Abstract
Totally minimally invasive oesophagectomy (TMIE) has been utilised to reduce respiratory and cardiac complications, offering favourable clinical and oncological outcomes. A 62-year-old male patient underwent two-stage TMIE for a Siewert type I tumour. During thoracoscopic oesophageal mobilisation and lymphadenectomy, a 10-mm bone-like mass was recognised and dissected along the subcarinal nodes, revealing a 2–3mm opening on the inferomedial aspect of the right main bronchus. The airway opening was repaired after conversion. This is the first report of an accessory cardiac bronchus encountered during oesophagectomy. Recognition of its characteristic position and features may result in early diagnosis and avoidance of a potentially lethal injury.
Keywords: Totally minimally invasive oesophagectomy, Accessory cardiac bronchus, Thoracoscopy
Background
Oesophagectomy is the mainstay of surgical treatment for local and locoregional disease. However, it has been associated with significant rates of postoperative morbidity and mortality. Minimally invasive oesophagectomy is on the rise, offering reduced respiratory complications, shorter length of hospital stay and favourable clinical and oncological outcomes compared with standardised open oesophagectomy, becoming the new norm for the treatment of oesophageal and gastro-oesophageal tumours.
Case history
Herein, we present an extremely rare and interesting case of a 62-year-old male patient who underwent minimally invasive two-stage oesophagectomy (Ivor Lewis) for a Siewert I oesophageal tumour. The operation consisted of a laparoscopic abdominal phase in the supine position, with abdominal D2-lymphadenectomy and construction of the gastric conduit. Following that, the patient was turned to the prone position with the operating table broken at the mid-chest level, for the thoracoscopic thoracic part of the procedure.
At this stage, a double-lumen endotracheal tube was utilised to block the right bronchus and achieve one-lung ventilation through the left lung. Three 10-mm ports were placed under direct vision: one posterior to the angle of the scapula at the fifth intercostal space (camera port); one at the posterior edge of the scapula at the third intercostal space (operating port); and one at the eighth intercostal space posterior to the scapular line (operating port).
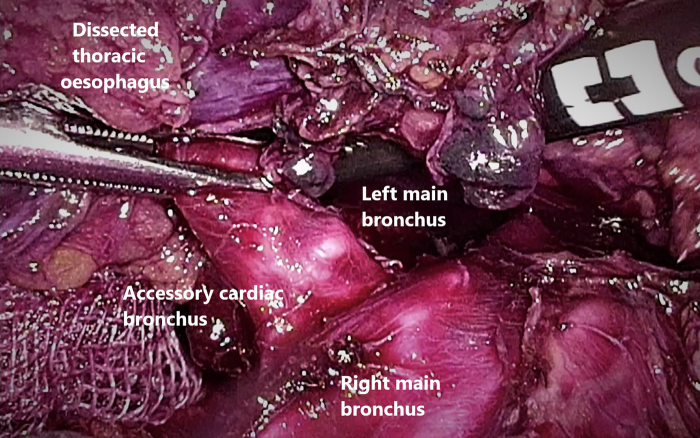
Routine oesophageal mobilisation with en-block lymphadenectomy of the peri-oesophageal, para-aortic and subcarinal nodes was performed. During dissection of the thoracic oesophagus a 10-mm long, cartilage-like semi-mobile mass was recognised within the subcarinal area lymph nodes and was dissected with this lymph node group (Figure 1). At this time, the 10-mm port site at the eighth intercostal space was converted to a 3-cm mini-thoracotomy for specimen extraction. Intraoperatively, blood-stained fluid was subsequently observed through the endotracheal tube by the anaesthetist.
Figure 1 .
View of the operating field during the thoracoscopic oesophagectomy. The right main bronchus is blocked (one lung ventilation) and the bone-like mass can be recognised.
Thoracotomy was concluded, conversion to open thoracotomy was decided upon and a right posterolateral thoracotomy was performed on the seventh intercostal space. The airway defect was sutured with interrupted 4/0 Prolene sutures and further buttressed with an intercostal pleural patch. An intraoperative air-leak test was negative; the operation was concluded with construction of the oesophagogastric anastomosis using a circular stapler. The lung was inflated and checked again, and a chest tube was placed before closure.
However, surgical repair did not offer complete sealing of the airway opening and on postoperative day 10 an air leak was noticed via the chest drain, formatting a tracheopleural fistula. The patient was treated conservatively with antibiotics, and the chest drain remained for 20 days. Liquids were commenced on postoperative day 4, and a soft diet was started the following day. Histology confirmed a pT2N1 oesophageal adenocarcinoma and the patient was planned for postoperative chemotherapy.
