Abstract
Background
Health-promoting actions might benefit from adolescent health literacy (AHL), however, there is scant research on it in Nepal. This study identifies adolescent students’ health literacy (HL) needs and trials an intervention to improve their HL and intention to take health-promoting actions.
Methods
This study employs a pre-and post-test mixed-method intervention involving three phases. First, we will conduct a formative and summative evaluation to identify participants’ HL needs and design an intervention using quantitative and qualitative methods. Second, the intervention will be administered to the intervention group. Finally, formative and summative post-tests will be conducted to assess the effectiveness of the intervention. We will select four community schools from Birendranagar municipality based on random sampling. In quantitative research, data will be collected from adolescents selected through a census with standardized scales such as the HLS-Child-Q15, self-efficacy, social support, and health-promoting actions. A framework analysis was conducted to analyze qualitative data collected from focus group discussions with purposively chosen adolescents and key informant interviews with Health and Physical Education teachers and school nurses. The difference in difference approach will be used to analyze the intervention’s outcome, i.e., the participants’ improved HL, and health-promoting actions.
Discussion
This is one of the first studies to explore HL in this group in Nepal. This study will provide the first insights into the overall level of AHL, potential AHL determinants, and the relationship between AHL and the intention to participate in health-promoting activities. The data can then be used to inform health promotion and health literacy initiatives.
Keywords: Health literacy, Adolescent students, Health-promoting actions, Intervention
Background
HL is a relatively new research field and an essential part of public health [1–4] and health promotion [5, 6]. Schools can play an influential role in promoting HL [7] by delivering health information through mandatory courses on health education to all school-aged children [8]. This makes HL a viable target for schools. Health education and promotion make a significant contribution to HL [5] and could be considered as a part of the Health Promoting School (HPS) [9, 10]. The growing interest in adolescent health literacy (AHL) in recent years has been discussed worldwide [9]. Moreover, it has been argued that AHL research is crucial [11], but received far less attention than research on adults’ HL in many contexts [9].
The understanding of AHL is limited due to a paucity of studies [9, 12, 13], particularly in developing countries [14]. Evidence shows that low AHL is common even in developed nations [15–17]. For example, the majority of school-going students (67.2%) in ten European countries have only a moderate level of HL [18, 19]. Studies show that the HL of school-aged children is low. According to a study on Thai school-aged children, 64.4% reported poor levels of HL [20], followed by one-third for Chinese children [21]; 20.9% of Pakistani children had very limited, and 53.4% limited HL [22] and almost (99.3%) of Iranian students from 15 to 18 had poor HL [23]. Only a few HL studies have been conducted in Nepal, revealing that the majority of female college students [24, 25] and school adolescents have inadequate HL scores [26]. These studies provide the first insights into AHL, but the overall distribution of AHL remains unclear [21] and differs among countries and subgroups [18]. As per our current understanding, not much is known about the distribution of AHL in the population [27].
The next issue is that there is currently a scarcity of theory-driven HL interventions in schools to increase AHL. A limited number of studies have been conducted to develop interventions to promote generic HL in adolescents. For example, a recent review found that no intervention has explicitly aimed to improve HL [28] and the majority of existing school-based HL interventions are domain-specific without a holistic model [29]. It is frequently ignored in school curricula [30] and an effective strategy for improving HL in schools is still lacking [31]. Further, the literature shows that most of the studies conducted on the HL of adolescents are cross-sectional designs. To our knowledge, this will be the first intervention study to promote health literacy among adolescent school students in Nepal. This is why a longitudinal research design is employed in this study.
Aims
Based on the available evidence, this study aims to.
-
(i)
explore the HL needs of adolescent students and.
-
(ii)
design, implement and evaluate the impact of a health literacy educational intervention to improve adolescent students’ health literacy and their intention to take health-promoting actions.
Methods
Research method
The study follows a pre-and post-test [32, 33], mixed-method intervention design [34] grounded in pragmatism. Researchers have identified pragmatic research as the preferred approach to mixed-methods research [32, 33, 35, 36].
