Abstract
Mendelian randomization using GWAS summary statistics has become a popular method to infer causal relationships across complex diseases. However, the widespread pleiotropy observed in GWAS has made the selection of valid instrumental variables problematic, leading to possible violations of Mendelian randomization assumptions and thus potentially invalid inferences concerning causation. Furthermore, current MR methods can examine causation in only one direction, so that two separate analyses are required for bi-directional analysis. In this study, we propose a ststistical framework, MRCI (Mixture model Reciprocal Causation Inference), to estimate reciprocal causation between two phenotypes simultaneously using the genome-scale summary statistics of the two phenotypes and reference linkage disequilibrium information. Simulation studies, including strong correlated pleiotropy, showed that MRCI obtained nearly unbiased estimates of causation in both directions, and correct Type I error rates under the null hypothesis. In applications to real GWAS data, MRCI detected significant bi-directional and uni-directional causal influences between common diseases and putative risk factors.
Subject terms: Diseases, Genome-wide association studies, Statistical methods
Mendelian randomization methods are prone to produce false positive results when assumptions are violated. Here, the authors propose a statistical model that offers good power to detect causation between traits while controlling the false positive rate.
Introduction
The advent of genome-wide association studies (GWASs) has confirmed widespread genetic correlations among numerous complex diseases and traits1. Such correlations may represent pleiotropic genetic effects on multiple phenotypes, or causal relationships between phenotypes2. The analysis of GWAS data may help to identify causal relationships between phenotypes, contributing to our understanding of disease etiology. In recent years, causal modeling using Mendelian randomization (MR) has been widely applied to GWAS summary data3,4. MR uses genetic variants, typically single nucleotide polymorphisms (SNPs), as instrumental variables (IVs) which, to be valid, should be (1) associated with the exposure (the relevance assumption), (2) not associated with confounders of exposure and outcome (the independence assumption), and (3) only associated with outcome through exposure (the exclusion restriction assumption)5. Basically, MR estimates the causal effect of an exposure on an outcome by the ratio of the effect of a genetic variant on the outcome to the effect of the same genetic variant on the exposure. In practice, due to the high polygenicity of complex traits, multiple SNPs may be necessary to increase the power and robustness of MR6.
However, using multiple SNPs as IVs also increases the chance of horizontal pleiotropy for some SNPs7, which would violate the assumption for methods like inverse-variance weights (IVW)4. MR-Egger8 and MR-PRESSO9 address the issue of horizontal pleiotropy under the InSIDE (instrument strength independent of direct effect) assumption, while Weighted Median10 and Weighted Mode11 are robust to horizontal pleiotropy provided that there is an adequate proportion of valid IVs in estimation. More recent methods such as MRMix12 assume a normal-mixture model to consider horizontal pleiotropic effects. While these methods address the violation of the MR assumptions by either removing pleiotropic SNPs or explicitly modeling pleiotropic effects, they still involve the selection of independent IVs, which may exclude the majority of SNPs, with consequent loss of information. One recent advance is to account for correlated pleiotropy by estimating the nuisance parameters of a mixture model from randomly selected genome-wide summary data. However, this method still requires a set of linkage disequilibrium (LD) pruned variants to calculate posterior distributions to fit the causation model13. As with other existing methods, inference of the causal relationship in the reverse direction requires a separate analysis with a different set of IVs7,14, which may not always be a nontrivial process.
In recent years, causal modeling based on MR approaches has been applied to investigate the inter-relationships between a wide range of phenotypes for which summary GWAS data are available15. With such widespread usage and the proneness of MR methodologies to violations of model assumptions, there is a risk of false positive findings from such studies. False positive causal inferences may be particularly likely when most causal SNPs are pleiotropic so that few SNPs can serve as valid IVs16.
In this article, we propose a statistical method called mixture model reciprocal causal inference (MRCI) to infer the causal paths simultaneously in both directions between two phenotypes. Our method uses GWAS summary statistics of all available SNPs for the two phenotypes, together with reference LD information on the SNPs. We consider SNPs to fall into four mutually exclusive effect categories (trait-specific, pleiotropic, and null SNPs) and construct a composite likelihood function that takes into account the LD among SNPs. Compared with existing MR approaches our method tests for reciprocal causation without the selection of IVs, thus making full use of genetic information while explicitly modeling pleiotropy. In particular, MRCI is robust even in situations where most causal variants are pleiotropic. We applied MRCI to cardiovascular and metabolic disorders and some of their putative risk factors using public GWAS summary data, with results that provided insights into the causal relationship between several pairs of phenotypes.
Results
Overview of MRCI
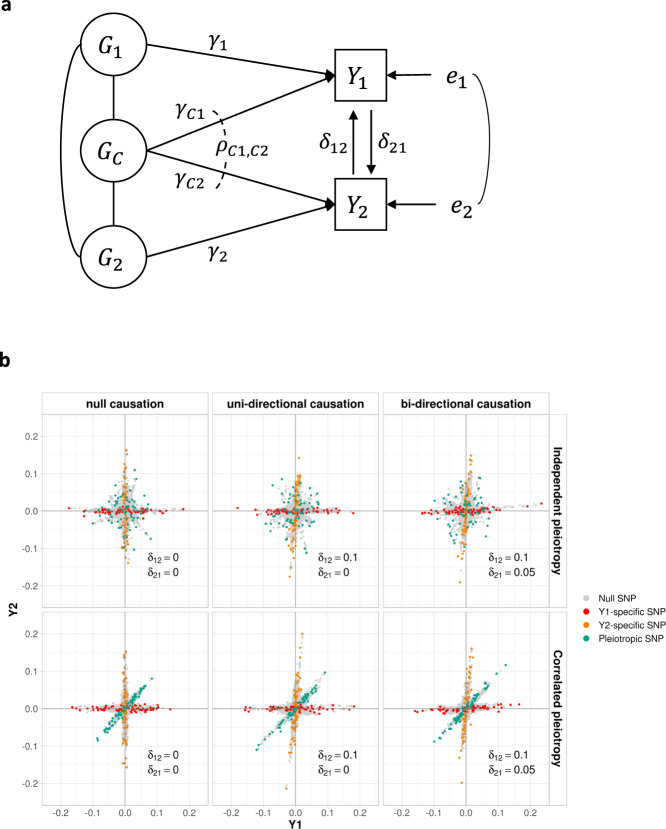
All phenotypes and additively coded genotypes were assumed to have been standardized to have unit variance. In the full model, SNPs were assumed to fall into four mutually exclusive components: trait-specific (), pleiotropic () and null SNPs (), with mixing proportions and , respectively. SNPs in the and components have direct effect sizes of and on phenotype and respectively, while SNPs have direct effect sizes of and with covariance , on and . The effect sizes , , and were assumed to be normally distributed, and their variances were denoted as , , and , respectively. Two reciprocal causal paths ( and ) were specified between and (Fig. 1). Additionally, we considered systemic biases such as population stratification ( and ) and sample overlap () in variance and covariance estimates for phenotype and in the model. From the above parameters, we also calculated the genetic correlation () between the two phenotypes.
