Abstract
[Purpose] This study aimed to identify kinematic gait indicators for a fall risk screening test through quantitative comparisons of gait characteristics measured using mobile inertial sensors between faller and non-faller groups in a population of community-dwelling older people. [Participants and Methods] We enrolled 50 people aged ≥65 years who used long-term care prevention services, interviewed them to determine their fall history during the past year, and divided them into faller and non-faller groups. Gait parameters (velocity, cadence, stride length, foot height, heel strike angle, ankle joint angle, knee joint angle, and hip joint angle) were assessed using the mobile inertial sensors. [Results] Gait velocity and left and right heel strike angles were significantly lower and smaller, respectively, in the faller versus non-faller group. Receiver operating characteristic curve analysis revealed areas under the curve of 0.686, 0.722, and 0.691 for gait velocity, left heel strike angle, and right heel strike angle, respectively. [Conclusion] Gait velocity and heel strike angle during gait assessed using mobile inertial sensors may be important kinematic indicators in a fall risk screening test to estimate the likelihood of falls among community-dwelling older people.
Keywords: Gait, Fall risk screening, Mobile inertial sensor
INTRODUCTION
The percentage of individuals aged ≥65 years who fall over the course of a year was approximately 30% in 20101), and the rate of injury caused by falls is reportedly between 6%2) and 13%3). With regard to the risk factors for falls, relative risks or odds ratios have been reported as follows: muscle weakness, 4.4; history of falls, 3.0; gait deficits, 2.9; balance deficits, 2.9; use of assistive devices, 2.6; visual deficits, 2.5; arthritis, 2.4; impaired activities of daily living, 2.3; depression, 2.2; cognitive impairment, 1.8; and age >80 years, 1.74). Similarly, Tinetti et al.5) reported that the strongest risk factors for falls among community-dwelling older people included a past history of falls as well as strength, gait, and balance impairments.
Fall prevention guidelines published in 2010 recommend an assessment of the history of falls, as well as gait and balance, during fall intervention screening6). For gait and balance assessments, the Timed Up and Go Test7), Performance-Oriented Mobility Assessment8), and Berg Balance Scale9) are frequently used.
In a survey that investigated fall situations in 589 older people (≥65 years), the activity immediately before the fall was most often ambulation (56.5%), and the cause of the fall was most often a balance/gait problem (61.9%)10). Other studies that examined pre-fall activities also reported walking (58.1%) as the most common activity immediately before the fall11). On the basis of these previous findings and reports of frequent fall occurrences while walking, the present study focused on the analysis of gait function as an index of the fall risk in community-dwelling older people.
Previous studies have used performance-based clinical tests, a video-based three-dimensional motion analysis system12), mobile inertial sensors13), an instrumented walkway14), and other methods to investigate gait function in relation to fall risk. However, a high cost and a complex operating system are limitations with the use of a three-dimensional motion analyzer for measurement and data analysis. Moreover, an instrumented walkway has limitations in terms of measurement of the range of motion in the hip, knee, and ankle joints. In contrast, Ejupi et al.15) reported that fall risk assessments based on mobile inertial sensor were low cost and objective, and required portable measuring instruments that have become available because of recent technological advances.
Accordingly, in the present study, we used mobile inertial sensors to analyze gait function in community-dwelling older people. Previous studies have also used these sensors to collect quantitative measurements of temporo-spatial gait parameters. Donath et al.13, 16) showed that the RehaGait® system (HASOMED GmbH, Magdeburg, Germany), which is constructed with inertial sensors, was valid and reliable for measuring temporo-spatial gait characteristics during treadmill walking. In addition, Nüesch et al.17) reported that for healthy participants, the sagittal plane joint kinematic waveforms measured with the RehaGait® inertial sensor system were comparable to those measured with the Vicon optoelectronic reference system (Vicon Motion Systems Ltd., Oxford, UK).
In a systematic review that compared temporo-spatial gait parameters between fallers and non-fallers in a group of older people, time variability, gait speed, stride length, and step length showed the maximum differences between the two groups. However, in the reviewed articles, the methodology, participant selection criteria, and definitions for discriminating fallers from non-fallers were not homogeneous18). Petraglia et al.19) reported that although many studies measured gait speed, step length, step time, stance time, stride time, cadence, and swing time, only a few studies measured other parameters. According to a report focusing on joint angles, fallers had fewer changes in the hip angle, ankle angle20), and maximal hip extension angle21) than did non-fallers.