Theoretical model
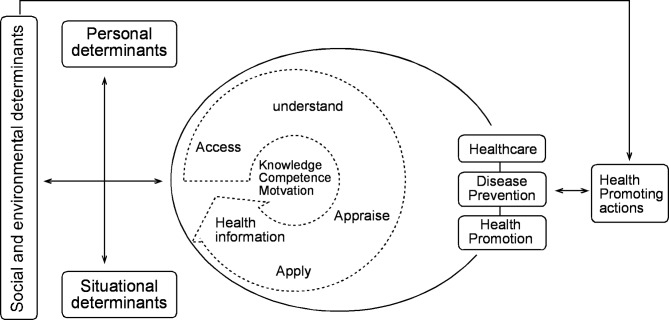
While reviewing the various models [37–39] in light of this study’s overall goals, the comprehensive and conceptual model appears to be applicable as a theoretical model [40]. The understanding of HL within this study is underpinned by the four core dimensions of the HL Model as presented by Sorensen et al. (2012): (1) accessing, (2) understanding, (3) appraising, and (4) applying health information. Based on this model, this study will explore the multiple determinants that shape HL (Fig. 1), namely (1) personal, (2) situational, as well as (3) societal and environmental determinants. All three factors influence how adolescents deal with health information. Also, the model covers many potential outcomes of HL. Of these outcomes, the study will cover only health-promoting actions as a specific form of health behaviors [6].
Fig. 1.
Simplified HLS-EU model of health literacy [40] adapted to the study design and needs
Study site
This study will be conducted in the governmental school of Birendranagar Municipality of Surkhet. There are a total of 21 schools in the municipality where 2500 (average: 156 per school) students are studying in class nine in this academic session [41]. Karnali Province is less developed, has low human development indicators, and has a low literacy rate compared to other provinces of Nepal [42, 43]. Birendranagar is an educational and cultural hub where students from different districts of Karnali province come to study. Therefore, it has been selected as a study area.
Research design
This study contains three phases (see Fig. 2). Formative and summative evaluation will be used to explore the impact of the intervention. Formative assessment will assess the feasibility and acceptability of interventions and help inform their implementation [34]. Summative evaluation will be used to investigate the impact of the intervention.
Fig. 2.
Overview of the research design
Phase 1 needs assessment
As part of the formative evaluation [34], all class nine students, as well as their Health and Physical Education (HPE) teachers and school nurses from the four schools will take part in quantitative and qualitative pre-tests. This phase will assess participants’ HL knowledge, and, needs. This phase [44] will also inform the implementation strategies [34, 45].
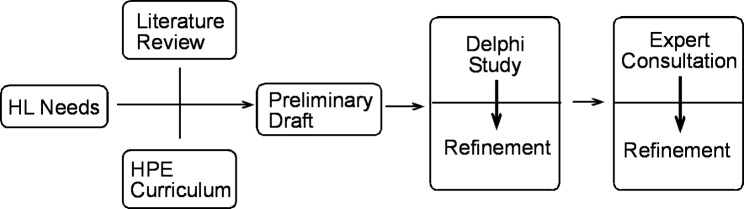
The HL Intervention will be developed in three steps. First, the researchers will prepare a preliminary draft of the intervention based on the IM’s four dimensions (accessing, understanding, appraising, and applying health information [40]), and the HPE curriculum of class nine. Second, the preliminary draft will be refined based on the HL needs of the target group. This will then be further refined by the Delphi study with HPE teachers, school nurse, health education, public health and medical care experts. As part of this process, the 9th -grade HPE curriculum will be integrated into the interventions’ contents, strategies, materials, and practical facilitation of the sessions. Third, to make it more aligned with HL needs, the curriculum, and the HL domains (accessing, understanding, evaluating, and applying), the refined draft will be finalized based on consultation with health educators and health literacy experts (see Fig. 3).
Fig. 3.
Flow chart of the intervention development process
Phase 2 implementation
In this phase, the refined intervention will be implemented in the intervention group in eight separate classroom sessions. One session will last for 1 h to 90 min. Teachers from participating schools, HPE teachers from participating local campuses, public health officers, and medical officers will conduct the sessions (Table 1).
Table 1.
