Abstract
Purpose of Review
Clinical trials for Huntington disease (HD) have primarily focused on managing chorea and, more recently, the development of disease-modifying therapies (DMTs). Nonetheless, understanding health services among patients with HD is essential for assessing new therapeutics, development of quality metrics, and overall quality of life of patients and families with HD. Health services assess health care utilization patterns, outcomes, and health care–associated costs, which can help shape the development of therapeutics and aid in policies that affect patients with a specific condition. In this systematic literature review, we analyze data of published studies looking at causes of hospitalization, outcomes, and health care costs in HD.
Recent Findings
The search yielded 8 articles published in the English language and comprising data from the United States, Australia, New Zealand, and Israel. The most common cause of hospitalization among patients with HD was dysphagia or dysphagia-related complications (e.g., aspiration pneumonia or malnutrition), followed by psychiatric or behavioral symptoms. Patients with HD had more prolonged hospitalizations than non-HD patients, and it was most prominent among those with advanced disease. Patients with HD were more likely to be discharged to a facility. A small percentage received inpatient palliative care consultation, and behavioral symptoms were a primary cause of discharge to another facility. Interventions such as gastrostomy tube placement had associated morbidity, and it was common among patients with HD with a diagnosis of dementia. Palliative care consultation and specialized nursing care were associated with more routine discharges and fewer hospitalizations. In terms of cost, patients with HD with private and public insurances had the highest expenditure with more advanced disease, and expenses were associated with hospitalization and medication costs.
Summary
In addition to DMTs, HD clinical trial development should also consider the leading causes of hospitalization, morbidity, and mortality in patients with HD, including dysphagia and psychiatric disease. No research study, to our knowledge, has systematically reviewed health services research studies in HD. Evidence from health services research is needed to evaluate the efficacy of pharmacologic and supportive therapies. This type of research is also critical in understanding health care costs associated with the disease and to better advocate and shape policies that can benefit this patient population.
Huntington disease (HD) is an autosomal dominant neurogenetic condition that presents with a triad of behavioral dysfunction, involuntary movements, and cognitive impairment. Symptoms usually present between the ages of 30 and 40 years, and life expectancy is between 10 and 20 years after diagnosis. Three disease stages exist based on the level of functional impairment of the individual, with people in early stages presenting with psychiatric and behavioral symptoms and those in late stages exhibiting significant physical disabilities, swallowing dysfunction, and dementia. Current HD epidemiology data report a prevalence of 4–7 per 100,000 persons among most European countries, although in certain regions such as British Columbia, Canada, it may be as high as 13.7 per 100,000.1,2 In the United States, it is estimated that the incidence rate of HD over 14 years is about 1.22 per 100,000 persons.3
Given a young age at onset during critical years of peak income potential, patients with HD are at risk of losing employment at an early age because of physical, mental, and cognitive disabilities before retirement. These features also lead to high health care expenditure for patients and families, leading to a generational downward socioeconomic drift in families with HD. Furthermore, individuals with a family history or a confirmed HD diagnosis are often denied long-term care disability insurance.4
HD research has focused on improving the biological understanding of the disease and the development of symptomatic treatments and disease-modifying therapies (DMTs) to halt the progression of the disease. Many DMTs involve genetic manipulations with complex modes of delivery through lumbar punctures or direct brain injections. These modes of delivery raise concerns about the cost and accessibility of these therapies.5-7
Given the potentially high costs of DMTs, understanding health care utilization patterns, outcomes, and costs will become increasingly important, as new HD therapeutics enter the market. This information will be important in the development of HD quality metrics. This review summarizes existing health services research in HD, including health care utilization patterns, outcomes, and associated costs. Based on the current literature, we discuss gaps in HD health services research and HD-specific policy suggestions.
