Abstract
Pelvic fractures are common in cases of blunt trauma, which is strongly associated with mortality. Transcatheter arterial embolization is a fundamental treatment strategy for fatal arterial injuries caused by blunt pelvic trauma. However, vascular injuries due to blunt pelvic trauma can show various imaging findings other than arterial hemorrhage. We present a pictorial review of common and uncommon vascular injuries, including active arterial bleeding, pseudoaneurysm, arteriovenous fistula, arterial occlusion, vasospasm, and active venous bleeding. Knowledge of these vascular injuries can help clinicians select the appropriate therapeutic strategy and thus save lives.
Keywords: Pelvic fracture, Arteriovenous fistula, Arterial occlusion, Vasospasm, Venous bleeding
Introduction
Pelvic fractures are not rare and account for approximately 3% of skeletal injuries [1]. Pelvic fractures are associated with high mortality risk due to the accompanying vascular injury and hemorrhage [2]. The reported in-hospital mortality rate of patients with unstable pelvic fractures is 8.3% [3].
Transcatheter arterial embolization (TAE) is the fundamental treatment strategy for patients with fatal arterial injuries caused by blunt pelvic trauma [4, 5]. However, these patients present with various findings other than arterial hemorrhage, which may hinder interventional radiologists from determining an appropriate treatment strategy. We present a pictorial review of real-world experiences of common and uncommon vascular injuries, including active arterial bleeding, pseudoaneurysm, arteriovenous fistula (AVF), arterial occlusion, vasospasm, and active venous bleeding.
Types of vascular injuries
Active arterial bleeding
TAE is the fundamental treatment strategy for active arterial bleeding due to pelvic fractures [4]. Embolization of the main trunk or branches of the internal iliac artery is the basic endovascular treatment. In cases of shock or multiple traumas, non-selective embolization of the internal iliac artery should be performed [6]. Selective embolization of the internal iliac artery branch can be considered when the patient’s hemodynamics are stable, and there is enough time to perform the procedure. Furthermore, it is necessary to look for bleeding from sources other than the internal iliac artery. Bleeding from the branches of the external iliac artery reportedly occurs in 17% of patients with pelvic fractures [7]. Angiography of the external iliac, median sacral, lumbar, and femoral arteries should be performed.
Embolic material is chosen according to the bleeding site and the presence or absence of coagulation abnormalities. Gelatin sponge particles are often used as embolic materials to avoid permanent arterial occlusion and ischemia. Coils may be used when the bleeding vessels are focal and the catheter can reach the vicinity of the bleeding sites. In coagulopathic patients, liquid embolization with n-butyl cyanoacrylate (NBCA) is useful for both selective and non-selective embolization; however, an experienced operator is desirable to prevent NBCA-related complications, such as reflux and non-target embolization [8].
Considering the risk of lower extremity ischemia after TAE of the main trunk of the common iliac and external iliac arteries, stent graft treatment can be used to stop the bleeding (Fig. 1) [8]. Antiplatelet therapy should be initiated in patients receiving stent graft treatment to prevent post-procedure graft occlusion. However, there is no consensus on the timing of the initiation and termination of the antiplatelet medication. In clinical emergencies, where prompt treatment is needed to save the patient’s life, TAE of the common and external iliac arteries may be considered despite the high risk of lower extremity ischemia (Fig. 2).
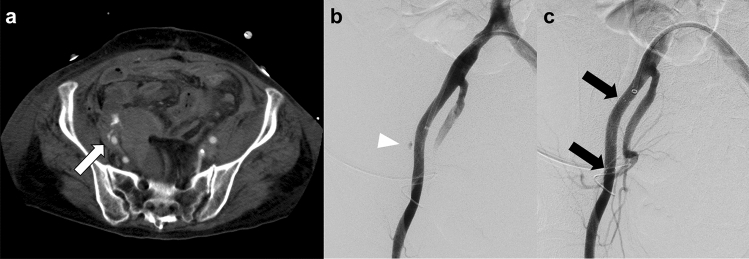
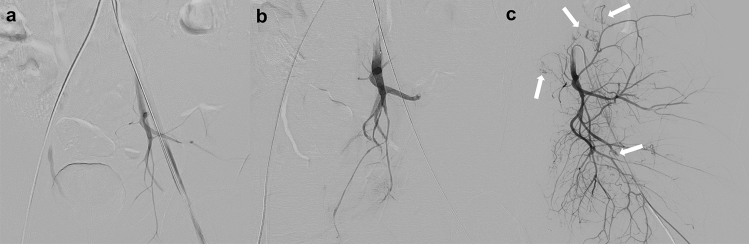
Fig. 1.
