Abstract
Background and Objective
Shared decision-making (SDM) aligns patient preferences with health care team treatment goals. This quality improvement initiative implemented a standardized SDM bundle within a neurocritical care unit (NCCU), where unique demands make existing, provider-driven SDM practices challenging.
Methods
An interprofessional team defined key issues, identified barriers, and created change ideas to drive implementation of an SDM bundle using the Institute for Healthcare Improvement Model for Improvement framework incorporating Plan-Do-Study-Act cycles. The SDM bundle included (1) a health care team huddle pre-SDM and post-SDM conversation; (2) a social worker–driven SDM conversation with the patient family, including core standardized communication elements to ensure consistency and quality; and (3) an SDM documentation tool within the electronic medical record to ensure the SDM conversation was accessible to all health care team members. The primary outcome measure was percentage of SDM conversations documented.
Results
Documentation of SDM conversations improved by 56%, from 27% to 83% pre/postintervention. Average time to documentation decreased by 4 days, from day 9 preintervention to day 5 postintervention. There was no significant change in NCCU length of stay, nor did palliative care consultation rates increase. Postintervention, SDM team huddle compliance was 94.3%.
Discussion
A team-driven, standardized SDM bundle that integrates with health care team workflows enabled SDM conversations to occur earlier and resulted in improved documentation of SDM conversations. Team-driven SDM bundles have the potential to improve communication and promote early alignment with patient family goals, preferences, and values.
Shared decision-making (SDM) is a practice aimed at aligning treatment goals between patients, patient families, and health care providers. Through SDM communication, patient preferences and values are uncovered to create an individualized approach to decision-making.1,2
The presence, timing, and format of SDM communication has been shown to have clinically relevant effects. Early and well-documented SDM is associated with treatment more consistent with patients' goals, reduced use of nonbeneficial medical care, reduced stress for patients and surrogates, and reduced costs.3-10
SDM is complex, particularly in the fast-paced environment of an intensive care unit (ICU).11 Critically ill patients often lack capacity to make decisions, necessitating surrogates to engage in these conversations with health care team members. The high prognostic uncertainty, high number of hand-offs, time sensitivity, and the sheer number of different providers in a typical ICU can all be causes of unwarranted variation in SDM practice, particularly when the SDM process is exclusively provider-driven.11,12 This unwarranted variation not only makes SDM practices more difficult to measure and improve but also prevents patients from receiving equitable care regardless of the provider, acuity, or ICU census.
A team-driven, as opposed to provider-driven SDM process, may reduce this unwarranted variation while also enabling earlier delivery of SDM. Because personnel resources are limited in many ICUs, there is a supply-demand mismatch between intensivists and consultative specialty palliative care providers and patients and families with SDM needs.13 This mismatch presents a significant barrier to early identification of patient goals, values, and preferences and can be removed by shifting to a team-driven SDM process.
We sought to implement such a process at a quaternary care system's neurocritical care unit (NCCU), using a microsystems quality improvement (QI) approach to develop a standardized SDM bundle.14 The bundle introduces no new burdens on unit staff and resources, and by standardizing our practices, lays a solid foundation for future SDM improvement.
Methods
Study Design and Population
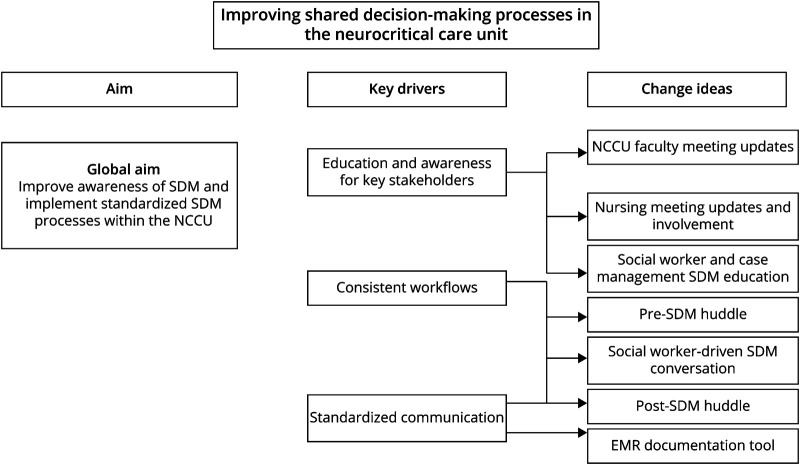
In this QI initiative, we used a microsystems QI approach, based on the Institute for Healthcare Improvement (IHI) Model for Improvement, incorporating iterative Plan-Do-Study-Act cycles within the NCCU.14 Standards for QI Reporting Excellence 2.0 (SQUIRE 2.0) guidelines were followed.15 An interprofessional team was convened to identify SDM barriers in the NCCU. Qualitative interviews and surveys were administered to delineate variations in practice and opportunities for improvement. Barriers were evaluated using an Ishikawa diagram. A driver diagram was formulated to identify key drivers of SDM and formulate change ideas to promote standardization (Figure 1). Candidate measures to evaluate SDM processes were mapped using the IHI clinical value compass.16 The global aim was to improve awareness of SDM and implement standardized SDM processes within the NCCU.
