we have avoided some factors that may affect the performance of children, such as diversity of patients, death of relatives, leaving the city, or diagnosed with major diseases where children need to have their school interrupted. Finally, we matched the baseline academic performance of the PE children with healthy children so that we can better observe whether their academic performance of PE is abnormal. This study found that the average baseline academic performance of the children with PE was lower than that of the healthy children, but the difference did not reach statistical significance. At the same time, we found that HI was a risk factor for the baseline academic performance of the children with PE; the reference point was 3.5. HI is the most important index to measure the severity of PE at present, and an HI greater than 3.5 is considered severe PE. The above results confirm that the aggravation of PE deformities may affect the academic performance of children.
Another key issue in the treatment of PE is the time of surgery. Although young age is not a decisive contraindication for the treatment of PE, finding a more appropriate age for surgery can improve the quality of life of children after surgery. The median age for repair has shifted from 6 years in the first decade to 15 years in the third decade according to the experience of Doctor Nuss.29 Some surgeons consider the optimal timing for PE repair to be 10–14 years of age based upon the presence of chest wall malleability and the relatively low risk of recurrent PE with subsequent growth.30 The Chinese Association of Thoracic Surgeons recommends that the appropriate age for conducting PE surgery is between 6 and 12 years old.27 The recommended age for surgery is 3 to 12 years old according to the Chinese Paediatric Surgery Association.31 Adolescent surgery is mainly expected to reduce the recurrence rate of surgery, while early surgery (under the age of 6) is mainly expected to reduce the potential disorders of PE.
This study also attempted to explore the impact of age on the academic performance of children with PE. We found that age is not a risk factor for the academic performance of PE children with definite surgical indications. There was no stable trend in the change in baseline academic performance of children with PE in the different age groups. No significant difference in academic performance was observed between the healthy and PE groups. However, at the end point of the study 6 years after baseline, the academic performance of the children in the nonsurgical group decreased significantly compared with their academic performance at baseline. The academic performance at the endpoint in the surgery group was significantly better than that in the nonsurgery group. This suggests that for children with surgical indications, timely surgery rather than observation is more conducive to reducing the adverse impact of PE on their academic performance.
There are still some limitations in the study. The first is the universality of the population. Although our institution has carried out nearly 3000 Nuss procedures in the past 20 years, the vast majority of children are from the western region in China (a relatively underdeveloped region), so they cannot represent the overall population of Nuss patients. The results of this study may not be generalizable to the population areas with high economic development levels especially outside China. Second, although we tried to reduce the relevant bias, in the real world, there are many factors that affect academic performance, so there may be potential unknown factors that affect the main conclusions of the study. Third, all patients included in the study were conformed to definite surgical indications. The conclusions of the study may not be suitable for patients with mild PE
However, to the best of our knowledge, this is the first article to study the impact of PE on academic performance. Through this study, we successfully demonstrated the potential impairment of PE to children on academic performance. This study provides evidence to help clinicians and families of children decide to actively choose surgery rather than observation. We hope that this article can attract more clinicians’ attention to the field of PE to better help children with PE make clinical decisions and reduce potential damage. Are we focusing too much on the physical manifestations of the disease only? A condition such as PE can have far deeper consequences for patients than surgeons realize.
Conclusion
For PE children with definite surgical indications, their academic performance will significantly decline under 6-year nonsurgical observation. The academic performance in the surgery group was better than that in the nonsurgery group after a follow-up of 6 years. A higher HI was a risk factor for academic performance.
Supplemental Material
Supplemental material, sj-docx-4-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-5-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-tif-2-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-tif-3-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-xlsx-1-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Acknowledgments
We would like to thank Jishizhan Chen for the graphical abstract production.
Footnotes
ORCID iDs: Hongbo Li  https://orcid.org/0000-0001-9263-7938
https://orcid.org/0000-0001-9263-7938
Quan Wang  https://orcid.org/0000-0003-4886-402X
https://orcid.org/0000-0003-4886-402X
Supplemental material: Supplemental material for this article is available online.
Contributor Information
Hongbo Li, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China; Chongqing Higher Institution Engineering Research Center of Children’s Medical Big Data Intelligent Application, Chongqing, China; Chongqing Key Laboratory of Pediatrics, Chongqing Medical University, Chongqing, China.
Shulei Fan, Department of Respiratory Medicine, Second Affiliated Hospital of Chongqing Medical University, Chongqing, China.
Xiangpan Kong, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China.
Zhengxia Pan, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China.
Chun Wu, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China.
Yonggang Li, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China.
Gang Wang, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China.
Jiangtao Dai, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, Chongqing, China.
Dawei He, Chongqing Higher Institution Engineering Research Center of Children’s Medical Big Data Intelligent Application, Chongqing, China; Chongqing Key Laboratory of Pediatrics, Chongqing Medical University, Chongqing, China.