Endovascular treatment with stent graft placement for active bleeding from the external iliac artery. a CT scan shows active bleeding from the right external iliac artery (white arrow). b Digital subtraction angiography of the right external iliac artery shows active bleeding (arrowhead). c Digital subtraction angiography of the right external iliac artery obtained after angioplasty with stent graft placement (VIABAHN®, W. L. Gore & Associates, Flagstaff, Ariz) shows cessation of active bleeding. Black arrows indicate the markers of the proximal and distal edges of the stent graft. CT computed tomography
Fig. 2.
Active bleeding from the external iliac artery due to a crush injury in a 54 year-old man. This patient experienced cardiopulmonary arrest during the procedure and required prompt hemostasis because circulation could not be restored with REBOA alone. a Digital subtraction angiography of the left external iliac artery shows active bleeding (arrow). b The bleeding point has been embolized with NBCA. NBCA was mixed with iodized oil in a ratio of 1:1. c Digital subtraction angiography of the left external iliac artery obtained after embolization shows cessation of active bleeding and occlusion of the external iliac artery. However, the patient died after the procedure without recovery of circulation. REBOA resuscitative endovascular balloon occlusion of the aorta; NBCA n-butyl cyanoacrylate
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is an important method for treating severe hemorrhagic shock due to pelvic trauma. In this procedure, occlusion of the aorta with a balloon catheter is conducted to increase proximal arterial pressure and maintain organ blood flow while controlling downstream bleeding [9]. However, REBOA can lead only to temporary hemostasis and is associated with a risk of organ ischemia. Definite hemostasis should be achieved with endovascular or surgical intervention, and the balloon should be deflated promptly to ensure sufficient blood supply to the organs. Furthermore, it should be noted that contrast-enhanced computed tomography (CT) may not demonstrate the extravasation of contrast medium as a result of temporary hemostasis of active bleeding by REBOA (Fig. 3) [10, 11]. In particular, the flow of the contrast medium into the site of active bleeding may be slowed due to the balloon occlusion, resulting in “hidden” bleeding (Fig. 3a). The optimal timing of delayed phase CT is difficult to determine, and the CT protocol for REBOA remains unestablished. We posit that multiple phase CT, including super-delayed phase imaging, may be useful. Further studies should be imperative.
Fig. 3.
Pelvic contrast-enhanced CT images obtained during complete REBOA. a Delayed-phase (second phase) contrast-enhanced CT image shows a massive hematoma (asterisk) without extravasation of the contrast material. b Digital subtraction angiography of the right internal iliac artery obtained during REBOA balloon deflation shows massive extravasation from the iliolumbar artery, which represents “hidden” bleeding on contrast-enhanced CT during complete REBOA (arrow). We embolized the iliolumbar artery with NBCA. CT computed tomography; REBOA resuscitative endovascular balloon occlusion of the aorta; NBCA n-butyl cyanoacrylate
Pseudoaneurysm
The formation of pseudoaneurysms in patients with blunt pelvic trauma, although rare, may occur immediately after the injury or later in the clinical course [12]. Pseudoaneurysms are made of a single layer of fibrous tissue and are often surrounded by a hematoma. [13]. They can rupture and should be treated as soon as they are identified [14]. On CT, a pseudoaneurysm appears as a sac filled with contrast material in the arterial phase, and it is stable in size and shape in the delayed phase, disappearing gradually [15].
Endovascular treatment of traumatic pseudoaneurysm is usually effective (Fig. 4) [16]. The sandwich method is used for TAE of pseudoaneurysms, i.e., embolization of the afferent and efferent vessels to cut off the blood supply to the lesion [17]. However, in this method, the parent blood vessel is occluded. Sac packing with detachable microcoils is another option for pseudoaneurysm treatment, and it preserves the parent arterial patency; however, this procedure is associated with the risk of secondary rupture [18]. In pseudoaneurysms without multiple collateral vessels, stent graft treatment can be considered to preserve the parent vessel [19]. In addition, stent graft treatment may also be effective in cases of failed sac packing.