Preliminary intervention draft based on IMHL [40] and HPE curriculum
| Input | Sessions | Objectives | Contents | Activities | Outcome |
|---|---|---|---|---|---|
| Program introduction | Researcher | To become familiar with the program | Introduction to program, and HL and health-promoting actions | Group teaching and interaction |
Increased HL awareness and skills Intention to engage in health promotion actions |
|
Human resources Time Money Materials Technology Partnership |
Health education experts | to raise adolescents’ awareness of health literacy. | Health Literacy (HL) concept | Storytelling and Dialogue | |
| HPE teacher/ school nurse | To develop Confidence in health literacy skills | Health information: access, understand, appraisal, and apply | Clear communication, photograph showing demonstration, experience sharing | ||
| Teacher’s educator | Confident to evaluate the determinants of health | Social determinants of health, health right, and responsibility | Video showing and Dialogue | ||
| Medical doctors | Confident to use health care | Health care literacy | Clear communication, role playing | ||
| School Nurse | To raise awareness on disease prevention | Disease prevention literacy | Experience sharing, playing game | ||
| Public health experts | To raise awareness on disease prevention | Health promotion literacy | self-assessment and reflection of text and presentation | ||
| Health education experts | to pursue health-promoting activities | Health-promoting actions | Case study, video show, playing game, group discussion |
Phase 3 evaluation
Both formative and summative evaluation methods will be employed to evaluate the impact of the health literacy educational intervention. Based on the above description, pre-interventional evaluation [34] information will be collected from students, HPE teachers, and nurses through quantitative and qualitative pre-tests, as well as a review of the grade nine curriculum. Discussion and meetings will be conducted with HPE teachers, students, and facilitators during the implementation process. This is to determine whether the plan is being implemented properly and whether there are any discrepancies [46].
To evaluate the overall success, usefulness, satisfaction, and additional suggestions [34], contextual appropriateness, relevancy, and acceptability [44] of the intervention, interpretative formative evaluation [46] will be used. Summative evaluation will be used to assess the overall effectiveness of the intervention at the end of the project.
Participants and sampling
The study will involve adolescent students in grade nine as primary participants, and HPE teachers and school nurses as secondary participants. Since academic grades and age affect HL, only grade nine will be taken for this study to construct the same group of intervention and control [39].
Sampling for a quantitative study
Firstly, four governmental secondary schools will be chosen from the study area using a random sampling method for the needs assessment. Then, two of the four selected schools will be considered as an intervention group randomly and the remaining two schools will be considered as a control group. The sample size of this study will be at least 384. All students of class nine of the selected schools will be selected via the census. Assuming that the margin of error is 5% and the level of confidence is 95%, the recommended standard sample size (SSS) is 384 [47]. Non-response samples will be added after the pilot test.
The formula of SSS [47]:  [where n= sample size, Z= standard error associated with the chosen level of confidence, p= variability/, q = 1-p, and e= acceptable sample error] will be used.
[where n= sample size, Z= standard error associated with the chosen level of confidence, p= variability/, q = 1-p, and e= acceptable sample error] will be used.
Sampling for a qualitative study
Twenty-four (six from each school) adolescents will be purposefully selected from the participating schools. Similarly, HPE teachers and school nurses of the respective schools will also be included as key informants for the study.
Inclusion and exclusion criteria
All students in class nine of selected schools in Surkhet, aged 13 to 19, who are willing to participate in the study, will be included. However, students with special needs and who skip two educational sessions will be excluded from the intervention.
Tools and materials
Quantitative data collection tools
Information about participants’ characteristics such as age, sex, caste, religion, parental education, family size, availability of TV, radio, mobile, internet, health status, educational outcome, and HL knowledge will be collected using a self-administered questionnaire. To collect quantitative data relating to the pre-test and post-test, standardized tools will be used, such as self-efficacy, social support, school environment, community environment, HLS CHILD-15, and health-promoting action scale (Table 2).
Table 2.
