Abstract
High levels of alcohol use and the development of alcohol use disorder (AUD) are associated with various adverse consequences. Resilience has been proposed as a protective factor against increased alcohol use, though the existing research is limited by inconsistencies in the conceptualization and measurement of resilience. As such, the current scoping review examined 14 studies on individual, trait-level resilience as a protective factor against alcohol use and related consequences in adults over the age of 21 in the United States. Findings from the included studies generally suggest resilience as a protective factor against various outcomes, though methodological limitations should be considered. Although future research in this area should improve upon methodological limitations, the present review suggests clinical implications of resilience as beneficial in prevention and intervention programming for alcohol use outcomes.
Keywords: resilience, alcohol, alcohol use disorder
Alcohol is the most widely-consumed recreational substance worldwide (Ferreira & Willoughby, 2008). Indeed, the World Health Organization estimates that in 2016 about 2.3 billion people aged 15 or older had consumed alcohol in the previous 12 months (WHO, 2018).
Alcohol consumption is associated with adverse health consequences such as cirrhosis of the liver, pancreatitis, certain types of cancer, and injuries from road accidents, falls, drownings, and self-harm, among many others, and was responsible for 7.2% of all premature deaths in 2016 (WHO, 2018). Further, alcohol consumption can lead to a significant reduction in the number of years a person lives disability-free, with full health. In 2016, harmful alcohol consumption resulted in a reduction of 132.6 million years of healthy living across the globe (WHO, 2018). In addition to alcohol consumption and harmful alcohol consumption, Alcohol Use Disorder (AUD) is associated with considerable disability (Samokhvalov et al., 2010d), as they are the third-most disabling disease category in high income countries (WHO, 2008).
Considering the prevalence rates and the associated health consequences, identifying protective factors that may buffer against excessive alcohol use is essential for informing prevention and intervention efforts. While there is a substantial body of literature examining the health consequences of increased alcohol consumption (e.g., increased risk for obesity, hypertension, etc; [Oesterle et al., 2004]), as well as various risk and protective factors (e.g., life stress [Gondre-Lewis, et al, 2016], religiosity, etc. [White et al., 2006]), there is a smaller body of literature examining trait-level resilience. Thus, the purpose of this review is to examine the relationship between alcohol and individual, trait-level resilience across adulthood.
Trait Resilience as a Protective Factor
Early research on resilience postulated that it is a crucial factor in determining how people react to and cope with adversity (Kobasa et al., 1982). This idea was further expanded upon to suggest that “resilient” people, when faced with adversity, tend to demonstrate adaptive behavior in the areas of morale, social functioning, and somatic health (e.g. Wagnild & Young, 1993). In more recent literature, resilience is defined as adaptive, lack of negative, or even positive outcomes following adversity and is most commonly conceptualized as a trait (Connor & Davidson, 2003), outcome (Bonanno, 2004) or process (Masten & Naryan, 2012).
Conceptualizing resilience as a trait proposes that resilience is inherent to an individual, such as a personality trait would be, and relatively stable over time (Hu, Zhang, & Wang, 2015). Examining the measures used to assess trait-level resilience throughout the literature provides a more comprehensive view of what is being measured when researchers refer to resilience as a trait. As shown in Table 3, there is no consistently utilized self-report measure of individual, trait-level resilience. Rather, there is a wide range of extant measures that include multiple items tapping into different facets of this construct (e.g., coping, personality traits, etc.). See Table 3 for sample items from measures used in the articles included in the current review.
Table 3.
Trait-level resilience measures
| Measure name | Sample item |
|---|---|
| Brief Resilience Scale (BRS; Smith et al. 2008) | “I bounce back quickly after a hard time” |
| Connor-Davidson Resilience Scale (CD-RISC; Connor & Davidson, 2003) | “I am able to adapt to change” |
| Quantitative resilience measure (Amstadter et al. 2014) | Residuals from a linear regression with interpersonal trauma load as the predictor and PTSD symptoms as the criterion |
| Author created phenotype categories (Nishimi et al., 2021) | Exposed vs. unexposed and higher vs. lower psychological health |
Conceptual Frameworks for the Resilience-Alcohol Relationship
There are two hypothesized pathways through which trait-level resilience may influence the relation between alcohol use and negative internal states/emotions. First, resilience may allow an individual to develop coping strategies that are more adaptive than alcohol use. Extant research exploring indirect pathways provides preliminary evidence for this relationship. Bartone, Hystad, Eid, and Brevik (2012) found that an avoidant coping style promotes alcohol consumption. Further research has demonstrated that resilience levels are associated with a less avoidant, more problem-focused coping style (Campbell-Sills, Cohan, Stein, 2006), perhaps leading to decreased likelihood of coping via alcohol consumption.
Secondly, those individuals with higher levels of resilience may experience negative emotional states less frequently than those with lower levels of resilience, thus using alcohol to cope less frequently. Research has indicated that those higher on resilience display higher levels of positive emotionality and lower levels of negative emotionality, decreasing their vulnerability to developing a substance use disorder (e.g., Belcher, Volkow, Moeller, & Ferre, 2014). Without an agreed upon theory for how resilience may impact alcohol consumption, the current literature has inconsistencies regarding the examination of resilience and alcohol use.
Present Study
As the literature base on individual, trait-level resilience and alcohol phenotypes is emerging, the existing research has yet to be reviewed. Thus, the purpose of this scoping review was to examine the extant research that examines the relationship between individual, trait-level resilience and alcohol use.
Methods
Study Search Procedures
A comprehensive literature search was conducted using two major databases (i.e., PubMed & PsycINFO). The search terms used were “(psychological resilience) + (alcohol use OR alcohol use disorder).” Searches were not limited by date range. These initial search completed in February 2019 yielded 434 studies from PSYCInfo and 238 studies from PubMed. Out of these, 402 articles were identified as duplicates. Next, the abstract of each of the remaining 270 articles were screened for further assessment, 76 being excluded due to not meeting inclusion/exclusion criteria. Of the 194 assessed for eligibility, 180 studies were excluded due to one or more of these criteria. This process resulted in a total of 11 studies for inclusion in the review (see Figure 1 for the PRISMA chart).
Figure 1.