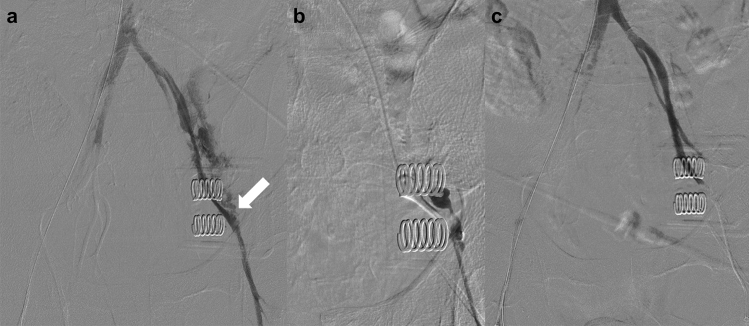
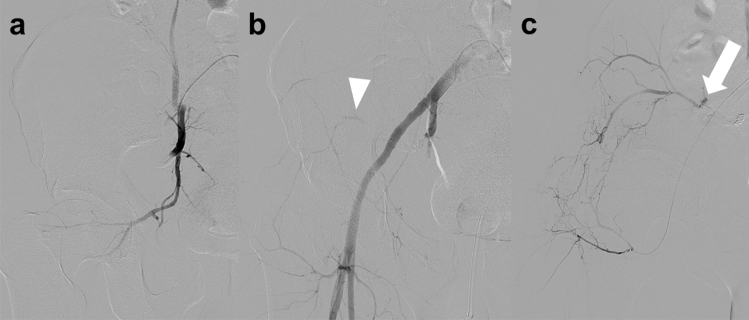
Fig. 4.
Pseudoaneurysm due to pelvic trauma in a 67 year-old man. a CT scan obtained 2 weeks after trauma shows pseudoaneurysm (arrow). b Digital subtraction angiography of the superior gluteal artery shows pseudoaneurysm (arrowhead). c Embolization of the obturator artery and distal portion of the superior gluteal artery has been performed with microcoils (black arrows) to avoid migration of NBCA to the peripheral arteries. d Selective embolization of the pseudoaneurysm with NBCA has been performed; digital subtraction angiography of the internal iliac artery shows the disappearance of the pseudoaneurysm. CT computed tomography; NBCA n-butyl cyanoacrylate
AVF
AVF is an abnormal anastomosis between arteries and veins and does not involve capillaries. Traumatic AVF can develop if arterial bleeding influxes into an adjacent injured vein [15]. On radiological imaging, early filling of a pelvic vein with contrast material may be the only finding in patients with traumatic AVF [20]. Radiologists should recognize the angiographic pseudovein sign that typically indicates gastrointestinal bleeding (extravasation of contrast agent), which may appear curvilinear, mimicking the appearance of veins [21]. It is important to differentiate the pseudovein sign from AVF for appropriate treatment selection. However, the clinical diagnosis of traumatic AVF is often delayed, and the rate of diagnosis within 1 week of injury is reported as only 20% [22]. The cause of the delayed AVF development is unclear. However, delayed AVF may occur when a potentially causative arterial bleeding is undetected and untreated, or when the initial endovascular treatment is inadequately embolized. Therefore, knowledge of traumatic AVF imaging features is essential for radiologists.
Because traumatic AVF can cause heart failure after highly variable latency periods [23], AVFs should be treated regardless of the presence of active bleeding. TAE may be a safe and efficient treatment method for traumatic AVF (Fig. 5) [24–26]. Embolic materials should be selected carefully to prevent migration to the venous flow. When the AVF lesion has multiple feeding arteries, concomitant transarterial and transvenous embolization may be an effective option (Fig. 6) [27].
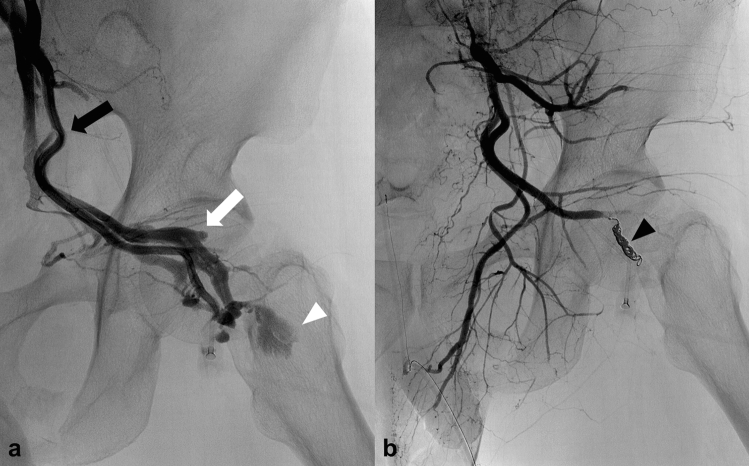
Fig. 5.
