This study identifies the self-reported stressors and coping mechanisms of Dermatology residency applicants during the 2020–2021 application cycle, occurring during the coronavirus disease 2019 pandemic. The most common stressors reported were academic, family crisis, and coronavirus disease 2019. The type of stressor differed by race/ethnicity of the applicants and their geographic location.
Key Words: coping mechanisms, COVID-19, dermatology resident applicants, secondary application, stressors
Abstract
Objectives
Our aim was to identify self-reported stressors and coping mechanisms during the 2020–2021 application cycle by dermatology residency applicants. We hypothesized that coronavirus disease 2019 (COVID-19) would be the most reported stressor.
Methods
During the 2020–2021 application season, the Mayo Clinic Florida Dermatology residency program sent a supplemental application to each applicant requesting that they describe a challenging life situation and how they handled it. Comparisons of self-reported stressors and self-expressed coping mechanisms according to sex, race, and geographic region were performed.
Results
The most common stressors reported were academic (18.4%), family crisis (17.7%), and COVID-19 (10.5%). The most frequent coping mechanisms expressed were perseverance (22.3%), seeking community (13.7%), and resilience (11.5%). The coping mechanism of diligence was observed more often in females than in males (2.8% vs 0.0%, P = 0.045). First in medicine was more often observed in Black or African American students (12.5% vs 0%, P = 0.001), immigrant experience was more often observed in Black or African American and Hispanic students (16.7% and 11.8% vs 3.1%, P = 0.021), and natural disaster was reported more often in Hispanic students (26.5% vs 0.5%, P < 0.001) as compared with White applicants. By geography, applicants in the northeastern United States were more likely to report the COVID-19 pandemic as a stressor (19.5%, P = 0.049), and the natural disaster stressor was more often reported by applicants from outside the continental United States (45.5%, P < 0.001).
Conclusions
Stressors reported by dermatology applicants in the 2020–2021 cycle included academic, family crisis, and the COVID-19 pandemic. The type of stressor reported varied by race/ethnicity and geographic location of the applicant.
Key Points
The most common stressors reported by dermatology residency applicants were academic, family crisis, and coronavirus disease 2019.
First in medicine and immigrant experience were more often observed in Black or African American applications.
Immigrant experience and natural disaster were more often reported by Hispanic applicants.
Coronavirus disease 2019 was reported more commonly as a stressor in applications from the northeastern United States.
Dermatology residency applicants face multiple stressors throughout medical school, during the residency application process, and during the years of residency training. There is an increasing awareness of stressors during medical training, as well as physician suicide. Elevated suicide rates among physicians compared with nonphysician peers are by a magnitude of 1.5 times in male physicians and 2.3 times in female physicians.1 The degree to which the global coronavirus disease 2019 (COVID-19) pandemic has altered the unique stressors for dermatology residency applicants is not yet known.
Before the COVID-19 pandemic, the medical student stressors reported included time commitment,2–4 pressure or competition,2,5 academic requirements,6 relationships,6 lack of sleep,3–5,7 and exposure to patient suffering and death.2 Higher levels of stress are reported in women than in men,3,8 especially in earlier years of training.8 For dermatology residency applicants specifically, before the COVID-19 pandemic, personal statements as part of the application that were written about personal struggles were a common theme for both matched (17%) and unmatched (23%) applicants, without a statistically significant difference in match rates.9
Since the COVID-19 pandemic, new sources of stress have emerged both directly and indirectly related to the global pandemic. Limited studies are available to understand the dermatology applicant perspective. Unique stressors that have been previously reported for dermatology learners during the COVID-19 pandemic included caring for patients infected with COVID-19, adaptation to telemedicine, decrease in dermatology case volumes, limited in-person away rotations, virtual interviews, moving cities or institutions, and social distancing/isolation.10
In spring 2020, the Association of Professors of Dermatology published two statements10,11 on behalf of program directors that included the recommendation to limit in-person away rotations, except for those students without home programs available, and to conduct all interviews virtually.11 The option of virtual rotations was encouraged by the Association of Professors of Dermatology11; however, this opportunity could not be provided by all of the programs. For many trainees, there is the added stress of adjusting to a new institution or city which the applicant had never visited during the interview season.10
The aim of our study was to identify self-reported stressors and coping mechanisms during the 2020–2021 applicant cycle for dermatology residency applicants, occurring during the COVID-19 pandemic, using a dedicated supplemental application. Self-reported stressors were additionally compared by sex, race, and geographic region. We hypothesized that COVID-19 would be the stressor self-reported by most applicants during this time frame.
