Abstract
Study Design:
Retrospective comparative study.
Objectives:
To compare the perioperative complications of propensity score-matched cohorts of patients with degenerative cervical myelopathy (DCM), who were treated with anterior cervical discectomy and fusion (ACDF), posterior laminectomy with fusion, or laminoplasty.
Methods:
The Humana PearlDiver Patient Record Database was queried using the International Classification of Diseases (ICD-9 and ICD-10) and the Current Procedural Terminology (CPT) codes. Propensity score-matched analysis was done using multiple Chi-squared tests with Bonferroni correction of the significance level.
Results:
Cohorts of 11,790 patients who had ACDF, 2,257 patients who had posterior laminectomy with fusion, and 477 patients who had laminoplasty, were identified. After propensity score matching, all the 3 groups included 464 patients. The incidence of dysphagia increased significantly following ACDF compared to laminoplasty, P < 0.001, and in laminectomy with fusion compared to laminoplasty, P < 0.001. The incidence of new-onset cervicalgia was higher in ACDF compared to laminoplasty, P = 0.005, and in laminectomy with fusion compared to laminoplasty, P = 0.004. The incidence of limb paralysis increased significantly in laminectomy with fusion compared to ACDF, P = 0.002. The revision rate at 1 year increased significantly in laminectomy with fusion compared to laminoplasty, P < 0.001, and in ACDF compared to laminoplasty, P < 0.001.
Conclusions:
The incidence of dysphagia following laminectomy with fusion was not different compared to ACDF. Postoperative new-onset cervicalgia and revisions were least common in laminoplasty. The highest rate of postoperative limb paralysis was noticed in laminectomy with fusion.
Keywords: degenerative cervical myelopathy, cervical spinal stenosis, ACDF, laminectomy and fusion, laminoplasty, propensity score matching
Introduction
With increasing age, spondylotic changes encroach on the spinal canal width, and a considerable proportion of the population shows radiological signs of spondylosis.1-3 Intervertebral disc degeneration is the initial step in the spine degenerative changes.4,5 Progressive degeneration is characterized by ligamentum flavum hypertrophy, facet arthropathy, generation of osteophytes, and/or ossification of the posterior longitudinal ligament, which cause spinal canal diameter narrowing.1,4-7 Cervical spinal stenosis can cause myelopathy, impairing the extremity functions and causing gait disturbances, due to direct compression, or blood flow compromise as a result of vascular compression, with repeated trauma during flexion and extension movements.2,8,9
The term degenerative cervical myelopathy (DCM) has been used as an overarching term to describe various cervical spine degenerative conditions.10,11 The majority of patients with degenerative cervical myelopathy need surgery to decompress the cervical spine and halt the development or deterioration of neurological deficits.7,12 The surgical options may include anterior, posterior, or combined approaches.13,14 Anterior cervical discectomy and fusion (ACDF) involves the decompression of the neural elements by removal of the disc material and posterior osteophytes, followed by disc space distraction and height restoration by a structural interbody graft.15,16 In addition to neural decompression, ACDF is effective for restoring cervical lordosis. 17 Despite the reported advantages of ACDF, some complications can occur, including dysphagia, hoarseness of voice, and hardware failure.15,18,19 Cervical laminectomy with instrumented fusion allows spinal cord decompression with immediate stability, therefore, prevents the development of kyphotic deformity.20,21 However, this approach is associated with some pitfalls like screw-related neurovascular injury, neurologic deterioration, and non-fusion.22,23 Cervical laminoplasty has been considered to be effective in multilevel cervical degenerative stenosis.24,25 In the open-door technique, hinges are created to elevate the lamina to widen the stenosed spinal canal to decompress the spinal cord. Plates are placed on the open side of the lamina to prevent reclosure of the opened lamina.26,27 However, some complications have been reported, including C5 palsy and progressive kyphosis.27-29
No previous study compared the perioperative complications of different surgical procedures for degenerative cervical myelopathy using matched patients’ cohorts. Therefore, we conducted a retrospective nationwide study, which included a propensity score-matched large cohort of patients, to compare the perioperative complications, reoperations, and 30-day readmission rates of ACDF, posterior laminectomy with fusion, and laminoplasty in patients with cervical degenerative cervical myelopathy.
Methods
Data source
This nationwide study used the Humana subset of the PearlDiver Patient Record Database (PearlDiver Technologies, Colorado Springs, CO, USA), a commercially available database with medical records of over 25 million patients from 2007 through the first quarter of 2017. This study has been carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA).
Patient Population
We retrospectively reviewed patients with degenerative cervical myelopathy who had undergone ACDF, laminectomy with fusion, or laminoplasty, at 2 or 3 spinal levels, from 2007 to the end of the first quarter of 2016 with a minimum of 1-year follow-up period.
Data Collection
The database was queried using the International Classification of Diseases (ICD-9-CM and ICD-10-CM) codes to identify patients diagnosed with degenerative cervical myelopathy. These codes included ICD-9-D-7230, ICD-9-D-7211, ICD-10-D-M4802, and ICD-10-D-M4712. Then, the Current Procedural Terminology (CPT) codes were used to identify patients who had undergone ACDF (CPT-22551 and CPT-22554), laminectomy with fusion (CPT-63001, CPT-63015, CPT-63045, and CPT-22600), or laminoplasty with reconstruction of the posterior bony elements (CPT-63051). Two and 3-level procedures were identified using addon codes for ACDF (22552), laminectomy with fusion (22614), and laminoplasty (modifier 52 of reduced service), Table 1. Patients with infections, fractures, trauma, or previous surgeries were excluded from the study.
Table 1.
Degenerative Cervical Myelopathy, ACDF, Laminectomy With Fusion, and Laminoplasty Codes.
| Codes | Definitions |
|---|---|
| Degenerative Cervical Myelopathy | |
| ICD-9-D-7230 | Spinal stenosis in cervical region. |
| ICD-9-D-7211 | Cervical spondylosis with myelopathy. |
| ICD-10-D-M4802 | Spinal stenosis, cervical region. |
| ICD-10-D-M4712 | Other spondylosis with myelopathy, cervical region. |
| ACDF * | |
| CPT-22551 | Arthrodesis, anterior interbody, including disc space preparation, discectomy, osteophytectomy and decompression of spinal cord and/or nerve roots; cervical below C2. |
| CPT-22554 | Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); cervical below C2. |
| Laminectomy with fusion* | |
| CPT-63001 | Laminectomy with exploration and/or decompression of spinal cord and/or cauda equina, without facetectomy, foraminotomy or discectomy (eg, spinal stenosis), 1 or 2 vertebral segments; cervical. |
| CPT-63015 | Laminectomy with exploration and/or decompression of spinal cord and/or cauda equina, without facetectomy, foraminotomy or discectomy (eg, spinal stenosis), more than 2 vertebral segments; cervical. |
| CPT-63045 | Laminectomy, facetectomy and foraminotomy (unilateral or bilateral with decompression of spinal cord, cauda equina and/or nerve root[s], [eg, spinal or lateral recess stenosis]), single vertebral segment; cervical. |
| CPT-22600 | Arthrodesis, posterior or posterolateral technique, single level; cervical below C2 segment. |
| Laminoplasty* | |
| CPT-63051 | Laminoplasty, cervical, with decompression of the spinal cord, 2 or more vertebral segments; with reconstruction of the posterior bony elements (including the application of bridging bone graft and non-segmental fixation devices [e.g., wire, suture, mini-plates] when performed). |
* Additional add-on codes were used to specify 2 or 3 levels procedures.
