Abstract
BACKGROUND
Hyperemesis gravidarum is the most severe form of nausea and vomiting of pregnancy, potentially affecting both maternal and pregnancy health. Hyperemesis gravidarum often results in emergency department visits, although the exact frequency and costs associated with these visits have not been well studied.
OBJECTIVE
This study aimed to analyze the trends in hyperemesis gravidarum emergency department visits, inpatient admissions, and the associated costs between 2006 and 2014.
STUDY DESIGN
Patients were identified from the 2006 and 2014 Nationwide Emergency Department Sample database files using International Classification of Diseases, Ninth Revision diagnosis codes. Patients with a primary diagnosis of hyperemesis gravidarum, nausea and vomiting of pregnancy, and all nondelivery pregnancy-related diagnoses (all antepartum visits) were identified. All groups were analyzed; trends in demographics, number of emergency department visits, and visit costs were compared. Costs were inflation-adjusted to 2021 US dollars.
RESULTS
Emergency department visits for hyperemesis gravidarum increased by 28% from 2006 to 2014; however, the proportion of those who were subsequently admitted to the hospital decreased. The average cost of an emergency department visit for hyperemesis gravidarum increased by 65% ($2156 to $3549), as opposed to an increase of 60% for all antepartum visits ($2218 to $3543). The aggregate cost for all hyperemesis gravidarum visits increased by 110% ($383,681,346 to $806,696,513) from 2006 to 2014, which was similar to the increase observed for all antepartum emergency department visits.
CONCLUSION
From 2006 to 2014, emergency department visits for hyperemesis gravidarum increased by 28%, with associated costs increasing by 110%, whereas the number of admissions from the emergency department for hyperemesis gravidarum decreased by 42%.
Key words: healthcare utilization, medical economics, Nationwide Emergency Department Sample, nausea and vomiting of pregnancy
AJOG Global Reports at a Glance.
Why was this study conducted?
This study was conducted to examine the use of the emergency room over time in the treatment of hyperemesis gravidarum and how these trends correlate with admissions and cost.
Key findings
The number of emergency department visits for hyperemesis gravidarum increased from 2006 to 2014, but the proportion of people admitted to inpatient care decreased. The cost of emergency department visits for hyperemesis gravidarum increased over time, even with adjustment for inflation.
What does this add to what is known?
This study adds to limited existing literature on emergency department visits for hyperemesis gravidarum, which is important given the large number of patients who use the emergency department for care.
Introduction
Hyperemesis gravidarum (HG) is the most disruptive and severe form of nausea and vomiting of pregnancy (NVP).1,2 HG is one of the most common indications for hospital admission during early pregnancy,3,4 and is estimated to occur in 0.5%5 to 1.2% of pregnant patients.6
HG is typically accompanied by loss of >5% of prepregnancy weight and inadequate nutrition.1,2 HG can also have a profound effect on mental health, including posttraumatic stress symptoms, and thoughts and actions of delaying or avoiding another pregnancy.7, 8, 9 Pregnancies complicated by HG are associated with higher antepartum and total pregnancy costs; a 2005 meta-analysis reported the average total cost over the pregnancy as $7499 without HG and $17,938 with HG (reported in 2005 US dollars).5
Increased risk of HG is associated with younger age, multiple gestations, and certain preexisting conditions such as hyperthyroidism, psychiatric illness, diabetes mellitus, and gastrointestinal disorders.5,10 The pathophysiology of HG is poorly understood, but some studies have shown a genetic predisposition to HG.11,12 A genome-wide association study found an association between the presence of HG in pregnant patients and the placenta and appetite genes GDF15 and IGFBP7.13 Petry et al14 found an association between higher GDF15 serum levels and second-trimester nausea and vomiting or antiemetics use in pregnant patients. HG is managed with rehydration, pyridoxine, and antiemetics, which have been shown to be effective at preventing emergency department (ED) revisits and rehospitalization.15, 16, 17, 18 However, randomized controlled trials have generally been of “low quality.”19
Despite the frequent use of the ED by pregnant patients for HG treatment, to the best of our knowledge there have been no previous studies quantifying ED use for HG, the cost of these visits, or trends in ED use and cost over time. This study aims to both update and add to the limited existing literature on the prevalence and cost of ED visits for HG.