Figure 1. Key Drivers and Change Ideas Implemented to Achieve the Project Aims.
Interventions were prioritized based on feasibility and impact and focused on 2 major domains: an educational campaign targeting interprofessional care team members and an SDM bundle targeting the health care team. The SDM bundle included (1) a health care team huddle pre-SDM and post-SDM conversation with a structured communication guideline; (2) a social worker–driven SDM conversation with the patient family, including core standardized communication elements to ensure consistency and quality; and (3) an SDM documentation tool within the electronic health record (EHR) to ensure the SDM conversation was accessible to all health care team members. SMART (specific, measurable, attainable, relevant, time-based) aims included the following: (1) increase utilization of the prebrief huddle from 0% to 80% over approximately 6 months, (2) increase utilization of the debrief huddle from 0% to 80% over approximately 6 months, and (3) increase the number of patients in the NCCU with documented goals of care conversations in the EHR from 30% to 80% in approximately 6 months.
Setting
The hospital is a large quaternary care health system with 396 inpatient hospital beds and is the sole level 1 trauma center in a large rural setting. The NCCU consists of 10 dedicated beds and an interprofessional care team model inclusive of neurointensivists, advanced practice providers, resident physicians, nursing staff, rehabilitation therapists, social workers, and case managers.
At the time of this initiative, there was no standard practice for initiating or structuring SDM conversations. Attending physicians would decide whether there was a need for an SDM conversation based on their experience and interactions with family, at which point the social worker would be notified. The social worker would then coordinate a meeting time for the family and NCCU attending physician to meet. These meetings would typically occur during the week because social workers were not present on the weekends. Presence of subspecialty consulting services at these meetings varied, with attendance mainly consisting of family, the NCCU attending physician, and the social worker.
This study took place during the SARS-CoV-2 (COVID) pandemic. During this time, hospital measures limited family presence at the hospital, with 1 to 2 family members allowed for in-person visitation for the purposes of family meetings and withdrawal of life support.
Organizing for the Intervention
The project was led by the primary author, HW, and the key champion was the NCCU social worker. The core project team included a QI coach, a neurointensivist lead, a NCCU social worker, the hospital manager of social work and case management, and a survey specialist. The project also involved interactions from a multidisciplinary staff, including other NCCU health care team members, the palliative care department, other critical care specialty teams, data analytics and support, QI analysis services, other survey specialists, social work, case management, and nursing leadership.
Interventions
Baseline Evaluation: Survey and Feedback
All NCCU staff, including attending physicians, nursing, social workers, and case management, were informally and formally surveyed. Surveys were used to gather insights pertaining to perceived barriers and facilitators to SDM communication with surrogates, as well as to identify change ideas, key drivers, measures, and potential variations in practice.