+ 22552: cervical below C2, each additional interspace. Used in conjunction with 22551.
+ 22614: each additional vertebral segment. Used in conjunction with 22600.
The database was then queried to identify the perioperative surgical and medical complications and reoperations during or following each of the primary procedures, using the relevant ICD-9-CM, ICD-10-CM, and CPT codes (Table 2). The perioperative complications were defined as that occurred during the primary procedure, within 1, 3, 6, or 12 months following the surgery.
Table 2.
Medical and Surgical Complications and Reoperations and Their Codes.
| Complications | ICD/ CPT Codes |
|---|---|
| Wound complications | ICD-9-D-99811, ICD-9-D-99812, ICD-9-D-99813, ICD-9-D-99830, ICD-9-D-99831, ICD-9-D-99832, ICD-9-D-99883, ICD-9-D-99851, ICD-9-D-99859, ICD-10-D-L7622, ICD-10-D-L7632, ICD-10-D-L7634, ICD-10-D-T8130XA, ICD-10-D-T8131XA, ICD-10-D-T8140XA, ICD-10-D-T8141XA, ICD-10-D-T8142XA |
| Surgical site infection | ICD-9-D-99851, ICD-9-D-99859, ICD-9-D-99660, ICD-9-D-99667, ICD-10-D-T8140XA, ICD-10-D-T8141XA, ICD-10-D-T8142XA, ICD-10-D-T8463XA, ICD-10-D-T847XXA, ICD-10-D-T8579XA |
| Spinal cord injury | ICD-9-D-95200:ICD-9-D-95209, ICD-10-D-S140XXA, ICD-10-D-S14101A, ICD-10-D-S14102A, ICD-10-D-S14103A, ICD-10-D-S14104A, ICD-10-D-S14105A, ICD-10-D-S14106A, ICD-10-D-S14107A, ICD-10-D-S14108A, ICD-10-D-S14109A |
| Nerve root injury | ICD-9-D-9530, ICD-10-D-S142XXA |
| Dural tear | ICD-9-D-34931, ICD-10-D-G9741, CPT-63707, CPT-63709, CPT-63710 |
| Dysphagia | ICD-9-D-78720:ICD-9-D-78729, ICD-10-D-R1310:ICD-10-D-R1319 |
| Dysphonia | ICD-9-D-78442, ICD-10-D-R490 |
| Cervicalgia | ICD-9-D-7231, ICD-10-D-M542 |
| Cervical kyphosis | ICD-9-D-73712, ICD-9-D-73719, ICD-10-D-M4012, ICD-10-D-M40202, ICD-10-D-M40292, ICD-10-D-M963 |
| Limb paralysis | ICD-9-D-34400:ICD-9-D-34409, ICD-9-D-3441, ICD-9-D-3442, ICD-9-D-34430:ICD-9-D-34432, ICD-9-D-34440:ICD-9-D-34442, ICD-9-D-3445, ICD-10-D-G8100:ICD-10-D-G8104, ICD-10-D-G8110:ICD-10-D-G8114, ICD-10-D-G8190:ICD-10-D-G8194, ICD-10-D-G8220:ICD-10-D-G8222, ICD-10-D-G8250:ICD-10-D-G8254, ICD-10-D-G830, ICD-10-D-G8310:ICD-10-D-G8314, ICD-10-D-G8320:ICD-10-D-G8324 |
| Pulmonary embolism/ deep venous thrombosis | ICD-9-D-41511, ICD-9-D-41513, ICD-9-D-41519, ICD-10-D-I2609, ICD-10-D-I2692, ICD-10-D-I2699, ICD-9-D-45340, ICD-9-D-45341, ICD-9-D-45342, ICD-10-D-I82401:ICD-10-D-I82409, ICD-10-D-I82411:ICD-10-D-I82419, ICD-10-D-I82431:ICD-10-D-I82439, ICD-10-D-I82441:ICD-10-D-I82449, ICD-10-D-I824Y1:ICD-10-D-I824Y9, ICD-10-D-I824Z1:ICD-10-D-I824Z9 |
| Cerebrovascular accident | ICD-9-D-430, ICD-9-D-431, ICD-9-D-4320:ICD-9-D-4329, ICD-9-D-99702, ICD-10-D-I6200:ICD-10-D-I6203, ICD-10-D-I621, ICD-10-D-I629, ICD-10-D-I97811, ICD-10-D-I97821, ICD-10-D-I609 |
| Myocardial infarction | ICD-9-D-41000:ICD-9-D-41002, ICD-9-D-41010:ICD-9-D-41012, ICD-9-D-41020:ICD-9-D-41022, ICD-9-D-41030:ICD-9-D-41032, ICD-9-D-41040:ICD-9-D-41042, ICD-9-D-41050:ICD-9-D-41052, ICD-9-D-41060:ICD-9-D-41062, ICD-9-D-41070:ICD-9-D-41072, ICD-9-D-41080:ICD-9-D-41082, ICD-9-D-41090:ICD-9-D-41092, ICD-10-D-I2101, ICD-10-D-I2102, ICD-10-D-I2109, ICD-10-D-I2111, ICD-10-D-I2119, ICD-10-D-I2121, ICD-10-D-I2129, ICD-10-D-I213, ICD-10-D-I214, ICD-10-D-I219, ICD-10-D-I21A1, ICD-10-D-I21A9 |
| Pneumonia | ICD-9-D-4800:ICD-9-D-4809, ICD-9-D-481, ICD-9-D-4820:ICD-9-D-4822, ICD-9-D-48230:ICD-9-D-48239, ICD-9-D-48240:ICD-9-D-48249, ICD-9-D-48281:ICD-9-D-48289, ICD-9-D-4829, ICD-10-D-J120:ICD-10-D-J123, ICD-10-D-J1281, ICD-10-D-J1289, ICD-10-D-J129, ICD-10-D-J13, ICD-10-D-J14, ICD-10-D-J150, ICD-10-D-J151, ICD-10-D-J1520, ICD-10-D-J15211, ICD-10-D-J15212, ICD-10-D-J1529, ICD-10-D-J153:ICD-10-D-J159 |
| Respiratory failure | ICD-9-D-51881, ICD-9-D-51851, ICD-10-D-J9600:ICD-10-D-J9602, ICD-10-D-J95821 |
| Renal failure | ICD-9-D-5845:5849, ICD-10-D-N170:ICD-10-D-N179 |
| Sepsis | ICD-9-D-99591, ICD-9-D-99592, ICD-10-D-T8144XA |
| Urinary tract infection | ICD-9-D-5990, ICD-9-D-59780, ICD-9-D-59789, ICD-9-D-5950, ICD-9-D-5959, ICD-10-D-N390, ICD-10-D-N341, ICD-10-D-N342, ICD-10-D-N3000, ICD-10-D-N3090 |
| Incision and drainage, exploration or evacuation | CPT-22010, CPT-22830, CPT-63265 |
| Hardware removal | CPT-22852 |
| Revision | CPT-22548, CPT-22551, CPT-22552, CPT-22554, CPT-22585, CPT-22595, CPT-22600, CPT-22614, CPT-22856, CPT-63001, CPT-63015, CPT-63035, CPT-63040, CPT-63043, CPT-63045, CPT-63048, CPT-63050, CPT-63051, CPT-63075, CPT-63076, CPT-0090T, CPT-0092T, ICD-9-P-8101, ICD-9-P-8102, ICD-9-P-8103, ICD-9-P-8132, ICD-9-P-8133, ICD-9-P-8461, ICD-9-P-8462 |
The demographic criteria of patients, including age, gender, hospital setting, geographical area, year of the procedure, and the Charlson Comorbidity Index (CCI), 30 an index predicting the 10-year survival rate in patients with comorbidities, were identified.