Materials and Methods
Data sources
This study evaluated the trends in ED visits for patients with a primary diagnosis of HG between 2006 and 2014 using the Nationwide Emergency Department Sample (NEDS), a database maintained by the Healthcare Cost and Utilization Project (HCUP) and the Agency for Healthcare Research and Quality (AHRQ). NEDS is the largest all-payer publicly available database on ED visits in the United States. The 2006 database contains approximately 26 million cases from 955 hospitals in 24 states, weighted to estimate 120 million ED visits; the 2014 database contains ∼31 million cases from 945 hospitals in 34 states, weighted to estimate almost 138 million ED visits.20 The database is a nationally representative patient-level sample of data with paired hospital and geographic characteristics. Statistics on ED trends over time and demographic data by International Classification of Diseases, Ninth Revision (ICD-9) codes are freely available on HCUPnet.21 The numbers of ED visits for the years between 2006 and 2014 were obtained from HCUPnet. Data for the number of births per year per age group were obtained from the National Vital Statistics Reports (NVSR) for each respective year.22
Study variables
HG cases were identified by primary diagnosis using ICD-9 codes for mild HG (643.0X) and severe HG (643.1X). Mild and severe diagnoses were combined into “hyperemesis gravidarum” because of the lack of consistent diagnostic criteria.23 In addition, patients with a primary diagnosis of NVP (643.2X, 643.8X, 643.9X) and all nondelivery pregnancy-related diagnoses (any antepartum condition) were analyzed as comparisons. Comparisons were made on variables predefined by HCUP, including age, ED cost, discharge status, household income, hospital location (large metropolitan, medium and small metropolitan, and micropolitan and rural), and primary insurer (Medicare, Medicaid, private, self-pay, no charge, and other). The secondary diagnoses were also reviewed to examine common secondary complaints.
HCUP defines a “large metropolitan area” as a central or suburban county of a city with ≥1 million population. “Medium and small” metro areas are counties with a population <1 million but >50,000. “Micropolitan and rural” areas are rural counties with a population <50,000. Household income is reported as the median income for the patient's zip code relative to the national median income. The median income of the patient's zip code is reported using demographic data from Claritas.24
Statistical analysis
The rate per 100,000 ED visits for a specific diagnosis was calculated by dividing the number of ED visits with that primary diagnosis by the total number of ED visits and multiplying by 100,000. Trends in admission over time are reported as percentage of ED visits that result in hospital admission. Rates of ED visits from 2006 to 2014 are reported as proportions of births in that year that resulted in an ED visit for HG. The percentage of US births with a visit to the ED for HG or NVP each year was calculated by extrapolating the NEDS data to NVSR data assuming an average of 1 fetus per pregnant patient. All cost data were adjusted for inflation to June 2021 US dollars using the Consumer Price Index inflation calculator.25 The total aggregate cost data were calculated by multiplying the mean cost by the total number of ED visits. Statistical analysis was performed on the 2006 and 2014 NEDS data using IBM SPSS Statistics, Version 28.0 (IBM Corp, Armonk, NY) and RStudio (RStudio, Boston, MA). For quantitative variables, the mean, median, standard deviation, and standard error were calculated. For categorical variables, the proportions for each category were tallied. The 95% confidence intervals (CIs) were calculated by adding and subtracting the standard error from the mean.