AVF due to a fall in a 43 year-old man. a Selective angiography of the inferior gluteal artery shows an AVF with active bleeding (white arrowhead). The black and white arrows indicate the inferior gluteal artery and inferior gluteal vein, respectively. b The main feeding artery of the AVF has been embolized with microcoils (black arrowhead). In addition, small branch arteries have also been embolized by injecting gelatin particles into the origin of the inferior gluteal artery. Subsequently, AVF and active bleeding disappeared. AVF arteriovenous fistula
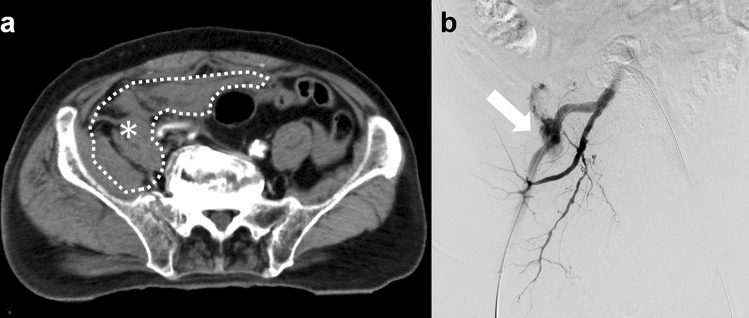
Fig. 6.
Delayed AVF due to a traffic accident in a 17 year-old boy. a, b CT scan and digital subtraction angiography of the right internal iliac artery obtained immediately after admission show active bleeding (arrows). Non-selective embolization of the right internal iliac artery with gelatin particles has been performed. c, d Coronal view CT scan and digital subtraction angiography of the internal pudendal artery obtained 3 weeks after injury show early filling of a pelvic vein (arrowhead). The AVF has multiple feeding arteries. e A transvenous approach has been used to embolize the drainer vein. f The main drainer vein has been embolized with microcoils (arrowhead), and the feeding arteries have been embolized with NBCA (black arrows), gelatin particles, and microcoils (white arrow). Digital subtraction angiography of the right internal iliac artery shows disappearance of the AVF. AVF arteriovenous malformation; CT computed tomography
Vasospasm
The middle layer of blood vessels is made up of smooth muscles, and smooth muscle cells may contract and become spasmodic following external compression, stretching, or endothelial injury due to trauma [28]. Active bleeding is not usually detected on the first angiogram due to vasospasm, but it can be detected through repeated angiography [29, 30]. Recurrent bleeding from a previously embolized artery can also be explained by vasospasm. With improved vessel diameter after resuscitation, the embolic material might not occlude the bleeding vessel (Fig. 7) [30, 31]. Therefore, patients with unstable blood pressure should undergo repeated angiography regardless of whether embolization was performed. To prevent rebleeding in coagulopathic patients with vasospasm, we recommend embolization with NBCA, which adheres to the vessels and is unlikely to migrate.
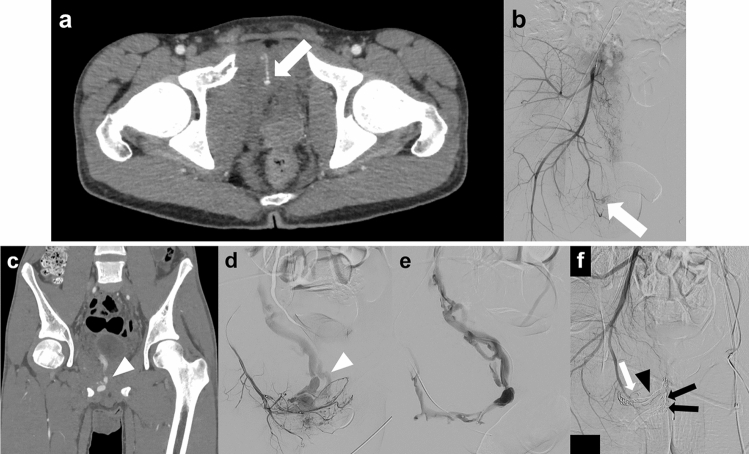
Fig. 7.
Arterial vasospasm after a traffic accident in a 29 year-old man with pelvic fractures and thoracic injury. a Digital subtraction angiography of the left common iliac artery shows arterial vasospasm. Peripheral branches of the internal iliac artery are poorly depicted, and active bleeding cannot be detected. b Digital subtraction angiography obtained after non-selective embolization of the internal iliac artery with gelatin particles shows no active bleeding. Thoracic surgical procedures have been performed to ensure hemostasis after the first embolization session. c The second session of endovascular treatment has been performed because of unstable hemodynamics after thoracic surgery. Digital subtraction angiography of the left internal iliac artery shows scattered active bleeding due to the release of vasospasm
Arterial occlusion
Arterial occlusion is caused by transmural injury or dissection with a thrombus [15]. Active bleeding is a serious concern in patients with arterial occlusion, even if extravasation of contrast material is not detected on CT [20]. In addition, traumatic arterial occlusion has the potential pathogenesis of delayed bleeding due to the mobilization of the thrombus [32]. Therefore, TAE of the occluded arteries in the branches of the internal iliac artery may be appropriate to prevent rebleeding. Furthermore, angiography of the collateral blood vessels should be performed to check for active bleeding distal to the occluded vessel (Fig. 8). In contrast, stent graft treatment for traumatic vessel occlusion is controversial, and further studies are warranted.
