Abstract
Objectives:
To compare the cone-beam computed tomography (CBCT) image quality and effective dose between low-dose scanning and standard manufacturer-recommended protocols among different CBCT units.
Methods:
Three human-equivalent phantoms were scanned using the ultra-low-dose (ULD), low dose (LD), and standard dose (STD) modes of ProMax 3D Mid (Planmeca Oy, Helsinki, Finland) and Orthophos SL (Sirona, Bensheim, German) for the CBCT images. The quality of the dental anatomical images was assessed by four experienced oral and maxillofacial radiologists using a 5-point Likert scale. OnDemand3D (Cybermed Co., Seoul, Korea) was used as the third-party software for viewing. The percentage of absolute agreement was calculated to determine intra- and interrater agreements among the observers. The effective doses for all CBCT scanning protocols were also calculated.
Results:
The STD protocol yielded a higher image quality than did the ULD and LD protocols in both ProMax 3D Mid and Orthophos SL. The ULD and LD protocols demonstrated an “acceptable-to-good” sense of visual perception of the CBCT images. The visibility scores significantly differed between the ULD and LD and the STD protocols in ProMax 3D Mid and Orthophos SL, except for the 120-kVp setting in ProMax 3D Mid. The average intra- and interrater agreement scores ranged from 0.63 to 0.89 and from 0.44 to 0.76, respectively. The ULD and LD protocols reduced the radiation dose sixfold compared with the STD protocol.
Conclusions:
High-tube-voltage protocols could remarkably reduce the imaging dose without degrading the image quality. Specifically, ULD and LD CBCT protocols may be adopted as routine practice for diagnosis and treatment planning.
Keywords: Low dose, cone-beam computed tomography, image quality, effective dose
Introduction
Cone-beam computed tomography (CBCT) has become a standard imaging method for the dentomaxillofacial area in recent years ago. It has less scanning time, a lower cost, a lower effective dose, and a higher image resolution than multislice computed tomography (MSCT). 1,2 The evolution of imaging technology has inevitably required the use of an increased radiation dose, which was why the “as low as diagnostically acceptable” (ALADA) principle was proposed at the National Council on Radiation Protection and Measurements in 2014. 3 This concept emphasizes the importance of dose optimization using low-dose strategies to obtain “diagnostically acceptable” rather than “pretty” images. Still, a wide range of CBCT application in dentomaxillofacial radiology is beyond the diagnostic task. Specific demands for CBCT application are also needed to determine appropriate surgical strategies or simulate complicated treatment plans. This is where the “as low as diagnostically acceptable being indication-oriented and patient-specific” (ALADAIP) principle presented by the DIMITRA project in 2018 plays a role in CBCT prescription for many purposes in dentistry. This principle encourages a clinician to focus on more personalized dose optimization for a particular diagnosis, pre-surgical treatment planning, model making, and three-dimensional (3D) printing. 4 Hence, recent CBCT units with a low-dose function have been gradually manufactured and are commercially available from several manufacturers to fit these particular needs. 5
The effective dose for CBCT mainly depends on the field of view (FOV) size. Based on FOV selection, current CBCT systems are classified into three categories: (1) small FOV (height: ≤5 cm); (2) medium FOV (height: 5.1–10 cm); and (3) large FOV (height: >10 cm). In 2007, the International Commission on Radiological Protection 6 reported a wide range of effective doses according to the FOV size: 9.7–197 µSv (median: 28.5 µSv) for a small FOV, 3.9–674 µSv (median: 69.9 µSv) for a medium FOV, and 8.8–1073 µSv (median: 114 µSv) for a large FOV. The effective dose for CBCT also depends on the exposure parameter settings and differences in the image acquisition procedures. Generally, the effective dose is somewhat high.
Several CBCT dose reduction strategies have been proposed, including the use of a limited FOV, 4 reduction in exposure factors (tube voltage, tube current, and exposure time), 7,8 use of partial rotation, 9,10 reduction in the number of basis projection, 11 and use of a larger voxel size. 4 In a clinical situation, mAs reduction is preferred to kVp reduction for low-dose CBCT protocols, while a higher kVp setting (e.g. more than 90 kVp) is recommended, as it yields a higher contrast-to-noise ratio (CNR). 12 Some current CBCT machines introduce a “high-power tube” that can be operated up to 120 kVp and provide radiographic images with less streak artifacts, resulting in an improved image quality. The size of the FOV is another factor affecting the sense of visual perception of the image quality. Minimizing the FOV to an area of interest reduces resultant scattered radiation and decreases image noise. 13,14 CBCT images obtained from a 10 × 16 cm FOV setting previously showed some graininess (noise) that interfered with the visibility of a vertical root fracture. This was possibly attributed to scattered radiation from using a large FOV. 15 Meanwhile, when the number of projection images decreases, the resultant images are less clear as the CBCT images become noisier and present more artifacts. 11 As with the number of projections, a partial rotation during CBCT provides resultant fewer basis projections, producing an image with greater noise and more reconstruction interpolation artifacts. 14 A rotation angle of less than 360° also indicates a limited angle tomography, which induces a sampling problem (undersampling) for the image reconstruction process, as an object is not sampled from all sides. 16
Nevertheless, when low-dose CBCT settings are applied, the resultant image quality may either be degraded or not even be affected. 9,17 This issue should be taken into account in the diagnostic process. In recent years, in vitro studies demonstrated the effect of reduction in the rotation angle, exposure time, and tube current on the diagnosis during endodontic tasks; no significant decrease in the diagnostic quality was found for the detection of either horizontal or vertical root fracture or external inflammatory root in CBCT images. 15,17–19 For larger anatomy and pathology, low-dose CBCT protocols yielded no effect or even only slightly affected the diagnosis, treatment plan, treatment outcome, and dimensional and measurement accuracies for orofacial cleft, periapical lesion, cystic lesion, tooth autotransplantation, 4 maxillary canine impaction, 7 dental implantation, 8 3D cephalometric analysis, 20 dimensional buccal cortical plate evaluation, 21 root angulation assessment, 9 and degenerative temporomandibular joint change evaluation. 10 These investigations mainly reduced the rotation angle, exposure time, and mA to achieve a lower dose, but seldom by reduction in FOV, kVp, and voxel size. Despite compromised image quality, CBCT images were still either acceptable or reliable for the mentioned indications.