Previous findings have shown that the temporo-spatial parameters of gait function analyzed by mobile inertial sensors such as RehaGait® may help estimate fall risk. However, few reports have verified the validity of analyzing temporo-spatial characteristics, including joint angle in gait, using mobile inertial sensors as an index for fall risk screening in community-dwelling older people. The purpose of this study was to identify kinematic gait indicators for a fall risk screening test through quantitative comparisons of gait characteristics, measured using mobile inertial sensors, between faller and non-faller groups in a population of community-dwelling older people.
PARTICIPANTS AND METHODS
Fifty older people (age ≥65 years) using long-term care prevention services were enrolled in this study after they provided written informed consent. The participants included 43 females and 7 males with a mean age of 82.6 ± 6.0 years. Inclusion criteria included the ability to walk independently without using aids. Exclusion criteria included a stroke diagnosis, Parkinson’s disease, rheumatism, and a history of hip or knee surgery. Participants with any history of falls that resulted in unintentional landing on the ground, floor, or lower level within the past year were categorized as the faller group (n=16; 4 males, 12 females)22). Participants without any previous incidence of falls were categorized as the non-faller group (n=34; 3 males, 31 females). The study was conducted with the approval of the Medical Ethics Committee of Shinshu University School of Medicine (No. 4004).
First, an interview was conducted to determine whether there was a history of falls during the past year. Next, participants walked barefoot at a normal speed for two trials using the mobile inertial sensor (RehaGait® system, HASOMED GmbH)23). Measurements were performed in a room with a straight 16-m flat wood floor as previously described24). Each trial was followed by a 1-min break. The RehaGait® system consisted of seven inertial sensors. Each sensor contained a 3-axial accelerometer, gyroscope, and magnetometer. Inertial sensors were attached laterally on the feet (below the lateral malleolus), the shanks (laterally above the ankle joints), the thighs (above the knee joints), and at lumbar vertebrae 4/5 using double-sided tape and elastic straps. The system and model were calibrated while the participant was in a neutral upright standing position for 10 s and successively moved their right and left leg forward 30° while bending the spine backwards 15°. Temporal parameters, such as velocity and cadence, and spatial parameters in gait, such as stride length, foot height, heel strike angle (the angle between the floor and the foot at the moment of the heel contact), ankle joint angle, knee joint angle, and hip joint angle, were analyzed as temporo-spatial characteristics in gait using manufacturer proprietary software (RehaGait® system).
The normality of the data from the temporo-spatial parameters in gait was analyzed using the Shapiro–Wilk test before comparing the parameters between the faller and non-faller groups. The differences in parameters were then compared using the t-test for normally distributed data and Mann–Whitney U test for non-normally distributed data. χ2 tests were used to assess differences between the faller and non-faller groups by gender. If significant differences between groups were observed, a receiver operating characteristic (ROC) curve was plotted to determine the area under the curve (AUC), cut-off, sensitivity, and specificity values. A p-value of ˂0.05 was considered statistically significant. All statistical analyses were conducted using IBM SPSS Statistics 25 (IBM Corporation, Armonk, NY, USA).
RESULTS
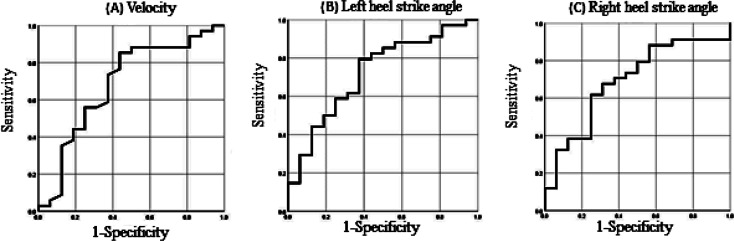
The characteristics of the faller and non-faller groups are summarized in Table 1. There were no significant differences between the two groups in terms of age, gender, height, and weight. Velocity and left and right heel strike angles were significantly different between the faller and non-faller groups (p<0.05). Although it was not statistically significant, the stride length of the faller group was shorter than that of the non-faller group (p=0.066). The results of ROC curve analysis for velocity and left and right heel strike angles are provided in Table 2, and the ROC curves are shown in Fig. 1. The AUC for the left heel strike angle (0.722) was the largest among the three parameters. The cut-off value for velocity was 0.83 m/s (85% sensitivity and 56% specificity), while those for the left and right heel strike angles were 15.8° (79% sensitivity and 63% specificity) and 16.5° (68% sensitivity and 69% specificity), respectively.
