Abstract
Purpose:
Gender-affirming hormones and/or surgeries seeking to change the body can have potentially lasting effects. Changes in requests for these therapies among gender diverse youth are not well understood. The study aim is to characterize factors associated with shifts in gender-related medical requests.
Methods:
This mixed-methods study used retrospective chart review and qualitative interviews with clinicians. Of 130 youth receiving clinical gender care at Children’s National Hospital, 68 met inclusion criteria. Qualitative interview analysis was performed to identify patterns and themes around shifts in gender-related medical requests over time. Statistical analysis employed chi-square and t-tests to compare characteristics in the shift versus no-shift groups and kappa statistics to calculate qualitative coding agreement.
Results:
Of the 68 youth followed over time (mean age 15.11 years, 47% autistic, 22% nonbinary), 20 (29%) reported a shift in request. No significant differences were found by age, autism status, or designated sex at birth. More youth with shifts were nonbinary (p = 0.012). Six shift profiles were identified from qualitative interviews with excellent reliability (κ = 0.865). Four of the profiles reflect shifts in request prior to starting treatment (85% sample); two involved shifts after commencing treatment (15%). The most common profile reflected a medical request that was made, withdrawn, and re-requested (45%).
Conclusions:
Shifts in gender-affirming medical requests by gender diverse youth may not be uncommon during the adolescent’s gender discernment process, and may more likely occur among nonbinary youth. Many individuals who experience shifts away from medical treatment may later resume the request.
Keywords: transgender, gender diverse, gender affirming hormones, gender affirming surgery, gender dysphoria, gender incongruence, adolescence
Best practices for providing care to gender diverse youth are of key interest, with sociocultural, medical, and legal implications.1,2 While difficult to estimate what proportion of youth are gender diverse, recent polls from 2021 note an increased prevalence of transgender identity among Generation Z (born 1997–2003), concordant with reports of increasing numbers of gender diverse youth presenting for clinical care.3,4
Gender-affirming medical options for gender-diverse youth include: (1) pubertal suppression in early puberty; (2) gender affirming hormones starting in mid-late adolescence; and, (3) gender affirming surgeries (often at the age of majority, with some surgeries available to minors [top surgery or chest wall/breast surgery]).5,6 Pubertal suppression affords gender-diverse youth time to consider whether to pursue gender affirming hormonal and/or surgical interventions, pausing endogenous puberty. Stopping pubertal suppression causes puberty to resume, so this intervention is currently believed to be fully reversible (though possible lasting side effects are currently the subject of research)4,7–9. Unlike pubertal suppression, gender-affirming hormones and/or surgery have less reversibility; current guidelines recommend them only after careful evaluation with the young person. Care standards for gender-diverse youth emphasize the importance of continuity of gender diversity over time to commence gender affirming hormonal and/or surgical interventions.5,6
The emphasis on continuity of a young person’s gender diversity is rooted in the current limited understanding of how gender diversity and gender-related needs may or may not change over time. Clinical research has described three patterns of gender diversity-related changes: (1) the “persistence or desistance” of gender diversity experiences, especially from prepuberty to puberty10–12; (2) the experience of detransition (or retransition)13,14, in which an individual assumes their designated gender at birth and/or concludes their gender-related treatment; and (3) the phenomenon of “persistence-after-interruption,” wherein an individual experiences an attenuation of gender-related requests post-pubertally, and goes on to request gender diversity-related treatments in adulthood15. These phenomena remain poorly understood, but are often motivating drivers of gender care decision-making and policies. A concern writ large, shared by many policy makers, the lay press, and families of gender diverse youth, is that a young individual might choose to pursue treatments with lasting effects, only to change their minds later.9 Evidence suggests, however, that when gender diverse youth are carefully assessed over time for their gender-related needs, and when those youth with confirmed and consistent gender-related needs are provided gender-affirming medical care, a large majority show positive outcomes in adulthood.16–18 One challenge in generalizing these clinical findings is understanding the nature of the extended evaluation processes used to determine youth readiness to commence medical care.19–21 Key questions include: what constitutes “persistence” or “continuity” of gender diversity/gender-related need over time? Are shiftsa in needs/requests (e.g., before a treatment is initiated) common, and do they follow any patterns? Are there developmental or environmental factors associated with shifts in gender-related medical requests in youth?
This study aims to lay a groundwork for addressing these questions by investigating pubertal/post-pubertal gender-diverse youth who have requested gender-affirming hormone therapy and/or surgery and who either show: (1) a continuity of that medical care request for two or more years or (2) fluctuations in that request over time. Through a mixed-methods approach, this study characterizes developmental factors and youth-reported experiential factors associated with shifts in gender-related medical requests. In accordance with findings of a significant over-representation of autism spectrum disorder among transgender populations, and questions regarding whether gender-related trajectories are consistent between autistic and non-autistic gender-diverse youth, this study includes samples of non-autistic and autistic gender-diverse adolescents.22
Methods
Participants
A total sample of 130 youth receiving care at a large, multidisciplinary US gender services program were monitored between 2010 and 2021. This sample was de facto enriched for autistic gender diverse youth, due to the presence of an autism and gender diversity specialized clinic; this enrichment facilitates analytics across non-autistic and autistic youth. Patient care within the Children’s National gender services program followed the model laid out by the Dutch youth gender care system in concordance with the World Professional Association for Transgender Health Standards of Care (WPATH SOC):5,23 (1) initial evaluations and ongoing monitoring and support provided by mental health professionals experienced in gender development and care, and (2) if youth meet criteria for gender-affirming hormones and/or surgery, they are referred to pediatric specialists with expertise in gender-affirming medical care. Referrals for gender-affirming genital surgeries are made at age 18 or older (top or chest surgery referrals can be made prior). After age 21, gender diverse patients are typically referred to adult clinicians with expertise in gender-affirming care. Additional gender-affirming services, such as menstrual suppression or voice therapy do not require prior mental health evaluation. This clinic’s gender care model differs from the traditional Dutch model notably in that gender-affirming hormones may be commenced as young as age 13. Families were provided a written summary followed by a verbal description of the study, and consent and assent were obtained by the clinician per IRB protocol. The IRB at Children’s National Hospital approved this study.
