Abstract
Objective
To evaluate the association of initial blood lactate with mortality and subsequent septic shock in non-shock septic patients.
Materials and methods
A retrospective cohort study was conducted at Maharaj Nakorn Chiang Mai Hospital, Chiang Mai University, Muang, Chiang Mai, Thailand. Inclusion criteria included septic patients admitted to a non-critical medical ward and had initial serum lactate at the emergency department (ED). Shock and other causes of hyperlactatemia were excluded.
Results
A total of 448 admissions were included with median age [interquartile range (IQR)] of 71 (59, 87) years and 200 males (44.6%). Pneumonia was the most common cause of sepsis (47.5%). The median systemic inflammatory response syndrome (SIRS) and quick sequential organ failure assessment (qSOFA) scores were 3 (2, 3) and 1 (1, 2), respectively. The median initial blood lactate was 2.19 (1.45, 3.23) mmol/L. The high blood lactate (≥2 mmol/L) group; N = 248, had higher qSOFA and other predictive scores and had significantly higher 28 days mortality (31.9% vs 10.0%; p < 0.001) and subsequent 3 days septic shock (18.1% vs 5.0%; p < 0.001) than the normal blood lactate group; N = 200. A combination of blood lactate above or equal to 2 mmol/L plus the national early warning score (NEWS) above or equal to 7 showed the highest prediction of 28 days mortality with the area under receiver-operating characteristic curve (AUROC) of 0.70 [95% confidence interval (CI): 0.65–0.75].
Conclusions
An initial blood lactate level above or equal to 2 mmol/L is associated with high mortality and subsequent septic shock among non-shock septic patients. The composite of blood lactate levels and other predictive scores yields better accuracy to predict mortality.
How to cite this article
Noparatkailas N, Inchai J, Deesomchok A. Blood Lactate Level and the Predictor of Death in Non-shock Septic Patients. Indian J Crit Care Med 2023;27(2):93–100.
Keywords: Early sepsis, Mortality, Non-shock, Sepsis, Serum lactate
Highlights
A high initial blood lactate level (≥2 mmol/L) is associated with high mortality and subsequent septic shock among non-shock septic patients.
The combination of blood lactate levels and clinical predictive scores, such as the NEWS, yields better accuracy to predict mortality.
Introduction
Sepsis is a syndrome of life-threatening organ dysfunction caused by a dysregulated host response to infection ranging from early sepsis to septic shock.1 In 2016, the Sepsis-3 Task Force recommended the use of the sepsis-related SOFA score as one of the diagnostic criteria because of the high accuracy to predict mortality.1,2 However, SOFA scores need multiple laboratory assessments, which may not be suitable for early septic patients, especially during their first presentation at the ED. The qSOFA score was proposed as a screening tool for patients outside the intensive care unit (ICU).1,2 Despite the simplicity, previous studies showed poor sensitivity of qSOFA in ED and non-ICU septic patients.3–5 To predict the adverse outcomes in early septic patients at the ED, initial blood lactate levels may be a potential predictor.
Increased blood lactate levels have demonstrated an association with worse outcomes such as mortality.6–10 Sepsis bundle has recommended measuring blood lactate level in every patient with severe sepsis and septic shock, as it may represent tissue hypoperfusion and tissue hypoxia.11,12 Initial lactate level greater than 2 mmol/L has been suggested as a cut point for hemodynamic resuscitation.12 However, the utility of lactate levels in early sepsis is still unknown because most previous trials included severe sepsis and septic shock. The objective of this study was to evaluate the association between initial blood lactate levels and adverse outcomes in early septic patients.
Materials and Methods
Study Design and Setting
This was a single-center, retrospective cohort study of patients presenting to the ED at Maharaj Nakorn Chiang Mai Hospital – a university, tertiary care hospital located in the Northern part of Thailand (Chiang Mai University, Muang, Chiang Mai, Thailand). The study period was from January 2018 to December 2018. The study protocol was approved by our center Research Ethics Committee (study code: MED-2562-06304); Thai Clinical Trials Registry No.: TCTR20220531004.
All patients were initially assessed at the ED by the emergency physician. History and physical examination were obtained to identify the source of the infection. Systemic inflammatory response syndrome criteria and qSOFA score were evaluated through our institutional sepsis protocol, which was adapted from the surviving sepsis campaign bundle.11,12 The SOFA score may be completely recorded if arterial blood gases and other laboratory tests were performed. Besides the SOFA score, NEWS13 was also used in our center.
Initial laboratory investigations and management at ED included the following: Hemoculture, venous blood lactate level, empiric broad-spectrum antibiotics, and intravenous fluid administration. Before admission to the medical ward, every patient was evaluated again by the internists to confirm the diagnosis and adjust proper management.
Patients
Patients aged 18 years or older who were admitted to a non-critical medical ward with a diagnosis of sepsis at ED were enrolled in the analysis. Patients whose initial blood lactate was not obtained at ED, who had any type of shock or cardiac arrest, seizure at presentation, and concurrent use of metformin were excluded from this study.
