Summary
Background
Recent literature has shown that many women worldwide are victims of obstetric violence during childbirth. Despite that, few studies are exploring the consequences of such violence on women's and newborn's health. Thus, the present study aimed to investigate the causal association between obstetric violence during childbirth and breastfeeding.
Methods
We used data from the study “Birth in Brazil”, a national hospital-based cohort of puerperal women and their newborns in 2011/2012. The analysis involved 20,527 women. Obstetric violence was a latent variable composed of seven indicators (physical or psychological violence, disrespect, lack of information, privacy and communication with the healthcare team, inability to ask questions, and loss of autonomy). We worked with two outcomes: 1) breastfeeding at the maternity and 2) breastfeeding 43–180 days after birth. We applied multigroup structural equation modelling, based on the type of birth.
Findings
Obstetric violence during childbirth may decrease the probability for women to leave the maternity ward breastfeeding exclusively, having a stronger effect on women who have vaginal birth. Also, being exposed to obstetric violence during childbirth could indirectly affect those women's ability to breastfeed 43–180 days after birth.
Interpretation
This research concludes that obstetric violence during childbirth is a risk factor for breastfeeding discontinuation. Such knowledge is relevant so interventions and public policies can be proposed in order to mitigate obstetric violence and provide a better understanding of the context that may lead a woman into discontinuing breastfeeding.
Funding
This research was funded by CAPES, CNPQ, DeCiT, and INOVA-ENSP.
Keywords: Obstetric violence during childbirth, Breastfeeding, Women's rights
Research in context.
Evidence before this study
We searched Medline, Embase, and LILACS for published articles with no restriction on language and publication date. The Medline search included the following terms (“disrespect and abuse” OR “disrespect & abuse” OR “mistreatment” OR “institutional violence” OR “obstetric violence”) AND (“Breast Feeding” [Mesh])–adapting for Embase and LILACS. All searches were for content published up to May 9, 2022. We have found two published articles in Medline, 12 in Embase, and five in LILACS. Two articles were common in all databases. Therefore, only 17 articles were available. Of these, only one manuscript focused on mistreatment in childbirth in breastfeeding. Nevertheless, this study approached theoretical and psychosocial mechanisms of how mistreatment could affect breastfeeding, not including data analysis.
The plausibility relationship between mistreatment and breastfeeding was suggested by the analogy of intimate partner violence and interruption of breastfeeding. Moreover, some studies involving traumatic births have also shown a negative impact on breastfeeding.
To the best of the author's knowledge, no epidemiological research has investigated the effect of the role of mistreatment of women during childbirth in breastfeeding.
Added value of this study
Brazil is one of the largest countries in the world. The great social and income inequality is a characteristic that accompanies our population, influencing the health and disease process. The same happens concerning maternal and child care.
In this context, the “Birth in Brazil” research was established. It was the first large perinatal survey involving 24,000 women from all Brazilian States. The survey was conducted by the Oswaldo Cruz Foundation–one of the leading health research institutes in Latin America.
In Brazil, maternal and child health is marked by the disparity in income, skin color/race, and mainly by the type of hospital where the birth took place, public or private sector. Health professionals normalized obstetric interventions such as scheduled cesarean sections without clinical indication, generating a large cohort of premature and early-term babies.
Concerning mistreatment during childbirth, the “Birth in Brazil” showed that the prevalence of mistreatment was 44%, considering at least one act of physical or psychological violence, disrespect, lack of information, privacy and communication with the health team, inability to ask questions, and loss of autonomy. However, few studies have demonstrated the negative effect of this form of violence on mothers and babies.
In this sense, the research “Birth in Brazil” has contributed by pointing out that mistreatment in childbirth affects women's mental health and takes mothers and babies away from postnatal health care. Moreover, with this publication, we demonstrate, for the first time, that mistreatment also affects negatively breastfeeding, especially in the first days of life.
To achieve these results, data analysis was conducted by Structural Equation Modeling. This approach allows measuring direct, indirect, and, total effects and was fundamental to understanding the effect of mistreatment in breastfeeding after labor and in the long term. Also, the multi-grouping strategy was used to observe the differences between vaginal and C-section births.
Implications of all the available evidence
In Brazil, it is challenging to address mistreatment in childbirth care. One of the reasons is the resistance of health professionals to the subject, commonly called obstetric violence by women. In addition, the Brazilian Ministry of Health also minimizes the occurrence of the event and denies that mistreatment is a reality for many women during the birth of their children.
Thus, this research contributes by giving visibility to the topic and showing that mistreatment in childbirth care has consequences on women and their babies. Thus, we expect the engagement of health professionals and the government to create public policies aimed at mitigating mistreatment in childbirth (or obstetric violence) in Brazilian hospitals. This type of abuse constitutes a serious violation of women's rights, unacceptable.
Introduction
The World Health Organization and the United Nations International Children's Emergency Fund recommend that children initiate breastfeeding within the first hour after birth and be exclusively breastfed for the first six months of life.1 Breastfeeding is a key intervention to prevent health adverse outcomes and improve the health of both the mother and the child. The literature indicates that children who are breastfed for longer periods have lower infectious morbidity and mortality.2 Also, growing evidence suggests that breastfeeding might protect against being overweight and developing diabetes later in life.2 Breastfeeding is also associated with improved human capital 30 years later.3 Regarding mothers, breastfeeding can prevent breast cancer, improve birth spacing, and reduce a woman's risk of diabetes and ovarian cancer.2
Despite the well-known benefits, the prevalence of exclusive breastfeeding is low worldwide. In low- and middle-income countries, when it comes to children younger than six months, 36.3 million (63%) are not exclusively breastfed.2 A Brazilian study analysed data from four national population-based surveys and showed an increase in exclusive breastfeeding from 2.9% in 1986 to 36.6% in 2013,4 and a more recent survey showed an increase to 45.7% in 2019.5 However, despite the advance, the estimative remains below 50%.
The literature highlights the importance of a calm, comfortable, and distress-free environment for successful breastfeeding. Some authors recognise that a traumatic birth can influence the onset and maintenance of breastfeeding.6 Considering victimization by any violence as stressful and, in a way, traumatic7; and using the extensive literature on intimate partner violence and cessation of breastfeeding, we can extrapolate this reasoning to women who become victims of obstetric violence during childbirth.8 Furthermore, it is important to mention that healthcare professionals who assist these women during prenatal, childbirth, and postpartum can influence (positively and negatively) this process.9
In Latin America and Brazil, the term “obstetric violence” is used to characterise acts such as mistreatment, disrespect, abuse, and neglect during pregnancy, childbirth, and puerperium.10 Some researchers have encouraged the utilization of this term over “mistreatment” due to the overlapping acts of gender violence and mistreatment in care that compose the event.10 However, it is important to highlight that there is no consensus in the literature worldwide on the terminology and the definition of this issue.11,12 Therefore, information on the prevalence of such events among postpartum women are difficult to compare.