Methods
We performed a systematic literature review using MEDLINE, reviewing primary literature published between 2000 and 2021. The search took place between November 2021 and April 2022. One author (A.M.) conducted a literature extraction and examination in November 2021, and the second author (J.D.) examined the extracted literature in March 2022. A review by the second author led to the same findings as the first author. The inclusion criteria included studies on hospitalization patterns in adults with HD and health care costs associated with the disease. We were interested in articles discussing the causes of hospitalization for patients with HD, causes for morbidity/mortality, in-hospital procedures, posthospital discharge and placement, and causes of readmission. The primary MeSH term used was “Huntington's Disease,” in addition to health services research terms including “Healthcare Utilization,” “Hospitalizations,” “Emergency Room,” “Emergency Services,” and “Healthcare Costs.” Literature reviews, case reports, and case studies were excluded from the search. COVID-19–related studies were also excluded because this represents an extraordinary epidemiologic presentation and not usual HD care.
Results
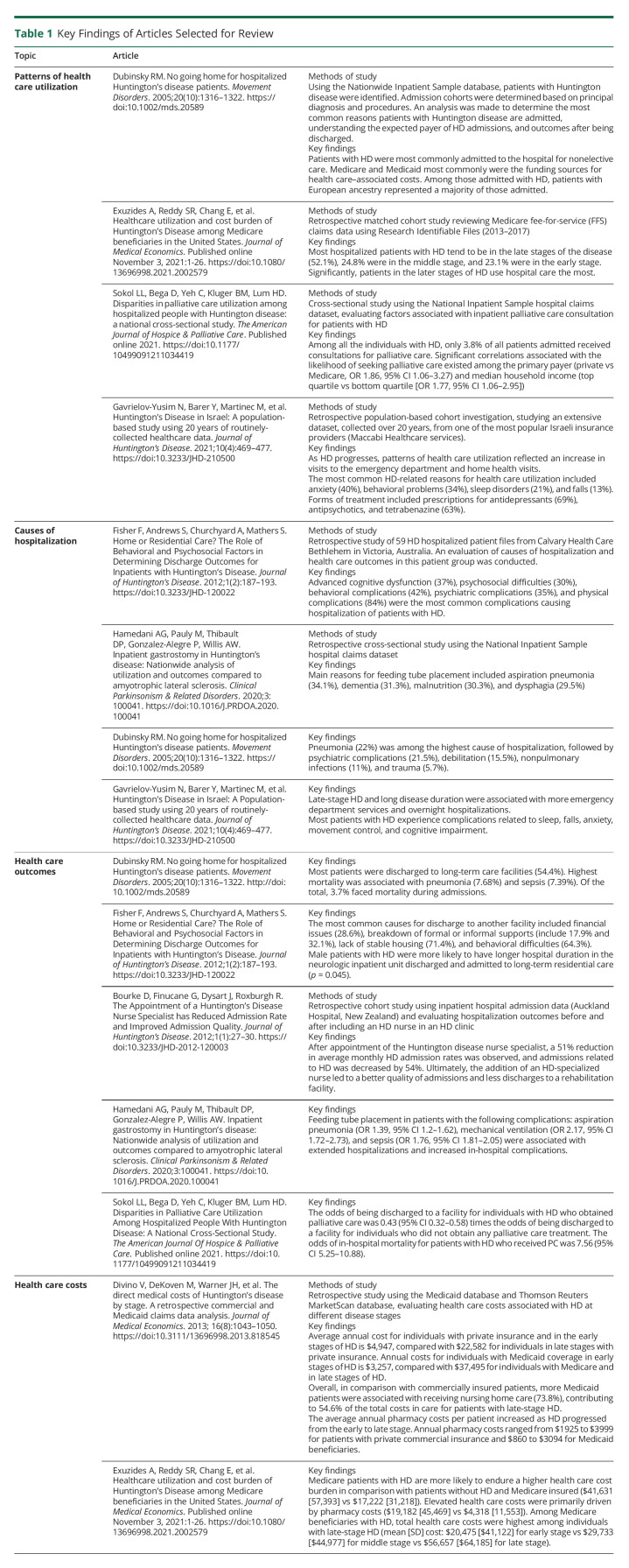
The search yielded 25 articles. Ten abstracts met inclusion criteria. One paper was excluded because it discussed patients' perceived needs and outcomes8 (Figure). Five studies used the US claims datasets, with the Nationwide Inpatient Sample or National Inpatient Sample being the most used datasets. One study presented claims data from 1 of 4 publicly funded insurance companies in Israel, and the retrospective chart reviews presented data from hospitals in Australia and New Zealand. A total of 8 articles met the inclusion criteria for assessment. One report was not available online nor through an interlibrary loan request. Abstract data from this article are included in the review. Table 1 summarizes the key findings of the articles selected for review.