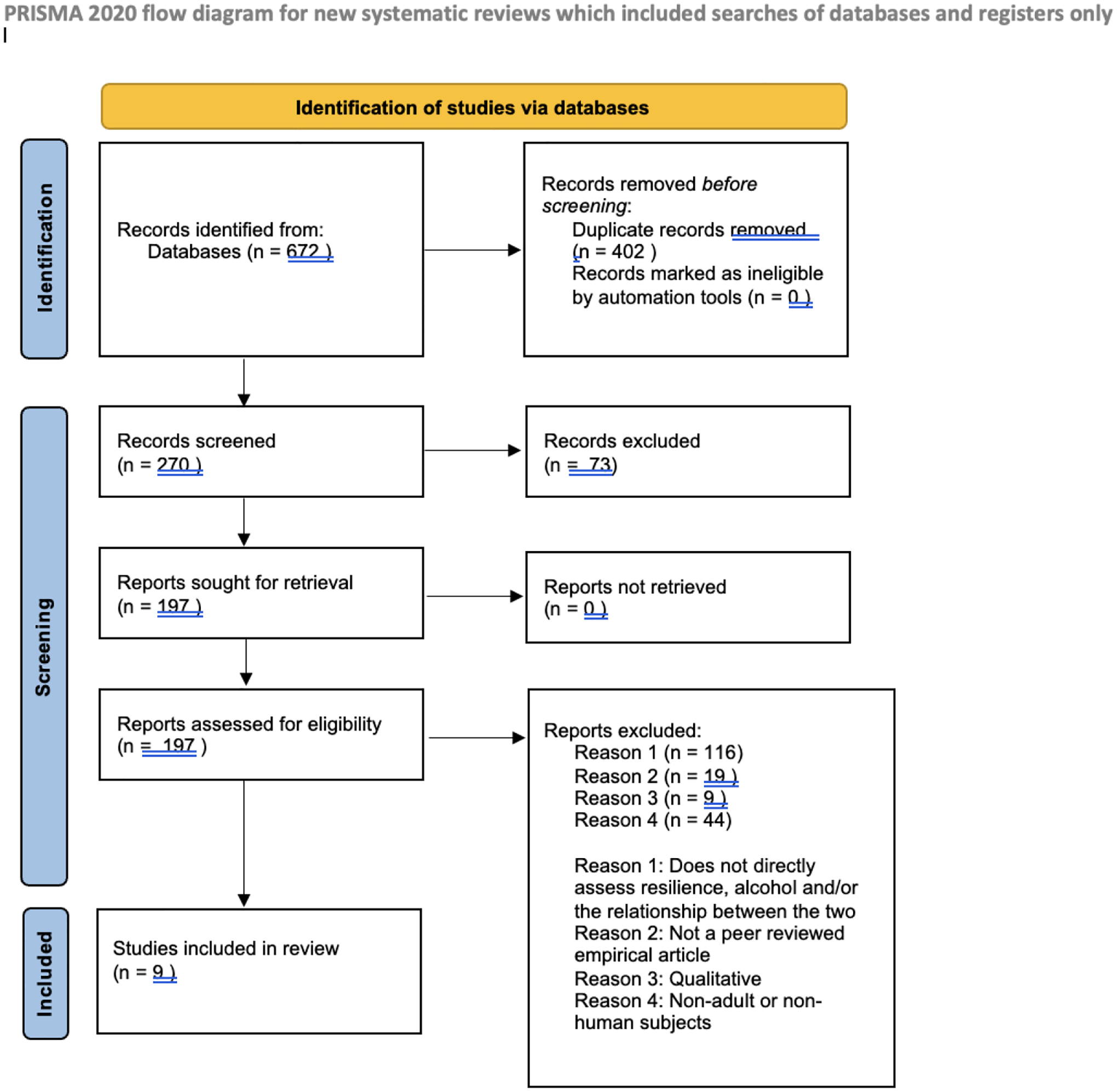
PRISMA flowchart of initial search.
Our search was updated in September 2022 resulting in an additional 190 articles screened, five of which met criteria and were added to the review, for a final total of 14 articles (see Figure 2 for the PRISMA flow chart). Two authors (S.E.C and A.W.W) independently coded articles based on the inclusion and exclusion criteria and found no discrepancies during the coding process (i.e., 100% agreement). Given that this paper is a review, it was exempt from ethical compliance review by the institution’s IRB.
Figure 2.
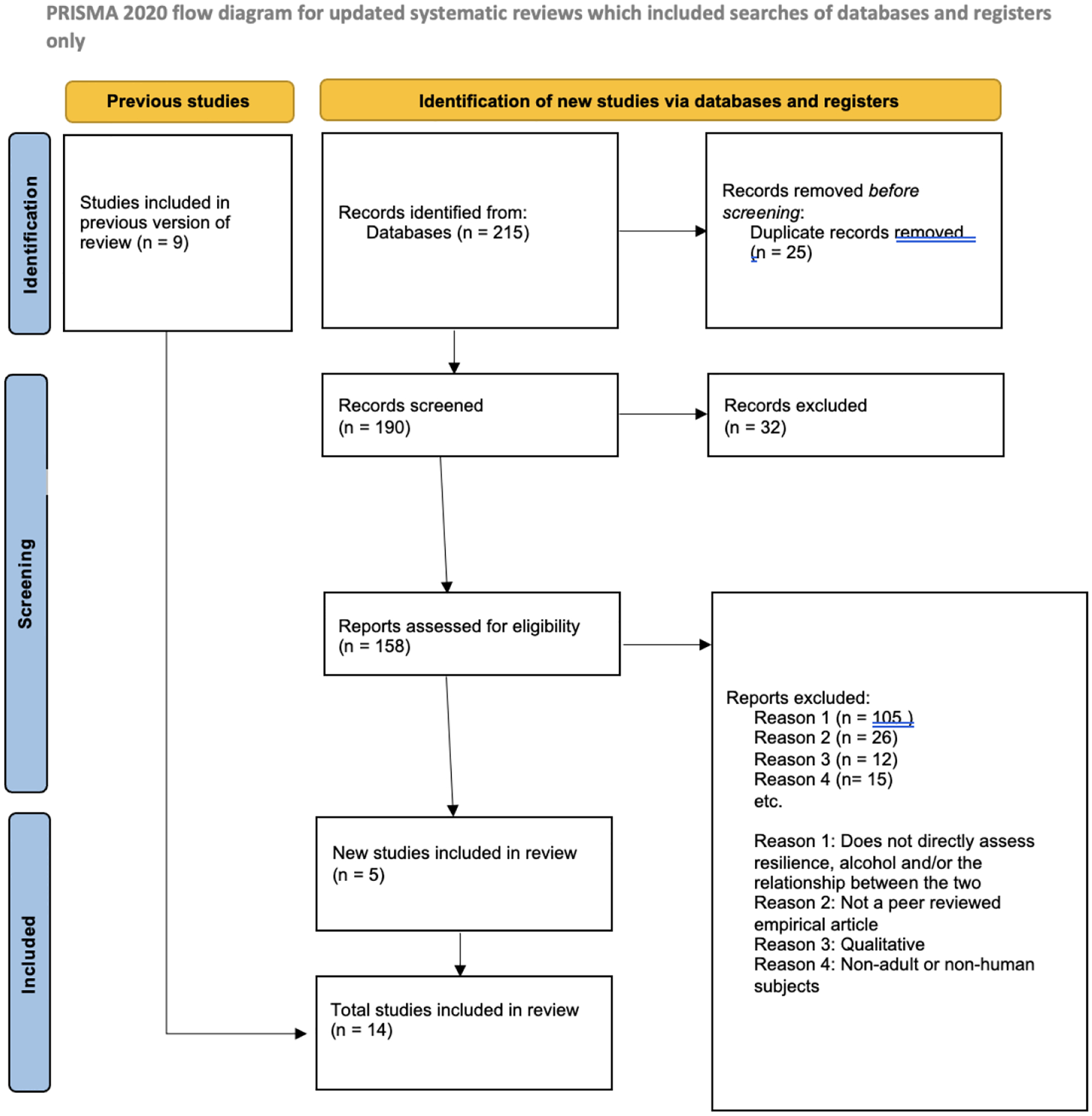
PRISMA flowchart of updated search.