In a systematic review regarding Latin American countries, 43.0% of women suffered at least one form of obstetric violence during childbirth.13 In Brazil, two large studies investigated the prevalence of this violence considering the last birth. The first, a hospital-based survey, is called “Birth in Brazil”. This nationally representative study involving 24,000 women, estimated that 44% of women reported at least one act of physical or psychological violence, disrespect, lack of information, privacy and communication with the healthcare team, inability to ask questions, and loss of autonomy.14 The second study, a population-based cohort, was carried out in Pelotas (a city located in the Brazilian southern region) with baseline data from 2015. This research involved 4.275 postpartum women and 18.3% of women reported disrespect or abuse during childbirth.15
Despite the high prevalence of obstetric violence during childbirth in Brazil and other countries around the world, few studies explore the consequences of these acts for mother's and newborns' health. Two Brazilian recent studies showed a causal association between obstetric violence during childbirth and an increased likelihood of developing postpartum depression.16,17 Another study showed that abuse during childbirth can reduce and/or delay the use of healthcare services during the postpartum period, both for the woman and the newborn.18
Therefore, the hypothesis to be investigated in this study is whether women who suffered obstetric violence during their childbirth hospitalization have greater difficulty breastfeeding the newborn when compared to women who did not experience any violence. Thus, this study aimed to investigate the causal association between obstetric violence during childbirth hospitalization and breastfeeding. To the best of the authors’ knowledge, no epidemiological research has investigated this phenomenon.
Methods
Brazilian context in childbirth care
In Brazil, according to a National Survey of Demography and Children's and Women's Health conducted in 2006, most women (98.4%) give birth in a hospital, whether public or private.19 The public sector is responsible for 80% of all childbirth.
Some critical context information is the significant difference between public and private assistance. The physician is responsible for prenatal care and labour in the private sector. In such cases, money-saving and comfort can increase the probability of elective C-section. In public hospitals, the staff on duty provides women and baby assistance, and vaginal birth is most frequent.
The duration of a hospital stay may vary from 24 h to 48 h. Women having vaginal birth can be discharged within 24 h, while women who have C-sections wait, at least, 48 h.
Study design
We used data from the study “Birth in Brazil”, a national hospital-based cohort of puerperal women and their newborns, carried out between February 2011 and October 2012.
Study population
All women and newborns (live births or stillbirths) admitted for childbirth in the selected hospitals was considered eligible for “Birth in Brazil”. The following cases were excluded: a) women who gave birth in a location other than a hospital; b) women with their gestational age under 20 weeks or who had a stillbirth baby weighing less than 500 g; c) women with severe mental disorders; d) women who did not understand Portuguese; e) women hospitalized for pregnancy legal termination; and f) deaf and mute women.
For this analysis, we excluded cases of perinatal death (363), twin pregnancies (459), women living with HIV (104), women or newborns staying in ICUs (1.139), and gestational age under 36 weeks (1.608). In all of the abovementioned cases, breastfeeding is or could be unviable. Thus, 3.673 women were excluded.
Sample design
The “Birth in Brazil” study applied a three-stage cluster sampling method, with stratification based on the five macro-regions of the country, the location (capital or non-capital), and the type of hospital (public or private) in which the birth occurred. Hospitals were selected having, in each stratum, a proportional probability based on the number of births per year. In the first stage, we selected hospitals with 500 or more births in 2007. Thus, 272 hospitals from all regions in Brazil participated in the study. In the second stage, we applied inverse transform sampling to select samples based on the number of days required to interview 90 mothers in each hospital (with a minimum of 7 days). The weights were based on the inverse probability of inclusion in the sample. Further information about the sampling process has been previously published.20
Data collection
The first stage of the “Birth in Brazil” study consisted of face-to-face interviews with hospitalized mothers. The interviews were conducted within 24 h after birth. Electronic questionnaires were used to obtain data from the medical records of the women and their newborns. The study conducted then two follow-up telephone interviews to obtain additional information on maternal and neonatal outcomes. The first interview was conducted between 43 and 180 days after birth, and the second one was conducted between 6 and 12 months after birth. Further information on data collection can be found in Leal et al. (2015).21
Theoretical model, variables, and measurement instruments
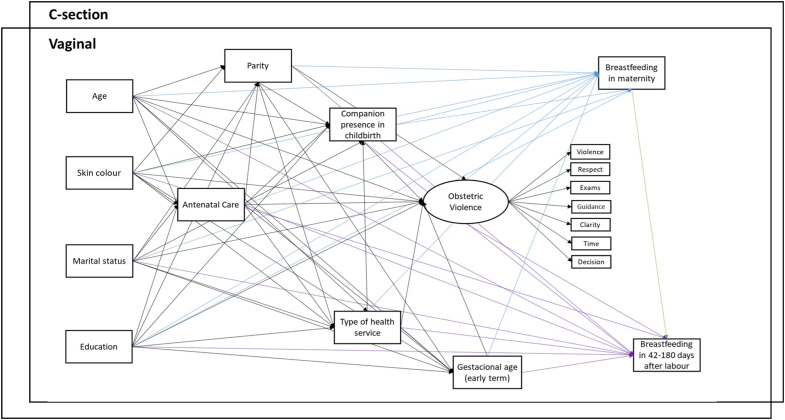
Fig. 1 shows the theoretical model examining the association between obstetric violence during childbirth and breastfeeding. Observed variables are represented by rectangles, while ellipses represent latent variables.
Fig. 1.
The theoretical model was used to test the association between obstetric violence during childbirth and breastfeeding.
The exposure was the occurrence of obstetric violence during childbirth. The outcomes were defined as “Breastfeeding at the maternity”, and “Breastfeeding 43–180 days after birth”. Other variables were confounding factors as they are, according to the literature, associated with exposure and also risk factors for the outcomes.14,22
The theoretical model considered the temporality of the information obtained by the questionnaire. Thus, the socioeconomic variables are visible at the first level. As these characteristics are not likely to change in a short time, we thought it was reasonable to use them as a proxy for the socioeconomic characteristics at the beginning of the pregnancy. Antenatal care quality occupies the second level. The third, fourth and fifth levels consist of birth information, including major exposure. The outcomes are placed in the last levels.
The model postulated that younger women, with black skin colour, who did not live with a partner, with low education levels, low parity, who did not have antenatal care, who did not have a companion during childbirth, and who used a public healthcare system, were more likely to suffer obstetric violence.15,23 Such characteristics are also risk factors for those women who have fewer opportunities to breastfeed their newborns. In addition, the theoretical model also proposed that such associations vary according to the type of birth (C-section and vaginal), due to the influence of the birth type on the breastfeeding initiation.24,25
Obstetric violence during childbirth
As previously mentioned, there is no consensus in the literature on the terminology and definition that best expresses the acts of violence, abuse, disrespect, and neglect against women during childbirth.14 For this reason, we chose to work on obstetric violence as a latent variable. At first, we started with eleven indicators (episiotomy, fundal pressure, presence of a companion, trichotomy, Abuse, Respect, Exams, Guidance, Clarity, Time, and Decision). Nonetheless, the items referring to episiotomy, fundal pressure, presence of a companion, and trichotomy did not have satisfactory factor loadings and were therefore not entered into the latent variable.
Thus, seven items were used to measure Obstetric Violence during childbirth. Information about all these items were collected from mothers by telephone. These mothers were contacted between 43 days and 180 days after birth. In the descriptive analyses, we calculated the sum of all indicators, giving rise to a variable with a score ranging from 0 to 7. After that, a dichotomous was created (No = 0; Yes = 1–7). In the main model, Obstetric Violence was a latent variable. The indicators for this variable were:
Indicator 1 (Abuse): occurrence of verbal/psychological/physical abuse towards hospitalized women. Response options: Yes or No.
Indicator 2 (Respect): respectful treatment to hospitalized women. Response options: very good, good, average, poor, and very poor.
Indicator 3 (Exams): respect for comfort/privacy during intimate physical examinations. Response options: very good, good, average, poor, and very poor.
Indicator 4 (Guidance): level of care received after birth, up until discharge from the hospital. Response options: very good, good, average, poor, and very poor.
Indicator 5 (Clarity): transparency of information provided. Response options: very good, good, average, poor, and very poor.
