Abstract
Introduction
There is wide variation in the management of simple subcutaneous abscesses in the UK and no national guidelines describing best practice. During the SARS-CoV-2 pandemic, regional or local anaesthesia (LA) use was recommended instead of general anaesthesia. This study aimed to assess the effect of anaesthetic use on outcomes following incision and drainage (I&D) of simple subcutaneous abscesses.
Methods
Two cohorts of patients undergoing abscess incision and drainage at St. James’ University Hospital in Leeds were identified retrospectively over a 14-week period before (P1) and after (P2) the introduction of the COVID-19 anaesthetic guidelines. The number of follow-up appointments for repacking and representation to healthcare services 30 days after I&D were used as surrogate endpoints for wound healing.
Results
A total of 133 patients were included (n=70, P1 and n=63, P2). Significantly more procedures were performed under LA after the intervention (84.1% vs 5.7%; p<0.0001) with a significant reduction in wound packing (68.3% vs 87.1%; p=0.00473). Follow-up analysis found no significant difference in the median number of follow-up appointments (7.46 vs 5.11; p=0.0731) and the number of patients who required ongoing treatment after 30 days (n=14, P1 vs n=14, P2; p=0.921).
Conclusions
Drainage of simple subcutaneous abscess under 5cm in diameter is safe under LA, with no significant difference in surrogate endpoints of wound healing observed in this patient cohort. Recurrent packing may not be required. Future work should explore patient-reported outcomes, including pain management, cosmesis and the cost and sustainability implications of a change in this common procedure.
Keywords: Abscess, Drainage, COVID-19, Anaesthetic
Introduction
A subcutaneous abscess is a superficial pus-filled cavity formed in the dermis or hypodermis layers of the skin, typically caused by a localised microbial infection (most commonly Staphylococcus aureus).1 Abscesses commonly present to primary care or the emergency department (ED) as a localised, tender, fluctuant swelling, with an overlying pustule and surrounding, localised cellulitis.2
There are currently no accurate data available describing the incidence of subcutaneous abscesses in the UK. In the US, the incidence has increased steadily over the last 23 years, now accounting for 1.5 million ED visits per annum.3,4
The National Institute for Health and Care Excellence (NICE) guidance recommends same-day attendance to a surgical unit for I&D of all fluctuant boils or carbuncles.5 Incision and drainage (I&D) is the accepted management of subcutaneous abscesses internationally with the sole purpose of draining local sepsis to promote healing through secondary intention.2 Variation exists in choice of anaesthetic, incision (linear vs elliptical), capsule excision (if present) as well as the use of curettage, irrigation, packing (primary and recurrent) and antibiotics. There remains no specific guidance for the management of simple subcutaneous abscesses in the UK.6–8
To minimise pain and allow for thorough debridement of the abscess, surgical management requires anaesthesia. Choice of anaesthetic (ie, local, regional, or general) remains at the discretion of the operating surgeon and patient preference.9 The evidence regarding anaesthesia for surgical abscess management is limited and heterogeneous.8 Whereas abscess I&D under both local anaesthetia (LA) and general anaesthesia (GA) is accepted as safe and effective, there is no randomised comparison in the literature.
The SARS-CoV-2 pandemic instigated significant changes to clinical practice to manage hospital capacity and to limit healthcare worker exposure to the virus. The intubation and ventilation required for GA was identified as a high-risk aerosol-generating procedure, resulting in the Royal College of Surgeons of England introducing guidance encouraging the use of LA whenever possible.10 This rationale was strengthened by observational data that demonstrated a large increase in postoperative complications and mortality in patients positive for the virus receiving a GA.11 We aimed to assess this change in guidance and determine the effect of anaesthetic choice on surrogate markers of wound healing in simple subcutaneous abscess management in a single centre.
Methods
Sample
All adult patients (>16 years old) attending the Surgical Assessment Unit (SAU) at St James’ University Hospital (SJUH), Leeds, UK, with subcutaneous abscesses were identified from attendance records over a 14-week period before and after the intervention. The first cohort (P1) attended SAU and underwent I&D between 16 October 2018 and 31 January 2019. The second cohort of patients (P2) underwent I&D during the COVID-19 pandemic between 29 March 2020 and 15 June 2020. Ethical approval was received from the University of Leeds School of Medicine Research Ethics Committee (MREC 18-060).