SDM Bundle
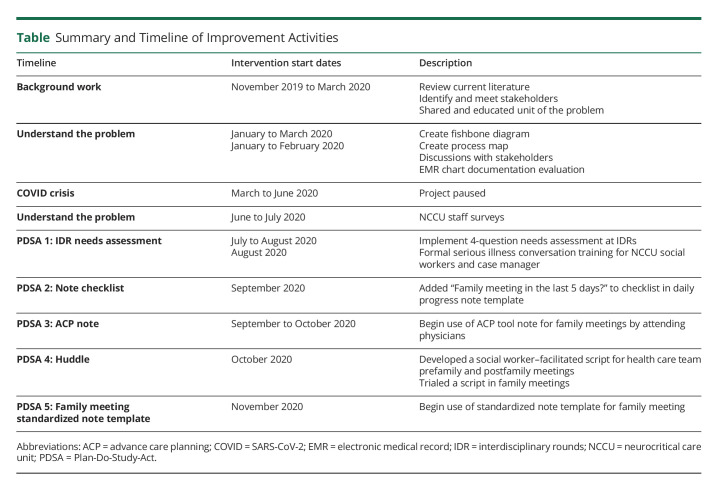
The results of the surveys were used to identify change ideas for testing and to develop the SDM bundle (Table).
Table.
Summary and Timeline of Improvement Activities
Change Idea: Social Worker–Driven SDM Conversation
An educational campaign focused on SDM and serious illness conversations was provided to the NCCU social workers (2 providers) and case manager (1 provider), consisting of a 3-hour training and simulation with palliative care department attending physicians. Based on this training, social workers and case managers were equipped to assist and run SDM conversations in the NCCU in collaboration with the neurointensivist.
Change Idea: Implement Social Worker–Driven Documentation
Through discussion with the social worker and a neurointensivist lead, an EHR documentation tool was created in the form of a standardized note template. This template was created by evaluating other health care system's advanced care planning (ACP) tools online using the Epic Systems software (Epic, Verona, WI) national Epic UserWeb database. It was then vetted by the neurointensivist lead and the NCCU social worker to ensure it met the inpatient needs of the critically ill. The template incorporated additional questions which overlapped with social workers' needs and were important for neuroprognostication (eFigure 1, links.lww.com/CPJ/A396). It was targeted for social worker use because they were present at all family meetings and would consistently document social needs after SDM meetings. The social worker already worked very closely with families and now also had training in serious illness conversations and language. These qualities made them ideal candidates for driving comprehensive and consistent documentation. The standardized note template was searchable within a patient's chart so providers could efficiently locate previous discussion content and was developed to make it easy for researchers to track discussion components in defined fields in the EHR, to better facilitate measurement of utilization.
Change Idea: Implement Social Worker–Driven Health Care Team Huddle
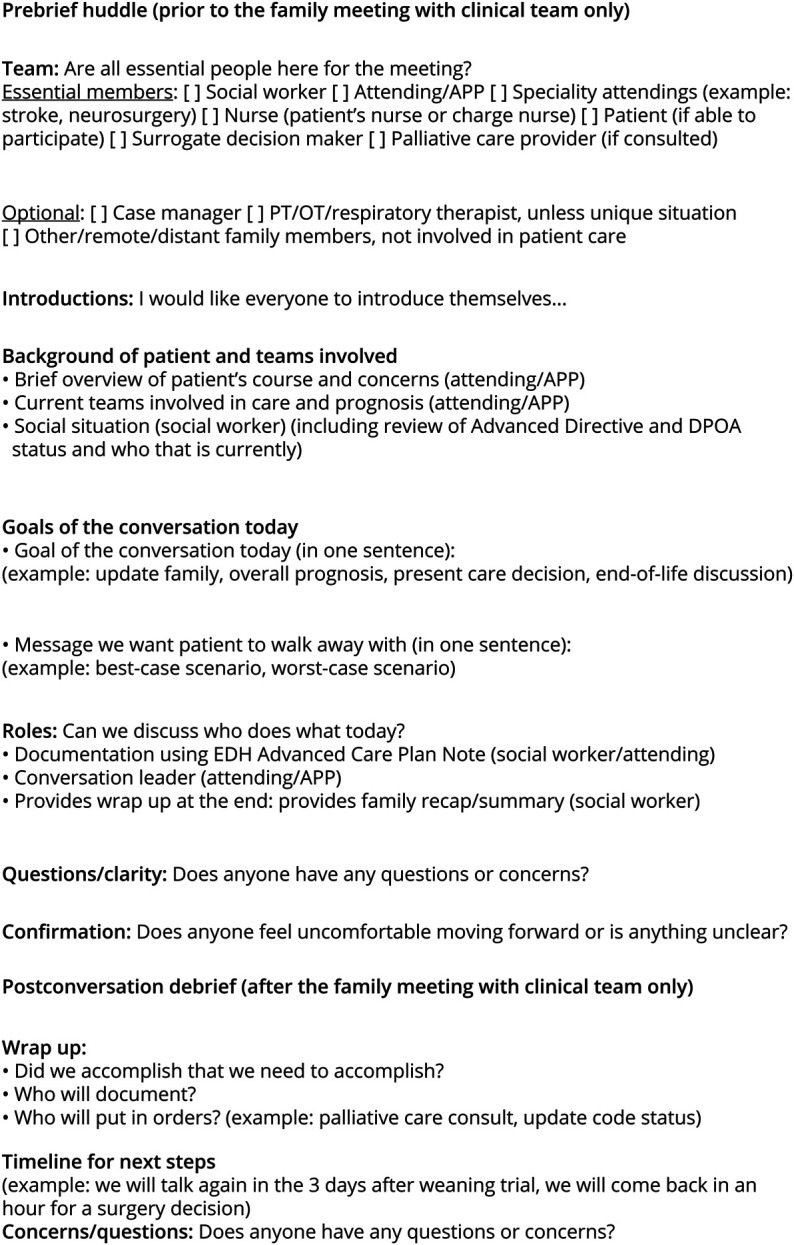
To create consistent messaging between health care teams, including subspecialties, and patient families, an SDM workflow for health care team huddles facilitated by the NCCU social worker was incorporated into the NCCU workflow. Two huddles were performed with a short scripted guide (Figure 2), one before (a “prebrief”) and one after (a “debrief”). The social worker led the huddles. The huddles required, at a minimum, attendance from the NCCU attending physician, consulting subspecialists critical for prognostication messaging, the social worker, and the patient's nurse. Additional team members would be required depending on the patient case. The conduct of a prebrief and debrief would be documented and monitored in the new standardized note template.
Figure 2. Prebrief and Debrief Huddle Template.
Data Measures and Collection
