Abstract
Background
The oral Janus kinase (JAK) inhibitor baricitinib has demonstrated efficacy for severe alopecia areata (AA) over 36 weeks. There are limited data on the longer-term treatment of AA.
Objective
The aim of this study was to evaluate the efficacy and safety of baricitinib for AA in adults with ≥50% scalp hair loss through 52 weeks of continuous therapy in two phase III trials (BRAVE-AA1 and BRAVE-AA2).
Methods
Patients randomized to baricitinib at baseline in BRAVE-AA1 (N = 465) and BRAVE-AA2 (N = 390) retained their treatment allocation through Week 52. Efficacy outcomes included the proportion of patients achieving a Severity of Alopecia Tool (SALT) score ≤ 20 (≤ 20% scalp hair loss). Data were censored after permanent treatment discontinuation or if collected remotely due to the coronavirus disease 2019 (COVID-19) pandemic.
Results
Response rates for hair regrowth increased over the 52-week period. Of patients treated with baricitinib 4 mg and 2 mg, respectively, 40.9% and 21.2% in BRAVE-AA1 and 36.8% and 24.4% in BRAVE-AA2 achieved a SALT score ≤ 20 at Week 52. The most frequent treatment-emergent adverse events included upper respiratory tract infection, headache, nasopharyngitis, acne, urinary tract infection, creatine phosphokinase elevation, and COVID-19 infection.
Limitation
There were no comparisons with placebo.
Conclusion
Efficacy of baricitinib for adults with severe AA continuously improved over 52 weeks, indicating that long-term treatment may be necessary to observe maximum clinical benefit. There were no new safety signals.
ClinicalTrials Registration
ClinicalTrials.gov NCT03570749 and NCT03899259.
Video abstract
Efficacy and Safety of Baricitinib in Patients with Severe Alopecia Areata: Week-52 Results from BRAVE-AA1 and BRAVE-AA2
Supplementary Information
The online version contains supplementary material available at 10.1007/s40257-023-00764-w.
Plain Language Summary
Alopecia areata (AA) is an autoimmune disease that causes patchy hair loss on the scalp, face, and body. Baricitinib is a Janus kinase inhibitor that is approved to treat AA in several countries, based on results from two studies, BRAVE-AA1 and BRAVE-AA2. In these studies, adults with at least 50% scalp hair loss were treated with baricitinib for 36 weeks. Long-term therapy is important in AA, and hair regrowth can take longer in some patients with severe disease. Therefore, we assessed outcomes from a longer course of therapy. In this study, we report the results after 52 weeks of continuous treatment with baricitinib 4 mg or 2 mg in 465 patients in BRAVE-AA1 and 390 patients BRAVE-AA2. The goal was to reduce scalp hair loss to 20% or less by Week 52. In BRAVE-AA1, 40.9% of patients who took baricitinib 4 mg and 21.2% of patients who took baricitinib 2 mg had 20% or less missing scalp hair by Week 52. Similarly, in BRAVE-AA2, 36.8% of patients who took baricitinib 4 mg and 24.4% of patients who took baricitinib 2 mg had 20% or less missing scalp hair by Week 52. The most common adverse effects that were reported during the study period were upper respiratory tract infection, headache, nasopharyngitis, acne, urinary tract infection, creatine phosphokinase elevation, and coronavirus disease 2019 (COVID-19) infection. The results of longer-term treatment indicate that hair regrowth continues to improve without any new safety concerns for adults with severe AA taking baricitinib.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40257-023-00764-w.
| Digital Features for this article can be found at 10.6084/m9.figshare.22129661. |
Key Points
| The oral Janus kinase inhibitor baricitinib has demonstrated efficacy for adults with severe alopecia areata (≥ 50% scalp hair loss) over 36 weeks. |
| In two phase III trials, efficacy of baricitinib for severe alopecia areata continued to improve over 52 weeks. |
Introduction
Alopecia areata (AA) is an autoimmune disorder causing non-scarring hair loss on the scalp, face, and body. Severe AA (≥ 50% scalp hair loss) is unlikely to remit without treatment, with only 3.3–6.2% of patients achieving ≥ 80% scalp hair coverage with placebo in recent 36-week trials [1].
Clinical studies indicate Janus kinase (JAK) inhibitors may interrupt inflammatory pathways that contribute to the immunopathogenesis of AA [2–4]. The oral, selective, and reversible JAK1/JAK2 inhibitor baricitinib is the first FDA-approved treatment for adults with severe AA and is in late-stage development for pediatric patients with severe AA. There are limited data on longer-term outcomes with oral JAK inhibitors in large cohorts of patients with severe AA.
In two phase III randomized trials of adults with severe AA, baricitinib was superior to placebo in hair regrowth over 36 weeks of treatment [1]. Using data from the long-term extension periods of BRAVE-AA1 and BRAVE-AA2, we report the efficacy and safety of baricitinib 4 mg and 2 mg over 52 weeks of continuous therapy.