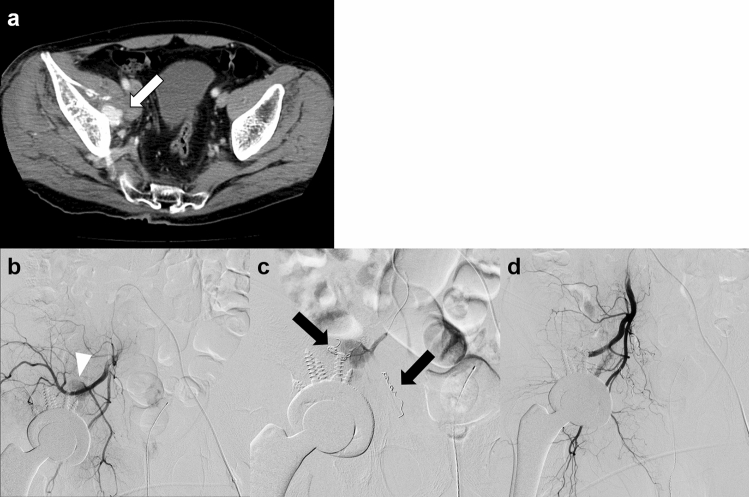
Fig. 8.
Arterial obstruction due to a crush injury in a 50 year-old man. a Digital subtraction angiography of the right internal iliac artery shows complete obstruction of the superior gluteal artery. b Embolization with microcoils of the superior gluteal artery and non-selective embolization with gelatin particles of the internal iliac artery have been performed. Digital subtraction angiography of the right common iliac artery obtained after embolization of the right internal iliac artery shows blood flow from a branch of the external iliac artery to the distal portion of the occluded superior gluteal artery (arrowhead). c Digital subtraction angiography of the lateral femoral circumflex artery shows collateral circulation to the distal portion of the superior gluteal artery with extravasation of contrast material (arrow). Embolization with gelatin particles led to successful hemostasis
Traumatic occlusion of the main trunk of the common/external iliac artery can cause critical lower limb ischemia, making recanalization crucial [33]. Vascular surgery is a treatment option for traumatic occlusion of the main trunk of the common/external iliac artery. Furthermore, endovascular treatment with covered stents, aspiration thrombectomy, and balloon dilation can also be performed [34, 35]. In addition, using a cutting balloon may be helpful when intimal thickening is present at the traumatic occluded site [35].
Active venous bleeding
Bleeding due to pelvic fractures occurs more frequently from veins (80%) than from arteries (20%); the main venous sources of bleeding are the presacral plexus and prevesical veins [36]. Peritoneal pelvic packing and mechanical pelvic ring fixation can be performed to treat venous bleeding [37]. Endovascular treatment may be optimal for active bleeding from the main trunk of the iliac vein.
Active venous bleeding can be visualized using CT as the extravasation of contrast material in venous phase images without extravasation in arterial phase images (Fig. 9) [20]. Iliac vein injury causes massive bleeding and hemorrhagic shock, and venography is useful in detecting active bleeding from the iliac vein in some patients with blunt pelvic trauma [38]. Surgical or endovascular therapies can be used for treating iliac vein injuries.
Fig. 9.
Venous injury due to a traffic accident in a 50 year-old man. a Arterial phase pelvic CT scan shows no extravasation of contrast material within the hematoma (black arrow). b, c Venous phase CT scan (b: axial view, c: coronal view) shows extravasation of contrast material (arrowheads) with a narrowed external iliac vein (arrows). CT, computed tomography
Transcatheter venous embolization with NBCA can potentially control critical bleeding from the iliac vein. However, it may cause some complications, such as leg swelling, deep vein thrombosis, and pulmonary embolism by obstruction of venous flow [39]. Endovascular treatment with covered stents is considered a favorable treatment option [40, 41], if an appropriately sized stent is readily available. When a covered stent is not immediately available, uncovered stent placement is an alternative option for endovascular treatment for critical iliac vein injury [38, 42, 43]. Stenting of venous injuries covers the injured area and promotes hemostasis by reducing venous pressure, which is elevated because of the surrounding hematoma [43].
When surgical treatment is chosen for a venous injury, balloon catheters can reduce bleeding and help obtain the necessary visualization of the operative field by occluding the proximal and distal portions of the injury [44].