Fig. 1. Schematic diagram of MRCI.
a and represent a pair of phenotypes. Genotypes can be divided into four components: -specific causal SNPs (), -specific causal SNPs (), pleiotropic causal SNPs () and null SNPs (, not shown). Lines connecting these genotypes represent the LD correlation between SNPs. Arrow lines from genotype to phenotype represent the direct effect of corresponding SNPs (, , and ) on the phenotypes. Covariance () between and is allowed. Arrow lines between the two phenotypes represent the reciprocal causal paths ( and ). Non-additive genetic effects on phenotypes are represented by and . In real situations, one or two components in the model could be absent and our method could handle these sub-model scenarios in a robust way. b Illustration of several representative simulation scenarios. simIDs are LoS1, LoS3, LoS7 (upper panel from left to right), LoS2, LoS4, LoS8 (lower panel from left to right) (see Supplementary Table 1). -axis and -axis show the standardized effect size estimates for GWAS and , respectively. Red, orange, green, and gray points represent -specific, -specific, pleiotropic, and null SNPs in the simulation respectively. For null causation, ; for uni-directional causation, , ; for bi-directional causation, , . For independent pleiotropy, ; for correlated pleiotropy, . In these plots, the mixing proportions for non-null components were set as , and the heritabilities contributed by -specific, -specific, and pleiotropic SNPs were set as 0.3, 0.3, and 0.1, respectively (see Supplementary Fig. 1 for other simulated scenarios).
From these assumptions, we derived the bivariate distribution of the marginal effect size estimates of the two phenotypes from their respective GWAS. The covariance matrix of this bivariate distribution is determined by the mixture distribution of the direct effect sizes , the reciprocal causal effects and the nuisance parameters , , and (see the “Methods” section). We then calculated the composite likelihood function for all available SNPs to estimate the two causal effects as well as other nuisance parameters by an expectation-maximization (EM) algorithm, together with robust sandwich estimates of their standard errors. Besides the above full model scenario, we further considered four sub-model scenarios in which one or two components were absent (Supplementary Fig. 1). Under these sub-model scenarios, we found that full model estimation often produced poor estimates, and developed a method based on model averaging to achieve more robust model fitting.
We then performed comprehensive simulations, including the full model and sub-model scenarios, to evaluate the estimation accuracy, Type I error rate, and statistical power of MRCI, compared to existing MR methodologies.
Simulation results
Estimation and hypothesis testing under the full model
We compared the accuracy of the causal estimates between MRCI and IV-based MR methods under several simulated low polygenicity scenarios in which the true IVs could be considered nearly independent to satisfy the assumption of classic MR methods. MRCI produced nearly unbiased estimates for both causal directions under both independent and correlated pleiotropy scenarios. Not surprisingly, using exposure-specific true causal SNPs as IVs in IV-based MR methods always obtained unbiased estimates. However, many IV-based MR methods generated biased estimates when GWAS significant SNPs for the exposure phenotype were used as IVs, especially under scenarios with correlated pleiotropy, except for Weighted Mode. In these scenarios, excluding IVs which showed strong GWAS association with the outcome phenotype reduced the magnitude of the bias (Fig. 2a–c and Supplementary Fig. 2).
Fig. 2. Comparison of estimates for the reciprocal causal effect by our method and instrumental variable (IV)-based MR methods in simulations with correlated pleiotropy.
a Estimates in null causation scenarios (, LoS2). b Estimates in uni-directional causation scenarios ( and , LoS4). c Estimates in bi-directional causation scenarios ( and , LoS8). d Rejection rates of the null hypothesis in bi-directional, uni-directional, and null scenarios. In plots a–c, our method took genome-scale SNPs for estimation and produced nearly unbiased estimates in different scenarios; the true values of and are indicated by up- and down-pointing triangles, respectively. For MR methods, IVs were selected in three ways: (1) use the exposure-specific true causal SNPs in the simulation as IVs; (2) use exposure-associated SNPs (p-value < ) after clumping but exclude potential outcome-associated SNPs (defined as p-value < with the outcome); (3) use significant exposure-associated SNPs after clumping regardless of their association with outcome. In plot d, the exclusion criteria were applied to IV-based MR methods and our method shows well-controlled Type I error rates and adequate power. In these plots, for the correlated pleiotropy is 0.1; the mixing proportions for non-null components were ; the heritabilities contributed by -specific, -specific, and pleiotropic SNPs were 0.3, 0.3, and 0.1, respectively (note: The selection of exposure-specific true causal SNPs was not applied to MRMix due to its assumption of a normal-mixture distribution).
MRCI achieved correct control of the Type I error rates under all scenarios when the exposure phenotype had no effect on the outcome phenotype. Not surprisingly, IV-based MR methods also correctly controlled Type I error rates in the perfect scenario where all IVs were exposure-specific true causal SNPs. However, when IVs were selected according to statistical significance in GWAS of the exposure phenotype, most of the MR methods showed severely inflated Type I error rates in simulations with correlated pleiotropy. Excluding SNPs which showed a strong association with the outcome phenotype decreased the Type I error rates, sometimes to the correct level (Weighted Median), when correlated pleiotropy was present (Fig. 2d and Supplementary Tables 2–4).
In terms of statistical power under the alternative hypothesis, we only considered MR methods (MR-Egger, Weighted Mode, and MRMix) that demonstrated correct control of Type I error rates when using statistically significant exposure-associated SNPs as IVs. MRCI and MR methods achieved comparable power in low polygenicity simulations: as high as almost 1 in the stronger causal direction and slightly lower in the weaker causal direction. For IV-based MR methods, excluding potential outcome-associated significant SNPs did not guarantee a sufficient power increase in correlated pleiotropy scenarios (Supplementary Tables 3–7).
Additionally, simulations of other scenarios, including high polygenicity and asymmetry between the two phenotypes (different levels of heritability and polygenicity, and where one phenotype was binary and the other quantitative) showed that MRCI achieved nearly unbiased estimates, well-controlled Type I error rates, and favorable statistical power in both causal directions (Supplementary Table 8). Sample overlap was reflected in the estimates of the nuisance parameter and had no obvious effects on causal estimates in the simulation (Supplementary Fig. 3). Genetic correlation estimates calculated from the MRCI parameter estimates were highly consistent with those obtained from LD Score regression (LDSC)1 (Supplementary Table 9). Simulations with different sample sizes show that when the sample sizes of the GWAS of the two phenotypes are unequal, the accuracy of the causal effect estimate from the phenotype with the larger sample size to the phenotype with the smaller sample size is disproportionately reduced compared to the causal effect estimate in the other direction (Supplementary Table 10).