Definition
Sepsis was defined as the patient with suspected or confirmed infection who either met the SIRS criteria or qSOFA score of two or greater. Despite the new definition, the SOFA score was not completely collected in every patient, especially in normotensive patients. We chose SIRS as one of the inclusion criteria because was routinely used in our center.
Systemic inflammatory response syndrome criteria (range: 0–4) was defined by two or more of the following: (1) Respiratory rate greater than 20 breaths/minute or PaCO2 less than 32 mm Hg; (2) temperature greater than 38°C or less than 36°C; (3) heart rate greater than 90 beats/minute; and (4) white blood cell count greater than 12,000 or less than 4000 cells/mm3 or more than 10% band forms.14 The qSOFA score (range: 0–3) includes a respiratory rate of 22 breaths/minute or greater, abnormal mental status (Glasgow coma scale score of 14 or less), and systolic blood pressure of 100 mm Hg or less.1
Septic shock was defined as sepsis with persisting hypotension requiring vasopressors to maintain mean arterial pressure (MAP) above or equal to 65 mm Hg and having serum lactate level above 2 mmol/L.1
Sample Size Estimation
According to a previous study,8 the 28 days mortality rate in septic patients without shock was 18.3%. Using a Cox proportional hazards model for a retrospective study, 358 patients were needed with a two-sided α level of 0.05 and a trailing power of 80%.
Data Collection
The data were obtained from the electronic medical record. All non-critical ward admissions with the International Classification of Diseases (ICD)-10 based diagnosis of infectious disease were screened. Patients whose initial blood lactate was not measured were excluded. After the exclusion of other ineligible patients, SIRS criteria and qSOFA score were calculated for the final analysis.
The components of SIRS criteria, qSOFA, SOFA score, and NEWS; blood lactate level; source and site of infection; microbiological data; the amount of intravenous fluid during ED stay; time to initial antibiotic at ED; initial effective antibiotic regarding the microbiological results; 28 days mortality and 3 days septic shock status.
Initial blood lactate levels of 2 or more mmol/L were stratified as the high blood lactate group. The cut point of 2 mmol/L was chosen based on the “hour-1 bundle” of the surviving sepsis campaign bundle.12 Concerning the clinical application, the cut point value of each tool (SIRS ≥2, qSOFA ≥2, and NEWS ≥7) were selected based on the guideline's recommendations.1,12,13
Outcomes
The primary outcome was 28 days mortality. The secondary outcome was a 3 days subsequent in-hospital septic shock.
Statistical Analysis
The categorical variables were presented as a percentage, while the continuous variables were presented as median with IQR. The Mann–Whitney U test was used to compare the non-normally distributed continuous variables, and Fisher's exact test was used for categorical variables.
A receiver-operating characteristic (ROC) curve was analyzed to assess the cut point of qSOFA score, and NEWS related to 28 days mortality. The prognostic accuracy of those predictive scores, as a screening tool for early septic patients, were compared with and without blood lactate level combination. Focusing on screening to detect early septic patients, we excluded the SOFA score in this comparison due to incomplete components of this score.
Survival analysis was determined using the Kaplan–Meier method. Univariable and multivariable Cox proportional hazard regression were performed to evaluate predictive factors for 28 days mortality which were described as hazard ratio (HR) with a 95% CI. A p < 0.05 was considered significant. All statistical analysis was computed by statistical package for the social sciences (SPSS), version 23.0 (IBM), and STATA 16.1 (STATA Corporation, College Station, TX).
Results
Baseline Patient Characteristics
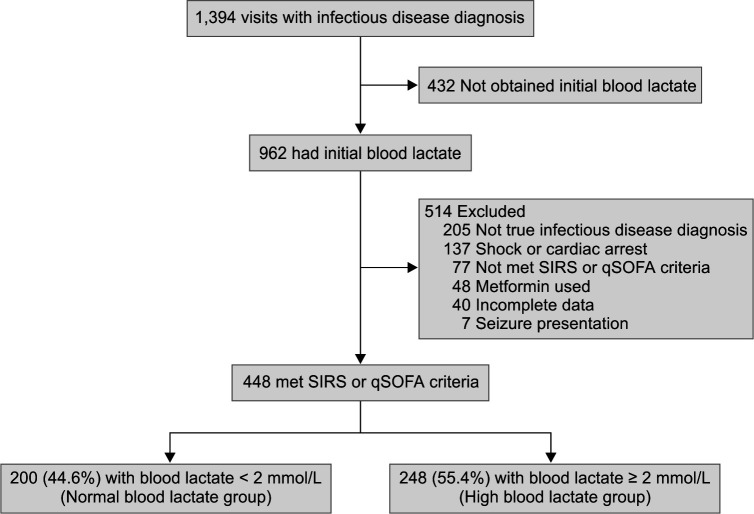
A total of 448 admissions were included in this cohort (Flowchart 1). The median age IQR was 71 (59, 87) years and 200 (44.6%) were males. The most prevalent comorbidities were cancer (29.9%), cerebrovascular accident (19.6%), and diabetes mellitus (19.0%). Only 284 admissions (63.4%) had a complete measurement of the SOFA score, because of the lack of arterial blood gas assessment. Median IQR of SIRS criteria, qSOFA score, and NEWS were 3 (2, 3), 1 (1, 2), and 7 (5, 9), respectively. The overall median blood lactate level IQR was 2.19 (1.45, 3.23) mmol/L. Pneumonia was the most common infection (47.5%) followed by urinary tract infection (17.6%).