Of 130 youth monitored, 68 met inclusion criteria for the current study analyses (see Figure 1), which were as follows: (1) youth presented in clinic with requests for gender-affirming sex hormones and/or surgery and (2) youth were pubertal or post-pubertal during at least part of the study monitoring period. Exclusion criteria were: (1) age at first visit over 21 years, (2) age during study monitoring period did not overlap with the age range for which gender-affirming hormones could be commenced (i.e., in this clinic model, younger than age 13), (3) youth did not request gender-affirming hormones and/or surgery, or (4) the youth had a consistency of medical request (i.e., did not experience a shift) but was followed for less than 2 years. The rationale behind these criteria were to identify all pubertal youth who had experienced a shift in request for gender-affirming hormones and/or surgery, while providing a comparison group that had a consistency of request for at least 2 years. See Table A1 for participant characteristics, including comparisons between the 68 included and the 62 excluded youth.
Figure 1.
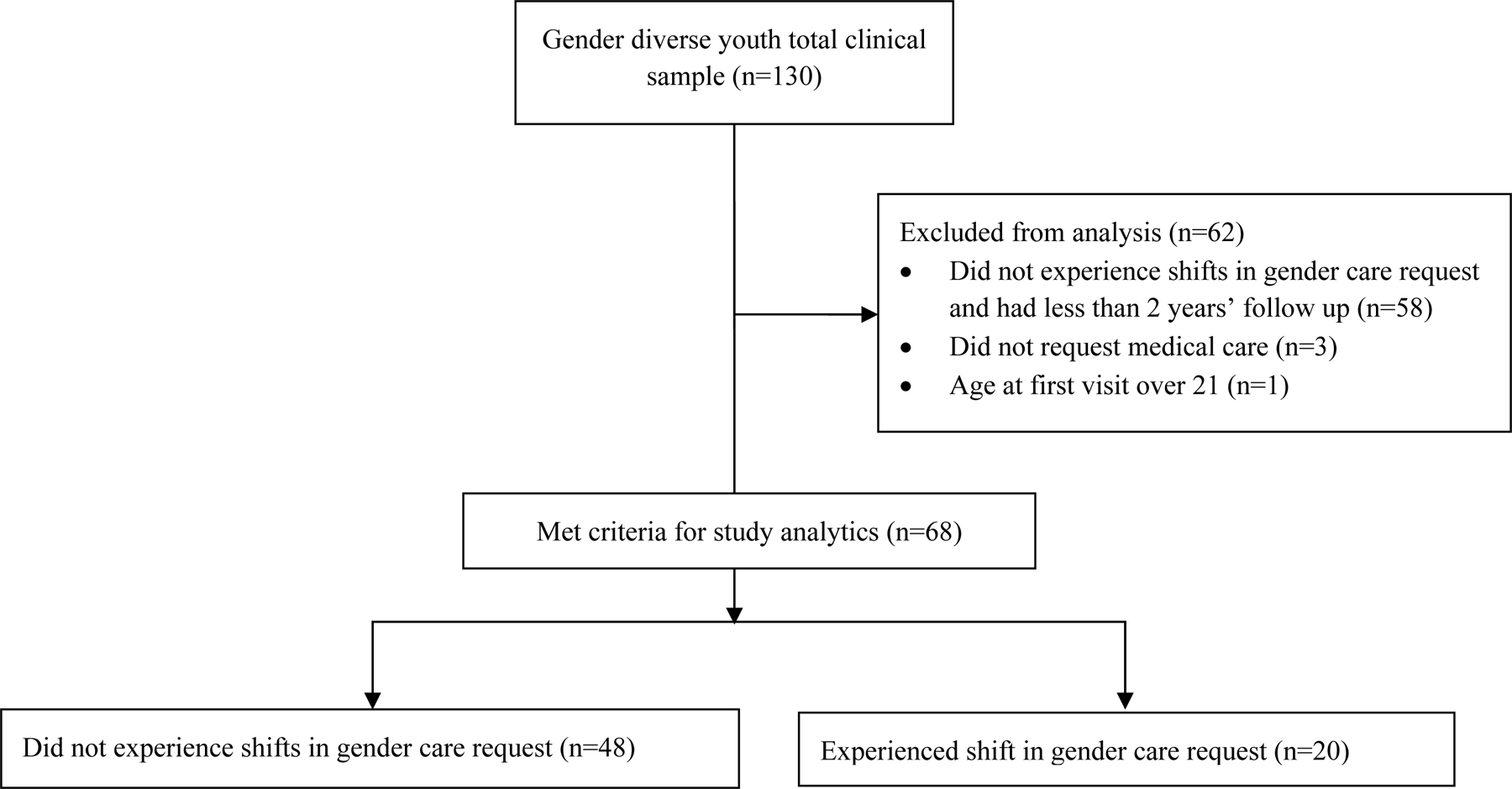
Participant inclusion and exclusion algorithm
Individuals who received pubertal suppression were only included if they presented with additional medical request(s) for gender-affirming hormone therapy and/or surgery. Rationale for this distinction is that pubertal suppression has a different purpose in gender-affirming care, as it does not seek to produce the sex characteristics of one’s identified gender and is considered to be reversible.5,6,24 Given the contrasting nature of pubertal suppression versus gender-affirming hormone therapy and/or surgery, there is the potential that motivators for the former may differ substantially from the motivators for the latter. Shifts in requests for puberty suppression were thus beyond the scope of this study.