Results
Patient demographics
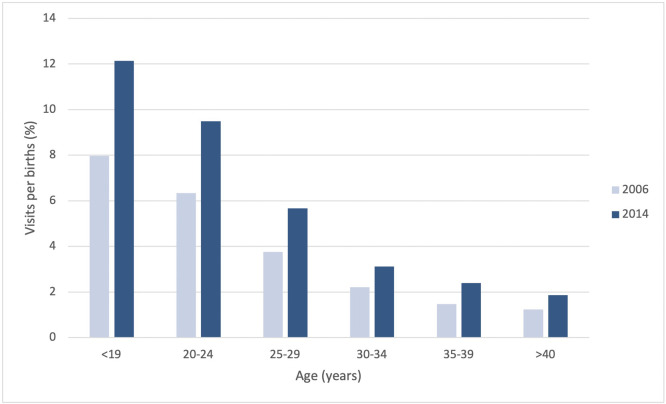
The mean age at presentation for pregnant patients with HG visiting the ED increased slightly from 2006 to 2014 (24.2–25.3 years) (Figure 1). The proportion of patients in the youngest group (<19 years old) had the largest decrease from 2006 to 2014 (19.8% to 13.4%), whereas the proportion of patients aged >30 years increased from 16.7% to 21.2%. The proportion of patients in the lowest-income quartile increased from 34.5% to 37.7%, whereas those in the highest-income quartile decreased from 13.6% to 12.4% between 2006 and 2014. The proportion of patients with HG covered by Medicaid increased from 47.9% to 57.6% (Table 1). Per US births, the percentage of pregnant patients with a visit to the ED for HG increased across all age brackets, with the largest increase in the youngest group (Figure 2). The trends for pregnant patients with NVP visiting the ED were similar to those observed in pregnant patients with HG (Table 2). Demographic data for patients visiting the ED with any antepartum condition also follow similar trends (Supplementary Table 1).
Figure 1.
Mean age by diagnosis over time
Trends in mean age of all pregnant patients presenting to the ED with a primary diagnosis of NVP or HG compared with the mean age of childbirth in the United States between 2006 and 2014.
ED, emergency department; HG, hyperemesis gravidarum; NVP, nausea and vomiting of pregnancy.
Geeganage. Emergency department burden of hyperemesis gravidarum. Am J Obstet Gynecol Glob Rep 2023.
Table 1.
Emergency department visits with primary diagnosis of hyperemesis gravidarum
| Observation | 2006 N (%) Mean (SD) |
2014 N (%) Mean (SD) |
|---|---|---|
| N primary dx of HG N per 100,000 ED visits Mean age (y) Range <19 20–24 25–29 30–34 35–39 >40 Mean ED cost ($) Median ED cost ($) Total aggregate cost ($) Mean number of diagnoses Range Discharge status Discharged Admitted Median-income quartile Highest-income level Second quartile Third quartile Lowest-income level Region Northeast Midwest South West Patient location Large metropolitan Medium and small metropolitan Micropolitan and rural Primary insurer Medicare Medicaid Private insurance Self-pay No charge Other |
177,940 148.2 24.2 (5.3) 12–54 35,195 (19.8) 68,531 (38.5) 44,495 (25.0) 21,004 (11.8) 7322 (4.1) 1392 (0.8) 2156.24 (1757.02) 1808.57 383,681,345.60 2.2 (1.6) 1–21 164,229 (92.3) 13,711 (7.7) 24,060 (13.6) 38,868 (21.9) 50,557 (28.6) 61,929 (34.5) 26,623 (15.0) 41,685 (23.4) 76,602 (43.0) 33,030 (18.6) 94,571 (53.2) 55,557 (31.2) 27,241 (15.3) 1506 (0.9) 85,316 (47.9) 56,069 (31.5) 27,748 (15.6) 1947 (1.1) 4769 (2.7) |
227,298 164.9 25.3 (5.4) 11–52 30,559 (13.4) 83,698 (36.8) 64,968 (28.6) 33,658 (14.8) 12,214 (5.4) 2203 (1.0) 3549.07 (3119.55) 2848.02 806,696,512.86 2.9 (2.1) 1–25 217,043 (95.5) 10,256 (4.5) 28,160 (12.4) 44,102 (19.4) 66,586 (29.3) 85,726 (37.7) 37,184 (16.4) 53,486 (23.5) 96,270 (42.3) 40,358 (17.8) 118,337 (52.1) 77,617 (34.2) 30,558 (13.4) 2879 (1.3) 130,890 (57.6) 62,868 (27.7) 22,809 (10.0) 842 (0.4) 6697 (2.9) |
Descriptive statistics for all pregnant patients who visited the ED with a primary dx of HG. All charges reported in 2021 US dollars. Percentages may not add up to 100% because of missing data.
dx, diagnosis; ED, emergency department; HG, hyperemesis gravidarum; SD, standard deviation.
Geeganage. Emergency department burden of hyperemesis gravidarum. Am J Obstet Gynecol Glob Rep 2023.
Figure 2.
Hyperemesis gravidarum visits by age group over time
Percentage of US births with an emergency department visit for hyperemesis gravidarum by age group, 2006 vs 2014. Similar trends were observed for nausea and vomiting of pregnancy.