Perioperative Complications
Surgical complications included intraoperative dural tear, spinal cord injury, and nerve root injury, postoperative wound complications, including hemorrhage, hematoma, seroma, wound disruption, non-healing wound, and surgical site infection within 1 and 3 months, dysphagia, dysphonia, new-onset cervicalgia that was not present preoperatively, limb paralysis (monoplegia, diplegia, paraplegia, or quadriplegia) within 1 month, and cervical kyphosis within 6 and 12 months.
Medical complications included pulmonary embolism (PE) or deep venous thrombosis (DVT) within 3 months, cerebrovascular accident (CVA), myocardial infarction (MI), pneumonia, respiratory failure, renal failure, sepsis, and urinary tract infection within 1 month.
Reoperations
Reoperations included incision and drainage, exploration or evacuation within 1 and 3 months postoperatively, hardware removal, and revision surgeries within 1 year.
Statistical Analysis
Results were reported as numbers, percentages, and incidence per 100 000 Humana insured patients. One-way ANOVA test was used to compare the mean CCI between the 3 groups. Propensity score matching was conducted to control the potential confounding factors, including age, gender, and CCI. Pairwise Chi-squared tests with the Bonferroni correction of the significance level (P < 0.017) were used to compare the complications and reoperation rates between the 3 procedures. Statistical analysis of data was conducted using the PearlDiver R statistical analysis software.
Results
Study Populations
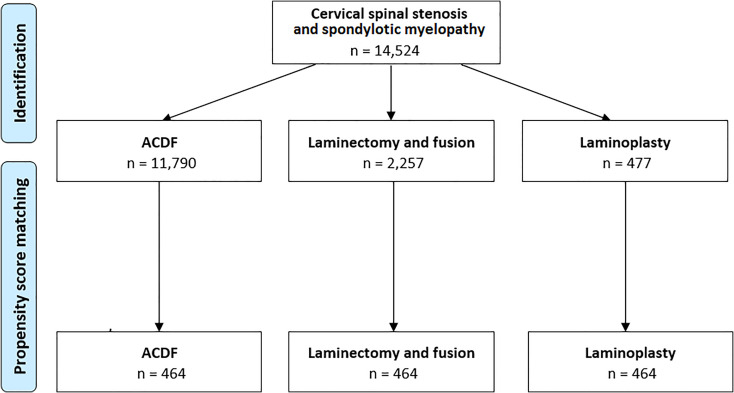
Throughout the study period, a total number of 14 524 patients had undergone surgical treatment for degenerative cervical myelopathy at 2 or 3 levels; 11 790 patients had ACDF, 2,257 patients had laminectomy with fusion, and 477 patients had laminoplasty, Figure. 1.
Figure 1.
Flow chart showing the number of patients in each group before and after propensity score matching.
The 65-to-69 years age group was the most common age group in the 3 groups of patients; 21.5% in the ACDF group, 23.8% in the laminectomy with fusion group, and 22.9% in the laminoplasty group.
The ACDF group included 5,640 male (47.8%) and 6,150 female (52.2%) patients. The laminectomy with fusion group included 1,335 male (59.1%) and 922 female (40.9%) patients. In the laminoplasty group there were 305 male (63.9%) and 172 female (36.1%) patients.
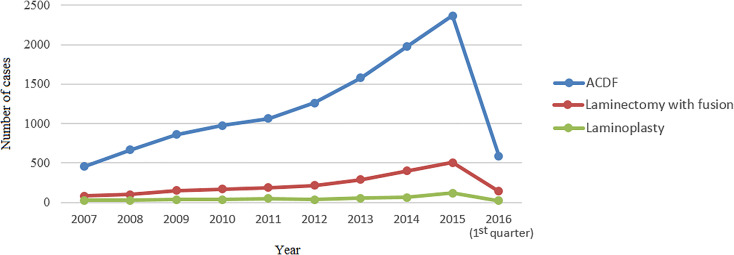
The incidence of each procedure continued to increase over time, with the highest number of cases reported in 2015 (2367 (20.1%) in ACDF, 508 (22.5%) in laminectomy with fusion, and 118 (24.7%) in laminoplasty, Figure 2).
Figure 2.
Number of cases of the 3 procedures by year.
For service location, 89.7% of the ACDF procedures were hospital inpatient, while 10.3% were hospital outpatient. For the laminectomy with fusion procedures, 98.4% were inpatient, while 1.6% were outpatient. For the laminoplasty procedures, 97.3% were inpatient, while 2.7% were outpatient, Table 3.
Table 3.
Age, Gender, Regional, Service Location and Case Year Distributions of the Studied Patients.