Conclusion
Endovascular treatment is effective for vascular injuries due to blunt pelvic trauma. Knowledge of the various forms and imaging findings of vascular injuries is essential for the astute planning of treatment strategies and life-saving maneuvers.
Author contributions
All authors read and approved the final manuscript.
Funding
No funding or sponsorship was received for this study or publication of this article.
Declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors. Personal information was removed from this article according to the privacy policy of Japan Radiological Society.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Grotz MRW, Allami MK, Harwood P, Pape HC, Krettek C, Giannoudis PV. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury. 2005;36:1–13. doi: 10.1016/j.injury.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 2.Sathy AK, Starr AJ, Smith WR, Elliott A, Agudelo J, Reinert CM, et al. The effect of pelvic fracture on mortality after trauma: an analysis of 63,000 trauma patients. JBJS. 2009;91:2803. doi: 10.2106/JBJS.H.00598. [DOI] [PubMed] [Google Scholar]
- 3.Yoshihara H, Yoneoka D. Demographic epidemiology of unstable pelvic fracture in the United States from 2000 to 2009: trends and in-hospital mortality. J Trauma Acute Care Surg. 2014;76:380–385. doi: 10.1097/TA.0b013e3182ab0cde. [DOI] [PubMed] [Google Scholar]
- 4.Padia SA, Ingraham CR, Moriarty JM, Wilkins LR, Bream PR, Jr, Tam AL, et al. Society of interventional radiology position statement on endovascular intervention for trauma. J Vasc Interv Radiol. 2020;31(363–9):e2. doi: 10.1016/j.jvir.2019.11.012. [DOI] [PubMed] [Google Scholar]
- 5.Vaidya R, Waldron J, Scott A, Nasr K. Angiography and embolization in the management of bleeding pelvic fractures. J Am Acad Orthop Surg. 2018;26:e68–e76. doi: 10.5435/JAAOS-D-16-00600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cullinane DC, Schiller HJ, Zielinski MD, Bilaniuk JW, Collier BR, Como J, et al. Eastern association for the surgery of trauma practice management guidelines for hemorrhage in pelvic fracture—update and systematic review. J Trauma Acute Care Surg. 2011;71:1850–1868. doi: 10.1097/TA.0b013e31823dca9a. [DOI] [PubMed] [Google Scholar]
- 7.Johnson GE, Sandstrom CK, Kogut MJ, Ingraham CR, Stratil PG, Valji K, et al. Frequency of external iliac artery branch injury in blunt trauma: improved detection with selective external iliac angiography. J Vasc Interv Radiol. 2013;24:363–369. doi: 10.1016/j.jvir.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 8.Wijffels DJ, Verbeek DO, Ponsen KJ, Carel Goslings J, van Delden OM. Imaging and endovascular treatment of bleeding pelvic fractures: review article. Cardiovasc Intervent Radiol. 2019;42:10–18. doi: 10.1007/s00270-018-2071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King DR. Initial care of the severely injured patient. N Engl J Med. 2019;380:763–770. doi: 10.1056/NEJMra1609326. [DOI] [PubMed] [Google Scholar]
- 10.Aoki R, Kobayashi Y, Nawata S, Kamide H, Yamamoto T, Furugori S, et al. Computed tomography imaging of resuscitative endovascular balloon occlusion of the aorta (REBOA): pearls and pitfalls. Jpn J Radiol. 2021;39:1133–1140. doi: 10.1007/s11604-021-01166-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakajima K, Yamaguchi K, Abe T, Taniguchi H, Mizukami S, Sekikawa Z, et al. Extravasation and outcomes in computed tomography and angiography in patients with pelvic fractures requiring transcatheter arterial embolization: a single-center observational study. J Trauma Acute Care Surg. 2022;92:873. doi: 10.1097/TA.0000000000003446. [DOI] [PubMed] [Google Scholar]
- 12.Costa RF, Yoshida RDA, Gibin RJ, Sobreira ML, Pimenta REF, Bertanha M, et al. Inferior gluteal artery pseudoaneurysm after fall from a bicycle: case report. Jornal vascular brasileiro. 2018;17:353–357. doi: 10.1590/1677-5449.003018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keeling AN, McGrath FP, Lee MJ. Interventional radiology in the diagnosis, management, and follow-up of pseudoaneurysms. Cardiovasc Intervent Radiol. 2009;32:2–18. doi: 10.1007/s00270-008-9440-3. [DOI] [PubMed] [Google Scholar]