Estimation and hypothesis testing under sub-models
When the true model does not contain all four SNP components, there is a risk of incorrect inference from estimation that assumes the full model. To examine the robustness of MRCI, we performed estimations under four sub-models which allowed for the absence of one or two specific components. Writing the full model as (indicating the presence of -specific SNPs, -specific SNPs, and pleiotropic SNPs, as well as the omnipresent null SNPs), the four sub-models were , and (indicating the presence of the corresponding SNP components). We performed simulations to investigate model fitting performance under these sub-models, excluding as it is equivalent to (Supplementary Fig. 1 and Table 1). We found that estimation assuming the full model often did not correctly infer the absent component, which resulted in biased causal effect estimates and inflated Type I error rates (Supplementary Fig. 4a).
Table 1.
Descriptive summary statistics of included traits
| Traits | Total reported sample size | Number of reported cases | Number of reported controls | Number of independent significant SNPs/loci | Variance explained by significant SNPs/loci (%) | Publication |
|---|---|---|---|---|---|---|
| CAD | 148,172 | 10,801 | 137,371 | 66 | 21.2 | Nelson et al. (2017)33 |
| IS | 440,328 | 34,217 | 406,111 | 2 | 0.6–1.8 | Malik et al. (2018)34 |
| T2D | 898,130 | 74,124 | 824,006 | 243 | 18.0a | Mahajan et al. (2018)35 |
| BirthWeight | 298,142 | – | – | 190 | 7.0 | Warrington et al. (2019)36 |
| BMI | 681,275 | – | – | 941 | 6.0 | Yengo et al. (2018)37 |
| BodyFat | 89,297 | – | – | 7 | 0.6 | Lu et al. (2016)38 |
| Height | 693,529 | – | – | 3290 | 24.6 | Yengo et al. (2018)37 |
| FastGluc | 140,595b | – | – | 7c | – | Lagou et al. (2021)39 |
| FastInsulin | 98,210b | – | – | 1c | – | Lagou et al. (2021)39 |
| HDL | 188,577 | – | – | 70 | 1.6 | Willer et al. (2013)40 |
| LDL | 188,577 | – | – | 57 | 2.4 | Willer et al. (2013)40 |
| Triglycerides | 188,577 | – | – | 37 | 2.1 | Willer et al. (2013)40 |
| CRP | 418,642 | – | – | 526 | 13.0 | Han et al. (2020)41 |
| CigPerDay | 337,334 | – | – | 55 | ~1.1 | Liu et al. (2019)42 |
| DrinksPerWeek | 941,280 | – | – | 99 | ~0.2 | Liu et al. (2019)42 |
| pulsePressure | 757,601 | – | – | 143/62d | 2.6 | Evangelou et al. (2018)43 |
| dBP | 757,601 | – | – | 130/120d | 4.5 | Evangelou et al. (2018)43 |
| sBP | 757,601 | – | – | 183/81d | 4.8 | Evangelou et al. (2018)43 |
| MDD | 500,199 | 170,756 | 329,443 | 102e | 1.5–3.2% | Howard et al. (2019)44 |
CAD coronary artery disease, IS ischemic stroke, T2D type 2 diabetes, BirthWeight birth weight, BMI body mass index, BodyFat body fat percentage, FastGluc fasting glucose level, FastInsulin fasting insulin level, HDL high-density lipoprotein cholesterol level, LDL low-density lipoprotein cholesterol level, Triglycerides triglyceride level, CRP C-reactive protein level, CigPerDay cigarettes per day, DrinksPerWeek drinks per week, pulsePressure pulse pressure, dBP diastolic blood pressure, sBP systolic blood pressure, MDD major depressive disorder.
aTrait variance explained by all GWAS SNPs/loci.
bMaximum number of samples used for meta-analysis, not only European population.
cDiscoveries in this study.
dTwo-stage/one-stage. One-stage analysis criteria: p-value < 5 × 10−9 for the discovery meta-analysis (757,601 samples), p-value < 0.01 for UKB (458,577 samples), p-value < 0.01 for ICBP (299,024 samples) and concordant direction of effect between UKB and ICBP. Two-stage analysis criteria: genome-wide significance in the combined meta-analysis, p-value < 0.01 in the replication meta-analysis and concordant direction of effect.
eFor all meta-analysis, not specific to European populations.
While estimation under the true model performed well in simulations, the true model is not known when applied to real data. Accordingly, to improve the robustness of MRCI we implemented an additional model fitting procedure which involved estimation under each sub-model and the full model, and performed model averaging of parameter estimates with weights that optimized the composite likelihood. Simulation results showed that this procedure usually assigned low weights to incorrect sub-models (Supplementary Fig. 4b). When the averaged model was preferred, which was usually the case when the exposure-specific component is absent (Supplementary Fig. 4c), parameter estimates from the model averaging procedure were adopted, instead of the full model estimates. In simulations under null, uni-directional, and bi-directional causation models, this method gave nearly unbiased estimates of the reciprocal causal effects (Fig. 3a) and correct control of Type I error rates when a causal effect was absent, and acceptable power when a causal effect was present and the model included exposure-specific SNPs (Fig. 3b). We also tested sub-model scenarios with unbalanced pleiotropy effects and observed similar estimation results of the reciprocal causations (Supplementary Fig. 5).
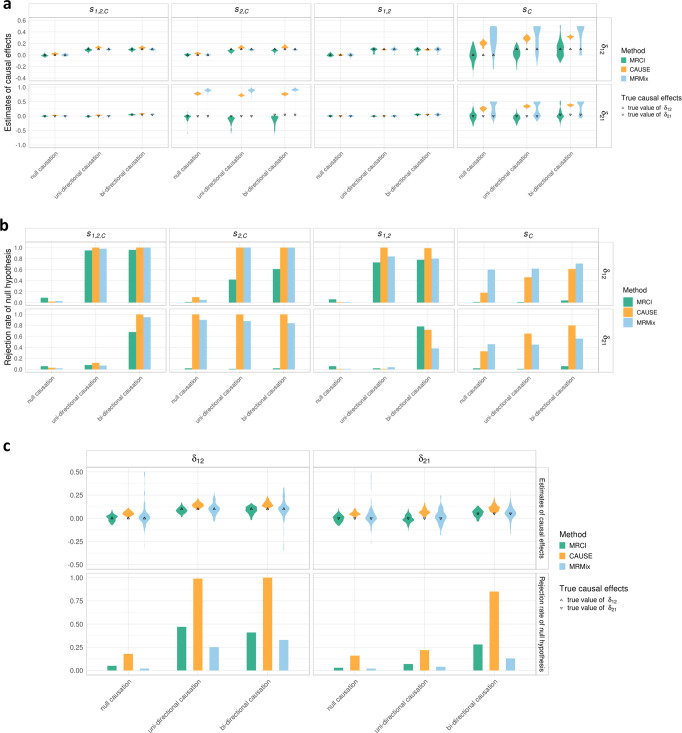
Fig. 3. Estimation after model averaging.