Methods
Patients and Study Design
BRAVE-AA1 (NCT03570749) and BRAVE-AA2 (NCT03899259) are ongoing, independent, randomized, double-blind, parallel-group, placebo-controlled studies evaluating the efficacy and safety of baricitinib for AA. Eligibility criteria were detailed previously [1]. Patients included adults who had a Severity of Alopecia Tool (SALT) score ≥ 50 (≥ 50% scalp hair loss) and a current AA episode lasting > 6 months to < 8 years without spontaneous improvement (i.e., no more than 10-point SALT score reduction) over the 6 months prior to screening.
The trials had identical design for the first 52 weeks. Patients were randomized 2:2:3 to receive once-daily oral placebo, baricitinib 2 mg, or baricitinib 4 mg for 36 weeks. All patients who completed the 36-week placebo-controlled period entered an extension phase, for up to 68 weeks of additional treatment. At Week 36, placebo non-responders (SALT score > 20) were rescued to baricitinib, while placebo responders (SALT score ≤ 20) remained on placebo through Week 52. The present analyses focus on patients randomized to either of the baricitinib doses at baseline, who retained their treatment allocation through Week 52 regardless of response at Week 36. Patients and investigators remained blinded to treatment assignment.
First and last patients, respectively, entered treatment in March 2019 and June 2020 in BRAVE-AA1 and July 2019 and May 2020 in BRAVE-AA2. The trials were conducted in accordance with the ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines. The research protocols were approved by each center’s Institutional Review Board (IRB) or Ethics Committee. All patients provided written informed consent.
Endpoints
Efficacy outcomes at 52 weeks included the proportion of patients achieving SALT score ≤ 20 (≤ 20% scalp hair loss), which is considered a clinically meaningful outcome for patients with ≥ 50% scalp hair loss at baseline [5]. The SALT score is a weighted sum of percentage hair loss in four areas of the scalp, ranging from 0 (no hair loss) to 100 (complete hair loss) [6]. Other endpoints included the percentage change from baseline in SALT score, the proportions of patients achieving ≥ 50% and ≥ 90% improvements from baseline in SALT score (SALT50 and SALT90, respectively), and the proportion achieving a SALT score ≤ 10 (≤ 10% scalp hair loss). Also assessed were the proportion of patients achieving Clinician-Reported Outcome (ClinRO) Measure for Eyebrow Hair Loss™ 0 or 1 (full coverage or minimal gaps) with ≥ 2-point improvement from baseline among patients with baseline scores of 2 or 3 (significant gaps or no notable eyebrows) and the proportion achieving ClinRO Measure for Eyelash Hair Loss™ 0 or 1 (no or minimal gaps) with ≥ 2-point improvement from baseline among patients with baseline scores of 2 or 3 (significant gaps or no notable eyelashes) [7].
Safety assessments included adverse events (AEs), serious AEs (SAEs), and clinical laboratory tests. An independent data and safety monitoring committee periodically reviewed unblinded efficacy and safety data. Deaths, major adverse cardiovascular events (MACEs), and arterial (ATEs) and venous thromboembolic events (VTEs) were adjudicated by an independent blinded clinical endpoint committee.
Statistical Analysis
Efficacy analysis included all patients randomized to baricitinib at baseline (intention-to-treat analysis). Data were censored after permanent study drug discontinuation or if collected remotely due to the coronavirus disease 2019 (COVID-19) pandemic. For categorical outcomes, non-responder imputation was applied to missing and censored data. For continuous outcomes, missing and censored data were imputed with modified last observation carried forward, using the most recent non-missing post-baseline assessment. Results from these prespecified analyses are presented below. Placebo-controlled outcomes at Week 36 were previously reported with both the prespecified analyses and with multiple imputation applied to missing data [1]; Week-52 results using multiple imputation are available in the electronic supplementary material (ESM) for comparison with the Week 36 results. Differences in outcomes between baricitinib doses were not analyzed.
Safety analysis included all patients randomized to baricitinib at baseline who received one or more doses of study drug and who did not discontinue for the reason ‘lost to follow-up’ at first post-baseline visit. Safety analysis included data collected through 23 August 2021 in BRAVE-AA1 and 30 August 2021 in BRAVE-AA2. Safety findings thus reflect data collected beyond 52 weeks, with up to 128 weeks in BRAVE-AA1 and 108 weeks in BRAVE-AA2. Incidence rates (IRs) were calculated based on time at risk for a patient with an event.
Results
Patients
Among patients randomized at baseline to baricitinib 4 mg and 2 mg, respectively, 252/281 (89.7%) and 163/184 (88.6%) in BRAVE-AA1 and 209/234 (89.3%) and 134/156 (85.9%) in BRAVE-AA2 completed 52 weeks of study treatment (ESM Fig. S1). The most common reasons for discontinuation in BRAVE-AA1 and BRAVE-AA2 were patient withdrawal (n = 21 and n = 21, respectively), AEs (n = 8 and n = 11, respectively), and loss to follow-up (n = 11 and n = 9, respectively).
Baseline characteristics were comparable across baricitinib groups in both trials (Table 1). For patients randomized to baricitinib in BRAVE-AA1 and BRAVE-AA2, respectively, mean age was 37.0 and 38.4 years, 58.9% and 63.3% were female, and mean SALT scores at baseline were 85.9 and 85.1. For ClinRO Measures for Eyebrow Hair Loss and Eyelash Hair Loss, respectively, 69.7% and 59.8% in BRAVE-AA1 and 67.9% and 58.7% in BRAVE-AA2 had scores of 2 or 3 (significant gaps or no notable hair) at baseline.
