Abstract
Due to the challenges and restrictions posed by COVID-19 pandemic, technology and digital solutions played an important role in the rendering of necessary healthcare services, notably in medical education and clinical care. The aim of this scoping review was to analyze and sum up the most recent developments in Virtual Reality (VR) use for therapeutic care and medical education, with a focus on training medical students and patients. We identified 3743 studies, of which 28 were ultimately selected for the review. The search strategy followed the most recent Preferred Reporting Items for Systematic Reviews and Meta-Analysis for scoping review (PRISMA-ScR) guidelines. 11 studies (39.3%) in the field of medical education assessed different domains, such as knowledge, skills, attitudes, confidence, self-efficacy, and empathy. 17 studies (60.7%) focused on clinical care, particularly in the areas of mental health, and rehabilitation. Among these, 13 studies also investigated user experiences and feasibility in addition to clinical outcomes. Overall, the findings of our review reported considerable improvements in terms of medical education and clinical care. VR systems were also found to be safe, engaging, and beneficial by the studies’ participants. There were huge variations in studies with respect to the study designs, VR contents, devices, evaluation methods, and treatment periods. In the future, studies may focus on creating definitive guidelines that can help in improving patient care further. Hence, there is an urgent need for researchers to collaborate with the VR industry and healthcare professionals to foster a better understanding of contents and simulation development.
Keywords: Virtual reality, healthcare, medical education, clinical care, treatment
Background
Since the inception of Virtual Reality (VR) in 1960s, where it was initiated for computer graphics, it has extended steadily to different disciplines—from gaming tools at homes to work-related tools for professionals and researchers.1 The remarkable progress of VR was observed in the past few decades when the industry pioneers like Google, Samsung, and Sony started making huge investments in this field and thousands of articles were published by the researchers from the interdisciplinary community.1 One of the industries where VR has made a significant impact is healthcare, where VR has proved its potential benefits in medical training, clinical evaluation, and healthcare care delivery.2–5 Due to the emergence of COVID-19 pandemic, the educators were looking for the alternate solutions for medical education and training instead of the traditional face-to-face teaching methods due to the social distancing restrictions. Given the lack of supervision and ideal practice situations, medical and healthcare trainees had few opportunities to practice vocational skills during their clinical rotations.6 At that time, the digital learning/e-learning solutions, such as VR, mobile learning, and digital skills trainers appeared to be the best solution in transforming face-to-face teaching to the digital education modalities.7 Similarly, in the clinical care settings, the risk of contamination and constrained access to healthcare resources made it difficult to provide patient care, such as hospitalizations and emergency services during the COVID-19 pandemic.8 In those scenarios, the latest VR technologies demonstrated their abilities to build effective therapeutic experiences for patients by offering safe and multi-modal simulations.9 Therefore, overall in the COVID-19 pandemic, medical institutions and hospitals observed great uplift in the implementation of latest VR technologies in order to train medical students for enhancing their technical skills and to support healthcare professionals in clinical care and crisis management.10,11
VR technologies can be categorized into three primary categories, namely fully immersive, semi-immersive, and non-immersive experiences.12 An immersive VR system projects the visual scene using VR headsets, head-mounted displays (HMDs), controller devices, motion detectors, or large projection surfaces so that users feel as if they had been transported into a virtual environment. Semi-immersive systems use 3D graphics with a high-performance computing system combined with a large monitor; while non-immersive VR system uses a monitor, keyboard, and mouse.12,13
VR simulations offer an environment where users can move around, interact with, and manipulate virtual objects, and see the results of their actions in real-time.14 Different strategies can be used in VR for medical education, including virtual patients and serious games. Interactive virtual simulations of actual clinical circumstances are known as VR patient simulations. Meanwhile, VR serious games combine gaming principles like varying degrees of difficulty, incentives, and feedback.15 Additionally, smartphones can also create VR visuals that can be seen using VR glasses equipped with sophisticated lenses.16 One benefit of adopting virtual reality to upgrade health professional skills is that it aids in overcoming obstacles including the lack of cadavers, concerns for patient safety, and resource and budget constraints.13 Furthermore, VR deployment enables unbiased and documented evaluations of user experience.17 VR-based education has been encouraging and beneficial for building confidence in abilities,17–20 self-efficacy,6,21 and knowledge and skill development.6,17,19,21–23 Moreover, VR provides a variety of other educational opportunities, including the development of nontechnical competencies, such as awareness and understanding, which are essential elements in developing empathy.24 Due to the increasing demand for distance learning brought on by the COVID-19 pandemic, the use of VR in healthcare education has never been more prevalent than now.
VR also has the potential to be a therapeutic tool.9 One of the main clinical applications of VR is to enhance mental health, such as alleviating pain during medical treatments,16,25 and decreasing stress,26 depression,27 and anxiety.16,25,28 VR has also demonstrated significant levels of effectiveness in rehabilitation programs, where the focus is on patient recovery, including motor performance29–35 and cognitive function rehabilitation.27,30,31,35 When completing certain therapeutic tasks in the virtual world, patients can engage with various sensory information from multiple modalities.8
Considering the wide range of VR simulations with the ability to enhance medical education and clinical care, it is time to identify research gaps that might be highly useful as a teaching tool for medical students in maintaining patient care. It will also be beneficial to study the influence of VR-based medical training and patient care in existing intervention studies.
Objectives
The aim of this scoping review was to present state-of-the-art developments in VR use, for medical education and therapeutic care, oriented towards training medical students and treating patients. This scoping review also aimed to identify any gaps in the existing literature and make recommendations for the future research. The objectives of our study are given below:
The primary objective was to evaluate the effectiveness of VR systems in terms of medical education training (knowledge, skills, attitude, confidence, and self-efficacy) and clinical care (rehabilitation and mental health).
The secondary objective was to evaluate the feasibility and acceptability of VR systems in medical education training and clinical care.
Methods
Search strategy
The search strategy followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for scoping review (PRISMA-ScR) guidelines.36 A comprehensive literature search was conducted to identify scientific studies that analysed VR-based training and interventions targeting to healthcare professionals and patients.
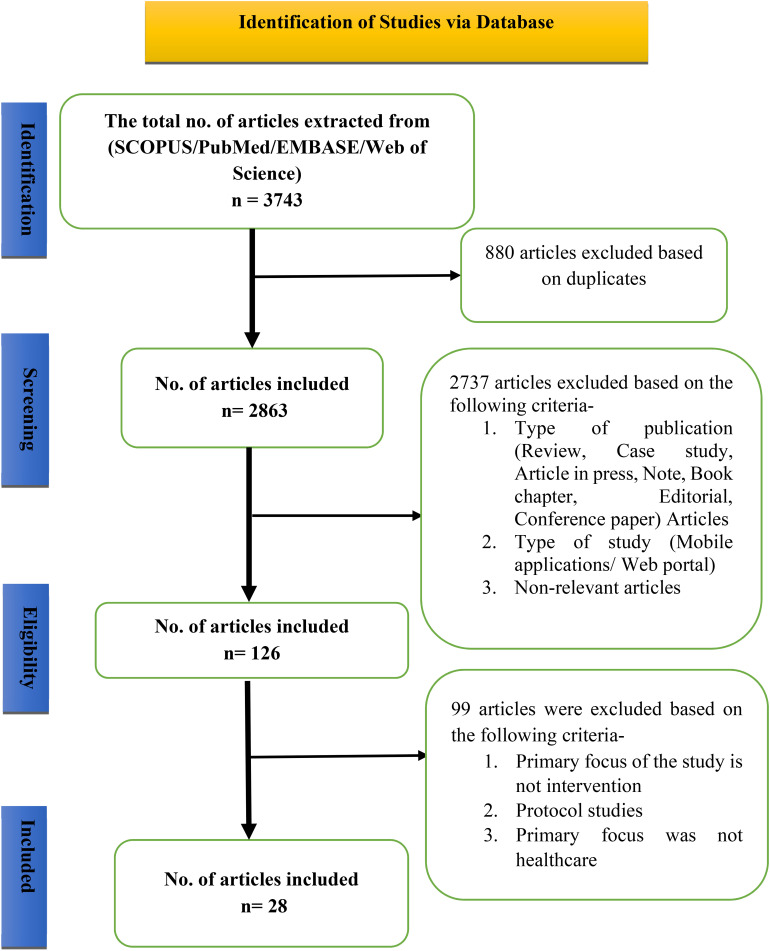
We searched for studies published between January 1, 2017, and March 18, 2022, in the PubMed, Scopus, Embase, and Web of Science electronic databases. The search for studies was conducted on March 18, 2022. Two of the authors of this study (ED and UP) independently reviewed the titles and abstracts of all search yields to identify eligible articles. If either reviewer thought an article was potentially significant, the complete text of the publication was retrieved. Furthermore, duplicate articles were removed. The authors used a preliminary search method based on medical subject heading (MeSH) terms and relevant publication text keywords that had been commonly used before. The following search terms were used: ‘Metaverse and Healthcare’ or ‘3D Modeling and Healthcare’ or ‘Virtual Reality and Healthcare’. The detailed search strategy and results are shown in Figure 1.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses extension for scoping review (PRISMA-ScR) flow chart of study identification and selection.