Study Inclusion/Exclusion Criteria
Studies included in the review were those published in peer-reviewed journals, in English. Studies were excluded if they were a conceptual or review article, used qualitative analyses, assessed family- or community-level resilience, evaluated an intervention, included a sample who were under the age of 21 and therefore did not have legal access to alcohol, did not include a proxy for alcohol use as an outcome, did not measure resilience as an individual-based trait, and was not conducted with a U.S. sample. Studies with samples outside the U.S. were excluded in order to control for variance related to the legal age of consumption across countries. Similarly, we only included studies with participants with a mean age of at least 21 or older due to potential skewness and bias in reporting on alcohol consumption in studies with participants under the age of 21. Adolescents who obtain alcohol illegally are less likely to report their consumption in research settings, thus introducing potential bias in findings when examining the relationship between alcohol and resilience.
Studies were coded based on the following characteristics:
Peer-reviewed empirical article, used quantitative methods, non-intervention study, sample age of 21+, study occurring in the U.S., used a self-report measure of individual-based resilience, inclusion of a measure of alcohol consumption [quantity or frequency], alcohol use disorder diagnosis and/or symptoms, or alcohol-related problems/consequences, a statistical test of the direct relationship between resilience and alcohol phenotype.
Quality Assessment
The quality of studies was assessed using The Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies developed by the NIH. This measure contains 14 items (see Figure 3) that assess study design indicators and potential sources of bias.. For each included study, items were marked as “Yes”, “No”, “Cannot determine”, or “Not Applicable” for indicators not relevant to certain study designs. Each “Yes” that a study receives was coded as “1”, with other responses coded as “0”. A total score was created for each study, with higher scores indicating higher quality of research.
Figure 3.
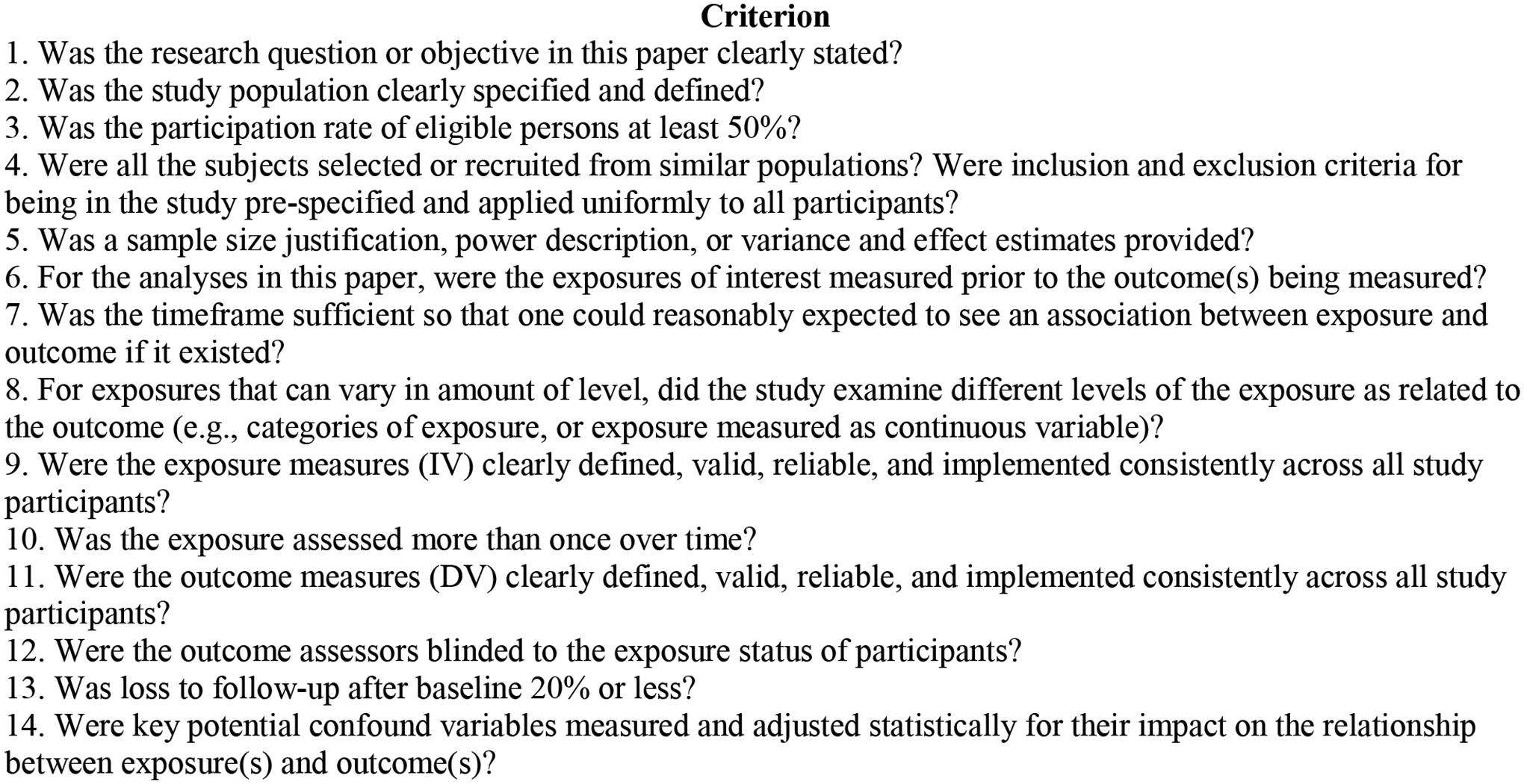
NIH Quality Assessment Criterion.
Results
Fourteen studies were included in the present review. Approximately half of the studies were recruited via the community (k=6), which included samples such as adults living on the U.S./Mexico border, inner-city adults with high rates of childhood abuse, or sexual minority women recruited via Facebook. The remainder of the studies targeted more specific populations such as the adult children of nurses (k=1) to military-involved individuals or Veterans (k=4). Studies were fairly balanced in terms of whether they were majority male (k= 6) or majority female (k=7) participants. One study did not report sample sex distributions for all participants. Twelve studies reported the race/ethnicity breakdown of their sample; ten had majority White samples, and the other two had majority Black samples. Additional study characteristics and key findings are presented in Table 1. Results from a qualitative review of findings and from the quality assessment are summarized below.
Table 1.