Table 1.
Baseline demographics and clinical characteristics
| Characteristic | BRAVE-AA1 | BRAVE-AA2 | ||
|---|---|---|---|---|
| Baricitinib 2 mg [N = 184] | Baricitinib 4 mg [N = 281] | Baricitinib 2 mg [N = 156] | Baricitinib 4 mg [N = 234] | |
| Age, years [mean (SD)] | 38.0 (12.8) | 36.3 (13.3) | 39.0 (13.0) | 38.0 (12.7) |
| Female | 109 (59.2) | 165 (58.7) | 103 (66.0) | 144 (61.5) |
| Racea | ||||
| White | 93 (50.8) | 123 (43.9) | 92 (59.0) | 144 (61.5) |
| Asian | 76 (41.5) | 114 (40.7) | 49 (31.4) | 67 (28.6) |
| Black or African American | 7 (3.8) | 28 (10.0) | 12 (7.7) | 18 (7.7) |
| Other | 7 (3.8) | 15 (5.4) | 3 (1.9) | 5 (2.1) |
| Geographic regionb | ||||
| North America | 102 (55.4) | 153 (54.4) | 54 (34.6) | 82 (35.0) |
| Asia | 70 (38.0) | 107 (38.1) | 42 (26.9) | 63 (26.9) |
| Rest of world | 12 (6.5) | 21 (7.5) | 60 (38.5) | 89 (38.0) |
| Duration since AA onset, years [mean (SD)] | 12.1 (9.8) | 11.8 (11.1) | 13.1 (11.8) | 11.9 (11.1) |
| Duration of current episode of AA, years [mean (SD)] | 3.9 (4.7) | 3.5 (3.4) | 4.4 (6.1) | 3.9 (3.4) |
| < 4 years | 127 (69.0) | 189 (67.3) | 103 (66.0) | 140 (59.8) |
| ≥ 4 years | 57 (31.0) | 92 (32.7) | 53 (34.0) | 94 (40.2) |
| Proportion of patients with alopecia universalisc | 83 (45.1) | 127 (45.2) | 70 (44.9) | 111 (47.4) |
| Proportion of patients with atopic backgroundd | 67 (36.4) | 97 (34.5) | 63 (40.4) | 87 (37.2) |
| Weight, kg [mean (SD)] | 74.3 (17.8) | 74.7 (17.0) | 72.3 (16.1) | 74.0 (15.7) |
| Body mass index [mean (SD)] | 26.0 (5.4) | 26.4 (5.5) | 26.2 (5.1) | 26.4 (4.9) |
| SALT score [mean (SD)] | 86.8 (18.0) | 85.3 (18.2) | 85.6 (18.1) | 84.8 (18.1) |
| SALT score [median] | 99.0 | 96.0 | 97.0 | 95.0 |
| Severity | ||||
| Severe (SALT score 50–94) | 77 (41.8) | 133 (47.3) | 70 (44.9) | 115 (49.1) |
| Very severe (SALT score 95–100) | 107 (58.2) | 148 (52.7) | 86 (55.1) | 119 (50.9) |
| ClinRO Measure for Eyebrow Hair Loss™ score of 2 or 3e | 136 (73.9) | 188 (67.6) | 104 (66.7) | 161 (69.1) |
| ClinRO Measure for Eyelash Hair Loss™ score of 2 or 3e | 111 (60.3) | 167 (60.1) | 89 (57.1) | 140 (60.1) |
Data are expressed as n (%) unless otherwise specified
Percentages are for non-missing values
AA alopecia areata, ClinRO clinician-reported outcome, n number of patients in the specified category, N total population size, SALT Severity of Alopecia Tool, SD standard deviation
a‘Other’ includes American Indian or Alaska Native, Native Hawaiian or other Pacific Islander, or multiple races
bGeographic regions for BRAVE-AA1 include Asia (South Korea) and rest of world (Mexico), and for BRAVE-AA2 include Asia (South Korea, Japan, Taiwan, China) and rest of world (Israel, Australia, Brazil, Argentina). North America in both studies includes the United States
cDiagnosis of alopecia universalis was according to the investigator’s assessment
dAtopic background is defined as medical history or current atopic dermatitis, allergic rhinitis, allergic conjunctivitis, or allergic asthma
eA ClinRO score of 2 indicates significant gaps in eyebrow(s)/eyelashes, and a score of 3 indicates no notable eyebrow(s)/eyelashes
Efficacy
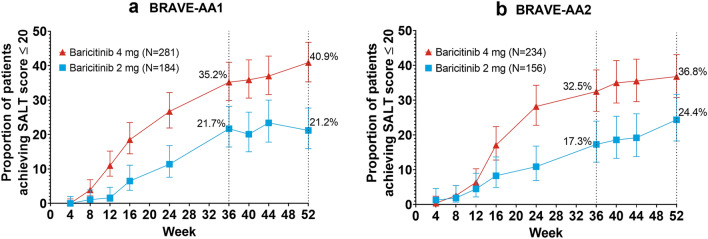
The proportions of patients achieving SALT score ≤ 20 continuously increased over the treatment period, with response rates for patients treated with baricitinib 4 mg and 2 mg, respectively, reaching 40.9% and 21.2% in BRAVE-AA1 and 36.8% and 24.4% in BRAVE-AA2 at Week 52 (Fig. 1, ESM Table S1). Among patients with severe baseline disease (SALT score 50–94) treated with baricitinib 4 mg and 2 mg, respectively, a SALT score ≤ 20 was achieved in 55.6% and 36.4% in BRAVE-AA1 and 46.1% and 35.7% in BRAVE-AA2. Among patients with very severe disease at baseline (SALT score 95–100) in the baricitinib 4 mg and 2 mg groups, respectively, 27.7% and 10.3% in BRAVE-AA1 and 27.7% and 15.1% in BRAVE-AA2 achieved a SALT score ≤20.