Intervention
On 29 March 2020, RSC England released guidance stipulating that abscesses should be drained under LA where possible (intervention). In this study, I&D under GA was performed in CEPOD theatres, whereas I&D under LA was performed in the SAU. There was no standardised protocol for I&D of a simple subcutaneous abscess.
Inclusion criteria
All adult patients (>16 years) attending SAU at SJUH with a subcutaneous abscess during the relevant periods (Table 1).
Table 1 .
Inclusion and exclusion criteria used for study participant selection
| Inclusion | Exclusion |
|---|---|
| Patients with subcutaneous abscesses | Paediatrics population (<16 years old) |
| Admitted to SJUH via SAU | Pilonidal disease |
| Perianal disease | |
| Groin abscesses in IVDU (ex or current) | |
| Abscesses related to inflammatory bowel disease | |
| Abscesses related to malignancy |
IVDU = intravenous drug users; SAU = Surgical Assessment Unit; SJUH = St James’ University Hospital
Exclusion criteria
All patients with pilonidal or perianal disease, groin abscesses in intravenous drug users, breast abscesses and abscesses related to inflammatory bowel disease or malignancy (Table 1).
Data collection
Data pertaining to the demographics, clinical intervention and follow-up were collected for all patients through operation note, clerking and discharge letters. Follow-up data were obtained through PPM+ (Leeds, UK) (local integrated online healthcare record) or through direct contact with patients’ general practitioner (GP). Up to two attempts were made to obtain follow-up information directly from practice using three questions: (i) ‘Did the patient attend follow-up for packing/dressing change?’ (ii) ‘What was the total number of attendances for packing/dressing change?’ (iii) ‘What was the date of the final packing/dressing change?’.
Outcomes
Number of follow-up appointments for re-packing and re-presentation to healthcare services after 30 days after I&D were used as surrogate endpoints for wound healing.
Analysis
All data were analysed using Excel (Microsoft Corporation). Statistical comparisons were made between the two cohorts (P1 and P2) of patients using a t-test for continuous data and chi-square test for categorical data to determine the statistical significance of the differences in baseline demographics, anaesthetic choice, wound packing and surrogate endpoints for wound healing outcomes (number of follow-up appointments and representation after 30 days). The distribution of outcome measure data was assessed and appropriate averages used. Statistical significance was set at p<0.05. For each outcome, patients who were lost to follow-up were excluded from the analysis as per protocol (Table 2).
Table 2 .
Reasons for exclusion of participants from data analysis in P1 and P2. (CCG are groups of GPs that come together in each area.)
| Reasons for exclusion | P1 n (%) |
P2 n (%) |
|---|---|---|
| GP practice unknown | 4 (5.71) | 0 (0.00) |
| Out of CCG area | 2 (2.86) | 2 (3.17) |
| Deceased | 1 (1.43) | 0 (0.00) |
| No response | 4 (5.71) | 0 (0.00) |
| Total | 11 (18.6) | 2 (3.33) |
CGC = clinical commissioning groups; GP = general practice
Results
Patient demographics
In total, 132 patients (133 abscesses) were included in the study, with 70 in P1 and 63 in P2. The mean age of the P2 group was significantly higher than that of P1, whereas the male-to-female ratio did not differ significantly between the two groups (Table 3).
Table 3 .