Standardized data collection tools
| SN | Variable | Tools | Literature | Total items and components | Reliability | Validity |
|---|---|---|---|---|---|---|
| 1 | Personal factors | General Self-efficacy Scale (GSE) | R Schwarzer and M Jerusalem [48] | 10 items 4 scales, ranges between 10 and 40 | α = 76 to 0.90 | Strong structural validity |
| 2 | Situational factors: | Multi-dimensional scale for perceived social support Scale (MSPSS) | GD Zimet, NW Dahlem, SG Zimet and GK Farley [49] | 12-item scale family (4), friends (4), significant other (4). | α = 0.86–0.93) | good construct validity |
| 3 | School Environment | The school environment scale (SES) | R Glaser, ML Van Horn, M Arthur, J Hawkins and R Catalano [50] | 17 items: chances for pro-social participation (5), rewards for pro-social involvement (4), academic performance (2), commitment to school (6) | α = 0.70–0.76) | Strong construct validity |
| 4 | Community Environment | The community environment scale (CES) | M Gray and A Sanson [51] | Nine items related to a neighborhood environment | α = 0.84 | Satisfactory construct validity |
| 5 | Subjective health literacy | HLS-CHILD-Q15 | TM Bollweg, O Okan, P Pinheiro, J Bröder, D Bruland, AM Freţian, OM Domanska, S Jordan and U Bauer [52] | 15-items, access, understand, and apply | α = 0.71 to 0.74 | Significant |
| 6. | Assessing health-promoting actions |
Health-promoting actions questionnaire (HPAQ) |
SN Walker, KR Sechrist and NJ Pender [53] | 6 aspects; Self-actualization, health responsibility, nutrition, interpersonal support stress management, and exercise. | 0.92 and | Significant |
Qualitative data collection methods
To collect qualitative data, eight focus group discussions (FGDs) [54] will be held with students: four as a pre-test to get information regarding HL needs [40, 55], and four as a post-test to evaluate the outcome. Each FGD will last for an hour. Similarly, four key informant interviews (KIIs) with HPE teachers and school nurses from selected schools will be conducted before and after the intervention to get feedback on the intervention.
Reliability, validity, and trustworthiness
First, HLS-Child-Q15 and other data collection tools will be translated by two professional translators using independent back-translation. After that, expert consultation will be received, and a Nepali version scale will be drafted. Then, the HLS-Child-Q15 will be pilot-tested qualitatively in nine adolescent students and modified based on the received feedback. Second, the pilot test will be conducted on 10 percent of total population for all standardized scales. They share the same features as the study area but are not incorporated into the study.
Participants’ opinions shall be properly documented with as much use of their own opinions as feasible for credibility. Themes will be explored and developed through author agreement. By contrasting and comparing data collected from students, HPE teachers, and school nurses for corroboration, we will triangulate qualitative data. Themes will be generated from the interview data by combining information from many sources (transcribe, memos, field reports, theory, and authors), and we’ll carry out member checks, requesting the participants to read the key themes and findings [54].
Data collection procedure
The study will begin in the summer of 2022, at the beginning of the academic year. At two different points, data will be collected. Before and after the intervention is implemented in the study population, data will be collected simultaneously in both groups using the same way. Randomly, two schools will be selected from four to form the intervention group. The students from the remaining three schools will comprise the control group. After that, baseline data from both groups will be obtained. The characteristics of the intervention and control groups will then be matched based on the baseline data. Propensity Score Matching (PSM) will be used to obtain an unbiased estimation of the impact of the intervention and match the sociodemographic characteristics of both intervention groups [45]. Immediately after the intervention, the effect will be examined by post-test [56]. The self-reported questionnaire, and scales such as socio-demographic profile, HL knowledge, HLS-Child-Q15, HPA, and FGD for the students and KII for the teachers, and nurses will be employed to collect data related to the effectiveness of the intervention.
To collect quantitative data, students will use paper-and-pencil methods to complete self-reported scales. While conducting FGDs, a separate person will be employed as the note keeper and the principal researcher himself will moderate. Similarly, we will conduct KII to HPE teachers and school nurses about what they think is relevant regarding AHL. Based on the objectives and comprehensive model, semi-structured FGD and KII guidelines will be developed. Their information will be recorded with their consent.
Data analysis procedure
For the formative assessment of HL needs, quantitative data will be analyzed by descriptive analysis. The software SPSS version 20.0 will be used to conduct all statistical analyses for quantitative data. Ritchie & Spencer’s (1994) five- steps framework analysis [57] will be applied to analyze the qualitative data from the pre-and post-tests. The verbatim recordings will be transcribed and ATLAS-TI software will be used for coding and categorization.
The summative evaluation methods will be used to compare pre-test and post-test results to determine if there has been any change in response. The Different in Different (DID) method will be applied to measure the impact of the program [58] which is also known as the double-difference method. Differences in the outcomes before and after intervention in both groups will be analyzed [45]. Mean, standard errors, mean differences, and a comparison of the results between the pretest and posttest will be examined.
Ethical consideration
The Nepal Health Research Council (NHRC) approved this study protocol (NHRC, Ref. No. 2688). Students will be asked for written consent before participating in the study, and participation will be voluntary. Similarly, permission to record will be obtained, confidentiality and privacy will be ensured, and the COVID-19 protocol will be adhered to.
