Purpose of review
Examine Setmelanotide use in patients with rare genetic variants that disrupt the melanocortin pathway.
Recent findings
Between February 2017 and September 2018, 10 participants with pro-opiomelanocortin (POMC)/ proprotein convertase subtilisin/kexin type 1 (PCSK1) deficiency and 11 participants with leptin receptor (LEPR) deficiency were enrolled in open-label, phase 3 trials at 10 centers in the United States and internationally to assess the efficacy and safety of the melanocortin-4 receptor (MC4R) agonist Setmelanotide. 80% of POMC participants and 45% of LEPR participants achieved at least 10% weight loss at 1 year. Significant changes in hunger scores were seen for both cohorts as well. Setmelanotide was well tolerated with injection site reactions and hyperpigmentation being the most common adverse events reported. As a result, Setmelanotide was approved by the U.S. FDA in 2020 for chronic weight management in adult and pediatric patients ≥6 years of age with POMC, LEPR, or PCSK1 deficiency. In 2022, its approval was extended to include patients with Bardet–Biedel syndrome (BBS) after phase 3 trial data showed that, on average, Setmelanotide treatment resulted in a BMI loss of 7.9% for the 44 BBS participants.
Summary
Rare genetic variants such as POMC, LEPR, and PCSK1 deficiency disrupt MC4R pathway signaling, resulting in severe early-onset obesity, hyperphagia, and increased risk for metabolic co-morbidities. Patients with BBS also demonstrate severe early-onset obesity and hyperphagia, due in part to defective MC4R signaling. Setmelanotide has shown promising benefits in improving satiety scores and weight-related outcomes in patients with these early-life genetic obesity conditions, although longer-term studies are needed.
Keywords: hyperphagia, melanocortin receptor, pharmacotherapy, rare genetic obesity
INTRODUCTION
Obesity is a global pandemic that increasingly affects a significant number of children and adolescents. According to the World Health Organization, the percentage of children and adolescents aged 5–19 with overweight or obesity increased from 4% in 1975 to 18% in 2016 [1]. A recent cross-sectional study, which collected data from nearly 15 000 US children and adolescents who took part in the National Health and Nutritional Examination Survey (NHANES), revealed that among children and adolescents aged 2–19 years of age in the United States, the prevalence of obesity increased from 17.7% between 2011–2012 to 21.5% in the 2017–2020 survey. This increase was seen in children and adolescents from every racial and/or ethnic background. Obesity rates in males have increased from 18% to 21.4%, and in females from 17% to 21.6% over the past decade [2]. Genetic factors are estimated to account for 40–70% of an individual's predisposition for excess adiposity [3]. Although obesity is a complex condition that is multifactorial in its origins, severe early-onset obesity may be due to rare genetic variants that result in disruption of the melanocortin pathway, which is critical for energy homeostasis and appetite regulation [4,5].
In the ‘fed’ state, leptin binds to the leptin receptor (LEPR), expressed on pro-opiomelanocortin (POMC) neurons in the hypothalamus, resulting in increased expression of POMC. POMC is cleaved by proprotein convertase subtilisin/kexin type 1 (PCSK1) into α- and β-melanocyte–stimulating hormones (α- and β-MSH). These melanocortin peptides bind to and activate the melanocortin-4 receptor (MC4R) to promote satiety and increase energy expenditure, which help to control body weight. Rare variants in POMC, LEPR, or PCSK1 disrupt MC4R pathway signaling, which results in extreme hunger, or hyperphagia, and severe early-onset obesity that place patients at risk for related metabolic co-morbidities such as type 2 diabetes, dyslipidemia, and cardiovascular disease [5,6].
Until recently, lifestyle modifications and bariatric procedures were the primary options available to patients with these rare genetic obesity conditions. However, these interventions have typically shown limited success, not least because they do not curtail the hyperphagia experienced by patients. Therapies that specifically target the melanocortin pathway have been in development for over 20 years, but many of these agents either failed to show clinical efficacy and/or had undesirable adverse effect profiles [7,8].