Indicator 6 (Time): time provided for asking questions. Response options: very good, good, average, poor, and very poor.
Indicator 7 (Decision): the ability to talk to a professional about care. Response options: very good, good, average, poor, and very poor.
To compose the latent variable (in the causal analysis), indicators 2–7 were used in two categories, aggregating very good/good (Yes) and average/poor/very poor (No).
Breastfeeding
We worked with two outcomes: 1) Breastfeeding at the maternity and 2) Breastfeeding 43–180 days after birth. The questions were collected during a first telephone interview conducted 43–180 days after birth. We asked women if the newborn had been discharged from the maternity breastfeeding exclusively (yes/no). Regarding the second outcome, women were asked if the baby had breastfed in the last 24 h (not exclusive) (yes/no). We opted to work with no exclusive breastfeeding due to the great range of days after birth.
Other variables of the model
We identified socioeconomic and demographic variables (women's education, race/ethnicity, age, and marital status) and variables related to childbirth through a structured questionnaire conducted in the hospital after childbirth.
We measured a woman's education as full years of school attendance: a) up to nine years of study, representing complete or incomplete elementary education; b) up to twelve years of study, corresponding to complete or incomplete high school education; and c) thirteen or more years of study, referring to complete or incomplete higher education. Race/ethnicity was self-reported and collected according to the Brazilian Institute of Geography and Statistics (IBGE) parameters: black, light-skinned black, white, Asian, and indigenous and grouping as white and non-white. We divided women's age into 12–19 years old, 20–34 years old, and 35 years old or more. Marital status was divided into two categories: cohabiting with a partner or not cohabiting with a partner. The parity level consisted of three categories: (primiparous, one or two previous births, and three or more births). Gestational age was categorized into the early term (37 0/7–38 6/7 weeks of gestation), and others (above 39 0/7 weeks of gestation).
We assessed antenatal care using the Kotelchuck index, adapted for Brazil, which combines information about the timing of prenatal care initiation (early is considered as the first 16 weeks) and the number of appointments attended by the pregnant woman (a minimum of six appointments: one in the first trimester, two in the second and three in the third). In the descriptive analysis, we used three categories: inadequate, partially adequate, and adequate/more than adequate. In the main analysis, we considered prenatal care as a discrete variable.26
We classified the type of birth as either a vaginal birth (including forceps and vacuum-assisted deliveries) or a C-section.
The presence of a companion was assessed in order to verify whether the woman had a companion during labour and childbirth.
As for the type of healthcare service in which the birth had occurred, we considered women who gave birth in public hospitals as “childbirth public payment”. Women who were covered by health insurances and those who gave birth in private establishments (regardless of whether they were covered by health insurances) were considered as “childbirth private payment”.
Statistical analysis
We performed descriptive and bivariate analyses, considering all births, vaginal and C-sections. To compare frequencies, we implemented a chi-square test. This analysis was performed using the Stata 15.0 (Stata) software.
To account for those lost to follow-up, we analysed the characteristics of the non-responding women. From this data, we assigned different weights to each respondent to compensate for the information loss. We carried out logistic regression to estimate the probability of each baseline woman who participated by answering the telephone interview, using a set of variables to differentiate between respondents and non-respondents. A non-response adjustment factor was defined to compensate for the tendency of women's specific characteristics. Based on the non-response adjustment factor, we calculated specific sampling weights for the telephone interviews analysis. The rationale for applying non-response weights is the assumption that non-respondents would have provided similar answers for each stratum and adjustment category, meaning that a higher weight in the analysis is assigned to women who answer the phone contact and have the same profile as those who were lost to follow-up. Further information on the calibration process has been previously described.27,28
After applying the calibration process described above, we performed the analysis using structural equation models with Mplus 8.0. Obstetric Violence constituted a continuous latent variable. We considered a factor loading greater than 0.5, with a p-value of less than 0.05, indicative of a good correlation between the observed variable and the construct of interest.29
According to the literature, women who had vaginal birth have a higher probability of breastfeeding the newborn. Therefore, we carried out multigroup modelling to assess the association between Obstetric Violence and breastfeeding, considering the singularities of C-sections and vaginal births.
We performed weighted least squares mean and variance adjusted (WLSMV) estimation and theta parameterization. Considering the loss of information in some variables, we implemented the full information method, in which missing values were imputed.
We calculated the modification indices, using the MODINDICES command, to obtain suggestions for changes to our initial hypotheses. We developed a new model when the proposed modifications (modification rates greater than 10) were considered plausible from a theoretical standpoint. In all analyses, a path was considered significant when the p-value was less than or equal to 0.05.29
We used the Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), and Tucker–Lewis Index (TLI) to evaluate model fit. The RMSEA compensates for the effect of a model's complexity by estimating the adjustment considering the number of parameters involved (the degrees of freedom). Values less than 0.06 indicate a good fit. We considered confidence limits greater than 90% of the RMSEA and below 0.08 as a good fit. Incremental adjustment index values (the CFI and TLI) above 0.95 indicated adequate model fit.30,31 Both the CFI and the RMSEA are sensitive to the lack of model specification and are affected only slightly by sample size.29
Ethics
The “Birth in Brazil” study was approved by a Research Ethics Committee recognized by the Brazilian Ministry of Health and the Brazilian National Research Ethics Committee (CONEP), under CAAE number 0096.0.031.000-10.
Role of the funding source
The funders had no role in the study design, data collection, data analysis, interpretation, or report writing.
Results
The data analysis was conducted with 20.527 women (85.5% of the total sample). Of these, 11.752 (57.2%) had a C-section, and 8.775 (42.8%) had a vaginal birth. Considering the follow-up, 13,879 women were recovered (67% of all sample).
Table 1 shows the descriptive analysis of the study population and type of birth. Considering the total study population, we can observe that the majority were 20–34 years old, light-skinned black, had until 9 schooling years, and were married or were living together with a companion. Also, a great part of our sample had their childbirth in the public sector, considered their antenatal care adequate or more than adequate, and had the right to have a companion during childbirth. Babies were early terms in almost 40% of our sample. Considering the exposure, the seven indicators which compose the obstetric violence construct vary from 5.7% (abuse) to 18.6% (time) considering the negative response and 41.1% of women reported some form of violence (combined). About the outcome, 93.4% of women were breastfeeding exclusively when they were discharged from maternity, and 43–180 days after birth, 87.4% of women reported to be still breastfeeding the baby (exclusively or not).
Table 1.
Descriptive characteristics of women by vaginal births and C-section.