Methods
During the 2020–2021 application season, the Mayo Clinic Florida Dermatology residency program received 488 applications through the Electronic Residency Application Service (ERAS). All of the applicants were e-mailed a set of three secondary questions, including, “Please describe a challenging time in your life—professional or personal. How did you handle it? What did you learn from the experience?” A total of 418 applicants responded to some element of the secondary questions and were included in this retrospective study.
Information collected by the program director from the ERAS application included self-reported sex, race, and geographic location. Geographic location was based on medical school location if currently in medical school or current address provided if the applicant was already a medical school graduate. Geographic locations were categorized based on regional divisions used by the US Census Bureau.12 For those applicants who did not have a location that could be categorized based on the US regional divisions, such as US territories or international students, the designation of “other” was used.
The secondary application responses were reviewed and categorized by the dermatology program director and deidentified before sharing with the research team. Stressors and coping mechanisms were categorized based on the most common themes reported by applicants. Stressor categories included the following: no answer, COVID-19, family crisis, friend crisis, bias, first in medicine (defined as being the first in their family to be in medicine), immigrant experience, academic, patient care, mental health, physical health, natural disaster, environment, community outreach, work–life balance, financial, and other. Applicant self-expressed coping mechanism categories included no answer, adaptability, seeking community, perseverance (eg, continuing a course of action without regard for discouragement), diligence (eg, determination when doing something), flexibility, resilience, compartmentalization, gratitude, prioritization, empathy, communication, advocacy, teamwork, self-reflection, work–life balance, and other. If there was more than one provided by the applicant, then only the main coping mechanism was included in the study analysis.
Comparisons of self-reported stressors and self-expressed coping mechanisms according to sex, race, and geographic region were made using the Fisher exact test. A P < 0.05 was considered to be statistically significant, and all of the statistical tests were two sided and were performed using SAS version 9.4 (SAS Institute, Cary, NC).
The initial purpose of the secondary questionnaire sent to applicants by the program was for aiding in the holistic review of each applicant. The question of reported stressors was retrospective to the application cycle; therefore, the applicants were not aware that their responses would be categorized for research. The project was approved by our institutional review board. The information obtained was recorded by the program director in such a manner that the identity of the human subjects cannot readily be ascertained, directly or through identifiers linked to the subjects. This study meets exempt criteria, and the data obtained can be used for research without consent from the subjects. It underwent a separate review by our Education Research Committee, which approved the project with the stipulation that only those directly involved in the interview process would review the deidentified data. The program director was the only research member who reviewed the deidentified data and categorized all of the data. The statistician and remaining authors had access only to the categorized deidentified data.
Results
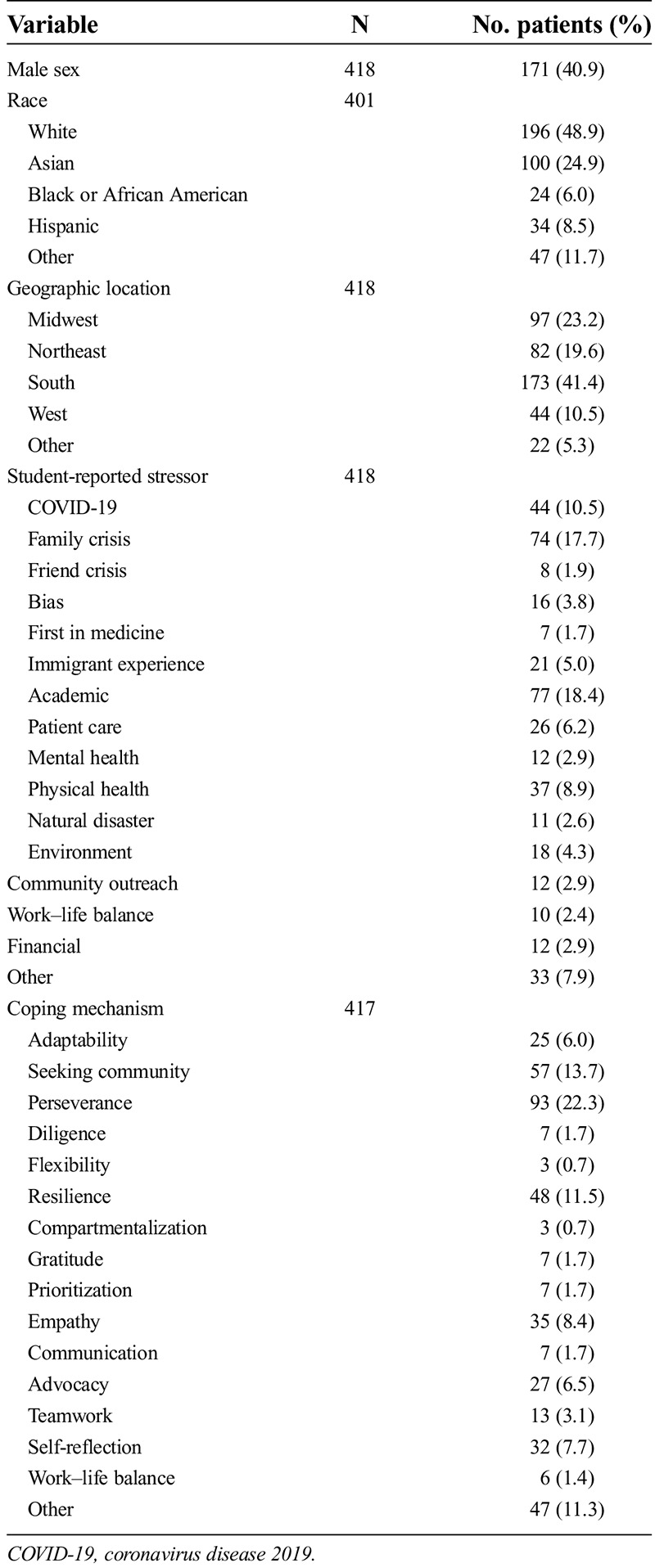