Summary of Studies Included in the Scoping Review
| Study | Sample | Adversity measure | Resilience measure | Alcohol measure | Analysis | Study design | Relevant findings |
|---|---|---|---|---|---|---|---|
| Baum et al., (2022) | N= 1430, Mage= NR, 77.0% male, 57.8% Black, non-Hispanic | -None | -BRS | -AUDIT-C | -Multivariate generalized linear mixed models | -Self-report -Cross-sectional |
-Higher levels of resilience were associated with lower risk of alcohol misuse |
| Foley et al., (2022) | N= 191, Mage= 29.3, SD= 6.92, 100% female, 84.5% White | -PSS | -CD-RISC | -AUDIT-C | -Linear and logistic regressions | -Self-report -Cross-sectional |
-Resilience was associated with a lower likelihood of drinking at hazardous levels, but did not moderate the relationship between discrimination and alcohol use |
| Nishimi, Koenen, Coull, & Kubzansky (2021) | N= 3,767; Mage= 25.3, SD= 1.6, 70.0% female, 94.0% White | -Dichotomous exposure to 7 childhood adverse events | -Four phenotype categories based on adversity and psychological health | -Self-report on drinking quantity at baseline and at follow-up | -Repeated measure generalized estimating equation models | -Self-report -Longitudinal |
-Moderate alcohol consumption percentiles did not differ by resilience phenotype -Resilience phenotypes did not predict differential change in likelihood of being healthy (i.e., moderate drinking) over follow-up |
| Wattick, Hagedorn, & Olfert (2021) | N= 2,018, Mage= 24.9, SD= 5.4, 70.7% female, 83.1% White | -PSS-10 item | -BRS | -AUDIT-C | -Standard least squares regression models | -Self-report -Longitudinal |
-Resilience predicted change in alcohol use from pre COVID to since COVID times, with greater resilience predicting a decrease in alcohol consumption |
| Springfield et al., (2020) | N= 77,395, Mage= 77.0, SD= 6.4, 100% female, 89.7% white | −12 items from the Beta-Blocker Heart Attack Trial | -BRS | -Quantity of alcohol use in past 3 months | -Logistic regression models | -Cross-sectional -Self-report |
-High and moderate levels of resilience associated with moderate alcohol intake(no more than 1 drink/day) |
| Green, Beckham, Youssef, & Elbogen (2014) | N=866 Mage=37.0, SD=9.6 73% male; 78% White | -CES | -CD-RISC | -AUDIT -Lifetime history of alcohol abuse |
-Pearson correlations -Multiple linear regression -Logistic regression |
-Longitudinal -Self-report |
-Lower baseline resilience associated with alcohol misuse at 1 year FU |
| Sheerin et al., (2021) | N= 7,441; Mage= 35.5, SD= 9.2, 57% male, Race/ethnicity unreported | −15-item checklist assessing for presence of a variety of negative SLEs | -DBR | -DSM-IV AD symptoms -Lifetime alcohol use, prior year alcohol use |
-Regression analyses; moderation | -Self-report -Longitudinal |
-No significant interaction between resilience and new onset SLEs on AD symptoms -Those with greater resilience and less SLEs reported fewer AD symptoms |
| Sheerin et al., (2019) | N= 1,046, Mage= 36.2, SD= 9.9, 88.0% male, 55.4% White/Caucasian | -Combat Exposure Scale (CES) | -DBR | -AUDIT | -Path analyses | -Cross-sectional -Self-report |
-Greater resilience was associated with lower AUDIT scores |
| Amstadter, Maes, Sheerin, Myers, & Kendler (2016) | N=7,500 twins; Mage=35.1, SD=7.5 Race/ethnicity unreported | -Stressful life events past year | -DBR | -Past 12-month AAD via DSM-IV version of the SCID | -Twin modeling -ACE design with Cholesky decomposition |
-Longitudinal -Self-report -Interview |
-Genetic influence on resilience overlaps with the genetic contribution to AAD |
| Overstreet et al. (2017) | N=6,288 (Mage=46.9, SD=14.5) 59.5% female; 57.8% Non-Hispanic White | -Lifetime “trauma load” -Stressful life events past year |
-DBR | -AUDADIS-IV | -Hierarchical logistic regressions | -Cross-sectional -Interview |
-Resilience scores related to lifetime AD whereby higher resilience was associated with decreased likelihood of dx |
| Wingo, Ressler, & Bradley (2014) | N= 2,2024 Mage=39.0, SD=14.0 70.4% female; 93.4% Black/African American | -CTQ -TEI |
-Abbreviated CD-RISC | -AUDIT | -Linear regression -Logistic regression |
-Cross-sectional -Self-report |
-Resilience negatively related to lifetime alcohol use -Resilience interacted with severity of childhood abuse to reduce harmful alcohol use -Higher resilience scores associated with lower odds of AUD dx |
| Sanchez, Gainza Perez, & Field (2022) | N= 443, Mage= 22.6, SD= 5.09, 68% female, 72.1% White | -None | -BRS | -Frequency and quantity of weekly use -BYAACQ |
-Multiple linear regression, moderation | -Self-report -Cross-sectional |
-Resilience did not moderate the relationship between drinking motive and alcohol use. -Resilience moderated the association between alcohol consequences and drinking motive |
| Green et al. (2010) | N=497 Mage=36.6, SD=10.1 83% male; 52% White | -CES | -CD-RISC | -AUDIT | -Logistic regression | -Cross-sectional -Self-report -Interview |
-Higher resilience associated with lower AUDIT scores, |
| Morgan, Brown, & Bray (2018) | N=320 74% between ages 26 and 60 70.0% male; 64.0% White | -Number of reported stressors and sources of stress | -CD-RISC | -Alcohol related serious consequences | -Multiple regression -Moderation analyses using the PROCESS SPSS macro |
-Cross-sectional -Self-report |
-Resilience predicted alcohol-related consequences -Resilience interacts with stressors to predict alcohol related problems |
Note. Studies in this table are organized by alcohol outcome of interest starting with alcohol consumption, AUD diagnosis, and alcohol-related problems, respectively. AAD=Alcohol abuse or dependence; ACASI= AD=Alcohol dependence; AD= Alcohol dependence; AUD=Alcohol use disorder; AUDADIS-IV= Alcohol Use Disorder and Associated Disabilities Interview; AUDIT=Alcohol Use Disorders Identification Test; ANOVA=analysis of variance; BRS= Brief Resilience Scale; BYAACQ= Brief-Young Alcohol Consequences Questionnaire; CCQ=California Child Q-Sort; CD-RISC= Connor-Davidson Resilience Scale; CTQ=Childhood Trauma Questionnaire; CAGE=Cut-down, Annoyed, Guilty, Eye-Opener; CES=Combat Experiences Scale; DARBI=Dis-regulated Alcohol-Related Behaviors Inventory; DBR=Discrepancy based measure of resilience; DDHx=Drinking and drug history; DISC-IV=Diagnostic Interview Schedule for Children-Version IV; DSM-IV= Diagnostic and Statistical Manual of Disorders IV; Dx=Diagnosis; EGEP-5= Global Posttraumatic Stress Scale; ERI-Q=Effort-Reward Imbalance Questionnaire; ERS= Essential Resilience Scale; MCMI-III= Millon Clinical Multiaxial Inventory-III; OLS=Ordinary Least Squares Regression; PARQ= Parental Acceptance and Rejection Questionnaire; PCS=Perceived Stress Scale; RS=Resilience Scale; RS-14=14-item Resilience Scale; SCID= Structured Clinical Interview; SEM=Structural Equation Modeling; SLE= Stressful life event; SMAST= Short Michigan Alcoholism Screening Test; TEI=Traumatic Events Inventory; YSR=Youth Self-Report Scale;
Qualitative Review
Resilience and Alcohol Consumption
Five studies (35.7%) examined resilience as related to alcohol consumption levels. Four studies out of these five documented that higher resilience was associated with lower rates of alcohol consumption, including a study by Wattick, Hagedorn, and Olfert (2021) who found that, over the transition from prior to the COVID-19 pandemic to during, resilience predicted a decrease in consumption. Wingo, Ressler, and Bradley (2014) demonstrated that resilience was negatively associated with lifetime alcohol use. Most recently, both Baum and colleagues (2022) found that higher levels of resilience were related to lower alcohol consumption in the context of the COVID-19 pandemic. Springfield and colleagues (2020) found high and moderate levels of resilience to be associated with moderate alcohol intake, which they defined as no more than one drink per day. In contrast, one study did not find support for a significant relationship between resilience and alcohol consumption (i.e., Nishimi, Koenen, Coull, & Kubzansky, 2021).