Quan Wang, Department of Cardiothoracic Surgery, Ministry of Education Key Laboratory of Child Development and Disorders, National Clinical Research Center for Child Health and Disorders, China International Science and Technology Cooperation Base of Child Development and Critical Disorders, Children’s Hospital of Chongqing Medical University, No.136 Zhongshan Second Road, Yuzhong District, Chongqing 400014, China; Chongqing Higher Institution Engineering Research Center of Children’s Medical Big Data Intelligent Application, Chongqing, China; Chongqing Key Laboratory of Pediatrics, Chongqing Medical University, Chongqing, China.
Declarations
Ethics approval and consent to participate: All of the children’s guardians signed a consent form authorizing the authors to collect the clinical data and report research results This study was approved by the Ethics Committee of Children’s Hospital of Chongqing Medical University (approval number: 2019-211) and was registered in the Chinese Clinical Trail registry (registry number: ChiCTR1900028575).
Consent for publication: Not appliable.
Author contributions: Hongbo Li: Conceptualization; Data curation; Formal analysis; Funding acquisition; Methodology; Project administration; Software; Supervision; Validation; Writing – original draft.
Shulei Fan: Data curation; Formal analysis; Resources; Validation; Writing – original draft.
Xiangpan Kong: Data curation; Formal analysis; Software; Visualization.
Zhengxia Pan: Data curation; Formal analysis; Supervision.
Chun Wu: Resources; Software; Supervision.
Yonggang Li: Formal analysis; Resources; Software.
Gang Wang: Formal analysis; Software; Supervision.
Jiangtao Dai: Data curation; Formal analysis.
Dawei He: Data curation; Formal analysis; Resources.
Quan Wang: Conceptualization; Data curation; Formal analysis; Funding acquisition; Methodology; Resources; Software; Supervision; Visualization; Writing – original draft; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This study was supported by the youth programme of clinical medicine research of National Children’s health and disease clinical medicine research centre (No. NCRCCHD-2021-YP-17). This work is supported by the Extreme Smart Analysis platform (https://www.xsmartanalysis.com/).
The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Availability of data and materials: The dataset supporting the conclusion of this article is included in Raw-data.
References
- 1. Kelly RE, Goretsky MJ, Obermeyer R, et al. Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg 2010; 252: 1072–1081. [DOI] [PubMed] [Google Scholar]
- 2. Nuss D. Recent experiences with minimally invasive pectus excavatum repair ‘Nuss procedure’. Jpn J Thorac Cardiovasc Surg 2005; 53: 338–344. [DOI] [PubMed] [Google Scholar]
- 3. Kelly RE, Jr, Lawson ML, Paidas CN, et al. Pectus excavatum in a 112-year autopsy series: anatomic findings and the effect on survival. J Pediatr Surg 2005; 40: 1275–1278. [DOI] [PubMed] [Google Scholar]
- 4. Brungardt JG, Chizek PW, Schropp KP. Adult pectus excavatum repair: national outcomes of the Nuss and Ravitch procedures. J Thorac Dis 2021; 13: 1396–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. de Loos ER, Pennings AJ, van Roozendaal LM, et al. Nuss procedure for pectus excavatum: a comparison of complications between young and adult patients. Ann Thorac Surg 2021; 112: 905–911. [DOI] [PubMed] [Google Scholar]
- 6. Lomholt JJ, Jacobsen EB, Thastum M, et al. A prospective study on quality of life in youths after pectus excavatum correction. Ann Cardiothorac Surg 2016; 5: 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Steinmann C, Krille S, Mueller A, et al. Pectus excavatum and pectus carinatum patients suffer from lower quality of life and impaired body image: a control group comparison of psychological characteristics prior to surgical correction. Eur J Cardiothorac Surg 2011; 40: 1138–1145. [DOI] [PubMed] [Google Scholar]
- 8. Krille S, Müller A, Steinmann C, et al. Self- and social perception of physical appearance in chest wall deformity. Body Image 2012; 9: 246–252. [DOI] [PubMed] [Google Scholar]
- 9. Wang Q, Fan S, Wu C, et al. Changes in resting pulmonary function testing over time after the Nuss procedure: a systematic review and meta-analysis. J Pediatr Surg 2018; 53: 2299–2306. [DOI] [PubMed] [Google Scholar]
- 10. Jeong JY, Park HJ, Lee J, et al. Cardiac morphologic changes after the Nuss operation for correction of pectus excavatum. Ann Thorac Surg 2014; 97: 474–478. [DOI] [PubMed] [Google Scholar]
- 11. Li HJ, Wu C, Pan Z, et al. Behavioural disorders in children with pectus excavatum in China: a retrospective cohort study with propensity score matching and risk prediction model. Eur J Cardiothorac Surg 2019; 56: 596–603. [DOI] [PubMed] [Google Scholar]