Figure. Literature Review Selection Process.
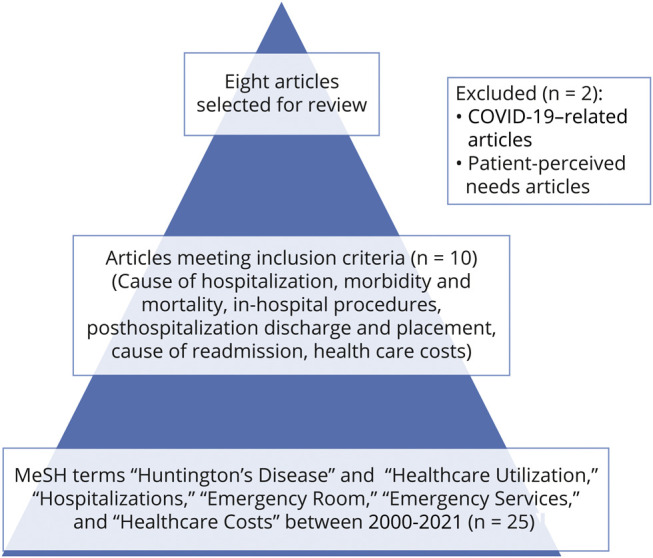
Table 1.
Key Findings of Articles Selected for Review
Patterns of Health Care Utilization
Hospitalized patients with HD tend to be in the late stages of the disease.9 Late-stage HD and long disease duration were associated with more emergency department services and overnight hospitalizations.9,10 However, Medicare patients with HD in any stage of the disease were more likely to use emergency department services, be hospitalized, and less likely to use office visits.9 Based on data using the National Inpatient Sample between 2003 and 2010, there has been a linear increase in the number of HD admissions in the United States.
Of the US studies that presented data on all insurance types, patients with HD were mainly covered by Medicaid or Medicare.11-13 There was a noteworthy representation of Medicare beneficiaries in the US claims data literature.9,11-13 This finding is notable considering that the average onset of HD is 30–40 years of age, and life expectancy ranges between 10 and 20 years, which suggests that patients with HD with Medicare are eligible because of their level of disability and not necessarily based on age. The over-representation of Medicare benefitiares also indicates that hospitalization data in HD may be biased towards patients with more disability.
Causes of Hospitalization
Most patients with HD were hospitalized because of swallowing dysfunction and its associated complications, psychiatric conditions, cognitive impairment, and physical disabilities.9-16 Common complications of swallowing dysfunction included aspiration pneumonia, malnutrition, and dehydration.12 The most common psychiatric conditions associated with admission were depression and anxiety,9,10,14,15 and regardless of the stage of the disease, most patients with HD were prescribed an antidepressant or anxiolytics.9,16 Patients with HD with depression were also less likely to receive palliative care consultation services.13 Although the authors did not explain the reason for this finding, it is possible that those admitted due to depression tended to be younger patients with HD with less advanced disease requiring palliative consultation. Nonetheless, psychiatric illness was a common comorbidity and cause of admission in patients with HD, although it is unclear whether it is associated with a specific disease stage.
Advanced cognitive impairment or dementia is a hallmark of late stages of HD. Cognitive dysfunction, senility, and dementia are common causes of admission in patients with HD.12,14,16 In a study reviewing feeding tube placements in HD, the authors noted that dementia was commonly associated with this procedure.11 Feeding tube placement is not recommended for patients with Alzheimer dementia. Physicians recommend against this procedure in this patient group because of high rates of medical complications with little survival benefit or improvement in the quality of life.17 It is not clear whether there is a survival benefit for patients with HD because quality metrics for HD do not exist currently. Additional studies are necessary to evaluate the cost effectiveness of this procedure in HD.