Resilience and Alcohol Misuse
Seven of the reviewed studies (50.0%) explored whether resilience was related to disordered drinking or alcohol-related problems in one’s life. One study documented a negative association between resilience and alcohol-related consequences (Morgan et al., 2018). Sheerin and colleagues (2019) found that greater levels of resilience was associated with lower levels of unhealthy alcohol use, as measured by scores ≥8 on the AUDIT. In additional work, Sheerin et al., (2021) demonstrated that resilience and new onset stressful life events did not interact to predict Alcohol Dependence symptoms. Results from Green et al. (2014) support the longitudinal relationship between resilience and alcohol, demonstrating that higher baseline resilience was associated with lower alcohol misuse, as measured by scores on the Alcohol Use Disorders Identification test (AUDIT), at one-year follow up. Additional work by Green and colleagues (2010) found that higher resilience scores were related to lower AUDIT scores, even after account for PTSD symptoms. Findings from both Baum et al., (2022) and Foley et al., (2022) demonstrated that higher levels of resilience were associated with a lower likelihood of engaged in hazardous drinking as assessed by the AUDIT-C. All studies examining the relationship between resilience levels and alcohol misuse found a significant relationship between the two.
Resilience and Alcohol Use Disorder/Alcohol Dependence
Three studies (21.4%)examining the relationship between resilience and AUD symptoms found that higher resilience was associated with lower odds of developing AUD. In their investigation of genetic influences on resilience and alcohol use, Amstadter et al. (2014) found that, resilience and Alcohol Abuse/Dependence (AAD) are negatively correlated, and that the genetic influence on resilience modestly overlapped with the genetic contribution to AAD, with 20% of the heritability being common to both. Overstreet and colleagues (2017), in their sample of community-dwelling U.S. adults, demonstrated that resilience scores were related to a lifetime diagnosis of AD whereby higher resilience was associated with a decreased likelihood of being diagnosed with AD. Similarly, results from Wingo et al., (2014) support higher levels of resilience as related to a lower likelihood of being diagnosed with AUD.
Resilience as a Moderator and/or Mediator
Seven studies examined resilience as a moderating or mediating variable, three supported resilience as a moderating or mediating variable. Sanchez, Gainza Perez, and Field (2022) found that resilience moderated the association between alcohol consequences and drinking motive, though did not moderate the relationship between drinking motive and alcohol use. More specifically, the authors found that resilience moderated the relationship between social and enhancement drinking motives and alcohol consequences as measured by the Brief-Young Alcohol Consequences Questionnaire, whereby at higher levels of resilience, higher social and enhancement motives no longer predicted higher alcohol consequences.
Resilience frequently mediated or moderated the relation between stress or trauma and alcohol use. Wingo, Ressler, and Bradley (2014) demonstrated that resilience interacted with the severity of childhood abuse to reduce harmful alcohol use. Sheerin and colleagues (2021) found no significant interaction between resilience and new onset of a stressful life event with alcohol dependence symptoms, though participants with greater resilience and fewer stressful life events reported fewer symptoms of alcohol dependence. Resilience was also found to interact with stressors to predict alcohol related problems, where at high levels of stress, the number of alcohol related consequences were twice as many for the low resilience group as were for the high (Morgan et al., 2018). One study did not find support for resilience as a moderating variable in the context of discrimination (Foley et al., 2022), on past three-month alcohol consumption quantity.
Quality Assessment
The scientific quality of studies varied. The number of quality indicators ranged from 6 to 12 out of a maximum of 14 (M= 8.29, SD=2.094).
Quality indicator scores of outlier (i.e., non-significant) studies are useful in providing additional context to explain the mixed findings outlined in the qualitative assessment above. Table 2 provides a list of each study’s quality indicators. The one study that did not find a significant relationship between individual-level resilience and alcohol outcome had a quality rating score that fell just at the overall mean (Nishimi et al., 2021). Nishimi and colleagues (2021) assessed resilience categorically based on exposure to childhood adverse events and reported psychological health, whereas the majority of the studies with significant findings operationalized resilience in a continuous way. The studies that did find a significant relationship between individual-level resilience and alcohol outcome had approximately equal proportions of studies with quality ratings above and below the overall mean (6 above; 7 below). Taken together, there is a wide range in the quality of the existing research examining resilience and alcohol outcomes. In turn, the specific methodological limitations of the extant literature will be discussed.
Table 2.
NIH Quality Assessment.
| Item Number | Sanchez, Gainza Perez, & Field (2022) | Nishimi, Koenen, Coull, & Kubzansky, 2021 | Sheerin et al., 2021 | Wattick, Hagedorn, & Olfert, 2021 | Morgan, Brown, & Bray., 2018 | Overstreet et al., 2017 | Wingo, Ressler, & Bradley, 2014 | Green, Beckham, Youssef, & Elbogen, 2014 | Amstadter et al., 2016 | Green et al., 2010 | Springfield et al., 2020 | Sheerin et al., 2019 | Baum et al., 2022 | Foley et al., 2022 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 2 | Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y |
| 3 | N | N | NR | N | NR | NR | NR | Y | Y | NR | Y | NR | NR | NR |
| 4 | N | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 5 | N | Y | Y | Y | N | N | N | Y | N | N | Y | Y | Y | Y |
| 6 | N | Y | N | N | N | N | N | Y | Y | N | Y | N | N | N |
| 7 | N | Y | Y | Y | N | N | N | Y | Y | N | Y | Y | Y | Y |
| 8 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 9 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 10 | N | Y | N | N | N | N | N | Y | Y | N | N | N | N | N |
| 11 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y |
| 12 | N | N | N | N | N | N | N | N | N | N | N | N | N | N |
| 13 | NA | N | NA | NA | NR | NR | NR | N | N | NR | Y | NA | Y | NA |
| 14 | Y | Y | Y | Y | Y | NA | Y | Y | N | N | Y | Y | Y | Y |
| Total: | 6 | 8 | 7 | 7 | 7 | 6 | 7 | 12 | 10 | 6 | 12 | 9 | 10 | 9 |
Discussion
The primary aim of this review was to examine the association between individual, trait-level resilience and alcohol use. Of the 14 studies reviewed, 13 found a significant relationship between resilience and alcohol use outcomes. The primary theme that emerges suggests resilience may protect against excessive alcohol consumption, AUD symptoms, and alcohol-related problems.