Geeganage. Emergency department burden of hyperemesis gravidarum. Am J Obstet Gynecol Glob Rep 2023.
Table 2.
Emergency department visits with primary diagnosis of nausea and vomiting of pregnancy
| Observation | 2006 N (%) Mean (SD) |
2014 N (%) Mean (SD) |
|---|---|---|
| N primary dx of NVP N per 100,000 ED visits Mean age (y) Range <19 20–24 25–29 30–34 35–39 >40 Mean ED cost ($) Median ED cost ($) Total aggregate cost ($) Mean number of diagnoses Range Discharge status Discharged Admitted Median-income quartile Highest-income level Second quartile Third quartile Lowest-income level Region Northeast Midwest South West Patient location Large metropolitan Medium and small metropolitan Micropolitan and rural Primary insurer Medicare Medicaid Private insurance Self-pay No charge Other |
34,873 29.1 24.1 (5.4) 12-47 7182 (20.6) 13,669 (39.2) 8279 (23.7) 3928 (11.3) 1559 (4.5) 256 (0.7) 1993.93 (1596.81) 1649.63 69,534,320.89 2.3 (1.6) 1–19 33,984 (97.4) 890 (2.6) 3729 (10.7) 7270 (20.8) 10,346 (29.7) 12,975 (37.2) 4348 (12.5) 7278 (20.9) 17,680 (50.7) 5567 (15.9) 16,363 (47.0) 12,038 (34.5) 6351 (18.2) 272 (0.8) 19,811 (54.2) 9818 (28.2) 4587 (13.1) 248 (0.7) 940 (2.7) |
58,436 42.4 25.4 (5.4) 12-52 7342 (12.6) 21,410 (36.6) 16,713 (28.6) 9099 (15.6) 3171 (5.4) 682 (1.2) 3441.37 (2878.65) 2776.01 201,099,897.32 2.9 (2.0) 1–28 57,571 (98.5) 865 (1.5) 5845 (10.0) 10,397 (17.8) 17,004 (29.1) 24,342 (41.7) 11,752 (20.1) 12,371 (21.1) 26,929 (46.1) 7384 (12.6) 29,563 (50.6) 20,506 (35.1) 8155 (13.9) 1053 (1.8) 34,888 (59.7) 15,589 (26.7) 5083 (8.7) 163 (0.3) 1598 (2.7) |
Descriptive statistics for all pregnant patients who visited the ED with a primary dx of NVP. All charges reported in 2021 US dollars. Percentages may not add up to 100% because of missing data.
dx, diagnosis; ED, emergency department; NVP, nausea and vomiting of pregnancy; SD, standard deviation.
Geeganage. Emergency department burden of hyperemesis gravidarum. Am J Obstet Gynecol Glob Rep 2023.
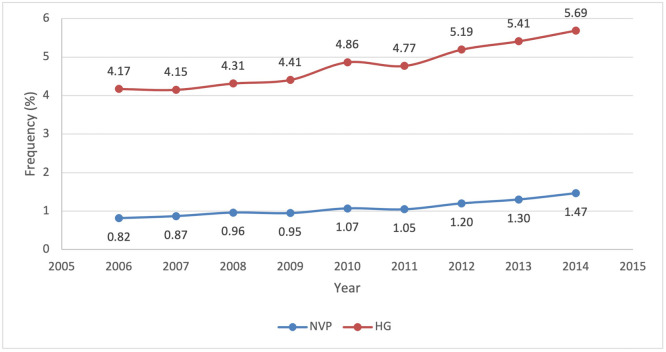
Emergency department visits
In 2014, HG was the third most common reason, after threatened abortion and genitourinary tract infection, for early pregnancy ED visits (Supplementary Table 2), with 7.2% of those visits having reported HG as the primary diagnosis. The number of ED visits with HG as the primary diagnosis increased by 27.7% from 2006 to 2014, as opposed to a 15% increase in all ED visits. Per 100,000 ED visits, the visit rate increased from 148.2 to 164.9. Out of all US births, the percentage of pregnant patients with HG or NVP who visited the ED increased from 4.2% to 5.7% between 2006 and 2014 (Figure 3). Despite the increase in ED visits for HG, admission rates from the ED decreased from 7.7% to 4.5% from 2006 to 2014 (Supplemental Figure 1). In 2014, HG was the fourth most common reason for admission for pregnant patients (Supplementary Table 3). Similarly, in that time, the number of ED visits for NVP increased by 67%, and the rate per 100,000 ED visits increased from 29.1 to 42.4. NVP admission rates decreased from 2.6% to 1.5% (Supplementary Figure 1).