Health Care Outcomes
Hospitalized patients with HD are likely to be discharged to a long-term care facility.12,16 In a small study of patients with HD seen in a neurologic unit in Australia, the authors found that psychosocial difficulties, such as financial issues, breakdown of formal or informal supports, and unstable housing, were some of the factors associated with discharge to a long-term facility.16 The same study found that irritability, aggression, and apathy were associated with a discharge to another facility. On average, these patients also had more prolonged hospitalizations. At the end of life, patients with HD also have high utilization of health care services, including inpatient hospitalizations and emergency department visits.9 A small percentage, however, of all patients with HD received inpatient palliative care consultation, and privately insured and high-income patients were more likely to receive these services.13 Feeding tube placement was also associated with more prolonged hospitalizations and in-hospital complications, including death.11 This same study found that patients with HD with feeding tube placement were more likely to be discharged to a long-term facility, primarily if they had a diagnosis of dementia or delirium during the admission.
Only 2 studies discussed interventions lowering health care utilization. One retrospective study from New Zealand found that HD-specialized nursing services were associated with fewer hospitalizations, a better quality of admissions, and more discharges to patients' original residence.14 Palliative consultation was also associated with a greater likelihood of discharge to home with services.13
Health Care Costs
Admissions for respiratory dysfunction, debilitation, trauma, and sepsis were associated with the highest inpatient hospital charges.12 For all patients with HD, regardless of the insurance payor type, health care costs increased as the disease progresses.9,15
Among commercially insured patients with HD, the average annual cost during the early stages of the disease is $4,947 and in late stages is $22,582.15 For Medicaid patients, the yearly cost in the early stages is $3,257 and $37,495 in the late stages.15 Among Medicare beneficiaries, the mean annual cost in early HD was $13,264 compared with $40,761 in late HD.9
The main drivers of health care costs varied based on insurance coverage. In commercially insured patients with early-stage HD, most of the expenses were ancillary services, followed by pharmacy costs.15 With disease progression, there were more costs associated with inpatient hospitalizations. Medicaid beneficiaries also saw a similar trend. With disease progression, the costs shifted from outpatient costs (including ancillary services) and pharmacy costs to inpatient hospitalization costs.15 Patients with Medicaid were also more likely to use inpatient services in earlier stages of the disease, and pharmacy costs were lower than those commercially insured.
Compared with Medicaid, patients with HD with Medicare incur higher health care costs. In this group, most of the costs are driven by pharmacy costs. On average, patients with HD with Medicare pay $19,182 a year in prescription drugs.9 Inpatient hospitalizations are the second source of expenses ($13,325), followed by outpatient costs ($10,213). Similarly, with disease progression, there is an increase in health care costs.
Discussion
Patients with HD in late stages are likely to be hospitalized and incur high health care costs, particularly during the end of life.9,12,15 The most common causes of hospitalizations in patients with HD are those associated with late-stage HD, including swallowing dysfunction and related complications such as aspiration pneumonia, malnutrition, and sepsis.12 These conditions are also associated with the highest morbidity, mortality, and long inpatient hospitalizations.12 Psychiatric disorders, behavioral disturbances, and cognitive impairment are other common causes of hospitalization.10,12,15,16 Patients with HD are also more likely to be discharged to long-term facilities, and dementia, behavioral disturbances, and psychosocial difficulties are associated with a greater likelihood of long-term placement.11,12,16 Multidisciplinary approaches such as HD-specialized nursing care and palliative care consultation are associated with a lower length of hospitalization and a lower likelihood of discharge to a long-term facility.13,14 Other interventions such as feeding tube placement may be related to high inpatient comorbidities, and more studies are needed to evaluate its utility in patients with HD.11
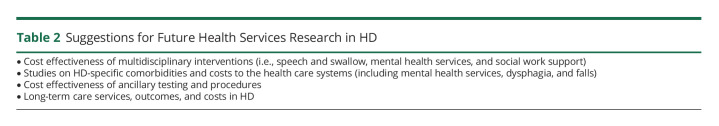
This literature review highlights critical areas of intervention for developing HD quality metrics and future research areas that can identify cost-effective interventions for the care of patients with HD (Table 2). Swallowing difficulties and their complications were the leading cause of hospitalization for patients with HD. Speech and swallow therapy is crucial in preserving swallowing function and early recognition of interventions necessary to improve swallowing or avoid complications. These therapies may reduce morbidity and mortality associated with malnutrition or aspiration pneumonia. It has been recognized that psychological and psychiatric care is vital in the management of HD. This review found that psychiatric conditions and behavioral disturbances were a common cause of hospitalization. In the United States, however, many challenges continue to exist in accessing mental health services. Considering that mental health illnesses such as substance abuse are also associated with earlier onset of motor symptoms, HD18,19 psychiatric care should be consistently incorporated in the care of all patients with HD, and policy interventions advocating for better access and reimbursement of mental health services are critical for the adequate care of patients with HD. Other interventions that can reduce health care utilization and costs include palliative and hospice care services and HD-specialized nursing care. Avoiding high health care use at the end of life is important to contain overall health care costs for the health care system but even more so for families with HD who may be at risk of developing the disease themselves, along with its related financial difficulties. More studies evaluating the cost effectiveness of multidisciplinary interventions in HD care are needed.
