Abstract
Introduction:
In children, idiopathic intracranial hypertension (IIH) is relatively uncommon. It is characterized by an increase in intracranial pressure, in the absence of evidence of underlying brain disease, structural abnormalities, hydrocephalus, or abnormal meningeal improvement. However, very rarely it can occur without papilledema, even though it is the most recognizable clinical sign. Due to this, a delay in diagnosis can lead to severe visual impairments.
Case presentation:
We describe a patient with a chronic headache but no papilledema. His neurological and systemic examinations were otherwise unremarkable. A lumbar puncture revealed a high opening pressure of 450 mmH2O and normal cerebrospinal fluid (CSF) parameters. Magnetic resonance imaging of the brain revealed only tortuous optic nerves, no parenchymal lesions, and no evidence of venous sinus thrombosis. He required acetazolamide treatment. Our patient’s symptoms improved significantly in 2 months with medical treatment, weight loss, and exercise, with no development of papilledema.
Conclusion:
There is a wide range of clinical manifestations of IIH, making it difficult to decide when to begin treatment.
Keywords: Headache, idiopathic intracranial hypertension, children
Introduction
Chronic headache is a difficult clinical condition to manage because the treatment is sophisticated and not usually effective.1 Patients with chronic refractory headache who do not respond to prophylactic prophylaxis should be evaluated for idiopathic intracranial hypertension (IIH).1
Headache caused by IIH often resembles chronic migraine or chronic tension-type headache, making differentiation from primary headache clinically difficult.2 Lumbar puncture is needed to confirm the diagnosis, but there is disagreement about the CSF opening pressure cut-off value for the diagnosis of intracranial hypertension, the opening pressure of 200 mmH2O was the previously accepted upper limit of normal CSF pressure.2
In children, IIH is rare. It is characterized by an increase in intracranial pressure (ICP) without any underlying brain disease, structural abnormalities, hydrocephalus, or abnormal meningeal enhancement.3 Among children in the United States, the incidence is 0.9 per 100 000, while in Canada, it is 4 per 100 000.3
The precise pathophysiology of IIH is not known. Normally, ICP remains constant and maintained within a normal range due to cerebral autoregulation.4 Elevated ICP is caused by disturbances in cerebrospinal fluid (CSF), cerebrospinal fluid dynamics, and molecular mechanisms.5
The Monro-Kellie doctrine states that the volume of the brain, cerebrospinal fluid, and blood within the brain is constant. An increase in one should cause a mutual decrease in the other two, in addition, increased CSF production, decreased outflow, increased volume, venous system obstruction, endocrine causes, metabolic causes, and chronic inflammation may also be involved.6,7 Obesity is associated with IIH, but the association cannot be explained pathophysiologically.8
Headache are usually throbbing, intermittent, diffuse in approximately 90%,9 and worsen upon awakening. In addition to headache, neck and back pain should resort to IIH, not pseudotumor. IIH remains a diagnosis of exclusion. Prompt diagnosis and comprehensive evaluation are essential to prevent vision loss and improve associated symptoms.10 Symptoms such as nausea and vomiting are common. Other complaints include blurred or double vision, temporary visual disturbances, tinnitus, and neck stiffness.11 Irritability may be the only symptom of IIH in younger patients.12 Children with IIH are usually conscious.13
Friedman et al14 propose updated diagnostic criteria for pediatric IIH. It provides specific recommendations for CSF opening pressure in pediatric patients and addresses issues when IIH is not clearly diagnosed.14
In addition, Friedman and Jacobson3 recognized MRI’s recent diagnostic criteria and set the upper limit at 250 mmH2O. Diagnostic criteria for IIH without papilledema or sixth nerve palsy have been proposed, combined with increased opening pressure and at least 3 of the following imaging findings: empty sella, preoptic subarachnoid dilatation with or without optic nerve distortion, posterior flattened sclera, and transverse sinus stenosis.3,14
Case Presentation
A 12-year-old boy, previously healthy, with excellent academic performance, presented to the Pediatric Emergency Department of our hospital, with a 7-day history of moderate to severe headache with frontal localization, without vomiting, altered level of consciousness, abnormal movements, or seizures. The headache was constant, aggravated by physical activity with no relieving factors.
The patient had no visual symptoms, vertigo, or tinnitus. There was no history of fever, recent febrile illness, or medication intake including herbal medications. Other neurological symptoms were negative. Other body systems symptomatology was unremarkable.