a Final estimates of causal effects under null, uni-directional, and bi-directional causations in four scenarios (, and ). When the exposure-specific SNPs exist, the final estimates after model averaging still produced nearly unbiased estimates in simulated scenarios. For null causation (gray) ; for uni-directional causation (blue), and ; for bi-directional causation (purple), and . The true causation values of and are indicated by up- and down-pointing triangles, respectively. b Rejection rates of the null hypothesis of the final and estimates after model averaging in different scenarios. For the zero-effect causal direction, the Type I error rates were well-controlled; for the non-zero-effect causal direction, the presence of the exposure-specific SNPs showed reasonably good power, and the absence of the exposure-specific SNPs showed conservative power of estimation. In the simulations, the mixing proportions of the present component were ; the pleiotropic effects were correlated (); and the heritabilities contributed by -specific, -specific and pleiotropic SNPs (if present in the sub-model scenario) were 0.3, 0.3, and 0.1, respectively.
Comparison with CAUSE and MRMix
CAUSE13 and MRMix12 are two recent methods that share similarities with MRCI. With large samples (50,000 for both phenotypes), when the true model was or , simulation results showed that these two methods produced unbiased estimates and correct Type I error rates. However, under scenarios where trait-specific SNPs were absent for one or both phenotypes (i.e., and ) these methods obtained biased causal estimates and inflated Type I error rates for the causal direction in which the exposure-specific SNPs were absent (Fig. 4a, b). With small samples (20,000 for both phenotypes), CAUSE produced biased estimates and increased Type I error rates, even under the full model. Under these small sample scenarios, both MRCI and MRMix maintained unbiased estimates and corrected Type I error rates, with MRCI achieving slightly smaller estimation variance and greater statistical power (Fig. 4c).
Fig. 4. Estimation comparison with CAUSE and MRMix.
a Estimates from MRCI (green), CAUSE (orange), and MRMix (blue) under null, uni-directional, and bi-directional causations in four scenarios (, and ). CAUSE and MRMix produced severely over-estimated causal effects when exposure-specific SNPs were absent in the sub-model and . For null causation, ; for uni-directional causation, and ; for bi-directional causation, and . The true causation values of and are indicated by up- and down-pointing triangles, respectively. b Rejection rates of the null hypothesis for and estimates from MRCI (green), CAUSE (orange), and MRMix (blue) in different simulated scenarios. CAUSE and MRMix produced inflated Type I error rates for the causal direction where exposure-specific SNPs were absent ( and ). c Estimates of causal effects and rejection rates of null hypothesis from MRCI (green), CAUSE (orange) and MRMix (blue) under null, uni-directional, and bi-directional causations in scenarios with small sample sizes (20,000 individuals). Decreased GWAS power led to over-estimates for CAUSE and larger estimation variance for MRMix. MRCI produced nearly unbiased estimates and correct Type I error rates. In these results, the estimates of MRCI came from the final estimates after model averaging; p-value thresholds for CAUSE and MRMix were and , respectively. In the simulations, the mixing proportions of the present component were ; the pleiotropic effects were correlated (); the heritabilities contributed by -specific, -specific and pleiotropic SNPs (if present in the sub-model scenario) were 0.3, 0.3, and 0.1, respectively.
Causation of risk factors on common diseases
We applied MRCI to study causal relationships between 3 common diseases (coronary artery disease, CAD; ischemic stroke, IS; type 2 diabetes, T2D) and 16 putative risk factor phenotypes (Table 1). Figure 5 shows the estimated reciprocal causal effects () between these diseases and phenotypes. Considering that 96 tests were performed, the Bonferroni adjusted significance level is . Causal influences significant at this level were from low-density lipoprotein level (LDL) to CAD (δ = 0.32, 95% CI = [0.18,0.47], p-value = 1.7 × 10−5), and from body mass index (BMI) to T2D (δ = 0.72, 95% CI = [0.59,0.85], p-value = 3.8 × 10−30). In the reverse direction, significant causal influences were detected from T2D to BMI (δ = −0.17, 95% CI = [−0.24,−0.10], p-value = 2.2 × 10−6) and fasting glucose (δ = 0.32, 95% CI = [0.20, 0.44], p-value = 6.9 × 10−8).
Fig. 5. Summary of estimates for three common diseases and sixteen risk factors.

In the figure, the upper triangle in a box represents the causal direction from the risk factor to the disorder, and the lower triangle represents the reverse causal direction. Darker color represents stronger causation estimates. Stars in the triangle represent different significance levels of the estimation. CAD coronary artery disease, IS any ischemic stroke, T2D type 2 diabetes, BirthWeight birth weight, BMI body mass index, BodyFat body fat percentage, FastGluc fasting glucose level, FastInsulin fasting insulin level, HDL high-density lipoprotein cholesterol level, LDL low-density lipoprotein cholesterol level, Triglycerides triglyceride level, CRP C-reactive protein level, CigPerDay cigarettes per day, DrinksPerWeek drinks per week, pulsePressure pulse pressure, dBP diastolic blood pressure, sBP systolic blood pressure, MDD major depressive disorder.
A number of nominally significant (p-value < 0.05) causal effects that did not survive multiple testing adjustments were detected (Fig. 5). These included effects of fasting glucose on CAD and LDL on both IS and T2D. Nominally significant effects in the reverse direction included CAD on BMI, LDL and diastolic blood pressure (dBP), and T2D on birth weight.
Discussion
We have developed a new method, MRCI, to jointly estimate the reciprocal causal effects between two phenotypes using GWAS summary statistics and reference LD data. Our extensive simulation studies, under both independent pleiotropy and correlated pleiotropy scenarios, indicate that MRCI obtains nearly unbiased estimates of causation in both directions, and maintains well-controlled Type I error rates under the null hypothesis, even when most causal SNPs for one or both phenotypes are pleiotropic. MRCI also achieves comparable statistical power to other methods when Type I error rates are controlled.