[59]. Approval will also be sought from the concerned authors for the adapting of the standardized tools.
Discussion
The purpose of this research is to explore the design and impact of a school-based health literacy intervention for improving AHL and the intention to engage in health-promoting actions. To the extent of our knowledge, this is the first study to measure AHL needs and develop an intervention to promote AHL in schools in Nepal.
Previous studies reported that no intervention has explicitly aimed to improve HL[28]. The majority of existing school-based HL interventions are domain-specific without a holistic model [31]. It is emphasized that HL education may be increased by providing information, effective communication, media, organized education, and various methods in a range of settings [60]. HL education aims to increase knowledge, to promote health-promoting attitudes and beliefs (KAB framework) [31]. School adolescents have a low HL level and health-promoting activities. HL is a concept that focuses on education and training to improve the HL of individuals and populations, both individually and collectively [61]. According to our understanding, there were few interventional studies on HL and health-promoting actions in adolescent students. These findings provide evidence that an HL intervention may contribute to promoting HL and health-promoting actions in adolescents.
The intervention’s strengths include a school-based health literacy intervention and execution in the school context. Furthermore, the Ministry of Health and Education, as well as other related sectors, may use the findings of this study to support policy and planning to enhance health literacy among school-aged adolescents. The intervention’s components will be matched to the school’s HPE curriculum and the participants’ needs. This study incorporates a comprehensive model of HL to guide, embed, and respond to the participants’ health literacy needs and interventions. This research will provide preliminary evidence that school-aged adolescents who received an HL intervention increased their HL knowledge, competencies, and intention to engage in health-promoting actions.
The main limitation of this study will be that it is not properly randomized and only took place in the Surkhet district of Nepal. Because participants were asked survey questions, we could not rule out the possibility of measurement errors. This study does not offer a multi-level approach to changing environmental and societal factors. More research is needed to develop an effective intervention to address these societal and environmental factors.
Conclusion
It would be very useful to study HL among young people in schools. A study will be conducted to determine the health literacy needs of adolescents. School-based health literacy interventions may influence adolescents’ health literacy and health-promoting behaviors.
Acknowledgements
The authors would like to thank the Graduate School of Education, Tribhuvan University for supporting this study. Similarly, we would like to thank to Prof. Bhimsen Devkota, Tribhuvan University, Nepal, and Torsten Michael Bollweg, Technical University Munich, UM Department of Sport and Health Sciences, Germany for their critical comments.
Abbreviations
- AHL
Adolescent Health Literacy
- FGD
Focus Group Discussion
- HL
Health Literacy
- IMHL
Integrated Model of Health Literacy
- KII
Key Informant Interview
- HPE
Health and Physical Education
- KAB
Knowledge, Attitude and Behaviour
- NHRC
The Nepal Health Research Council
- DID
Different in Different
- HLS-Child-Q15
Health Literacy Scale- Child Questions 15
- HPA
Health promoting Actions
- PSM
Propensity Score Matching
- SSS
Standard Sample Size
- HLEI
Health Literacy educational intervention
- HPS
Health Promoting School
Authors’ contributions
SPK, CBB and OO co-designed the project, SPK wrote the manuscript. OO was the key contributor to writing the manuscript. OO contributed manuscript revision. All authors read and approved the final manuscript.
Funding
Funding was obtained for this study from University Grant Commission, Nepal.
Data availability
Not applicable as this article does not present data.
Declarations
Ethical approval and consent to participate
Ethical approval for this study has been received by the Nepal Health Research Council (Ref. no. 2688). Informed written consent will be obtained from all adolescent students and their parents. All methods will be carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Institute of Medicine. In: Health Literacy: A Prescription to End Confusion eds. Edited by Nielsen-Bohlman L, Panzer AM, Kindig DA. Washington (DC): National Academies Press (US); 2004. [PubMed]
- 2.World Health Organization. Regional Office for South-East A: Health literacy toolkit for low- and middle-income countries: A series of information sheets to empower communities and strengthen health systems. New Delhi:WHO Regional Office for South-East Asia; 2015.