Fig. 1.
Proportions of patients achieving SALT score ≤20 through Week 52 in a BRAVE-AA1 and b BRAVE-AA2. A SALT score ≤20 indicates ≤20% scalp hair loss. Bars represent 95% confidence intervals. Non-responder imputation was applied to missing data (prespecified analysis). Week-36 data points reflect results from the placebo-controlled period. SALT Severity of Alopecia Tool
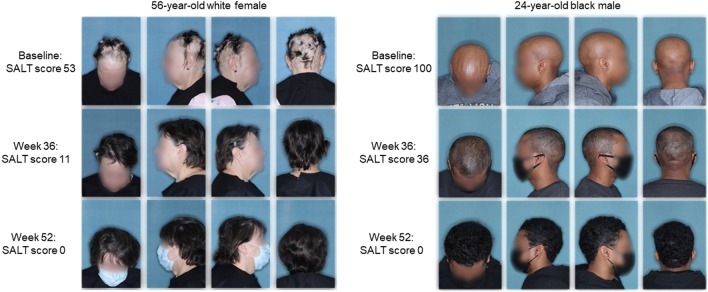
In the baricitinib 4 mg and 2 mg groups, respectively, 29.9% and 14.1% in BRAVE-AA1 and 27.8% and 16.7% in BRAVE-AA2 achieved a SALT score ≤ 10 (ESM Table S1). With the baricitinib 4 mg and 2 mg doses, respectively, SALT50 was achieved at Week 52 in 52.0% and 31.0% in BRAVE-AA1 and 52.6% and 37.2% in BRAVE-AA2; 28.5% and 11.4% in BRAVE-AA1 and 26.1% and 14.1% in BRAVE-AA2 achieved SALT90 at Week 52 (ESM Table S1). Representative photographs of patients who responded to baricitinib in BRAVE-AA1 are presented in Fig. 2.
Fig. 2.
Clinical photographs of patients with alopecia areata at baseline and after 36 weeks and 52 weeks of treatment with baricitinib 4 mg in BRAVE-AA1. SALT scores indicate percentage of scalp hair loss as assessed by the investigator.
Patient images ©Eli Lilly and Company. SALT Severity of Alopecia Tool
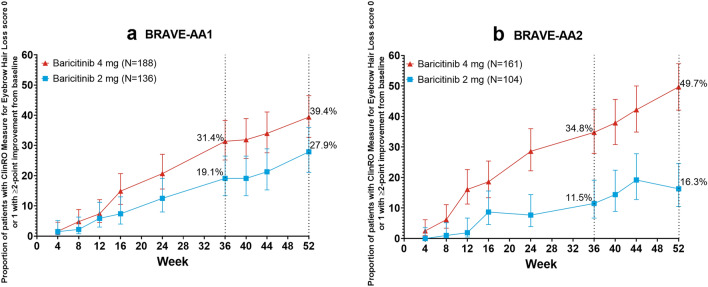
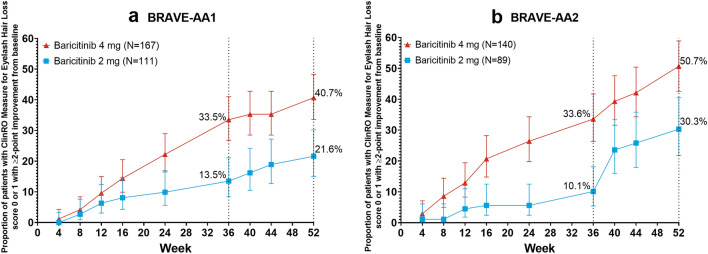
Eyebrow and eyelash response rates also increased over the 52-week period. Among patients with ClinRO Measure for Eyebrow Hair Loss baseline scores of 2 or 3 who were treated with baricitinib 4 mg and 2 mg, respectively, 39.4% and 27.9% in BRAVE-AA1 and 49.7% and 16.3% in BRAVE-AA2 improved ≥ 2 points and scored 0 or 1 at Week 52 (Fig. 3, ESM Table S1). Of those with ClinRO Measure for Eyelash Hair Loss baseline scores of 2 or 3 in the baricitinib 4 mg and 2 mg groups, respectively, 40.7% and 21.6% in BRAVE-AA1 and 50.7% and 30.3% in BRAVE-AA2 had ≥ 2-point improvements and achieved scores of 0 or 1 at Week 52 (Fig. 4, ESM Table S1).
Fig. 3.