| Characters | ACDF, n = 11790 | Laminectomy with fusion, n = 2257 | Laminoplasty, n = 477 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | Incidence* | No. | % | Incidence* | No. | % | Incidence* | |
| Age in years: | |||||||||
| < 30 | < 11 | † | † | < 11 | † | † | < 11 | † | † |
| 30 to 34 | 54 | 0.5 | 2.9 | < 11 | † | † | < 11 | † | † |
| 35 to 39 | 178 | 1.5 | 8.8 | < 11 | † | † | < 11 | † | † |
| 40 to 44 | 438 | 3.7 | 18.5 | 27 | 1.2 | 1.1 | < 11 | † | † |
| 45 to 49 | 864 | 7.3 | 30.1 | 61 | 2.7 | 2.1 | 21 | 4.4 | 0.7 |
| 50 to 54 | 1268 | 10.8 | 36.4 | 108 | 4.8 | 3.1 | 35 | 7.3 | 1 |
| 55 to 59 | 1547 | 13.1 | 39.9 | 191 | 8.5 | 4.9 | 49 | 10.3 | 1.3 |
| 60 to 64 | 1604 | 13.6 | 39.7 | 283 | 12.5 | 7 | 61 | 12.8 | 1.5 |
| 65 to 69 | 2534 | 21.5 | 18.7 | 537 | 23.8 | 4 | 109 | 22.9 | 0.8 |
| 70 to 74 | 1909 | 16.2 | 15.9 | 474 | 21 | 4 | 91 | 19.1 | 0.8 |
| 75 to 79 | 983 | 8.3 | 10.9 | 340 | 15.1 | 3.8 | 51 | 10.7 | 0.6 |
| 80 to 84 | 329 | 2.8 | 5.4 | 158 | 7 | 2.6 | 37 | 7.8 | 0.6 |
| 85 to 89 | 49 | 0.4 | 2.1 | 37 | 1.6 | 1.6 | < 11 | † | † |
| ≥ 90 | 31 | 0.3 | 0.7 | 31 | 1.4 | 0.7 | < 11 | † | † |
| Gender: | |||||||||
| Male | 5640 | 47.8 | 17.5 | 1335 | 59.1 | 4.1 | 305 | 63.9 | 0.9 |
| Female | 6150 | 52.2 | 14 | 922 | 40.9 | 2.1 | 172 | 36.1 | 0.4 |
| Region: | |||||||||
| Midwest | 2598 | 22 | 13.2 | 630 | 27.9 | 3.2 | 156 | 32.7 | 0.8 |
| Northeast | 196 | 1.7 | 3.7 | 53 | 2.3 | 1 | < 11 | † | † |
| South | 7932 | 67.3 | 19.4 | 1349 | 59.8 | 3.3 | 279 | 58.5 | 0.7 |
| West | 1064 | 9 | 10.3 | 225 | 10 | 2.2 | 32 | 6.7 | 0.3 |
| Service location: | |||||||||
| Inpatient | 10571 | 89.7 | † | 2221 | 98.4 | † | 464 | 97.3 | † |
| Outpatient | 1219 | 10.3 | † | 36 | 1.6 | † | 13 | 2.7 | † |
| Case year: | |||||||||
| 2007 | 454 | 3.9 | 7.2 | 85 | 3.8 | 1.3 | 28 | 5.9 | 0.4 |
| 2008 | 667 | 5.7 | 9.7 | 101 | 4.5 | 1.5 | 27 | 5.7 | 0.4 |
| 2009 | 859 | 7.3 | 13.7 | 152 | 6.7 | 2.4 | 37 | 7.8 | 0.6 |
| 2010 | 978 | 8.3 | 16.6 | 169 | 7.5 | 2.9 | 37 | 7.8 | 0.6 |
| 2011 | 1063 | 9 | 16.3 | 189 | 8.4 | 2.9 | 50 | 10.5 | 0.8 |
| 2012 | 1261 | 10.7 | 17.5 | 217 | 9.6 | 3 | 37 | 7.8 | 0.5 |
| 2013 | 1579 | 13.4 | 20 | 292 | 12.9 | 3.7 | 55 | 11.5 | 0.7 |
| 2014 | 1974 | 16.7 | 20.5 | 401 | 17.8 | 4.2 | 66 | 13.8 | 0.7 |
| 2015 | 2367 | 20.1 | 20.7 | 508 | 22.5 | 4.4 | 118 | 24.7 | 1 |
| 2016 (1st Q) | 588 | 5 | 7.3 | 143 | 6.3 | 1.8 | 22 | 4.6 | 0.3 |
* Incidence per 100,000 Humana insured patients.
Due to patient privacy and contractual agreements with PearlDiver Inc, data on cohorts with less than 11 patients is not reported.
The mean CCI ± SD was 6 ± 3.3 in the ACDF patients, 7.6 ± 3.9 in the laminectomy with fusion patients, and 6.9 ± 3.5 in the laminoplasty patients, P < 0.001.
Perioperative Complications
In the ACDF group, the most common surgical complications were new-onset cervicalgia at 1 month (44.8%), dysphagia at 1 month (10%), and wound complications (2.5% at 1 month and 3% at 3 months). The most common medical complications were urinary tract infections at 1 month (4.6%), respiratory failure at 1 month (3.6%), and renal failure at 1 month (2%). The revision rate at 1 year was 5.1%.
In the laminectomy with fusion group, the most common surgical complications were new-onset cervicalgia at 1 month (43.9%), limb paralysis at 1 month (9.9%), dysphagia at 1 month (8.6%), and wound complications (6.4% at 1 month and 8% at 3 months). The most common medical complications were urinary tract infections at 1 month (12.1%), respiratory failure at 1 month (9.7%), renal failure at 1 month (6.7%), and deep venous thrombosis or pulmonary embolism at 3 months (4.2%). The revision rate at 1 year was 7.6%.
In the laminoplasty group, the most common surgical complications were new-onset cervicalgia at 1 month (35.8%), limb paralysis at 1 month (6.5%), and wound complications (3.8% at 1 month and 4.4% at 3 months). The most common medical complications were urinary tract infections at 1 month (6.5%), respiratory failure at 1 month (4.2%), deep venous thrombosis or pulmonary embolism at 3 months (3.1%), and renal failure at 1 month (2.9%). The revision rate at 1 year was less than 2.3%, Table 4.
Table 4.
Perioperative Surgical and Medical Complications and Reoperation Rates Following the Three Procedures.
| Complications | ACDF n = 11 790 |
Laminectomy & fusion n = 2257 |
Laminoplasty n = 477 |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Surgical complications | ||||||
| Wound complications | ||||||
| At 1 month | 289 | 2.5 | 144 | 6.4 | 18 | 3.8 |
| At 3 months | 348 | 3 | 181 | 8 | 21 | 4.4 |
| Surgical site infection | ||||||
| At 1 month | 96 | 0.8 | 75 | 3.3 | 12 | 2.5 |
| At 3 months | 136 | 1.2 | 93 | 4.1 | 14 | 2.9 |
| Spinal cord injury | 100 | 0.8 | 80 | 3.5 | 14 | 2.9 |
| Nerve root injury | 43 | 0.4 | < 11 | < 0.5 | < 11 | < 2.3 |
| Dural tear | 57 | 0.5 | 33 | 1.5 | < 11 | < 2.3 |
| Dysphagia at 1 month | 1179 | 10 | 194 | 8.6 | < 11 | < 2.3 |
| Dysphonia at 1 month | 67 | 0.6 | < 11 | < 0.5 | 0 | 0 |
| Cervicalgia at 1 month | 5286 | 44.8 | 990 | 43.9 | 171 | 35.8 |
| Cervical kyphosis | ||||||
| At 6 months | 167 | 1.4 | 59 | 2.6 | < 11 | < 2.3 |
| At 12 months | 177 | 1.5 | 68 | 3 | < 11 | < 2.3 |
| Limb paralysis at 1 month | 278 | 2.4 | 223 | 9.9 | 31 | 6.5 |
| Medical complications | ||||||
| DVT/PE at 3 months | 185 | 1.6 | 95 | 4.2 | 15 | 3.1 |
| CVA at 1 month | 37 | 0.3 | 27 | 1.2 | 0 | 0 |
| MI at 1 month | 66 | 0.6 | 32 | 1.4 | < 11 | < 2.3 |
| Pneumonia at 1 month | 92 | 0.8 | 40 | 1.8 | < 11 | < 2.3 |
| Respiratory failure at 1 month | 430 | 3.6 | 220 | 9.7 | 14 | 2.9 |
| Renal failure at 1 month | 239 | 2 | 151 | 6.7 | 20 | 4.2 |
| Sepsis at 1 month | 116 | 1 | 46 | 2 | < 11 | < 2.3 |
| UTI at 1 month | 537 | 4.6 | 274 | 12.1 | 31 | 6.5 |
| Reoperations | ||||||
| I&D, exploration, or evacuation | ||||||
| At 1 month | 177 | 1.5 | 51 | 2.3 | < 11 | < 2.3 |
| At 3 months | 191 | 1.6 | 59 | 2.6 | < 11 | < 2.3 |
| Hardware removal at 1 year | 18 | 0.2 | < 11 | < 0.5 | < 11 | < 2.3 |
| Revision at 1 year | 602 | 5.1 | 172 | 7.6 | < 11 | < 2.3 |
DVT/PE deep venous thrombosis/pulmonary embolism, CVA cerebrovascular accident, MI myocardial infarction, UTI urinary tract infection, I&D incision and drainage.