Baseline SDM conversation documentation in the NCCU was manually abstracted from the EHR prospectively. During the intervention, an EHR data analytics query was used to retrieve specific data. To ensure accuracy of the data, a manual evaluation and comparison of the intervention data was also conducted.
We defined our primary outcome measure, standardized note template utilization, as the proportion of family meetings occurring in the NCCU which were using the standardized note template. Process measures included (1) the day of standardized note template utilization, (2) the proportion of documented conversations occurring in the NCCU which were using the prebrief huddle, and (3) the proportion of documented conversations occurring in the NCCU which were using the debrief huddle. Balancing measures included (1) proportion of palliative care consults within the NCCU, (2) day of palliative care consultation within the NCCU, (3) NCCU length of stay (LOS), and (4) hospitalization mortality rate.
Analysis
Survey
Qualitative evaluation was performed on the NCCU survey results to better understand themes surrounding communication barriers (eTable 1, links.lww.com/CPJ/A396). The following themes were identified: (1) inconsistencies with messaging to patients' families, (2) inconsistent and difficult to locate documentation, and (3) lack of a protocolized system for communication. Representative quotes from the qualitative evaluation can be found in eTable 2.
NCCU staff (attending physicians, nursing, social workers, and case management) were then formally surveyed, with a response rate of 68.6% (24 of 35). More than 60% of respondents identified 3 main barriers for SDM conversations: (1) team member conflicting prognostic views, (2) meeting coordination, and (3) coordinating specialists. More than 65% of respondents attributed documentation challenges to (1) lack of a protocolized checklist for SDM conversations or (2) lack of an EHR documentation system for SDM conversations. 31% of respondents believed a premade EHR note template with checkboxes would be the best solution for documentation challenges, and 40% of respondents preferred a standardized approach, including prespecified diagnostic criteria or a needs checklist.
Measures
All measures were examined using QI Macros 2020 (KnowWare International, Inc., Denver) to construct statistical process control (SPC) charts for analysis with special cause variation evaluated using Westgard detection rules.17,18 The primary outcome measure, standardized note template utilization, was evaluated using proportions analysis (p-chart). A subanalysis looking at the average days between failure of note template utilization was also performed, using time to event analysis for rare events (t-chart). The day of standardized note template utilization process measure was evaluated using SPC analyses for individual continuous measures (XmR chart). The prebrief and debrief huddle utilization process measures were evaluated using an SPC p-chart. The day of palliative care consult and NCCU LOS balancing measures were evaluated using SPC analyses for multiple continuous measures (XBarS charts). The proportion of palliative care consults and NCCU mortality rate balancing measures were evaluated using p-charts.