| Total (n = 20.527) |
Vaginal (n = 8.775) |
C-section (n = 11.752) |
p-valuea | |
|---|---|---|---|---|
| % (CI 95%) | % (CI 95%) | % (CI 95%) | ||
| Baseline characteristics | ||||
| Woman's age (n = 20.525) | ||||
| 12–19 years | 19.2 (18.3–20.1) | 24.6 (23.8–25.9) | 14.5 (13.5–15.4) | <0.001 |
| 20–34 years | 70.7 (69.7–71.5) | 68.3 (67.0–69.5) | 72.7 (71.6–73.8) | |
| 35 or more years | 10.1 (9.5–10.8) | 7.1 (6.4–7.9) | 12.8 (11.8–13.8) | |
| Woman's ethnicity (n = 20.524) | ||||
| Brown | 57.9 (56.1–59.5) | 63.1 (61.0–35.1) | 53.3 (51.1–55.3) | <0.001 |
| White | 32.3 (30.5–34.1) | 25.6 (23.5–27.7) | 38.3 (36.0–40.5) | |
| Black | 8.3 (7.4–9.3) | 9.6 (8.4–11.0) | 7.1 (6.2–8.6) | |
| Indigenous/Asian | 1.5 (1.2–1.8) | 1.7 (1.2–2.1) | 1.3 (1.0–1.7) | |
| Woman's education (n = 20.435) | ||||
| Until 9 years | 45.3 (43.8–46.8) | 57.4 (55.5–59.1) | 34.7 (32.9–36.4) | <0.001 |
| 10–12 years | 41.8 (40.5–43.1) | 38.1 (36.5–39.8) | 45.1 (43.4–46.7) | |
| More than 13 years | 12.9 (11.7–13.9) | 4.5 (3.8–5.1) | 20.2 (18.4–22.1) | |
| Marital status (n = 20.516) | ||||
| Marriage or living together | 81.8 (81.0–82.6) | 79.3 (78.0–80.4) | 84.1 (83.1–85.0) | <0.001 |
| Do not cohabit with a companion | 18.2 (17.3–18.9) | 20.7 (19.5–21.9) | 15.9 (14.9–16.8) | |
| Antenatal care (n = 20.008) | ||||
| Inadequate | 15.4 (14.4–16.3) | 20.9 (19.3–22.3) | 10.4 (9.6–11.4) | <0.001 |
| Partial adequate | 18.3 (17.5–19.2) | 20.9 (19.8–22.2) | 16.2 (14.9–17.2) | |
| Adequate/more than adequate | 66.3 (64.9–67.5) | 58.2 (56.2–60.0) | 73.4 (71.8–74.9) | |
| Parity (n = 20.526) | ||||
| Primiparous | 46.7 (45.5–47.8) | 41.9 (40.2–43.6) | 50.8 (49.4–52.3) | <0.001 |
| 1 or 2 previous births | 43.4 (42.3–44.4) | 44.1 (42.3–45.7) | 42.8 (41.5–44.0) | |
| 3 or more previous births | 9.9 (9.2–10.7) | 14.0 (12.7–15.4) | 6.4 (5.7–7.0) | |
| Presence of companion during childbirth (n = 20.517) | ||||
| Yes | 75.6 (72.0–78.8) | 67.9 (63.2–72.2) | 82.4 (79.3–85.0) | <0.001 |
| No | 24.4 (21.2–27.9) | 32.1 (27.0–36.7) | 17.6 (14.9–20.6) | |
| Type of health service (n = 20.527) | ||||
| Public | 80.1 (78.4–81.5) | 95.1 (93.2–96.3) | 66.8 (64.5–69.0) | <0.001 |
| Private | 19.9 (18.4–21.5) | 4.9 (3.6–6.8) | 33.2 (30.9–35.4) | |
| Gestational age (n = 20.521) | ||||
| Early term | 39.2 (37.7–40.5) | 35.4 (33.6–37.3) | 42.3 (40.6–44.0) | <0.001 |
| Others (full term and postterm) | 60.8 (59.4–62.2) | 64.6 (62.6–66.3) | 57.7 (55.9–59.3) | |
| Exposure | ||||
| Abuse (n = 14.722) | ||||
| Yes | 5.7 (5.0–6.4) | 6,3 (5.3–7.3) | 5.3 (4.4–6.1) | 0.056 |
| No | 94.3 (93.5–94.6) | 93.7 (92.6–94.6) | 94.7 (93.9–95.5) | |
| Respect (n = 14.765) | ||||
| Yes | 85.8 (84.6–86.8) | 83.7 (81.8–85.3) | 87.6 (86.4–88.7) | <0.001 |
| No | 14.2 (13.4–15.3) | 16.3 (14.6–18.3) | 12.4 (11.3–13.5) | |
| Exams (n = 14.725) | ||||
| Yes | 88.1 (87.1–88.4) | 85.9 (84.2–87.5) | 89.9 (88.9–90.8) | <0.001 |
| No | 11.9 (11.0–12.8) | 14.1 (12.5–15.8) | 10.1 (9.2–11.0) | |
| Guidance (n = 14.768) | ||||
| Yes | 86.9 (85.9–87.9) | 86.3 (84.7–87.7) | 87.5 (86.3–88.6) | 0.132 |
| No | 13.1 (12.0–14.0) | 13.7 (12.3–15.3) | 12.5 (11.3–13.6) | |
| Clarity (n = 14.796) | ||||
| Yes | 82.6 (81.3–83.6) | 81.4 (79.7–83.0) | 83.5 (82.1–84.7) | 0.027 |
| No | 17.4 (16.3–18.6) | 18.6 (16.9–20.2) | 16.5 (15.2–17.8) | |
| Time (n = 14.822) | ||||
| Yes | 81.4 (80.1–82.4) | 78.7 (77.0–80.3) | 83.5 (82.2–84.7) | <0.001 |
| No | 18.6 (17.5–19.8) | 21.3 (19.6–22.9) | 16.5 (15.2–17.7) | |
| Decision (n = 14.753) | ||||
| Yes | 82.8 (81.8–83.8) | 80.6 (78.9–82.2) | 84.7 (83.6–85.8) | <0.001 |
| No | 17.2 (16.1–18.1) | 19.4 (17.8–21.0) | 15.3 (14.1–16.3) | |
| Obstetric violence (n = 13.879) | ||||
| Yes | 41.1 (39.3–42.7) | 45.3 (42.8–47.6) | 37.5 (35.7–39.3) | <0.001 |
| No | 58.9 (57.2–30.6) | 54.7 (52.3–57.1) | 62.5 (60.6–64.2) | |
| Outcomes | ||||
| Breastfeeding in maternity (n = 13.845) | ||||
| Yes | 93.4 (92.4–94.1) | 96.2 (95.1–97.0) | 90.8 (89.5–92.0) | <0.001 |
| No | 6.6 (8.8–7.5) | 3.8 (2.9–4.8) | 9.2 (7.9–10.4) | |
| Breastfeeding 43–180 days (n = 13.845) | ||||
| Yes | 87.4 (86.3–88.3) | 89.2 (87.6–60.5) | 85.8 (84.7–86.9) | <0.001 |
| No | 12.6 (11.6–13.6) | 10.8 (9.4–12.3) | 14.2 (13.0–15.3) | |
Values in bold are statistically significant (>0.05).
Regarding all characteristics described above, differences were observed between women who have vaginal birth and women who have a C-section (excepted for Guidance and Abuse). Women who had vaginal births were younger, there was a greater proportion of light-skinned black women, and women who did not live together with a companion, were less educated and had a greater parity. Still, concerning the higher proportion of women not entitled to the right of having a companion during childbirth, the birth was conducted in a public healthcare unit in most of the cases, and they received a less quality antenatal care when compared to women who had a C-section. The prevalence of early-term deliveries was higher in C-section women. Considering Obstetric Violence, 45.3% of women who had vaginal births have suffered at least one form of Obstetric Violence versus 37.5% of women who have a C-section. As expected, the breastfeeding outcomes were better in women with vaginal births.
Table 2 shows the main results. The model has a good adjustment with RMSEA equals to 0.008, with CFI and TLI to 0.982 and 0.969, respectively.
Table 2.