- 3.Sentell T, Vamos S, Okan O. Interdisciplinary Perspectives on Health Literacy Research Around the World: More Important Than Ever in a Time of COVID-19. 2020, 17(9):3010. [DOI] [PMC free article] [PubMed]
- 4.Kanj M, Mitic W. Health literacy and health promotion: Definitions, concepts and examples in the Eastern Mediterranean region. In: 7th Global Conference on Health Promotion Promoting Health and Development: Closing the Implementation Gap: 2009; 2009: 26–30.
- 5.Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000;15(3):259–67. doi: 10.1093/heapro/15.3.259. [DOI] [Google Scholar]
- 6.Sorensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H. (HLS-EU) Consortium Health literacy project european. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nutbeam D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies in the 21st century.Health Promotion International2000,15.
- 8.Okan O, Kirchhoff S, Bauer U. Health Literate Schools (HeLit-Schools): Organizational Health Literacy in the School Setting.European Journal of Public Health2021, 31(Supplement_3).
- 9.Okan O, Paakkari L, Aagaard-Hansen J, Barnekow V, Weber M, Sorensen K. WHO Concept Paper on Health literacy in the context of Health, Well-being, and learning outcomes: the case of children and adolescents in schools: concept paper. In. Copenhagen: WHO Regional Office for Europe; 2020. [Google Scholar]
- 10.Langford R, Bonell CP, Jones HE, Pouliou T, Murphy SM, Waters E, Komro KA, Gibbs LF, Magnus D, Campbell R. The WHO Health Promoting School framework for improving the health and well-being of students and their academic achievement.Cochrane Database of Systematic Reviews2014(4). [DOI] [PMC free article] [PubMed]
- 11.Fleary SA, Joseph P, Pappagianopoulos JE. Adolescent health literacy and health behaviors: a systematic review. J Adolesc. 2018;62:116–27. doi: 10.1016/j.adolescence.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 12.Okan O, Jochimsen M, Hendricks J, Wasem J, Bauer U. Health literacy in children and adolescents: associations between health literacy and health inequalities. J Eur J Public Health. 2018;28(suppl4):cky213. [Google Scholar]
- 13.Devraj R, Gordon EJ. Health literacy and kidney disease: toward a New line of Research. Am J Kidney Dis. 2009;53(5):884–9. doi: 10.1053/j.ajkd.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 14.Lee S-YD, Tsai T-I, Tsai Y-W, Kuo KN. Health literacy, health status, and healthcare utilization of taiwanese adults: results from a national survey. BMC Public Health. 2010;10(1):614. doi: 10.1186/1471-2458-10-614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bröder J, Okan O, Bauer U, Bruland D, Schlupp S, Bollweg TM, Saboga-Nunes L, Bond E, Sørensen K, Bitzer EM, et al. Health literacy in childhood and youth: a systematic review of definitions and models. BMC Public Health. 2017;17(1):361. doi: 10.1186/s12889-017-4267-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Okan O, Lopes E, Bollweg TM, Bröder J, Messer M, Bruland D, Bond E, Carvalho GS, Sørensen K, Saboga-Nunes L, et al. Generic health literacy measurement instruments for children and adolescents: a systematic review of the literature. BMC Public Health. 2018;18(1):166. doi: 10.1186/s12889-018-5054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sansom-Daly U, Lin M, Robertson E, Wakefield C, McGill B, Girgis A, Cohn R. Health Literacy in Adolescents and Young Adults: An Updated Review.Journal of adolescent and young adult oncology2016, 5. [DOI] [PubMed]
- 18.Paakkari L, Torppa M, Mazur J, Boberova Z, Sudeck G, Kalman M, Paakkari O. A Comparative Study on Adolescents’ Health Literacy in Europe: Findings from the HBSC Study.Int J Environ Res Public Health2020, 17(10). [DOI] [PMC free article] [PubMed]
- 19.Sørensen K, Pelikan JM, Röthlin F, Ganahl K, Slonska Z, Doyle G, Fullam J, Kondilis B, Agrafiotis D, Uiters E, et al. Health literacy in Europe: comparative results of the european health literacy survey (HLS-EU) Eur J Public Health. 2015;25(6):1053–8. doi: 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Intarakamhang U, Intarakamhang P. Health literacy scale and causal model of Childhood overweight. J Res health Sci. 2017;17(1):e00368. [PubMed] [Google Scholar]
- 21.Guo S, Yu X, Davis E, Armstrong R, Riggs E, Naccarella L. Adolescent health literacy in Beijing and Melbourne: a cross-cultural comparison. Int J Environ Res Public Health. 2020;17(4):1242. doi: 10.3390/ijerph17041242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jabeen R, Rehman MU, Masood S, Mahmood H, Mashhadi SF. Assessment of functional health literacy among adolescents of model schools of Islamabad.Pakistan Armed Forces Medical Journal2018(3):545–549.