Our simulations showed that existing MR methods that require the selection of IVs produced unbiased estimates and correct Type I error rates when using genome-wide significant exposure-associated IVs, for scenarios with independent pleiotropy. However, some methods often produced biased estimates and severely inflated Type I error rates in the presence of correlated pleiotropy. For MR-Egger8 and MR-PRESSO9, designed to cope with horizontal pleiotropy under the InSIDE assumption, excluding potential outcome-associated SNPs according to a p-value cut-off helped control Type I error, but in practice, the optimal choice for cut-off is unknown and may vary depending on the genetic architecture of the phenotypes as well as GWAS sample sizes. These are important limitations as pleiotropy is common for complex traits9, and independent pleiotropy is implausible8.
The robustness of MRCI is partly derived from the explicit consideration of sub-models with absent SNP components during model fitting. When an SNP component is absent, estimation under the full model sometimes incorrectly infers the absent SNP components which can lead to spurious inferences on the causal effects. Thus, we perform estimation under both the full model and sub-models, but the goal is not to select a single best model. Rather, our aim is to obtain robust causal estimates. Based on simulation performance, our method of model averaging reduces the chance of such spurious inferences and produces unbiased estimates and correct control of Type I error rates even in these challenging scenarios. Two recent methods, CAUSE13 and MRMix12, which share some similarities with MRCI, nevertheless produced biased estimates and inflated Type I error rates when a trait-specific SNP component was absent.
MRCI also provides estimates for nuisance parameters such as heritabilities and genetic correlation, which may help clarify the genetic architecture of the two phenotypes. In our model, the parameters for the population stratification are also considered nuisance parameters, which behave similarly to genomic control when testing in mixed population simulations and barely affect the causal estimates in the simulated scenarios (Supplementary Fig. 6). Since most reported GWAS would have minimized population stratification effects prior to association testing, including these parameters during estimation represents an additional safeguard. The genetic correlation estimates from MRCI are consistent with results obtained from LDSC. Moreover, our model takes the sample overlap into consideration, including complete overlap which enables GWAS results obtained from the same sample (e.g., UK Biobank) to be analyzed for causal relationships.
When applied to real GWAS data, MRCI was able to identify several well-established causal relationships at a Bonferroni-corrected significance level, including a reciprocal causal relationship between body mass index and type 2 diabetes. Being overweight is known to be strongly associated with an increased risk of type 2 diabetes17–19, while weight loss is a known clinical feature of type 2 diabetes20. MRCI also confirmed low-density lipoprotein level but not high-density lipoprotein level as a causal factor for coronary artery disease21–23. MRCI did not detect additional causal effects at the Bonferroni-corrected significance level, which may reflect the ability of MRCI to control the Type I error rate. It is also possible that GWAS for some of the phenotypes may not have adequate statistical power because of small sample sizes or high polygenicity.
The current formulation of MRCI has certain limitations. Our assumption of bivariate normality of standardized marginal effects in the four SNP components may not hold in practice, and serious violation of this assumption may affect the performance of the method. Further simulations to evaluate the sensitivity of the method to violations of this assumption are desirable. A second limitation is that we used composite likelihood for model fitting because marginal SNP effects are correlated. This necessitated the use of robust sandwich standard errors, which may lead to conservative, less powerful tests. Finally, in the scenario where pleiotropic effects are very strong and nearly no causal SNPs contribute specifically to the exposure, MRCI will typically produce very large standard errors for the causal path estimate from exposure to the outcome, so there is little power to detect such a causal effect even when it is present. However, this situation of having almost no SNPs that can be used as valid IVs could be a limitation for the MR approach in general, rather than for MRCI specifically.
Methods
Data and the full model
MRCI uses the GWAS summary statistics of the two phenotypes ( and ) and reference LD information (~1 million SNPs from 1000 Genomes Project data). For a pair of reciprocal causal phenotypes (Fig. 1a), each available SNP belongs to one of four mutually exclusive SNP components:
-specific component (): SNPs that contribute directly to only;
-specific component (): SNPs that contribute directly to only;
pleiotropic component (): SNPs that contribute directly to both phenotypes;
null component (): SNPs with no direct effects on either phenotype.
The proportions of all SNPs in the four components are and . The values of the two phenotypes in an individual are given by:
Here, and are the two standardized phenotypes; is the causal effect and is the causal effect ; and represent the standardized genotype of th, th and th SNP in and component, respectively; and denote the direct effect sizes of phenotype-specific SNPs for and ; and denote the direct effect sizes of pleiotropic SNPs for and , respectively; and are residual effects. Since the SNPs in have no direct effects on either phenotype, they are not included. For the direct effect sizes of SNPs, we assume , and for and , where and denote the per-SNP variances of and , and and the per-SNP variances of for and respectively, with covariance . Therefore, the model encompasses both independent pleiotropy () and correlated pleiotropy ().
The above formulae can be expressed in the bivariate matrix form , where is a vector of the two standardized phenotypes, is the identity matrix, , is the direct effect of the th SNP on the phenotypes depending on its component membership , i.e. and , , , , is the standardized genotype for the th SNP and is the residual effects of any non-additive genetic and environmental factors. This expression is similar to that used for reciprocal causal modeling in twin data24 and requires that to ensure that the reciprocal causation between the two phenotypes results in a steady state rather than unlimited growth25. In practice, we constrain both and to be between −1.0 and 1.0, since both phenotypes are standardized variances as 1.0, ensuring the inequality.
If we define as a vector of the component-dependent joint effect sizes for the th SNP, including any effect mediated through one phenotype on the other, then the model can be expressed as . For each phenotype, the marginal effect of SNP is , where is the total number of SNPs tagged by the th SNP, is the LD correlation between th and th SNP, and is the joint effect size of the th SNP tagged by the th SNP26, taking account of the reciprocal causations.
Composite likelihood estimator
We assume that the estimates of the marginal effects of the th SNP from the GWAS summary statistics have a bivariate normal distribution:
In the formula, and represent the marginal effect size estimates of the th SNP from GWAS summary statistics of phenotype and , respectively. are the possible combinations of counts of SNPs in LD with SNP that belong to the four SNP components. The probability of each combination, , can be calculated based on the multinomial distribution with total counts over , where is a latent variable denoting the number of -component SNPs tagged by the th SNP. and can be derived from the relationships between the marginal and joint regression coefficients in mixture form (see Supplementary Note):
where is the LD score for the th SNP; and are additional inflation factors accounting for systematic bias in variance estimates (e.g., due to population stratification) for phenotype and respectively26; is a factor accounting for bias in the covariance estimates (e.g., due to sample overlap); and are the sample sizes for the two GWAS of the two phenotypes. In this way, the partitioned genetic variances, LD conditions as well as reciprocal causal effects are reflected in the assumed bivariate distribution.