Standardized coefficients, standard error, and p-value of the direct and indirect effect of the Obstetric Violence in childbirth on breastfeeding “Birth in Brazil”.
| Model adjustment | RMSEA |
0.008 (0.006–0.010) |
||||
|---|---|---|---|---|---|---|
| CFI |
0.982 |
|||||
| TLI |
0.969 |
|||||
| Total sample |
Total N: 20.362a |
|||||
| Vaginal (N = 8.734) |
C-section (N = 11.628) |
|||||
| Standardized coefficient (95% CI) | Standard error | p-value | Standardized coefficient (95% CI) | Standard error | p-valueb | |
| Latent variable | ||||||
| Obstetric violence | ||||||
| Violence | 0.625 (0.560; 0.691) | 0.040 | <0.001 | 0.648 (0.609; 0.687) | 0.024 | <0.001 |
| Respect | 0.767 (0.738; 0.795) | 0.017 | <0.001 | 0.762 (0.736; 0.789) | 0.016 | <0.001 |
| Exams | 0.729 (0.686; 0.771) | 0.026 | <0.001 | 0.768 (0.742; 0.794) | 0.016 | <0.001 |
| Guidance | 0.746 (0.726; 0.766) | 0.012 | <0.001 | 0.728 (0.701; 0.754) | 0.016 | <0.001 |
| Clarity | 0.787 (0.753; 0.821) | 0.021 | <0.001 | 0.849 (0.828; 0.470) | 0.013 | <0.001 |
| Time | 0.726 (0.677; 0.776) | 0.030 | <0.001 | 0.764 (0.727; 0.801) | 0.023 | <0.001 |
| Decision | 0.732 (0.699; 0.765) | 0.020 | <0.001 | 0.746 (0.719; 0.746) | 0.016 | <0.001 |
| Direct effect of the obstetric violence in childbirth on breastfeeding | ||||||
| Breastfeeding 42–180 days after birth | ||||||
| Obstetric violence | −0.058 (−0.113; −0.003) | 0.034 | 0.084 | 0.019 (−0.048; 0.086) | 0.041 | 0.639 |
| Breastfeeding in maternity | 0.500 (0.370; 0.630) | 0.079 | <0.001 | 0.519 (0.464; 0.574) | 0.033 | <0.001 |
| Gestational age | 0.048 (−0.10; 0.106) | 0.035 | 0.174 | 0.063 (0.012; 0.115) | 0.031 | 0.044 |
| Presence of companion | 0.063 (−0.065; 0.190) | 0.078 | 0.421 | 0.054 (−0.021; 0.129) | 0.046 | 0.236 |
| Type of health service (public) | −0.050 (−0.230; 0.129) | 0.109 | 0.643 | −0.060 (−0.169; 0.049) | 0.066 | 0.364 |
| Parity | −0.065 (−0.187; 0.057) | 0.074 | 0.383 | −0.058 (−0.125; 0.008) | 0.040 | 0.148 |
| Antenatal care | −0.055 (−0.128; 0.018) | 0.044 | 0.214 | 0.008 (−0.061; 0.077) | 0.042 | 0.849 |
| Skin color/ethnicity (white) | −0.008 (−0.071; 0.056) | 0.039 | 0.840 | −0.070 (−0.116; −0.025) | 0.028 | 0.011 |
| Age | 0.084 (−0.028; 0.187) | 0.068 | 0.217 | 0.046 (0.002; 0.090) | 0.027 | 0.088 |
| Marital status (marriage or living together) | 0.029 (−0.012; −0.070) | 0.025 | 0.252 | 0.036 (0.000; 0.072) | 0.022 | 0.096 |
| Education | 0.025 (−0.109; 0.159) | 0.081 | 0.755 | 0.041 (0.006; 0.041) | 0.029 | 0.149 |
| Breastfeeding in maternity | ||||||
| Obstetric violence | −0.267 (−0.346; −0.188) | 0.048 | <0.001 | −0.105 (−0.157; −0.054) | 0.031 | 0.001 |
| Gestational age | −0.009 (−0.095; 0.076) | 0.052 | 0.857 | −0.115 (−0.176; −0.055) | 0.037 | 0.002 |
| Presence of companion | 0.054 (−0.072; 0.054) | 0.076 | 0.481 | 0.098 (−0.033; 0.229) | 0.079 | 0.217 |
| Type of health service (public) | −0.356 (−0.570; −0.143) | 0.130 | 0.006 | −0.145 (−0.317; 0.027) | 0.105 | 0.166 |
| Parity | 0.434 (0.331; 0.537) | 0.063 | <0.001 | 0.201 (0.119; 0.283) | 0.050 | <0.001 |
| Antenatal care | 0.088 (−0.042; 0.218) | 0.079 | 0.266 | −0.030 (−0.086; 0.025) | 0.034 | 0.367 |
| Skin colour/ethnicity (white) | −0.025 (−0.112; 0.061) | 0.052 | 0.626 | −0.018 (−0.065; 0.029) | 0.028 | 0.524 |
| Age | −0.276 (−0.419; −0.134) | 0.087 | 0.001 | −0.172 (−0.224; −0.119) | 0.032 | <0.001 |
| Marital status (marriage or living together) | 0.050 (−0.041; 0.142) | 0.056 | 0.365 | 0.047 (−0.011; 0.105) | 0.035 | 0.187 |
| Education | 0.304 (0.174; 0.435) | 0.079 | <0.000 | 0.029 (−0.021; 0.080) | 0.031 | 0.342 |
| Obstetric violence | ||||||
| Presence of companion (yes) | −0.073 (−0.143; −0.003) | 0.042 | 0.086 | −0.084 (−0.133; −0.034) | 0.030 | 0.005 |
| Type of health service (public) | −0.232 (−0.330; −0.135) | 0.059 | <0.001 | −0.422 (−0.489; −0.355) | 0.041 | <0.001 |
| Parity | −0.077 (−0.147; −0.006) | 0.043 | 0.074 | −0.154 (−0.198; −0.109) | 0.027 | <0.001 |
| Antenatal care | −0.112 (−0.173; −0.050) | 0.037 | 0.003 | −0.064 (−0.112; −0.015) | 0.029 | 0.030 |
| Skin colour/ethnicity (white) | −0.026 (−0.080; 0.028) | 0.033 | 0.422 | −0.035 (−0.076; 0.006) | 0.025 | 0.161 |
| Age | 0.033 (−0.018; −0.083) | 0.031 | 0.287 | −0.007 (−0.043; 0.029) | 0.025 | 0.161 |
| Marital status (marriage or living together) | 0.043 (0.006; 0.080) | 0.022 | 0.054 | 0.036 (0.000; 0.071) | 0.022 | 0.100 |
| Education | 0.116 (0.044; 0.188) | 0.044 | 0.008 | 0.217 (0.192; 0.241) | 0.015 | <0.001 |
| Gestational age | ||||||
| Type of health service | 0.007 (−0.092; 0.106) | 0.060 | 0.907 | 0.371 (0.290; 0.452) | 0.049 | <0.001 |
| Parity | 0.013 (−0.025; −0.051) | 0.023 | 0.584 | 0.076 (0.021; 0.131) | 0.034 | 0.023 |
| Antenatal care | −0.111 (−0.170; −0.051) | 0.036 | 0.002 | −0.059 (−0.102; −0.015) | 0.027 | 0.028 |
| Skin color/ethnicity (white) | −0.006 (0.038; 0.025) | 0.019 | 0.742 | 0.016 (−0.013; 0.045) | 0.018 | 0.375 |
| Age | −0.011 (−0.056; 0.035) | 0.028 | −0.384 | 0.016 (−0.023; 0.054) | 0.023 | 0.502 |
| Marital status (marriage or living together) | 0.017 (−0.007; 0.040) | 0.014 | 0.238 | 0.002 (−0.024; 0.029) | 0.016 | 0.884 |
| Education | −0.017 (−0.070; 0.035) | 0.032 | 0.587 | −0.135 (−0.190; −0.079) | 0.034 | <0.001 |
| Presence of companion | ||||||
| Parity | −0.122 (−0.189; −0.056) | 0.040 | 0.002 | −0.054 (−0.103; −0.004) | 0.030 | 0.074 |
| Type of health service | 0.402 (0.301; 0.504) | 0.062 | <0.001 | 0.545 (0.409; 0.681) | 0.083 | <0.001 |
| Antenatal care | 0.066 (0.010; 0.122) | 0.034 | 0.053 | −0.020 (−0.081; 0.042) | 0.037 | 0.595 |
| Skin color/ethnicity (white) | 0.028 (−0.017; 0.028) | 0.027 | 0.303 | −0.016 (−0.072; 0.040) | 0.034 | 0.633 |
| Age | −0.070 (−0.131; −0.009) | 0.037 | 0.060 | −0.034 (−0.066; −0.002) | 0.019 | 0.082 |
| Marital status (marriage or living together) | −0.039 (−0.092; 0.013) | 0.032 | 0.219 | 0.008 (−0.033; 0.048) | 0.025 | 0.755 |
| Education | −0.132 (−0.197; −0.066) | 0.040 | 0.001 | −0.069 (−0.141; 0.003) | 0.044 | 0.117 |