Flowchart 1.
Flow diagram of patient selection
A total of 248 admissions (55.4%) were categorized to a high blood lactate group, which had a median IQR of 3.07 (2.46, 4.22) mmol/L. Compared with the normal blood lactate group, cancer (35.1% vs 23.5%; p = 0.008) and cirrhosis (6.9% vs 2.5%; p = 0.046) were of higher prevalence. The median of all four clinical predictive scores was significantly higher in the high blood lactate group (Table 1). Both groups had similar proportions of the source of infection and the final diagnosis of infection except for intraabdominal infection which was more prevalent in the high blood lactate group (12.1% vs 5.5%; p = 0.016).
Table 1.
Baseline characteristics of normal (<2 mmol/L) and High (≥2 mmol/L) blood lactate level groups
| Characteristics | Blood lactate <2 mmol/L (n = 200) | Blood lactate ≥2 mmol/L (n = 248) | p-value |
|---|---|---|---|
| Age, years | 71.5 (59.0, 81.0) | 70.0 (59.0, 82.0) | 0.965 |
| Male gender, n (%) | 78 (39.0) | 122 (49.2) | 0.031 |
| Underlying diseases, n (%) | |||
| Coronary artery disease | 16 (8.0) | 18 (7.3) | 0.768 |
| Congestive heart failure | 26 (13.0) | 32 (12.9) | 0.976 |
| Chronic obstructive pulmonary disease | 23 (11.5) | 34 (13.7) | 0.485 |
| Cerebrovascular accident | 39 (19.5) | 49 (19.8) | 0.946 |
| Diabetes mellitus | 41 (20.5) | 44 (17.7) | 0.459 |
| End-stage renal disease | 29 (14.5) | 22 (8.9) | 0.062 |
| Cirrhosis | 5 (2.5) | 17 (6.9) | 0.046 |
| Cancer | 47 (23.5) | 87 (35.1) | 0.008 |
| Immunocompromised status | 20 (10.0) | 14 (5.6) | 0.084 |
| Vital signs | |||
| Body temperature (C) | 38.2 (37.6, 38.9) | 38.0 (37.0, 38.8) | 0.011 |
| Heart rate (beats/minute) | 104.5 (92.0, 115.0) | 110.0 (98.25, 121.75) | 0.001 |
| Respiratory rate (breaths/minute) | 24.0 (20.5, 30.0) | 24.0 (20.0, 32.0) | 0.283 |
| Systolic blood pressure (mm Hg) | 126.0 (109.25, 153.0) | 125.0 (105.0, 145.0) | 0.207 |
| Diastolic blood pressure (mm Hg) | 70.0 (60.0, 81.0) | 71.0 (59.0, 83.75) | 0.737 |
| MAP (mm Hg) | 90.0 (77.4, 103.25) | 90.7 (75.7, 102.6) | 0.625 |
| Hypotension at presentation, n (%) | 16 (8.0) | 31 (12.5) | 0.122 |
| Oxygen saturation (%) | 94.0 (90.0, 97.0) | 94.0 (90.0, 97.0) | 0.565 |
| Glasgow coma scale | 15 (15, 15) | 15 (14, 15) | 0.010 |
| Laboratory | |||
| Hemoglobin (gm/dL) | 10.8 (9.1, 12.5) | 11.2 (9.3, 13.0) | 0.052 |
| White blood cell count (cells/mm3) | 10,310 (7,117, 14,267) | 12,745 (7,190, 18,717) | 0.007 |
| Platelet count (× 103/mm3) | 238.5 (163.5, 317.5) | 225.0 (148.75, 307.5) | 0.213 |
| Creatinine (mg/dL) | 1.06 (0.68, 2.18) | 1.06 (0.72, 1.98) | 0.689 |
| Total bilirubin (mg/dL) | 0.57 (0.37, 0.91) | 0.87 (0.49, 1.74) | <0.001 |
| Lactate level (mmol/L) | 1.37 (1.12, 1.65) | 3.07 (2.46, 4.22) | <0.001 |
| Arterial blood gases exam, n (%) | 125 (62.5) | 159 (64.1) | 0.725 |
| PaO2/FiO2 | 295.2 (238.1, 359.4) | 304.8 (234.0, 361.9) | 0.905 |
| Clinical predictive score | |||
| SIRS criteria | 3 (2, 3) | 3 (2, 3) | 0.020 |
| SIRS criteria ≥2, n (%) | 191 (95.5) | 237 (95.6) | 0.974 |
| qSOFA score | 1 (1, 1) | 1 (1, 2) | 0.046 |
| qSOFA score ≥2, n (%) | 49 (24.5) | 83 (33.5) | 0.038 |
| SOFA measurement, n (%) | 125 (62.5) | 159 (64.1) | 0.725 |
| SOFA score | 3 (2, 5) | 4 (3, 6) | 0.002 |