The patient had a past medical history of chronic headache that have occurred on and off over the past 7 months. The headache did not affect his activities of daily living, and he does not have any sinister symptoms. There was no history of head trauma. His birth weight was normal, and his head circumference was normal. No family history of epilepsy or chronic headache.
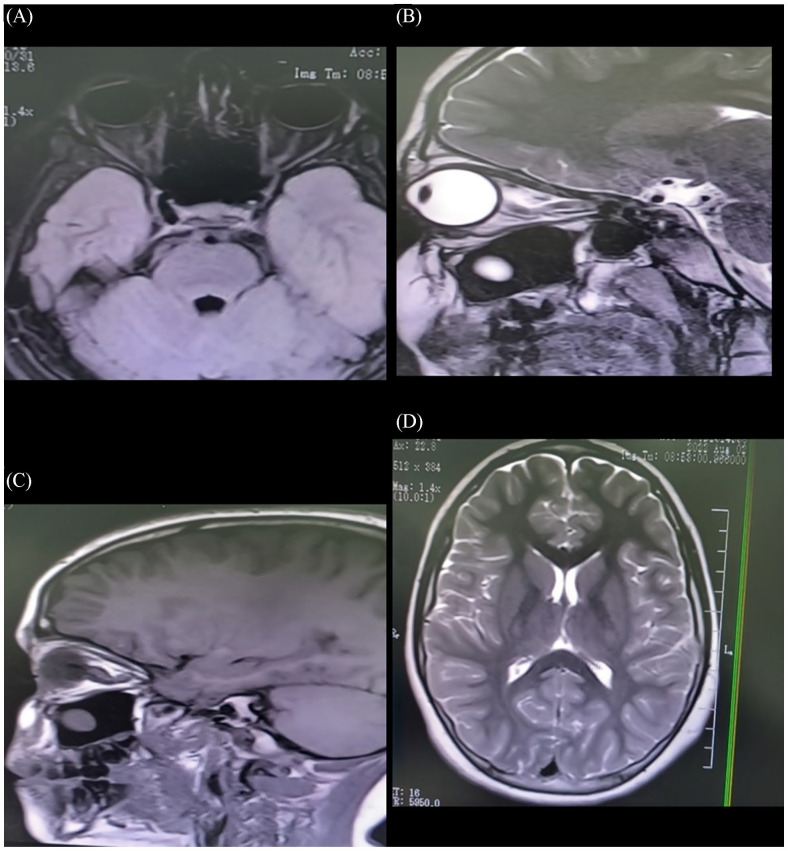
Physical examination revealed a conscious nonobese child. His body weight was 45 kg (above the 50th centile). His eye examination showed no diplopia and no evidence of abducens nerve palsy. Visual acuity was 20/20 in both eyes with normal color vision, pupillary light responses, and normal fundus examination (Figure 1). The remaining neurological and systemic reviews were normal.
Figure 1.
Patient’s fundus examination was normal.
His laboratory investigations revealed normal complete blood count, renal functions, liver functions, thyroid profile, anti-nuclear antibodies, anti-double-stranded DNA, and vitamin A and D levels.
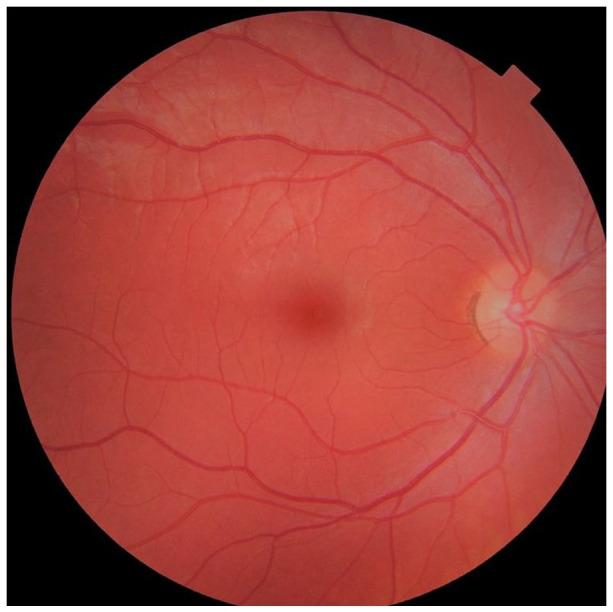
His brain imaging using computed brain tomography was normal, with no evidence of space-occupied lesions. Brain and orbit magnetic resonance imaging (MRI) with contrast showed some evidence of elevated ICP, slight vertical tortuosity of both optic nerves and slightly prominent CSF around optic nerves, no flattening of the posterior sclera (Figure 2A–D). There were no parenchymal abnormalities or areas of enhancement, normal spinal cord anatomy, and no abnormal signal intensity. Magnetic resonance venography (MRV) showed no venous sinus thrombosis.