Implications
The current review suggests that individual-based resilience is an important protective factor in relation to alcohol use. Although the literature contains notable methodological limitations, the evidence holds important clinical implications, suggesting resilience may improve alcohol use and related outcomes. Many of the self-report measures of resilience used in the included studies assess facets (e.g., coping style,) that can be improved with treatment efforts to increase resilience, and thus improve functional outcomes. Indeed existing work has examined the broadness of one’s repertoire of coping skills as related to alcohol treatment outcomes, and has demonstrated that those with broad repertoires of coping strategies have the best treatment outcomes (Roos & Witkiewitz, 2016).
It is likely that improving resilience is an effective strategy to improve alcohol outcomes. In adults seeking treatment for AUD, assessing for resilience levels at baseline would allow clinicians to identify which participants need additional assistance building resiliency to improve intervention outcomes. In a sample of military adults, Griffith and West (2013) found that the Army’s Master Resilience Training (MRT), which includes modules on optimism, self-awareness, mental agility, communication, and self-regulation enhanced Veteran’s abilities to cope with stressful events. Applying and adapting existing intervention modules that target facets of trait resilience to populations with AUD may improve treatment outcomes and reduce the burden of alcohol use.
Methodological Considerations
Although the articles reviewed have advanced our understanding of individual, trait-based resilience as a protective factor for alcohol use and related problems, there are several limitations that should be addressed.
Measurement Considerations
There is heterogeneity in the literature with regard to how both the stressor and resilience are measured, creating the potential for error and bias, and limiting the ability to synthesize the literature as a whole. As, theoretically, resilience can only be studied in the context of having experienced adversity, it would follow that studies include only participants who have experienced adversity, and report on the sample’s exposure to adversity. Twelve studies included in the present review assessed for exposure to a stressor, though fewer reported descriptive statistics for the stressor variable, precluding the ability to know the degree of exposure within their sample Including participants with no exposure to adversity in an examination of resilience poses a conceptual concern about the meaning of findings, as resilience cannot truly be measured in the absence of adversity.
When a measure of adversity was included, measures ranged greatly in terms of severity and timing (i.e., childhood trauma vs. current job stress). The timing and type of an adverse event (e.g., interpersonal trauma in childhood vs. life stress in adulthood) has been consistently shown to be associated with alcohol use and related consequences (e.g., Rothman et al., 2008), suggesting that trait-level resilience may be more important in samples exposed to early, or more severe adversity. Although assessing a wide variety of stressors allows for inferences to be made to a wider breadth of individuals, it creates difficulties in comparing across studies, and poses a threat to internal validity.
The second measurement issue is the lack of a consistent conceptualization of individual, trait-based resilience. As such, synthesizing the literature on resilience and alcohol is made increasingly difficult by the variety of measures used. Across the 14 reviewed studies, four different measures of resilience were used (see Table 3). Broadly, two themes emerged: measures that include a majority of items that assess one’s perceived ability and strategies for coping and measures that include a majority of items that assess individual, personality characteristics that may promote a resilient response. Results showed that when resilience was conceptualized as facets of personality, other internal assets, or as a quantitative construct considering stressor load and reported distress, it was significantly related to decreased alcohol-use (e.g., Sheerin et al., 2019). This highlights the importance of differentiating items assessing coping abilities versus personality assets when creating measures of individual based, trait-level resilience.
A third measurement issue is the heterogeneity in measures used to assess alcohol use and associated outcomes. Consistency in measurement of alcohol outcomes is a difficult feat, given the vast heterogeneity of alcohol outcomes, which can be operationalized on a continuum of severity, ranging from occasional binge drinking to chronic heavy drinking. The present review included proxies for alcohol outcomes ranging from present consumption, to alcohol use disorder diagnosis, among others, with some studies assessing more than one of these outcomes. The lack of consistency in proxies used for alcohol outcomes does not allow for straightforward comparisons across studies, further limiting the inferences that can be made about the literature as a whole.
Lastly, the biases inherent in the use of self-report measures are critical to consider when assessing resilience. While these measures are useful in providing information about one’s perceived level of resilience, self-report measures do not provide information about any functional outcome, which may be more representative of how one is adapting following adversity. Four studies (Sheerin et al., 2021; Sheerin et al., 2019; Amstadter et al. 2016; Overstreet et al. 2017) operationalized resilience in a quantitative way, accounting for reported stressor load and symptoms of distress, whereby those with high amounts of trauma exposure and low symptoms were classified as more resilient when compared to those with low trauma exposure and high symptomology. All studies found significant results for a relationship between alcohol use and resilience. Taking into account stressor load as well as a functional outcome (e.g., symptoms of anxiety/depression), although still self-report, provides more concrete information about the ability to adapt after adversity as compared to one’s reported perceived ability to cope.
Sample Considerations
The variation in sample recruitment and constitution is both an empirical strength and a weakness. This variability certainly limits the ability to compare and synthesize results across studies. However, the extension of the examination of resilience and alcohol use beyond convenience samples (e.g., college undergraduates) increases external validity. The inclusion of samples from a diversity of backgrounds allows for inferences to be made across a wider breadth of individuals, and ideally, will lead to a more broad dissemination of prevention and intervention efforts.
Race/ethnicity and sex are important sample characteristics to consider, as rates of trauma/adversity exposure and alcohol use vary across these demographic lines. Males are more likely to be exposed to potentially traumatic events (e.g., physical assault, combat exposure, etc.), but females are more likely to experience sexual assault, child sexual abuse, and nonsexual child abuse or neglect (for a review see Tolin and Foa, 2008). Males are more than twice as likely than women to develop AUD (Goldstein, Dawson, Chou, & Grant, 2012). However, the prevalence of alcohol consumption, binge drinking, and rates of AUD are increasing more in females than in males (White et al., 2015). Further, extant studies have demonstrated that females are more vulnerable to alcohol-related consequences such as liver inflammation, cardiovascular disease, hangovers, and certain cancers (e.g., CDC, 2019; Kirpich et al., 2017, etc.) Although sex differences are not well-established for individual, trait-level resilience, the sex discrepancies in stressor exposure and alcohol use highlight the need for consideration of sex in both sample ascertainment and data analytic plan.