Although many research studies have investigated the relevance of low-dose CBCT in dentistry, most of them used only one CBCT machine and focused on the image quality, effective dose, and specific dentistry tasks. There is paucity in research comparing the radiation dose and image quality among different low-dose CBCT machines. Thus, the aim of this study was to compare the CBCT image quality and effective dose between low-dose scanning and reference standard manufacturer-recommended protocols using two different CBCT units.
Methods and materials
CBCT scanning protocols
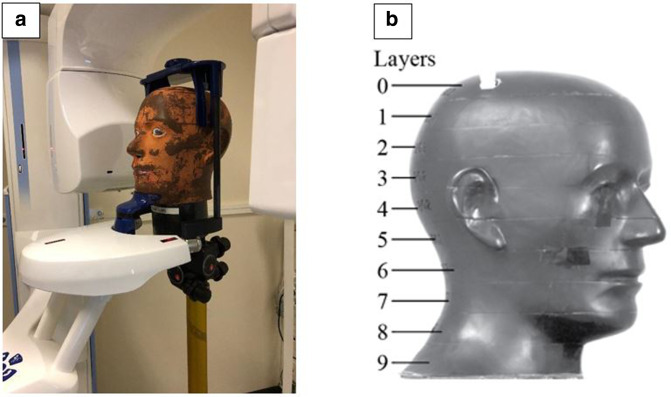
Three human-equivalent phantoms with 0.2 × 0.2 mm2 MOSFET-based sensors provided by Planmeca (Planmeca Oy, Helsinki, Finland) were used to evaluate the image quality (Figure 1a). CBCT images of the anterior maxilla of all phantoms were obtained using ProMax 3D Mid (Planmeca Oy) and Orthophos SL (Sirona, Bensheim, Germany). All scans were performed at the Department of Radiology, Tampere University Hospital, Tampere, Finland, wherein there were six protocols of CBCT scanning. For ProMax 3D Mid, two reference standard dose (STD) exposure protocols [(1) 90 kVp, 5.6 mA, and 3 s; (2) 120 kVp, 4 mA, and 8 s] and two ultra-low-dose (ULD) exposure protocols [(1) 90 kVp, 2 mA, and 3 s; (2) 120 kVp, 2 mA, and 3 s] were used. The other parameters for ProMax 3D Mid were kept constant at an FOV of 4 × 5 cm2, a voxel size of 0.2 × 0.2 × 0.2 mm3, and a rotation angle of 210°. For Orthophos SL, the reference STD exposure protocol was 85 kVp, 10 mA, and 5 s, while the low dose (LD) exposure protocol 85 kVp, 7 mA, and 2.1 s. The other parameters for Orthophos SL were kept constant at an FOV of 5 × 5.5 cm2, a voxel size of 0.16 × 0.16 × 0.16 mm3, and a rotation angle of 210°. All scanning parameters and technical specifications are outlined in Table 1. A total of 18 CBCT scans were investigated in this study. Examples of the CBCT images for evaluation of the subjective image quality are shown in Figure 2a–f.
Figure 1.
(a) Anthropomorphic RANDO RAN 102 phantom head setting for cone-beam computed tomography scanning; (b) an anthropomorphic RANDO RAN 102 phantom with 10 2.5-cm-thick layers (0–9).
Table 1.
Technical specifications and exposure parameters of ProMax 3D Mid and Orthophos SL
| Parameters | ProMax 3D Mid | Orthophos SL | ||||
|---|---|---|---|---|---|---|
| ULD (90 kVp) |
STD (90 kVp) |
ULD (120 kVp) |
STD (120 kVp) |
LD (85 kVp) |
STD (85 kVp) |
|
| Tube voltage (kVp) | 90 | 90 | 120 | 120 | 85 | 85 |
| Tube current (mA) | 2 | 5.6 | 2 | 4 | 7 | 10 |
| Exposure time (s) | 3 | 6 | 3 | 8 | 2.1 | 5 |
| Exposure time product (mAs) | 6 | 33.6 | 6 | 32 | 14.7 | 50 |
| Field of view (cm2) | 4 × 5 | 5 × 5.5 | ||||
| Voxel size (mm3) | 0.2 × 0.2 × 0.2 | 0.16 × 0.16 × 0.16 | ||||
| Scan angle | 210 degree | 210 degree | ||||
| Focal spot size (mm2) | 0.5 × 0.5 | 0.5 × 0.5 | ||||
| Radiation source | Pulsed | Pulsed | ||||
| Number of projections | 251 | 381 | 384 | |||
| Image detector | Flat panel | Flat panel | ||||
| Effective dose (µSv) | 2.8 | 16.0 | 5.8 | 30.9 | 5 | 31 |
LD, low dose; SD, standard dose; ULD, ultra-low-dose.
Figure 2.