Procedure
Demographics and electronic record abstraction:
All demographic, diagnostic, and treatment characteristics were obtained from the adolescent’s electronic health record with each participant’s gender development clinician. Abstracted elements included: (1) designated sex at birth of the adolescent, (2) age at first assessment, (3) gender identity at initial evaluation for gender services (based on youth self-report in clinical interview), (4) current gender identity, (5) race/ethnicity, (6) diagnostic confirmation regarding autism spectrum disorder (ASD) status, and (7) duration of gender-related monitoring/support. Gender identities included transmasculine, transfeminine, gender nonbinary, and cisgender (i.e., 1 participant had a shift to cisgender identity during the course of gender monitoring).
Clinician Interviews:
To characterize individuals who experienced shifts in gender-related medical requests, qualitative interviews were conducted with three mental health providers of the gender services program (DC, JFS, and LW). Providers were given a list of participants they have evaluated and followed over time, all of whom expressed gender-related medical request(s). They were then asked to identify any youth who experienced a shift in gender-related medical requests by reviewing the electronic health record. The three clinicians categorized participants into one of two categories: (1) youth experienced a shift in gender-related medical request, defined as requesting gender-affirming hormones and/or surgery and later withdrawing that request one or more times or (2) youth had a continuity of medical intervention request without any fluctuations during the study monitoring period. For the first of the subgroups (i.e., those with a shift), a topic list for a semi-structured clinician-based interview was developed to capture available information about these shifts in medical requests. The questions on this list focused on the types of medical requests the participants made (Did the participant request sex hormone therapy, such as estrogen or testosterone? Was the participant requesting surgery, and if so, what kind of surgery?), participant explanations about their shift in request (What did the participant say about the reasons why they changed their request[s]?), and the most up-to-date report on the participant’s medical request(s), if any (Does the participant have any ongoing gender-related medical requests?). These questions were asked of the clinicians regarding each of the participants who had experienced a change of medical request, and they reviewed the electronic health records as part of the interview process. These interviews were completed by the first author (AC) and were transcribed into a summary for each participant.
Data analysis
To compare those with and without experienced shifts in gender-related medical requests by age at first visit, autism status (autistic versus non-autistic), gender identity classification (i.e. transgender binary versus transgender nonbinary), and designated sex at birth, chi-square tests and t-tests were conducted with false discovery rate corrections for multiple comparisons.
For analytics regarding patterns and reasons for shifts in gender-related medical request, a multi-stage qualitative analytic process was employed. Coding team 1 (i.e., coders 1 and 2) included a pediatric neuropsychologist with expertise in youth gender development as well as the intersection of neurodivergence and gender diversity and a pediatric gynecologist experienced in gender care. Coder 3, who worked independently from coding team 1, is a pediatric gynecologist specialized in youth gender care—including care for youth with co-occurring gender diversity and neurodivergence. The coding sequence was as follows. Coding team 1 coded the clinician interview summaries for the youth who experienced shifts in gender-related medical requests. The aims of coding were to identify: (1) patterns of gender-related medical request(s) and shift(s) over time (hereafter referred to as “shift profiles”) and (2) overarching themes summarizing youth self-reported reasons for these shifts (hereon referred to as “shift reasons”). Each youth experiencing shifts in gender-related medical requests was preliminarily categorized according to one of the shift profiles and any applicable shift reasons.
Coder 3 then independently evaluated the interview summaries of the participants to identify shift reasons. Coder 3 also evaluated the shift profile framework from coding team 1, assigning one profile to each participant. Then, inconsistencies in thematic descriptions of shift reasons were reconciled between coding team 1 and coder 3 through a consensus method. Two sets of Kappa statistics were calculated to assess reliabilities between coding team 1 and coder 3: (1) reliability of the shift profile assignment and (2) reliability in identification of each participant’s shift reasons.
Results
Ratio of participants with and without shifts in medical request
Of the 68 youth who met inclusion criteria for the study (i.e., youth who had requested gender-related medical treatments), 20 (29%) reported a shift in gender-related medical request, while 48 (71%) did not.
Characteristics of participants with and without shifts in medical request
There were no significant differences in age at first visit, autism diagnostic status (autistic versus non-autistic), or designated sex at birth, between participants with and without shifts in gender-related medical requests (ps > 0.620, see Table 1). The groups did differ significantly in terms of transgender binary versus nonbinary identities, where a greater proportion of youth with shifting medical requests reported a nonbinary gender identity. This finding survived false-discovery rate correction (Χ2 (1, N=68) = 8.673, FDR-corrected p = 0.012).
Table 1.
Characteristics of participants who experienced or did not experience a shift in gender-related medical request
| Shift in Medical Request n = 20 | No Shift in Medical Request n = 48 | Test of differences | |
|---|---|---|---|
|
|
|||
| Age at first visit (years) M (SD) | 15.34 (1.89) | 15.02 (2.64) |
t(66) = −0.498 p=0.620 |
| Gender identity at baseline (number transbinary / nonbinary) | 11 / 9 | 42 / 6 |
Χ2(1) = 8.673 p = 0.003 FDR Adjusted p = 0.012 |
| Designated sex at birth (number male / female) | 9 / 11 | 20 / 28 |
Χ2(1) = 0.064 p = 0.800 |
| Autism diagnostic status (number autistic / nonautistic) | 10 / 10 | 22 / 26 |
Χ2(1) = 0.098 p = 0.754 |
| Race (number of participants) | |||
| Asian | 1 | 3 | |
| Black or African American | 0 | 1 | |
| White | 18 | 38 | |
| Other | 1 | 5 | |
| More than 1 reported | 0 | 0 | |
| Ethnicity | |||
| Number Hispanic or Latinx | 1 | 1 | |
Shift profiles
Six patterns of shift(s) in gender-related medical request(s) over time (i.e., shift profiles) were generated (see Figure 2). Inter-rater reliability in classifying the 20 participants who experienced shifts into one of the six shift profiles was excellent (unweighted κ = 0.865). Four of the six profiles (Profiles 1–4) reflect shifts in medical request prior to starting treatment; two of the profiles (Profiles 5 and 6) involve shifts after treatment commenced.