Figure 2.
(A–C): MRI/T2 FLIAR MRI showed prominence of the optic nerve head as well as tortuosity of optic nerves and prominent perioptic nerve sheath. (D): Normal brain parenchymal, no lesions.
He underwent lumber puncture which was notable for an opening pressure of 450 mmH2O. CSF cytology, chemistry, and cultures were normal with white blood cells being only 3/mm3, no red blood cells, the protein was 40 mg/dl, and glucose being 35 mmol/l. The viral panel for neurotrophic viruses including herpes simplex viruses 1 & 2, cytomegalovirus, Epstein Barr virus, and neurotrophic enteroviruses, were negative. His CSF IgG index was 0.5 (normal range 0.3-0.6), there were no oligoclonal bands, normal autoimmune serology, aquaporin 4 antibodies titer 1:10 (negative), and myelin oligodendrocyte glycoprotein antibodies were negative.
After draining 30 ml of CSF, acetazolamide was commenced based on clinical case profiling and assimilation. It was started at 10 mg/kg/day and escalated. Nonpharmacologic intervention, including dietary advice and regular physical exercise, was also commenced. The patient lost 5 kg and his weight became 40 kg on the 50th centile.
After 2 months of acetazolamide therapy, the patient showed a reduction in headache frequency and severity and an improved quality of life. Repeated lumbar puncture revealed normal opening pressure with normal CSF parameters. His most recent clinic visit revealed no visual symptoms or the development of papilledema with a resolution of MRI findings.
Discussion
Idiopathic intracranial hypertension is a disorder of unknown etiology.15 Classic symptoms and signs of IIH include headache, papilledema, diplopia, and pulsatile tinnitus. Atypical presentations include highly asymmetric or even unilateral papilledema and IIH without papilledema. Although atypical findings should raise a red flag and prompt further investigation for an alternative etiology, clinicians should be familiar with these unusual presentations.15
In multiple reports, papilledema was not present, and the majority of patients were nonobese.16,17 Our case is similar to this. The results of both studies contradict the current medical practice of associating papilledema and obesity with IIH in childhood. We emphasize the need for revised diagnostic criteria in this population to detect and manage this condition.16
Favoni et al18 found in their study to determine the prevalence of IIH without papilledema, testing revised diagnostic criteria by Friedman in refractory chronic headache patients, 23% had opening pressure greater than 200 mmH2O. The 5% of patients with IIH had neuroimaging findings suggestive of elevated ICP, which was consistent with our patient. Papilledema is an essential sign in children, but its absence does not exclude IIH. Based on a previous study, 48% of patients did not have papilledema, which highlights the importance of evaluating any child with chronic headache. The consequences of idiopathic intracranial hypertension with papilledema are unclear regarding vision and require further research.19
Bashiri et al20 observed that 2% of their patients had no papilledema when they presented. The neuroimaging criteria were consistent with raised ICP and high opening pressure, and headache and visual disturbances were the most common presentations. Our report contradicted this. We found no visual disturbances and only 2 signs of elevated ICP. It is possible to attribute the difference in clinical presentation and imaging to the magnitude of the pressure and other factors.
In the study of Favoni et al,18 they found only 2 patients (5%) that satisfied neuroimaging criteria, both had opening pressure higher than 200 mmH2O, but only one higher than 250 mmH2O, and one of them (2.5%) met the newly proposed diagnostic criteria by Friedman for idiopathic intracranial hypertension without papilledema, they also found all patients had retinal nerves fiber layer thickness within normal range, supporting the hypothesis that long duration of headache does not affect the eye. In our case we found, only 2 signs suggestive of the raised ICP and opening pressure of 35 mmg, and the patient was symptomatic, had a headache, and had no gross visual disturbance.
In a study done by Digre et al,21 they found patients without papilledema reported visual disturbances (20%), spontaneous venous pulsations (75%), and non-physiologic visual field constriction (20%) more often than did those with papilledema. This finding is inconsistent with our case. They also found lower opening pressure in patients without papilledema, this is also inconsistent with our case where we found a markedly elevated opening pressure of 450 mmH2O.