Cone-beam computed tomography images used for evaluation taken at the following settings: (a) 90 kVp and ULD for ProMax 3D MID; (b) 90 kVp and STD for ProMax 3D MID; (c) 120 kVp and ULD for ProMax 3D MID; (d) 120 kVp and STD for ProMax 3D MID; (e) 85 kVp and LD Orthophos SL; and (f) 85 kVp and STD for Orthophos SL. LD, low dose; STD, standard dose; ULD, ultra-low-dose.
Effective dose assessment
The effective dose was assessed on an anthropomorphic phantom with cervical vertebrae (RANDO RAN102 male head phantom; Radiation Analogue Dosimetry System; The Phantom Laboratory, Salem, NY). The phantom comprised a natural human skeleton casted inside a soft-tissue simulation material to match the attenuation and scattering conditions of the bones, soft tissues, and airways of the human head. It was composed of ten 2.5-cm-thick layers (0–9) (Figure 1b) with dosimeters inserted in the head and neck organs, according to a protocol described by Ludlow et al, 1 for effective dose calculation in the region. The position of the dosimeters is presented in Table 2. The measurements were conducted according to the methods described by Koivisto et al using the TN-RD-70-W20 MOSFET device comprising 1 TN-RD-38 wireless Bluetooth transceiver, 4 TN-RD-16 reader modules, 20 reinforced high-sensitivity TN-1002RD-H dosimeters, and 1 TH-RD-75M software (Best Medical Canada, Ottawa, ON). Prior to the measurements, the MOSFET dosimeters were calibrated using a RADCAL 1015 dosimeter equipped with a RADCAL 10 × 5–6 ionization chamber (Radcal Corporation, Monrovia, CA). 22,23
Table 2.
Locations of the MOSFET dosimeters in RANDO phantom
| Tissue | Phantom location | Phantom layer | Dosimeter number |
|---|---|---|---|
| Bone marrow | Calvarium anterior | 2 | 1 |
| Brain | Mid brain | 3 | 2 |
| Brain | Pituitary fossa | 3 | 3 |
| Eyes | Right orbit | 4 | 4 |
| Eyes | Right lens | 4 | 5 |
| Skin | Right cheek | 6 | 6 |
| Bone marrow | Right ramus | 7 | 7 |
| Bone marrow | Left ramus | 7 | 8 |
| Salivary gland | Right parotid | 6 | 9 |
| Salivary gland | Left parotid | 6 | 10 |
| Bone marrow | Center C-spine | 7 | 11 |
| Skin | Left back neck | 8 | 12 |
| Bone marrow | Right mandible body | 7 | 13 |
| Bone marrow | Left mandible body | 7 | 14 |
| Salivary gland | Right submandibular gland | 8 | 15 |
| Salivary gland | Left submandibular gland | 8 | 16 |
| Salivary gland | Center sublingual gland | 8 | 17 |
| Thyroid | Midline thyroid | 9 | 18 |
| Thyroid | Thyroid surface | 9 | 19 |
| Esophagus | Pharyngeal–esophageal space | 9 | 20 |
The equivalent dose in tissue T (HT) was calculated using the following equation 24,25 :
where the radiation weighing factor WR = 1 (Sv/Gy) for x-rays, fi the fraction irradiated in tissue T in layer i, and DTi being the average absorbed dose of tissue T in layer i. Summation was performed for all phantom layers.
The effective dose (E) was obtained from the measured organ doses using the revised guidelines given by the ICRP 103. 6 The effective dose was calculated using the following equation:
where WT is the weighting factor of tissue T. The ICRP 103 weighting factors of tissue and the fraction of irradiation used in the calculations are shown in Table 3.
Table 3.
ICRP 103 (2007) tissue weighting factors (WT), fraction irradiated (fi ), and dosimeter number used to calculate the equivalent dose and the effective dose
| Tissue | WT | fi | Dosimeter number |
|---|---|---|---|
| Thyroid | 0.04 | 1 | 18, 19 |
| Esophagus | 0.04 | 0.1 | 20 |
| Brain | 0.01 | 1 | 2, 3 |
| Skin | 0.01 | 0.05 | 5, 6, 12 |
| Salivary glands | 0.01 | 1 | |
| Parotid | 9, 10 | ||
| Submandibular | 15, 16 | ||
| Sublingual | 17 | ||
| Bone marrow | 0.12 | 0.165 | |
| Mandible | 0.013 | 7, 8, 13, 14 | |
| Calvaria | 0.118 | 1, 4 | |
| Cervical spine | 0.034 | 15 | |
| Bone surfacea | 0.01 | 0.165 | |
| Mandible | 0.013 | 7, 8, 13, 14 | |
| Calvaria | 0.118 | 1, 4 | |
| Cervical spine | 0.034 | 15 | |
| Remainder | 0.12 |
Bone surface dose = bone marrow dose x 3.23.
Image quality assessment
The image quality was assessed by four oral and maxillofacial radiologists with work experience ranging from 13 to 36 years in dentistry. All observers assessed the CBCT image quality in terms of visibility of the dental anatomical structures using a 5-point Likert scale: 0, non-visibility; 1, poor visibility; 2, acceptable visibility; 3, good visibility; and 4, excellent visibility of anatomical structures. Each observer assessed the image quality twice, with at least a 1 week interval between each evaluation session. The seven following small fine anatomical structures in the maxilla that are commonly related to routine dental works were evaluated: periodontal ligament (PDL) space of tooth numbers 12 and 21; dentino–enamel junction of tooth numbers 12 and 21; cemento–enamel junction of tooth numbers 12 and 21; nasal septum; anterior nasal spine; cortical border of the incisive canal; and root canal of tooth number 13. To obtain a comparable image quality, we viewed the multiplanar reconstructed CBCT images in the axial, coronal, and sagittal planes using OnDemand3D (Cybermed Co., Seoul, Korea) at a 1 mm slice thickness (Figure 2).