Proportion of patients achieving ClinRO Measure for Eyebrow Hair LossTM 0 or 1 with ≥2-point improvement from baseline through Week 52 among patients with a score of ≥ 2 at baseline in a BRAVE-AA1 and b BRAVE-AA2. A ClinRO score of 0 indicates full coverage and a score of 1 indicates minimal gaps in eyebrows. Bars represent 95% confidence intervals. Non-responder imputation was applied to missing data (prespecified analysis). Week-36 data points reflect results from the placebo-controlled period. ClinRO Clinician-Reported Outcome
Fig. 4.
Proportion of patients achieving ClinRO Measure for Eyelash Hair LossTM 0 or 1 with ≥ 2-point improvement from baseline through Week 52 among patients with a score of ≥ 2 at baseline in a BRAVE-AA1 and b BRAVE-AA2. A ClinRO score of 0 indicates full coverage and a score of 1 indicates minimal gaps in eyelashes. Bars represent 95% confidence intervals. Non-responder imputation was applied to missing data (prespecified analysis). Week-36 data points reflect results from the placebo-controlled period. ClinRO Clinician-Reported Outcome
Results of the post hoc analysis of efficacy outcomes using multiple imputation for missing data are reported in ESM Figs. S2–S4 and ESM Table S2.
Safety
A total of 280 (patient-years exposure [PYE] = 385.5) and 183 (PYE = 197.9) patients in BRAVE-AA1 and 233 (PYE = 284.8) and 155 (PYE = 168.7) patients in BRAVE-AA2 were exposed to baricitinib 4 mg and 2 mg, respectively. Among patients in the baricitinib 4 mg and 2 mg groups, respectively, treatment-emergent AEs (TEAEs) were reported in 69.6% (IR = 110.8) and 58.5% (IR = 94.5) in BRAVE-AA1 and 77.3% (IR = 159.1) and 74.2% (IR = 168.7) in BRAVE-AA2 (Table 2). Most TEAEs were mild or moderate in severity. The most frequently reported TEAEs were upper respiratory tract infection, headache, nasopharyngitis, acne, urinary tract infection, increased blood creatinine phosphokinase (CPK), and COVID-19 infection (Table 2). There were no patterns in types of SAEs; the most common SAEs were bone fractures due to injury (ESM Table S3). The frequency of discontinuations due to AEs was low and similar across groups (ESM Table S4).
Table 2.
Summary of safety outcomes
| BRAVE-AA1 | BRAVE-AA2 | |||
|---|---|---|---|---|
| Baricitinib 2 mg [N = 183] |
Baricitinib 4 mg [N = 280] |
Baricitinib 2 mg [N = 155] |
Baricitinib 4 mg [N = 233] |
|
| Any TEAE | 107 (58.5) [94.5] | 195 (69.6) [110.8] | 115 (74.2) [168.7] | 180 (77.3) [159.1] |
| TEAE severitya | ||||
| Mild | 59 (32.2) [36.9] | 101 (36.1) [35.6] | 57 (36.8) [45.7] | 90 (38.6) [42.2] |
| Moderate | 43 (23.5) [24.6] | 81 (28.9) [24.4] | 54 (34.8) [39.4] | 73 (31.3) [32.2] |
| Severe | 5 (2.7) [2.4] | 13 (4.6) [3.3] | 4 (2.6) [2.3] | 17 (7.3) [5.9] |
| Serious AE | 5 (2.7) [2.4] | 11 (3.9) [2.8] | 4 (2.6) [2.3] | 13 (5.6) [4.5] |
| Death | 0 | 0 | 0 | 0 |
| AE leading to study drug discontinuation | 4 (2.2) [1.9] | 8 (2.9) [2.0] | 4 (2.6) [2.3] | 10 (4.3) [3.4] |
| TEAEs occurring in ≥ 5% of patients in any group | ||||
| Upper respiratory tract infection | 12 (6.6) [6.0] | 24 (8.6) [6.5] | 17 (11.0) [10.3] | 20 (8.6) [7.2] |
| Headache | 11 (6.0) [5.4] | 18 (6.4) [4.8] | 15 (9.7) [9.0] | 29 (12.4) [10.6] |
| Nasopharyngitis | 13 (7.1) [6.5] | 23 (8.2) [6.2] | 5 (3.2) [2.8] | 20 (8.6) [7.2] |
| Acne | 13 (7.1) [6.5] | 19 (6.8) [5.1] | 9 (5.8) [5.4] | 13 (5.6) [4.6] |
| Urinary tract infection | 5 (2.7) [2.4] | 13 (4.6) [3.4] | 16 (10.3) [9.6] | 14 (6.0) [4.9] |
| Blood creatine phosphokinase increased | 3 (1.6) [1.4] | 26 (9.3) [6.9] | 0 | 8 (3.4) [2.8] |
| COVID-19 infection | 3 (1.6) [1.4] | 6 (2.1) [1.5] | 4 (2.6) [2.3] | 13 (5.6) [4.5] |
| Infectious AEs | ||||
| At least one treatment-emergent infection | 57 (31.1) [35.7] | 111 (39.6) [39.9] | 75 (48.4) [65.5] | 101 (43.3) [49.9] |
| Serious infection | 0 | 0 | 2 (1.3) [1.1] | 4 (1.7) [1.4] |