Table 1. Characteristics of the faller and non-faller groups.
| Non-faller group (n=34) | Faller group (n=16) | |
| Age [years]a | 81.7 ± 6.2 (83.0) | 84.6 ± 5.7 (85.5) |
| gender [n males, n females]b | 3, 31 | 4, 12 |
| Height [cm]c | 147.0 ± 8.0 (147) | 150.0 ± 11.0 (148) |
| Weight [kg]a | 54.3 ± 9.4 (53.6) | 49.8 ± 10.4 (47.9) |
| Stride duration [s]a | 1.03 ± 0.07 (1.04) | 1.10 ± 0.28 (1.02) |
| Stride length [m]c | 0.96 ± 0.16 (0.99) | 0.87 ± 0.17 (0.87) |
| Velocity [m/s]c | 0.93 ± 0.16 (0.94) | 0.82 ± 0.22 (0.78)* |
| Cadence [/min]a | 116.8 ± 8.1 (115.4) | 113.7 ± 20.1 (118.3) |
| Left stance [%]a | 64.2 ± 4.2 (63.2) | 64.7 ± 4.1 (63.7) |
| Right stance [%]a | 64.7 ± 4.0 (63.4) | 65.0 ± 5.3 (63.5) |
| Left single support [%]a | 36.4 ± 2.0 (36.6) | 35.8 ± 3.3 (36.5) |
| Right single support [%]a | 35.9 ± 4.0 (36.6) | 35.4 ± 4.1 (36.3) |
| Left double support [%]a | 17.7 ± 14.1 (13.4) | 17.1 ± 9.3 (13.8) |
| Right double support [%]a | 21.0 ± 22.2 (13.4) | 21.2 ± 22.2 (13.4) |
| Left max. foot height [cm]a | 10.1 ± 1.8 (10.0) | 10.2 ± 1.7 (10.3) |
| Right max. foot height [cm]c | 11.3 ± 1.7 (11.5) | 11.3 ± 1.8 (11.3) |
| Left heel strike angle [°]a | 18.1 ± 5.0 (19.6) | 14.2 ± 6.2 (15.0)* |
| Right heel strike angle [°]a | 18.3 ± 8.0 (19.4) | 13.6 ± 8.0 (14.9)* |
| Left max. ankle plantarflexion angle [°]a | 12.5 ± 7.9 (10.6) | 11.8 ± 7.3 (10.3) |
| Right max. ankle plantarflexion angle [°]a | 9.0 ± 4.3 (8.1) | 10.8 ± 7.1 (8.4) |
| Left max. ankle dorsiflexion angle [°]a | 10.6 ± 4.2 (10.3) | 10.6 ± 3.6 (10.6) |
| Right max. ankle dorsiflexion angle [°]a | 9.4 ± 2.8 (9.5) | 9.7 ± 3.9 (10.7) |
| Left max. knee flexion angle [°]a | 41.7 ± 8.5 (43.5) | 43.7 ± 15.1 (40.5) |
| Right max. knee flexion angle [°]a | 41.7 ± 15.4 (38.7) | 40.4 ± 16.5 (38.2) |
| Left max. knee extension angle [°]a | 0.5 ± 0.1 (0.5) | 0.5 ± 0.1 (0.5) |
| Right max. knee extension angle [°]c | 0.5 ± 0.1 (0.5) | 0.5 ± 0.1 (0.5) |
| Left max. hip flexion angle [°]c | 28.2 ± 6.6 (27.8) | 27.8 ± 4.6 (27.3) |
| Right max. hip flexion angle [°]c | 27.3 ± 6.3 (28.6) | 25.2 ± 9.2 (24.5) |
| Left max. hip extension angle [°]a | 12.1 ± 6.3 (11.3) | 10.9 ± 6.0 (10.0) |
| Right max. hip extension angle [°]a | 13.2 ± 7.8 (11.8) | 13.5 ± 8.2 (11.3) |
Data are presented as mean ± standard deviation (median).
a: Mann–Whitney’s U test, b: χ2 test, c: t-test. *p<0.05.