Figure 2.
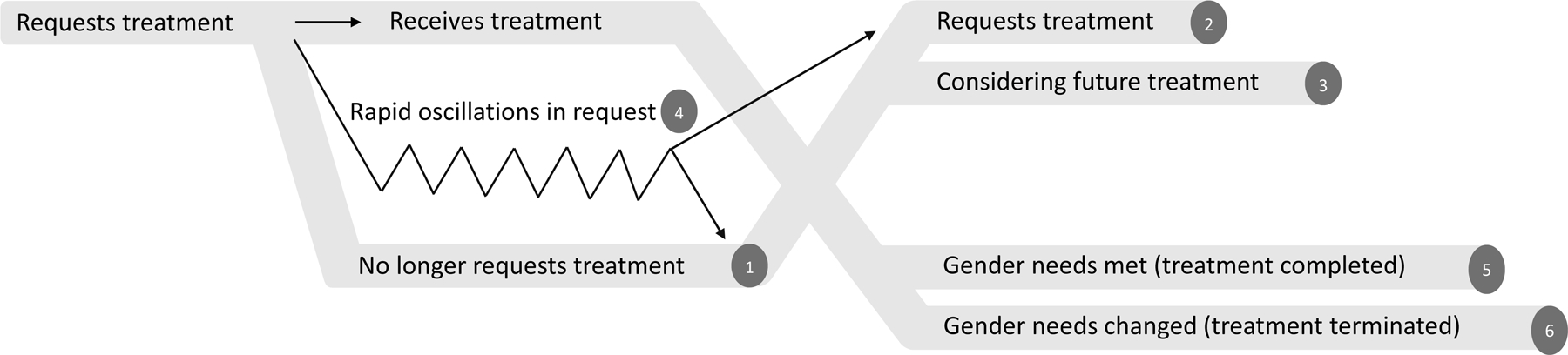
Diagram of the six Shift Profiles
Shift profile 1: Requests treatment ➔ No longer requests treatment
Shift profile 2: Requests treatment ➔ No longer requests treatment ➔ Requests treatment
Shift profile 3: Requests treatment ➔ No longer requests treatment ➔ Considering future treatment
Shift profile 4: Requests treatment ➔ Oscillations for request ➔ Requests treatment or no longer requests treatment
Shift profile 5: Requests treatment ➔ Receives treatment ➔ Gender needs met (treatment completed)
Shift profile 6: Requests treatment ➔ Receives treatment ➔ Gender needs changed (treatment terminated)
Profile 1 is the pattern in which a medical request was made and then withdrawn. Five of the participants demonstrated this profile (25%). Profile 2 begins with the pattern of Profile 1, but eventually includes a return to the original request. This pattern was the most common observed (9 participants representing 45% of the sample). Profile 3 is similar to Profile 2, but instead of returning to the original request with certainty, the participant was considering the original request as a future possibility (1 participant; 5% of the sample). Profile 4 follows a distinctive pattern in which the time following the initial request was characterized by numerous oscillations between making and withdrawing requests for gender-affirming hormones and/or surgery. Two of the participants (10% of sample) exhibited this pattern, one ultimately settling on a consistent request for treatment and the other deciding not to pursue treatment.
Of the two profiles that involve changes in request following initiation of treatment, Profile 5 (2 participants, 10% of sample) involves no negative report of treatment history. This profile was identified in youth who received gender-affirming hormone therapy, and who later decided to stop hormone treatments after having met gender-related goals (i.e. sufficient progression of secondary sex characteristics according to each participant’s goals). Profile 6 was rare, with only one participant (5% of sample). This profile is distinguished by stopping treatment due to negative report regarding commencing the treatment.
Reported shift reasons
The three coders worked to consensus, identifying eight overall shift reasons (see Tables 2 and 3). Two meta-themes also emerged, summarizing six of the eight shift reasons: Ongoing Gender Discovery and Interpersonal Influences. Two of the eight shift reasons stood independent of a meta-theme: Reluctance towards maleness and Delusions/thought instability. Inter-rater reliabilities were acceptable for 7 of the 8 shift reasons. Exploring gender identity had fair inter-rater reliability and therefore this classification should be interpreted with caution (see Table 2). See Table 3 for thematic descriptions of the eight shift reasons.
Table 2.