- 23.Motamedi M, Peyman N, Afzalaghaee M. Relationship of health literacy and regular physical activity self-efficacy with body mass index in adolescent girls aged 15–18 years. J Health Lit. 2020;5(3):64–73. [Google Scholar]
- 24.Khanal SP. Role of health literacy on Menstrual Hygiene Practice among the girl students. J Health Promotion. 2019;7:83–90. doi: 10.3126/jhp.v7i0.25518. [DOI] [Google Scholar]
- 25.Khanal SP, Sharma MK, Kharel S, Sharma C. Role of Health Literacy on Health Behaviour Change among the College Girl Students.Scholars’ Journal2021.
- 26.Shrestha MK. Health literacy of teachers and students in secondary community schools of Lalitpur metropolitan city. Kathmandu University; 2019.
- 27.Shrestha A, Singh SB, Khanal VK, Bhattarai S, Maskey R, Pokharel PK. Health literacy and knowledge of chronic Diseases in Nepal. Health Lit Res Pract. 2018;2(4):e221–30. doi: 10.3928/24748307-20181025-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pleasant A, Griffin KH, Maish C, O’Leary C, Carmona R. Health literacy interventions for children or adolescents: An overview and insights into practical applications.International Handbook of Health Literacy2019:307.
- 29.Smith C, Goss HR, Issartel J, Belton S. Health literacy in schools? A systematic review of Health-Related interventions aimed at disadvantaged adolescents. Children. 2021;8(3):176. doi: 10.3390/children8030176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schulenkorf T, Krah V, Dadaczynski K, Okan O. Addressing health literacy in schools in Germany: Concept Analysis of the Mandatory Digital and media literacy School Curriculum. Front public health. 2021;9:687389–9. doi: 10.3389/fpubh.2021.687389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. Regional Office for Europe: Health literacy in the context of health, well-being and learning outcomes the case of children and adolescents in schools: the case of children and adolescents in schools. In. Copenhagen: World Health Organization. Regional Office for Europe; 2021.
- 32.Morgan DL. Pragmatism as a paradigm for social research. Qualitative Inq. 2014;20(8):1045–53. doi: 10.1177/1077800413513733. [DOI] [Google Scholar]
- 33.Morgan DL. Paradigms lost and pragmatism regained: methodological implications of combining qualitative and quantitative methods. J mixed methods Res. 2007;1(1):48–76. doi: 10.1177/2345678906292462. [DOI] [Google Scholar]
- 34.Elwy AR, Wasan AD, Gillman AG, Johnston KL, Dodds N, McFarland C, Greco CM. Using formative evaluation methods to improve clinical implementation efforts: description and an example. Psychiatry Res. 2020;283:112532. doi: 10.1016/j.psychres.2019.112532. [DOI] [PubMed] [Google Scholar]
- 35.Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educational researcher. 2004;33(7):14–26. doi: 10.3102/0013189X033007014. [DOI] [Google Scholar]
- 36.Feilzer MY. Doing mixed methods research pragmatically: implications for the rediscovery of pragmatism as a research paradigm. J mixed methods Res. 2010;4(1):6–16. doi: 10.1177/1558689809349691. [DOI] [Google Scholar]
- 37.Wharf Higgins J, Begoray D, MacDonald M. A social-ecological conceptual Framework for understanding adolescent health literacy in the Health Education Classroom. Am J Community Psychol. 2009;44(3–4):350. doi: 10.1007/s10464-009-9270-8. [DOI] [PubMed] [Google Scholar]
- 38.Manganello JA. Health literacy and adolescents: a framework and agenda for future research. Health Educ Res. 2008;23(5):840–7. doi: 10.1093/her/cym069. [DOI] [PubMed] [Google Scholar]
- 39.Paakkari L, Paakkari O. Health literacy as a learning outcome in schools. Health Educ. 2012;112(2):133–52. doi: 10.1108/09654281211203411. [DOI] [Google Scholar]
- 40.Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, Brand H. Consortium Health literacy project E: Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Municipality B. Shaikshik Darpan 2078: Birendranagar Municipality, 2078.