Standard Protocol Approvals, Registrations, and Patient Consents
This study was reviewed by the hospital's Institutional Review Board and was determined to be a QI activity and exempt from review as human subjects research.
Data Availability
Data not provided in the article because of space limitations may be shared (anonymized) at the request of any qualified investigator for purposes of replicating procedures and results.
Results
Baseline evaluation of NCCU characteristics was performed before any intervention. Over 12 months of NCCU operations, a total of 600 patients were admitted to the unit, with an average monthly admission of 50 patients, 46.5% female and 53.5% male. The overall mortality rate was 10.7%. The average NCCU LOS was 4.7 days with an average hospitalization length of 10.2 days. The overall proportion of patients with palliative care consultations was 11.0%, and the average day of consultation was day 8.5.
SPC analysis was conducted before interventions to evaluate the stability of the baseline estimates. The baseline characteristics did not vary significantly except for NCCU LOS and day of palliative care consult. These both exhibited stable variation over time.
We manually abstracted a convenience sample of 26 patient records over a 2-month period to serve as a baseline for comparison. To be selected, patients had to be admitted to the NCCU for over 24 hours. Of the 26 patients, only 7 (27%) had documented SDM conversations, with no specific or consistent format of documentation. On average, the day of SDM documentation was NCCU day 9, with only 2 (28.6%) patients having documented conversations before or at day 7 (the first full week) of NCCU LOS.
During the intervention, we followed 24 individual patients with 35 family meeting notes documented. For our primary outcome measure, 35 (83.3%) of 42 total family meetings used the standardized note template method introduced by the SDM bundle. This is a 56% increase in the documentation rate from baseline. On SPC proportion analyses over time, we found an average standardized note template utilization rate of 83.3% with only 1 area of nonrandom variation observed, suggesting that most estimates were stable and reliable. The variation was secondary to a social worker not being present in the NCCU. Of note, there was also a ceiling effect identified (eFigure 2, links.lww.com/CPJ/A396). The subanalysis SPC t-chart (time-to-event analysis) found the average days between failure of standardized note template utilization was 6.0 days and had no special cause variation.
For our process measures, the average day of standardized note template use was day 4.9, which is a 4.1 day reduction from the baseline documentation average. In addition, 19 patients (79%) were documented using the standardized note template before or at day 7 of NCCU LOS, which is a 50.4% increase from baseline documentation. On SPC analysis, the day of standardized note template utilization SPC XmR chart had a statistically stable overall average of day 4.9 (eFigure 3, links.lww.com/CPJ/A396). Thirty-three (94.3%) of the 35 documented meetings using the standardized note template performed a prebrief huddle, and 22 (62.9%) of the meetings performed a debrief huddle. On SPC analysis, the prebrief huddle SPC p-chart average was 91.4%, and the debrief huddle SPC p-chart average was 60.0%. Both demonstrated statistically stable patterns, although a ceiling effect was again noted on the prebrief huddle analysis (eFigure 4).
All 4 balancing measure estimates remained unchanged over the course of the intervention. The baseline mortality rate which had fluctuated preintervention between the period of May and December 2020 from 10% to 14%, remained stable at 14% during the intervention.
NCCU LOS did not change from 4.7 days, palliative care consultation rate stayed at 11.0%, and day of palliative care consult slightly decreased to day 8.1.
Discussion
We successfully identified and implemented a new SDM bundle in an NCCU. This bundle included an SDM documentation system, improving documentation rates by 56% (a 3-fold increase) and decreasing time to documentation by 4.9 days. It also included an SDM conversation workflow with a social worker–facilitated huddle system, resulting in huddle rates of 94.3% (prebrief) and 62.9% (debrief). There were no significant changes in palliative care consult workflows, NCCU LOS, or mortality rates. This demonstrates that it is possible to implement an SDM bundle that is effective at standardizing communication and enabling SDM conversations to occur sooner, without introducing new burdens on the unit.