| Opportunistic infection | 0 | 0 | 0 | 0 |
| Herpes zoster | 2 (1.1) [1.0] | 2 (0.7) [0.5] | 6 (3.9) [3.4] | 8 (3.4) [2.7] |
| Herpes simplex | 1 (0.5) [0.5] | 9 (3.2) [2.3] | 7 (4.5) [4.1] | 4 (1.7) [1.4] |
| Tuberculosis | 0 | 0 | 0 | 0 |
| Infections leading to study treatment discontinuation | 0 | 0 | 1 (0.6) [0.6] | 1 (0.4) [0.3] |
| AEs of special interest | ||||
| Major adverse cardiovascular event | 1 (0.5) [0.5]b | 0 | 0 | 0 |
| Venous thromboembolism | 0 | 0 | 0 | 0 |
| Malignancies other than non-melanoma skin cancer | 0 | 1 (0.4) [0.3]c | 0 | 1 (0.4) [0.3]d |
| Non-melanoma skin cancer | 1 (0.5) [0.5]e | 0 | 0 | 0 |
| Gastrointestinal perforations | 0 | 0 | 0 | 0 |
Data are expressed as n (%) [IR]
AE adverse event, COVID-19 coronavirus disease 2019, IR incidence rate, n number of patients in the specified category, N number of patients in the analysis set, TEAE treatment-emergent adverse event
aPatients with multiple occurrences of the same event are counted under the highest severity
bMyocardial infarction in a patient with multiple risk factors, including current tobacco use, obesity, atrial fibrillation, hypertension, and a history of hypercholesterolemia. This was reported during the placebo-controlled period and occurred after approximately 9 months of treatment (also adjudicated as arterial thromboembolism) [1]
cDuctal carcinoma in situ diagnosed after approximately 10 months of treatment
dB-cell lymphoma diagnosed after approximately 4 months of treatment and reported during the placebo-controlled period
eSquamous cell carcinoma diagnosed after approximately 16 months of treatment
AEs during the 36-week placebo-controlled period have been previously reported [1]. Newly reported herpes zoster infections that occurred after the placebo-controlled period were localized; all patients recovered, and none discontinued. Herpes simplex infections were all mild or moderate and there were no discontinuations. After the placebo-controlled period, serious infections during the extension phase of BRAVE-AA2 included one (0.4%, IR = 0.3) case each of appendicitis, herpes zoster, and COVID-19 with baricitinib 4 mg; all patients recovered, and none discontinued (ESM Table S3). During the extension period of BRAVE-AA2, one (0.4%, IR = 0.3) COVID-19 infection with baricitinib 4 mg led to study discontinuation. No serious infections or infections leading to discontinuation were reported in BRAVE-AA1. Malignancies reported during the trial extension periods included one (0.5%, IR = 0.5) squamous cell carcinoma after 16 months with baricitinib 2 mg, and one (0.4%, IR = 0.3) ductal carcinoma in situ after 10 months with baricitinib 4 mg in BRAVE-AA1; the latter patient discontinued per protocol. No VTEs, opportunistic infections, cases of tuberculosis, gastrointestinal perforations, or deaths were reported in either trial over the observation period (Table 2).
Most laboratory changes were balanced across baricitinib groups in both studies. Increases in CPK, low-density lipoprotein, and high-density lipoprotein were more frequent with the 4 mg dose (Table 3). CPK increases were mostly Common Terminology Criteria for Adverse Events (CTCAE) [8] grade 1 or 2, and there were no cases of rhabdomyolysis. CTCAE grade 4 neutropenia (neutrophils < 0.5 billion/L) was seen in one baricitinib 4 mg patient in the extension period of BRAVE-AA1; the patient recovered and continued the study. During the trial extension periods, thrombocytosis (platelets > 600 billion/L) occurred in one patient with baricitinib 4 mg in BRAVE-AA1 and one patient with baricitinib 2 mg in BRAVE-AA2; both patients recovered and continued the study. Frequencies of hepatic test abnormalities were consistent with those previously reported [1] and were not associated with TEAEs leading to study drug interruption or discontinuation.
Table 3.