Characteristics, shift profiles, shift reasons of participants who experienced changes in gender-related medical request
| Profile | Ongoing Gender Discovery | Interpersonal Influences | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Participant | Autistic? |
Gender at baseline | Sex assigned at birth | Ages followed |
Treatment requested | Wants more life experiences | Exploring gender identity | Shifts in gender identity | Worries about coming out | Lack of support for gender | Perceived peer pressure | Delusions/thought instability | Reluctance towards maleness | |
| Profile 1 (25%) Requests ➔ No Longer Requests | 1 | N | M | F | 17 | H | * | ✓ | ✓ | ✓ | ||||
| 2 | N | M | F | 14–15 | H/S | ✓ | ||||||||
| 3 | Y | F | M | 16 | H | ✓ | ||||||||
| 4 | Y | F | M | 18–22 | H/S | ✓ | ||||||||
| 5 | Y | F | M | 14 | H | ✓ | ✓ | |||||||
| Profile 2 (45%) Requests ➔ No Longer Requests ➔ Requests | 6 | N | F | M | 16–17 | H | ✓ | * | ✓ | |||||
| 7 | N | F | M | 16–18 | H | ✓ | ||||||||
| 8 | N | M | F | 15–18 | H | ✓ | ✓ | |||||||
| 9 | Y | NB | F | 16–18 | S | ✓ | ||||||||
| 10 | Y | NB | F | 12–17 | H/S | ✓ | ✓ | |||||||
| 11 | N | F | M | 4–19 | H | ✓ | ✓ | |||||||
| 12 | Y | NB | F | 12–16 | H | * | ✓ | |||||||
| 13 | Y | NB | F | 16–20 | H | ✓ | * | |||||||
| 14 | Y | F | M | 12–15 | H | * | ||||||||
| Profile 3 (5%) Requests ➔ No Longer Requests ➔ Considering | 15 | N | M/NB | F | 17–20 | S | * | |||||||
| Profile 4 (10%) Requests ➔ Oscillation ➔ Requests/No Longer Requests | 16a | Y | Q | M | 17 | H/S | ✓ | |||||||
| 17b | N | M | F | 15–20 | S | ✓ | ✓ | |||||||
| Profile 5 (10%) Requests ➔ Treatment Completed | 18 | N | M | F | 16–18 | H | ✓ | |||||||
| 19 | Y | NB | F | 17–20 | H | ✓ | ||||||||
| Profile 6 (5%) Requests ➔ Treatment Terminated | 20 | N | F | M | 12–17 | H | ✓ | |||||||
| Inter-rater reliability (κ) | 0.77 | 0.34 | 0.50 | 1.00 | 0.64 | 0.77 | 0.77 | 0.77 | ||||||
Legend:
ended at no longer requests
ended at requests
= inconsistencies between coders Y = has autism diagnosis
N = does not have autism diagnosis
M = transmasculine gender identity or male sex designated at birth F = transfeminine gender identity or female sex designated at birth Q = queer
NB = nonbinary gender
H = gender-affirming hormone therapy (excludes blockers) S = gender-affirming surgery
Table 3.
Codebook descriptions of Shift Reasons
| Ongoing Gender Discovery |
| Wants more life experiences: The young person describes a desire for more time or to wait for a later stage of maturity prior to pursuing the gender-related medical request. |
| Exploring gender identity: The young person describes ongoing active exploration of gender, such as trying out new identities, pronouns, and/or the ways they express their gender (i.e. outfits, social cues). |
| Shifts in gender identity: During the monitoring period, the young person described a clear change in their gender identity. For example, they experienced themselves as transmasculine and then later shifted to a nonbinary identity; or they experienced themselves as nonbinary and then shifted to cisgender. |
| Interpersonal Influences |
| Lack of support for gender (external): The young person describes actions on the part of the family and larger community that discouraged gender affirmation and medical gender interventions. |
| Worries about coming out (internal): The young person describes worries that affirming their gender and commencing medical gender intervention would be negatively perceived. In these cases, there was no concrete evidence that the young person’s family was unsupportive of the young person’s gender affirmation. |
| Perceived peer pressure: The young person describes peer group influences, in person and/or online, that encouraged them to seek gender affirming medical care. |
| Additional Reasons |
| Delusions/thought instability: The young person’s delusions or severely shifting moods/cognitions (i.e from schizophrenia or bipolar disorder) were linked directly to self-perceptions of gender and gender-related medical requests. When the presence of delusions or the mood cycle shifted, the gender-related medical request also shifted. |
| Reluctance towards maleness: The young people (designated female at birth) report a history of negative experiences with cisgender males, and come to express a reluctance toward becoming male, which impacts their gender-related medical requests. |
Three shift reasons classified within the Ongoing Gender Discovery theme are: Wants more life experiences, Exploring gender identity, and Shifts in gender identity. Wants more life experiences encompassed reports from participants concerning a need for additional time prior to consideration of a gender-related medical request. Exploring gender identity and Shifts in gender identity refer to the participant reports of ongoing gender exploration, with the former identifying continued experimentation with gender and the latter representing a distinct change in experienced gender identity. Of note, nine of the participants who experienced shifts in gender-related medical requests (45% of this sample) also reported a shift in gender identity: five moving from binary transgender to nonbinary, and four experiencing more complex progressions of gender identity (e.g. nonbinary to cisgender to transmasculine).
The three shift reasons within the Interpersonal Influences theme are: Worries about coming out, Lack of support for gender, and Perceived peer pressure. When describing Worries about coming out, participants reported concerns regarding the social acceptability of gender transition. Importantly, these concerns appeared to be without clear external causes, as these participants did not report specifically that their family or friends were unsupportive of their gender transition. In contrast, Lack of support for gender was identified in participants who explicitly reported actions by their family, friends, or larger community that discouraged their gender diversity. Perceived peer pressure was described by two participants who reported gender diverse peers had encouraged their initial decision to pursue gender-affirming medical treatments; in time, they realized their own needs were different (i.e. realizing they did not desire gender-affirming medical treatment).
Delusions/thought instability was a shift reason present for some participants with severe psychiatric disorders (i.e. schizophrenia or bipolar illness). In this shift reason, variations in gender-related medical requests were linked to changes in the participants’ psychiatric status, tracking with periods of remittance versus recurrence. Specifically, the gender-related medical requests accompanied periods of mania or delusions/psychosis, whereas these participants no longer requested medical treatment during periods of psychiatric stability.
Reluctance towards maleness was a shift reason described by two participants, both designated female at birth, who reported a history of negative experiences with cisgender males.