Due to patient privacy and contractual agreements with PearlDiver Inc, data on cohorts with less than 11 patients is not reported.
Propensity-Score Matched Analysis
After propensity score matching, each group included 464 patients.
Wound complications at 1 and 3 months were less common in the ACDF group, < 2.4% and 2.8%, respectively, compared with laminectomy and fusion, 4.5% and 6%, and laminoplasty, 3.9% and 4.5%, respectively. However, this difference was not statistically significant, Table 5.
Table 5.
Comparison of Perioperative Surgical and Medical Complications and Reoperation Rates Between a Propensity-Score Matched Cohorts of the Three Groups.
| Complications | ACDF n = 464 | Laminectomy & fusion n = 464 | Laminoplasty n = 464 | P value* | |||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ACDF vs. laminectomy & fusion | ACDF vs. laminoplasty | Laminectomy & fusion vs. laminoplasty | |
| Surgical complications | |||||||||
| Wound complications | |||||||||
| At 1 month | < 11 | < 2.4 | 21 | 4.5 | 18 | 3.9 | 0.07 | 0.18 | 0.74 |
| At 3 months | 13 | 2.8 | 28 | 6 | 21 | 4.5 | 0.03 | 0.22 | 0.38 |
| Surgical site infection | |||||||||
| At 1 month | < 11 | < 2.4 | 11 | 2.4 | 12 | 2.6 | 0.12 | 0.08 | 1 |
| At 3 months | < 11 | < 2.4 | 16 | 3.4 | 14 | 3 | 0.03 | 0.06 | 0.85 |
| Spinal cord injury | < 11 | < 2.4 | 13 | 2.8 | 14 | 3 | 0.05 | 0.03 | 1 |
| Nerve root injury | < 11 | < 2.4 | < 11 | < 2.4 | < 11 | < 2.4 | 1 | 1 | 1 |
| Dural tear | < 11 | < 2.4 | < 11 | < 2.4 | < 11 | < 2.4 | 0.15 | 1 | 0.26 |
| Dysphagia at 1 month | 59 | 12.7 | 44 | 9.5 | < 11 | < 2.4 | 0.14 | < 0.001 | < 0.001 |
| Dysphonia at 1 month | < 11 | < 2.4 | 0 | 0 | 0 | 0 | 0.48 | 0.48 | 1 |
| Cervicalgia at 1 month | 211 | 45.5 | 212 | 45.7 | 168 | 36.2 | 1 | 0.005 | 0.004 |
| Cervical kyphosis | |||||||||
| At 6 months | < 11 | < 2.4 | 12 | 2.6 | < 11 | < 2.4 | 0.08 | 0.75 | 0.23 |
| At 12 months | < 11 | < 2.4 | 14 | 3 | < 11 | < 2.4 | 0.03 | 0.38 | 0.28 |
| Limb paralysis at 1 month | 17 | 3.7 | 41 | 8.8 | 30 | 6.5 | 0.002 | 0.07 | 0.22 |
| 30-days readmission | 43 | 9.3 | 90 | 19.4 | 56 | 12.1 | < 0.001 | 0.2 | 0.003 |
| Medical complications | |||||||||
| DVT/PE at 3 months | 19 | 4.1 | 13 | 2.8 | 14 | 3 | 0.37 | 0.48 | 1 |
| CVA at 1 month | < 11 | < 2.4 | < 11 | < 2.4 | 0 | 0 | 0.75 | 0.13 | 0.04 |
| MI at 1 month | < 11 | < 2.4 | < 11 | < 2.4 | < 11 | < 2.4 | 1 | 0.54 | 0.54 |
| Pneumonia at 1 month | < 11 | < 2.4 | < 11 | < 2.4 | < 11 | < 2.4 | 0.77 | 1 | 0.77 |
| Respiratory failure at 1 month | 28 | 6 | 43 | 9.3 | 14 | 3 | 0.08 | 0.04 | < 0.001 |
| Renal failure at 1 month | 12 | 2.6 | 24 | 5.2 | 20 | 4.3 | 0.06 | 0.21 | 0.64 |
| Sepsis at 1 month | < 11 | < 2.4 | < 11 | < 2.4 | < 11 | < 2.4 | 0.81 | 0.38 | 0.18 |
| UTI at 1 month | 27 | 5.8 | 37 | 8 | 30 | 6.5 | 0.24 | 0.79 | 0.45 |
| Reoperations | |||||||||
| I&D, exploration, or evacuation | |||||||||
| At 1 month | < 11 | < 2.4 | 11 | 2.4 | < 11 | < 2.4 | 0.33 | 0.75 | 0.12 |
| At 3 months | < 11 | < 2.4 | 13 | 2.8 | < 11 | < 2.4 | 0.16 | 1 | 0.26 |
| Hardware removal at 1 year | < 11 | < 2.4 | < 11 | < 2.4 | < 11 | < 2.4 | 1 | 0.62 | 1 |
| Revision at 1 year | 24 | 5.2 | 33 | 7.1 | < 11 | < 2.4 | 0.27 | < 0.001 | < 0.001 |
DVT/PE deep venous thrombosis/pulmonary embolism, CVA cerebrovascular accident, MI myocardial infarction, UTI urinary tract infection, I&D incision and drainage.
The level of significance was set at P < 0.017 after Bonferroni correction.
Due to patient privacy and contractual agreements with PearlDiver Inc, data on cohorts with less than 11 patients is not reported.