- 42.Ministry of Social Development, Province K, New ERA. ICF: Karnali Province: Key Findings from the 2015 Nepal Health Facility Survey and 2016 Nepal Demographic and Health Survey. In. Kathmandu, Nepal; 2019.
- 43.Poudel T, Amgain K, Sanjel S. Health scenario of Karnali Province, Nepal. J Karnali Acad Health Sci. 2019;1(03):1–7. [Google Scholar]
- 44.Nastasi BK, Hitchcock J, Sarkar S, Burkholder G, Varjas K, Jayasena A. Mixed methods in intervention research: theory to adaptation. J Mixed Methods Res. 2007;1(2):164–82. doi: 10.1177/1558689806298181. [DOI] [Google Scholar]
- 45.White H, Sabarwal S. Quasi-experimental design and methods. Methodological briefs: impact evaluation. 2014;8:1–16. [Google Scholar]
- 46.Hagedorn HJ, Brown R, Dawes M, Dieperink E, Myrick DH, Oliva EM, Wagner TH, Wisdom JP, Harris AH. Enhancing access to alcohol use disorder pharmacotherapy and treatment in primary care settings: ADaPT-PC. Implement Sci. 2016;11:64. doi: 10.1186/s13012-016-0431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cochran WG. Sampling techniques. 2nd ed. John Wiley and Sons Inc.; 1963.
- 48.Schwarzer R, Jerusalem M. Generalized Self-Efficacy scale. Measures in health psychology: A user’s portfolio Causal and control beliefs 1995.
- 49.Zimet GD, Dahlem NW, Zimet SG, Farley GK. Multidimensional scale of perceived social support (MSPSS) J Pers Assess. 1988;52(1):30–41. doi: 10.1207/s15327752jpa5201_2. [DOI] [Google Scholar]
- 50.Glaser R, Van Horn ML, Arthur M, Hawkins J, Catalano R. Measurement Properties of the Communities that Care® Youth Survey Across demographic groups. J Quant Criminol. 2005;21:73–102. doi: 10.1007/s10940-004-1788-1. [DOI] [Google Scholar]
- 51.Gray M, Sanson A. Growing up in Australia: The longitudinal study of Australian children.Family Matters2005(72):4–9.
- 52.Bollweg TM, Okan O, Pinheiro P, Bröder J, Bruland D, Freţian AM, Domanska OM, Jordan S, Bauer U. Adapting the european health literacy survey for Fourth-Grade students in Germany: Questionnaire Development and qualitative Pretest. HLRP: Health Literacy Research and Practice. 2020;4(2):e119–28. doi: 10.3928/24748307-20200326-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: development and psychometric characteristics. Nurs Res. 1987;36(2):76–81. doi: 10.1097/00006199-198703000-00002. [DOI] [PubMed] [Google Scholar]
- 54.Cresswell JW. Educational Research: planning, conducting and evaluating quantitative and qualitative research. 4th ed. Pearson Education Inc.; 2012.
- 55.Baumeister A, Chakraverty D, Aldin A, Seven ÜS, Skoetz N, Kalbe E, Woopen C. “The system has to be health literate, too” - perspectives among healthcare professionals on health literacy in transcultural treatment settings. BMC Health Serv Res. 2021;21(1):716. doi: 10.1186/s12913-021-06614-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Révész J, Rogers J. Experimental and quasi-experimental design.Research Gate Publication2019,135.
- 57.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Anal Qual Data Edited by Bryman A, Burgess R. London: Routledge; 1994: 173–194.
- 58.Martorano B, Sanfilippo M. Innovative Features in Conditional Cash Transfers: An impact evaluation of Chile Solidario on households and children. Innocenti Working Papers no 2012-03 2012.
- 59.WHO. : Coronavirus disease (COVID-19) advice for the public. In.; 2019.
- 60.Nutbeam D, McGill B, Premkumar P. Improving health literacy in community populations: a review of progress. Health Promot Int. 2017;33(5):901–11. doi: 10.1093/heapro/dax015. [DOI] [PubMed] [Google Scholar]
- 61.Okan O. Improving health literacy in the community for the next pandemic. In. Baptist University, School of Continuing Education, Hongkong.; 2022/ July 7.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable as this article does not present data.