Table 2. Parameters of the receiver operating curves (ROC) for velocity and heel strike angles (cf. Fig. 1).
| Parameter | AUC | Cut-off point | Sensitivity | Specificity |
| Velocity [m/s] | 0.686 | 0.83 | 0.85 | 0.56 |
| Left heel strike angle [°] | 0.722 | 15.8 | 0.79 | 0.63 |
| Right heel strike angle [°] | 0.691 | 16.5 | 0.68 | 0.69 |
AUC: area under the curve.
Fig. 1.
Receiver operating characteristic (ROC) curves for (A) velocity, (B) left heel strike angle, and (C) right heel strike angle analyzed in community-dwelling older individuals.
DISCUSSION
This study clarified the validity of a fall risk screening index using mobile inertial sensors to measure temporo-spatial characteristics of gait in community-dwelling older people. The results showed that velocity and heel strike angles during gait were significantly slower and smaller, respectively, in the faller group than in the non-faller group, and the sensitivity, specificity, and cut-off values of these parameters were analyzed.
Previous studies of gait velocity have shown a high risk of falls among groups with gait speeds ranging from 0.6 to 1.0 m/s25). In this study, the non-faller and faller groups had gait speeds of 0.93 ± 0.16 and 0.82 ± 0.22 m/s, respectively. Therefore, the older people in both groups had a high risk of falling based on previous reports concerning gait velocity. Our study results revealed that the gait velocity cut-off value of 0.83 m/s allows distinguishing a faller from a non-faller.
The left and right heel strike angles were significantly different between the faller and non-faller groups. In particular, the left heel strike angle exhibited a high AUC in the ROC curve. Among studies of joint angles in gait, a few include ankle angles. Kemoun et al.20) reported that dorsiflexion of the ankle during the second phase of double support and plantar flexion of the ankle at the beginning of swing were significantly lower in the faller group than in the non-faller group. Winter et al.26) reported that the angle of the foot relative to the ground at heel contact, measured by a video digitizing system and a force platform, was decreased in older participants because of a shorter step length; thus, the need for energy absorption by the dorsiflexors when the foot was lowered to the ground was also reduced.
Previous research reported that a faller group showed a lesser change in the ankle joint angle from the late stance phase to the early swing phase than did a non-faller group20, 26). Similarly, this study showed that the angle of the foot relative to the ground at heel contact in the faller group was smaller than that in the non-faller group. Although the difference was statistically marginally significant (p=0.066), the stride length in the faller group tended to be shorter than that in the non-faller group.
Based on these results, it was considered that the decrease in heel strike angle at heel contact in the faller group might be affected by the shortened stride length; this could affect the increase in fall risk in community-dwelling older people.
This study has some limitations. The participants were community-dwelling older people who were recruited from long-term care prevention services centers and were able to walk independently. Although they were divided into the faller and non-faller groups, they were already considered to be at risk of falling based on their gait velocity data. Therefore, the results of this study may have limited applicability to healthy older people who do not use long-term care prevention services.
In conclusion, the findings of this study suggest that kinesiological temporo-spatial parameters, including gait velocity and heel strike angle during gait, measured by mobile inertial sensors may be valid indicators in a fall risk screening test aimed at preventing falls in community-dwelling older people.
Funding
This work was supported by the Japan Society for the Promotion of Science Grants-in-Aid for Scientific Research [Grant Number JP16k13027]. The funding sources had no role in the study design, execution, analysis, and interpretation of the data, or writing of this manuscript.
Conflict of interest
The authors indicated no conflicts of interest.