Eligibility criteria
We included original research articles that were published in English language and met the following criteria:
Focused on VR-based medical education training and interventions.
Included medical students/trainees/healthcare providers or patients undergoing VR simulation.
Used VR-based systems and devices like HMDs, motion tracking technology, VR glasses, VR robotics system, VR headsets, VR controllers, desktop computers, headphones, mobile devices, or any other types of VR tools for training and assessing health.
Included different immersion levels such as immersive VR systems, non-immersive VR systems, and semi-immersive VR systems.
Designed as a randomized controlled trial (RCT), clinical trial, quasi-experimental study, feasibility study, observational study, qualitative, randomized comparison/parallel group study, pre-post study, mixed methods, or pilot study.
We excluded studies based on the following criteria:
Focused on predicting any health issue.
Did not involve the use of VR devices or system.
The primary focus of study was not training or intervention in healthcare.
Focused on design, development, usefulness of a VR system.
Review articles, trial protocols, trial registrations, conference papers, book chapters, preprints, notes, brief reports, letters, editorials, or case studies or published in a language other than English.
Study selection and data extraction
On the basis of titles and abstracts, an initial screening was conducted. For all abstracts that initially fulfilled the inclusion criteria and articles that could not be rejected with certainty, the full text articles were obtained. The references of the studies that met the inclusion criteria were manually searched to identify additional relevant research articles. Two researchers independently reviewed the full text of articles and extracted the following data from each included article:
Characteristics of the study (authors, country of origin, publication year, study design, sample size and outcome measures, assessment tools, and results of the study).
Patient characteristics (target population and mean age).
Intervention characteristics (VR set-up, VR-type, and VR exposure–training or intervention duration).
Study focus (medical education training and clinical care). For this scoping review, the data on clinical outcomes of VR training and interventions were retrieved.
Clinical outcomes
The reported outcomes in this scoping review were categorized into two categories, namely medical education and therapeutic care. We collected data on the following primary outcomes to assess the effectiveness of VR as an educational tool: learners’ knowledge, skills, attitudes, confidence, and self-efficacy after the intervention. We also collected data on the following primary outcomes to assess the effectiveness of VR as a therapeutic treatment: patients’ clinical improvement in rehabilitation (motor/cognitive function) and mental health outcomes (skills, stress, anxiety, pain, depression, motivation, mood, and mentalization). All information was presented in a descriptive manner.
Feasibility and user experience
Secondary outcomes included in this review were assessed in terms of user experience, feasibility, acceptability, and adherence. These outcomes were assessed through personal interviews, feedback surveys, and drop-out rates.
Ethical considerations
This review did not require the approval of any national or institutional ethical committee.
Results
Study selection
In total, 3743 articles were retrieved from PubMed (n = 91), Embase (n = 790), Scopus (n = 2435), and Web of Science (n = 427). After removing duplicates, 2863 articles were evaluated. Finally, out of the 2863 articles, the full text of 126 relevant articles was reviewed. At this stage, articles were screened on the basis of their study characteristics, including the type of VR immersion and the primary focus of the study. The main reasons for exclusion are described in the methodology and presented in Figure 1. In total, 28 publications were ultimately included in this analysis.
Study characteristics
Of the selected 28 studies, four studies were conducted in the United States and United Kingdom each; three in Italy, Taiwan, and Korea; two in Australia and Canada; and one in Turkey, Germany, Mexico, Jordan, the Netherlands, Denmark, and China.
Among the 28 studies, eight were designed as RCTs, seven as pilot studies, four as feasibility studies (mixed methods study, pilot and feasibility study, and feasibility only study), two as quasi-experimental studies (pilot and pre-post), two as qualitative studies, one as an explorative pilot study as an RCT, one as an observational cross-sectional study, one as a single-blind randomized parallel-group study, one as a pre-post study, and one as a randomized comparison study, as described in Table 1.
Table 1.
Summary of the findings.
| Author, Year, Country | Study focus | Study design | Sample characteristic | VR set-up | VR type | VR exposure (training or intervention) |
|---|---|---|---|---|---|---|
| Chiang et. al., 202121 Taiwan |
Medical education training | Pre–post study | N = 60 (physicians, nurses, therapists) | VR HMD | Immersive | 2 h (120 min) |
| Hood et al., 202117 Australia |
Medical education training | Pilot study | N = 104 (specialists, nurses, radiographers) | VR HMD | Immersive | 21 min |
| Adhikari et al., 202118 UK |
Medical education training | Mixed-methods feasibility study | N = 19 (nursing students) | VR headset | Immersive | 20∼30 min |
| Andersen et al., 202122 Denmark | Medical education training | Explorative pilot study as an RCT | N = 19 (medical students) | VR HMD, controllers | Immersive | 20 min |
| Amini et al., 202137 USA |
Medical education training | Quasi-experimental (pilot study) | N = 27 (dental residents, faculty) | VR headset | Immersive | 30 min |
| Gunn et al., 202119 Australia |
Medical education training | Qualitative study | N = 66 (UG RT, MI students) | VR headset, controllers | Immersive | N/A |
| Mallik et al., 202120 UK |
Medical education training | Pilot study | N = 39 (junior doctors) | VR headset | Immersive | 15 min |
| Giordano et al., 202038 USA |
Medical education training | Quasi-experimental pre-post test pilot study | N = 50 (UG nursing science students) | Mobile VR headset (cardboard) | Immersive | 20 min |
| Slater et al., 201924 UK |
Medical education training | Qualitative study | N = 18 (carers, befrienders, senior management) | Simulation glasses, headphones, sensor gloves | Immersive | N/A |
| Hoogenes et al., 201723 Canada | Medical education training | Randomized comparison study | N = 39 (junior, senior medical trainees, surgical students) | Robotic dVSSS, dV-T simulator platform | Immersive | Average 2.5 h (150 min) |
| Chang et al., 20226 Taiwan |
Medical education training | RCT | N = 23 (medical students) | 3D VR glasses, motion sensor, 3D VR controller (CAVE VR system) | Immersive | 3 sessions/week for 2 weeks and each session was for 2 h (total 12 h or 720 min) |
| Mrakic-Sposta et al., 201839 Italy | Clinical care | Pilot study | N = 10 (MCI patients); mean age 73.3 years | Cycle-ergometer, smart garment, finger touch projector, PlayStation controller | Immersive | 3 sessions/week for 6 weeks (total 18 sessions) and each session was 40∼45 min |
| Thapa et al., 202030 Korea |
Clinical care | RCT | N = 68 (MCI patients); mean age 72.5 years | VR headset, hand controllers | Immersive | 3 sessions/week for 8 weeks; total duration was 100 min (three 20-min VR training sessions, and three 10-min eye relaxation) |
| De Luca et al., 201731 Italy |
Clinical care | Pilot study | N = 12 (post-stroke patients); mean age 40 years | BTs-nirvana | Semi-immersive | 3 sessions/week for 8 weeks; each session lasted 45 min |