The observer-specific calibration sessions for the CBCT image quality assessment were performed prior to the study. All observers could adjust the contrast and brightness when necessary during radiographic evaluation in the clinical settings. The observers scored their level of confidence on the visibility of each anatomical structure in the axial, coronal, and sagittal planes and provided only one overall image quality score for each anatomical structure. A 5-point score level was used in this study. The lowest score indicated the lowest confidence level, while the highest score indicated the highest confidence level.
The subjective image quality was assessed in two separate institutes in Finland and Thailand. The DICOM monitors of these institutes are different. Thus, to ensure equal image quality in both settings, we used an HP EliteBook 850 G3 Zbook with a monitor size of 17 in and a pixel resolution of 1920 × 1080. The monitor quality test was created using methods published by the Radiological Department of the University of Oulu, Finland. These methods are officially accepted in Finland for clinical use as follows:
Gray shades: https://www.oulu.fi/radiologia/monitorit/hsavy.html
Statistical analysis
The median scores of the visibility of all anatomical structures were evaluated for all CBCT scanning modalities. The percentage of absolute agreement was used to determine inter- and intrarater agreements among the observers, which was calculated from the number of times the raters agreed on a rating divided by the total number of rating. The inter- and intrarater agreement scores ranged from 0 to 1. The agreement level was interpreted as follows: <0.50, poor; between 0.50 and 0.75, fair; between 0.75 and 0.90, good; and above 0.90, excellent agreement. 26 A pair comparison of the median scores was conducted using the Wilcoxon signed-rank test and a multiple comparison (more than two groups) using the Friedman test, with the level of significance set at 0.05.
Results
The median scores for all anatomical structures are presented in Table 4. For the overall anatomical structures, most median scores were higher in the STD protocol than in the ULD and LD protocols in both ProMax 3D Mid and Orthophos SL. This indicates that STD protocols yield a higher image quality than do ULD and LD protocols. In ProMax 3D Mid at the 90-kVp setting, the visibility scores of the anatomical structures significantly differed (p = 0.034) between the ULD and STD protocols. Meanwhile, the scores did not significantly differ (p = 0.317) between the ULD and STD protocols in ProMax 3D Mid at the 120-kVp setting.
Table 4.
Median visibility scores of all anatomical structures of the three skulls seen from the CBCT images produced by six scanning protocols
| Anatomical structures | ProMax 3D Mid | Orthophos SL | ||||
|---|---|---|---|---|---|---|
| ULD (90 kVp) |
STD (90 kVp) |
ULD (120 kVp) |
STD (120 kVp) |
LD (85 kVp) |
STD (85 kVp) |
|
| Periodontal ligament space | 2 | 3 | 2 | 3 | 1 | 3 |
| Dentino–enamel junction | 3 | 3 | 3 | 3 | 2 | 3 |
| Cemento–enamel junction | 3 | 3 | 3 | 3 | 2 | 3 |
| Nasal septum | 2 | 3 | 3 | 3 | 2 | 3 |
| Anterior nasal spine | 2 | 3 | 3 | 3 | 2 | 2 |
| Cortical border of the incisive canal | 3 | 4 | 4 | 4 | 2.5 | 3 |
| Root canal | 3 | 3.5 | 3 | 3 | 2 | 3 |
CBCT, cone-beam computed tomography; LD, low dose; SD, standard dose; ULD, ultra-low-dose.
Score: 0 = not seen; 1 = poor; 2 = acceptable; 3 = good; 4 = excellent.
The reference STD protocol was taken from ProMax 3D Mid and Orthophos SL, the ULD protocol from ProMax 3D Mid, and the LD from Orthophos SL.
In Orthophos SL at the 85-kVp setting, the visibility scores of the anatomical structures significantly differed (p = 0.024) between the LD and STD protocols. The visibility scores for the STD protocol did not significantly differ (p = 0.097) between ProMax 3D Mid (90 and 120 kVp) and Orthophos SL (85 kVp). Meanwhile, the visibility scores significantly differed (p = 0.04) between the ULD protocol in ProMax 3D Mid and LD protocol in Orthophos SL. A pair comparison was subsequently performed, which revealed a significant difference (p < 0.05) between each ULD protocol in ProMax 3D Mid and LD protocol in Orthophos SL. Nevertheless, there was no significant difference (p = 0.083) found between the 90-kVp ULD and 120-kVp ULD protocols in ProMax 3D Mid.
The overall intra- and interrater agreements among all radiographic assessments of the observers ranged from poor to excellent (0.43–1.0) and from poor to good (0.3–0.9), respectively. The details of the intra- and interrater agreements are shown in Tables 5 and 6. As shown in Table 6, the interrater variation of the mean scores in relation to the STD and ULD or LD protocols revealed that the ULD and LD protocols yielded a much lower agreement than did the STD protocol: 90-kVp ProMax 3D Mid, 0.50 vs 0.76; 120-kVp ProMax 3D Mid, 0.62 vs 0.71; and 85-kVp Orthophos SL, 0.44 vs 0.62. The overall intra- and interrater agreement scores for the STD protocol appeared generally higher than those for the ULD and LD protocols in both ProMax 3D Mid and Orthophos SL.
Table 5.
