Abstract
Study Design:
Retrospective review of consecutive series.
Objective:
The study sought to assess the effect of prolonged pre-operative halo gravity traction (HGT) on the c-spine radiographs
Methods:
Data of 37 pediatric and adult patients who underwent ≥ 12wks pre-op HGT prior to definitive spine surgery from 2013-2015 at a single site in West Africa was reviewed. Radiographic assessment of the c-spine including ADI, SVA and C2-C7 Lordosis were done at pre HGT and at 4 weekly intervals. Paired T-Test was performed to evaluate changes in these parameters during HGT.
Results:
37pts, 18/19 (F/M). Average age 18.2yrs. Diagnoses: 22 idiopathic, 6 congenital, 3 Post TB, 2 NM and 4 NF. Average duration of HGT: 125 days. Baseline coronal Cobb:130 deg, corrected 30% in HGT; baseline sagittal Cobb:146 deg, corrected 32% post HGT. Baseline ADI (3.17 ± 0.63 mm) did not change at 4wks (P > 0.05) but reduced at 8wks (2.80 ± 0.56 mm) and 12wks (2.67 ± 0.51 mm) post HGT (P < 0.05). Baseline HGT SVA (20.7 ± 14.98 mm) significantly improved at 4wks (11.55 ± 10.26 mm), 8wks (7.54 ± 6.78 mm) and 12wks (8.88 ± 4.5 mm) (P < 0.05). Baseline C2-C7 lordosis (43 ± 20.1 deg) reduced at 4wks (26 ± 16.37 deg), 8wks (17.8 ± 14.77 deg) and 12wks (16.7 ± 11.33 deg) post HGT (P < 0.05). There was no incidence of atlanto-axial instability on flexion extension radiographs at any interval.
Conclusion:
Prolonged HGT, while providing partial correction of severe spine deformities, also appeared to have no adverse effect on atlanto-axial stability or cervical alignment. Therefore, HGT can be safely applied for several weeks in the preoperative management of severe spine deformities in pediatric/adult patients.
Keywords: cervical spine, halo gravity traction, atlanto-dental interval, sagittal, vertical axis, sagittal balance
Introduction
Studies have shown the need to view the spine as a unit rather than independent regions in the management of spine deformities.1-3 Thoracolumbar spine deformities have also been found to have concomitant deformities of the cervical spine. 4 Smith et al. (2014) 5 determined that cervical kyphosis and cervical positive sagittal malalignment (C2-C7 SVA ≥ 4 cm) occurs in 31% and 29% respectively in patients with thoracolumbar spine deformities. Changes which occur in one region of the spine lead to changes in the other parts.2-3
Halo gravity traction (HGT) has become an integral part in the preoperative management of patients with severe thoracolumbar spine deformities.6-10 The benefits are immense. Its gradual correction of the deformity allows the spinal cord time to adjust to these changes. It also allows for pre-op optimization of the patient’s nutritional status 6 and pulmonary function.8,10 It can improve curve magnitudes by 30-40% 6-7 and by this HGT helps convert a potentially very risky and complex corrective surgery to a less complicated one. 7 Complications of HGT include pain, pin site infection7-8 cerebral abscess11,12 and brachial plexus nerve palsies. 13 However, the effect of prolonged HGT on the cervical spine parameters has not been adequately reported in literature.
C2-C7 Sagittal Vertical Axis (SVA) and C2-C7 lordosis have been variously used to study the cervical spine and to determine if they have any bearing on the health related quality of life (HRQoL) in patients with thoracolumbar Spine Deformities both pre and post operatively.4,14-16 High C2-C7 SVA has been shown to be associated with high Neck Disability Index (NDI) scores especially when C2-C7 SVA >40 mm. 14 Large baseline C2-C7 SVA and C2-C7 lordosis are generally associated poor HRQoL scores pre-operatively and at follow up time points.14,15 Large pre-op SVA (≥ 4 cm) in thoracolumbar deformities is predictive of failure to reach Minimum Clinically Important Difference (MCID) for HRQoL scores.