| Bergmann et al., 201829 Germany | Clinical care | Pilot RCT (2 parallel groups) | N = 20 (subacute stroke patients); mean age 64 years | Display screens, robotic-assisted devices | Semi-immersive | 12 sessions (for 4 weeks) |
| Lee et al., 202027 Korea |
Clinical care | RCT | N = 22 (sub-acute stroke patients); mean age 58.18 years | Cognitive rehabilitation training system (Moto Cog) | Semi-immersive | 5 sessions/week for 4 weeks; each session was 30 min/day |
| Al-Sharman et al., 201932 Jordan | Clinical care | Observational cross-sectional study | N = 40; (20 MS patients and 20 controls); mean age 34.7 years | Nintendo Wii Plus, balance board, LCD monitor | Non-immersive VR | 6 weeks; every day 10-min game session |
| Pot-Kolder et al., 201825 Netherlands | Clinical care | RCT | N = 116 (patients suffering from a psychotic disorder) | HMD | Immersive | Total 16 sessions over 8–12 weeks; session lasted 1 h, 40 min |
| Falconer et al., 201743 UK | Clinical care | Mixed-methods, feasibility and acceptability study | N = 15 (patients with BPD); mean age 31.2 years | Desktop, mouse, keyboard | Non-immersive VR | 45–60 min for 2–3 days per week; for whole treatment |
| Yeh et al., 201733 Taiwan |
Clinical care | Feasibility study | N = 16 (stroke patients) | 3D game engine unity™ | Semi-immersive | 3 sessions/week for 8 weeks; each session was 30 min |
| Buccellato et al., 202042 US | Clinical care | Feasibility trial and pilot study | N = 21 (participants with ABI); mean age 41 years | Computer and monitor, wireless headphones, remote server, bimanual game controllers | Semi-immersive | 6 weeks |
| Mekbib et al., 202134 China | Clinical care | Single blind, randomized, parallel-group study | N = 23 (stroke patients); mean age 56.5 years | HMD, tracking device, link box | Immersive | 4 sessions/week for 2 weeks; each session for 1 h |
| Jonsdottir et al., 202135 Italy | Clinical care | Pilot study | N = 34 (chronic stroke patients); mean age 55 years | Television screen, motion sensors | Semi-immersive | Clinic HEAD: 3 sessions/week for 4 weeks, each 45 min (total 12 sessions) and Home HEAD: 5 sessions/week for 12 weeks (total 60 sessions) |
| Beverly et al., 202226 USA | Clinical care | Pilot study | N = 90 (HCPs suffering from stress); mean age 29.5 years | HMD | Immersive | 3-min 360° Cine-VR session |
| Mosso Vázquez et al., 201840 Mexico | Clinical care | Pilot study (randomized) | N = 44 (patients needing lipoma resection) | VR 3D glasses, HMD, phone (with Google Cardboard headset) | Immersive | Session lasted for 30 min after surgery |
| Ryu et al., 201828 Korea | Clinical care | RCT | N = 69; (undergoing general anesthesia/elective surgery); mean age 7 years | HMD, saturation monitor, hand and finger motion controller, leap motion controller | Immersive | Session was for 5 min |
| Osmanlliu et al., 202041 Canada | Clinical care | Pilot RCT | N = 62 (undergoing IV procedure); mean age 11.7 years | HMD | Immersive | Throughout the IV procedure |
| Karaman et al., 202116 Turkey | Clinical care | RCT | N = 60 (during breast biopsy); mean age 43.5 years | Smartphone, 3D VR Player app, VR Box Glasses | Immersive | Throughout the breast biopsy |
UG, undergraduate; RT, radiotherapy; MI, medical imaging; RCT, randomized controlled trial; dVSSS,da Vinci surgical skills simulator; dVT,da Vinci trainer; CAVE, Cave automatic virtual environment; MCI, mild cognitive impairment; MS, multiple sclerosis; BPD, borderline personality disorder; ABI, acquired brain injury; HCPs, healthcare professionals; HEAD, Human Empowerment Aging and Disability; IV, intravenous.
Characteristics of the intervention
VR type
The majority of the research included modalities that were fully immersive (20/28, 71.42%) followed by semi-immersive (6/28, 21.42%) and non-immersive (2/28, 7.142%). A fully immersive virtual technology provides users with a realistic experience within the virtual world by utilizing VR equipment, such as HMDs, headsets, 3D glasses, and motion sensors. The VR technology gives them the impression that they are in person in a virtual environment and that everything is occurring to them in real-time. Semi-immersive VR depends on powerful processors with cutting-edge 3D graphics. This innovation uses a computer, controllers, or a room specifically designed for this technology to partially imitate the operation of real-world mechanisms. With non-immersive VR, users could access a virtual space through a computer and controllers to control certain characters or activities inside without really interacting with the surrounding environment.
VR exposure/duration
Our review indicated that the average period of training medical groups using virtual reality was between one session (15 min) and six sessions (12 h) (see Table 1). The VR intervention period for clinical care varied from one session (3 min) to 60 sessions (45 h).
VR systems/tools
Many VR tasks were conducted using Windows operating systems that provide a platform, in which the user appears to enter into an interactive 3D virtual world; virtual environments with vehicle and sound systems that simulate motion in the virtual world; simulator tasks practiced on a 3D-printed model; cave automatic virtual environment (CAVE) systems in which one enters a room where they are surrounded by large screens that project a nearly continuous virtual space; VR training games using VR headsets and controllers; a simple desktop with mouse and keyboard; and a phone (with a Google cardboard headset). Studies also included interactive and tracking tools, such as VR glasses, sensor gloves, and leap motion sensors in addition to HMDs.
VR content
The VR content used for medical education varied greatly depending on the scope of the research, and type of education and learning. The majority of studies used virtual scenarios to give VR training by simulating the actual tasks or workflow processes.6,17,19–21,23,37 Three studies incorporated pre-recorded videos for training purposes.22,37,38 Two studies used experiential learning to help medical professionals understand the difficulties that patients faced, such as language barriers, cultural barriers, financial limits, or the impact of the disease.24,37 Two studies provided additional web-based VR materials or resources to participants.17,21
The majority of studies for clinical care were primarily focused on providing patients with virtual environments in which they were required to execute physical or mental tasks and activities.6,25,29,31,33–35,39 Four studies explored virtual nature experiences as relaxation or distraction therapies for stress and pain management.16,26,40 Four studies employed VR-based games as rehabilitation interventions (motor and cognitive functions).28,32,41,42 There was only one study that used VR to build a virtual world where patients could think about outside events and internal feelings.43
Characteristics of research participants
The studies addressed two target populations: medical students and the patients. 11 of the 28 studies focused on teaching medical professionals, while the remaining 17 focused on treating the patients. Numbers of participants in the studies ranged from 10 to 116 (see Table 1). Medical professionals comprised of undergraduate medical students, pre-registered nurses, therapists, radiographers, dental residents/faculty, junior trainees, senior trainees, senior management staff, and surgical students. Patients included for therapeutic treatment in the trials were dealing with stress, psychotic disorders, borderline personality disorder (BPD), stroke (sub-acute, chronic, and post-stroke), multiple sclerosis, acquired brain injury, and preoperative anxiety. In addition to these, there were participants who were undergoing a breast biopsy, anesthesia, and IV treatment.