Of the 418 students, 171 (40.9%) identified as male and 247 (59.1%) identified as female. The applicants’ self-reported races/ethnicities through ERAS were as follows: 48.9% White, 24.9% Asian, 6% Black or African American, and 11.7% other. The most frequent geographic locations were the South (41.4%), the Midwest (23.2%), and the Northeast (19.6%). The most common stressors reported were academic (18.4%), family crisis (17.7%), and COVID-19 (10.5%), whereas the most frequent coping mechanisms expressed were perseverance (22.3%), seeking community (13.7%), and resilience (11.5%; Table 1).
Table 1.
Subject characteristics
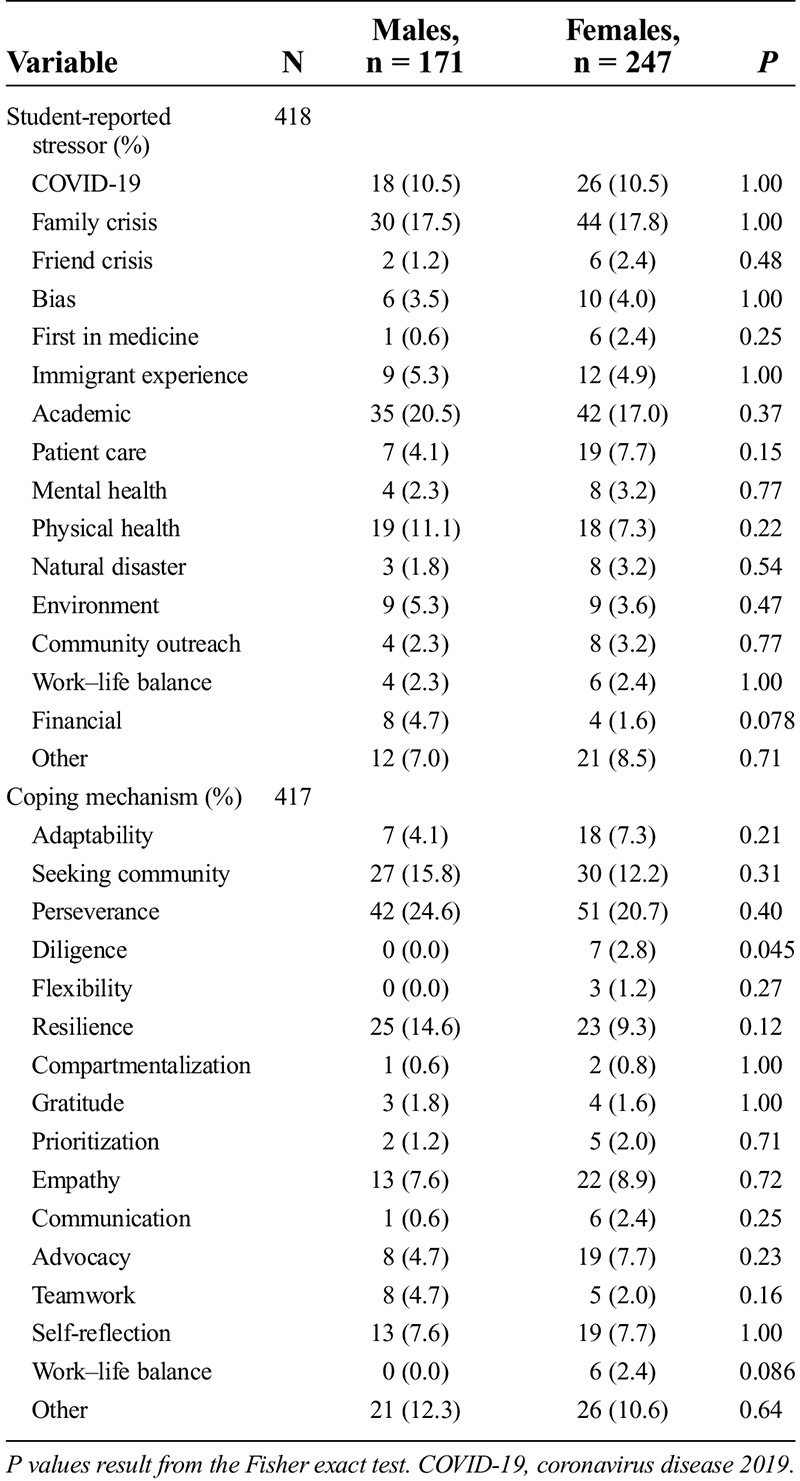
No statistically significant differences were found between males and females regarding stressors. The coping mechanism of diligence was reported more often by females than males (2.8% vs 0.0%, P = 0.045; Table 2), however.
Table 2.
Comparison of stressors and coping mechanisms according to sex
Comparisons between racial groups identified statistically significant differences in the following: first in medicine was more often observed in Black or African American students (12.5% vs 0%, P = 0.001), immigrant experience was more often observed in Black or African American and Hispanic students (16.7% and 11.8% vs 3.1%, P = 0.021), and natural disaster reported more often in Hispanic students (26.5% vs 0.5%, P < 0.001) as compared with White applicants (Table 3).
Table 3.
Comparison of stressors and coping mechanisms according to race
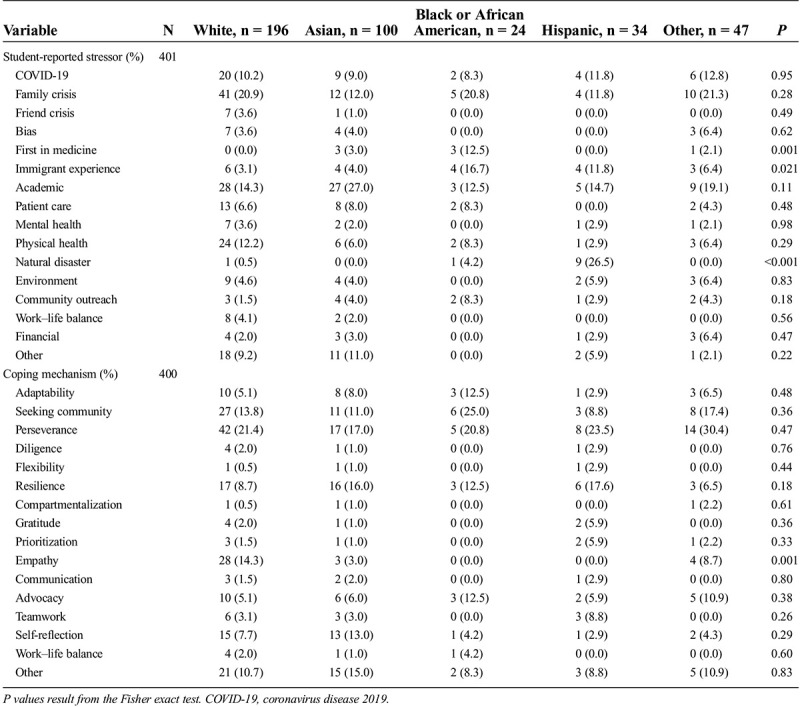
Within each racial group, general trends also were identified. The most common student-reported stressors among White applicants were family crisis, academic, and physical health. Academic and family crisis were most commonly reported among Asian applicants. Black or African American applicants identified family crisis, immigrant experience, and first in medicine as most common stressors. Hispanic applicants reported natural disasters, academic, COVID-19, family crisis, and immigrant experience as the most common stressors.