Setmelanotide, a MC4R agonist, was approved by the U.S. Food and Drug Administration (FDA) in 2020 for chronic weight management in adult and pediatric patients at least 6 years of age with obesity due to three rare genetic conditions: POMC, LEPR, or PCSK1 deficiency [9▪]. The use of Setmelanotide for other rare genetic disorders associated with obesity such as Bardet–Biedl syndrome (BBS), Alström syndrome, POMC and other MC4R pathway heterozygous deficiency obesity, and POMC epigenetic disorders, continues to be studied. In June 2022, the indication for Setmelanotide was extended by the FDA to include patients with BBS. These developments have ushered in a new era of targeted therapy for select early-life genetic obesity syndromes.
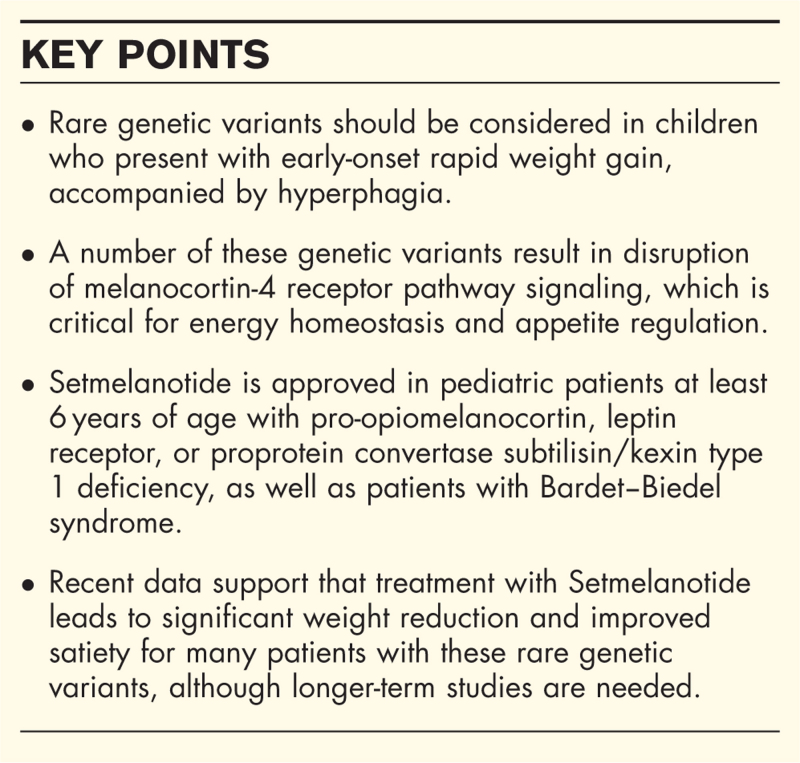
Box 1.
no caption available
Genetic variants of obesity
There are a number of rare genetic variants that result in disruption of the melanocortin pathway, which is essential for regulation of appetite and body weight. Proopiomelanocortin (POMC) deficiency is an autosomal recessive disorder that is characterized by early-onset obesity and hyperphagia. It may also lead to adrenal crisis due to adrenocorticotropic hormone (ACTH) deficiency with resultant hypopigmentation and inadequate cortisol production [10]. Leptin receptor (LEPR) mutations have been identified in up to 3% of individuals with severe, early-onset obesity; these patients present with extreme hyperphagia, delayed puberty secondary to hypogonadotropic hypogonadism, and frequent infections due to T-cell abnormalities [10,11]. Loss-of-function mutations in the PCSK1 gene, which encodes prohormone convertase 1/3 (PC1/3), result in early-onset obesity and hyperphagia [12]. PCSK1 deficiency is a very rare autosomal-recessive disorder that, in addition to obesity and hyperphagia, may also lead to other endocrinopathies such as hypogonadotropic hypogonadism, central hypothyroidism, and adrenal insufficiency.