Another important radiographic parameter which helps to evaluate c-spine instability is the Atlanto-Dental Interval (ADI).16-21 The normal anterior ADI in healthy adults is less than 3 mm, 17 and it generally decreases with age. 16 Locke et al. 22 reported a maximum normal value of 4 mm and 5 mm in supine and upright positions, respectively. The risk of spinal cord compression increases with increasing ADI. 18 Some authors suggest the need for surgery when ADI is more than 8 mm in patients with Rheumatoid Arthritis.19-20
Reservations among some surgeons, patients and their relatives have been the potential effect of prolonged HGT on the neck and c-spine. However, there is a dearth of literature on the effects of prolonged HGT on these c-spine radiographic parameters, especially in patients with complex spine deformities. Therefore, this study sought to assess the effect of prolonged pre-op HGT on ADI, C2-C7 SVA and C2-C7 lordosis using computer assisted Digital radiography–Picture archiving and communication system (PACS).
Materials and Methods
We retrospectively reviewed the radiographs of 37 patients with severe thoracolumbar spine deformity (sagittal or coronal cobb angle >100 degrees or >100 degrees in both planes) who underwent HGT pre-operatively between 2013 and 2015. Prior to commencement of this study, ethical approval was obtained from the Noguchi Memorial Institute for Medical Research (NMIMR) to use secondary data from the FOCOS Spine registry (Certified Protocol Number: 058/16-17 revd. 2018). Consents were obtained from patients prior to enrollment into the Spine Registry. No additional consents were obtained for this study. Data of patients with cervical spine deformities and congenital patients with cervical abnormalities was excluded from the study. Traction weight was commenced with 20% body weight and gradually increased by 10% weekly as tolerated to a maximum 50% body weight by 4weeks. Patients were kept in continuous traction except during feeding and hygiene. Traction was maintained with walking frame while patients were walking, traction wheelchair while seated and bed traction while in bed and similar weight calibration was maintained for all these devices. Pin sites were inspected and cleaned daily with iodine by medical officers. Patients were evaluated daily by a team of spine surgeons for neurological changes.
X-rays were acquired in the standing position with patients in HGT. Traction was taken off for Flexion–Extension cervical x-rays. The following x-ray measurements were done using the PACS system at 4 weeks, 8 weeks and 12 weeks post HGT: ADI in the neutral, flexion and extension positions; C2-C7 SVA and C2-C7 Cobb angle. A single fellow trained spine surgeon did the measurements.
ADI was measured as the distance between the midpoint of the posterior border of the anterior tubercle of C1 and the anterior margin of the odontoid. The line drawn was kept perpendicular to the posterior border of anterior tubercle of C1 (Figure 1).
Figure 1.

Shows the measurement of Atlanto dental interval (ADI): ADI was measured as the distance between the midpoint of the posterior border of the anterior tubercle of C1 and the anterior margin of the odontoid. ADI was measured as the distance between the 2 lines. The line drawn was kept perpendicular to the posterior border of anterior tubercle of C1.
C2-C7 SVA was measured as the horizontal distance between the antero-inferior edges of C2 and C7 (Figure 2).
Figure 2.
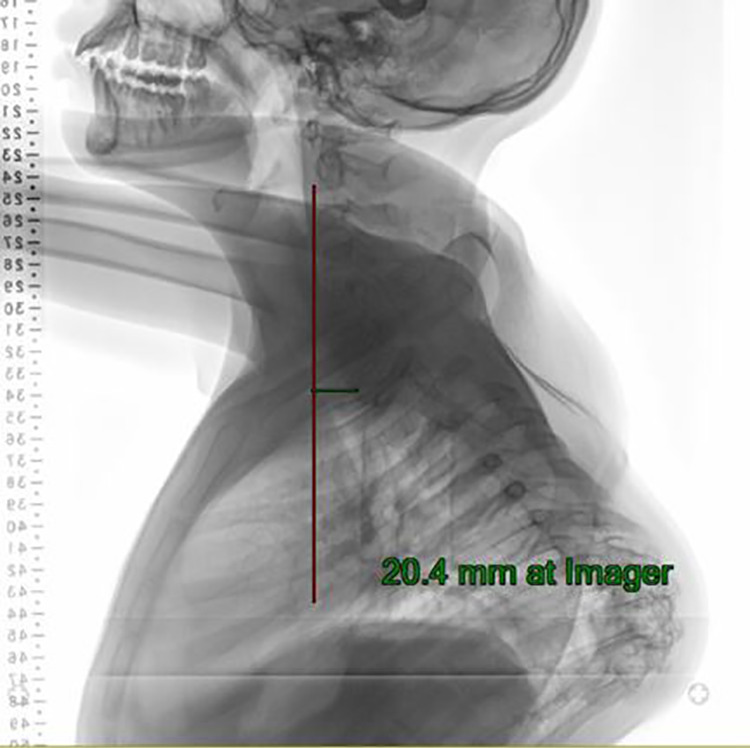
Showing the measurement of C2-C7 Sagittal Vertical Axis (SVA). C2-C7 SVA was measured as the horizontal distance between the antero-inferior edges of C2 and C7.