Figure 3.
Percentage of ED visits per US births
Trends in percentage of total US births with an ED visit for NVP and HG between 2006 and 2014.
ED, emergency department; HG, hyperemesis gravidarum; NVP, nausea and vomiting of pregnancy.
Geeganage. Emergency department burden of hyperemesis gravidarum. Am J Obstet Gynecol Glob Rep 2023.
Emergency department costs
The mean ED cost per patient for HG increased from $2156.25 (95% CI, 2151.54–2160.96) to $3549.07 (95% CI, 3549.05–3556.09)—a 65% increase (Supplementary Figure 2). The aggregate cost for HG increased by 110% from $383,681,346 (95% CI, 382,843,692–384,518,999) to $806,696,513 (95% CI, 805,100,999–808,292,027) (Supplementary Figure 3). Similarly, the mean ED cost per patient for NVP increased by 73% from $1993.93 (95% CI, 1984.43–2003.43) to $3441.27 (95% CI, 1990.93–2015.92). The aggregate cost of NVP increased from $69,534,321 (95% CI, 69,203,121–69,865,521) to $201,099,897 (95% CI, 200,369,751–201,830,044)—a 189% increase. For patients with any antepartum condition visiting the ED, the trends in costs are similar (Supplementary Table 1).
Secondary diagnoses
The most common secondary diagnoses after a primary diagnosis of HG were dehydration, genitourinary tract infection, diarrhea, and abdominal pain. In 2006, 12.5% of HG patients who visited the ED had dehydration as a secondary diagnosis; in 2014, the incidence decreased to 8.1%. Patients with a primary diagnosis of NVP had similar common secondary diagnoses. In 2006, 5.2% of NVP patients had dehydration listed as a secondary diagnosis, and 4.8% had a coexisting urinary tract infection (UTI). In 2014, 5.0% of NVP patients had UTI listed as a secondary diagnosis, and 3.0% of patients had dehydration as a secondary diagnosis.
Discussion
Principal findings
Using the NEDS data on all US ED visits, this study found an over 27% increase in all ED visits for HG between 2006 and 2014. Despite this, there was a nearly 60% reduction in HG admissions during the same time. Comparable with the increase in costs of all antepartum ED visits between 2006 to 2014, the average cost of an ED visit for HG increased by 65%, and the aggregate cost increased by 110%.
Results
Demographic findings of this study are consistent with previous studies. The mean age of HG patients at ED visit increased from 24.2 to 25.3 years from 2006 to 2014, comparable with the increase in mean age for any (related to HG or not) antepartum visit from 25.2 to 26.3 years. The average age at ED visit of HG patients was 1.11 years lower than the average age at any antepartum ED visit, which is consistent with current belief that HG primarily affects pregnant patients of younger ages.5 We also observed a decrease in HG and NVP patients aged <24 years, and an increase in HG and NVP patients aged >25 years. This follows the upward trend of the average age of giving birth.
Our findings are consistent with previous work with respect to insurance status and payer mix.26 The proportion of patients with Medicaid as the primary insurer increased from 47.9% to 57.6% from 2006 to 2014, which is comparable with the increase observed for all antepartum visits. Pregnant patients in the lowest 2 income quartiles visit the ED more frequently than pregnant patients in the higher income levels, likely because of the lack of access to established obstetrical care in early pregnancy.27
Recent reviews report HG as the most common reason for hospitalization in the first half of pregnancy, and as second only to preterm labor for hospitalization overall.3,28 In contrast, our study shows that HG was the third most common indication for ED visits during early pregnancy (Supplementary Table 2) and the fourth most common reason for inpatient admission from the ED (Supplementary Table 3). Similarly, Monti et al29 recently published a study using 2017 data from 246 hospitals in the state of California identifying HG as the fourth most common reason for ED visit in early pregnancy and the third most common reason for inpatient admission from the ED during pregnancy.