A relationship between IIH in children and age, as well as obesity, remains unclear. While 45% of patients between the ages of 3 and 11 are obese, our patient is not.8 According to the study, young children with IIH had a lower obesity rate than older children.
In their study, Brodsky and Vaphiades22 found distension of the perioptic subarachnoid space in 45%, and vertical tortuosity of the orbital optic nerve in 40%, which were in agreement with ours.
It has been reported that 65% of patients with idiopathic intracranial hypertension have distension of the perioptic subarachnoid space as well as tortuosity of the optic nerve, which is similar to our findings. They also found other narratives of idiopathic intracranial hypertension.23
In summary, considering the present data and previous reports (Table 1), physicians should not dismiss the possibility of intracranial hypertension in patients with symptoms suggesting intracranial hypertension based solely on the presence or absence of papilledema. When children are experiencing persistent headache that is not responding to standard treatment, intracranial hypertension with or without papilledema should be considered.
Table 1.
Summary of previous studies on IIH in children.
| Number of cases | Clinical manifestations | Prevalence of papilledema | Treatment | |
|---|---|---|---|---|
| Chelse and Epstein2 | 12 | Headache, visual reduction, and nausea | In 87% | Acetazolamide and weight reduction. |
| Two cases needed urgent neurosurgical intervention | ||||
| Faz et al16 | 27 | Headache, visual reduction, and nausea | In 52%. | Medical therapy: pharmacologic & non-pharmacologic such as weight reduction |
| The majority of patients were nonobese (70%) | ||||
| Lessell17 | 25 | Infants and young children: irritability, apathy, or somnolence, rather than headache. | In young children: infrequent. | Acetazolamide and weight reduction. |
| In adolescents: headache, lateral rectus paresis, vertical strabismus, facial paresis, and back, and neck pain. | In older children: 67% | Three cases needed urgent neurosurgical intervention. | ||
| Some cases were associated with tetracycline therapy, malnutrition or re-nutrition, and the correction of hypothyroidism | ||||
| Phillips et al11 | 45 | 13 patients (37%) were obese. | 80% with a variable grade of papilledema | Medical therapy in the majority of patients. |
| 4 patients had visual acuity less than 20/40 in the best eye. | Three patients needed surgical consideration. | |||
| 10 patients had visual field deficits. | ||||
| 17 patients (49%) had cranial nerve deficits and headache. | ||||
| 10 patients (33%) had optic nerve atrophy. | ||||
| Rangwala and Liu13 | 58 | Headaches and visual dysfunction were the most common presentation | Papilledema was associated in the majority of cases | Although most cases of pediatric idiopathic intracranial hypertension improve with medical treatment, those who have had visual progression despite medical treatment have undergone optic nerve sheath fenestration and lumboperitoneal shunting. |
| Walker4 | Headaches and visual dysfunction were the most common presentation. | Papilledema was associated in the majority of cases | Medical therapy | |
| Visual field restriction and sixth nerve palsy were common. | ||||
| Favoni et al18 | Headache and visual disturbances | Papilledema was associated in the majority of cases. Two patients had no papilledema | Medical therapy in the majority of patients | |
| Digre et al21 | 17 | Patients without papilledema reported visual disturbances (20%), spontaneous venous pulsations (75%), and non-physiologic visual field constriction (20%) more often than did those with papilledema | Papilledema was associated in the majority of cases. Two patients had no papilledema | Medical therapy |
Acknowledgments
Najmah Ali Alotaibi, Alhada Armed Forces hospital, Pediatric Resident, Department of Pediatrics, Taif, Kingdom of Saudi Arabia.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Authors’ Contributions: MAM, MFA, YAA, WE, SAA, SASA, NMK: conception and design, acquisition of data or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; final approval of the version published.
Availability of Data and Material: The data and materials generated and/or analyzed during the current study are available in the current manuscript.
Declarations: We declare that the work on which this case report is based is my original work (except where acknowledgments indicate otherwise) and that neither the whole work nor any part of it has been, is being, or is to be submitted for another degree in this or any other journals.
Ethics Approval and Consent to Participate: This study was approved by Human Research Ethics Committee, Alhada Armed Forces Hospital, Taif, Saudi Arabia. Written informed consent for publication was obtained from parents for the inclusion of their child in the current study.