Assessment tools
The research covered in this scoping review included subjective self-reported questionnaires, clinical test batteries, task performance tests, interviews, and VR tools or systems to assess medical students’ learning and patients’ healthcare outcomes. Written materials, like multiple-choice tests, were also used to determine what a student learned. A tool called Kirkpatrick's model was also utilized for evaluating the training programs.
Major study focus
The focus of our review was assessing the role of VR mainly in clinical care and medical training. The selected studies explored knowledge, skills, confidence, self-efficacy, learning efficacy, attitudes, and empathy as outcome measures in medical education training. The outcome measures for therapeutic care research included cognitive functioning, motor performance, depression, motivation, walking function, anxiety, paranoia, behavioral function, stress, pain distraction, social participation, mentalization, and mood (see Tables 2 and 3).
Table 2.
Virtual reality (VR) used as a medical education tool.
| Citations | Outcome measures | Assessment tools | Results |
|---|---|---|---|
| Chiang et. al., 202121 | Knowledge, care skills, and self-efficacy | Questionnaire and written/knowledge test | Increased trainees’ familiarity, enhanced their confidence, and decreased their anxiety with respect to tracheostomy-related knowledge and care skills. |
| Hood et al., 202117 | Knowledge, skills, and confidence | Questionnaire | Increased confidence in their ability to make improvements in stroke management. |
| Adhikari et al., 202118 | Knowledge, skills, and confidence | Questionnaire and interview | Improved confidence and anxiety post-intervention. |
| Andersen et al., 202122 | Skills (procedural) and learning efficacy (knowledge) | Skill/task test | Successful cannulation (skills) was significantly higher in the intervention group. |
| Amini et al., 202137 | Empathy (KSA) | Kirkpatrick's model, a quiz, and questionnaires | There was no significant difference in cognitive, affective or skill-based learning immediately post-training. |
| Gunn et al., 202119 | Skill acquisition and confidence | Questionnaire | Increased perceived confidence for performing CT scans. |
| Mallik et al., 202120 | Confidence | Questionnaire and Kirkpatrick's model for evaluating training programs | Increase confidence in managing diabetic emergencies. |
| Giordano et al., 202038 | Knowledge and attitudes | Questionnaires | There was no difference in knowledge or attitudes post-intervention. |
| Slater et al., 201924 | Empathy | Face-to-face and telephonic interviews | More awareness and greater appreciation of the effect of the environment upon dementia patients. |
| Hoogenes et al., 201723 | Knowledge and skills | Task performed (assessed automatically via robotic VR system) | Training with dVSSS over the dV-T showed improvement in junior trainees compared to seniors and medical students. |
| Chang et al., 20226 | Knowledge, attitudes, and self-efficacy | Questionnaire | Improved students’ oral care-related knowledge, attitudes, and self-efficacy. |
KSA, Knowledge Skills Attitude; CT, computed tomography; dVSSS, da Vinci surgical skills simulator; dVT, da Vinci trainer.
Table 3.
Virtual reality (VR) as a therapeutic tool.
| Citations | Outcome measures | Assessment tools | Results |
|---|---|---|---|
| Mrakic-Sposta et al., 201839 | Cognitive functions and oxidative stress | Neuropsychological test battery | No statistical difference was observed between the control and intervention groups. |
| Thapa et al., 202030 | Cognitive and physical functions | Questionnaires and functional task tests |
Improved cognitive and physical functions in MCI patients. |
| De Luca et al., 201731 | Cognitive and motor functions | Clinical-psychometric battery and questionnaires | Improved motor performance and cognitive functions. |
| Bergmann et al., 201829 | Motor performance (walking function) and motivation | Questionnaire and walking time evaluated during physiotherapy session | Enhanced motivation and walking time among patients. |
| Lee et al.,202027 | Cognitive function, motivation, and depression | Questionnaires | Improved cognitive function, rehabilitation motivation, and depression. |
| Al-Sharman et al., 201932 | Motor skill performance (cognitive and fatigue) | Questionnaires and VR game system (time to complete and errors) | Significant improvement was observed in motor skill performance. |
| Pot-Kolder et al., 201825 | Paranoia, momentary anxiety, and social participation | Questionnaires and social participation (time spent with others) | No significant improvement in social participation; but momentary paranoia and anxiety reduced post-treatment. |
| Falconer et al., 201743 | Mentalization and mood | Questionnaire and interview | No improvement in self-report measures. |
| Yeh et al., 201733 | Motor functions (upper extremity) | Questionnaires and task-oriented assessment | Effectively promoted motor function recovery. |
| Buccellato et al., 202042 | Cognitive, motor, and behavioral functioning | Questionnaires and task-oriented assessment | There was no significant improvement in cognitive, motor, or behavioral functioning. |
| Mekbib et al., 202134 | Motor functions (upper extremity) | Questionnaires and task-oriented assessment (via a VR system) | Reduced UE motor impairments and increased independence in ADLs. |
| Jonsdottir et al., 202135 | Physical activity, functional mobility, and cognitive abilities | Questionnaires and 2-min walking test | Motor and cognitive ability improved in both phases (clinic and home). |
| Beverly et al., 202226 | Subjective stress | Questionnaire | Effectively reduced stress. |
| Mosso Vázquez et al., 201840 | Pain distraction | Questionnaires and vital signs | VR devices (HMD and mobile) effectively reduced pain during ambulatory surgery. |
| Ryu et al., 201828 | Preoperative anxiety | Questionnaire | Reduced preoperative anxiety. |
| Osmanlliu et al., 202041 | Procedural pain and distress | Questionnaires | No significant improvement in pain or distress during an IV procedure. |
| 16 | Pain and state-trait anxiety | Questionnaires | Significant improvement in the reduction of pain and anxiety. |
MCI, mild cognitive impairment; HMD, head-mounted display; UE, upper extremity; ADLs, activities of daily living.
Effectiveness of VR training and intervention on clinical outcomes
Medical education teaching/training
Knowledge
In total, six studies assessed knowledge as an outcome.6,17,18,21,23,38 Five studies showed a significant increase in knowledge acquisition from pre- to post-VR training. The results showed that those who underwent VR simulation training had an improvement in tracheostomy-related knowledge and care skills, stroke management, pneumonia with sepsis management, surgical expertise for a urethrovesical anastomosis task, and oral care-related knowledge in the care of elderly people with disabilities. However, one study by Giordano et al.38 did not show a significant difference between the student's knowledge retention about opioid-related overdoses when administering intranasal naloxone compared to individuals participating in standard education.
Learning efficacy
One study focused on learning efficacy.22 The VR-based training simulation centered on tip tracking abilities in order to improve medical students’ learning efficacy in placing peripheral venous cannulas. The VR group had a considerably higher proportion of successful cannula emplacements.
Skills
Six studies, in total, evaluated skills as an outcome.17–19,21–23 The results showed that those trained with a VR simulation exhibited improved tracheostomy care skills, optimal stroke workflow processes, decision-making competency in managing pneumonia with sepsis, ultrasound-guided peripheral venous catheter placement, computed tomography (CT) scanning skills, and acquisition of surgical skills for a urethrovesical anastomosis task.
Confidence
Four studies focused on the effectiveness of VR simulation on learners’ self-confidence.17–20 According to all trials, VR education significantly increased confidence in learners’ ability to make improvements in stroke management, dealing with sepsis patients, clinical CT confidence, and managing diabetic emergencies.
Attitudes
Two studies investigated attitudes as an outcome.6,38 One of them discovered similar attitudes toward dealing with opioid overdoses and delivering emergency medical care as compared to the learners participating in conventional training.38 On the other hand, a study by Chang et al.6 managed to improve oral care-related attitudes in medical students. Those students successfully simulated treating senior citizens with various physical and oral ailments using virtual settings, and they used appropriate oral-care techniques for each situation.