The likelihood for the summary-statistic of the th SNP is then: = , where is the density function of a bivariate normal distribution with parameters . Thus, the composite log-likelihood function is in the form:
Thus, the maximum composite likelihood estimator is given by
Parameter estimation and testing
The reciprocal causal paths ( and ), together with nuisance parameters, are estimated by maximizing the likelihood with an expectation-maximization (EM) algorithm. For each M-step in the EM, parameters for mixing proportions ( and ) are estimated according to the closed form, while the remaining parameters (i.e. , ,, and ) are estimated by Nelder–Mead optimization (see Supplementary Note).
The standard errors of each parameter are calculated using a sandwich variance estimator adapted from Zhang et al.26 since sandwich estimators can provide valid variance estimation and tolerate the possible misspecification of the model. Briefly, if we define then the score function could be written as in the form: , where is the score vector for the th SNP. Then the sandwich form of variance-covariance matrix for the estimate is , which can be estimated by plugging in the estimated parameter values in lieu of . Thus, we can get and , where is the sum of likelihood scores for all SNPs tagged by the th SNP. In practice, we used the symmetric derivative to obtain the derivatives for parameter estimates (see Supplementary Note). To determine the significance of estimates for parameters of interest, estimates and the corresponding standard errors are converted to statistics.
Sub-models and model averaging
To increase the robustness of MRCI in real situations, we performed model fitting not only to the full model (referred to as the model) but also to four sub-models, each of which has one or two absent SNP components: (I) the model excludes SNPs; (II) the model excludes SNPs; (III) the model excludes both and SNPs; and (IV) the model excludes SNPs. For each sub-model, the parameters are estimated using the same composite likelihood estimator as above, only that the parameters of the corresponding absent components are set as zero during the EM process and are thus excluded in variance calculation. Accordingly, we define the complete model set .
After estimating all five models, we calculated weighted averages of the parameter estimates of these models to obtain an “averaged” model, and calculated its composite likelihood. The averaged estimate for the th parameter can be written as , where is the weight for the th model and is the estimate of the th parameter in the th model. is zero if the th parameter is not included in the th model. Then, the variance of the th averaged parameter can be calculated as , where is the variance of the th parameter in the th model and is defined as zero if the th parameter is not included in the th model27. The composite likelihood is then maximized over the weights for the five models, where the initial weights for the optimization are based on a modified Akaike information criterion (AIC) for composite likelihood28, for the five models (see Supplementary Note).
Finally, the averaged model will be selected as the final model if either of the following criteria is met: (1) the composite likelihood of the averaged model is higher than that of the model; or (2) for either of the two traits, the estimate of the trait-specific heritability from the model is <0.05 and the estimate of the corresponding trait-specific mixing proportion is not significant. Otherwise, the model is selected as the final model.
Genetic correlation calculation
Based on our reciprocal joint model, genetic correlation () between the two phenotypes is calculated as
The derivation of and the corresponding variance calculation can be found in Supplementary Note.
Simulation data
In summary, the simulation data were generated using imputed genotypes of 50,000 individuals randomly extracted from UK Biobank white British subjects. We only selected common SNPs (i.e., MAF ≥ 0.05) that are available in the HapMap 3 reference panel, resulting in a total of about 0.68 million SNPs. The majority of the simulations were based on 100% overlapping samples with a sample size of 50,000. Moreover, we tested our model using 0 and 50% overlapping samples with a sample size of 50,000. We also tested our model using 100% overlapping samples with a sample size of 20,000. The phenotypes were simulated using GCTA software29 based on these genotype data and the association tests were performed using PLINK software30. Detailed simulation scenarios (represented by simID in the table) and corresponding parameter settings can be found in Supplementary Table 1.
Specifically, in each simulation scenario, we first defined values of and for the scenario. The number of causal SNPs in each component was determined according to the assigned mixing proportions for the four SNP components. Then, the corresponding number of causal SNPs was randomly chosen from the set of available SNPs. For trait-specific SNPs, the direct effect sizes for causal SNPs were assigned based on and with and . For pleiotropic SNPs, the direct effect sizes for causal SNPs were assigned based on , with . Next, we converted the direct effect sizes to the component-dependent joint effect sizes using to take into account reciprocal causation. In this way, we could obtain the joint effect sizes of causal SNPs for each phenotype. Then we simulated the two phenotypes ( and ) with these joint effect sizes using GCTA software and performed the association test using PLINK to obtain the summary-level results. Finally, we repeated the simulations 100 times for each scenario.
For the full-model scenario (), we generated data under three causation scenarios: “bi-directional causation” when there are causal effects in both directions, “uni-directional causation” when there is a causal effect in only one direction, and “null causation” when there is no causal effect in either direction. We considered low and high polygenicity scenarios. For low polygenicity scenarios (LoS1—LoS12), we performed two sets of simulation studies: (I) independent pleiotropy ( and ); and (II) correlated pleiotropy ( and ) (Fig. 1b). For high polygenicity scenarios, we set and performed six simulation studies under correlated pleiotropy considering bi-directional, uni-directional and null causations (HiS1—HiS6). We also additionally simulated a high polygenicity scenario in which the two phenotypes had different mixing proportions and genetic variances (HiS7). For simulation studies with different sample sizes, we set and decreased the sample sizes to 20,000 under correlated pleiotropy scenarios (SS1–SS3).
For simulations involving binary phenotypes (HiS8), we assumed to be the continuous phenotype and to be the binary phenotype. For we used the above method (with 50,000 individuals) to obtain GWAS summary data. For , we generated the joint effect sizes on the liability scale, then took a total of 300,000 individuals to simulate a case-control study with a disease prevalence of 0.05 and case:control ratio of 1:2, using GCTA. Thus, we generated 15,000 cases from the 300,000 individuals and generated 30,000 controls from the remaining individuals. Consequently, the total sample size for the binary phenotype is 45,000. We then ran logistic regression analysis using PLINK to obtain the GWAS summary statistics for . Since the parameters in our model are on the liability scale, we converted the summary-level estimates of odds ratios to the liability scale effect size through approximation31,32 (see Supplementary Note).
For sub-model scenarios, we generated three sets of simulated data: no -specific component (), no pleiotropy component (), and pleiotropy component only (). For each sub-model, we further simulated data for bi-directional, uni-directional and null causations.
Moreover, we designed simulations using unbalanced effects for genetic components, which means that the genetic effects for each component are different. Under these scenarios, we first simulated data with sample overlapping changing from 0% to 100% (Unbalance 1–3). Then, we simulated sub-model scenarios with unbalanced settings (Unbalance , , and ).
Representative bivariate scatterplots for these simulations can be found in Fig. 1 and Supplementary Fig. 1.