Table 2.
Suggestions for Future Health Services Research in HD
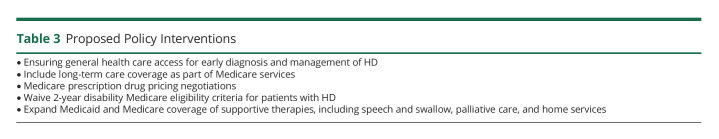
For patients at all stages of HD, there are high health care costs associated with ancillary services. Future research needs to identify which patients with HD are using ancillary services and whether these services are warranted.15 Given the health care costs associated with HD, policy interventions should be considered (Table 3). First of all, access to general health care services is key for the prompt diagnosis and early management of HD. In the United States, patients with disabilities are eligible for Medicare coverage, and many patients with HD qualify because of physical and cognitive disabilities associated with the disease. However, patients with a disability, including patients with HD, must wait 2 years before they are eligible for Medicare, which could lead to lapses in health care coverage during those 2 years and financially catastrophic out-of-pocket expenses for patients and their families. Among hospitalized patients with HD, most of them are discharged to long-term care facilities. In the United States, these services are not covered by Medicare, and most families pay out-of-pocket costs for these services. Policies expanding long-term care coverage for Medicare beneficiaries will benefit patients with HD and their families. Controlling prescription drug pricing is another important policy that will reduce health care costs for patients with HD, particularly Medicare beneficiaries. HD is a progressively disabling disease, and at some point, most patients with HD will become Medicare eligible before reaching the age of 65 years. Controlling drug prescription costs is also essential for this patient population and even more so with the development of DMTs with complex and costly delivery modes. Pharmaceutical companies should also consider including health care utilization as an outcome of interest during the drug development stage. Furthermore, additional health economics studies should be conducted to compare the overall health care costs of HD with other neurodegenerative conditions and use this information to shape policy around neurologic conditions.
Table 3.
Proposed Policy Interventions
As with any literature review, the initial search might not have captured all articles on health care utilization in HD. Most of the studies used US-based claims datasets, and these datasets used 5%–20% of hospital samples in the United States. These samples may not be representative of all HD care in the United States. These datasets also do not include data from long-term care or psychiatric facilities. US health care system structure may also lead to many patients with HD not having access to health care and never coming in contact with the health system. Claim datasets also use unique identifiers, which prevent the identification of multiple admissions for the same patient. These datasets do not identify conditions that require multiple hospitalizations each year. This limitation may underrepresent the severity of some comorbidities. We also presented data from 4 health care systems (Australia, Israel, New Zealand, and the United States). Given the differences in each system, there may be different incentives and resources available to patients, leading to differences in health care utilization and outcomes.
This study showed that health care utilization in HD is driven by patients with late-stage disease and its associated complications of swallowing dysfunction, psychiatric illness, and cognitive impairment. These comorbidities are associated with high health care utilization and high health care costs. More cost-effectiveness studies are needed to create quality metrics for HD care and reduce health care utilization and costs. Quality metrics, including health care utilization and outcomes, should guide the development of new therapeutic agents and improve health care outcomes in HD.