| Type of hospital | ||||||
| Parity | −0.017 (−0.090; 0.057) | 0.045 | 0.708 | −0.074 (−0.074; 0.030) | 0.022 | 0.001 |
| Antenatal care | −0.010 (−0.105; 0.085) | 0.058 | 0.861 | 0.126 (0.079; 0.172) | 0.028 | <0.001 |
| Skin color/ethnicity (white) | 0.124 (0.059; 0.189) | 0.040 | 0.002 | 0.117 (0.058; 0.175) | 0.035 | 0.001 |
| Age | 0.072 (0.009; 0.134) | 0.038 | 0.059 | 0.149 (0.119; 0.179) | 0.018 | <0.001 |
| Marital status (marriage or living together) | 0.097 (0.021; 0.174) | 0.047 | 0.037 | 0.033 (−0.004; 0.070) | 0.023 | 0.146 |
| Education | 0.421 (0.342; 0.499) | 0.048 | <0.001 | 0.509 (0.474; 0.543) | 0.021 | <0.001 |
| Parity | ||||||
| Antenatal care | −0.204 (−0.230; −0.179) | 0.015 | <0.001 | −0.177 (−0.203; −0.151) | 0.016 | <0.001 |
| Skin color/ethnicity (white) | 0.032 (0.003; 0.061) | 0.018 | 0.072 | −0.027 (−0.057; 0.002) | 0.018 | 0.130 |
| Age | 0.553 (0.531; 0.575) | 0.013 | <0.001 | 0.447 (0.418; 0.476) | 0.018 | <0.001 |
| Marital status (marriage or living together) | 0.100 (0.079; 0.122) | 0.013 | <0.001 | 0.095 (0.073; 0.116) | 0.013 | <0.001 |
| Education | −0.314 (−0.343; −0.285) | 0.018 | <0.001 | −0.323 (−0.349; −0.297) | 0.016 | <0.001 |
| Antenatal care | ||||||
| Skin color/ethnicity (white) | 0.088 (0.050; 0.127) | 0.023 | <0.001 | 0.059 (0.030; 0.089) | 0.018 | 0.001 |
| Age | 0.060 (0.039; 0.060) | 0.013 | <0.001 | 0.108 (0.090; 0.127) | 0.011 | <0.001 |
| Marital status (marriage or living together) | 0.141 (0.016; 0.166) | 0.015 | <0.001 | 0.099 (0.080; 0.118) | 0.012 | <0.001 |
| Education | 0.246 (0.223; 0.270) | 0.015 | <0.001 | 0.254 (0.211; 0.297) | 0.026 | <0.001 |
| Indirect effect of the obstetric violence in childbirth on breastfeeding | ||||||
| Obstetric violence → Breastfeeding in Maternity → Breastfeeding 43–180 days after birth | −0.134 (−0.197; −0.070) | 0.039 | 0.001 | −0.055 (−0.083; −0.026) | 0.018 | 0.002 |
| Total Effect (direct + indirect effect) of the obstetric violence in childbirth on breastfeeding | ||||||
| Obstetric violence → Breastfeeding in Maternity → Breastfeeding 43–180 days after birth | −0.192 (−0.248; −0.136) | 0.034 | <0.001 | −0.036 (−0.097; 0.026) | 0.037 | 0.342 |
RMSEA: Root mean square error of approximation; CFI: Comparative fit index; TLI: Tucker–lewis index.
The analysis missing 115 information due to a lack of information.
Values in bold are statistically significant (>0.05).
It is possible to observe that women who leave maternity breastfeeding exclusively have a −0.267 average score in obstetric violence (direct effect–vaginal). This effect happens regardless of the type of birth. However, for women with C-sections, Obstetric Violence had a weaker impact on breastfeeding (C-section = −0.105). Obstetric Violence is shown to have no direct effect on breastfeeding 43–180 days after birth.
Also in Table 2, it is possible to observe that Obstetric Violence has a moderate indirect effect on breastfeeding 43–180 days after birth through breastfeeding at the maternity. This fact can be seen in vaginal and C-section births, being stronger in the first one (vaginal = −0.134 versus C-section = −0.055). When we observe the whole effect (effect direct + effect indirect), we can see that the effect of Obstetric Violence is only significant for women having vaginal birth (vaginal = −0.192 versus C-section = −0.036). It means that Obstetric Violence affects breastfeeding 43–180 days after birth through mediation of breastfeeding at the maternity, and this situation happened only in vaginal births. Supplementary Figs. S1 and S2 (vaginal and C-section) in the Supplementary file also show these relationships.
Discussion
Obstetric violence during childbirth may decrease the probability for women to leave the maternity ward breastfeeding exclusively, having a stronger effect on women who have vaginal birth. Also, only women who had vaginal birth and were exposed to Obstetric Violence during childbirth had breastfeeding indirectly affected 43–180 days after birth. Direct and indirect effects persisted after adjustment for women's gestational age, type of healthcare service, the presence of a companion during childbirth, parity, antenatal care, age, race/ethnicity, marital status, and education.
An interesting finding in our study is that the effect of Obstetric Violence on breastfeeding at the maternity was stronger in women who having vaginal birth. It could suggest that vaginal births is not enough to overlay the Obstetric Violence effect.32 A hypothesis to explain this finding is that women who have vaginal birth suffer more severe forms of Obstetric Violence than women having C-sections.15,16 Thus, the distress and potential trauma could be higher, decreasing the probability of earlier breastfeeding initiation.
Another important point to be discussed is the indirect effect that Obstetric Violence causes on long-term breastfeeding. This effect is almost entirely mediated by breastfeeding at the maternity. This shows that most women who do not initiate breastfeeding in the first days have a greater risk of not breastfeeding later. Thus, establishing breastfeeding at the maternity is essential to maintain breastfeeding in the upcoming months.33
The importance of the healthcare professional to breastfeeding support and management is acknowledged especially during the first hours of a baby's life.9 Vieira and collaborators34 emphasize the importance of such support to mothers who have gone through situations where milk provision may be delayed, such as caesarean delivery and prematurity.34 When the healthcare professional, who is supposed to offer support and help to this woman, is the cause of distress by means of Obstetric Violence, all breastfeeding-related processes could be impacted. Due to the lack of studies focusing on the relationship between Obstetric Violence during childbirth and breastfeeding, we sought support in the related literature in order to understand the plausibility of this relationship and its possible mechanisms.