The most common self-expressed coping mechanisms reported among White applicants were perseverance, empathy, and community seeking. Perseverance, resilience, and self-reflection were most reported by Asian applicants. Black or African American applicants were most likely to report perseverance, seeking community, adaptability, resilience, and advocacy as coping mechanisms. Hispanic applicants most frequently reported perseverance, resilience, seeking community, and teamwork.
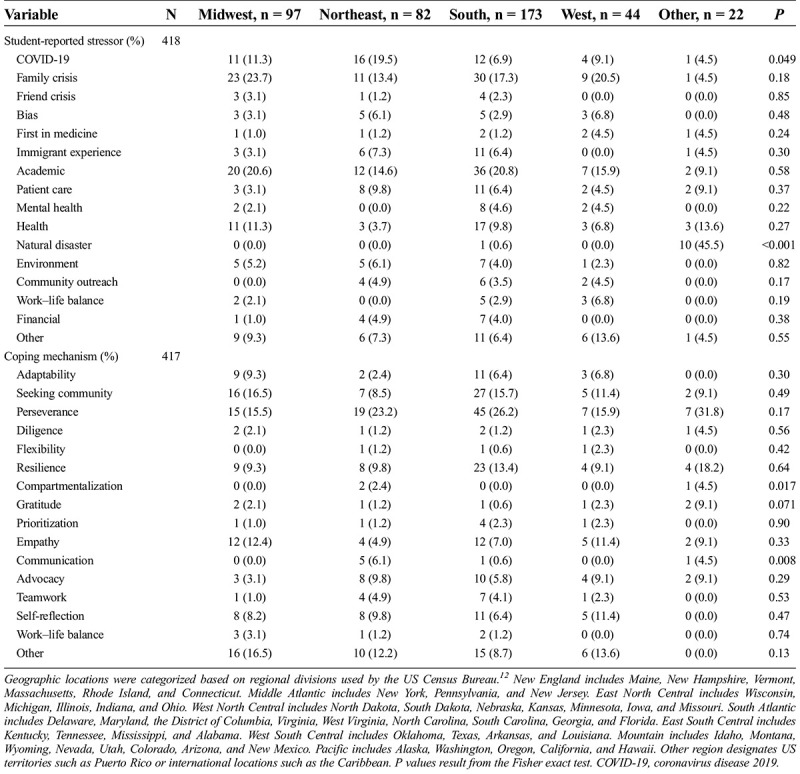
Comparing by geographic region of the applicant, the stressor of COVID-19 was observed most often for the Northeast region of the United States (P = 0.049) and the stressor of natural disaster was observed most often for the Other region (US territories, the Caribbean, and other international locations; P < 0.001). For coping mechanisms, compartmentalization was noted most often for the Other region (P = 0.017), whereas communication was seen most frequently for the Northeast region (P = 0.008; Table 4).
Table 4.