Despite the decrease in the number of births in the United States between 2006 and 2014, this study found an increase in HG and NVP ED visits.30,31 Although the reasons for this increase remain unknown, we believe that the following could help explain this trend: reduced capacity at outpatient infusion service, payer restrictions on admission for outpatient services, increased use of observation status, and reduced capacity of obstetrical services over time.32 Similarly, a possible explanation for the 65% increase in the average cost of a HG ED visit but a 110% increase in the aggregate cost of HG ED visits is that the cost burden of treating HG is shifted to the ED instead of being charged to the inpatient. Further research is also needed to determine why patients are decreasingly admitted as inpatients. However, it should be noted that the cost increased at a similar rate for HG as for all antepartum ED visits, which may indicate that increasing cost is not diagnosis-specific. By comparison, the average cost per patient for all ED visits increased by 93%, suggesting that treating HG may not be as costly as treating other diagnoses.
Clinical implications
As ED visits for HG and NVP rise, with concurrent rising ED visit costs, these trends raise the question of where is the best location for treatment of HG and NVP. We believe that seeking care in an emergency room setting for such symptoms is a poor utilization of ED resources, which are already strained during the current pandemic.33 In the increasingly restrictive climate regarding healthcare access, without new innovative care settings and additional access, patients and providers are limited to few alternatives to the ED. Furthermore, given the current global pandemic, there are additional safety concerns for pregnant patients, who may be particularly susceptible to infection.34
Research implications
This study found that although the number of HG ED visits has increased, the proportion of patients admitted has decreased. Further studies are needed to address the reason for these trends and potential correlations between treatments given in the ED and discharge status. In addition, many unanswered questions remain because of the limitations of the NEDS database, which does not include information on gestational age or fetal number, which has been shown to correlate with HG symptoms.12 This study also does not account for urgent care visits, obstetrics-specific triage units, or direct admissions bypassing the ED, which are not included in the NEDS, and may be interesting to examine and compare with ED care. Lastly, and critically important, the absence of race or ethnicity data in the NEDS database results in a critical void of data that are necessary to understand any disparities on this topic.
Strengths and limitations
This study has many strengths. First, we used the NEDS database, a weighted, nationally representative dataset of all ED visits, strengthening the generalizability of our findings across the United States. Second, despite the limitations of working with large databases, by using data from several national databases (NEDS, AHRQ, NVSR), we further increased the generalizability of these results. Third, relative to the existing literature, this was a large study on ED visits for HG and NVP.
This study also has limitations. As with other publicly available and nationally representative datasets, the NEDS contains deidentified data that are dependent on hospital coding; thus, we were unable to confirm the accuracy of the diagnoses or determine whether a single individual used the ED multiple times for the same diagnosis. The database only identifies the US region (Northeast, South, Midwest, West) with regard to hospital location, so it is not possible to address policy changes such as Medicaid expansion by state and their effect on ED visits. Lastly, cases were identified by primary diagnosis, raising the possibility that some patients with a secondary or tertiary diagnosis of HG were excluded from the analysis.
Conclusions
ED visits for HG have increased by 27.7% between the years 2006 and 2014, whereas inpatient admissions have decreased by 42%. The increase in HG ED visits is disproportional to the trends in US births over the same years. The costs associated with ED visits for HG have risen proportionally with costs associated with all antepartum ED visits.
Footnotes
G.G. and J.I. share first authorship.
The authors report no conflict of interest.
G.G. received research funding from the Charles Hamilton Houston Program at the Amherst College Loeb Center.
Patient consent was not required because no personal information or details were included.
The findings of this study were presented at the 45th annual meeting of the New England Perinatal Society, Newport, RI, April 8–10, 2022.
Cite this article as: Geeganage G, Iturrino J, Shainker SA, et al. Emergency department burden of hyperemesis gravidarum in the United States from 2006 to 2014. Am J Obstet Gynecol Glob Rep 2023;3:100166.
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.xagr.2023.100166.