| NEWS score | 7.0 (5.0, 8.0) | 7.5 (5.0, 10.0) | 0.013 |
| Source of infection, n (%) | |||
| Hospital acquired | 83 (41.5) | 117 (47.2) | 0.229 |
| Site of infection, n (%) | |||
| Pneumonia | 102 (51.0) | 111 (44.8) | 0.188 |
| Urinary tract infection | 31 (15.5) | 48 (19.4) | 0.287 |
| Intraabdominal infection | 11 (5.5) | 30 (12.1) | 0.016 |
| Other | 13 (6.5) | 14 (5.6) | 0.705 |
| Unknown | 43 (21.5) | 45 (18.1) | 0.374 |
Data are presented as median IQR or n (%). FiO2, fraction of inspired oxygen; NEWS, national early warning score; PaO2, partial pressure of oxygen in arterial blood; qSOFA, quick SOFA; SIRS, systemic inflammatory response syndrome; SOFA, sequential (sepsis-related) organ failure assessment
During ED stay, the high blood lactate group received a larger amount of intravenous fluid. The time to administration of the first empiric antibiotics was similar in both groups (Table 2). The positive initial hemoculture was higher in the high blood lactate group than the normal blood lactate group (24.2% vs 13.5%; p = 0.004); nevertheless, the effectiveness of initial antibiotics was not different (72.6% vs 76.0%; p = 0.595).
Table 2.
Baseline initial management during ED stay
| Variables | Blood lactate <2 mmol/L (n = 200) | Blood lactate ≥2 mmol/L (n = 248) | p-value |
|---|---|---|---|
| Volume of IV fluid (mL) | 300 (100, 700) | 500 (200, 1,100) | <0.001 |
| Volume of IV fluid ≥1500 mL, n (%) | 12 (6.0) | 48 (19.4) | <0.001 |
| Initial antibiotics administration, n (%) | 187 (93.5) | 238 (96.0) | 0.239 |
| Time to received antibiotics (minutes) | 48.0 (30.0, 85.0) | 46.5 (26.0, 89.25) | 0.724 |
| Antibiotics within first 60 minutes, n (%) | 116 (58.0) | 147 (59.3) | 0.785 |
| Positive initial hemoculture, n (%) | 27 (13.5) | 60 (24.2) | 0.004 |
| Effectiveness of initial antibiotics, n (%) | 57 (76.0) | 90 (72.6) | 0.595 |
Data are presented as median IQR or n (%). IV, intravenous
Outcomes
Initial Lactate Level as a Predictor of Adverse Outcomes
The overall 28 days mortality rate was 22.1% (99 of 448) and septic shock after 72 hours of admission was 12.3% (55 of 448). In the high blood lactate group, 28 days mortality and subsequent 3 days septic shock were 31.9 and 18.1%, respectively (Table 3). An initial blood lactate level of 2 or more mmol/L was associated with increased 28 days mortality (HR, 3.64; 95% CI: 2.23–5.95; p < 0.001) (Fig. 1).
Table 3.
Primary and secondary outcomes
| Outcomes | Blood lactate <2 mmol/L (n = 200) | Blood lactate ≥2 mmol/L (n = 248) | p-value |
|---|---|---|---|
| 28 days mortality, n (%) | 20 (10.0) | 79 (31.9) | <0.001 |
| 3 days septic shock, n (%) | 10 (5.0) | 45 (18.1) | <0.001 |
Fig. 1.
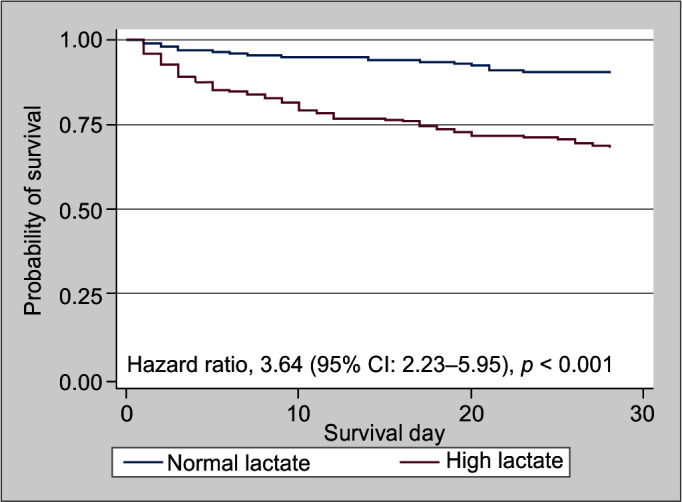
Kaplan–Meier survival curves or 28-day survival according to lactate level
Univariate analysis with baseline variables, clinical predictive scores, and blood lactate level was shown in Table 4. After multivariable analysis, high initial blood lactate level remained an independent factor associated with 28 days mortality (HR: 3.14; 95% CI: 1.91–5.16; p < 0.001). Other associated factors were cancer as a comorbidity (HR: 3.98; 95% CI: 2.54–6.22; p < 0.001) and NEWS above or equal to 7 (HR: 2.28; 95% CI: 1.38–3.76; p = 0.001) (Table 4).