Comparison of stressors and coping mechanisms according to geographic location
Discussion
In our study of the 2020–2021 application cycle for dermatology residency positions, the most common self-reported stressors by all of the applicants collectively were academic, family crisis, and COVID-19. We hypothesized that COVID-19 would be the stressor self-reported by most applicants during this time frame; however, this was the third most common stressor after academic challenges and family crisis, respectively. To further the understanding of the top-reported stressors, general examples within each category are included:
Academic stressors reported by applicants included an inadequate score on the initial attempt at the Medical College Admission Test, failing to be accepted to medical school on first attempt, not passing medical school examinations, and failure to meet expectations on clinical rotations.
Family crisis stressors reported include cancer diagnosis, stroke diagnosis, addiction use disorders or organ failure in a family member, serving as a primary caregiver for a family member, death of a family member, suicide attempt by a family member, and mental health issues of a family member. Often, the family crisis stressors occurred while the applicant reported also studying for shelf examinations and US Medical Licensing Examination (USMLE) examinations.
COVID-19 stressors included cancellation of USMLE Step examinations by testing centers, cancellation of dermatology rotations, caring for patients infected with COVID-19, personal COVID-19 infection, social isolation, and suspension of research projects. Cancellation of dermatology rotations was particularly stressful for applicants without a dermatology program at their home institution because many away rotations at other institutions were cancelled during the 2020–2021 application cycle. Students also expressed stress with learning clinical medicine online without the ability to interact with patients during this time. Some students reported having rotation schedules and USMLE board examination schedules change multiple times.
The COVID-19 global pandemic appears to have had effects directly or indirectly based on geographic region, race/ethnicity, but not sex, as follows:
Notably, in our study, COVID-19 was more commonly reported as a stressor by applicants located in the Northeast during the 2020–2021 application cycle. The COVID-19 surge in the northeastern United States was at its height in the spring of 202013 and directly affected the educational and personal experiences of students in that region.
African American or Black applicants were more likely to cite first in medicine as a stressor. This included additional stressors of being underrepresented in medicine, gender and racial bias concerns, and lack of mentorship. A possible explanation for the high impact of this stressor among this racial/ethnic group is the recognized lack of diversity in the field of dermatology, with only 3% of dermatologists identifying as Black or African American.14 Students seeking mentorship from an academic dermatologist who shares their racial dimension of diversity may be limited and may require seeking mentors outside their own institutions. The COVID-19 pandemic further limited away rotation opportunities that may have provided particularly beneficial mentorship for this group of applicants.
We did not identify any statistically significant difference in stressor categories by sex in our supplemental application review. For coping mechanisms, there was a statistical difference in self-endorsed diligence, favoring female applicants, but otherwise no statistically different sex differences in coping strategies were identified.
Additional relevant stressor information in the 2020–2021 application cycle that was not related to COVID-19 was immigrant status and natural disasters, as follows:
Stressors related to immigrant status were reported more commonly by Black or African American and Hispanic applicants. The immigration concerns included food insecurity, lack of safe or stable housing, lack of credit history, difficulty navigating the application process for medical school, and difficulty applying for financial aid. Although COVID-19 did affect the immigration process for many people, that was not reported in our secondary applications.
Natural disaster was a common stressor for applicants from US territories, the Caribbean, and other international locations. The majority of the natural disaster stressors in our study referenced Hurricane Maria, which devasted the US territory of Puerto Rico in September 2017. Challenges reported included completing medical school while living without essential utilities or basic telephone communications, inability to charge personal electronic devices, and lack of reliable Internet. Witnessing the suffering of local communities in the aftermath of the hurricane and coping with the unknown safety of friends and family members affected also were related stressors. Environmental effects such as damaged medical school buildings and hospitals necessitated relocations for available electricity and a compressed learning schedule. The lack of Internet increased stress in the learning environment because of the inability to share presentations online and the inability to access online question banks and study resources. Previous reports also have detailed the negative effects on medical education and infrastructure affecting studying, clinical requirements, and residency application deadlines as some of the stressors described by students affected by Hurricane Maria.15
The limitations of the present study are the retrospective design and subjects being limited to the dermatology applicants in a single program during a single application cycle. This likely explains the regional bias of the cohort who are primarily from the South, which is congruent with the location of our program. Other programs nationally may identify different stressors or patterns based on location or population. Another limitation is the self-reported nature of the residency application; thus, applicants may have chosen to share only stressors they believed they had effectively overcome or addressed and could share positive coping strategies. There may be many more stressors or ineffective coping mechanisms that applicants chose not to share in their application, especially if the applicant may have perceived a potential negative effect. A final limitation noted is that the secondary application did not specify the time frame of the stressor; therefore, applicants included both stressors occurring during the COVID-19 pandemic as well as past stressors.