Existing MR methods and LD score regression
We also ran several IV-based MR methods on the simulated data: Egger regression, Weighted Median, Weighted Mode, Inverse-Variance Weighted (IVW) (from the TwoSampleMR package3), MRMix12, and MR-PRESSO9. We tested three SNP selection methods: (a) use valid IVs, i.e. all the exposure-specific true causal SNPs assigned in the simulation as IVs; (b) use significant exposure-associated SNPs (p-value < ) but exclude potential outcome-associated SNPs by setting p-value > in outcome GWAS; (c) use significant exposure-associated SNPs regardless of their association with outcome. For SNPs selected in (b) and (c), we further performed clumping () to obtain the independent IVs for MR analysis. Additionally, we also compared with CAUSE13, a recent method using genome-wide summary statistics. The p-value thresholds for CAUSE and MRMix were set as 1 and , respectively. To calculate the genetic correlation using LD Score regression1, we followed the online tutorial and used the default settings.
Real data processing
We followed steps similar to those implemented by Zhang et al.26 to preprocess the public GWAS summary data. Briefly, SNPs were excluded if MAF was <5%; or if the imputation INFO score was low (INFO < 0.9); or if the available sample size was less than 0.67 of the 90th percentile of the available sample sizes for all SNPs; or if it was located within the major histocompatibility complex (MHC) region; or if the absolute value of standardized effect size is >0.1. The summary statistics of the remaining SNPs were merged with 1000 Genomes Project reference SNPs to obtain their corresponding LD scores.
Supplementary information
Acknowledgements
We thank the consortia for sharing the GWAS summary statistics. We thank Dr. Robert Porsch for critical advice on the model. The simulation studies were conducted using genotype data from the UK Biobank Resource accessed under Application Number 28732. The computations were performed using research computing facilities offered by Information Technology Services, The University of Hong Kong, and the High-Performance Computing Facility of Bioinformatics Core, Centre for PanorOmic Sciences (CPOS), LKS Faculty of Medicine, The University of Hong Kong. This work was supported by Hong Kong Research Grants Council Collaborative Research Grant C7044-19G, Hong Kong Innovation and Technology Bureau funding for the State Key Laboratory of Brain and Cognitive Sciences, and the National Natural Science Foundation of China (32170637).
Author contributions
P.C.S., Y.D.Z., Z.L., and Y.Q. conceived and designed the model and contributed to the interpretation of the results. Z.L. and Y.Q. designed the algorithm, implemented the software, and conducted analysis of simulation and real data. T.S.H.M. prepared the genotype data for simulation. T.W. contributed to statistical derivation. Y.D.Z. and M.L. prepared LD data and developed the software. L.B. and J.D.T. contributed to the interpretation of real data analysis. P.C.S., Z.L., and Y.Q. contributed to writing the manuscript. T.W., J.D.T., L.B., M.L., and Y.D.Z. contributed to the critical revision of the manuscript.
Peer review
Peer review information
Nature Communications thanks Frank Dudbridge and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. This article has been peer reviewed as part of Springer Nature’s Guided Open Access initiative.
Data availability
The genotype data for simulation were applied from UKB biobank (www.ukbiobank.ac.uk). LD infomation data were from GENESIS (https://github.com/yandorazhang/GENESIS) with permission. Public GWAS summary data were from the corresponding website: MAGIC consortium (ftp://ftp.sanger.ac.uk/pub/magic); CARDIoGRAMplusC4D (http://www.cardiogramplusc4d.org/data-downloads); Global Lipids Genetics Consortium (http://csg.sph.umich.edu/willer/public/lipids2013/); DIAGRAM consortium (https://diagram-consortium.org/downloads.html); EGG Consortium (http://egg-consortium.org/); GIANT consortium (http://portals.broadinstitute.org/collaboration/giant/index.php/Main_Page); GWAS catalog (https://www.ebi.ac.uk/gwas/downloads/summary-statistics).
Code availability
The MRCI program code can be found at https://github.com/zpliu/MRCI. Detailed results of all real data analyses can be visualized through the website: https://triangularcell.shinyapps.io/MRCI_Estimate_for_CommonDiseases.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Zipeng Liu, Yiming Qin.
Contributor Information
Miaoxin Li, Email: limiaoxin@mail.sysu.edu.cn.
Yan Dora Zhang, Email: doraz@hku.hk.
Pak Chung Sham, Email: pcsham@hku.hk.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-36490-4.
References
- 1.Bulik-Sullivan B, et al. An atlas of genetic correlations across human diseases and traits. Nat. Genet. 2015;47:1236–1241. doi: 10.1038/ng.3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O’Connor LJ, Price AL. Distinguishing genetic correlation from causation across 52 diseases and complex traits. Nat. Genet. 2018;50:1728–1734. doi: 10.1038/s41588-018-0255-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hemani G, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7:e34408. doi: 10.7554/eLife.34408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet. Epidemiol. 2013;37:658–665. doi: 10.1002/gepi.21758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ. 2018;362:k601. doi: 10.1136/bmj.k601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum. Mol. Genet. 2014;23:R89–R98. doi: 10.1093/hmg/ddu328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng J, et al. The effect of plasma lipids and lipid-lowering interventions on bone mineral density: a Mendelian Randomization Study. J. Bone Min. Res. 2020;35:1224–1235. doi: 10.1002/jbmr.3989. [DOI] [PubMed] [Google Scholar]
- 8.Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 2015;44:512–525. doi: 10.1093/ije/dyv080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 2018;50:693–698. doi: 10.1038/s41588-018-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted Median estimator. Genet. Epidemiol. 2016;40:304–314. doi: 10.1002/gepi.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int. J. Epidemiol. 2017;46:1985–1998. doi: 10.1093/ije/dyx102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qi G, Chatterjee N. Mendelian randomization analysis using mixture models for robust and efficient estimation of causal effects. Nat. Commun. 2019;10:1941. doi: 10.1038/s41467-019-09432-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morrison J, Knoblauch N, Marcus JH, Stephens M, He X. Mendelian randomization accounting for correlated and uncorrelated pleiotropic effects using genome-wide summary statistics. Nat. Genet. 2020;52:740–747. doi: 10.1038/s41588-020-0631-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu Z, et al. Causal associations between risk factors and common diseases inferred from GWAS summary data. Nat. Commun. 2018;9:224. doi: 10.1038/s41467-017-02317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burgess S, et al. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res. 2019;4:186. doi: 10.12688/wellcomeopenres.15555.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Qi G, Chatterjee N. A comprehensive evaluation of methods for Mendelian randomization using realistic simulations and an analysis of 38 biomarkers for risk of type 2 diabetes. Int. J. Epidemiol. 2021;50:1335–1349. doi: 10.1093/ije/dyaa262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeFronzo RA, et al. Type 2 diabetes mellitus. Nat. Rev. Dis. Prim. 2015;1:15019. doi: 10.1038/nrdp.2015.19. [DOI] [PubMed] [Google Scholar]