Summary of laboratory changes
| BRAVE-AA1 | BRAVE-AA2 | |||
|---|---|---|---|---|
| Baricitinib 2 mg [N = 183] |
Baricitinib 4 mg [N = 280] |
Baricitinib 2 mg [N = 155] |
Baricitinib 4 mg [N = 233] |
|
| Anemia CTCAE grade ≥3 (hemoglobin <4.9 mmol/L) | 0 | 1 (0.4) | 0 | 1 (0.4) |
| Neutrophils CTCAE grade ≥ 3 (< 1.0 billion/L) | 1 (0.6) | 3 (1.1) | 2 (1.3) | 5 (2.2) |
| Lymphocytes CTCAE grade ≥ 3 (< 0.5 billion/L) | 0 | 1 (0.4) | 0 | 2 (0.9) |
| Leukocytes CTCAE grade ≥ 3 (< 2.0 billion/L) | 0 | 0 | 0 | 0 |
| Thrombocytosis (platelets > 600 billion/L) | 1 (0.6) | 3 (1.1) | 1 (0.7) | 0 |
| ALT ≥ 3×ULN | 4 (2.2) | 9 (3.2) | 6 (3.9) | 7 (3.0) |
| AST ≥ 3×ULN | 6 (3.3) | 8 (2.9) | 1 (0.6) | 6 (2.6) |
| TBL ≥ 2×ULN | 0 | 5 (1.8) | 0 | 2 (0.9) |
| ALP ≥ 1.5×ULN | 4 (2.2) | 1 (0.4) | 3 (1.9) | 1 (0.4) |
| CPK CTCAE grade ≥ 3 (> 5×ULN)a | 6 (3.3) | 26 (9.5) | 4 (2.6) | 16 (7.0) |
| LDL ≥ 3.36 mmol/Lb | 31 (23.5) | 80 (38.6) | 37 (33.3) | 63 (35.4) |
| HDL ≥ 1.55 mmol/Lc | 43 (44.3) | 81 (49.7) | 33 (37.5) | 63 (46.7) |
| Triglycerides ≥ 5.65 mmol/Ld | 2 (1.2) | 5 (1.9) | 0 | 0 |
Data are expressed as n (%)
Percentages are based on number of patients at risk for the specified anomaly
ALP alkaline phosphatase, ALT alanine transaminase, AST aspartate transaminase, CPK creatine phosphokinase, CTCAE Common Terminology Criteria for Adverse Events, HDL high-density lipoprotein, LDL low-density lipoprotein, n number of patients in the specified category, N number of patients in the analysis, NCEP National Cholesterol Education Program, TBL total bilirubin, ULN upper limit of normal
aThere were no associated cases of rhabdomyolysis
bIncrease to borderline high, high, or very high (NCEP criteria)
cIncrease to high (NCEP criteria)
dIncrease to very high (NCEP criteria)
Discussion
In BRAVE-AA1 and BRAVE-AA2, response rates in scalp hair regrowth increased over 52 weeks of baricitinib treatment in adults with severe AA, with 40.9% and 36.8%, respectively, of baricitinib 4 mg-treated patients achieving a SALT score ≤ 20 at Week 52. Eyebrow and eyelash response rates also increased over time, indicating that long-term treatment may be required to observe maximum clinical benefit. In both studies, numerically greater proportions of patients achieved efficacy endpoints with baricitinib 4 mg versus 2 mg, and these differences were sustained over time.
No new safety signals were observed versus the 36-week placebo-controlled period [1]. The most common AEs included upper respiratory tract infection, headache, nasopharyngitis, acne, urinary tract infection, CPK elevation, and COVID-19 infection. The frequency of COVID-19 infections reflects the evolution of the COVID-19 pandemic during the conduct of the trials. No VTEs were reported in either study. Newly reported malignancies included one case each of squamous cell carcinoma and ductal carcinoma in situ. Long-term safety data in rheumatoid arthritis do not suggest increased incidence of malignancies with baricitinib [9], but longer-term data are needed in AA to assess causal associations. Most increases in CPK to ≥ 5 times the upper limit of normal in baricitinib-treated patients were related to physical exercise, and no cases of rhabdomyolysis were reported.
As most patients randomized to placebo at baseline were non-responders (SALT score > 20) at Week 36 [1], they were switched to treatment with baricitinib at Week 36. Thus, there were no statistical comparisons with placebo in the present analysis. Both trials excluded patients who had current episodes lasting ≥ 8 years without any hair regrowth and patients with previous inadequate response to JAK inhibitors. Thus, efficacy in these patients remains to be established. Due to the COVID-19 pandemic, some assessments were missed or performed remotely and censored. As this may lead to an underestimation of efficacy values, analyses using multiple imputation are provided in the ESM.
Response rates for most endpoints did not plateau over the study period, indicating that maximum benefit in scalp, eyebrow, and eyelash hair regrowth may require more than 52 weeks of treatment, in particular for patients with more extensive disease. The present analysis demonstrates the benefits of continuous baricitinib treatment over 1 year for severe AA; however, longer periods of observation are required to evaluate the full extent and stability of clinical response. BRAVE-AA1 and BRAVE-AA2 are ongoing and will follow patients for up to 200 weeks. Eligible patients entered randomized withdrawal or downtitration at Week 52 to assess the durability of clinical response and long-term safety, and these data will be reported in future publications.
Conclusions
In two independent phase III trials of adults with severe AA, the proportions of patients achieving scalp hair, eyebrow, and eyelash regrowth increased over 52 weeks of treatment with once-daily oral baricitinib. Clinical response was numerically greater with baricitinib 4 mg than 2 mg. Safety findings were consistent with the known safety profile of baricitinib. These results confirm the potential for baricitinib in the treatment of severe AA.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
The authors would like to thank the clinical trial participants and their caregivers, without whom this work would not be possible, as well as all investigators and study staff who participated in these trials. Medical writing and editorial support were provided by Amy K. Ellinwood, PhD, of Eli Lilly and Company. Results were presented in part at the American Academy of Dermatology Annual Meeting in March 2022.
Declarations
Funding
This study was sponsored by Eli Lilly and Company (Lilly), under license from Incyte Corporation.