Table 4.
Univariate and multivariate Cox proportional hazards regression models of 28 days mortality
| Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|
| Characteristics | HR | 95% CI | p-value | HR | 95% CI | p-value |
| Male gender | 1.57 | 1.06–2.33 | 0.026 | 1.29 | 0.85–1.94 | 0.229 |
| Cerebrovascular accident | 1.55 | 0.99–2.43 | 0.053 | |||
| Diabetes | 0.50 | 0.27–0.94 | 0.031 | 0.66 | 0.34–1.25 | 0.66 |
| Cirrhosis | 1.46 | 0.68–3.15 | 0.334 | |||
| Cancer | 4.07 | 2.72–6.07 | <0.001 | 3.98 | 2.54–6.22 | <0.001 |
| Hypotension at presentation | 1.72 | 1.01–2.95 | 0.046 | 1.20 | 0.67–2.14 | 0.537 |
| SIRS criteria ≥2 | 2.38 | 0.59–9.64 | 0.226 | |||
| qSOFA score ≥2 | 1.94 | 1.30–2.89 | 0.001 | 1.48 | 0.93–2.36 | 0.096 |
| NEWS ≥7 | 2.16 | 1.37–3.40 | 0.001 | 2.28 | 1.38–3.76 | 0.001 |
| Lactate level ≥2 mmol/L | 3.64 | 2.23–5.95 | <0.001 | 3.14 | 1.91–5.16 | <0.001 |
| Hospital source | 1.77 | 1.19–2.64 | 0.005 | 1.01 | 0.66–1.56 | 0.948 |
CI, confidence interval; HR, hazard ratio; NEWS, national early warning score; qSOFA, quick sequential (sepsis-related) organ failure assessment; SIRS, systemic inflammatory response syndrome
Comparison of Lactate and Clinical Predictive Scores
The AUROC with 95% CI to predict 28 days mortality of blood lactate level, SIRS criteria, qSOFA score, and NEWS were 0.68 (0.62–0.74), 0.51 (0.45–0.56), 0.61 (0.55–0.66), and 0.64 (0.58–0.71), respectively. The AUROC of blood lactate level was significantly higher than the AUROC of SIRS criteria (p < 0.001) but was similar to other scores.
The clinical predictive scores with each cut point were combined with blood lactate levels to assess predictive validity (Table 5). The highest AUROC was shown with the combination of blood lactate level above or equal to 2 mmol/L and NEWS above or equal to 7 (0.70; 95% CI: 0.65–0.75) (Fig. 2).
Table 5.
Screening performance characteristics of lactate level, SIRS criteria, qSOFA score, NEWS, and their combinations
| Criteria | AUROC% (95% CI) | Sensitivity% (95% CI) | Specificity% (95% CI) | NPV% (95% CI) | PPV% (95% CI) |
|---|---|---|---|---|---|
| Lactate level ≥2 mmol/L | 0.66 (0.61–0.70) | 79.8 (70.5–87.2) | 51.6 (46.2–56.9) | 90.0 (85.0–93.8) | 31.9 (26.1–38.0) |
| SIRS criteria ≥2 | 0.52 (0.50–0.53) | 98.0 (92.9–99.8) | 5.2 (3.1–8.0) | 90.0 (68.3–98.8) | 22.7 (18.8–26.9) |
| qSOFA score ≥2 | 0.58 (0.53–0.64) | 42.4 (32.5–52.8) | 74.2 (69.3–78.7) | 82.0 (77.3–86.0) | 31.8 (24.0–40.5) |
| NEWS ≥7 | 0.60 (0.55–0.65) | 74.7 (65.0–82.9) | 44.4 (39.1–49.8) | 86.1 (80.2–90.8) | 27.6 (22.3–33.4) |
| SIRS criteria ≥2 and lactate level ≥2 mmol/L | 0.67 (0.62–0.71) | 78.8 (69.4–86.4) | 54.4 (49.1–59.8) | 90.0 (85.2–93.7) | 32.9 (27.0–39.3) |
| qSOFA score ≥2 and lactate level ≥2 mmol/L | 0.69 (0.64–0.75) | 35.4 (26.0–45.6) | 86.2 (82.2–89.7) | 82.5 (78.2–86.2) | 42.2 (31.4–53.5) |
| NEWS ≥7 and lactate level ≥2 mmol/L | 0.70 (0.65–0.75) | 58.6 (48.2–68.4) | 72.5 (67.5–77.1) | 86.1 (81.6–89.8) | 37.7 (30.0–45.8) |
AUROC, area under receiver-operating characteristic curve; CI, confidence interval; NEWS, national early warning score; NPV, negative predictive value; PPV, positive predictive value; qSOFA, quick sequential (sepsis-related) organ failure assessment; SIRS, systemic inflammatory response syndrome
Fig. 2.