Intrarater absolute agreement on the CBCT scanning protocols
| Observers | ProMax 3D Mid | Orthophos SL | ||||
|---|---|---|---|---|---|---|
| ULD (90 kVp) |
STD (90 kVp) |
ULD (120 kVp) |
STD (120 kVp) |
LD (85 kVp) |
STD (85 kVp) |
|
| Observer 1 | 0.97 | 1.00 | 1.00 | 1.00 | 0.83 | 1.00 |
| Observer 2 | 0.47 | 0.93 | 0.70 | 0.73 | 0.67 | 0.80 |
| Observer 3 | 0.43 | 0.77 | 0.57 | 0.67 | 0.87 | 0.77 |
| Observer 4 | 0.63 | 0.87 | 0.87 | 0.87 | 0.73 | 0.83 |
| Mean | 0.63 | 0.89 | 0.79 | 0.82 | 0.78 | 0.85 |
CBCT, cone-beam CT; LD, low dose; SD, standard dose; ULD, ultra-low-dose.
Table 6.
Interrater absolute agreement of CBCT scanning protocols
| Observers | ProMax 3D Mid | Orthophos SL | ||||
|---|---|---|---|---|---|---|
| ULD (90 kVp) |
STD (90 kVp) |
ULD (120 kVp) |
STD (120 kVp) |
LD (85 kVp) |
STD (85 kVp) |
|
| Observer 1 vs Observer 2 | 0.67 | 0.90 | 0.70 | 0.70 | 0.57 | 0.53 |
| Observer 1 vs Observer 3 | 0.30 | 0.63 | 0.47 | 0.63 | 0.43 | 0.47 |
| Observer 1 vs Observer 4 | 0.53 | 0.87 | 0.80 | 0.83 | 0.30 | 0.47 |
| Observer 2 vs Observer 3 | 0.37 | 0.63 | 0.50 | 0.70 | 0.57 | 0.73 |
| Observer 2 vs Observer 4 | 0.57 | 0.90 | 0.70 | 0.70 | 0.37 | 0.77 |
| Observer 3 vs Observer 4 | 0.57 | 0.63 | 0.53 | 0.67 | 0.37 | 0.73 |
| Mean | 0.50 | 0.76 | 0.62 | 0.71 | 0.44 | 0.62 |
CBCT, cone-beam CT; LD, low dose; SD, standard dose; ULD, ultra-low-dose.
The effective doses for 90-kVp ULD ProMax 3D Mid, 120-kVp ULD ProMax 3D Mid, and 85-kVp LD Orthophos SL were 2.8, 5.8, and 5 µSv, respectively. Meanwhile, those for 90-kVp STD ProMax 3D Mid, 120-kVp STD ProMax 3D Mid, and 85-kVp STD Orthophos SL were 16, 30.9, and 31 µSv, respectively. Regardless of the CBCT machines used, the overall effective doses for the ULD and LD protocols were approximately six times lower than those for the STD protocols.
Discussion
Herein, we compared the subjective image quality of dental anatomical structures in a phantom study, in which CBCT images were obtained from the STD protocol in ProMax 3D Mid and Orthophos SL, ULD protocol in ProMax 3D Mid, and LD protocol in Orthophos SL. The results indicate that the visibility of the anatomical structures taken from STD protocols is generally better than that taken from ULD and LD protocols. Considering the median visibility scores (Table 4), we also found varying image qualities of the anatomical structures observed from the LD and ULD protocols, ranging from acceptable to excellent, except for the poor quality noted on the PDL space from the LD protocol in Orthophos SL. While most visibility scores of the anatomical structures observed from the STD protocol were relatively good with well-defined images in both ProMax 3D Mid and Orthophos SL, our findings show that reducing the CBCT radiation dose using exposure factors at 85–120 kVp, 2–7 mA, and 2.1–3 s causes a slight decrease in the overall image quality while preserving an acceptable-to-excellent diagnostic image quality for the evaluation of small fine anatomy. Thus, low-dose exposure CBCT may be a reliable and valid method of detecting delicate dental anatomical landmarks and obtaining images of large dentomaxillofacial structures in certain dental works not requiring high resolutions.
CBCT has various applications in diverse diagnostic tasks and therapeutic planning in many dental specialties, including oral surgery, pediatric dentistry, orthodontics, endodontics, implant dentistry, periodontology, 5 diagnostic science, and digital dentistry. When CBCT is indicated, the exposure setting should be adjusted and optimized as per the ALADA principle. Presently, some modern CBCT units provide three modalities for exposure setting: LD mode, STD mode, and high-resolution mode. However, the range of CBCT indications is closely connected to the diagnostic task and the image quality requirements to fit the task for image quality assessment. For example, a volume acquired for endodontic lesion assessment has diverse image-quality demands. High-resolution CBCT images may be required to help diagnose root fractures and root resorptive defects more accurately. 27,28 In periodontology, although CBCT is not generally indicated, high-resolution CBCT images may be helpful for further investigation in case clinical examination and 2D radiography fail to provide sufficient information for the management of infrabony defects, dehiscence and fenestration defects, and furcation lesions. 29 In fact, high-resolution CBCT images in LD and ULD modes can also be obtained using some CBCT machines. Such images are clear, but with greater radiation burden. 30 Our study supports the use of either a basic LD mode or an SD mode of CBCT over a high-resolution setting for diverse general diagnostic tasks when CBCT is indicated, unless in cases involving the ALADAIP principle. In select cases that require clearly visible details for subtle anatomical structures, a CBCT protocol with a high resolution and a higher exposure setting is required.