Setmelanotide development and mechanism of action
Setmelanotide was developed as a ligand of the MC4R. Setmelanotide is an eight amino-acid peptide that preferentially binds to and activates MC4 receptors in the paraventricular nucleus of the hypothalamus and in the lateral hypothalamic area, both of which are involved in appetite regulation [13▪]. In addition to its appetite suppressive effects, Setmelanotide has also been shown to increase resting energy expenditure in both animals and humans with obesity. Unlike earlier generation MC4R agonists, individuals taking Setmelanotide have not exhibited concerning elevations in heart rate or blood pressure that led to the termination of first-generation MC4R agonist development [14,15].
Early use of Setmelanotide for melanocortin-4 receptor deficiency
Collet et al.[16] examined the use of Setmelanotide in individuals with MC4R deficiency in a 28-day randomized, double blind placebo-controlled phase 1b clinical trial. Setmelanotide led to similar amounts of weight lost in individuals heterozygous for complete or partial loss-of-function mutations in MC4R, compared to placebo. This early study also highlighted that Setmelanotide appeared to be more efficacious for patients with MC4R pathway upstream defects, such as POMC, in comparison to MC4R deficient patients or controls. As such, one conclusion reached from this study was that there was unlikely to be an advantage for Setmelanotide usage in heterozygous individuals. Subsequent development of Setmelanotide focused on identifying individuals homozygous for genetic defects that could prove responsive to Setmelanotide therapy [17].
Clinical trial results for Setmelanotide in patients with rare genetic variants
Between February 2017 and September 2018, single-arm, open-label multicenter phase 3 trials were conducted at 10 different centers, both in the United States and internationally, to evaluate the efficacy and safety of Setmelanotide therapy [18▪▪]. Recruited patients with POMC, PCSK1, or LEPR deficiency aged 6 years or older received open-label Setmelanotide for 12 weeks. Those who demonstrated at least 5 kg of weight loss compared to baseline then entered an 8-week placebo-controlled withdrawal sequence, which was followed by 32 weeks of open-label Setmelanotide treatment. The primary endpoint of these trials, which was evaluated for all individuals who received at least one dose of medication and had baseline assessments, was the percentage of participants who sustained at least 10% weight loss compared to their baseline at 1 year. Change in hunger scores was also examined.
Ten participants enrolled in the POMC/PCSK1 trial with mean percentage change in the most hunger score of −27·1% (n = 7; 90% confidence interval [CI] −40.6 to −15.0; P = 0.0005). Eight participants (80%) achieved at least 10% weight loss at approximately 1 year with mean weight loss of –25.6%. Eleven participants were enrolled in the LEPR trial. Five participants (45%) were found to achieve at least 10% weight loss at approximately 1 year with mean percentage change in the most hunger score of −43.7% (n = 7; −54.8 to −29.1; P < 0.0001). Of note, five participants achieved 15% or greater weight loss with two participants reaching 20% or greater weight loss [18▪▪].
There was only one enrolled patient with PCSK1 deficiency in the POMC/PCSK1 trial; this individual's weight was greater than the 95th percentile at the time of study recruitment [19]. This patient lost 7.1% of their body weight during the initial 12-week treatment period. Weight regain was demonstrated upon Setmelanotide withdrawal. Complicating the clinical picture, this individual was also started on risperidone, which is commonly associated with weight gain, during the withdrawal phase. Risperidone was stopped by week 48 of the trial. After approximately one year of Setmelanotide treatment, this patient lost 2.4% of their body weight compared to baseline.
In addition to investigating the effects of Setmelanotide on body weight and hunger, researchers also examined quality of life (QOL) and depression scores of participants using the disease-specific Impact of Weight on Quality of Life-Lite (IWQOL-Lite) self-report measure for patients ≥18 years of age, the age-appropriate Pediatric Quality of Life Inventory (PedsQL) for those under 18 years of age, and the Patient Health Questionnaire-9 (PHQ-9). Results from these assessments showed that at baseline, both adults and children with POMC and LEPR deficiency reported impaired QOL. For pediatric participants with POMC and LEPR deficiency, the PedsQL scores were lower than a comparative population without obesity or when compared to scores from children and adolescents with other chronic conditions. Three out of five participants reported improvements in PedsQL scores at week 52 that were considered clinically meaningful. Of these 5 children and adolescents, 3 also reported improvements in physical functioning scores and 4 reported improvements in psychosocial health scores, which are secondary analyses of the PedsQL [20].