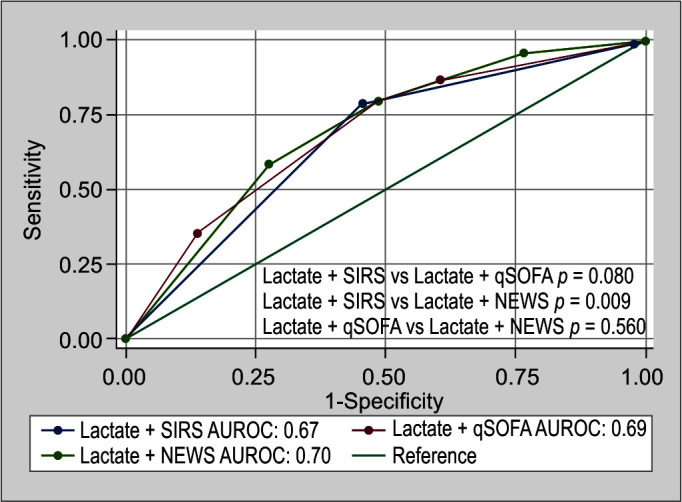
Graph showing AUROC of the combination between lactate level above or equal to 2 mmol/L and other predictive scores with cut-off value for predicting 28-day mortality
Discussion
This study demonstrated that even in non-shock septic patients, initial blood lactate was an independent factor of adverse outcomes. Studies focused on normotensive sepsis were limited. Mikkelsen et al.8 showed that blood lactate above or equal to 2 mmol/L was associated with increased 28 days mortality even in non-shock septic patients, whereas Casserly et al.15 found the association between increasing blood lactate level and in-hospital mortality even in the absence of hypotension. The adjusted odds ratio of in-hospital mortality in the normotensive patients with blood lactate above 4 mmol/L was not significantly higher than in the patients with blood lactate below or equal to 4 mmol/L.
Underlying malignancy was also the associated factor of death in our study. Infection is a common complication of patients with malignancy due to its host dysregulation and immunosuppression from treatment.16 In the absence of hypotension, we found a significantly higher proportion of high blood lactate group in patients with cancer which may indicate a unique metabolism of lactate in this group. Alteration of lactate production and transportation in patients with cancer was demonstrated in a recent study.17
Non-shock septic patients were the focused group in this observation. The stage of sepsis which had a lactate level above or equal to 4 mmol/L with normal blood pressure was referred to as “cryptic shock.”18 The in-hospital mortality of cryptic shock varied from 7.0–35.2% which was lower than that of septic shock.15,18,19 Thus, a screening tool for normotensive patients during the early period of infection, especially in ED, is essential.
To screen patients with early sepsis, the Sepsis-3 Take Force recommended the use of qSOFA as a screening tool due to similar predictive validity with SOFA.1 In our study, we confirmed the higher AUROC of qSOFA score than that of SIRS criteria. This was also shown in other previous ED population studies.2,20,21 However, qSOFA score above or equal to 2 had significantly lower sensitivity than SIRS criteria in our study as shown in other recent studies.3–5 These findings reflected the screening problem of qSOFA.
The poor sensitivity of qSOFA may be explained by that there are only three clinical parameters in qSOFA, whereas NEWS uses many parameters. We demonstrated this concept with the higher sensitivity of NEWS above or equal to 7 (74.7%) than qSOFA score above or equal to 2 (42.4%) which was also reported as a high accuracy scoring in other observations.22,23 As it is a non-laboratory-based test and also easy to repeat, NEWS may be a substitute screening tool. The current sepsis guidelines have not recommended using qSOFA as a single screening tool for sepsis.24
Initial high blood lactate levels in our study had the highest prediction of mortality and subsequent septic shock which was not different from the clinical screening tools (qSOFA and NEWS). Liu et al.25 also found blood lactate levels had similar AUROC for predicting mortality as SOFA score in severe sepsis patients.
The combination of blood lactate level with NEWS or qSOFA increased the accuracy to predict adverse events in both septic and non-septic ED patients.26–29 Our findings indicated that initial high blood lactate level may add the ability to predict the mortality and subsequent shock in patients with early sepsis. Both combinations of blood lactate levels with qSOFA or NEWS demonstrated increased AUROC when compared to single score criteria.