- 12. Ji Y, Liu W, Chen S, et al. Assessment of psychosocial functioning and its risk factors in children with pectus excavatum. Health Qual Life Outcomes 2011; 9: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wada H, Kimura M, Shirahama R, et al. Pectus excavatum is associated with sleep-related breathing disorders in children. Eur Respir J 2019; 54: 1900524. [DOI] [PubMed] [Google Scholar]
- 14. Cheng YL, Lan CC, Wu YK, et al. Poorer sleep quality among adult patients with pectus excavatum in Taiwan: a pilot study. J Thorac Cardiovasc Surg 2019; 157: 769–780. [DOI] [PubMed] [Google Scholar]
- 15. Zhang X, Dimitriou D, Halstead EJ. Sleep, anxiety, and academic performance: a study of adolescents from public high schools in China. Front Psychol 2021; 12: 678839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013; 310: 2191–2194. [DOI] [PubMed] [Google Scholar]
- 17. Agha R, Abdall-Razak A, Crossley E, et al. STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int J Surg 2019; 72: 156–165. [DOI] [PubMed] [Google Scholar]
- 18. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014; 12: 1495–1499. [DOI] [PubMed] [Google Scholar]
- 19. Kelly RE., Jr. Pectus excavatum: historical background, clinical picture, preoperative evaluation and criteria for operation. Semin Pediatr Surg 2008; 17: 181–193. [DOI] [PubMed] [Google Scholar]
- 20. Xing W, long F, Qing Z, et al. Analysis of related factors affecting the academic performance of urban middle school students. Chin J Ment Health 2003; 17: 45–46, 44. (Chinese). [Google Scholar]
- 21. Lin L, Lu S, Zheng L, et al. Multivariate regression analysis of junior high school students with poor academic performance. Chin J Ment Health 2000; 14: 193–195 (Chinese). [Google Scholar]
- 22. Zhu L, Liming D. Diagnosis of pulmonary function. Chin J Tuberculosis Respir 2017; 35: 235–237. (Chinese) [Google Scholar]
- 23. Harder VS, Stuart EA, Anthony JC. Propensity score techniques and the assessment of measured covariate balance to test causal associations in psychological research. Psychol Methods 2010; 15: 234–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kelly RE, Jr, Cash TF, Shamberger RC, et al. Surgical repair of pectus excavatum markedly improves body image and perceived ability for physical activity: multicenter study. Pediatrics 2008; 122: 1218–1222. [DOI] [PubMed] [Google Scholar]
- 25. Zens TJ, Casar Berazaluce AM, Jenkins TM, et al. The severity of pectus excavatum defect is associated with impaired cardiopulmonary function. Ann Thorac Surg 2022; 114: 1015–1021. [DOI] [PubMed] [Google Scholar]
- 26. Chung JH, Park HJ, Kim KT. Scoliosis after pectus excavatum correction: does it improve or worsen? Eur J Cardiothorac Surg 2017; 52: 76–82. [DOI] [PubMed] [Google Scholar]
- 27. Shi R, Xie L, Chen G, et al. Surgical management of pectus excavatum in China: results of a survey amongst members of the Chinese Association of Thoracic Surgeons. Ann Transl Med 2019; 7: 202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Jacobsen EB, Thastum M, Jeppesen JH, et al. Health-related quality of life in children and adolescents undergoing surgery for pectus excavatum. Eur J Pediatr Surg 2010; 20: 85–91. [DOI] [PubMed] [Google Scholar]
- 29. Kelly RE, Jr, Obermeyer RJ, Goretsky M, et al. Recent modifications of the Nuss procedure: the pursuit of safety during the minimally invasive repair of pectus excavatum. Annals of Surgery 2022; 275: e496–e502. [DOI] [PubMed] [Google Scholar]
- 30. Frantz FW. Indications and guidelines for pectus excavatum repair. Curr Opin Pediatr 2011; 23: 486–491. [DOI] [PubMed] [Google Scholar]
- 31. Qiao G X M, Q Z, et al. Chinese experts’ consensus on surgical treatment of pectus excavatum. Chin J Pediatr Surg 2020; 1: 7–12 (Chinese). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-4-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-docx-5-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-tif-2-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
Supplemental material, sj-tif-3-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease
This article is distributed under the terms of the Creative Commons Attribution 4.0 License (http://www.creativecommons.org/licenses/by/4.0/) which permits any use, reproduction and distribution of the work without further permission provided the original work is attributed as specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
sj-xlsx-1-tar-10.1177_17534666231155779 for Academic performance in children with pectus excavatum: a real-world research with propensity score matching by Hongbo Li, Shulei Fan, Xiangpan Kong, Zhengxia Pan, Chun Wu, Yonggang Li, Gang Wang, Jiangtao Dai, Dawei He and Quan Wang in Therapeutic Advances in Respiratory Disease