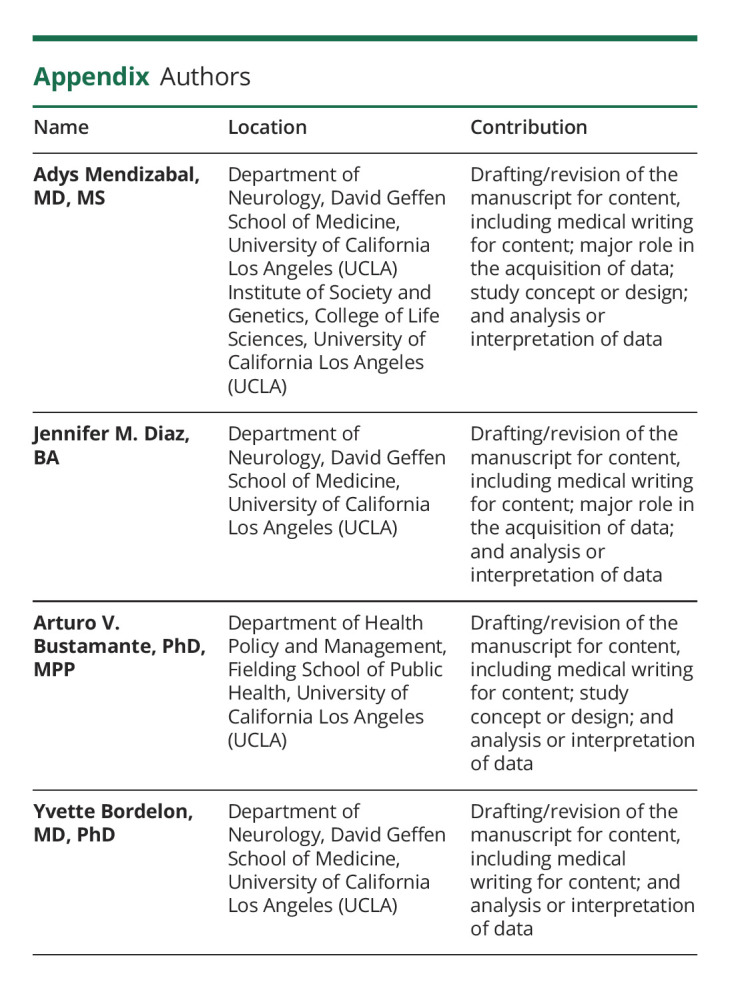
Appendix. Authors
Study Funding
This study was possible through the Huntington's Disease Society of America (HDSA) Berman-Topper Career Development Award.
Disclosure
A. Mendizabal receives grant support from the Huntington's Disease Society of America (HDSA); J.M. Diaz, A.V. Bustamante, and Y. Bordelon report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ This literature review highlights patterns of health care utilization, causes of hospitalization, health care outcomes, and health care costs in HD, information that can be used to develop HD quality metrics and identify cost-effective interventions for the care of patients with HD and their families.
→ The most common causes of hospitalizations in patients with HD are among those classified in late-stage HD and associated with complications of swallowing dysfunction, all of which are correlated with high morbidity and complications during hospitalization.
→ Multidisciplinary approaches to treatment such as HD-specialized nursing care and palliative care may be associated with decreased duration of hospitalization, and policy interventions should consider greater support for nursing and palliative care in HD.
→ Extreme costs associated with care and treatment for patients with HD reveal the importance of implementing innovative policies such as expanding long-term care coverage for Medicare beneficiaries and controlling prescription drug pricing.
References
- 1.Fisher E, Semaka A. How many people have Huntington disease? HD insights; 2011. Accessed September 26, 2018. huntingtonstudygroup.org/hd-insights/how-many-people-have-huntington-disease/.
- 2.Fisher ER, Hayden MR. Multisource ascertainment of Huntington disease in Canada: prevalence and population at risk. Mov Disord. 2014;29(1):105-114. doi: 10.1002/mds.25717. [DOI] [PubMed] [Google Scholar]
- 3.Bruzelius E, Scarpa J, Zhao Y, Basu S, Faghmous JH, Baum A. Huntington's Disease in the United States: variation by demographic and socioeconomic factors. doi: 10.1002/mds.27653 [DOI] [PMC free article] [PubMed]
- 4.Insurance and HD–HOPES Huntington's Disease Information. Accessed November 8, 2021. hopes.stanford.edu/insurance-and-hd-2/.