The effective dose for small-FOV CBCT scanning protocol in the ULD and LD modes in the present investigation (5–5.8 µSv) is very low compared with the minimum effective dose for the small-FOV scanning protocol (11 µSv) reported by Bornstein et al. 31 Meanwhile, the effective doses for CBCT scanning protocols in the STD mode is comparable to the median effective dose of a small-FOV scanning protocol (28.5 µSv). ULD with high definition (ULDHD) setting is also available in ProMax 3D Mid. Compared with STD protocols, ULDHD and ULD protocols could reduce the radiation dose by 63 and 77%, respectively, in the anterior maxilla region. 30
In our experiment, we kept the exposure area and FOV similar to simulate the effect of the different technical factors, mainly kVp and mA, as provided by the manufacturers. Our results show that most of the visibility scores of the LD modes in Orthophos SL are lower than those of the ULD modes (90 and 120 kVp) in ProMax 3D Mid, although the number of projections (n = 381) is higher in Orthophos SL than in ProMax 3D Mid (n = 251) for image reconstruction. A shift from 90 to 120 kVp setting for CBCT scanning in the ULD and STD modes of ProMax 3D Mid barely increases the effective dose, providing better image quality and contrast of resultant images. When a high kVp mode is applied, the number of powerful X-ray photon penetrations and number of X-ray photons hitting a detector increase, and the number of medium or low X-ray photons being absorbed in an organ decreases. 32 Thus, we suggest adjustments to the highest kVp setting for low-dose CBCT. Even at a high kVp (120 kVp) and low mA (2 mA) setting, the image quality is comparable to that at the standard setting. For adjustments on mA, our results indicate that mA reduction can degrade the CBCT image quality, similar to the findings reported by Jones et al. 17
The CBCT software may also affect the image quality. In clinical practice, a user usually views CBCT images opened with the software that comes with the device as a data viewer. Major hospitals, health care units, and imaging companies use Picture Archiving and Communication Systems (PACS) and have DICOM data sets opened with a PACS software. Hence, CBCT images viewed under different third party CBCT software based on DICOM data sets exported from one CBCT software could result in different image qualities due to specificity of each third-party software. Furthermore, the acquired image quality may be reduced by exporting from a dedicated software to another vendor-specific software. To simulate a PACS environment and ensure equal image quality in our study, we exported the DICOM data set from each of the CBCT units and opened them in one CBCT software viewer, OnDemand3D.
For the observer reproducibility issues of ULD and LD modes in the current study, the intrarater agreement ranged from poor to excellent (absolute agreement: 0.43 to 1.00), whereas the interrater agreement ranged from poor to good (absolute agreement: 0.30 to 0.80). This indicates that subjective preference in image quality considerably varies between observers. The low intra- and interrater agreements could be explained by the difference in the visually pleasing perception of a noisy CBCT image the viewers subjectively visualized. Of 90-kVp ULD ProMax 3D Mid, 120-kVp ULD ProMax 3D Mid, and 85-kVp LD Orthophos-SL, the 120-kVp ULD ProMax 3D Mid setting yielded the best observer reproducibility. Observer 1 noted an outstanding reproducibility for the intrarater agreement. A possible reason for this finding is that Observer 1 had much more working experience in viewing LD and ULD CBCT images than the other observers. The great variance in the intra- and interrater agreements for LD and ULD CBCT protocols in this study exhibits the different subjective preferences of the radiologists in terms of image quality in an actual clinical situation of dentomaxillofacial radiology. Nevertheless, the image grading criteria were verbally explained among the observers prior to the actual evaluation session. Samples of cropped CBCT images, including all levels in the 5-point Likert scale, were shown to train the observers for precalibration. These CBCT image samples were taken from the same skulls used for the actual evaluation session. At low exposure, a noise reduction filter should be applied to improve image quality, which may increase the intra- and interrater agreements. 30
The limitations of this study are discussed in the following: (1) we performed CBCT on phantom heads; thus, the characteristics of the resulting CBCT images may differ from those of real skin and soft tissue. (2) We did not measure the quantitative image quality, including the SNR and CNR, as in other studies. (3) There was no movement during CBCT on the phantom heads. Notably, slight patient motion introduces geometric errors in the reconstruction and hence produces predominantly motion blurs (i.e. reduced spatial resolution). Visible artifacts, such as double or multiple contours, may be more pronounced, and specific motion patterns may occur. (4) The subjective image quality evaluation is also a limitation, since there is no information on actual clinical situations. This is very important because the observers subjectively judged the image quality with respect to the visibility of certain anatomical features from the phantoms comprising real skull features and artificial soft tissue-equivalent materials. Subjective image quality evaluation of anatomy may have different results between a phantom study model and a real patient. (5) We also excluded ULDHD protocols in the study. A high-resolution CBCT image may be prescribed in an indication-oriented and patient-specific case as per the ALADAIP principle. Such an image can be obtained with a small voxel size setting to achieve a reasonable signal-to-noise ratio for better image quality, but with a higher patient radiation dose as a consequence. 14 Our main aim was to compare the image quality of CBCT images acquired from Orthophos SL and ProMax 3D Mid, in LD and STD modes at similar effective doses but different radiation parameters. However, a noisy image may distract the visual appearance, particularly a CBCT image acquired from the LD and ULD modes. This challenged a clinician to clearly visualize certain delicate anatomical structures in a CBCT image when the LD and ULD modes were applied. Another example of common CBCT prescription in pediatric patients and teenagers is to investigate impacted maxillary canine in which a low-dose CBCT protocol is of great concern. 30 In these cases, a high-resolution mode is seldom used. We then emphasize the importance of anatomical evaluation using the basic LD and ULD modes. Accordingly, a high-resolution mode was not investigated in the ULD mode in the current study. Future studies are needed to solve the issue on high-resolution settings in other parts of the dentomaxillofacial region.