The C2-C7 Cobb angle was measured as the angle subtended between the inferior end plate of C2 and the inferior end plate of C7 (Figure 3).
Figure 3.

Showing the measurement of C2-C7 Lordosis using computer assisted digital radiography system. The C2-C7 Cobb angle was measured as the angle subtended between the inferior end plate of C2 and the inferior end plate of C7.
Paired t-test was used to evaluate changes from baseline ADI, C2-C7 lordosis and C2-C7SVA parameters. Analysis was performed in Stata 14 software.
Results
37 patients were reviewed and they included 19 males and 18 females with an average age of 18.2 (7-32yrs). The etiologies were: idiopathic (n = 22), congenital (n = 6), Neuromuscular (n = 2), Neurofibromatosis (n = 4) and Post Tuberculous (n = 3). The curve type was Scoliosis (n = 2), Kyphosis (n = 5) and Kyphoscoliosis (n = 30), Table 1.
Table 1.
Demographic and Clinical Characteristics.
| Variable | Category | Frequency | % (N = 37) |
|---|---|---|---|
| Gender | Male | 19 | 51.34 |
| Female | 18 | 48.65 | |
| Curve Etiology | Idiopathic | 22 | 59.46 |
| congenital | 6 | 16.22 | |
| Neuromuscular | 2 | 5.41 | |
| Neurofibromatosis | 4 | 10.81 | |
| Post Tuberculous | 3 | 8.11 | |
| Curve Type | Scoliosis | 2 | 5.41 |
| Kyphosis | 5 | 13.51 | |
| Kyphoscoliosis | 30 | 81.08 |
The average pre HGT body mass index (BMI) was 17.37 ± 2.58 kg/m2 and the average duration of HGT was 125 ± 35 days. The average pre HGT coronal and sagittal Cobb angles were 129.97 deg (77-178) and 146.46 deg (30-233), respectively. The average coronal and sagittal Cobb correction following HGT were 30.35% and 31.75%, respectively (Table 2).
Table 2.
Demographic and Clinical Characteristics.
| Observation (n) | Mean | SD | Min | Max | |
|---|---|---|---|---|---|
| Age | 37 | 18.23 | 5.07 | 7.46 | 32.43 |
| Pre HGT BMI | 37 | 17.37 | 2.58 | 12.31 | 24.70 |
| Pre HGT coronal cobb | 32 | 129.97 | 25.92 | 77 | 178 |
| Pre HGT sagittal cobb | 37 | 146.46 | 46.66 | 30 | 233 |
| Duration in HGT (Days) | 37 | 125.16 | 35.34 | 71 | 239.00 |
| % correction (Coronal) | 31 | 30.35 | 11.00 | 0 | 55.21 |
| % correction (sagittal) | 36 | 31.75 | 14.93 | 0 | 65.73 |
BMI: Body Mass Index; HGT: Halo Gravity Traction.
The average baseline ADI (neutral) was 3.16 ± 0.63 mm and this did not significantly change at 4weeks in HGT (3.07 ± 0.63 mm, P > 0.05) but reduced significantly at 8 weeks in HGT (2.80 ± 0.50 mm, P < 0.05) and at 12weeks in HGT (2.67 ± 0.51 mm, P < 0.05). ADI at 6 weeks post-Op (3.01 ± 0.64 mm, P > 0.05) was not significantly different from baseline values (Table 3). There was no incidence of atlanto-axial instability. The displacement in ADI in flexion and extension at 4wks, 8wks, and 12wks in HGT were all less than 3 mm (Table 4).