- 5.Kim A, Lalonde K, Truesdell A, et al. New avenues for the treatment of Huntington's disease. Int J Mol Sci. 2021;22(16):8363. doi: 10.3390/IJMS22168363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan L, Feigin A. Huntington's disease: new frontiers in therapeutics. Curr Neurol Neurosci Rep. 2021;21(3):10. doi: 10.1007/S11910-021-01093-3. [DOI] [PubMed] [Google Scholar]
- 7.Guttman M, Pedrazzoli M, Ponomareva M, et al. The impact of upcoming treatments in Huntington's disease: resource capacity limitations and access to care implications. J Huntingtons Dis. 2021;10(2):303-311. doi: 10.3233/JHD-200462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Walsem MR, Howe EI, Ruud GA, Frich JC, Andelic N. Health and quality of life outcomes. doi: 10.1186/s12955-016-0575-7 [DOI] [PMC free article] [PubMed]
- 9.Exuzides A, Reddy SR, Chang E, et al. Healthcare utilization and cost burden of Huntington's Disease among Medicare beneficiaries in the United States. J Med Econ. 2021;24:1327-1336. doi: 10.1080/13696998.2021.2002579. [DOI] [PubMed] [Google Scholar]
- 10.Gavrielov-Yusim N, Barer Y, Martinec M, et al. Huntington's disease in Israel: a population-based study using 20 years of routinely-collected healthcare data. J Huntingtons Dis. 2021;10(4):469-477. doi: 10.3233/JHD-210500. [DOI] [PubMed] [Google Scholar]
- 11.Hamedani AG, Pauly M, Thibault DP, Gonzalez-Alegre P, Willis AW. Inpatient gastrostomy in Huntington's disease: Nationwide analysis of utilization and outcomes compared to amyotrophic lateral sclerosis. Clin Park Relat Disord. 2020;3:100041. doi: 10.1016/J.PRDOA.2020.100041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dubinsky RM. No going home for hospitalized Huntington's disease patients. Mov Disord. 2005;20(10):1316-1322. doi: 10.1002/mds.20589. [DOI] [PubMed] [Google Scholar]
- 13.Sokol LL, Bega D, Yeh C, Kluger BM, Lum HD. Disparities in palliative care utilization among hospitalized people with Huntington disease: a national cross-sectional study. Am J Hosp Palliat Care. 2022;39(5):516-522. doi: 10.1177/10499091211034419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bourke D, Finucane G, Dysart J, Roxburgh R. The appointment of a Huntington's disease nurse specialist has reduced admission rate and improved admission quality. J Huntingtons Dis. 2012;1(1):27-30. doi: 10.3233/JHD-2012-120003. [DOI] [PubMed] [Google Scholar]
- 15.Divino V, DeKoven M, Warner JH, et al. The direct medical costs of Huntington's disease by stage. A retrospective commercial and Medicaid claims data analysis. J Med Econ. 2013;16(8):1043-1050. doi: 10.3111/13696998.2013.818545. [DOI] [PubMed] [Google Scholar]
- 16.Fisher F, Andrews S, Churchyard A, Mathers S. Home or residential care? The role of behavioral and psychosocial factors in determining discharge outcomes for inpatients with Huntington's disease. J Huntingtons Dis. 2012;1(2):187-193. doi: 10.3233/JHD-120022. [DOI] [PubMed] [Google Scholar]
- 17.Li I. Feeding tubes in patients with severe dementia. Am Fam Physician. 2002;65(8):1605-1610, 1515. Accessed November 12, 2021. aafp.org/afpAMERICANFAMILYPHYSICIAN1605. [PubMed] [Google Scholar]
- 18.Byars JA, Beglinger LJ, Moser DJ, Gonzalez-Alegre P, Nopoulos P. Substance abuse may be a risk factor for earlier onset of Huntington disease. J Neurol. 2012;259(9):1824-1831. doi: 10.1007/S00415-012-6415-8. [DOI] [PubMed] [Google Scholar]
- 19.Schultz JL, Kamholz JA, Moser DJ, Feely SME, Paulsen JS, Nopoulos PC. Substance abuse may hasten motor onset of Huntington disease: evaluating the Enroll-HD database. Neurology. 2017;88(9):909-915. doi: 10.1212/WNL.0000000000003661. [DOI] [PMC free article] [PubMed] [Google Scholar]