Empathy
Two studies assessed empathy as an outcome.24,37 The study by Slater and colleagues24 enabled the emotive, moral, and cognitive components of empathy and helped to educate healthcare professionals about the realities of a person with dementia. Ultimately, the experiential education program was considered effective. Emotionally, it gave participants the chance to understand what it is like to live with dementia, which improved their capacity for empathy. The results of the other trial37 indicated immediate post-training improvements in dental care delivery and patient relationships. However, there was no notable difference between skills assessed just after training and in the survey administered one month later.
Self-efficacy
The impact of VR education on self-efficacy was examined in two trials.6,21 Both studies showed a significant trend of improvement in self-efficacy for tracheostomy care skills and oral healthcare behavior among healthcare professionals.
Clinical care
Rehabilitation
Motor performance
Eight rehabilitation studies focused primarily on VR-based therapy and analyzed their impact on motor performance.29–35,42 Seven VR-based training programs improved patients’ physical abilities, including fine motor recovery, upper extremity, dexterity functions, gait resistance/speed, balance, gripping, mobility, walking time, and the extent to which they could independently carry out daily activities. Although one trial failed to reach statistical significance, it demonstrated the VR system's potential to increase the access to care.42
Cognitive functioning
Six rehabilitation studies investigated the effects of VR-based treatment on cognitive functioning.27,30,31,35,39,42 Four of six trials reported successful improvement in different domains of cognition, including patients’ attention, executive function, memory, processing speed, and awareness.27,30,31,35
Mental health
Anxiety
Three studies assessed anxiety as an outcome.16,25,28 One study employed VR-based relaxation and distraction therapy that managed to lower anxiety in patients undergoing a biopsy.16 Another study utilized VR-based gaming and successfully reduced anxiety in kids receiving anesthesia.28 Cognitive behavior therapy (CBT) was also conducted via VR in patients suffering from a psychotic illness. The treatment was effective in reducing paranoia and momentary anxiety. However, the therapy was unable to promote social participation, which they defined as the duration of time spent with other people in one of the studies.25
Pain
The impact of VR therapy on pain was examined in three trials.16,40,41 Two out of three trials demonstrated a positive effect of VR on pain management.16,40 While, in contrast, the third one—Osmanlliu et al.41 found no significant difference in levels of pain during an intravenous (IV) procedure, which was the main clinical outcome. However, in this study VR-based treatment proved to be a feasible and acceptable treatment.
Stress
Two studies investigated distress as an outcome.26,41 Beverly et al.26 reported that presenting tranquil CINEVR as an intervention had a significant influence on the psychological stress of participants (who were frontline healthcare professionals in COVID-19 treatment facilities). The other study showed no significant improvement in stress reduction.41
Motivation
Two studies assessed motivation as an outcome.27,29 According to one study,29 VR therapy was well-received and boosted patients’ motivation to walk for longer periods of time. The other study27 demonstrated the effectiveness of VR-based cognitive training on participants’ motivation for rehabilitation.
Depression
A study conducted by Lee et al.27 focused on depression as a clinical outcome. The VR cognitive rehabilitation training program significantly improved symptoms of depression.
Mentalization and mood
Only one study evaluated mentalization and mood as part of the treatment of BPD.43 However, no changes in self-reported measures of mentalization or mood were observed in the trial. The symptoms did not worsen as measured by a subjective questionnaire.
Feasibility and user experience
In our review, 13 studies assessed the feasibility and user experience in addition to clinical outcomes (see Table 4). Five studies explored the feasibility and acceptability of VR systems via qualitative interviews or paper-based questionnaires or surveys.18,29,35,43 All reported studies showed positive responses to VR intervention/training with high acceptability and feasibility. Participants found the VR systems to be useful and engaging. In addition to these studies, two studies investigated the feasibility as their primary outcome.20,42 Self-reported questionnaires and surveys were used to assess the feasibility of using this system in clinical trials. Six studies assessed user experience or feedback to the VR systems via interviews, questionnaires, or surveys.6,17,19,21,33,37 The feedback from participants was positive, insightful, and constructive; and they considered VR to be accessible, pleasurable, and effective. Two studies used the criteria of the dropout rate (adherence) to evaluate the feasibility and showed good adherence.29,35
Table 4.
Assessment of virtual reality (VR) feasibility and user experience.
| Citations | Focus | Assessment method | Results |
|---|---|---|---|
| Chiang et al., 202121 | User feedback | Open-ended questions | VR system significantly motivated learners: trainees gave positive feedback. |
| Hood et al., 202117 | Usability and acceptability | VR user survey feedback | Feedback was constructive and useful. VR was convenient, enjoyable, and accessible. |
| Adhikari et al., 202118 | Feasibility (acceptability and applicability) | Qualitative feedback (one-to-one interviews) | VR system was useful, appropriate, and relevant for nursing education. |
| Amini et al., 202137 | User feedback | Qualitative feedback (One-to-one interviews) | Feedback provided ways to improve the training application and to support extending the virtual training format beyond technical skills. |
| Gunn et al., 202119 | User experience | Qualitative feedback (survey) | Showed positive responses to perceived usefulness, ease of use, and enjoyment. |
| Mallik et al., 202120 | Feasibility | E-survey (feedback) | The study delivered effective VR training for clinicians. |
| Chang et al., 20226 | User feedback | Satisfaction survey | Students were satisfied with the system. The VR-based training system was easy to use. |
| Bergmann et al., 201829 | Feasibility and acceptability | Dropout rate and questionnaire (about the VR scenarios) | Showed high acceptability and a low drop-out rate. |
| Falconer et al., 201743 | Feasibility and acceptability | Qualitative feedback (interviews) | Positive response to the VR intervention. All participants wanted to continue with VR therapy. |
| Yeh et al., 2017 33 | Usability of the VR system | Questionnaire | Participants considered the system to be useful, playful, easy to use, and wanted to continue using the VR system. |
| Buccellato et al., 202042 | Feasibility | Feedback form (questionnaires) | High system enjoyment and usability. |
| Jonsdottir et al., 202135 | Feasibility and acceptability | Adherence and usability satisfaction scale (questionnaire) | Results showed high level of usability. Adherence was good. |
| Osmanlliu et al., 202041 | Feasibility and acceptability | Recruitment rate and satisfaction survey | Recruitment rate was slightly lower (78.7%) than the expected threshold (80%); the VR intervention was feasible and acceptable. |
Discussion
Focus of study
The aim of this scoping review was to investigate the existing literature on the use of VR for training medical students, supporting clinical care provided by healthcare professionals and interventions for the patients. 28 VR-based studies were reviewed to determine the effectiveness of VR training and interventions on medical professionals and patients. Despite the wide variety of studies considered for our review, outcomes showed that VR-based training and interventions were beneficial and well-received.
We initially found 3743 studies using our search strategy, out of which 28 were ultimately included in this scoping review. The included studies comprised of RCTs (28.6%), feasibility studies (14%), and pilot studies (25%), while the remaining 32.4% studies comprised of qualitative, observational, and randomized parallel and group studies. Sample sizes ranged between 10 and 116. VR systems and tools were employed in all of the trials, as well as subjective questionnaires, task performance tests, and interviews. The intervention duration varied from one to 60 sessions. Furthermore, 60.7% of studies in the review evaluated individuals seeking therapeutic treatment, while 39.3% focused on training medical students and professionals. In our review, clinical outcomes were divided into two categories: medical education and therapeutic treatment. 11 of the 28 studies were classified as medical education-based trials, while the remaining 17 were identified as clinical care-based trials. Of the 28 studies, 22 reportedly improved clinical outcomes. In nine of 11 trials, VR training enhanced knowledge, skills, competency (confidence, attitudes, and self-efficacy), and empathy of medical trainees. Only two of 11 (18%) trials that investigated the impact of VR training for educational purposes found no significant difference in clinical outcomes. Our findings are consistent with a review,44 that found evidence of improvements in knowledge and skills among participants using VR interventions compared to those participating in traditional digital learning methods. Inconclusive results were found for attitudes and satisfaction outcomes, although none of the studies included in their review reported any patient-related outcomes or behavioral changes in either patients or students.