The high rate of standardized note template and huddle utilization was achieved after pivoting from a provider-driven approach to a team-driven approach focused on utilization of the social worker. Because palliative care providers are limited in number and in high demand, critical care units must focus on creating workflows which use internal resources to achieve their needs.13 Solutions which incorporate existing members of the health care team in new and suitable roles that allow them to practice at the highest level of licensure represent effective and innovative strategies for team-based care. Social workers are often trained in counseling and have close, consistent interactions with patients and their families. In our case, the SDM bundle was well-received and implemented by the care team and social workers were eager to help develop SDM practices within the unit.
Creating a standardized note template tailored to the inpatient needs of the NCCU attending physicians and social worker helped to reduce friction and drive support for the project. With the streamlined note, the SDM bundle takes very little time to perform, adding only a few minutes for the huddle, and approximately 10–15 minutes for documentation. No additional consult burden is introduced, and no new temporary or permanent staff is required.
Our findings are consistent with studies within Accountable Care Organizations, where case managers and social workers have demonstrated effectiveness in SDM communication.19,20 Lally et al.20 described an SDM system in which nurse case managers delivered a 6-question script through the telephone, resulting in an overall increase of documented conversations from 33% to 86% within a year. Billie et al.19 focused on both case managers and social workers using an SDM protocol to achieve a documentation rate of 76%. No social worker–driven SDM processes have been described in the ICU literature.
SDM is becoming an important component of high-quality care practices. The American College of Physicians has recommended that such discussions begin early because earlier discussions are associated with improved quality of life, reduced use of nonbeneficial medical care, care more consistent with patients' goals, improved family outcomes, and reduced costs.4 They also recommend that barriers to this communication be overcome using a structured communication format and improved documentation.4 Related studies of ACP show that a lack of documentation around ACP can lead to reduced quality of life, increased stress for patients and surrogate decision makers, and care that is misaligned with patient wishes.3,5-10,21
Measuring the “when, where, and with whom” SDM communication happens is a prerequisite for delivering goal concordant care (GCC), an important priority in many ICUs.22 The literature suggests that verbal ACP interventions alone are unlikely to be effective without documentation, meaning that a comprehensive bundle, inclusive of documentation, verbal communication, and standardization, is a better option.23,24 Our standardized SDM bundle meets these needs, which removes a major barrier to the improvement of GCC, while being feasible to implement, and not overly burdensome to the unit. In the NCCU literature, no other specific, implemented, standardized SDM process has been described which satisfies these requirements.
This work has several limitations. This project was implemented at a single-center, quaternary rural academic setting. This may limit the generalizability of the work. Patient demographics were not collected. Given the magnitude of the effect on documentation rate, it is unlikely to be explained by a bias in sampling. Secondary to the COVID pandemic, the scope of the project's measures had to be narrowed. Initially we anticipated including patient experiences and cost outcomes. Hospital visitation rules markedly decreased visits, and patient surrogate experiences were limited. The hospital's financial team had been interested in monitoring progress of the intervention for cost analysis; however, with the pandemic, their services were required in other areas of the hospital.
The interventions implemented in this SDM bundle initiative improved SDM documentation by 56%, an overall 3-fold improvement, decreased day of documentation by approximately 5 days, and implemented a new social worker–driven SDM conversation workflow. These changes were achieved without altering other workflows, such as palliative care needs, and recognized using all members of the health care team, including social workers, as key contributors to achieving improved SDM processes.
With the tools to begin measuring SDM processes in the unit, additional interventions specifically aimed at improving the quality of SDM can be undertaken. These could build on improvements sustained from the implementation of this intervention alone. Future directions can focus on improving the quality of documentation when the social worker is not present and continuing to improve the quality of our SDM conversations by implementing an NCCU-tailored serious illness conversation and training for the NCCU health care team. Another future direction to consider is focusing on the variation of SDM conversations between different patient types and improving equity with consideration for non-native English speakers, the healthcare-illiterate, or family members unable to be constantly present. This project has recognized there is limited understanding of SDM processes, GCC, and QI within the critical care setting, specifically neurocritical care. Further studies focused on the neurocritical care population could help drive future interventions.
Study Funding
Dartmouth-Hitchcock Medical Center's Diamond Mini Grant.