Participant demographics in P1 and P2
| Demographic data | P1 | P2 | |
|---|---|---|---|
| Sex | n (%) | n (%) | |
| Male | 34 (48.6) | 32 (50.8) | p=0.798 |
| Female | 36 (51.4) | 31 (49.2) | |

|

|
||
| Age (years) | 39.1 (±15.3) | 45.5 (±18.8) | p=0.0357 |
Abscess site and size
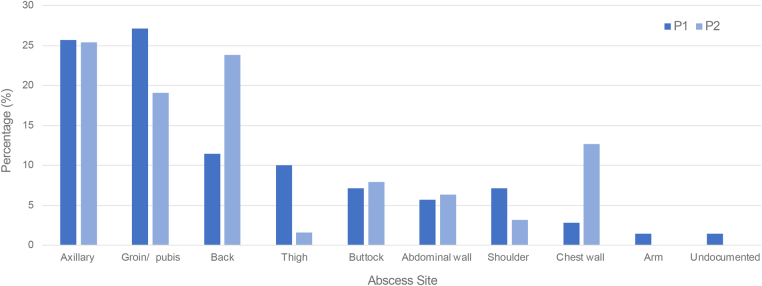
Patients presented with a range of abscess sizes and anatomical locations (Figure 1). The most common anatomical site in P1 was groin/pubis (n=19, 27.1%), followed by the axilla (n=18, 25.7%). In P2, the axilla was the most common site (n=16, 25.4%), followed by the back (n=15, 23.8%) (Figure 1).
Figure 1 .
Anatomical location of abscesses included in the study between P1 and P2.
There was no significant difference between mean abscess size between P1 and P2 (4.12cm±2.75 vs 4.48cm±2.88; p=0.598) or between those managed under GA vs LA (4.74cm±3.05 vs 4.19cm±2.75; p=0.440).
Operating surgeon
I&D was performed most commonly by a junior trainee in both cohorts (Table 4), In P2, 19.0% (n=12) of the procedures were performed by an FY1 (foundation year 1) under supervision.
Table 4 .
Grade of surgeon performing I&D in P1 and P2
| Operating Surgeon | P1 | P2 | |
|---|---|---|---|
| n=70 (%) | n=63 (%) | ||
| Junior trainee | FY1 | 0 (0) | 12 (19.1) |
| SHO | 58 (82.9) | 34 (54.0) | |
| Senior trainee | SpR | 8 (11.4) | 14 (22.2) |
| Consultant | 3 (4.29) | 2 (3.17) | |
| Not documented | 1 (1.43) | 1 (1.59) | |
FY1 = foundation year 1; I&D = incision and drainage; SHO = senior house officer; SpR = specialist registrar
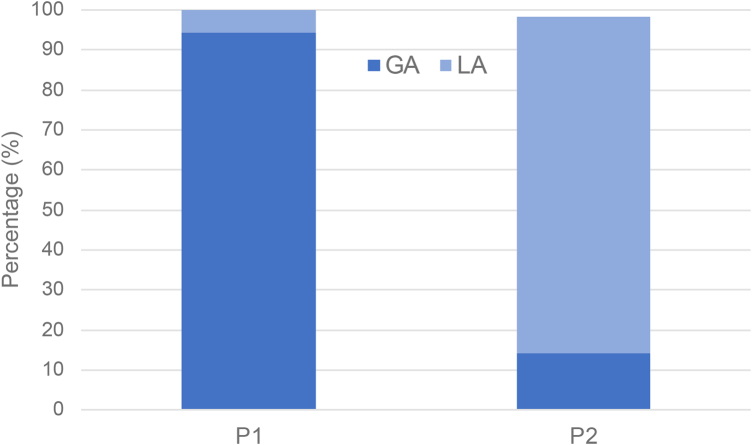
Anaesthetic choice
In P1, 94.3% of procedures (n=66) were performed under GA compared with 14.3% (n=9) in P2 (Figure 2). Following the intervention, significantly more procedures were performed under LA (n=53; 84.1% after intervention vs n=4; 5.7% before intervention p<0.0001). There was one reoperation in the P2 cohort. A 3cm abdominal wall abscess was unsuccessfully drained under LA and required I&D under GA the following day due to worsening cellulitis.
Figure 2 .
Use of LA versus GA in P1 and P2. GA = general anaesthesia; LA = local anaesthetia
Wound packing
In P1, corrugated drains were inserted for two groin and one thigh abscess. Across both cohorts, wound packing was used in 78.2% (n=104); however, the use of packing was significantly lower after the intervention in P2 (n=43, 68.3% vs n=61, 87.1%; p=0.00473).