Patterns of shift profiles by demographics and shift reasons
Due to the small sample size of participants who experienced a shift in medical request, as well as stratification across six shift profiles and eight shift reasons, statistical tests of linkages between demographics, shift profiles, and shift reasons were not conducted. However, some observations regarding patterns were noted. Overall, there was no clear pattern of shift profile or shift reasons by autism status, gender identity, or sex assigned at birth. However, the Reluctance towards maleness reason was reported only by participants assigned female at birth. The Wants more life experiences and Perceived peer pressure shift reasons, were only reported by participants classified to Profile 2. Notably, Profile 4 (which described oscillations in request and no request) included only participants with both significant psychiatric illnesses and an associated Delusions/thought instability shift reason. Separately, the one participant classified as Profile 6 (terminating gender-affirming medical treatment and reporting regret about pursuing this treatment) also reported the Delusion/thought instability shift reason.
Discussion
To our knowledge, this is the first study to examine experienced shifts in gender-related medical requests during adolescence. Of the 68 individuals who met criteria for analysis, nearly a third experienced shifts in requests for gender-affirming hormones and/or surgery during their discernment process. This novel finding suggests that this phenomenon is not uncommon. Only three of the twenty individuals who experienced shifts in request did so after beginning gender-affirming hormone treatments (shift profiles 5 and 6). Of those three, only one individual reported regret for having undergone treatment, consistent with previous reports that regret is a relatively rare outcome.17 The majority of shifts in request occurred prior to initiating gender-affirming hormone therapy and/or surgery (seventeen of the twenty individuals). Important for contextualization of this this study, the excluded cohort was older than the analyzed sample at first visit; when patients arrive in late adolescence, they transition to adult care more quickly and were therefore less likely to meet the inclusion requirement for the two-year study monitoring period.
In identifying the shift profiles, we observed that fluctuations in requests for gender-affirming hormones and/or surgery can take a variety of pathways. These findings suggest the importance of clinicians recognizing that a shift away from requesting gender-affirming hormones and/or surgery does not imply a single pathway or outcome regarding gender care.25 Notably, the most common shift profile in our cohort was shift profile 2, where the request was re-established (9 of our 20 youth). In fact, many youth who shift away from a request may do so temporarily, and later come back to the request. A similar phenomenon has been previously described as “persistence-after-interruption,” though this latter pattern was characterized as taking place over a longer timespan extending into young adulthood.15 Gender programs should consider ways to accommodate a continued relationship with a gender exploring young person who has moved away from a gender-affirming treatment request to support ongoing exploration.19
Our analysis of gender identity and shift in requests showed a significantly higher proportion of youth with transgender nonbinary identity experiencing a shift in request for gender-affirming hormones and/or surgery. However, this association should be interpreted with care, as nonbinary youth may have treatment goals and needs that are being reflected by these reported shifts. To date, there is no formal guidance specific to furnishing gender-affirming hormones and/or surgery for youth (or adults) with a transgender nonbinary identity. Some studies focusing on transgender binary and nonbinary individuals have found distinctions in utilization of affirming gender services.26–28 There are reported increased barriers to gender-affirming care among nonbinary youth, particularly when seeking hormone therapy.27 Some gender nonbinary youth may be able to meet their gender-related needs and goals without gender-affirming hormones and/or surgery (i.e., through pronouns, gender expression in hairstyle, and clothes), though whether this is related to the aforementioned barriers remains unclear. In offering gender-affirming hormones and/or surgery for any young person, prescribers must continue to ascertain their needs and goals of treatment. In the absence of clear guidelines, this principle is of critical significance to transgender nonbinary youth.9
Some phenomena described in our cohort should be interpreted with caution, particularly as it pertains to youth with significant mental illness and the very small sample size of this subgroup. Individuals who experienced shift profile 4 or shift profile 6 had concomitant profound psychiatric impairment. For the individuals with shift profile 4, a relapsing/remitting request was observed in concordance with symptomatic changes in mood. For gender-diverse youth with concomitant profound mental illness, it is recommended to provide both gender services and psychiatric treatment, and treatment plans must be individualized to each person’s unique circumstance. Several guidance documents have reaffirmed that significant mental illness should not necessarily preclude gender-affirming supports.5,6,21
A strength of the analyzed group is that the youth were followed over time and had an ongoing therapeutic relationship with the gender development program. Demographically, this study’s inclusion of youth with intersecting autism and gender diversity is a strength as well. Our finding of no significant difference in the proportion of autistic versus non-autistic youth experiencing a shift is important. Current care decisions for autistic transgender youth are guided by limited care guidelines, with almost no longitudinal findings to inform care.29 Relevant for clinical practice, our study finds that autistic and non-autistic youth may experience shifts in request at the same rates. This observation adds to an emerging literature suggesting that the gender diversity experiences of autistic youth are similar to those of non-autistic youth.30
Our study was limited in that it only included a single referral center and the demographics that it serves, which were predominantly Caucasian. This does not represent the racial and ethnic makeup of the gender diverse population at large, limiting the generalizability of these findings. While this study provides many shift reasons that youth may experience a shift in their request for gender-affirming hormones and/or surgery, it is by no means complete. Our sample of 20 youth experiencing a shift, which is the largest described to date, is still relatively small and thus limits generalizability of the findings. The youth-reported reasons for experiencing a shift are unlikely to be fully comprehensive across all gender diverse youth, given the small sample size, our sample’s demographic, and even smaller subgroup sizes (these sizes precluded statistical analysis, particularly among the different shift profile groups). In addition to our identified shift reasons, social factors may play a large role and have major impacts on adolescent decision-making processes. Youth who are frequently receiving negative socio-cultural signals about gender diversity may not be able to bear the social burden of medically transitioning, even if they feel it best aligns with their gender identity.
Additionally, simplifying our shift profiles to whether a young person re-requests a treatment or stopped a treatment may not capture a complete picture of how their goals and needs are met by gender-affirming hormones and/or surgery. For example, the youth who fit into shift profile 5 included individuals whose gender-related needs and goals were met by the gender-affirming hormone therapy to that point. In these cases, the individuals expressed satisfaction with their changes and no longer felt they required gender-affirming hormone treatment.