Disclosure
The authors report no relevant disclosures. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Elwyn G, Laitner S, Coulter A, Walker E, Watson P, Thomson R. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. [DOI] [PubMed] [Google Scholar]
- 2.Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Soc Sci Med. 1997;44(5):681-692. [DOI] [PubMed] [Google Scholar]
- 3.Abbott KH, Sago JG, Breen CM, Abernethy AP, Tulsky JA. Families looking back: one year after discussion of withdrawal or withholding of life-sustaining support. Crit Care Med. 2001;29(1):197-201. [DOI] [PubMed] [Google Scholar]
- 4.Bernacki RE, Block SD. American College of Physicians High Value Care Task F. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Intern Med. 2014;174(12):1994-2003. [DOI] [PubMed] [Google Scholar]
- 5.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. 2010;340:c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fried TR, O'Leary JR. Using the experiences of bereaved caregivers to inform patient- and caregiver-centered advance care planning. J Gen Intern Med. 2008;23(10):1602-1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heyland DK, Cook DJ, Rocker GM, et al. Decision-making in the ICU: perspectives of the substitute decision-maker. Intensive Care Med. 2003;29(1):75-82. [DOI] [PubMed] [Google Scholar]
- 8.Houben CHM, Spruit MA, Groenen MTJ, Wouters EFM, Janssen DJA. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(7):477-489. [DOI] [PubMed] [Google Scholar]
- 9.Walker E, McMahan R, Barnes D, Katen M, Lamas D, Sudore R. Advance care planning documentation practices and accessibility in the electronic health record: implications for patient safety. J Pain Symptom Manage. 2018;55(2):256-264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wubben N, van den Boogaard M, van der Hoeven JG, Zegers M. Shared decision-making in the ICU from the perspective of physicians, nurses and patients: a qualitative interview study. BMJ Open. 2021;11(8):e050134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Couet N, Desroches S, Robitaille H, et al. Assessments of the extent to which health-care providers involve patients in decision making: a systematic review of studies using the OPTION instrument. Health Expect. 2015;18(4):542-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weissman DE, Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23. [DOI] [PubMed] [Google Scholar]
- 14.Langley GLMR, Nolan KM, Nolan TW, Normal Cl, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance, 2 ed Edition. Jossey-Bass Publishers; 2009. [Google Scholar]
- 15.Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (standards for QUality improvement reporting excellence): revised publication guidelines from a detailed consensus process. Perm J. 2015;19(4):65-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson EC, Mohr JJ, Batalden PB, Plume SK. Improving health care, Part 1: the clinical value compass. Jt Comm J Qual Improv. 1996;22(4):243-258. [DOI] [PubMed] [Google Scholar]
- 17.Perla RJ, Provost LP, Murray SK. The run chart: a simple analytical tool for learning from variation in healthcare processes. BMJ Qual Saf. 2011;20(1):46-51. [DOI] [PubMed] [Google Scholar]
- 18.Benneyan JC, Lloyd RC, Plsek PE. Statistical process control as a tool for research and healthcare improvement. Qual Saf Health Care. 2003;12(6):458-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Billie ME, Letizia M. Serious illness conversations: a case management quality improvement project. Prof Case Manag. 2020;25(4):220-229. [DOI] [PubMed] [Google Scholar]
- 20.Lally K, Tuya Fulton A, Ducharme C, Scott R, Filpo J. Using nurse care managers trained in the serious illness conversation guide to increase goals-of-care conversations in an accountable care organization. J Palliat Med. 2020;23(1):112-115. [DOI] [PubMed] [Google Scholar]
- 21.Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med. 2014;28(8):1000-1025. [DOI] [PubMed] [Google Scholar]
- 22.Sanders JJ, Curtis JR, Tulsky JA. Achieving goal-concordant care: a conceptual model and approach to measuring serious illness communication and its impact. J Palliat Med. 2018;21(S2):S17–S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Turnbull AE, Hartog CS. Goal-concordant care in the ICU: a conceptual framework for future research. Intensive Care Med. 2017;43(12):1847-1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Halpern SD. Goal-concordant care - searching for the holy grail. N Engl J Med. 2019;381(17):1603-1606. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data not provided in the article because of space limitations may be shared (anonymized) at the request of any qualified investigator for purposes of replicating procedures and results.