Antibiotic use
Of the patients in P1 and P2, 67.1% (n=47) and 63.5% (n=40), respectively, did not receive antibiotic therapy following incision and drainage. There was no significant difference in antibiotic use between P1 and P2 (n=22, 31.4% vs n=23, 36.5%; p=0.623). If a patient did receive antibiotics, flucloxacillin was most commonly used (n=16, 35.6%).
Discharge
There was a higher incidence of same-day discharge in P2 versus P1 (n=44, 62.7% vs n=55, 87.3%; p=0.00164).
Follow-up
Follow-up data were collected for 122 patients (91.7%). In total, 11 patients (18.6%) in P1 and 2 patients (3.33%) in P2 were lost to follow-up and excluded from the follow-up analysis (Table 5).
Table 5 .
Comparison of the mean number of follow-up appointments between P1 and P2
| Variable | Mean (SD) | p-value | |
|---|---|---|---|
| P1 n=59 |
P2 n=61 |
||
| Number of follow-up appointments | 7.46 (±7.55) | 5.11 (±6.45) | 0.0731 |
Across both cohorts, 70.7% (n=94) of patients accessed follow-up appointments at community or secondary healthcare facilities following their I&D procedure. A total of 19% (n=12) of patients in P2 engaged with their GP telephone appointment service. One patient re-presented following incision and drainage of the same abscess in P1.
Wound healing
The surrogate endpoints for wound healing were analysed (Table 5). Follow-up data were obtained, and there was no significant difference between the mean number of follow-up appointments in P1 and P2 following I&D (7.46, vs 5.11; p=0.0731). There was no significant difference between the number of patients who attended after 30 days for reoperation (n=14, vs n=14; p=0.921). Of these 14 patients in P1, all were performed under GA. In P2, I&D was performed for one patient under GA and 13 patients under LA. There was no significant difference between the age of these patients in P1 and P2 (n=48.1 years vs 51.6 years; p=0.577). Sensitivity analysis of the abscess size found that the average size in the 14 patients with P1 was significantly smaller than that of the 14 patients in P2 (3.29cm vs 6.35cm; p=0.0218).
Discussion
This study demonstrates a significant shift in the management of simple subcutaneous abscesses in a single centre following COVID-19 RCS England recommendations.10 These data suggest that performing I&D of subcutaneous abscesses under LA does not affect surrogate outcomes of wound healing. NHS guidance to primary care service providers during the COVID-19 pandemic discouraged the use of face-to-face consultations and encouraged the increased utilisation of telephone or video consultations.12 In keeping with this guidance, 19% (n=12) of patients in P2 engaged with the telephone appointment service. Following the intervention there were significantly fewer overnight hospital admissions and a significant reduction in the use of wound packing.
A limitation of the study is the use of surrogate outcomes for wound healing; average number follow-up appointments (indication of nonhealing) and re-presentation (indication of recurrence). However, re-presentation to primary and secondary care during the pandemic for well, ambulatory patients was discouraged to reduce the chances of virus spread. This removed the possibility of using exact measures such as rate of wound healing as endpoints.
A sensitivity analysis was performed to determine whether there was a delay in wound healing or recurrence due to the abscess size and choice of anaesthetic. This analysis supports the use of LA for subcutaneous abscess I&D because the abscess size in patients requiring ongoing management beyond 30 days was significantly larger in P2 (92.9%). This may be because more abscesses were being treated initially with antibiotics in the community and only the more severe (size being the measure of implied severity) were referred to tertiary care.
There was a significant difference in the mean patient age, with a higher mean age in the P2 cohort. The availability of access to healthcare during the follow-up periods was not equal across the two cohorts given COVID-19 restrictions in P2. In addition, the cohorts were not matched in this retrospective study, a key consideration when interpreting these findings.
In the study centre, all I&D procedures were performed under GA in CEPOD theatres, and those under LA in the SAU. Although the exact financial burden of abscess management is unknown, there are several economic and sustainability implications of performing I&D under LA compared with GA. There is likely to be a reduction in the cost of anaesthetic agents, equipment, and anaesthetist and theatre staff time. A reduced duration of inpatient stay until discharge was demonstrated in P2 of this patient cohort. This was likely due to a reduction in the number of abscesses retuning for treatment the following day due to CEPOD theatre capacity.