Adverse reactions in pro-opiomelanocortin/leptin receptor trials
Setmelanotide was generally well tolerated by the majority of trial participants for whom there is published data. Injection site reactions and hyperpigmentation were the most commonly reported adverse reactions, experienced by all ten participants in the POMC trial. Additionally, five participants reported nausea and three others experienced emesis. Injection site reactions were reported for all 11 participants in the LEPR trial. Hyperpigmentation was reported by five individuals and nausea occurred for four patients with LEPR deficiency [18▪▪].
Setmelanotide use in patients with Bardet−Biedel syndrome
BBS is a rare ciliopathy characterized by a number of clinical features including retinal cone-rod dystrophy, polydactyly, cognitive impairment, renal disease, and early-onset obesity with hyperphagia [21]. Although the pathophysiology of BBS is incompletely understood, previous research has elucidated that the obesity and hyperphagia is likely due in part to impaired MC4R pathway activity, suggesting that a MC4R agonist could be of potential therapeutic benefit [22].
Results of a phase 2 trial published in 2020 examined the effects of Setmelanotide on weight outcomes in individuals with BBS aged 12 years or older [13▪]. The primary outcome measure was percent change in body weight after 3 months of treatment at therapeutic dosing. A number of exploratory outcomes were also examined, including hunger scores. Participants who had achieved weight reduction of at least 5 kg or greater compared to baseline were enrolled in a 52-week treatment extension phase to further evaluate the efficacy and safety of Setmelanotide at 6 and 12 months. Eight participants completed the 3-month treatment phase and seven completed the 52-week extension phase. Although this trial only included a small number of participants, there was a significant mean percent change in body weight at 3 months, which continued at 6 and 12 months (% change in body weight at 12 months was −16.3% [90% CI −19.9% to −12.8%]; n = 7; P < 0.0001). Hunger scores among participants also showed improvement at all time points. Similar to results from the POMC and LEPR trials, the most common adverse events noted for participants with BBS were injection site reactions and hyperpigmentation.
A randomized, placebo-controlled, double-blind multicenter phase 3 trial to evaluate the efficacy and safety of Setmelanotide for treatment of obesity and hyperphagia in individuals ≥6 years of age with BBS or Alström syndrome completed enrollment of its primary cohort in 2019 [23]. Participants initially were randomized 1:1 to receive treatment or placebo for a 14-week period, followed by 52 weeks of open-label treatment with Setmelanotide. The primary outcome measure was the proportion of participants aged 12 years and older who showed ≥10% reduction in body weight compared to baseline after 52 weeks of treatment. A key secondary endpoint was the proportion of participants with ≥ 25% improvement in hunger scores after the full treatment period. In June 2022, the U.S. FDA extended use of Setmelanotide for chronic weight management in adult and pediatric patients ≥6 years of age with BBS [24]. This approval was granted due to Phase 3 trial data which showed benefit in both weight-related outcomes, as well as hunger reduction, in patients with BBS [25▪▪]. Thirty-two patients with BBS enrolled as part of the initial cohort with 32.3% of patients with BBS aged 12 years or older achieving at least a 10% reduction in body weight after 52 weeks of Setmelanotide therapy compared to baseline, with a mean percentage change in body weight of –5·2% (SD 7·9; p = 0·0005). There was a mean percentage change in maximal hunger score of –30·5% in 57.1% of BBS patients aged 12 years or older after 52 weeks of Setmelanotide therapy (–45·7% to –15·2%; p = 0·0004) [25▪▪].
Setmelanotide approval for rare genetic variants and future directions
Setmelanotide was approved in 2020 for use in children aged 6 years or older who have POMC, PCSK1, or LEPR deficiency in whom genetic testing has confirmed variants in POMC, PCSK1, or LEPR genes that are considered to be pathogenic, those likely to be pathogenic, or those of uncertain significance. Additionally, in 2022, the FDA granted supplemental approval of Setmelanotide for patients with BBS, making it the first medication specifically indicated for chronic weight management in patients with this rare condition. Setmelanotide continues to be studied in ongoing clinical trials for those with other alterations in the MC4R pathway, as well as those with deletions on chromosome 16p11.2. The goal of these trials has been to investigate the efficacy and safety of Setmelanotide for individuals with various heterozygous genetic mutations in the MC4R pathway [26] (https://clinicaltrials.gov/ct2/show/NCT04963231).