- 14.Cordova AC, Sumpio BE. Visceral artery aneurysms and pseudoaneurysms—should they all be managed by endovascular techniques? Ann Vasc Dis. 2013;6:687–693. doi: 10.3400/avd.ra.13-00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raniga SB, Mittal AK, Bernstein M, Skalski MR, Al-Hadidi AM. Multidetector CT in vascular injuries resulting from pelvic fractures: a primer for diagnostic radiologists. Radiographics. 2019;39:2111–2129. doi: 10.1148/rg.2019190062. [DOI] [PubMed] [Google Scholar]
- 16.Shreve L, Jarmakani M, Javan H, Babin I, Nelson K, Katrivesis J, et al. Endovascular management of traumatic pseudoaneurysms. CVIR Endovasc. 2020;3:88. doi: 10.1186/s42155-020-00182-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jesinger RA, Thoreson AA, Lamba R. Abdominal and pelvic aneurysms and pseudoaneurysms: imaging review with clinical, radiologic, and treatment correlation. Radiographics. 2013;33:E71–96. doi: 10.1148/rg.333115036. [DOI] [PubMed] [Google Scholar]
- 18.Loffroy R, Rao P, Ota S, De Lin M, Kwak BK, Krause D, et al. Packing technique for endovascular coil embolisation of peripheral arterial pseudo-aneurysms with preservation of the parent artery: safety, efficacy and outcomes. Eur J Vasc Endovasc Surg. 2010;40:209–215. doi: 10.1016/j.ejvs.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Roblin P, Alexiou T, Sabharwal T, Reidy J, Ross DA. Successful stent-graft placement for the treatment of a superior gluteal artery pseudoaneurysm in a patient following complex pelvic surgery. Br J Radiol. 2007;80:e7–e10. doi: 10.1259/bjr/21729994. [DOI] [PubMed] [Google Scholar]
- 20.Kertesz JL, Anderson SW, Murakami AM, Pieroni S, Rhea JT, Soto JA. Detection of vascular injuries in patients with blunt pelvic trauma by using 64-channel multidetector CT. Radiographics. 2009;29:151–164. doi: 10.1148/rg.291085508. [DOI] [PubMed] [Google Scholar]
- 21.Ring EJ, Athanasoulis CA, Waltman AC, Baum S. The pseudo-vein: an angiographic appearance of arterial hemorrhage. J Can Assoc Radiol. 1973;24:242–244. [PubMed] [Google Scholar]
- 22.Robbs JV, Carrim AA, Kadwa AM, Mars M. Traumatic arteriovenous fistula: experience with 202 patients. Br J Surg. 1994;81:1296–1299. doi: 10.1002/bjs.1800810912. [DOI] [PubMed] [Google Scholar]
- 23.Wenzl FA, Miljkovic SS, Dabestani PJ, Kessler JJ, 2nd, Kotaru TR, Kalamchi LD, et al. A systematic review and individual patient data meta-analysis of heart failure as a rare complication of traumatic arteriovenous fistulas. J Vasc Surg. 2021;73(1087–94):e8. doi: 10.1016/j.jvs.2020.08.138. [DOI] [PubMed] [Google Scholar]
- 24.Perinjelil V, Maraqa T, Chavez Yenter A, Ohaeri H, Mercer L, Bansal A, et al. Traumatic arteriovenous fistula formation secondary to crush injury. J Surg Case Rep. 2018;2018:rjy240. doi: 10.1093/jscr/rjy240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cho HS, Kim Y, Lee J, Yi KS, Choi CH. Use of N-butyl cyanoacrylate in the successful transcatheter arterial embolization of an arteriovenous fistula caused by blunt pelvic fracture: a case report and review of literature. Medicine (Baltimore) 2021;100:e24215. doi: 10.1097/MD.0000000000024215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen JK, Johnson PT, Fishman EK. Diagnosis of clinically unsuspected posttraumatic arteriovenous fistulas of the pelvis using CT angiography. AJR Am J Roentgenol. 2007;188:W269–W273. doi: 10.2214/AJR.05.1230. [DOI] [PubMed] [Google Scholar]
- 27.Erbahceci Salik A, Islim F, Akgul A, Cil BE. Concomitant transarterial and transvenous embolization of a pelvic arteriovenous malformation using a new liquid embolic agent, squid-12 and detachable coils. Case Rep Vasc Med. 2014;2014:972870. doi: 10.1155/2014/972870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goerlich CE, Challa AB, Malas MM. Acute limb ischemia from gunshot wound secondary to arterial vasospasm. J Vasc Surg Cases Innov Tech. 2019;5:99–103. doi: 10.1016/j.jvscit.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shapiro M, McDonald AA, Knight D, Johannigman JA, Cuschieri J. The role of repeat angiography in the management of pelvic fractures. J Trauma. 2005;58:227–231. doi: 10.1097/01.TA.0000152080.97337.1F. [DOI] [PubMed] [Google Scholar]