These results lead to the potential creation of a new screening model for sepsis with blood lactate levels. In clinical practice, patients should be initially assessed by clinical parameters. According to this study, NEWS should be used as an alternative to the qSOFA score. Blood lactate level measurement may be obtained when NEWS is above or equal to 7 to improve mortality prediction. Blood lactate above or equal to 2 mmol/L and NEWS above or equal to 7 should trigger the awareness of the physician to choose proper monitoring and level of care. Concerning the easy and rapid result of the screening tool, point-of-care blood lactate may be an alternative test.
There are several limitations to our study. First, sepsis was defined by both SIRS criteria and qSOFA score, even though SIRS criteria were suggested to be abandoned by the 2016 Task Force due to the low specificity. Second, we acknowledged that this cohort had the potential to have a selection bias. There were 432 (31.0%) unobtained blood lactate patients from the early screening. Third, serial blood lactate measurements or lactate clearance was shown as a good predictor of mortality in septic patients.10,30 However, serial blood lactate level was not routinely done in our center; thus, the beneficial effect of lactate clearance was not performed in this study. Lastly, death by do-not-resuscitate order was included in the primary outcome, which may explain why the overall mortality in early sepsis was higher than in other observations.
Conclusion
Among the early sepsis patients, initial blood lactate level above or equal to 2 mmol/L was an independent factor of 28 days mortality and subsequent septic shock. Adding initial blood lactate level increased the predictive ability of SIRS criteria, qSOFA, and NEWS.
Acknowledgments
The authors would like to thank Antika Wongthanee and the staff of the Research Unit, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University for their contribution to this trial. The authors would like to thank Ruth Leatherman, Research Administration Section, Faculty of Medicine, Chiang Mai University for native-English proofreading.
Footnotes
Source of support: Nil
Conflict of interest: None
Authors’ Contributions
Conception: NN and AD. Design: NN and AD. Acquisition of data: NN and JI. Analysis of data: NN and JI. Interpretation of data: NN, JI, and AD. Draft manuscript: NN and AD. Revised manuscript: NN, JI, and AD. All authors read and approved the final manuscript.
Availability of Date and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Orcid
Nabhat Noparatkailas https://orcid.org/0000-0002-1234-2062
Juthamas Inchai https://orcid.org/0000-0001-5497-7704
Athavudh Deesomchok https://orcid.org/0000-0003-1375-4541
References
- 1.Singer M, Deutschman CS, Seymour CW, Shankar–Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seymour CW, Liu VX, Iwashyna TJ, Brunkhorst FM, Rea TD, Scherag A, et al. Assessment of clinical criteria for sepsis: For the third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):762–774. doi: 10.1001/jama.2016.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maitra S, Som A, Bhattacharjee S. Accuracy of quick sequential organ Failure Assessment (qSOFA) score and systemic inflammatory response syndrome (SIRS) criteria for predicting mortality in hospitalized patients with suspected infection: A meta-analysis of observational studies. Clin Microbiol Infect. 2018;24(11):1123–1129. doi: 10.1016/j.cmi.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 4.Fernando SM, Tran A, Taljaard M, Cheng W, Rochwerg B, Seely AJE, et al. Prognostic accuracy of the quick sequential organ failure assessment for mortality in patients with suspected infection: A systematic review and meta-analysis. Ann Intern Med. 2018;168(4):266–275. doi: 10.7326/M17-2820. [DOI] [PubMed] [Google Scholar]
- 5.Hwang SY, Jo IJ, Lee SU, Lee TR, Yoon H, Cha WC, et al. Low accuracy of positive qSOFA criteria for predicting 28-day mortality in critically ill septic patients during the early period after emergency department presentation. Ann Emerg Med. 2018;71(1):1–9.e2. doi: 10.1016/j.annemergmed.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 6.Khosravani H, Shahpori R, Stelfox HT, Kirkpatrick AW, Laupland KB. Occurrence and adverse effect on outcome of hyperlactatemia in the critically ill. Crit Care. 2009;13(3):R90. doi: 10.1186/cc7918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nichol AD, Egi M, Pettila V, Bellomo R, French C, Hart G, et al. Relative hyperlactatemia and hospital mortality in critically ill patients: A retrospective multi-centre study. Crit Care. 2010;14(1):R25. doi: 10.1186/cc8888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mikkelsen ME, Miltiades AN, Gaieski DF, Goyal M, Fuchs BD, Shah CV, et al. Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock. Crit Care Med. 2009;37(5):1670–1677. doi: 10.1097/CCM.0b013e31819fcf68. [DOI] [PubMed] [Google Scholar]