Consent for Publication: Written informed parental consent was obtained for the publication of this case report.
References
- 1. Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004;24 Suppl 1:9-160. [DOI] [PubMed] [Google Scholar]
- 2. Chelse AB, Epstein LG. Intracranial hypertension in children without papilledema. Pediatr Neurol Briefs. 2015;29:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology. 2002;59:1492-1495. [DOI] [PubMed] [Google Scholar]
- 4. Walker RW. Idiopathic intracranial hypertension: any light on the mechanism of the raised pressure? J Neurol Neurosurg Psychiatry. 2001;71:1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Eftekhari S, Westgate CSJ, Uldall MS, Jensen RH. Preclinical update on regulation of intracranial pressure in relation to idiopathic intracranial hypertension. Fluids Barriers CNS. 2019;16:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Donaldson JO. Pathogenesis of pseudotumor cerebri syndromes. Neurology. 1981;31:877-880. [DOI] [PubMed] [Google Scholar]
- 7. Calabrese VP, Selhorst JB, Harbison JW. CSF infusion test in pseudotumor cerebri. Trans Am Neurol Assoc. 1978;103:146-150. [PubMed] [Google Scholar]
- 8. Balcer LJ, Liu GT, Forman S, et al. Idiopathic intracranial hypertension: relation of age and obesity in children. Neurology. 1999;52:870-872. [DOI] [PubMed] [Google Scholar]
- 9. Ko MW, Liu GT. Pediatric idiopathic intracranial hypertension (pseudotumor cerebri). Horm Res Paediatr. 2010;74:381-389. [DOI] [PubMed] [Google Scholar]
- 10. Binder DK, Horton JC, Lawton MT, McDermott MW. Idiopathic intracranial hypertension. Neurosurg. 2004;54:538-551; discussion 551. [DOI] [PubMed] [Google Scholar]
- 11. Phillips PH, Repka MX, Lambert SR. Pseudotumor cerebri in children. J AAPOS. 1998;2:33-38. [DOI] [PubMed] [Google Scholar]
- 12. Spennato P, Ruggiero C, Parlato RS, et al. Pseudotumor cerebri. Childs Nerv Syst. 2011;27:215-235. [DOI] [PubMed] [Google Scholar]
- 13. Rangwala LM, Liu GT. Pediatric idiopathic intracranial hypertension. Surv Ophthalmol. 2007;52:597-617. [DOI] [PubMed] [Google Scholar]
- 14. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology. 2013;81:1159-1165. [DOI] [PubMed] [Google Scholar]
- 15. Chen BS, Newman NJ, Biousse V. Atypical presentations of idiopathic intracranial hypertension. Taiwan J Ophthalmol. 2021;11:25-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Faz G, Butler IJ, Koenig MK. Incidence of papilledema and obesity in children diagnosed with idiopathic “benign” intracranial hypertension: case series and review. J Child Neurol. 2010;25:1389-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lessell S. Pediatric pseudotumor cerebri (idiopathic intracranial hypertension). Surv Ophthalmol. 1992;37:155-166. [DOI] [PubMed] [Google Scholar]
- 18. Favoni V, Pierangeli G, Toni F, et al. Idiopathic intracranial hypertension without papilledema (IIHWOP) in chronic refractory headache. Front Neurol. 2018;9:503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aylward SC, Aronowitz C, Roach ES. Intracranial hypertension without papilledema in children. J Child Neurol. 2016;31:177-183. [DOI] [PubMed] [Google Scholar]
- 20. Bashiri FA, Al Abdulsalam HK, Hassan SM, et al. Pediatric intracranial hypertension. Experience from 2 tertiary centers. Neurosci. 2019;24:257-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Digre KB, Nakamoto BK, Warner JE, Langeberg WJ, Baggaley SK, Katz BJ. A comparison of idiopathic intracranial hypertension with and without papilledema. Headache. 2009;49:185-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Brodsky MC, Vaphiades M. Magnetic resonance imaging in pseudotumor cerebri. Ophthalmology. 1998;105:1686-1693. [DOI] [PubMed] [Google Scholar]
- 23. Lim MJ, Pushparajah K, Jan W, Calver D, Lin JP. Magnetic resonance imaging changes in idiopathic intracranial hypertension in children. J Child Neurol. 2010;25:294-299. [DOI] [PubMed] [Google Scholar]