Competing Interests
Ohsang Kwon reports grants from Lilly during the conduct of the study and grants from Pfizer, Amorepacific Corporation and Juvic Co., and personal fees from Yuhan Pharmaceuticals outside the submitted work. Maryanne M. Senna has served on scientific advisory boards for Lilly, Pfizer, Concert, Arena, Follica, Deciphera, Cassiopea; as a speaker for Lilly & Pfizer; and as principal investigator (PI) for Lilly and Concert. Rodney Sinclair is a member of the Lilly advisory board and was PI in the Lilly-sponsored BRAVE clinical trials. Taisuke Ito has served on advisory boards and/or is a consultant and/or clinical trial investigator for Bristol-Myers Squibb, Lilly, Pfizer, Regeneron, and Maruho Co Ltd. Brett King has served on advisory boards and/or is a consultant and/or clinical trial investigator for AbbVie, AltruBio Inc., Almirall, AnaptysBio, Arena, Bioniz Therapeutics, Bristol-Myers Squibb, Concert, Horizon Therapeutics, Lilly, Incyte, LEO Pharma, Otsuka/Visterra Inc., Pfizer, Regeneron, Sanofi Genzyme, TWi Biotechnology Inc., and Viela Bio. He is on speaker bureaus for AbbVie, Incyte, Lilly, Pfizer, Regeneron, and Sanofi Genzyme. Yves Dutronc, Guanglei Yu, Chiara Chiasserini, Jill McCollam, and Wen-Shuo Wu are employees and shareholders of Lilly. Chen-Yen Lin was an employee of Lilly during the period the studies were conducted.
Authorship
Each author has met the authorship criteria established by the International Committee of Medical Journal Editors. All authors contributed to study design and data interpretation. Statistical analysis was performed by GY and CL. All authors contributed to writing and reviewing the manuscript, and all authors read and approved the final manuscript.
Data Availability
Lilly provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the US and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.
Ethics Approval
The trials were performed in accordance with ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The research protocols were approved by each center’s IRB or Ethics Committee; BRAVE-AA1 was first approved by Advarra IRB on 13 August 2018, and BRAVE-AA2 was first approved by Quorum Review IRB on 19 February 2019
Patient Consent to Participate
Written informed consent was obtained from all individual participants included in the study.
Patient Consent to Publish
Patients signed informed consent regarding publishing their data and photographs.
Code Availability
Not applicable.
References
- 1.King B, Ohyama M, Kwon O, Zlotogorski A, Ko J, Mesinkovska NA, et al. two phase 3 trials of baricitinib for alopecia areata. N Engl J Med. 2022;386(18):1687–1699. doi: 10.1056/NEJMoa2110343. [DOI] [PubMed] [Google Scholar]
- 2.Phan K, Sebaratnam DF. JAK inhibitors for alopecia areata: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33(5):850–856. doi: 10.1111/jdv.15489. [DOI] [PubMed] [Google Scholar]
- 3.Damsky W, King BA. JAK inhibitors in dermatology: the promise of a new drug class. J Am Acad Dermatol. 2017;76(4):736–744. doi: 10.1016/j.jaad.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xing L, Dai Z, Jabbari A, Cerise JE, Higgins CA, Gong W, et al. Alopecia areata is driven by cytotoxic T lymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20(9):1043–1049. doi: 10.1038/nm.3645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wyrwich KW, Kitchen H, Knight S, Aldhouse NVJ, Macey J, Nunes FP, et al. The Alopecia Areata Investigator Global Assessment scale: a measure for evaluating clinically meaningful success in clinical trials. Br J Dermatol. 2020;183(4):702–709. doi: 10.1111/bjd.18883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olsen EA, Hordinsky MK, Price VH, Roberts JL, Shapiro J, Canfield D, et al. Alopecia areata investigational assessment guidelines—Part II. National Alopecia Areata Foundation. J Am Acad Dermatol. 2004;51(3):440–447. doi: 10.1016/j.jaad.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 7.Wyrwich KW, Kitchen H, Knight S, Aldhouse NVJ, Macey J, Nunes FP, et al. Development of clinician-reported outcome (ClinRO) and patient-reported outcome (PRO) measures for eyebrow, eyelash and nail assessment in alopecia areata. Am J Clin Dermatol. 2020;21(5):725–732. doi: 10.1007/s40257-020-00545-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Common Terminology Criteria for Adverse Events. Version 5.0. Published 27 November 2017. US Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2020.
- 9.Taylor PC, Takeuchi T, Burmester GR, Durez P, Smolen JS, Deberdt W, et al. Safety of baricitinib for the treatment of rheumatoid arthritis over a median of 4.6 and up to 9.3 years of treatment: final results from long-term extension study and integrated database. Ann Rheum Dis. 2022;81(3):335–343. doi: 10.1136/annrheumdis-2021-221276. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Lilly provides access to all individual participant data collected during the trial, after anonymization, with the exception of pharmacokinetic or genetic data. Data are available to request 6 months after the indication studied has been approved in the US and EU and after primary publication acceptance, whichever is later. No expiration date of data requests is currently set once data are made available. Access is provided after a proposal has been approved by an independent review committee identified for this purpose and after receipt of a signed data sharing agreement. Data and documents, including the study protocol, statistical analysis plan, clinical study report, and blank or annotated case report forms, will be provided in a secure data sharing environment. For details on submitting a request, see the instructions provided at www.vivli.org.