Appendix. Supplementary materials
References
- 1.Havnen GC, Truong MBT, Do MH, Heitmann K, Holst L, Nordeng H. Women's perspectives on the management and consequences of hyperemesis gravidarum – a descriptive interview study. Scand J Prim Health Care. 2019;37:30–40. doi: 10.1080/02813432.2019.1569424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fejzo MS, Trovik J, Grooten IJ, et al. Nausea and vomiting of pregnancy and hyperemesis gravidarum. Nat Rev Dis Primers. 2019;5:62. doi: 10.1038/s41572-019-0110-3. [DOI] [PubMed] [Google Scholar]
- 3.Loh KY, Sivalingam N. Understanding hyperemesis gravidarum. Med J Malaysia. 2005;60:394–399. [PubMed] [Google Scholar]
- 4.Gazmararian JA, Petersen R, Jamieson DJ, et al. Hospitalizations during pregnancy among managed care enrollees. Obstet Gynecol. 2002;100:94–100. doi: 10.1016/s0029-7844(02)02024-0. [DOI] [PubMed] [Google Scholar]
- 5.Bailit JL. Hyperemesis gravidarium: epidemiologic findings from a large cohort. Am J Obstet Gynecol. 2005;193:811–814. doi: 10.1016/j.ajog.2005.02.132. [DOI] [PubMed] [Google Scholar]
- 6.Einarson TR, Piwko C, Koren G. Prevalence of nausea and vomiting of pregnancy in the USA: a meta analysis. J Popul Ther Clin Pharmacol. 2013;20:e163–e170. [PubMed] [Google Scholar]
- 7.Fell DB, Dodds L, Joseph KS, Allen VM, Butler B. Risk factors for hyperemesis gravidarum requiring hospital admission during pregnancy. Obstet Gynecol. 2006;107:277–284. doi: 10.1097/01.AOG.0000195059.82029.74. [DOI] [PubMed] [Google Scholar]
- 8.Nana M, Tydeman F, Bevan G, et al. Hyperemesis gravidarum is associated with increased rates of termination of pregnancy and suicidal ideation: results from a survey completed by >5000 participants. Am J Obstet Gynecol. 2021;224:629–631. doi: 10.1016/j.ajog.2021.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Poursharif B, Korst LM, Macgibbon KW, Fejzo MS, Romero R, Goodwin TM. Elective pregnancy termination in a large cohort of women with hyperemesis gravidarum. Contraception. 2007;76:451–455. doi: 10.1016/j.contraception.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Christodoulou-Smith J, Gold JI, Romero R, et al. Posttraumatic stress symptoms following pregnancy complicated by hyperemesis gravidarum. J Matern Fetal Neonatal Med. 2011;24:1307–1311. doi: 10.3109/14767058.2011.582904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trogstad LI, Stoltenberg C, Magnus P, Skjaerven R, Irgens LM. Recurrence risk in hyperemesis gravidarum. BJOG. 2005;112:1641–1645. doi: 10.1111/j.1471-0528.2005.00765.x. [DOI] [PubMed] [Google Scholar]
- 12.Fejzo MS, Ingles SA, Wilson M, et al. High prevalence of severe nausea and vomiting of pregnancy and hyperemesis gravidarum among relatives of affected individuals. Eur J Obstet Gynecol Reprod Biol. 2008;141:13–17. doi: 10.1016/j.ejogrb.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fejzo MS, Sazonova OV, Sathirapongsasuti JF, et al. Placenta and appetite genes GDF15 and IGFBP7 are associated with hyperemesis gravidarum. Nat Commun. 2018;9:1178. doi: 10.1038/s41467-018-03258-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petry CJ, Ong KK, Burling KA, et al. Associations of vomiting and antiemetic use in pregnancy with levels of circulating GDF15 early in the second trimester: a nested case-control study. Wellcome Open Res. 2018;3:123. doi: 10.12688/wellcomeopenres.14818.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vutyavanich T, Wongtra-ngan S, Ruangsri R. Pyridoxine for nausea and vomiting of pregnancy: a randomized, double-blind, placebo-controlled trial. Am J Obstet Gynecol. 1995;173:881–884. doi: 10.1016/0002-9378(95)90359-3. [DOI] [PubMed] [Google Scholar]
- 16.Abas MN, Tan PC, Azmi N, Omar SZ. Ondansetron compared with metoclopramide for hyperemesis gravidarum: a randomized controlled trial. Obstet Gynecol. 2014;123:1272–1279. doi: 10.1097/AOG.0000000000000242. [DOI] [PubMed] [Google Scholar]