Table 3.
Evaluation of Neutral ADI Values in HGT.
| Time-points in HGT | ADI (neutral) | 95% CI |
|---|---|---|
| Pre-HGT (baseline) | 3.16 ± 0.63 | 2.96-3.39 |
| 4weeks in HGT | 3.07 ± 0.63 | 2.84-3.31 |
| 8weeks in HGT | 2.80 ± 0.50** | 2.59-3.00 |
| 12weeks in HGT | 2.67 ± 0.51** | 3.41-2.94 |
| 6weeks post-op | 3.01 ± 0.64 | 2.78-3.25 |
Values are presented as the mean ± SD.
Values with ** indicates that significant difference was observed from baseline values (P < 0.05).
ADI: Atlanto-Dental Interval; CI: Confidence interval of mean estimates.
Table 4.
Evaluation Atlanto-Axial Stability During HGT.
| Time-points in HGT | ADI: Flexion | ADI: Extension | ADI Displacement on dynamic views |
|---|---|---|---|
| Pre-HGT | 3.36 ± 0.78 | 3.12 ± 1.08 | 0.73 ± 0.78 [0.36-1.09] |
| 4weeks in HGT | 3.46 ± 1.02 | 2.79 ± 0.61 | 0.76 ± 0.77 [0.39-1.13] |
| 8weeks in HGT | 3.25 ± 0.63 | 2.72 ± 0.77 | 0.65 ± 0.62 [0.42-0.88] |
| 12weeks in HGT | 3.47 ± 1.26 | 3.12 ± 1.59 | 0.66 ± 0.36 [0.48-0.85] |
| 6weeks post-op | 3.16 ± 0.60 | 2.95 ± 0.93 | 0.59 ± 0.43 [0.39-0.78] |
Values are presented as the mean ± SD.
Values in [] represents 95% Confidence interval of mean estimates
HGT: Halo Gravity Traction; ADI: Atlanto-Dental Interval.
The average baseline C2-C7 SVA was 20.67 ± 14.98 mm. This significantly improved to 11.55 ± 10.26 mm at 4wks post HGT (P < 0.05), 7.55 ± 6.78 mm at 8wk post HGT (P < 0.05) and 8.86 ± 4.55 mm at 12wks (P < 0.05). SVA at 6wks post op was 16.73 ± 14.11 mm which was not significantly different from the baseline value (P > 0.05).
The average baseline C2-C7 Lordosis was 43.12 ± 20.08 deg. This reduced significantly to 25.94 ± 16.37 deg at 4weeks (P < 0.05), 17.75 ± 14.77 deg at 8weeks (P < 0.05), 16.67 ± 11.13 deg at 12weeks (P < 0.05) and 26.28 ± 23.24 deg at 6weeks post-op (P < 0.05), Table 5.
Table 5.
Effect of HGT on C2-C7 SVA, C2-C7 Lordosis and NDI Scores.
| Pre HGT (Baseline) | 4 week HGT | 8 weeks HGT | 12 weeks HGT | 6 weeks post op | |
|---|---|---|---|---|---|
| C2-C7 SVA (mm) | 20.67 ± 14.98 | 11.55 ± 10.26** | 7.55 ± 6.78** | 8.86 ± 4.55** | 16.73 ± 14.11 |
| C2-C7 Lordosis | 43.12 ± 20.08 | 25.94 ± 16.37** | 17.75 ± 14.77** | 16.67 ± 11.13** | 26.28 ± 23.24** |
Values are presented as the mean ± SD.
Values with ** indicates that significant difference was observed from baseline values (P < 0.05).
HGT: Halo Gravity Traction; SVA: Sagittal Vertical Axis (SVA).