Race and ethnicity were represented to a less balanced degree than sex within the current review. This imbalance in representation is a noteworthy limitation given the evidence suggesting ethnic and racial differences in both trauma exposure and alcohol use. Prevalence rates of alcohol consumption and AUD vary according to ethnicity whereby Native Americans/Alaska Natives display the highest prevalence of lifetime AUD (43.4% percent), followed by White (32.6%), Latinx (22.9%), Black (22.0%), and Asian American/Pacific Islander/Native Hawaiian (15.0%) individuals (Vaeth, Wang-Schweig, & Caetano, 2017). Although the extant literature has largely focused only on monoracial people, multiracial individuals report an increased likelihood of using alcohol as compared to monoracial individuals (e.g., Goings et al., 2018) as well as increased rates of AUD (i.e., 57.1% [Chong et al., 2016]), highlighting the need to incorporate diverse samples with regard to race and ethnicity in future research.
Additionally, research has consistently demonstrated racial and ethnic differences in trauma exposure whereby Whites are more likely to experience any trauma, while those identifying as either Black or Latinx are at a higher risk of experiencing interpersonal trauma such as childhood maltreatment (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). Further, those identifying as American Indian and/or Alaskan Native experience higher rates of domestic violence, sexual violence, homicide and other violent crimes as compared to Nnon-Hispanic White populations (Rosay, 2016; Yuan et al., 2006), which in turn lead to higher rates of substance use disorders (SAMHSA, 2017). Given that interpersonal trauma is typically more severe in nature, Black, Latinx, and American Indian/Alaskan Native individuals may be more prone to experiencing adverse outcomes (e.g., increased alcohol use) as aresult. Additionally, individuals identifying as a racial or ethnic minority are expected to show resilience in the wake of racial discrimination and trauma, likely furthering the disparity in alcohol consumption and related outcomes (e.g., Skewes & Blume, 2019). These prevalence rates warrant the comparing of differences between ethnic and racial minorities, as opposed to using White as a reference group and subsequently comparing minority groups to Whites, as is commonly seen throughout the literature (Huang et al., 2006). Further, internal validity is threatened by the failure to account for important demographic variables whereby sex and race/ethnicity may explain study outcomes, even when they are not the independent variable. Low internal validity across studies produces an inconsistent literature, resulting in a lack of empirically-based treatments for problematic alcohol consumption (i.e., resilience building approaches).
Study Design Considerations
Extant research theorizes that resilience acts as a buffer, protecting against adverse outcomes (i.e., alcohol consumption) in the face of new onset adversity. Given the assumed ordering of the buffering hypothesis whereby resilience levels are assessed at “baseline,” adversity exposure as occurring after that, and alcohol consumption assessed subsequent to the adversity, longitudinal designs are required to truly test the buffering hypothesis. However, nine studies used a cross-sectional design, which precludes any resolve in the temporal ordering between these variables (Kazdin, 2003). Further, although five studies employed a longitudinal design, only four tested the buffering hypothesis in which resilience buffers the onset of new stressors against alcohol use outcomes. Although the buffering hypothesis is used to theoretically explain the relation between resilience and alcohol, few test this hypothesis in a sound research design, precluding methodologically rigorous evidence.
Future Directions
There were consistent methodological limitations across the papers reviewed, and as such, future research would greatly benefit from addressing these limitations. The heterogeneity in resilience, alcohol, and adversity measurement should be addressed in future work. For example, in designing a longitudinal study, a measure of adversity should not only be administered at each time-point, but should serve as an inclusion criterion at baseline upon entry into the study. Further, measures of both trait-level resilience, as well as alcohol consumption should be kept consistent across time-points to allow for comparison.
In addition to addressing the aforementioned limitations, incorporating genetic research methodology into investigations of resilience and alcohol use would help to elucidate potential underlying mechanisms through which the two are related. For example, polygenic risk scores (PRS; see Dudbridge, 2013, for a detailed description) is an approach that allows for better understanding of the shared molecular etiology between resilience and AUD. Improved understanding of the etiology of resilience, and how it may overlap with the etiology of AUD, may inform the advancement, timing, and delivery of specialized prevention/intervention efforts. Further, identifying variants associated with psychiatric resilience through methods such as Genome Wide Association studies (GWAS) can serve to suggest resilience promoting pathways and genes that can be targeted by pharmacotherapies (i.e., “precision medicine”; Manchia, Pisanu, Squassina, & Carpiniello, 2020)
Conclusions
Results from the current review suggest that trait-level resilience is important relative to alcohol outcomes. However, there are notable methodological constraints that make it difficult to compare across studies. With future research addressing the aforementioned limitations, namely: using longitudinal data sources, aiming for consistency in measurement approaches, and more rigorously considering adversity in their samples, the synthesis of the extant literature base will be made much stronger. Nevertheless, the current review provides evidence for individual-based resilience as an important protective factor in relation to various alcohol phenotypes.
Highlights:
Alcohol consumption is associated with mental and physical health consequences
Resilience is a protective factor against risky alcohol consumption
The extant literature suggests resilience is worth further investigating
Future work should address methodological limitations of the extant literature
Funding and Conflicts of Interest:
The authors do not have any conflicts of interest to report. SC’s time is supported by 5T32MH020030-23 and AA’s time is supported by 1R01AA030010-01.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data Availability Statement:
No new data were generated or analysed in support of this research.