- 9.Filho RR, Rocha LL, Correa TD, Pessoa CM, Colombo G, Assuncao MS. Blood lactate levels cutoff and mortality prediction in sepsis: Time for a reappraisal? A retrospective cohort study. Shock. 2016;46(5):480–485. doi: 10.1097/SHK.0000000000000667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhari M, Agarwal N. Study of significance of serum lactate kinetics in sepsis as mortality predictor. Indian J Crit Care Med. 2022;26(5):591–595. doi: 10.5005/jp-journals-10071-23935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock – 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 12.Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018;44(6):925–958. doi: 10.1007/s00134-018-5085-0. [DOI] [PubMed] [Google Scholar]
- 13.Royal College of Physicians. National early warning score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. London: Royal College of Physicians; 2017. Available at: https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2. Accessed on: 1 June 2022. [Google Scholar]
- 14.Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;101(6):1644–1655. doi: 10.1378/chest.101.6.1644. [DOI] [PubMed] [Google Scholar]
- 15.Casserly B, Phillips GS, Schorr C, Dellinger RP, Townsend SR, Osborn TM, et al. Lactate measurements in sepsis-induced tissue hypoperfusion: Results from the surviving sepsis campaign database. Crit Care Med. 2015;43(3):567–573. doi: 10.1097/CCM.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 16.Williams MD, Braun LA, Cooper LM, Johnston J, Weiss RV, Qualy RL, et al. Hospitalized cancer patients with severe sepsis: Analysis of incidence, mortality, and associated costs of care. Crit Care. 2004;8(5):R291–R298. doi: 10.1186/cc2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baltazar F, Afonso J, Costa M, Granja S. Lactate beyond a waste metabolite: Metabolic affairs and signaling in malignancy. Front Oncol. 2020;10:231. doi: 10.3389/fonc.2020.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hwang SY, Shin TG, Jo IJ, Jeon K, Suh GY, Lee TR, et al. Association between hemodynamic presentation and outcome in sepsis patients. Shock. 2014;42(3):205–210. doi: 10.1097/SHK.0000000000000205. [DOI] [PubMed] [Google Scholar]
- 19.Ranzani OT, Monteiro MB, Ferreira EM, Santos SR, Machado FR, Noritomi DT. Reclassifying the spectrum of septic patients using lactate: Severe sepsis, cryptic shock, vasoplegic shock and dysoxic shock. Rev Bras Ter Intensiva. 2013;25(4):270–278. doi: 10.5935/0103-507X.20130047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freund Y, Lemachatti N, Krastinova E, Van Laer M, Claessens YE, Avondo A, et al. Prognostic accuracy of sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department. JAMA. 2017;317(3):301–308. doi: 10.1001/jama.2016.20329. [DOI] [PubMed] [Google Scholar]
- 21.Wang JY, Chen YX, Guo SB, Mei X, Yang P. Predictive performance of quick sepsis-related organ failure assessment for mortality and ICU admission in patients with infection at the ED. Am J Emerg Med. 2016;34(9):1788–1793. doi: 10.1016/j.ajem.2016.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Usman OA, Usman AA, Ward MA. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the emergency department. Am J Emerg Med. 2019;37(8):1490–1497. doi: 10.1016/j.ajem.2018.10.058. [DOI] [PubMed] [Google Scholar]
- 23.Almutary A, Althunayyan S, Alenazi K, Alqahtani A, Alotaibi B, Ahmed M, et al. National early warning score (NEWS) as prognostic triage tool for septic patients. Infect Drug Resist. 2020;13:3843–3851. doi: 10.2147/IDR.S275390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–e143. doi: 10.1097/CCM.0000000000005337. [DOI] [PubMed] [Google Scholar]
- 25.Liu Z, Meng Z, Li Y, Zhao J, Wu S, Gou S, et al. Prognostic accuracy of the serum lactate level, the SOFA score and the qSOFA score for mortality among adults with sepsis. Scand J Trauma Resusci Emerg Med. 2019;27(1):51. doi: 10.1186/s13049-019-0609-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ho KM, Lan NSH. Combining quick sequential organ failure assessment with plasma lactate concentration is comparable to standard sequential organ failure assessment score in predicting mortality of patients with and without suspected infection. J Crit Care. 2017;38:1–5. doi: 10.1016/j.jcrc.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 27.Shetty A, MacDonald SP, Williams JM, van Bockxmeer J, de Groot B, Cuevas LME, et al. Lactate ≥2 mmol/L plus qSOFA improves utility over qSOFA alone in emergency department patients presenting with suspected sepsis. Emerg Med Australas. 2017;29(6):626–634. doi: 10.1111/1742-6723.12894. [DOI] [PubMed] [Google Scholar]
- 28.Baumann BM, Greenwood JC, Lewis K, Nuckton TJ, Darger B, Shofer FS, et al. Combining qSOFA criteria with initial lactate levels: Improved screening of septic patients for critical illness. Am J Emerg Med. 2020;38(5):883–889. doi: 10.1016/j.ajem.2019.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Hwang TS, Park HW, Park HY, Park YS. Prognostic value of severity score change for septic shock in the emergency room. Diagnostics (Basel) 2020;10(10):743. doi: 10.3390/diagnostics10100743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishna U, Joshi SP, Modh M. An evaluation of serial blood lactate measurement as an early predictor of shock and its outcome in patients of trauma or sepsis. Indian J Crit Care Med. 2009;13(2):66–73. doi: 10.4103/0972-5229.56051. [DOI] [PMC free article] [PubMed] [Google Scholar]