Similarly, surgical site infections at 1 and 3 months were less common in the ACDF group, < 2.4% and < 2.4%, compared with laminectomy and fusion, 2.4% and 3.4%, and laminoplasty, 2.6% and 3%, respectively (Table 5).
The incidences of intraoperative spinal cord injury, nerve root injury, and dural tear, postoperative dysphonia, and kyphosis were not significantly different between the 3 groups.
The incidence of dysphagia at 1 month increased significantly following ACDF (12.7%) compared to laminoplasty (< 2.4%), P < 0.001, and it also increased significantly in laminectomy with fusion (9.5%) compared to laminoplasty, P < 0.001. However, the incidence was not significantly significant between ACDF and laminectomy with fusion, P = 0.14.
The incidence of new-onset cervicalgia at 1 month had a statistically significant difference between ACDF (45.5%) and laminoplasty (36.2%), P = 0.005, and between laminectomy with fusion (45.7%) and laminoplasty, P = 0.004. The incidence was not different between ACDF and laminectomy with fusion, P = 1.
The incidence of limb paralysis at 1 month increased significantly in laminectomy with fusion (8.8%) compared to ACDF (3.7%), P = 0.002. There was no significant difference between laminectomy with fusion and laminoplasty (6.5%), P = 0.22, or between ACDF and laminoplasty, P = 0.07.
Out of the medical complications, the incidence of respiratory failure at 1 month was significantly different between laminectomy with fusion (9.3%) and laminoplasty (3%), P < 0.001, but it was not significantly different between laminectomy with fusion and ACDF (6%), P = 0.08, or between ACDF and laminoplasty, P = 0.04.
Reoperation and Readmission Rates
The revision rate at 1 year increased significantly in laminectomy with fusion (7.1%) compared to laminoplasty (< 2.4%), P < 0.001, and between ACDF (5.2%) and laminoplasty, P < 0.001, but it was not significantly different between ACDF and laminectomy with fusion, P = 0.27, Table 5.
The 30-day readmission rates were 90 (19.4%) in the laminectomy with fusion group, 56 (12.1%) in the laminoplasty, and 43 (9.3%) in the ACDF group. There was a statistically significant difference between laminectomy with fusion and ACDF, P < 0.001, and between laminectomy with fusion and laminoplasty, P = 0.003, but there was no statistically significant difference between ACDF and laminoplasty, P = 0.2.
Discussion
Surgical treatment for degenerative cervical myelopathy is recommended when there is evidence of worsening neurological impairment.13,31 Surgical decision making concerning anterior versus posterior cervical surgery is multifactorial with many determinants that need to be considered, and the choice of the procedure should be made on a case-by-case basis. 32 The dominant site of cord compression, anterior or posterior, affects the chosen approach.32,33 Moreover, cervical lordosis can be adequately restored from an anterior approach, while multilevel degenerative spine may be more easily to be addressed from a posterior approach.34,35 The high risk of infection rates following posterior surgeries may favor an anterior approach. 36
The current study compared the perioperative surgical and medical complications among 3 standard procedures; ACDF, laminectomy with fusion, and laminoplasty, at 2 or 3 levels. Moreover, in order to control for any confounding factors, a propensity-score matched analysis was conducted.
The incidence of dysphagia following ACDF was 12.7%. This coincided with previous studies that have reported that the incidence of dysphagia following ACDF is 11% to 65% due to esophageal manipulation and retraction during the procedure.37-39 However, the incidence of dysphagia in the laminectomy with fusion group was not significantly different compared to the ACDF group. In a study of 85 patients who had undergone posterior cervical surgery, Radcliff et al. 40 reported that the incidence of new dysphagia was significantly lower than that following ACDF at 2 and 6 weeks. However, the incidence of dysphagia after posterior cervical surgeries was significantly higher than that of lumbar surgeries. 40 Dysphagia after posterior laminectomy with fusion may be attributed to the loss of cervical motion, pain from posterior neck dissection, or cervical collar immobilization.
The incidence of postoperative new-onset cervicalgia was significantly lower in laminoplasty compared to ACDF or laminectomy with fusion. The lower incidence in laminoplasty may be attributed to the preserved cervical motion in laminoplasty compared to the loss of motion associated with fusion procedures.41-43 Excessive distraction of the disc space during ACDF could result in stretching the posterior ligaments and facet joint injury, which may lead to subsequent postoperative neck pain. 44 Choi et al. 45 reported postoperative intractable cervicalgia following ACDF. The postoperative disc heights were noticeably greater than the disc heights preoperatively due to over-sized implant insertion. 45 This finding emphasizes the importance of applying proper distraction forces and choosing a properly sized implant during ACDF surgery.
The highest incidence of postoperative limb paralysis was observed in the laminectomy with fusion. This could be attributed to excessive intraoperative traction and manipulation of neurological structures, direct injury from instruments, or screw malposition. 22
C5 palsy is a well-known complication following cervical spine surgery. 46 Bydon et al. 47 compared the incidence of C5 palsy in patients undergoing anterior or posterior decompression procedures. The highest incidence was reported in the laminectomy and fusion cohort, with a rate of 8.6% compared to 1.6% in the anterior cohort. 47 In a study of 750 patients who had anterior or posterior decompression procedures, Nassr et al. 46 reported a trend toward higher rates of C5 palsy with laminectomy and fusion compared to the anterior procedures.
In a prospective randomized trial, Jiang et al. 13 compared the outcomes following ACDF versus laminoplasty in patients with multilevel degenerative spinal stenosis and reported that the rate of complications was not significantly different between the 2 procedures. Hitchon et al. 35 compared ACDF versus laminectomy and fusion in patients with cervical stenosis and myelopathy and reported that the incidence of complications between the 2 groups was not different significantly. In Cole et al. 31 study, the 30-day complication rates were lower in the anterior fusion group than the posterior fusion group, except for dysphagia, in patients with multilevel degenerative cervical disease.
In our study, the revision rate at 1 year was significantly lower in laminoplasty compared to ACDF or laminectomy with fusion. The 30-day readmission rate was significantly higher in laminectomy and fusion compared to ACDF or laminoplasty. Highsmith et al. 48 compared laminoplasty versus laminectomy and fusion in 56 patients with multilevel cervical stenotic myelopathy and reported that the overall reoperation rates were higher in the fusion group (27%) than in the laminoplasty group (13%). Similarly, Liu et al., 49 in their systematic review and meta-analysis, reported a significantly lower reoperation rate with laminoplasty (3.5%) compared to ACDF (20.5%).
Expanding the evidence on the difference of perioperative complications between cervical spine surgeries is essential for spine surgeons. Additionally, patients undergoing spine surgeries should be informed about the possibility of perioperative complications potentially associated with their surgeries such as a possibility of postoperative dysphagia following anterior cervical surgeries.
This study has some limitations, including its retrospective database nature with its susceptibility to errors in coding. Moreover, the database does not provide detailed data for individual patients due to privacy issues. The propensity score matching controlled some potential confounding factors, including age, gender, and comorbidities; however, other confounders may have been presented and could not be controlled. The severity of each complication cannot be determined from the database. Additionally, postoperative mortality could not be determined with certainty due to database limitations. Finally, the database does not have reports on functional clinical and radiological outcomes.