A subsequently reconstructed three-dimensional image of the tracheobronchial tree based on the preoperative computed tomography (CT) scan revealed the accessory cardiac bronchus (ACB) (Figure 2). Careful intraoperative inspection of the operating field revealed a 2–3-mm opening on the inferomedial aspect of the right main bronchus about 1cm from the tracheal bifurcation, at the area of the subcarinal nodes and the dissected mass.
Figure 2 .
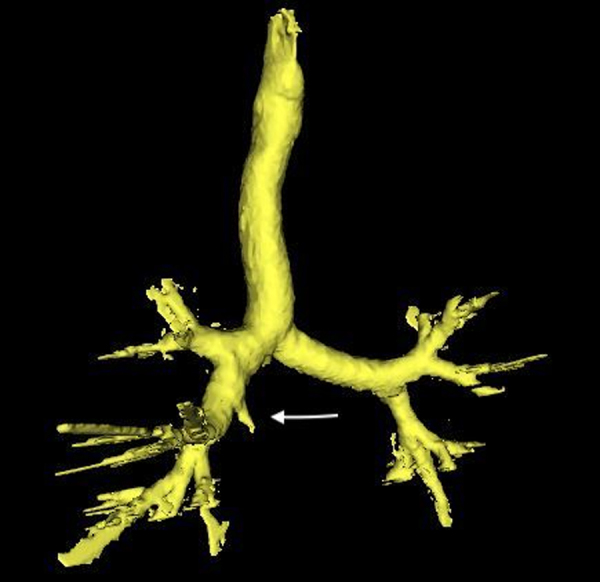
Accessory cardiac bronchus originating from the right main bronchus
Discussion
ACB is a congenital anatomical abnormality of the bronchial tree, originating from the medial aspect of the right main stem bronchus or, in some cases, from the bronchus intermedius. Typically, it is an isolated finding and is very rare, especially in adults, with an incidence of 0.07%–0.5%.1 Is thought to result from abnormal morphology of the cardiac bud during weeks 4–6 of embryonic development that failed to involute during gestation.2
According to Mangiulea et al,3 there are three reported variations depending on the presence of accessory lung tissue: a short type with a blind extremity; an accessory-lobed type with small, undeveloped lobules; and a long diverticular type without bronchial or alveolar arborisation. It has been observed that ACB heads medially and caudally towards the heart, most frequently ending in a blind pouch.2 ACBs are usually asymptomatic, but according to Unlu et al4 there may be associated cough, haemoptysis, recurrent respiratory infections, empyema or malignancy.
Blind ACBs can be short type or long type. Cases with an ACB long type, >1cm, are more susceptible to complications.4
Totally minimally invasive oesophagectomy (TMIE) has been utilised to reduce respiratory and cardiac complications associated with open oesophagectomy, while offering favourable clinical and oncological outcomes.5 To our knowledge, this is the first reported case of such an anomaly encountered during TMIE for oesophageal cancer. Our patient was treated for a Siewert type I gastro-oesophageal adenocarcinoma. The lesion was recognised upon the right main bronchus; however, because of its size, locoregional lymph node disease and previously administered chemotherapy, it was considered as a metastatic node.
Conclusions
ACB is unrecognisable on plain radiography. CT features of ACB are frequently missed because the anomaly is rare and literature describing the process is scarce.3 Radiologists need to recognise and comprehensively report this anomaly. Because the abnormality can be encountered by thoracic and oesophageal surgeons, recognition of its characteristic position and features may result in improved diagnosis and avoidance of a potentially lethal complication, as in our case.
References
- 1.Volpe A, Bozzetto S, Baraldi Eet al. Accessory-lobed accessory cardiac bronchus: presentation and treatment in a pediatric patient. Pediatr Pulmonol 2017; 52: E85–E87. [DOI] [PubMed] [Google Scholar]
- 2.Ghaye B, Collard P, Pierard Set al. CT presentation of left-sided accessory cardiac bronchus. Diagn Interv Imaging 2018; 99: 827–828. [DOI] [PubMed] [Google Scholar]
- 3.Mangiulea VG, Stinghe RV. The accessory cardiac bronchus. bronchologic aspect and review of the literature. Dis Chest 1968; 54: 433–436. [DOI] [PubMed] [Google Scholar]
- 4.Unlu EN, Yilmaz Aydin L, Bakirci Set al. Prevalence of the accessory cardiac bronchus on multidetector computed tomography: evaluation and proposed classification. J Thorac Imaging 2016; 31: 312–317. [DOI] [PubMed] [Google Scholar]
- 5.Ising MS, Smith SA, Trivedi JRet al. Minimally invasive esophagectomy Is associated with superior survival compared to open surgery. Am Surg 2022; 23: 31348221078962. [DOI] [PubMed] [Google Scholar]