CONCLUSION
Rare genetic variants such as POMC, LEPR, and PCSK1 deficiency disrupt MC4R pathway signaling, resulting in severe early-onset obesity, pronounced hyperphagia, and increased risk for metabolic co-morbidities. Patients with BBS also demonstrate severe early-onset obesity and hyperphagia, thought to be due in part to defective MC4R signaling. These early-life genetic obesity conditions place a tremendous burden on patients and caregivers with significant impact on QOL and long-term health outcomes. Setmelanotide, a MC4R agonist, has been shown in a limited number of trials to result in short-term weight reduction and improved satiation for patients with these rare genetic variants. Continued development of targeted therapies, such as Setmelanotide, offer promising benefit for improving appetite regulation and weight-related outcomes in patients with early-life genetic obesity conditions, but further research is needed.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1. Organization WH. Fact sheets: obesity and overweight. 2020. Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. [Google Scholar]
- 2.Hu K, Staiano AE. Trends in obesity prevalence among children and adolescents aged 2 to 19 years in the US from 2011 to 2020. JAMA Pediatr 2022; 176:1037–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ranadive SA, Vaisse C. Lessons from extreme human obesity: monogenic disorders. Endocrinol Metab Clin North Am 2008; 37:733–751. x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huvenne H, Dubern B, Clement K, Poitou C. Rare genetic forms of obesity: clinical approach and current treatments in 2016. Obes Facts 2016; 9:158–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yazdi FT, Clee SM, Meyre D. Obesity genetics in mouse and human: back and forth, and back again. PeerJ 2015; 3:e856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huszar D, Lynch CA, Fairchild-Huntress V, et al. Targeted disruption of the melanocortin-4 receptor results in obesity in mice. Cell 1997; 88:131–141. [DOI] [PubMed] [Google Scholar]
- 7.Yeo GSH, Chao DHM, Siegert AM, et al. The melanocortin pathway and energy homeostasis: from discovery to obesity therapy. Mol Metab 2021; 48:101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fani L, Bak S, Delhanty P, et al. The melanocortin-4 receptor as target for obesity treatment: a systematic review of emerging pharmacological therapeutic options. Int J Obes (Lond) 2014; 38:163–169. [DOI] [PubMed] [Google Scholar]
- 9▪.Markham A. Setmelanotide: first approval. Drugs 2021; 81:397–403. [DOI] [PubMed] [Google Scholar]; This article highlights the development of Setmelanotide and discussed its approval for chronic weight management in patients with POMC, PCSK1, and LEPR deficiency. It also discusses other genetic obesity conditions where Setmelanotide use is being studied.
- 10. Farooqi IS, O’Rahilly S. The Genetics of Obesity in Humans. [Updated 2017 Dec 23]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279064/UMFCXA. [Google Scholar]
- 11.Mason K, Page L, Balikcioglu PG. Screening for hormonal, monogenic, and syndromic disorders in obese infants and children. Pediatr Ann 2014; 43 (9):e218–e224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jackson RS, Creemers JW, Ohagi S, et al. Obesity and impaired prohormone processing associated with mutations in the human prohormone convertase 1 gene. Nat Genet 1997; 16:303–306. [DOI] [PubMed] [Google Scholar]
- 13▪.Haws R, Brady S, Davis E, et al. Effect of setmelanotide, a melanocortin-4 receptor agonist, on obesity in Bardet–Biedl syndrome. Diabetes Obes Metab 2020; 22:2133–2140. [DOI] [PMC free article] [PubMed] [Google Scholar]; This phase 2 trial evaluated the efficacy and safety of Setmelanotide treatment in patients with BBS. 8 individuals completed the 3-month treatment period and 7 completed the 52-week extension phase. Mean percentage change in body weight was significant at −16.3% at 12 months and hunger scores also showed improvement for participants. No severe treatment-related adverse events were reported.