Despite these limitations, our propensity-score matched analysis eliminated the confound variables of the study cohorts, making it more accurate in characterizing the complication rates following 3 standard procedures for treating patients with degenerative cervical myelopathy.
Conclusions
Management of degenerative cervical myelopathy with ACDF, laminectomy with fusion, or laminoplasty is associated with certain perioperative complications. The incidence of dysphagia following laminectomy with fusion was not different compared to ACDF. Laminoplasty was associated with the lowest incidence of postoperative new-onset cervicalgia and revisions. The highest incidence of postoperative limb paralysis was associated with posterior laminectomy with fusion, followed by laminoplasty. Understanding the incidence of these complications will help guide spine surgeons and patients in treatment and recovery planning.
Footnotes
Authors’ Note: Location where the work was performed: Department of Orthopaedic Surgery, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA. This study has been carried out in accordance with relevant regulations of the US Health Insurance Portability and Accountability Act (HIPAA). Disclosures outside of submitted work are: ZB-consultancy: Cerapedics (past), Xenco Medical (past), AO Spine (past); Research Support: SeaSpine (past, paid to the institution), Next Science (paid directly to institution), Motion Metrics (paid directly to the institution); North American Spine Society: committee member; Lumbar Spine Society: Co-chair Research committee, AOSpine Knowledge Forum Degenerative: Associate member; AOSNA Research committee—committee member; JCW—Royalties—Biomet, Seaspine, Amedica, DePuy Synthes; Investments/Options—Bone Biologics, Pearldiver, Electrocore, Surgitech; Board of Directors—AO Foundation, Society for Brain Mapping and Therapeutics; Fellowship Funding (paid directly to institution): AO Foundation.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mohamed Kamal Mesregah, MD  https://orcid.org/0000-0002-8047-9159
https://orcid.org/0000-0002-8047-9159
Blake Formanek, BA  https://orcid.org/0000-0003-3557-9350
https://orcid.org/0000-0003-3557-9350
Zorica Buser, PhD  https://orcid.org/0000-0002-5680-0643
https://orcid.org/0000-0002-5680-0643
References
- 1.Meyer F, Borm W, Thome C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Dtsch Arztebl Int. 2008;105(20):366–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Melancia JL, Francisco AF, Antunes JL. Spinal stenosis. Handb Clin Neurol. 2014;119:541–549. [DOI] [PubMed] [Google Scholar]
- 3.Ko S, Choi W, Chae S. Comparison of inter- and intra-observer reliability among the three classification systems for cervical spinal canal stenosis. Eur Spine J. 2017;26(9):2290–2296. [DOI] [PubMed] [Google Scholar]
- 4.Kushchayev SV, Glushko T, Jarraya M, et al. ABCs of the degenerative spine. Insights Imaging. 2018;9(2):253–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dowdell J, Erwin M, Choma T, Vaccaro A, Iatridis J, Cho SK. Intervertebral disk degeneration and repair. Neurosurgery. 2017;80(3S): S46–S54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Altinkaya N, Yildirim T, Demir S, Alkan O, Sarica FB. Factors associated with the thickness of the ligamentum flavum: is ligamentum flavum thickening due to hypertrophy or buckling? Spine (Phila Pa 1976). 2011;36(16): E1093–E1097. [DOI] [PubMed] [Google Scholar]
- 7.Li H, Wang J, Chen G, Li F, Zhu J, Chen Q.Combined upper cervical canal stenosis and cervical ossification of the posterior longitudinal ligament resulting in myelopathy: a case series and literature review. J Clin Neurosci. 2017;45:270–275. [DOI] [PubMed] [Google Scholar]
- 8.Iyer A, Azad TD, Tharin S. Cervical spondylotic myelopathy. Clin Spine Surg. 2016;29(10):408–414. [DOI] [PubMed] [Google Scholar]
- 9.Edwards CC, II, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AF. Cervical myelopathy. current diagnostic and treatment strategies. Spine J. 2003;3(1):68–81. [DOI] [PubMed] [Google Scholar]
- 10.Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976). 2015;40(12): E675–E693. [DOI] [PubMed] [Google Scholar]
- 11.Badhiwala JH, Ahuja CS, Akbar MA, et al. Degenerative cervical myelopathy—update and future directions. Nat Rev Neurol. 2020;16(2):108–124. [DOI] [PubMed] [Google Scholar]
- 12.Ren DJ, Li F, Zhang ZC, et al. Comparison of functional and radiological outcomes between two posterior approaches in the treatment of multilevel cervical spondylotic myelopathy. Chin Med J (Engl). 2015;128(15):20542058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jiang YQ, Li XL, Zhou XG, et al. A prospective randomized trial comparing anterior cervical discectomy and fusion versus plate-only open-door laminoplasty for the treatment of spinal stenosis in degenerative diseases. Eur Spine J. 2017;26(4):1162–1172. [DOI] [PubMed] [Google Scholar]
- 14.Fehlings MG, Barry S, Kopjar B, et al. Anterior versus posterior surgical approaches to treat cervical spondylotic myelopathy: outcomes of the prospective multicenter AOSpine North America CSM study in 264 patients. Spine (Phila Pa 1976). 2013;38(26):2247–2252. [DOI] [PubMed] [Google Scholar]
- 15.Quinn JC, Kiely PD, Lebl DR, Hughes AP. Anterior surgical treatment of cervical spondylotic myelopathy: review article. HSS J. 2015;11(1):15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schroeder GD, Kurd MF, Millhouse PW, Vaccaro AR, Hilibrand AS. Performing an anterior cervical discectomy and fusion. Clin Spine Surg. 2016;29(5):186–190. [DOI] [PubMed] [Google Scholar]
- 17.Muzevic D, Splavski B, Boop FA, Arnautovic KI. Anterior cervical discectomy with instrumented allograft fusion: lordosis restoration and comparison of functional outcomes among patients of different age groups. World Neurosurg. 2018;109:e233–e243. [DOI] [PubMed] [Google Scholar]
- 18.Wu B, Song F, Zhu S. Reasons of dysphagia after operation of anterior cervical decompression and fusion. Clin Spine Surg. 2017;30(5):E554–E559. [DOI] [PubMed] [Google Scholar]
- 19.Lord EL, Cohen JR, Buser Z, et al. Trends, costs, and complications of anterior cervical discectomy and fusion with and without bone morphogenetic protein in the United States Medicare population. Global Spine J. 2017;7(7):603–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singrakhia MD, Malewar NR, Singrakhia SM, Deshmukh SS. Cervical laminectomy with lateral mass screw fixation in cervical spondylotic myelopathy: neurological and sagittal alignment outcome: do we need lateral mass screws at each segment? Indian J Orthop. 2017;51(6):658–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Du W, Zhang P, Shen Y, Zhang YZ, Ding WY, Ren LX. Enlarged laminectomy and lateral mass screw fixation for multilevel cervical degenerative myelopathy associated with kyphosis. Spine J. 2014;14(1):57–64. [DOI] [PubMed] [Google Scholar]