An overarching limitation in the current study design is that the information of youth-reported shift reasons and trajectories of the shift profiles were identified from interviews with each young person’s mental health clinician and from their medical record, but not the youth themselves. All interviews were conducted while mental health clinicians referenced the youths’ electronic health record to mitigate potential recall bias. Because the qualitative information was not obtained directly from the youth, this study should be followed up with studies that directly interview youth over time. Finally, our data set did not include the time interval between intake and patient evaluation.
Conclusions
Shifts in requests for gender-affirming hormone therapy and/or surgery by gender diverse youth may not be uncommon during their gender discernment process. These shifts may be more likely to occur among nonbinary youth. Initial evidence suggests that these shifts may not be more common among autistic youth. Many youth who experience shifts away from medical treatment may later resume the request. Given these findings, to meet the gender-affirming goals and needs of youth, clinicians providing gender-affirming hormones and/or surgery must continue to clarify goals of treatment, intended outcomes, or stop-points (e.g., once a specific amount of secondary sex development occurs) over time.
The clinic for this study employed most elements of the Dutch gender care approach. It is important to note that not all gender clinics employ this approach (e.g. some gender services programs advocate for informed consent for gender-affirming medical treatment without mental health evaluations).31 By requiring a relationship with mental health services to obtain gender-affirming hormones and/or surgery, the Dutch model may be challenging to provide, given limited availability of mental health providers with gender expertise. Our study shows that there is likely a benefit and a potential role for mental health services to support youth even when shifting away from a request for medical gender-affirming interventions, as a shift in request is not necessarily a final ending point in the gender discernment process.
Data Statement:
Due to the sensitive nature of the questions asked in this study, we have kept raw data confidential.
Supplementary Material
Implications and Contributions:
Shifts in gender-related medical requests for hormones and/or surgery are not uncommon among gender diverse youth. There is likely a benefit and a role for continuing mental health services to support youth who have shifted away from a request for intervention, as a shift is not necessarily a final ending point in the gender discernment process.
Acknowledgments:
We thank Shane Henise for his editorial assistance in reviewing an earlier version of this manuscript.
Funding:
This work was supported by the National Institutes of Health [grant number Z1A HD008985].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of interests
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Given varied uses of the word “shifts” in the youth gender-related literature, for the purposes of this paper, we use “shift” to describe experienced changes in expressed needs for gender-related treatment requests, not to refer to patterns of shifts in referral rates or gender of referrals, as commonly reported in gender clinics.
References
- 1.Edwards-Leeper L, Anderson E. The Mental Health Establishment is Failing Trans Kids: Gender-exploratory therapy is a key step. Why aren’t therapists providing it? Washington Post November 24, 2021.
- 2.Ghorayshi A A Teen Trans Divide. New York Times January 18, 2022:1.
- 3.Jones JM. LGBT Identification in U.S. Ticks Up to 7.1%. Gallup February 23, 2022, 2022. Accessed February 23, 2022, 2022. https://news.gallup.com/poll/389792/lgbt-identification-ticks-up.aspx
- 4.Olson-Kennedy J, Cohen-Kettenis PT, Kreukels BPC, et al. Research priorities for gender nonconforming/transgender youth: gender identity development and biopsychosocial outcomes. Current opinion in endocrinology, diabetes, and obesity 2016;23(2):172–179. doi: 10.1097/MED.0000000000000236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coleman E, Bockting W, Botzer M, et al. Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7. The international journal of transgenderism 2012;13(4):165–232. doi: 10.1080/15532739.2011.700873 [DOI] [Google Scholar]
- 6.Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab Nov 1 2017;102(11):3869–3903. doi: 10.1210/jc.2017-01658 [DOI] [PubMed] [Google Scholar]
- 7.Chen D, Strang JF, Kolbuck VD, et al. Consensus Parameter: Research Methodologies to Evaluate Neurodevelopmental Effects of Pubertal Suppression in Transgender Youth. Transgender health 2020;5(4):246–257. doi: 10.1089/trgh.2020.0006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klink D, Caris M, Heijboer A, van Trotsenburg M, Rotteveel J. Bone Mass in Young Adulthood Following Gonadotropin-Releasing Hormone Analog Treatment and Cross-Sex Hormone Treatment in Adolescents With Gender Dysphoria. The journal of clinical endocrinology and metabolism 2015;100(2):E270–E275. doi: 10.1210/jc.2014-2439 [DOI] [PubMed] [Google Scholar]
- 9.O’Connell MA, Nguyen TP, Ahler A, Skinner SR, Pang KC. Approach to the Patient: Pharmacological Management of Trans and Gender-Diverse Adolescents. The journal of clinical endocrinology and metabolism 2022;107(1):241–257. doi: 10.1210/clinem/dgab634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steensma TD, Biemond R, de Boer F, Cohen-Kettenis PT. Desisting and persisting gender dysphoria after childhood: a qualitative follow-up study. Clinical child psychology and psychiatry 2010;16(4):499–516. doi: 10.1177/1359104510378303 [DOI] [PubMed] [Google Scholar]