- 14.Kievit P, Halem H, Marks DL, et al. Chronic treatment with a melanocortin-4 receptor agonist causes weight loss, reduces insulin resistance, and improves cardiovascular function in diet-induced obese rhesus macaques. Diabetes 2013; 62:490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen KY, Muniyappa R, Abel BS, et al. RM-493, a melanocortin-4 receptor (MC4R) agonist, increases resting energy expenditure in obese individuals. J Clin Endocrinol Metab 2015; 100:1639–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Collet TH, Dubern B, Mokrosinski J, et al. Evaluation of a melanocortin-4 receptor (MC4R) agonist (Setmelanotide) in MC4R deficiency. Mol Metab 2017; 6:1321–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryan DH. Next generation antiobesity medications: setmelanotide, semaglutide, tirzepatide and bimagrumab: what do they mean for clinical practice? J Obes Metab Syndr 2021; 30:196–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18▪▪.Clement K, van den Akker E, Argente J, et al. Efficacy and safety of setmelanotide, an MC4R agonist, in individuals with severe obesity due to LEPR or POMC deficiency: single-arm, open-label, multicentre, phase 3 trials. Lancet Diabetes Endocrinol 2020; 8:960–970. [DOI] [PubMed] [Google Scholar]; These authors report on the results of phase 3 trials, which showed at least 10% weight loss after one year of Setmelanotide treatment in 8 of 10 patients with POMC deficiency and 5 of 11 patients with LEPR deficiency. This is an important article because not only did the trials demonstrate efficacy of Setmelanotide, the results also highlighted no serious treatment-related adverse events.
- 19.Wabitsch M, Farooqi S, Fluck CE, et al. Natural history of obesity due to POMC, PCSK1, and LEPR deficiency and the impact of Setmelanotide. J Endocr Soc 2022; 6:bvac057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuhnen P, Wabitsch M, von Schnurbein J, et al. Quality of life outcomes in two phase 3 trials of setmelanotide in patients with obesity due to LEPR or POMC deficiency. Orphanet J Rare Dis 2022; 17:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chung WK. An overview of mongenic and syndromic obesities in humans. Pediatr Blood Cancer 2012; 58:122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feuillan PP, Ng D, Han JC, et al. Patients with Bardet-Biedl syndrome have hyperleptinemia suggestive of leptin resistance. J Clin Endocrinol Metab 2011; 96:E528–E535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haws RM, Gordon G, Han JC, et al. The efficacy and safety of setmelanotide in individuals with Bardet-Biedl syndrome or Alstrom syndrome: phase 3 trial design. Contemp Clin Trials Commun 2021; 22:100780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. U.S. Food and Drug Administration. (2022, June 16). FDA approves treatment for weight management in patients with Bardet-Biedl Syndrome aged 6 or older [Press release]. https://www.fda.gov/drugs/news-events-human-drugs/fda-approves-treatment-weight-management-patients-bardet-biedl-syndrome-aged-6-or-older. [Google Scholar]
- 25▪▪.Haqq AM, Chung WK, Dollfus H, et al. Efficacy and safety of setmelanotide, a melanocortin-4 receptor agonist, in patients with Bardet-Biedl syndrome and Alström syndrome: a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial with an open-label period. Lancet Diabetes Endocrinol 2022; 10:859–868. [DOI] [PMC free article] [PubMed] [Google Scholar]; These authors report on the results of a phase 3 trial evaluating use of Setmelanotide in patients with Bardet-Biedl syndrome and Alström syndrome. Setmelanotide use was associated with greater weight loss and reduction in hunger scores after 14 weeks of treatment, with further reductions seen after 52 weeks in patients with BBS. Tolerability was similar to results reported in previous trials.
- 26.Cuda S, Censani M. Progress in pediatric obesity: new and advanced therapies. Curr Opin Pediatr 2022; 34:407–413. [DOI] [PubMed] [Google Scholar]