- 22.Mayer M, Meier O, Auffarth A, Koller H. Cervical laminectomy and instrumented lateral mass fusion: techniques, pearls and pitfalls. Eur Spine J. 2015;24 Suppl 2:168–185. [DOI] [PubMed] [Google Scholar]
- 23.Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion: a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009;9(1):31–38. [DOI] [PubMed] [Google Scholar]
- 24.Kurokawa R, Kim P.Cervical laminoplasty: the history and the future. Neurol Med Chir (Tokyo). 2015;55(7):529–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yeh KT, Yu TC, Chen IH, et al. Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosis. J Orthop Surg Res. 2014;9:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lara-Almunia M, Hernandez-Vicente J.Open door laminoplasty: creation of a new vertebral arch. Int J Spine Surg. 2017;11:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang LN, Wang L, Song YM, Yang X, Liu LM, Li T. Clinical and radiographic outcome of unilateral open-door laminoplasty with alternative levels centerpiece mini-plate fixation for cervical compressive myelopathy: a five-year follow-up study. Int Orthop. 2016;40(6):1267–1274. [DOI] [PubMed] [Google Scholar]
- 28.Lee CK, Shin DA, Yi S, et al. Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament. J Neurosurg Spine. 2016;24(1):100–107. [DOI] [PubMed] [Google Scholar]
- 29.Lee HJ, Ahn JS, Shin B, Lee H. C4/5 foraminal stenosis predicts C5 palsy after expansive open-door laminoplasty. Eur Spine J. 2017;26(9):2340–2347. [DOI] [PubMed] [Google Scholar]
- 30.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 31.Cole T, Veeravagu A, Zhang M, Azad TD, Desai A, Ratliff JK. Anterior versus posterior approach for multilevel degenerative cervical disease: a retrospective propensity score-matched study of the MarketScan database. Spine (Phila Pa 1976). 2015;40(13):1033–1038. [DOI] [PubMed] [Google Scholar]
- 32.Kato S, Ganau M, Fehlings MG. Surgical decision-making in degenerative cervical myelopathy—anterior versus posterior approach. J Clin Neurosci. 2018;58:7–12. [DOI] [PubMed] [Google Scholar]
- 33.Piazza M, McShane BJ, Ramayya AG, et al. Posterior cervical laminectomy results in better radiographic decompression of spinal cord compared with anterior cervical discectomy and fusion. World Neurosurg. 2018;110:e362–e366. [DOI] [PubMed] [Google Scholar]
- 34.Cabraja M, Abbushi A, Koeppen D, Kroppenstedt S, Woiciechowsky C. Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: sagittal alignment and clinical outcome. Neurosurg Focus. 2010;28(3): E15. [DOI] [PubMed] [Google Scholar]
- 35.Hitchon PW, Woodroffe RW, Noeller JA, Helland L, Hramakova N, Nourski KV. Anterior and posterior approaches for cervical myelopathy: clinical and radiographic outcomes. Spine (Phila Pa 1976). 2019;44(9):615–623. [DOI] [PubMed] [Google Scholar]
- 36.Barnes M, Liew S. The incidence of infection after posterior cervical spine surgery: a 10 year review. Global Spine J. 2012;2(1):3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bazaz R, Lee MJ, Yoo JU. Incidence of dysphagia after anterior cervical spine surgery: a prospective study. Spine (Phila Pa 1976). 2002;27(22):2453–2458. [DOI] [PubMed] [Google Scholar]
- 38.Siska PA, Ponnappan RK, Hohl JB, Lee JY, Kang JD, Donaldson WF. III. Dysphagia after anterior cervical spine surgery: a prospective study using the swallowing-quality of life questionnaire and analysis of patient comorbidities. Spine (Phila Pa 1976). 2011;36(17):1387–1391. [DOI] [PubMed] [Google Scholar]
- 39.Papavero L, Heese O, Klotz-Regener V, Buchalla R, Schroder F, Westphal M. The impact of esophagus retraction on early dysphagia after anterior cervical surgery: does a correlation exist? Spine (Phila Pa 1976). 2007;32(10):1089–1093. [DOI] [PubMed] [Google Scholar]
- 40.Radcliff KE, Koyonos L, Clyde C, et al. What is the incidence of dysphagia after posterior cervical surgery? Spine (Phila Pa 1976). 2013;38(13):1082–1088. [DOI] [PubMed] [Google Scholar]
- 41.Abdullah KG, Yamashita T, Steinmetz MP, et al. Open-door cervical laminoplasty with preservation of posterior structures. Global Spine J. 2012;2(1):15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mitsunaga LK, Klineberg EO, Gupta MC. Laminoplasty techniques for the treatment of multilevel cervical stenosis. Adv Orthop. 2012;2012:307916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mesregah MK, Buchanan IA, Formanek B, Wang JC, Buser Z. Intra- and post-complications of cervical laminoplasty for the treatment of cervical myelopathy: an analysis of a nationwide database. Spine (Phila Pa 1976). 2020;45(20):E1302–E1311. [DOI] [PubMed] [Google Scholar]
- 44.Ha SM, Kim JH, Oh SH, Song JH, Kim HI, Shin DA. Vertebral distraction during anterior cervical discectomy and fusion causes postoperative neck pain. J Korean Neurosurg Soc. 2013;53(5):288–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Choi MK, Kim SB, Lee JH. Rare intractable cervicalgia related to exaggerated disc height distraction: report of two cases and literature review. J Korean Neurosurg Soc. 2018;61(4):530–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nassr A, Eck JC, Ponnappan RK, Zanoun RR, Donaldson WF, III, Kang JD. The incidence of C5 palsy after multilevel cervical decompression procedures: a review of 750 consecutive cases. Spine (Phila Pa 1976). 2012;37(3):174–178. [DOI] [PubMed] [Google Scholar]
- 47.Bydon M, Macki M, Kaloostian P, et al. Incidence and prognostic factors of c5 palsy: a clinical study of 1001 cases and review of the literature. Neurosurgery. 2014;74(6):595–604. discussion 604-595. [DOI] [PubMed] [Google Scholar]
- 48.Highsmith JM, Dhall SS, Haid RW, Jr, Rodts GE, Jr, Mummaneni PV. Treatment of cervical stenotic myelopathy: a cost and outcome comparison of laminoplasty versus laminectomy and lateral mass fusion. J Neurosurg Spine. 2011;14(5):619–625. [DOI] [PubMed] [Google Scholar]
- 49.Liu W, Hu L, Chou PH, Liu M, Kan W, Wang J. Comparison of anterior decompression and fusion versus laminoplasty in the treatment of multilevel cervical ossification of the posterior longitudinal ligament: a systematic review and meta-analysis. Ther Clin Risk Manag. 2016;12:675–685. [DOI] [PMC free article] [PubMed] [Google Scholar]