Studies about the relationship between Obstetric Violence and breastfeeding are non-existent. In an attempt to understand the impact of experiencing a stressful event, such as violence, on breastfeeding, we resorted to the literature on intimate partner violence (IPV) and breastfeeding. Some studies have pointed out that women who suffer IPV during pregnancy have lower probability of intending to breastfeed, initiating breastfeeding, have a shorter duration of breastfeeding, and, finally, a greater risk of early interruption of exclusive breastfeeding.8
Despite recognizing that IPV and Obstetric Violence are two distinct forms of violence against women, it is known that the experience of any violent episode can trigger a series of hormonal and behavioural changes that can influence the practice of breastfeeding, providing some possible explanatory mechanisms. The first mechanism is related to distress and milk production. The literature has long shown that distress reduces or inhibits oxytocin production, leading to a delay in milk production.35 Note that some forms of obstetric violence may happen in a critical moment like labour, and this may cause irreversible changes to the entire physiology that a woman's body require to breastfeed within the first hours after birth. Presuming that experiencing an episode of Obstetric Violence is a stressful situation, it could cause a delay in the milk production. Another possibility is that women exposed to violence could have an increased risk of developing depression and other mental disorders.36 This condition increase the risk to inadequate food practices.37 Finally, mental disorders could increase women's risk of using drugs and alcohol.37,38 This situation may lead women into breastfeeding discontinuation since the practice is unsafe for the baby. Although these three possible mechanisms have been presented, the literature on the matter still needs further exploration.
As far as we know, no epidemiological research has studied the consequences of Obstetric Violence for breastfeeding as its major objective. We identified only one research about factors related to healthcare services that could determine breastfeeding within 1 h of birth. This study did not find an association between physical/verbal violence and neglect at childbirth with breastfeeding.39 However, this study enrolled only women in immunization services. Knowing that women victims of obstetric violence attend postnatal visits less often, there may have been an important selection bias that justifies the non-association.18
It is important to address the limitations of this study. Firstly, the importance of lost to follow-up percentual. High rates of such loss could introduce bias when measuring the occurrence in causal analysis. However, sampling weights calibration was conducted to minimize the possible bias. Secondly, it was not possible to incorporate postpartum depression (mediator) in the theoretical model. Only the second phone call could assess perinatal mental health. Thus, it broke the causal temporality of the events. Finally, unmeasured variables could be part of the causal pathways, such as the presence of a birth assistant (doula), whether the hospital participates in the “Baby friendly initiative”,40 and breastfeeding social support.
The biggest strength of our study is its originality. As far as we know, it is the first study evaluating the causal association between obstetric violence and breastfeeding. It can be a starting point for the discussion of a novel relevant topic in reproductive, maternal, and child health, aligned with the Sustainable Development Objectives related to healthcare quality and gender inequality. Using structural equation modelling analysis allowed us to explore the direct and indirect path connecting Obstetric Violence and breastfeeding. In addition, our study includes a large national hospital based in Brazil. Finally, the results could be generalized to other populations in which the context of childbirth care is similar.
Concluding, Obstetric Violence during childbirth has adverse effects on breastfeeding at the maternity ward regardless of the type of birth, and may continue to negatively influence breastfeeding 43–180 days postpartum in women who have had a vaginal birth. Understanding Obstetric Violence during childbirth as a risk factor for breastfeeding discontinuation is relevant so interventions and public policies can be proposed in order to mitigate Obstetric Violence, and provide a better understanding of the context that may lead a woman into discontinuing breastfeeding.
Contributors
THL – Conceptualization, Data curation, Formal analysis, Writing - original draft; Writing - review & editing; ESM – Conceptualization, Formal analysis, Writing - original draft, Writing - review & editing; MAM – Conceptualization, Writing - original draft; Writing - review & editing; MFS – Conceptualization, Writing - original draft, Writing - review & editing; MCL – Conceptualization, Funding acquisition, Methodology; Project administration; Writing - review & editing and Supervision.
Data sharing statement
The data could be shared upon request, please contact the correspondence author.
Declaration of interests
Authors declare no competing interests.
Acknowledgments
This research was funded by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES); Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ); Departamento de Ciência e Tecnologia (DeCiT); Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (Faperj); Oswaldo Cruz Foundation (INOVA-ENSP).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100438.
Appendix A. Supplementary data
References
- 1.World Health Organization Breastfeeding. 2022. https://www.who.int/health-topics/breastfeeding#tab=tab_1
- 2.Victora C.G., Bahl R., Barros A.J.D., et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387:475–490. doi: 10.1016/S0140-6736(15)01024-7. [DOI] [PubMed] [Google Scholar]
- 3.Victora C.G., Horta B.L., de Mola C.L., et al. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. Lancet Glob Health. 2015;3(4):e199–e205. doi: 10.1016/S2214-109X(15)70002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boccolini C.S., Boccolini P. de MM., Monteiro F.R., Venâncio S.I., Giugliani E.R.J. Breastfeeding indicators trends in Brazil for three decades. Rev Saude Publica. 2017;51:108. doi: 10.11606/S1518-8787.2017051000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kac G., Anjos L.A.D., Lacerda E.M.A., et al. 2019. Estudo nacional de alimentação e nutrição infantil: resultados preliminares de indicadores de aleitamento materno no Brasil. [Google Scholar]
- 6.Banyard V.L., Edwards V.J., Kendall-Tackett K. Trauma and physical health: understanding the effects of extreme stress and of psychological harm. 2009. The impact of traumatic childbirth on health through the undermining of breastfeeding | request PDF; pp. 65–90.https://www.researchgate.net/publication/272507311_The_impact_of_traumatic_childbirth_on_health_through_the_undermining_of_breastfeeding [Google Scholar]
- 7.Ribeiro W.S., Andreoli S.B., Ferri C.P., Prince M., Mari J.D.J. Exposure to violence and mental health problems in low and middle-income countries: a literature review. Braz J Psychiatry. 2009;31(Suppl. 2):S49–S57. doi: 10.1590/S1516-44462009000600003. [DOI] [PubMed] [Google Scholar]
- 8.Normann A.K., Bakiewicz A., Kjerulff Madsen F., Khan K.S., Rasch V., Linde D.S. Intimate partner violence and breastfeeding: a systematic review. BMJ Open. 2020;10(10):e034153. doi: 10.1136/BMJOPEN-2019-034153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silva L.A.T., Fonseca V.M., Oliveira M.I.C., Silva K.S.D., Ramos E.G., Gama S.G.N.D. Professional who attended childbirth and breastfeeding in the first hour of life. Rev Bras Enferm. 2020;73(2):e20180448. doi: 10.1590/0034-7167-2018-0448. [DOI] [PubMed] [Google Scholar]