In 14 of 17 trials, VR training was effective in providing rehabilitation therapy (cognitive and motor rehabilitation) and improving mental health outcomes (stress, anxiety, depression, pain, mentalization, and mood) in patients. Only four of 17 (23.5%) trials that investigated the effectiveness of VR intervention in delivering therapeutic treatment reported no substantial improvement. Our findings were similar to other reviews where effects of virtual training helped patients in their health outcomes.45,46
Both RCTs and trials using a pre-test/post-test design were included in our review. Since there is a vast amount of quantitative study literature, it can be implied that virtual simulation was a helpful tool for participants (medical professionals and patients) to learn and experience fewer symptoms during clinical trials.
Our review reported that the duration of the research (in weeks or sessions) had no effect on the effectiveness of the majority of outcome measures. However, in studies exploring medical education learning,17–24,37,38 all training were scheduled within a single session and lasted from 15 min to a maximum of 2.5 h. Only one research focusing on medical education carried out six therapy sessions of 720 min.6 Therefore, it still needs to be seen whether long-term VR training can result in more-productive learning and improved functional results. Meanwhile, studies focusing on clinical care16,25–35,39–43 indicated a wide range of treatment durations (rehabilitation and mental health). Both long-term treatment with 60 sessions 35 and short-term treatment of one session26 were found to be effective in our review. Unfortunately, there was no consensus or standardization of the optimal duration of VR treatment sessions.
Despite the positive VR outcomes, one study26 in our review did state that the length, number of sessions, and setting of many VR therapies may be significant hurdles to VR interventions. They concluded that in order to meet the demands of participants, particularly frontline healthcare professionals, VR treatments in the future must be fast and easy to access.
In our review, VR technologies were classified into three broad categories: non-immersive, semi-immersive, and fully immersive. Immersion is an essential element of VR study since it affects users’ experiences and their feeling of involvement.47 The level of immersion may potentially have an effect on the effectiveness of VR-based therapy.48,49 Our findings are consistent with these studies, as 16 of the 20 trials included in our review used immersive technology and demonstrated significant improvements in training and clinical care.
Of the studies included in the review, 46% assessed feasibility and user experiences in addition to clinical outcomes. The qualitative analysis emphasized how highly engaged and perceptive the learners were, which motivated them to continue using VR for training or treatment purposes.
Though, there was a lack of guidance on how to conduct usability tests for VR health interventions, but patients’ acceptability and users’ feedback are crucial factors to take into account because they indicate whether or not users will use/adopt a technology in the future.42,50 Overall, patients and healthcare providers seemed to be satisfied with the VR experience and indicated that they would like to use this technology (VR) in the future as well. Recently, one study did attempt to create a summary of evaluation approaches in order to provide developers and researchers with an understanding of key factors to consider when integrating VR, allowing them to make continual improvements prior to clinical use.50
Future of VR
In the near future, it is possible that VR might be used to provide standardized clinical training in therapeutic settings. But in order to succeed in that, it must be decided which devices or tools best meet the requirements of both patients and therapists. The use of VR in various clinical contexts would necessitate further investigations in this regard in future.51 The need for collaboration with software developers, clinical users, therapists, and researchers is indeed significant.51,52
Our review supports the role of VR technologies in the terms of medical education and clinical care among the healthcare professionals, students, and patients. A recent review literature also highlights the benefits of VR technology for patients’ education and treatment.53 In contrast to this review, our study found that 75% of the total included articles reported improvements in patient care. Besides this, our study also assessed the user experience along with the effectiveness of VR on outcome measures.
Our results are in agreement with those of previously published review studies ,7,54–57 showing the positive effects of VR. A review conducted by Jiang et al.7 focused on the diverse applications of VR in medical education. In terms of outcomes, our findings are comparable to those of this study, including surgical abilities, anatomical skills, clinical knowledge, and clinical scenario management. Additionally, our review also categorized different VR modalities based on the level of immersion. The primary difference was that we made an attempt to assess the effects of VR-based education on participants learning skills.
The findings of our review have been mirrored in other literature,54,55 showing the positive effects of VR in terms of clinical care for pain and anxiety. The results of other studies by Afsoon Asadjadeh et al.56 and Omar Mubin et al.57 also support the findings of our review, showing that VR rehabilitation has a considerable favorable impact on motor function and cognitive impairment.
Impact of COVID-19
During the COVID-19 pandemic, VR simulation training proved to be crucial in rendering healthcare services, improving both operational and clinical care.58 According to Michael Co et al.,59 web-based surgical skills learning (WSSL) can be a feasible alternative to face-to-face surgical skills teaching. Another study with similar conclusions claims that VR skill training is a beneficial substitute for traditional methods of learning for surgical residents.60 Technologies for remote communication are being explored as prospective options for supporting medical treatments for rehabilitation.61,62 Thus, given the current scenario, immediate action in the healthcare delivery system is needed to address challenges post COVID-19 pandemic. During this period, medical facilities were temporarily shut down, and patients with other conditions received much less attention.63 However, it also paved the way for the employment of digital technology in the provision of medical treatment and education. As educators throughout the world struggle with how to continue offering education, many institutions now use pre-recorded or live videoconferencing services.63 Prior to COVID-19, only 10 studies were published that focused on the application of virtual reality in medicine. During and post COVID-19, we found 18 studies were conducted in 2.5 years and the number is continuously rising. One of the studies included in our review looked into the use of virtual reality (VR) to reduce stress and anxiety among COVID-19 frontline health professionals.26 This study demonstrated its effectiveness.
Strengths
Our scoping review is the first of its kind to focus on patient care, which involved both medical education for students and therapeutic treatment of patients. In addition, the review examined studies using different VR modalities, such as semi-immersive, non-immersive, and immersive technologies. The majority of the studies showed an improvement in outcome measures in both patient care domains. Certain studies not only investigated improvements in learners’ abilities or patients’ clinical outcomes but also the users’ experiences and feasibility of using VR systems. The findings implied that VR system was safe, entertaining, and effective for the participants. Despite the benefits of using VR technology in health care, there were various limitations in our review, as described below.
Limitations
The major limitation of this scoping review was that we were unable to conduct a meta-analysis or systematic review due to numerous variations in the study designs and clinical outcomes. As a result, we conducted a scoping review and presented a tabulated analysis of the studies. The wide heterogeneity in study designs, outcome measures, types of VR (devices, immersion levels, contents, and durations), and evaluation methodologies also made reliable comparisons challenging. One aspect that stood out was the lack of continuous monitoring of the level of immersion, which might have an effect on outcome measures. Moreover, many of the included studies had small sample sizes, which makes it difficult to generalize the findings. Thus, large intervention studies with big sample sizes are required for a greater understanding of VR and its implications in the future. In order to effectively sustain the long-term impacts of VR interventions, much rigorous research is required, particularly in the case of therapeutic care where rehabilitation and recovery are long processes that can last for a lifetime.