- 30.Gourlay D, Hoffer E, Routt M, Bulger E. Pelvic angiography for recurrent traumatic pelvic arterial hemorrhage. J Trauma. 2005;59:1168–1173. doi: 10.1097/01.ta.0000189043.29179.e4. [DOI] [PubMed] [Google Scholar]
- 31.Fang JF, Shih LY, Wong YC, Lin BC, Hsu YP. Repeat transcatheter arterial embolization for the management of pelvic arterial hemorrhage. J Trauma. 2009;66:429–435. doi: 10.1097/TA.0b013e31817c969b. [DOI] [PubMed] [Google Scholar]
- 32.Scemama U, Dabadie A, Varoquaux A, Soussan J, Gaudon C, Louis G, et al. Pelvic trauma and vascular emergencies. Diagn Interv Imaging. 2015;96:717–729. doi: 10.1016/j.diii.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 33.Hussain B, Sitto TM, Sethuraman U. Thrombosis of external iliac and common femoral arteries secondary to blunt trauma due to handlebar injury. Am J Emerg Med. 2021;49:291–293. doi: 10.1016/j.ajem.2021.06.035. [DOI] [PubMed] [Google Scholar]
- 34.Sternbergh WC, 3rd, Conners MS, 3rd, Ojeda MA, Money SR. Acute bilateral iliac artery occlusion secondary to blunt trauma: successful endovascular treatment. J Vasc Surg. 2003;38:589–592. doi: 10.1016/S0741-5214(03)00295-7. [DOI] [PubMed] [Google Scholar]
- 35.Watanabe Y, Naganuma T, Hosawa K, Amano T, Yabushita H, Warisawa T, et al. Successful endovascular treatment with a cutting balloon for traumatic obstruction of an external iliac artery in a young male. Int J Cardiol. 2015;201:339–341. doi: 10.1016/j.ijcard.2014.12.147. [DOI] [PubMed] [Google Scholar]
- 36.Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, et al. Pelvic trauma: WSES classification and guidelines. World J Emergency Surg. 2017;12:5. doi: 10.1186/s13017-017-0117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lustenberger T, Störmann P, Eichler K, Nau C, Janko M, Marzi I. Secondary angio-embolization after emergent pelvic stabilization and pelvic packing is a safe option for patients with persistent hemorrhage from unstable pelvic ring injuries. Front Surg. 2020;7:601140. doi: 10.3389/fsurg.2020.601140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kataoka Y, Maekawa K, Nishimaki H, Yamamoto S, Soma K. Iliac vein injuries in hemodynamically unstable patients with pelvic fracture caused by blunt trauma. J Trauma. 2005;58:704–708. doi: 10.1097/01.TA.0000159346.62183.8F. [DOI] [PubMed] [Google Scholar]
- 39.Sueyoshi E, Sakamoto I, Uetani M. Embolization for massive bleeding due to spontaneous left external iliac vein rupture: report of a successful case. CVIR Endovasc. 2021;4:33. doi: 10.1186/s42155-021-00219-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Merchant M, Pallan P, Prabhakar N, Saker M, Resnick SA. Treatment of traumatic thoracic and iliac venous injury with endovascular stent-grafts. J Vasc Interv Radiol. 2013;24:1920–1923. doi: 10.1016/j.jvir.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 41.Mosquera Rey V, Fernandez C, Zanabili A, Del Castro JA, Pandavenes MG, Alonso M. Endovascular repair of iliac vein laceration associated with complex pelvic fracture. Ann Vasc Surg. 2019;54(336):e9–e12. doi: 10.1016/j.avsg.2018.06.020. [DOI] [PubMed] [Google Scholar]
- 42.Sofue K, Sugimoto K, Mori T, Nakayama S, Yamaguchi M, Sugimura K. Endovascular uncovered Wallstent placement for life-threatening isolated iliac vein injury caused by blunt pelvic trauma. Jpn J Radiol. 2012;30:680–683. doi: 10.1007/s11604-012-0100-9. [DOI] [PubMed] [Google Scholar]
- 43.Cha JG, Lee SY, Hong J, Park JM, Lim KH, Kim D. Traumatic iliac vein rupture managed using a bare-metal stent. Trauma Case Reports. 2022;37:100589. doi: 10.1016/j.tcr.2021.100589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tillman BW, Vaccaro PS, Starr JE, Das BM. Use of an endovascular occlusion balloon for control of unremitting venous hemorrhage. J Vasc Surg. 2006;43:399–400. doi: 10.1016/j.jvs.2005.10.034. [DOI] [PubMed] [Google Scholar]