- 10.Amorim M.M., da Silva Bastos M.H., Katz L. Mistreatment during childbirth. Lancet. 2020;396(10254):816. doi: 10.1016/S0140-6736(20)31563-4. [DOI] [PubMed] [Google Scholar]
- 11.Savage V., Castro A. Measuring mistreatment of women during childbirth: a review of terminology and methodological approaches. Reprod Health. 2017;14(1):1–27. doi: 10.1186/s12978-017-0403-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leite T.H., Marques E.S., Esteves-Pereira A.P., Portela Y., Do Carmo Leal M. Ciência e saúde coletiva; 2020. Desrespeitos e abusos, maus tratos e violência obstétrica: um desafio para epidemiologia e para a saúde pública no Brasil. [DOI] [PubMed] [Google Scholar]
- 13.Tobasía-Hege C., Pinart M., Madeira S., et al. Disrespect and abuse during childbirth and abortion in Latin America: systematic review and meta-analysis. Rev Panam Salud Publica. 2019;43:e36. doi: 10.26633/RPSP.2019.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leite T.H., Pereira A.P.E., Leal M.D.C., Silva A.A.M. 2019. Disrespect and abuse of women during birth and postpartum depression: findings from a national survey on childbirth in Brazil. [DOI] [PubMed] [Google Scholar]
- 15.Mesenburg M.A., Victora C.G., Jacob Serruya S., et al. Disrespect and abuse of women during the process of childbirth in the 2015 Pelotas birth cohort. Reprod Health. 2018;15(1):1–8. doi: 10.1186/s12978-018-0495-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leite T.H., Pereira A.P.E., Leal M.D.C., Silva A.A.M. Disrespect and abuse towards women during childbirth and postpartum depression: findings from birth in Brazil study. J Affect Disord. 2020;273:391–401. doi: 10.1016/j.jad.2020.04.052. [DOI] [PubMed] [Google Scholar]
- 17.Silveira M.F., Mesenburg M.A., Bertoldi A.D., et al. The association between disrespect and abuse of women during childbirth and postpartum depression: findings from the 2015 Pelotas birth cohort study. J Affect Disord. 2019;256(April):441–447. doi: 10.1016/j.jad.2019.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leite T.H., Gomes T., Marques E.S., et al. Association between mistreatment of women during childbirth and postnatal maternal and child health care: findings from “Birth in Brazil”. Women Birth. 2021;35:e28. doi: 10.1016/j.wombi.2021.02.006. [DOI] [PubMed] [Google Scholar]
- 19.Ministério da Saúde, Centro Brasileiro de Análise e Planejamento B . 2009. Pesquisa Nacional de Demografia e Saúde Da Criança e Da Mulher – PNDS 2006: dimensões Do Processo Reprodutivo e Da Saúde Da Criança.https://bvsms.saude.gov.br/bvs/publicacoes/pnds_crianca_mulher.pdf Brasília, DF. [Google Scholar]
- 20.Vasconcellos M.T., Silva P.L., Pereira A.P., Schilithz A.O., Souza Junior P.R., Szwarcwald C.L. Sampling design for the birth in Brazil: national survey into labor and birth. Cad Saude Publica. 2014;30(Suppl 1):S1–S10. doi: 10.1590/0102-311x00176013. http://www.ncbi.nlm.nih.gov/pubmed/25167189 [DOI] [PubMed] [Google Scholar]
- 21.Leal C., Augusto A., Augusto M., et al. Birth in Brazil: national survey into labor and birth. Reprod Health. 2012;9:1–8. doi: 10.1186/1742-4755-9-15. http://www.reproductive-health-journal.com.libproxy.lib.unc.edu/content/pdf/1742-4755-9-15.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amaral SA do, Bielemann R.M., Del-Ponte B., et al. Intenção de amamentar, duração do aleitamento materno e motivos para o desmame: um estudo de coorte, Pelotas, RS, 2014. Epidemiol Serv Saude. 2020;29(1):e2019219. doi: 10.5123/S1679-49742020000100024. [DOI] [PubMed] [Google Scholar]
- 23.Diniz C.S., d'Orsi E., Domingues R.M., et al. Implementation of the presence of companions during hospital admission for childbirth: data from the birth in Brazil national survey. Cad Saude Publica. 2014;30(Suppl 1):S1–S14. doi: 10.1590/0102-311x00127013. http://www.ncbi.nlm.nih.gov/pubmed/25167174 [DOI] [PubMed] [Google Scholar]
- 24.Smith L.J. Impact of birthing practices on the breastfeeding dyad. J Midwifery Womens Health. 2007;52(6):621–630. doi: 10.1016/J.JMWH.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 25.Smith L.I. 2nd ed. 2010. Impact of birthing practices on breastfeeding. [Google Scholar]
- 26.Leal Mdo C., Gama S.G., Ratto K.M., Cunha C.B. Use of the modified Kotelchuck index in the evaluation of prenatal care and its relationship to maternal characteristics and birth weight in Rio de Janeiro, Brazil. Cad Saude Publica. 2004;20:S63. doi: 10.1590/s0102-311x2004000700007. [DOI] [PubMed] [Google Scholar]
- 27.Theme Filha M.M., Ayers S., Da Gama S.G.N., Leal M.D.C. Factors associated with postpartum depressive symptomatology in Brazil: the birth in Brazil national research study, 2011/2012. J Affect Disord. 2016;194:159–167. doi: 10.1016/j.jad.2016.01.020. [DOI] [PubMed] [Google Scholar]
- 28.Vasconcellos M.T., Silva P.L., Szwarcwald C.L. Sampling design for the world health survey in Brazil. Cad Saude Publica. 2005;21(Suppl):89–99. doi: 10.1590/S0102-311X2005000700010. [DOI] [PubMed] [Google Scholar]
- 29.Kline R.B. Principles and practice of structural equation modeling. Vol. 3. Guilford Press; New York: 2016. [Google Scholar]
- 30.Bentler P., Yuan K. Structural equation modeling with small samples: test statistics. Multivariate Behav Res. 1999;34(2):181–197. doi: 10.1207/S15327906Mb340203. [DOI] [PubMed] [Google Scholar]
- 31.Wang J., Wang X. Higher Education Press; United Kingdom: 2012. Structural equation modeling: applications using Mplus. [Google Scholar]
- 32.Di Cesare M., Bentham J., Stevens G.A., et al. Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet. 2016;387(10026):1377–1396. doi: 10.1016/S0140-6736(16)30054-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.World Health Organization 3 in 5 babies not breastfed in the first hour of life. 2022. https://www.who.int/news/item/31-07-2018-3-in-5-babies-not-breastfed-in-the-first-hour-of-life
- 34.Vieira T.O., Vieira G.O., Giugliani E.R.J., Mendes C.M., Martins C.C., Silva L.R. Determinants of breastfeeding initiation within the first hour of life in a Brazilian population: cross-sectional study. BMC Public Health. 2010;10(1):1–6. doi: 10.1186/1471-2458-10-760/TABLES/3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ansari H., Yeravdekar R. Respectful maternity care and breastfeeding. Glob Health Promot. 2021;28(3):70–72. doi: 10.1177/1757975920984216. [DOI] [PubMed] [Google Scholar]
- 36.Neamah H.H., Sudfeld C., McCoy D.C., et al. Intimate partner violence, depression, and child growth and development. Pediatrics. 2018;142(1):e20173457. doi: 10.1542/peds.2017-3457. [DOI] [PubMed] [Google Scholar]
- 37.Hasselmann M.H., Lindsay A.C., Surkan P.J., de Barros Vianna G.V., Werneck G.L. Intimate partner violence and early interruption of exclusive breastfeeding in the first three months of life. Cad Saude Publica. 2016;32(10) doi: 10.1590/0102-311X00017816. [DOI] [PubMed] [Google Scholar]
- 38.Yount K.M., DiGirolamo A.M., Ramakrishnan U. Impacts of domestic violence on child growth and nutrition: a conceptual review of the pathways of influence. Soc Sci Med. 2011;72(9):1534–1554. doi: 10.1016/J.SOCSCIMED.2011.02.042. [DOI] [PubMed] [Google Scholar]
- 39.Bandeira de Sá N.N., Gubert M.B., dos Santos W., Santos L.M.P. Factors related to health services determine breastfeeding within one hour of birth in the Federal District of Brazil, 2011. Rev Bras Epidemiol. 2016;19(3):509–524. doi: 10.1590/1980-5497201600030004. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization & United Nations Children’s Fund (UNICEF) Baby-friendlt hospital initiative. 2009. https://apps.who.int/iris/handle/10665/43593
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.