Conclusions
Healthcare professionals are using VR to provide improved care for patients and better training for doctors and medical students. The literature reflects the popularity of VR as a tool for teaching medical students as well as for managing health and rehabilitation in patients with a variety of medical conditions. Nine out of eleven medical education-based studies have shown the positive outcomes in terms of knowledge, skills, confidence, and empathy. Besides this, VR has emerged as a promising tool for clinical care of patients. 13 out of 17 clinical care-based studies have revealed positive outcomes in rehabilitation programs and mental health. In the near future, more studies should compare intervention groups to control groups to ascertain whether VR therapies are superior or more effective. We also recommend a thorough examination of how levels of immersion affect the treatment response. Future research should also emphasize on establishing the standards that explicitly describe VR procedures with regard to immersion levels, study designs, VR contents, and intervention treatment periods. Hence, there is an urgent need for a collaboration between the VR simulation industries and healthcare professionals for more effective and specific VR contents development. Finally, more exploration is required to determine the feasibility and user experience of VR in health care among healthcare professionals and the patients.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This study is partially funded by European Union's funded H2020, iHelp project under the grant agreement (GA: 101017441) and MOST, Taiwan: 110-2923-E038- 001-MY3
Consent for publication: All authors have given their consent to publish the article.
Guarantor: Prof. Dr Shabbir Syed-Abdul
Author's contribution: SSA, have designed the study conception idea for publication. ED, UU, YH and MU have written the manuscript of an article. SSA, ED, UU, MU, GM, DK, YH, HA and UW have done the final editing of the manuscript.
ORCID iDs: Eshita Dhar https://orcid.org/0000-0001-6055-2593
Umashankar Upadhyay https://orcid.org/0000-0002-2581-8007
Dimosthenis Kyriazis https://orcid.org/0000-0001-7019-7214
Shabbir Syed Abdul https://orcid.org/0000-0002-0412-767X
References
- 1.Cipresso P, Giglioli IAC, Raya MA, et al. The past, present, and future of virtual and augmented reality research: a network and cluster analysis of the literature. Front Psychol 2018; 9: 2086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scalese RJ, Obeso VT, Issenberg SB. Simulation technology for skills training and competency assessment in medical education. J Gen Intern Med 2008; 23: 46–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zackoff MW, Young D, Sahay RD, et al. Establishing objective measures of clinical competence in undergraduate medical education through immersive virtual reality. Acad Pediatr 2021; 21: 575–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiederhold BK. The potential for virtual reality to improve health care. The Virtual Reality Medical Center 2006.
- 5.Bui J, Luauté J, Farnè A. Enhancing upper limb rehabilitation of stroke patients with virtual reality: a mini review. Frontiers in Virtual Reality 2021; 2: 595771. [Google Scholar]
- 6.Chang A-H, Lin P-C, Lin P-C, et al. Effectiveness of virtual reality-based training on oral healthcare for disabled elderly persons: a randomized controlled trial. J Pers Med 2022; 12: 218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jiang H, Vimalesvaran S, Wang JK, et al. Virtual reality in medical students’ education: scoping review. JMIR medical Education 2022; 8: e34860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matamala-Gomez M, Bottiroli S, Realdon O, et al. Telemedicine and virtual reality at time of COVID-19 pandemic: an overview for future perspectives in neurorehabilitation. Front Neurol 2021; 12: 646902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mekbib DB, Han J, Zhang L, et al. Virtual reality therapy for upper limb rehabilitation in patients with stroke: a meta-analysis of randomized clinical trials. Brain Inj 2020; 34: 456–465. [DOI] [PubMed] [Google Scholar]
- 10.Fealy S, Jones D, Hutton A, et al. The integration of immersive virtual reality in tertiary nursing and midwifery education: a scoping review. Nurse Educ Today 2019; 79: 14–19. [DOI] [PubMed] [Google Scholar]
- 11.Bracq M-S, Michinov E, Arnaldi B, et al. Learning procedural skills with a virtual reality simulator: an acceptability study. Nurse Educ Today 2019; 79: 153–160. [DOI] [PubMed] [Google Scholar]
- 12.Rose T, Nam CS, Chen KB. Immersion of virtual reality for rehabilitation-review. Appl Ergon 2018; 69: 153–161. [DOI] [PubMed] [Google Scholar]
- 13.Gasteiger N, van der Veer SN, Wilson P, et al. How, for whom, and in which contexts or conditions augmented and virtual reality training works in upskilling health care workers: realist synthesis. JMIR serious Games 2022; 10: e31644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Radianti J, Majchrzak TA, Fromm J, et al. A systematic review of immersive virtual reality applications for higher education: design elements, lessons learned, and research agenda. Comput Educ 2020; 147: 103778. [Google Scholar]
- 15.Car LT, Kyaw BM, Teo A, et al. Outcomes, measurement instruments, and their validity evidence in randomized controlled trials on virtual, augmented, and mixed reality in undergraduate medical education. Systematic mapping review. JMIR Serious Games 2022; 10: e29594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karaman D, Taşdemir N. The effect of using virtual reality during breast biopsy on pain and anxiety: a randomized controlled trial. J Perianesth Nurs 2021; 36: 702–705. [DOI] [PubMed] [Google Scholar]
- 17.Hood RJ, Maltby S, Keynes A, et al. Development and pilot implementation of TACTICS VR: a virtual reality-based stroke management workflow training application and training framework. Front Neurol 2021; 12: 2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Adhikari R, Kydonaki C, Lawrie J, et al. A mixed-methods feasibility study to assess the acceptability and applicability of immersive virtual reality sepsis game as an adjunct to nursing education. Nurse Educ Today 2021; 103: 104944. [DOI] [PubMed] [Google Scholar]
- 19.Gunn T, Rowntree P, Starkey D, et al. The use of virtual reality computed tomography simulation within a medical imaging and a radiation therapy undergraduate programme. J Med Radiat Sci 2021; 68: 28–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mallik R, Patel M, Atkinson B, et al. Exploring the role of virtual reality to support clinical diabetes training—A pilot study. J Diabetes Sci Technol 2022; 16: 844–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chiang D-H, Huang C-C, Cheng S-C, et al. Immersive virtual reality (VR) training increases the self-efficacy of in-hospital healthcare providers and patient families regarding tracheostomy-related knowledge and care skills: a prospective pre–post study. Medicine (Baltimore) 2022; 101: e28570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen NL, Jensen RO, Posth S, et al. Teaching ultrasound-guided peripheral venous catheter placement through immersive virtual reality: an explorative pilot study. Medicine (Baltimore) 2021; 100: e26394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoogenes J, Wong N, Al-Harbi B, et al. A randomized comparison of 2 robotic virtual reality simulators and evaluation of Trainees’ skills transfer to a simulated robotic urethrovesical anastomosis task. Urology 2018; 111: 110–115. [DOI] [PubMed] [Google Scholar]
- 24.Slater P, Hasson F, Gillen P, et al. Virtual simulation training: imaged experience of dementia. Int J Older People Nurs 2019; 14: e12243. [DOI] [PubMed] [Google Scholar]
- 25.Pot-Kolder RM, Geraets CN, Veling W, et al. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. The Lancet Psychiatry 2018; 5: 217–226. [DOI] [PubMed] [Google Scholar]
- 26.Beverly E, Hommema L, Coates K, et al. A tranquil virtual reality experience to reduce subjective stress among COVID-19 frontline healthcare workers. Plos one 2022; 17: e0262703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee C-H, Kim Y-S, Jung J-H. Effectiveness of virtual reality based cognitive rehabilitation on cognitive function, motivation and depression in stroke patients. Medico Legal Update 2020; 20: 1880–1886. [Google Scholar]