- 18.Bhupathiraju SN, Hu FB. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ. Res. 2016;118:1723–1735. doi: 10.1161/CIRCRESAHA.115.306825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bray GA, et al. The science of obesity management: an endocrine society scientific statement. Endocr. Rev. 2018;39:79–132. doi: 10.1210/er.2017-00253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chiu CJ, Li SL, Wu CH, Du YF. BMI trajectories as a Harbinger of pre-diabetes or underdiagnosed diabetes: an 18-year retrospective cohort study in Taiwan. J. Gen. Intern. Med. 2016;31:1156–1163. doi: 10.1007/s11606-016-3750-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Khera AV, Kathiresan S. Genetics of coronary artery disease: discovery, biology and clinical translation. Nat. Rev. Genet. 2017;18:331–344. doi: 10.1038/nrg.2016.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reiner Z. Hypertriglyceridaemia and risk of coronary artery disease. Nat. Rev. Cardiol. 2017;14:401–411. doi: 10.1038/nrcardio.2017.31. [DOI] [PubMed] [Google Scholar]
- 23.Malakar AK, et al. A review on coronary artery disease, its risk factors, and therapeutics. J. Cell Physiol. 2019;234:16812–16823. doi: 10.1002/jcp.28350. [DOI] [PubMed] [Google Scholar]
- 24.Toulopoulou T, et al. Reciprocal causation models of cognitive vs. volumetric cerebral intermediate phenotypes for schizophrenia in a pan-European twin cohort. Mol. Psychiatry. 2015;20:1386–1396. doi: 10.1038/mp.2014.152. [DOI] [PubMed] [Google Scholar]
- 25.Paxton, P., Hipp, J.R. & Marquart-Pyatt, S. Nonrecursive Models: Endogeneity, Reciprocal Relationships, and Feedback Loops (SAGE Publications, Inc, Thousand Oaks, CA, 2011).
- 26.Zhang Y, Qi G, Park J-H, Chatterjee N. Estimation of complex effect-size distributions using summary-level statistics from genome-wide association studies across 32 complex traits. Nat. Genet. 2018;50:1318–1326. doi: 10.1038/s41588-018-0193-x. [DOI] [PubMed] [Google Scholar]
- 27.Buckland ST, Burnham KP, Augustin NH. Model selection: an integral part of inference. Biometrics. 1997;53:603–618. doi: 10.2307/2533961. [DOI] [Google Scholar]
- 28.Varin C, Reid N, Firth D. An overview of composite likelihood methods. Stat. Sin. 2011;21:5–42. [Google Scholar]
- 29.Yang J, Lee SH, Goddard ME, Visscher PM. GCTA: a tool for genome-wide complex trait analysis. Am. J. Hum. Genet. 2011;88:76–82. doi: 10.1016/j.ajhg.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang CC, et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience. 2015;4:7. doi: 10.1186/s13742-015-0047-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu T, Sham PC. On the transformation of genetic effect size from logit to liability scale. Behav. Genet. 2021;51:215–222. doi: 10.1007/s10519-021-10042-2. [DOI] [PubMed] [Google Scholar]
- 32.Gillett AC, Vassos E, Lewis CM. Transforming summary statistics from logistic regression to the liability scale: application to genetic and environmental risk scores. Hum. Hered. 2018;83:210–224. doi: 10.1159/000495697. [DOI] [PubMed] [Google Scholar]
- 33.Nelson CP, et al. Association analyses based on false discovery rate implicate new loci for coronary artery disease. Nat. Genet. 2017;49:1385–1391. doi: 10.1038/ng.3913. [DOI] [PubMed] [Google Scholar]
- 34.Malik R, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat. Genet. 2018;50:524–537. doi: 10.1038/s41588-018-0058-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mahajan A, et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat. Genet. 2018;50:1505–1513. doi: 10.1038/s41588-018-0241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Warrington NM, et al. Maternal and fetal genetic effects on birth weight and their relevance to cardio-metabolic risk factors. Nat. Genet. 2019;51:804–814. doi: 10.1038/s41588-019-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yengo L, et al. Meta-analysis of genome-wide association studies for height and body mass index in approximately 700000 individuals of European ancestry. Hum. Mol. Genet. 2018;27:3641–3649. doi: 10.1093/hmg/ddy271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lu Y, et al. New loci for body fat percentage reveal link between adiposity and cardiometabolic disease risk. Nat. Commun. 2016;7:10495. doi: 10.1038/ncomms10495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lagou V, et al. Sex-dimorphic genetic effects and novel loci for fasting glucose and insulin variability. Nat. Commun. 2021;12:24. doi: 10.1038/s41467-020-19366-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Willer CJ, et al. Discovery and refinement of loci associated with lipid levels. Nat. Genet. 2013;45:1274–1283. doi: 10.1038/ng.2797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Han X, et al. Using Mendelian randomization to evaluate the causal relationship between serum C-reactive protein levels and age-related macular degeneration. Eur. J. Epidemiol. 2020;35:139–146. doi: 10.1007/s10654-019-00598-z. [DOI] [PubMed] [Google Scholar]
- 42.Liu M, et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 2019;51:237–244. doi: 10.1038/s41588-018-0307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Evangelou E, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat. Genet. 2018;50:1412–1425. doi: 10.1038/s41588-018-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Howard DM, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. Nat. Neurosci. 2019;22:343–352. doi: 10.1038/s41593-018-0326-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The genotype data for simulation were applied from UKB biobank (www.ukbiobank.ac.uk). LD infomation data were from GENESIS (https://github.com/yandorazhang/GENESIS) with permission. Public GWAS summary data were from the corresponding website: MAGIC consortium (ftp://ftp.sanger.ac.uk/pub/magic); CARDIoGRAMplusC4D (http://www.cardiogramplusc4d.org/data-downloads); Global Lipids Genetics Consortium (http://csg.sph.umich.edu/willer/public/lipids2013/); DIAGRAM consortium (https://diagram-consortium.org/downloads.html); EGG Consortium (http://egg-consortium.org/); GIANT consortium (http://portals.broadinstitute.org/collaboration/giant/index.php/Main_Page); GWAS catalog (https://www.ebi.ac.uk/gwas/downloads/summary-statistics).
The MRCI program code can be found at https://github.com/zpliu/MRCI. Detailed results of all real data analyses can be visualized through the website: https://triangularcell.shinyapps.io/MRCI_Estimate_for_CommonDiseases.