- 17.Lacasse A, Lagoutte A, Ferreira E, Bérard A. Metoclopramide and diphenhydramine in the treatment of hyperemesis gravidarum: effectiveness and predictors of rehospitalisation. Eur J Obstet Gynecol Reprod Biol. 2009;143:43–49. doi: 10.1016/j.ejogrb.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 18.Lowe SA, Steinweg KE. Review article: management of hyperemesis gravidarum and nausea and vomiting in pregnancy. Emerg Med Australas. 2022;34:9–15. doi: 10.1111/1742-6723.13909. [DOI] [PubMed] [Google Scholar]
- 19.McParlin C, O'Donnell A, Robson SC, et al. Treatments for hyperemesis gravidarum and nausea and vomiting in pregnancy: a systematic review. JAMA. 2016;316:1392–1401. doi: 10.1001/jama.2016.14337. [DOI] [PubMed] [Google Scholar]
- 20.Agency for Healthcare Research and Quality . 2017. The HCUP Nationwide Emergency Department Sample (NEDS)https://hcup-us.ahrq.gov/db/nation/neds/NEDS_Introduction_2017.jsp#census Available at: Accessed August 2, 2021. [Google Scholar]
- 21.Agency for Healthcare Research and Quality. Data Use Agreement for HCUPnet. Available at: https://hcupnet.ahrq.gov/. Accessed June 21, 2022.
- 22.CDC/National Center for Health Statistics . 2021. Products. National Vital Statistics Reports.https://www.cdc.gov/nchs/products/nvsr.htm Available at: Accessed July 29, 2021. [Google Scholar]
- 23.Koot MH, Boelig RC, Van't Hooft J, et al. Variation in hyperemesis gravidarum definition and outcome reporting in randomised clinical trials: a systematic review. BJOG. 2018;125:1514–1521. doi: 10.1111/1471-0528.15272. [DOI] [PubMed] [Google Scholar]
- 24.Agency for Healthcare Research and Quality. NEDS description of data elements. Healthcare Cost and Utilization Project. Available at:https://www.hcup-us.ahrq.gov/db/nation/neds/nedsdde.jsp. Accessed July 29, 2021.
- 25.US Bureau of Labor Statistics. CPI inflation calculator. Available at: https://www.bls.gov/data/inflation_calculator.htm. Accessed July 28, 2021.
- 26.Malik S, Kothari C, MacCallum C, Liepman M, Tareen S, Rhodes KV. Emergency department use in the perinatal period: an opportunity for early intervention. Ann Emerg Med. 2017;70:835–839. doi: 10.1016/j.annemergmed.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 27.Khan Y, Glazier RH, Moineddin R, Schull MJ. A population-based study of the association between socioeconomic status and emergency department utilization in Ontario. Canada. Acad Emerg Med. 2011;18:836–843. doi: 10.1111/j.1553-2712.2011.01127.x. [DOI] [PubMed] [Google Scholar]
- 28.London V, Grube S, Sherer DM, Abulafia O. Hyperemesis gravidarum: a review of recent literature. Pharmacology. 2017;100:161–171. doi: 10.1159/000477853. [DOI] [PubMed] [Google Scholar]
- 29.Monti D, Wang CY, Yee LM, Feinglass J. Antepartum hospital use and delivery outcomes in California. Am J Obstet Gynecol MFM. 2021;3 doi: 10.1016/j.ajogmf.2021.100461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martin JA, Hamilton BE, Sutton PD, et al. Natl Vital Stat Rep. 2009;57(7):1–101. [PubMed] [Google Scholar]
- 31.Hamilton BE, Martin JA, Osterman MJK, Curtin SC, Mathews TJ. Births: final data for 2014. Natl Vital Stat Rep. 2015;64:1–64. [PubMed] [Google Scholar]
- 32.Kozhimannil KB, Interrante JD, Tuttle MKS, Henning-Smith C. Changes in hospital-based obstetric services in rural US counties, 2014–2018. JAMA. 2020;324:197–199. doi: 10.1001/jama.2020.5662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382:2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 34.Wastnedge EAN, Reynolds RM, van Boeckel SR, et al. Pregnancy and COVID-19. Physiol Rev. 2021;101:303–318. doi: 10.1152/physrev.00024.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.