REFERENCES
- 1.Deandrea S, Lucenteforte E, Bravi F, et al. : Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology, 2010, 21: 658–668. [DOI] [PubMed] [Google Scholar]
- 2.Hausdorff JM, Rios DA, Edelberg HK: Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil, 2001, 82: 1050–1056. [DOI] [PubMed] [Google Scholar]
- 3.Bergland A, Wyller TB: Risk factors for serious fall related injury in elderly women living at home. Inj Prev, 2004, 10: 308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rubenstein LZ, Josephson KR: The epidemiology of falls and syncope. Clin Geriatr Med, 2002, 18: 141–158. [DOI] [PubMed] [Google Scholar]
- 5.Tinetti ME, Kumar C: The patient who falls: “It’s always a trade-off”. JAMA, 2010, 303: 258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society: Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc, 2011, 59: 148–157. [DOI] [PubMed] [Google Scholar]
- 7.Podsiadlo D, Richardson S: The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc, 1991, 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 8.Tinetti ME: Performance-oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc, 1986, 34: 119–126. [DOI] [PubMed] [Google Scholar]
- 9.Berg K, Wood-Dauphine S, Williams JI, et al. : Measuring balance in the elderly: preliminary development of an instrument. Physiother Can, 1989, 41: 304–311. [Google Scholar]
- 10.Talbot LA, Musiol RJ, Witham EK, et al. : Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health, 2005, 5: 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shin KR, Kang Y, Jung D, et al. : A comparative study on physical function test between faller group and nonfaller group among community-dwelling elderly. Asian Nurs Res, 2012, 6: 42–48. [DOI] [PubMed] [Google Scholar]
- 12.Kerrigan DC, Lee LW, Nieto TJ, et al. : Kinetic alterations independent of walking speed in elderly fallers. Arch Phys Med Rehabil, 2000, 81: 730–735. [DOI] [PubMed] [Google Scholar]
- 13.Donath L, Faude O, Lichtenstein E, et al. : Mobile inertial sensor based gait analysis: validity and reliability of spatiotemporal gait characteristics in healthy seniors. Gait Posture, 2016, 49: 371–374. [DOI] [PubMed] [Google Scholar]
- 14.Scott D, McLaughlin P, Nicholson GC, et al. : Changes in gait performance over several years are associated with recurrent falls status in community-dwelling older women at high risk of fracture. Age Ageing, 2015, 44: 287–293. [DOI] [PubMed] [Google Scholar]
- 15.Ejupi A, Lord SR, Delbaere K: New methods for fall risk prediction. Curr Opin Clin Nutr Metab Care, 2014, 17: 407–411. [DOI] [PubMed] [Google Scholar]
- 16.Donath L, Faude O, Lichtenstein E, et al. : Validity and reliability of a portable gait analysis system for measuring spatiotemporal gait characteristics: comparison to an instrumented treadmill. J Neuroeng Rehabil, 2016, 13: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nüesch C, Roos E, Pagenstert G, et al. : Measuring joint kinematics of treadmill walking and running: comparison between an inertial sensor based system and a camera-based system. J Biomech, 2017, 57: 32–38. [DOI] [PubMed] [Google Scholar]
- 18.Mortaza N, Abu Osman NA, Mehdikhani N: Are the spatio-temporal parameters of gait capable of distinguishing a faller from a non-faller elderly? Eur J Phys Rehabil Med, 2014, 50: 677–691. [PubMed] [Google Scholar]
- 19.Petraglia F, Scarcella L, Pedrazzi G, et al. : Inertial sensors versus standard systems in gait analysis: a systematic review and meta-analysis. Eur J Phys Rehabil Med, 2019, 55: 265–280. [DOI] [PubMed] [Google Scholar]
- 20.Kemoun G, Thoumie P, Boisson D, et al. : Ankle dorsiflexion delay can predict falls in the elderly. J Rehabil Med, 2002, 34: 278–283. [DOI] [PubMed] [Google Scholar]
- 21.Kerrigan DC, Lee LW, Collins JJ, et al. : Reduced hip extension during walking: healthy elderly and fallers versus young adults. Arch Phys Med Rehabil, 2001, 82: 26–30. [DOI] [PubMed] [Google Scholar]
- 22.Lamb SE, Jørstad-Stein EC, Hauer K, et al. Prevention of Falls Network Europe and Outcomes Consensus Group: Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc, 2005, 53: 1618–1622. [DOI] [PubMed] [Google Scholar]
- 23.RehaGait® analyzer user manual, version 3.0. Magdeburg: HASOMED GmbH, 2017, pp 1–49. [Google Scholar]
- 24.Middleton A, Fritz SL, Lusardi M: Walking speed: the functional vital sign. J Aging Phys Act, 2015, 23: 314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abu Samah Z, Mohd Nordin NA, Shahar S, et al. : Can gait speed test be used as a falls risk screening tool in community dwelling older adults? A review. Pol Ann Med, 2016, 23: 61–67. [Google Scholar]
- 26.Winter DA, Patla AE, Frank JS, et al. : Biomechanical walking pattern changes in the fit and healthy elderly. Phys Ther, 1990, 70: 340–347. [DOI] [PubMed] [Google Scholar]