Future areas of study include evaluation of how the program and institutional onboarding processes, support services, leave policies, mentorship opportunities, and immigration services can best address the commonly reported stressors experienced by applicants.
Conclusions
Stressors reported by dermatology applicants in the 2020–2021 application cycle included the COVID-19 pandemic, although this was not the most commonly reported stressor. The type of stressor reported varied by the race/ethnicity of the applicant as well as the geographic location.
Footnotes
The authors did not report any financial relationships or conflicts of interest.
Contributor Information
Ashley L. Walker, Email: walker.ashley3@mayo.edu.
Mingyuan Yin, Email: yin.mingyuan@mayo.edu.
Mindy Gillis, Email: gillis.melinda@mayo.edu.
Claire Haga, Email: haga.claire@mayo.edu.
Michael Heckman, Email: heckman.michael@mayo.edu.
Nancy Dawson, Email: dawson.nancy11@mayo.edu.
Mary S. Hedges, Email: hedges.mary@mayo.edu.
References
- 1.American Foundation for Suicide Prevention . Facts about mental health and suicide among physicians. https://www.datocms-assets.com/12810/1578319045-physician-mental-health-suicide-one-pager.pdf. Accessed January 13, 2022.
- 2.Damiano RF de Oliveira IN Ezequiel OS, et al. The root of the problem: identifying major sources of stress in Brazilian medical students and developing the Medical Student Stress Factor Scale. Braz J Psychiatry 2021;43:35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill M, Goicochea S, Merlo L. In their own words: stressors facing medical students in the millennial generation. Med Educ Online 2018;23:1530558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Omar Y Paxton J Hui R, et al. Medical students’ perspective on common stressors experienced at medical school and how to address them. Braz J Psychiatry 2021;43:222–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vyas K, Stratton T, Soares N. Sources of medical student stress. Educ Health 2017;30:232–235. [DOI] [PubMed] [Google Scholar]
- 6.Matheson K Barrett T Landine J, et al. Experiences of psychological distress and sources of stress and support during medical training: a survey of medical students. Acad Psychiatry 2016;40:63–68. [DOI] [PubMed] [Google Scholar]
- 7.Nechita F Nechita D Pirlog M, et al. Stress in medical students. Rom J Morphol Embryol 2014;55:1263–1266. [PubMed] [Google Scholar]
- 8.Prayson R, Bierer S, Dannefer E. Medical student resilience strategies: a content analysis of medical students’ portfolios. Perspect Med Educ 2017;6:29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lacy FA, Chen HX, Morrell DS. Dermatology residency applications: correlation of applicant personal statement content with match result. Cutis 2020;105:83–85. [PubMed] [Google Scholar]
- 10.Samimi S Choi J Rosman IS, et al. Impact of COVID-19 on dermatology residency. Dermatol Clin 2021;39:609–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Association of Professors of Dermatology . Dermatology residency program director information regarding the interview process during the 2020-2021 application cycle. https://www.dermatologyprofessors.org/files/5_Statement%20on%20Interviews_Oct2020.pdf. Accessed January 9, 2022.
- 12.US Census Bureau . 2010Census regions and divisions of the United States. https://www.census.gov/geographies/reference-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html. Accessed March 28, 2021.
- 13.Pei S Yamana TK Kandula S, et al. Burden and characteristics of COVID-19 in the United States during 2020. Nature 2021;598:338–341. [DOI] [PubMed] [Google Scholar]
- 14.Pandya AG Alexis AF Berger TG, et al. Increasing racial and ethnic diversity in dermatology: a call to action. J Am Acad Dermatol 2016;74:584–587. [DOI] [PubMed] [Google Scholar]
- 15.Colón-Flores LG Rosario-Cruz V Gonzalez-Soto MJ, et al. Challenges and lessons learned after Hurricane Maria: learning points for the medical student community. Yale J Biol Med 2020;93:429–432. [PMC free article] [PubMed] [Google Scholar]