References
- Administration, S. A. a. M. H. S. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS). Retrieved from Rockville, MD:
- Balmer GM, Pooley JA, & Cohen L (2014). Psychological resilience of Western Australian police officers: relationship between resilience, coping style, psychological functioning and demographics. Police practice and research, 15(4), 270–282. [Google Scholar]
- Bartone PT, Hystad SW, Eid J, & Brevik JI (2012). Psychological hardiness and coping style as risk/resilience factors for alcohol abuse. Military medicine, 177(5), 517–524. [DOI] [PubMed] [Google Scholar]
- Belcher AM, Volkow ND, Moeller FG, & Ferré S (2014). Personality traits and vulnerability or resilience to substance use disorders. Trends in cognitive sciences, 18(4), 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonanno GA (2004). Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol, 59(1), 20–28. doi: 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- Campbell-Sills L, Cohan SL, & Stein MB (2006). Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour research and therapy, 44(4), 585–599. [DOI] [PubMed] [Google Scholar]
- Claros E, & Sharma M (2010). The relationship between emotional intelligence and abuse of alcohol, marijuana, and tobacco among college students. Dissertation Abstracts International, 71(05). [Google Scholar]
- Cohen J (1992). A power primer. Psychological bulletin, 112(1), 155. [DOI] [PubMed] [Google Scholar]
- Connor KM, & Davidson JR (2003). Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety, 18(2), 76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Falk D, Yi HY, & Hiller-Sturmhöfel S (2008). An epidemiologic analysis of co-occurring alcohol and drug use and disorders: findings from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC). Alcohol Research & Health, 31(2), 100. [PMC free article] [PubMed] [Google Scholar]
- Ferreira MP, & Willoughby D (2008). Alcohol consumption: the good, the bad, and the indifferent. Appl Physiol Nutr Metab, 33(1), 12–20. doi: 10.1139/H07-175 [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Chou SP, & Grant BF (2012). Sex differences in prevalence and comorbidity of alcohol and drug use disorders: results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of studies on alcohol and drugs, 73(6), 938–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AL, Faulkner B, & Wekerle C (2013). The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child abuse & neglect, 37(1), 22–32. [DOI] [PubMed] [Google Scholar]
- Guo J, Hawkins JD, Hill KG, & Abbott RD (2001). Childhood and adolescent predictors of alcohol abuse and dependence in young adulthood. J Stud Alcohol, 62(6), 754–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KT, Beckham JC, Youssef N, & Elbogen EB (2014). Alcohol misuse and psychological resilience among US Iraq and Afghanistan era veterans. Addictive behaviors, 39(2), 406–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith J, & West C (2013). Master resilience training and its relationship to individual well-being and stress buffering among Army National Guard soldiers. The journal of behavioral health services & research, 40(2), 140–155. [DOI] [PubMed] [Google Scholar]
- Harford TC, & Muthen BO (2001). Alcohol use among college students: the effects of prior problem behaviors and change of residence. J Stud Alcohol, 62(3), 306–312. [DOI] [PubMed] [Google Scholar]
- Hill PL, & Edmonds GW (2017). Personality development in adolescence. In Personality development across the lifespan (pp. 25–38). Academic Press. [Google Scholar]
- Hjemdal O, Friborg O, Stiles TC, Rosenvinge JH, & Martinussen M (2006). Resilience predicting psychiatric symptoms: A prospective study of protective factors and their role in adjustment to stressful life events. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 13(3), 194–201. [Google Scholar]
- Hu T, Zhang D, & Wang J (2015). A meta-analysis of the trait resilience and mental health. Personality and Individual Differences, 76, 18–27. [Google Scholar]
- Johnson N, Dinsmore JA, & Hof DD (2011). The relationship between college students’ resilience level and type of alcohol use. International journal of psychology: a biopsychosocial approach, 2011,[Vol.] 8, p. 67–82. [Google Scholar]
- Kazdin AE (2003). Research design in clinical psychology.
- Kobasa SC (1982). The hardy personality: Toward a social psychology of stress and health. Social psychology of health and illness, 4, 3–32. [Google Scholar]
- Masten AS, & Narayan AJ (2012). Child development in the context of disaster, war, and terrorism: pathways of risk and resilience. Annu Rev Psychol, 63, 227–257. doi: 10.1146/annurev-psych-120710-100356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley PM, Johnston LD, & Bachman JG (1998). Alcohol use among adolescents. Alcohol Health Res World, 22(2), 85–93. [PMC free article] [PubMed] [Google Scholar]
- Oesterle S, Hill KG, Hawkins JD, Guo J, Catalano RF, & Abbott RD (2004). Adolescent heavy episodic drinking trajectories and health in young adulthood. J Stud Alcohol, 65(2), 204–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization, W. H. (2018). Global status report on alcohol and health 2018. Retrieved from Geneva:
- Overstreet C, Stratton KJ, Berenz E, Sheerin CM, Roberson-Nay R, & Amstadter AB (2017). Resilience to interpersonal trauma and decreased risk for psychopathology in an epidemiologic sample. Journal of Psychopathology and Behavioral Assessment, 39(3), 506–513. [Google Scholar]
- Pisarska A, Eisman A, Ostaszewski K, & Zimmerman MA (2016). Alcohol and cigarette use among Warsaw adolescents: Factors associated with risk and resilience. Substance Use Misuse, 51(10), 1283–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole JC, Dobson KS, & Pusch D (2017). Childhood adversity and adult depression: The protective role of psychological resilience. Child Abuse Negl, 64, 89–100. doi: 10.1016/j.chiabu.2016.12.012 [DOI] [PubMed] [Google Scholar]
- Reed D, Reno J, & Green D (2016). Sexual violence among youth in New Mexico. Family & community health, 39(2), 92–102. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological medicine, 41(1), 71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos CR, & Witkiewitz K (2016). Adding tools to the toolbox: The role of coping repertoire in alcohol treatment. Journal of Consulting and Clinical Psychology, 84(7), 599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheerin CM, Lind MJ, Brown EA, Gardner CO, Kendler KS, & Amstadter AB (2018). The impact of resilience and subsequent stressful life events on MDD and GAD. Depress Anxiety, 35(2), 140–147. doi: 10.1002/da.22700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spear LP (2000). The adolescent brain and age-related behavioral manifestations. Neurosci Biobehav Rev, 24(4), 417–463. [DOI] [PubMed] [Google Scholar]
- Sjölund S, Hemmingsson T, & Allebeck P (2015). IQ and level of alcohol consumption—findings from a national survey of Swedish conscripts. Alcoholism: clinical and experimental research, 39(3), 548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinhardt M, & Dolbier C (2008). Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. Journal of American college health, 56(4), 445–453. [DOI] [PubMed] [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive behaviors, 37(7), 747–775. [DOI] [PubMed] [Google Scholar]
- Squeglia LM, & Gray KM (2016). Alcohol and Drug Use and the Developing Brain. Curr Psychiatry Rep, 18(5), 46. doi: 10.1007/s11920-016-0689-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagnild G, & Young H (1993). Development and psychometric. Journal of nursing measurement, 1(2), 165–17847. [PubMed] [Google Scholar]
- Wingo AP, Ressler KJ, & Bradley B (2014). Resilience characteristics mitigate tendency for harmful alcohol and illicit drug use in adults with a history of childhood abuse: A cross-sectional study of 2024 inner-city men and women. Journal of psychiatric research, 51, 93–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A, & Hingson R (2013). The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res, 35(2), 201–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, McMorris BJ, Catalano RF, Fleming CB, Haggerty KP, & Abbott RD (2006). Increases in alcohol and marijuana use during the transition out of high school into emerging adulthood: The effects of leaving home, going to college, and high school protective factors. J Stud Alcohol, 67(6), 810–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhite ER, Ashenhurst JR, Marino EN, & Fromme K (2017). Freshman year alcohol and marijuana use prospectively predict time to college graduation and subsequent adult roles and independence. J Am Coll Health, 65(6), 413–422. doi: 10.1080/07448481.2017.1341892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M (2016). Drinking Over the Lifespan: Focus on Early Adolescents and Youth. Alcohol Res, 38(1), 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle G, Bennett KM, & Noyes J (2011). A methodological review of resilience measurement scales. Health and quality of life outcomes, 9(1), 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2018). Global status report on alcohol and health 2018. Accessed from https://www.who.int/publications/i/item/9789241565639
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research.