- 11.Steensma TDPD McGuire JKPDMPH, Kreukels BPCPD Beekman AJBS, Cohen-Kettenis PTPD. Factors Associated With Desistence and Persistence of Childhood Gender Dysphoria: A Quantitative Follow-Up Study. Journal of the American Academy of Child and Adolescent Psychiatry 2013;52(6):582–590. doi: 10.1016/j.jaac.2013.03.016 [DOI] [PubMed] [Google Scholar]
- 12.Wagner S, Panagiotakopoulos L, Nash R, et al. Progression of Gender Dysphoria in Children and Adolescents: A Longitudinal Study. Pediatrics (Evanston) 2021;148(1)doi: 10.1542/peds.2020-027722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turban JL, Keuroghlian AS. Dynamic Gender Presentations: Understanding Transition and “De-Transition” Among Transgender Youth. Journal of the American Academy of Child and Adolescent Psychiatry 2018;57(7):451–453. doi: 10.1016/j.jaac.2018.03.016 [DOI] [PubMed] [Google Scholar]
- 14.Vandenbussche E Detransition-Related Needs and Support: A Cross-Sectional Online Survey. Journal of homosexuality 2021;ahead-of-print(ahead-of-print):1–19. doi: 10.1080/00918369.2021.1919479 [DOI] [PubMed]
- 15.Steensma TD, Cohen-Kettenis PT. More than two developmental pathways in children with gender dysphoria? J Am Acad Child Adolesc Psychiatry Feb 2015;54(2):147–8. doi: 10.1016/j.jaac.2014.10.016 [DOI] [PubMed] [Google Scholar]
- 16.de Vries ALC, McGuire JK, Steensma TD, Wagenaar ECF, Doreleijers TAH, Cohen-Kettenis PT. Young Adult Psychological Outcome After Puberty Suppression and Gender Reassignment. Pediatrics (Evanston) 2014;134(4):696–704. doi: 10.1542/peds.2013-2958 [DOI] [PubMed] [Google Scholar]
- 17.Wiepjes CM, Nota NM, de Blok CJM, et al. The Amsterdam Cohort of Gender Dysphoria Study (1972–2015): Trends in Prevalence, Treatment, and Regrets. Journal of sexual medicine 2018;15(4):582–590. doi: 10.1016/j.jsxm.2018.01.016 [DOI] [PubMed] [Google Scholar]
- 18.Chew D, Anderson J, Williams K, May T, Pang K. Hormonal Treatment in Young People With Gender Dysphoria: A Systematic Review. Pediatrics 2018;141(4):e20173742. doi: 10.1542/peds.2017-3742 [DOI] [PubMed] [Google Scholar]
- 19.Edwards-Leeper L, Leibowitz S, Sangganjanavanich VF. Affirmative Practice With Transgender and Gender Nonconforming Youth: Expanding the Model. Psychology of sexual orientation and gender diversity 2016;3(2):165–172. doi: 10.1037/sgd0000167 [DOI] [Google Scholar]
- 20.Hidalgo MA, Ehrensaft D, Tishelman AC, et al. The Gender Affirmative Model: What We Know and What We Aim to Learn. Human development 2013;56(5):285–290. doi: 10.1159/000355235 [DOI] [Google Scholar]
- 21.Spivey LA, Edwards-Leeper L. Future Directions in Affirmative Psychological Interventions with Transgender Children and Adolescents. Journal of clinical child and adolescent psychology 2019;48(2):343–356. doi: 10.1080/15374416.2018.1534207 [DOI] [PubMed] [Google Scholar]
- 22.Warrier V, Greenberg DM, Weir E, et al. Elevated rates of autism, other neurodevelopmental and psychiatric diagnoses, and autistic traits in transgender and gender-diverse individuals. Nature communications 2020;11(1):3959-3959. doi: 10.1038/s41467-020-17794-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Vries AL, Cohen-Kettenis PT. Clinical management of gender dysphoria in children and adolescents: the Dutch approach. J Homosex 2012;59(3):301–20. doi: 10.1080/00918369.2012.653300 [DOI] [PubMed] [Google Scholar]
- 24.Panagiotakopoulos L Transgender medicine - puberty suppression. Reviews in endocrine & metabolic disorders 2018;19(3):221–225. doi: 10.1007/s11154-018-9457-0 [DOI] [PubMed] [Google Scholar]
- 25.Gerritse K, Hartman L, Antonides MF, Wensing-Kruger A, de Vries ALC, Molewijk BC. Moral Challenges in Transgender Care: A Thematic Analysis Based on a Focused Ethnography. Arch Sex Behav Nov 2018;47(8):2319–2333. doi: 10.1007/s10508-018-1287-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Breslow AS, Wojcik H, Cox R, Tran NM, Brewster ME. Toward Nonbinary Nuance in Research and Care: Mapping Differences in Gender Affirmation and Transgender Congruence in an Online National U.S. Survey. Transgender health 2021;6(3):156–163. doi: 10.1089/trgh.2020.0038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Clark BA, Veale JF, Townsend M, Frohard-Dourlent H, Saewyc E. Non-binary youth: Access to gender-affirming primary health care. The international journal of transgenderism 2018;19(2):158–169. doi: 10.1080/15532739.2017.1394954 [DOI] [Google Scholar]
- 28.Inwards-Breland DJ, Karrington B, Sequeira GM. Access to Care for Transgender and Nonbinary Youth: Ponder This, Innumerable Barriers Exist. JAMA pediatrics 2021;doi: 10.1001/jamapediatrics.2021.2068 [DOI] [PubMed]
- 29.Strang JF, Meagher H, Kenworthy L, et al. Initial Clinical Guidelines for Co-Occurring Autism Spectrum Disorder and Gender Dysphoria or Incongruence in Adolescents. Journal of clinical child and adolescent psychology 2016;47(1):105–115. doi: 10.1080/15374416.2016.1228462 [DOI] [PubMed] [Google Scholar]
- 30.Strang JF, Powers MD, Knauss M, et al. “They Thought It Was an Obsession”: Trajectories and Perspectives of Autistic Transgender and Gender-Diverse Adolescents. Journal of autism and developmental disorders 2018;48(12):4039–4055. doi: 10.1007/s10803-018-3723-6 [DOI] [PubMed] [Google Scholar]
- 31.Olson-Kennedy J Mental Health Disparities Among Transgender Youth: Rethinking the Role of Professionals. JAMA pediatrics 2016;170(5):423–424. doi: 10.1001/jamapediatrics.2016.0155 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