There is an indication in the data that packing of abscess cavities may not be required. Use of recurrent packing varies across the UK,9 but the clinical significance of this remains unknown. In perianal abscesses, the results of the PPAC2 trial should provide more guidance on the value of recurrent packing. However, the pathophysiology of perianal abscesses varies significantly; as such, this translation to nonperianal abscesses may not be as simple as expected.13
Given the retrospective study design, patient-reported outcomes were not collected. Patient opinion on the use of local versus general anaesthetic will be vital to fully assess the optimum anaesthetic choice for management of subcutaneous abscesses and this is likely to vary from patient to patient. For example, patients may choose to tolerate a higher level of pain or reduction in cosmetic outcome accepting that this may result in them receiving quicker treatment. This has implications for both consent and the allocation of resources. Optimisation of LA protocols could reduce burden on CEPOD theatres but the clinical and patient reported outcomes need to be fully assessed. Patient reported outcomes and the health economics of anaesthetic choice should be included in any future prospective study.
Conclusion
Drainage of simple subcutaneous abscess under 5cm in diameter is safe under LA, with no significant difference in surrogate endpoints of wound healing observed in this patient cohort. This study has several implications for funders given the likely cost benefits of optimising management of this pathology under LA protocols. Future work should explore patient-reported outcomes, including pain management, cosmesis as well as the cost and sustainability implications of a change in this common procedure. A robust patient and public involvement strategy and a formal health economics and sustainability evaluation are required to design to facilitate any future implementation of guidelines.
Sources of funding
This study was supported by the National Institute for Health Research (NIHR) infrastructure at the Leeds Teaching Hospital Trust and the University of Leeds. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
References
- 1.Cutaneous abscess, DermNet NZ. https://www.dermnetnz.org/topics/cutaneous-abscess/ (cited February 2023).
- 2.Stevens DL, Bisno AL, Chambers HFet al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin Infect Dis 2014; 59: e10–e52. [DOI] [PubMed] [Google Scholar]
- 3.Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med 2008; 168: 1585–1591. [DOI] [PubMed] [Google Scholar]
- 4.Gottlieb M, Peksa GD. Comparison of the loop technique with incision and drainage for soft tissue abscesses: a systematic review and meta-analysis. Am J Emerg Med 2018; 36: 128–133. [DOI] [PubMed] [Google Scholar]
- 5.https://cks.nice.org.uk/boils-carbuncles-and-staphylococcal-carriage#!management Boils, carbuncles, and staphylococcal carriage – NICE CKS. (cited February 2023).
- 6.O’Bright NE, Miller JE. Packing versus non-packing outcomes for abscesses after incision and drainage. J Okla State Med Assoc 2017; 110: 78–79. [PMC free article] [PubMed] [Google Scholar]
- 7.Wang W, Chen W, Liu Yet al. Antibiotics for uncomplicated skin abscesses: systematic review and network meta-analysis. BMJ Open 2018; 8: e020991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poulton T, Hogston SP, Bolton WSet al. Anaesthetic management of subcutaneous abscesses: current status. Br J Anaesth 2020; 125: e227–e229. [DOI] [PubMed] [Google Scholar]
- 9.Thomas O, Ramsay A, Yiasemidou Met al. The surgical management of cutaneous abscesses: a UK cross-sectional survey. Ann Med Surg (Lond) 2020; 60: 654–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.sitecore\jpjadwat@rcseng.ac.uk. COVID-19: Good Practice for Surgeons and Surgical Teams. Royal College of Surgeons. https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/covid-19-good-practice-for-surgeons-and-surgical-teams/ (cited February 2023).
- 11.COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gray DP, Sidaway-Lee K, Harding A, Evans P. Reduction in face-to-face GP consultations. Br J Gen Pract 2020; 70: 328–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Northwestern Research Collaborative. Packing of Perianal Abscess Cavities (PPAC2). 2020. https://clinicaltrials.gov/ct2/show/NCT03315169 (cited February 2023).