Discussion
The primary goal of HGT in most patients in our series was for partial deformity correction. We report a percentage of correction in HGT was about 30% and 32% in the coronal and sagittal planes, respectively. This is consistent with previous studies in similar settings and patients’ characteristics.6-8 The partial deformity correction with HGT helps to reduce the use of 3 column osteotomies (3CO) with the resultant decrease in surgical risk profile of patients. 7
We report that the mean baseline ADI (neutral) was 3.16 mm among our cohort. This reduced significantly at 8weeks in HGT (2.80 mm, P < 0.05) and at 12weeks in HGT (2.67 mm, P < 0.05) but relapsed to baseline at 6weeks post-Op (3.01 mm, P > 0.05). The normative ADI values have been previously described in literature.22-26 Locke et al. 22 reported a maximum normal value of 4 mm and 5 mm in the supine and upright positions, respectively. However, their study did not control for the magnification of radiographic anatomy due to the relative positions of the source of the x-ray, the patient and the x-ray detector. ADI measured from plain radiographs are greater than those measured from computed tomography images and this variation may be attributed to magnification error in the plain radiographs. 23 Cremers et al. 24 obtained a magnification correction factor during their radiographic evaluation of ADI among children with Down Syndrome. This magnification factor could reduce the maximum 4 mm ADI values found by Locke et al to 3.4 mm 24,25 The assessment of ADI with plain radiography appears to have low reliability,22,26 but its assessment with digital radiography may offer a better inter observer reliability over plain radiographs. Douglas et al, 25 for example, reported a maximum ADI value of 3.5 mm in children using digital radiographs. The authors found a higher intra-observer reliability of 0.72 and 0.85, and inter-observer reliability of 0.50. ADI in this instance was measured from the Posterior arch of C1 to anterior cortex dens on upright radiograph. 25 They reported that the mean ADI value in the supine position measured using computer assisted radiography was 2.17 mm with a range of 1.03 mm to 3.23 mm in children (1-12years). 25 Locke et al. 22 using plain radiographs found ADI values to be less than 4 mm in children (3-15years). Liu et al 16 reported that ADI ranges in age groups 18–39 years, 40–59years and ≥60years were 0.85–3.12 mm, 0.71–2.55 mm and 0.00–2.37 mm, respectively. This was among a large series of Chinese patients using computerized tomography (CT) scan imaging.
The average ADI we reported in the present study using digital radiography was higher compared to that of Liu et al 16 which used CT scan for their measurements. The use of CT scan provides more accurate measurement of ADI. 23 This may partly explain the differences observed. Moreover, our study included both pediatric and adult spine deformity patients. Another factor to consider is that we do not as yet have normative ADI measurement for patients with severe spinal deformities. Patients with thoracolumbar kyphoscoliosis tend to have an exaggerated subaxial cervical lordosis. This may be as a result of compensatory flexion at the C1-C2 region resulting in an increase in the ADI of these patients. The average ADI values in flexion-extension while patients were undergoing HGT were less than 3 mm suggesting that HGT did not result in C1/C2 instability. The risk of spinal cord compression is known increase with increasing ADI. 18 Although we observed a statistically significant reduction in ADI values at 8weeks and 12 weeks’ duration in HGT, we believe that in terms of clinical significance it does not make much difference if ADI changes from 3.16 mm to 2.80 or 2.67 mm. Nevertheless, the key message from this study is that there is no significant increase in ADI during prolonged pre-op HGT implying that the risk of spinal cord compression is not increased with the sustained HGT.
We show that baseline C2-C7 SVA reduces significantly at 4weeks, 8weeks, and 12weeks in HGT. Preoperative improvement in cervical alignment after HGT may be compensatory to the partial correction in thoracolumbar deformities after HGT. Scheer and Colleagues 4 reported that large pre-op C2-C7 SVA (≥4 cm) in adult thoracolumbar deformities is predictive of poor post-op outcomes for HRQOL and failure to reach MCID for HRQOL at 2-year follow-up. Protopsaltis et al (2015) 15 also showed that large pre-op C2–7 SVA is associated with high ODI scores, low Physical Component Summary (PCS), and low scores in SRS Activity and Appearance domains.
We report significant reduction in the baseline C2-C7 Lordotic angle preoperatively at 4weeks, 8weeks, and 12 weeks in HGT and at 6weeks post-op. The reduction in cervical lordosis post operatively is similar to results obtained by Scheer et al. 4 though their measurements were done 2years after surgery. Protopsaltis et al (2015) 15 reported that large C2-C7 lordosis is associated with high ODI scores, low Physical Component Summary (PCS), and low scores in SRS Activity and Appearance domains.