Conclusions
We demonstrated that small-FOV low-dose CBCT protocols using ProMax 3D Mid and Orthophos SL yielded an acceptable-to-good image quality for the evaluation of delicate dentomaxillofacial anatomy, except for the LD protocol in Orthophos SL, which resulted in a poor image quality for PDL space evaluation. The CBCT images obtained from the STD protocol showed a better quality than did those obtained from the low-dose protocols. For high kVp settings (i.e. 120 kVp), the subjective image quality did not significantly differ between the ULD and LD and the STD protocols. To date, there are only few position statements or clinical guidelines illustrating which low-dose CBCT protocols should be used in dental practice, even in specific cases. Subjective radiographic image evaluation of anatomical structures in an LD mode should be further studied in different clinical situations to identify how LD CBCT protocols can be applied in selected cases.
Footnotes
Acknowledgements: The authors would like to express their gratitude to the Department of Radiology, Tampere University Hospital, Tampere, Finland for providing all of materials and additional support during the study. A funding agency was not involved in the study for any materials, interpretation, data analysis, and writing of the report. Thanks to Dr Thanapat Sastraruji, the Research Center, Faculty of Dentistry, Chiang Mai University, for consultation of statistical analysis, and to Adjunct Professor Richard L. Wilson, the Faculty Consultant, Faculty of Dentistry, Chiang Mai University, for his for his assistance in the preparation of the manuscript in English. Declarations of interest: none.
Funding: Statement indicating any source of funding or financial interest where relevant should be included : A funding agency was not involved in the study for any materials, interpretation, data analysis, and writing of the report.
Ethics approval: Ethical approval was not obtained in the study as this study was a technical study using phantom heads for CBCT scans. Neither patient data nor patients were included in the study.
Contributor Information
Arnon Charuakkra, Email: arnon_cha903@hotmail.com.
Phattaranant Mahasantipiya, Email: drmaymh@gmail.com.
Antti Lehtinen, Email: antti.lehtinen@pshp.fi.
Juha Koivisto, Email: juha.koivisto@planmeca.com.
Jorma Järnstedt, Email: Jorma.Jarnstedt@pshp.fi.
REFERENCES
- 1. Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB mercuray, newtom 3G and i-CAT. Dentomaxillofac Radiol 2006; 35: 219–26. doi: 10.1259/dmfr/14340323 [DOI] [PubMed] [Google Scholar]
- 2. White SC and Pharoah MJ.. Oral Radiology principles and interpretation (7th edn). St.Louis: Mosby; 2014. [Google Scholar]
- 3. National Council on Radiation Protection and Measurements . NCRP: achievements of the past 50 years and addressing the needs of the future. Fiftieth annual meeting program. Bethesda: NCRP; 2014. Available from: http://www.ncrponline.org/Annual_Mtgs/2014_Ann_Mtg/PROGRAM_2-10.pdf [Google Scholar]
- 4. Oenning AC, Jacobs R, Pauwels R, Stratis A, Hedesiu M, Salmon B, et al. Cone-Beam CT in paediatric dentistry: dimitra project position statement. Pediatr Radiol 2018; 48: 308–16. doi: 10.1007/s00247-017-4012-9 [DOI] [PubMed] [Google Scholar]
- 5. Yeung AWK, Jacobs R, Bornstein MM. Novel low-dose protocols using cone beam computed tomography in dental medicine: a review focusing on indications, limitations, and future possibilities. Clin Oral Investig 2019; 23: 2573–81. doi: 10.1007/s00784-019-02907-y [DOI] [PubMed] [Google Scholar]
- 6. ICRP publication 105. radiation protection in medicine. Ann ICRP 2007; 37: 1–63. doi: 10.1016/j.icrp.2008.08.001 [DOI] [PubMed] [Google Scholar]
- 7. Hidalgo Rivas JA, Horner K, Thiruvenkatachari B, Davies J, Theodorakou C. Development of a low-dose protocol for cone beam CT examinations of the anterior maxilla in children. Br J Radiol 2015; 88(1054): 20150559. doi: 10.1259/bjr.20150559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dawood A, Brown J, Sauret-Jackson V, Purkayastha S. Optimization of cone beam CT exposure for pre-surgical evaluation of the implant site. Dentomaxillofac Radiol 2012; 41: 70–74. doi: 10.1259/dmfr/16421849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ludlow JB, Walker C. Assessment of phantom dosimetry and image quality of i-CAT FLX cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2013; 144: 802–17: S0889-5406(13)00774-9. doi: 10.1016/j.ajodo.2013.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yadav S, Palo L, Mahdian M, Upadhyay M, Tadinada A. Diagnostic accuracy of 2 cone-beam computed tomography protocols for detecting arthritic changes in temporomandibular joints. Am J Orthod Dentofacial Orthop 2015; 147: 339–44: S0889-5406(14)01056-7. doi: 10.1016/j.ajodo.2014.11.017 [DOI] [PubMed] [Google Scholar]
- 11. Lu B, Lu H, Palta J. A comprehensive study on decreasing the kilovoltage cone-beam CT dose by reducing the projection number. J Appl Clin Med Phys 2010; 11: 3274. doi: 10.1120/jacmp.v11i3.3274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pauwels R, Silkosessak O, Jacobs R, Bogaerts R, Bosmans H, Panmekiate S. A pragmatic approach to determine the optimal kvp in cone beam CT: balancing contrast-to-noise ratio and radiation dose. Dentomaxillofac Radiol 2014; 43(5): 20140059. doi: 10.1259/dmfr.20140059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bechara B, McMahan CA, Moore WS, Noujeim M, Geha H, Teixeira FB. Contrast-to-noise ratio difference in small field of view cone beam computed tomography machines. J Oral Sci 2012; 54: 227–32. doi: 10.2334/josnusd.54.227 [DOI] [PubMed] [Google Scholar]