- 28.Ryu J-H, Park J-W, Nahm FS, et al. The effect of gamification through a virtual reality on preoperative anxiety in pediatric patients undergoing general anesthesia: a prospective, randomized, and controlled trial. J Clin Med 2018; 7: 284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bergmann J, Krewer C, Bauer P, et al. Virtual reality to augment robot-assisted gait training in non-ambulatory patients with a subacute stroke: a pilot randomized controlled trial. Eur J Phys Rehabil Med 2017; 54: 397–407. [DOI] [PubMed] [Google Scholar]
- 30.Thapa N, Park HJ, Yang J-G, et al. The effect of a virtual reality-based intervention program on cognition in older adults with mild cognitive impairment: a randomized control trial. J Clin Med 2020; 9: 1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Luca R, Russo M, Naro A, et al. Effects of virtual reality-based training with BTs-nirvana on functional recovery in stroke patients: preliminary considerations. International Journal of Neuroscience 2018; 128: 791–796. [DOI] [PubMed] [Google Scholar]
- 32.Al-Sharman A, Khalil H, El-Salem K, et al. Motor performance improvement through virtual reality task is related to fatigue and cognition in people with multiple sclerosis. Physiother Res Int 2019; 24: e1782. [DOI] [PubMed] [Google Scholar]
- 33.Yeh S-C, Lee S-H, Chan R-C, et al. The efficacy of a haptic-enhanced virtual reality system for precision grasp acquisition in stroke rehabilitation. J Healthc Eng 2017; 2012: 9840273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mekbib DB, Debeli DK, Zhang L, et al. A novel fully immersive virtual reality environment for upper extremity rehabilitation in patients with stroke. Ann N Y Acad Sci 2021; 1493: 75–89. [DOI] [PubMed] [Google Scholar]
- 35.Jonsdottir J, Baglio F, Gindri P, et al. Virtual reality for motor and cognitive rehabilitation from clinic to home: a pilot feasibility and efficacy study for persons with chronic stroke. Front Neurol 2021; 12: 440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018; 169: 467–473. 2018/09/05.. [DOI] [PubMed] [Google Scholar]
- 37.Amini H, Gregory ME, Abrams MA, et al. Feasibility and usability study of a pilot immersive virtual reality-based empathy training for dental providers. J Dent Educ 2021; 85: 856–865. [DOI] [PubMed] [Google Scholar]
- 38.Giordano NA, Whitney CE, Axson SA, et al. A pilot study to compare virtual reality to hybrid simulation for opioid-related overdose and naloxone training. Nurse Educ Today 2020; 88: 104365. [DOI] [PubMed] [Google Scholar]
- 39.Mrakic-Sposta S, Di Santo SG, Franchini F, et al. Effects of combined physical and cognitive virtual reality-based training on cognitive impairment and oxidative stress in MCI patients: a pilot study. Front Aging Neurosci 2018; 10: 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mosso Vázquez JL, Mosso Lara D, Mosso Lara JL, et al. Pain distraction during ambulatory surgery: virtual reality and mobile devices. Cyberpsychology, Behavior, and Social Networking 2019; 22: 15–21. [DOI] [PubMed] [Google Scholar]
- 41.Osmanlliu E, Trottier ED, Bailey B, et al. Distraction in the emergency department using virtual reality for intravenous procedures in children to improve comfort (DEVINCI): a pilot pragmatic randomized controlled trial. Canadian Journal of Emergency Medicine 2021; 23: 94–102. [DOI] [PubMed] [Google Scholar]
- 42.Buccellato KH, Nordstrom M, Murphy JM, et al. A randomized feasibility trial of a novel, integrative, and intensive virtual rehabilitation program for service members post-acquired brain injury. Mil Med 2020; 185: e203–e211. [DOI] [PubMed] [Google Scholar]
- 43.Falconer CJ, Cutting P, Davies EB, et al. Adjunctive avatar therapy for mentalization-based treatment of borderline personality disorder: a mixed-methods feasibility study. Evid Based Ment Health 2017; 20: 123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kyaw BM, Saxena N, Posadzki P, et al. Virtual reality for health professions education: systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res 2019; 21: e12959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sevcenko K, Lindgren I. The effects of virtual reality training in stroke and Parkinson’s disease rehabilitation: a systematic review and a perspective on usability. Eur Rev Aging Phys Act 2022; 19: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen J, Xie Z, Or C. Effectiveness of immersive virtual reality-supported interventions for patients with disorders or impairments: a systematic review and meta-analysis. Health Technol (Berl) 2021; 11: 811–833. [Google Scholar]
- 47.Slater M, Sanchez-Vives MV. Enhancing our lives with immersive virtual reality. Frontiers in Robotics and AI 2016; 3: 74. [Google Scholar]
- 48.Coulter R, Saland L, Caudell T, et al. The effect of degree of immersion upon learning performance in virtual reality simulations for medical education. InMedicine Meets Virtual Reality 2007; 15: 155. [PubMed] [Google Scholar]
- 49.Chen J, Xie Z, Or CK. Head-Mounted display virtual reality in disease treatment: a systematic review and meta-analysis. In: Proceedings of the human factors and ergonomics society annual meeting. Los Angeles, CA: Sage Publications Sage CA, 2020, pp.1388–1389. [Google Scholar]
- 50.Zhang T, Booth R, Jean-Louis R, et al. A primer on usability assessment approaches for health-related applications of virtual reality. JMIR serious Games 2020; 8: e18153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boeldt D, McMahon E, McFaul M, et al. Using virtual reality exposure therapy to enhance treatment of anxiety disorders: identifying areas of clinical adoption and potential obstacles. Front Psychiatry 2019; 10: 773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Demers M, Mbiya N, Levin MF. Industry and academia collaboration in the design of virtual reality applications for rehabilitation. In: 2017 International Conference on Virtual Rehabilitation (ICVR), 2017, pp.1–2: IEEE. [Google Scholar]
- 53.López-Ojeda W, Hurley RA. Extended-reality technologies: an overview of emerging applications in medical education and clinical care. J Neuropsychiatry Clin Neurosci 2021; 33: A4–177. [DOI] [PubMed] [Google Scholar]
- 54.Ahmadpour N, Keep M, Janssen A, et al. Design strategies for virtual reality interventions for managing pain and anxiety in children and adolescents: scoping review. JMIR serious Games 2020; 8: e14565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Austin PD. The analgesic effects of virtual reality for people with chronic pain: a scoping review. Pain Medicine 2021; 23: 105–121. [DOI] [PubMed] [Google Scholar]
- 56.Asadzadeh A, Samad-Soltani T, Salahzadeh Z, et al. Effectiveness of virtual reality-based exercise therapy in rehabilitation: a scoping review. Informatics in Medicine Unlocked 2021; 24: 100562. [Google Scholar]
- 57.Mubin O, Alnajjar F, Al Mahmud A, et al. Exploring serious games for stroke rehabilitation: a scoping review. Disability and Rehabilitation: Assistive Technology 2022; 17: 159–165. [DOI] [PubMed] [Google Scholar]
- 58.Cheung VK-L, So EH-K, Ng GW-Y, et al. Investigating effects of healthcare simulation on personal strengths and organizational impacts for healthcare workers during COVID-19 pandemic: a cross-sectional study. Integrative Medicine Research 2020; 9: 100476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Co M, Chu KM. Distant surgical teaching during COVID-19-A pilot study on final year medical students. Surg Pract 2020; 24: 105–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gallardo FC, Martin C, Garcia AAT, et al. Home program for acquisition and maintenance of microsurgical skills during the coronavirus disease 2019 outbreak. World Neurosurg 2020; 143: 557–563. e551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mantovani E, Zucchella C, Bottiroli S, et al. Telemedicine and Virtual Reality for Cognitive Rehabilitation: A Roadmap for the COVID-19 Pandemic. Front Neurol 2020; 11. Perspective. DOI: 10.3389/fneur.2020.00926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Groenveld T, Achttien R, Smits M, et al. Feasibility of virtual reality exercises at home for post–COVID-19 condition: cohort study. JMIR rehabilitation and Assistive Technologies 2022; 9: e36836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mateen MA-O, Kan CA-O. Education during COVID-19: Ready, headset, go!. [DOI] [PMC free article] [PubMed]