One important contribution of this paper is its in-depth evaluation of the potential changes in c-spine during prolonged HGT. Our patients are typically seen when their spine deformities have already progressed. Patients are managed with prolonged pre-operative HGT to attain partial deformity correction and help mitigate surgical risk. 7 However, one concern for some surgeons, patients and their relatives has been the potential effect of prolonged traction on the c-spine. We have shown that long term HGT does not adversely affect cervical radiographic parameters such ADI, C2-C7 SVA and C2-C7 lordosis in pediatric and adult spine deformity patients. We did not record any incidence of brachial plexus palsies or related neurological deficits. On the contrary, we have managed some pre-op myelopathic patients with severe cervicothoracic deformities with satisfactory improvement after HGT and corrective surgery. Therefore, these findings help address the concerns of spinal surgeons interested in this technique.
Despite the merits of the paper, there were limited studies on the effect of HGT on these cervical parameters for discussion. In addition, we did not have adequate sample of patients with different etiologies to perform sub-group analysis. Moreover, the findings only reflect short term radiographic outcomes. We do not know what these results mean in the long-term for these patients.
Conclusion
Prolonged HGT, while providing partial correction of severe spine deformities, also appeared to have no adverse effect on atlanto-axial stability or cervical alignment. The results of this study show that HGT can be safely applied for several weeks in the pre-operative management of severe spine deformities in the pediatric and adult patients.
Footnotes
Authors’ Note: Harry Akoto currently practices as a consultant neurosurgeon at the Korle-Bu Teaching Hospital, P. O. Box KB 77, Accra-Ghana. Cristina Sacramento-Domínguez currently practices as a consultant orthopaedic spine surgeon at the Clınica Universidad de Navarra, Madrid, Spain. Rufai Mahmud is currently in private practice. OBA (grants, personal fees and other from K2 M, other from WEIGAO, outside the submitted work).
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Henry Ofori Duah, RN, MPH  https://orcid.org/0000-0002-4842-6006
https://orcid.org/0000-0002-4842-6006
Gerhard Ofori-Amankwah, MD  https://orcid.org/0000-0002-9692-3453
https://orcid.org/0000-0002-9692-3453
References
- 1.Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine. 2013. 15;38(22S):S149–S160. [DOI] [PubMed] [Google Scholar]
- 2.Klineberg E, Schwab F, Ames C, et al. Acute reciprocal changes distant from the site of spinal osteotomies affect global postoperative alignment. Adv Orthoped. 2011;2011:415946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ha Y, Schwab F, Lafage V, et al. Reciprocal changes in cervical spine alignment after corrective thoracolumbar deformity surgery. Eur Spine J. 2014;23(3):552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scheer JK, Passias PG, Sorocean AM, et al. Association between preoperative cervical sagittal deformity and inferior outcomes at 2-year follow-up in patients with adult thoracolumbar deformity: analysis of 182 patients: Presented at the 2015 AANS/CNS Joint Section on Disorders of the Spine and Peripheral Nerves. J Neurosurg Spine. 2016;24(1):108–115. [DOI] [PubMed] [Google Scholar]
- 5.Smith JS, Lafage V, Schwab FJ, et al. Prevalence and type of cervical deformity among 470 adults with thoracolumbar deformity. Spine. 2014;39(17):E1001–E1009. [DOI] [PubMed] [Google Scholar]
- 6.Nemani VM, Kim HJ, Bjerke-Kroll BT, et al. Preoperative halo-gravity traction for severe spinal deformities at an SRS-GOP site in West Africa: protocols, complications, and results. Spine. 2015;40(3):153–161. [DOI] [PubMed] [Google Scholar]
- 7.Iyer S, Boachie-Adjei O, Duah HO, et al. Halo gravity traction can mitigate preoperative risk factors and early surgical complications in complex spine deformity. Spine. 2019;44(9):629–636. [DOI] [PubMed] [Google Scholar]