- 14. Scarfe WC. Cone beam computed tomography: volume acquisition. In: Mallya SM, Lam EWN, eds. White and Pharoah’s oral radiology principles and interpretation. 8th edn. St. Louis Mosby; 2019, pp. 386–414. [Google Scholar]
- 15. Hassan B, Metska ME, Ozok AR, Stelt PV, Wesselink PR. Detection of vertical root fractures in endodontically treated teeth by cone beam computed tomography. J Endod 2010; 36: 126–29. [DOI] [PubMed] [Google Scholar]
- 16. Siltanen S, Kolehmainen V, Järvenpää S, Kaipio JP, Koistinen P, Lassas M, et al. Statistical inversion for medical X-ray tomography with few radiographs: I. General theory. Phys Med Biol 2003; 48: 1437–63. doi: 10.1088/0031-9155/48/10/314 [DOI] [PubMed] [Google Scholar]
- 17. Jones D, Mannocci F, Andiappan M, Brown J, Patel S. The effect of alteration of the exposure parameters of a cone-beam computed tomographic scan on the diagnosis of simulated horizontal root fractures. J Endod 2015; 41: 520–25: S0099-2399(14)01138-8. doi: 10.1016/j.joen.2014.11.022 [DOI] [PubMed] [Google Scholar]
- 18. Durack C, Patel S, Davies J, Wilson R, Mannocci F. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. Int Endod J 2011; 44: 136–47. doi: 10.1111/j.1365-2591.2010.01819.x [DOI] [PubMed] [Google Scholar]
- 19. Bechara B, McMahan CA, Nasseh I, Geha H, Hayek E, Khawam G, et al. Number of basis images effect on detection of root fractures in endodontically treated teeth using a cone beam computed tomography machine: an in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 115: 676–81. doi: 10.1016/j.oooo.2013.01.026 [DOI] [PubMed] [Google Scholar]
- 20. Brown AA, Scarfe WC, Scheetz JP, Silveira AM, Farman AG. Linear accuracy of cone beam CT derived 3D images. Angle Orthod 2009; 79: 150–57. doi: 10.2319/122407-599.1 [DOI] [PubMed] [Google Scholar]
- 21. Cook VC, Timock AM, Crowe JJ, Wang M, Covell DA. Accuracy of alveolar bone measurements from cone beam computed tomography acquired using varying settings. Orthod Craniofac Res 2015; 18 Suppl 1: 127–36. doi: 10.1111/ocr.12072 [DOI] [PubMed] [Google Scholar]
- 22. Koivisto J, Kiljunen T, Tapiovaara M, Wolff J, Kortesniemi M. Assessment of radiation exposure in dental cone-beam computerized tomography with the use of metal-oxide semiconductor field-effect transistor (MOSFET) dosimeters and Monte Carlo simulations. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114: 393–400. doi: 10.1016/j.oooo.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 23. Koivisto J, Kiljunen T, Wolff J, Kortesniemi M. Characterization of MOSFET dosimeter angular dependence in three rotational axes measured free-in-air and in soft-tissue equivalent material. J Radiat Res 2013; 54: 943–49. doi: 10.1093/jrr/rrt015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pauwels R, Beinsberger J, Collaert B, Theodorakou C, Rogers J, Walker A, et al. Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 2012; 81: 267–71. doi: 10.1016/j.ejrad.2010.11.028 [DOI] [PubMed] [Google Scholar]
- 25. Loubele M, Bogaerts R, Van Dijck E, Pauwels R, Vanheusden S, Suetens P, et al. Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 2009; 71: 461–68. doi: 10.1016/j.ejrad.2008.06.002 [DOI] [PubMed] [Google Scholar]
- 26. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 2016; 15: 155–63. doi: 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Taramsari M, Kajan ZD, Bashirzadeh P, Salamat F. Comparison of high-resolution and standard zoom imaging modes in cone beam computed tomography for detection of longitudinal root fracture: an in vitro study. Imaging Sci Dent 2013; 43: 171–77. doi: 10.5624/isd.2013.43.3.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ponder SN, Benavides E, Kapila S, Hatch NE. Quantification of external root resorption by low- vs high-resolution cone-beam computed tomography and periapical radiography: a volumetric and linear analysis. Am J Orthod Dentofacial Orthop 2013; 143: 77–91. doi: 10.1016/j.ajodo.2012.08.023 [DOI] [PubMed] [Google Scholar]
- 29. Tyndall DA, Rathore S. Cone-Beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am 2008; 52: 825–41. doi: 10.1016/j.cden.2008.05.002 [DOI] [PubMed] [Google Scholar]
- 30. Ihlis RL, Kadesjö N, Tsilingaridis G, Benchimol D, Shi XQ. Image quality assessment of low-dose protocols in cone beam computed tomography of the anterior maxilla. Oral Surg Oral Med Oral Pathol Oral Radiol 2022; 133: 483–91. doi: 10.1016/j.oooo.2021.10.001 [DOI] [PubMed] [Google Scholar]
- 31. Bornstein MM, Scarfe WC, Vaughn VM, Jacobs R. Cone beam computed tomography in implant dentistry: a systematic review focusing on guidelines, indications, and radiation dose risks. Int J Oral Maxillofac Implants 2014; 29 Suppl: 55–77. doi: 10.11607/jomi.2014suppl.g1.4 [DOI] [PubMed] [Google Scholar]
- 32. Bushong SC. Radiologic science for technologists: physics, biology, and protection. St. Louis: Mosby; 2008, pp.146–47. [Google Scholar]