- 8.Bogunovic L, Lenke LG, Bridwell KH, Luhmann SJ. Preoperative halo-gravity traction for severe pediatric spinal deformity: complications, radiographic correction and changes in pulmonary function. Spine Deform. 2013;1(1):33–39. [DOI] [PubMed] [Google Scholar]
- 9.Bouchoucha S, Khelifi A, Saied W, Ammar C, Nessib MN, Ben Ghachem M. Progressive correction of severe spinal deformities with halo-gravity traction. Acta Orthop Belg. 2011;77(4):529. [PubMed] [Google Scholar]
- 10.Koller H, Zenner J, Gajic V, Meier O, Ferraris L, Hitzl W. The impact of halo-gravity traction on curve rigidity and pulmonary function in the treatment of severe and rigid scoliosis and kyphoscoliosis: a clinical study and narrative review of the literature. Eur Spine J. 2012;21(3):514–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ray A, Iyer RV, King AT. Cerebral abscess as a delayed complication of halo fixation. Acta Neurochirur. 2006;148(9):1015–1016. [DOI] [PubMed] [Google Scholar]
- 12.Gelalis ID, Christoforou G, Motsis E, Arnaoutoglou C, Xenakis T. Brain abscess and generalized seizure caused by halo pin intracranial penetration: case report and review of the literature. Eur Spine J. 2009;18(2):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bang-ping Q, Yong Q, Bin W, Yang Y, Ze-zhang Z. Brachial plexus palsy caused by halo traction before posterior correction in patients with severe scoliosis. Chin J Traumatol. 2007;10(5):294–298. [PubMed] [Google Scholar]
- 14.Tang JA, Scheer JK, Smith JS, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurgery. 2012;71(3):662–669. [DOI] [PubMed] [Google Scholar]
- 15.Protopsaltis TS, Scheer JK, Terran JS, et al. How the neck affects the back: changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine. 2015;23(2):153–158. [DOI] [PubMed] [Google Scholar]
- 16.Liu K, Xie F, Wang D, et al. Reference ranges for atlantodental interval in adults and its variation with age and gender in a large series of subjects on multidetector computed tomography. Acta Radiol. 2015;56(4):465–470. [DOI] [PubMed] [Google Scholar]
- 17.Krauss WE, Bledsoe JM, Clarke MJ, Nottmeier EW, Pichelmann MA. Rheumatoid arthritis of the craniovertebral junction. Neurosurgery. 2010;66(3):A83–A95. [DOI] [PubMed] [Google Scholar]
- 18.Joaquim AF, Ghizoni E, Tedeschi H, Appenzeller S, Riew KD. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg Focus. 2015;38(4):E4. [DOI] [PubMed] [Google Scholar]
- 19.Boden SD, Dodge LD, Bohlman HH, Rechtine GR. Rheumatoid arthritis of the cervical spine. A long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am. 1993;75(9):1282–1297. [DOI] [PubMed] [Google Scholar]
- 20.Boden SD.Rheumatoid arthritis of the cervical spine: surgical decision making based on predictors of paralysis and recovery. Spine. 1994;19(20):2275–2280. [DOI] [PubMed] [Google Scholar]
- 21.Chen Y, Zhuang Z, Qi W, et al. A three-dimensional study of the atlantodental interval in a normal Chinese population using reformatted computed tomography. Surg Radiol Anat. 2011;33(9):801–806. [DOI] [PubMed] [Google Scholar]
- 22.Locke GR, Gardner JI, Van Epps EF. Atlas-dens interval (ADI) in children: a survey based on 200 normal cervical spines. Am J Roentgenol. 1966;97(1):135–140. [DOI] [PubMed] [Google Scholar]
- 23.Pueschel SM, Moon AC, Scola FH. Computerized tomography in persons with Down syndrome and atlantoaxial instability. Spine. 1992;17(7):735–737. [DOI] [PubMed] [Google Scholar]
- 24.Cremers MJ, Ramos L, Bol E, Van Gijn J. Radiological assessment of the atlantoaxial distance in Down’s syndrome. Arch Dis Child. 1993;69(3):347–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Douglas TS, Sanders V, Machers S, Pitcher R, van As AB. Digital radiographic measurement of the atlantodental interval in children. J Pediatr Orthop. 2007;27(1):23–26. [DOI] [PubMed] [Google Scholar]
- 26.Hinck VC, Hopkins CE. Measurement of the atlanto-dental interval in the adult. Am J Roentgenol, Radium Ther Nucl Med. 1960;84:945–951. [PubMed] [Google Scholar]


