Abstract
We aimed to determine the effects of isoproterenol on arrhythmia recurrence in atrioventricular nodal re‐entrant tachycardia (AVNRT) patients treated with catheter ablation. The present randomized controlled clinical trial was conducted on AVNRT patients candidates for radiofrequency ablation (RFA). The patients were randomly assigned to receive isoproterenol (0.5–4 μg/min) or not (control group) for arrhythmia re‐induction after ablation. The results of the electrophysiological (EP) study, the ablation parameters, and the arrhythmia recurrence rate were recorded. We evaluated 206 patients (53 males and 153 females) with a mean (SD) age of 49.87 (15.5) years in two groups of isoproterenol (n = 103) and control (n = 103). No statistically significant difference was observed between the two studied groups in age, gender, EP study, and ablation parameters. The success rate of ablation was 100% in both groups. During ~16.5 months of follow‐up, one patient (1%) in the isoproterenol group and four patients (3.8%) in the control group experienced AVNRT recurrence (HR = 0.245; 95% confidence interval [CI], 0.043–1.418; p = .173). Based on the Kaplan–Meier analysis, there was no significant difference in the incidence rate of arrhythmia recurrence during the follow‐up period between the two studied groups (p = .129). Additionally, there were no significant differences between the arrhythmia's recurrence according to age, gender, junctional rhythm, type of AVNRT arrhythmia, and DAVN persistence after ablation. Although isoproterenol administration for arrhythmia re‐induction after ablation did not alleviate the treatment outcomes and arrhythmia recurrence following RFA in AVNRT patients, further studies with a larger sample size and a longer duration of follow‐up are necessary.
Keywords: arrhythmia recurrence, atrioventricular nodal reentry, catheter ablation, isoproterenol
According to the findings, the presence or absence of isoproterenol administration for arrhythmia re‐induction after ablation did not ameliorate the treatment outcomes and arrhythmia recurrence following radiofrequency ablation in atrioventricular nodal re‐entrant tachycardiapatients. However, further clinical trials with larger sample sizes and longer duration of follow‐up are necessary to confirm our findings.

Abbreviations
- AV
atrioventricular
- AVNRT
atrioventricular nodal re‐entrant tachycardia
- ECG
electrocardiography
- EP
electrophysiological
- SVT
supraventricular arrhythmia
1. INTRODUCTION
Atrioventricular (AV) re‐entrant tachycardia (AVNRT) is considered the most common regular supraventricular arrhythmia (SVT) in children and adults, 1 , 2 whose standard treatment is catheter ablation of the slow pathway in the AV node. 3 Currently, the non‐inducibility of re‐entrant arrhythmia after the ablation with programmed electrical stimulation with or without provocative medication is a conventional method to ensure the desired result of ablation. 4 , 5 However, although each strategy has its proponents and opponents and is employed by professionals, there is still insufficient documentation for evidence‐based decision‐making in choosing a strategy for pharmacological or non‐pharmacological induction of arrhythmia after the ablation. 2 , 6 , 7
Isoproterenol is a medicine frequently used to induce arrhythmia and enhance heart rhythm during electrophysiological (EP) studies after ablation. 8 However, the administration of isoproterenol is time‐consuming and may lead to short‐term complications such as hot flashes and shortness of breath in some patients. In addition, some studies noticed that complications such as coronary artery spasm, paradoxical bradycardia, tachyarrhythmia, and ventricular arrhythmia might occur following isoproterenol. 9 Meanwhile, some observational studies have also shown that isoproterenol has no effect on the frequency of arrhythmia recurrence after ablation in the long term in certain groups of patients. 10 Although isoproterenol has been used for a long time for inducing arrhythmia following ablation, no interventional studies have shown its effect on clinical outcomes and arrhythmia recurrence. Some studies have shown that the administration of isoproterenol effectively improves ablation outcomes, while others have identified it as an unaffected and complicated action. 7 , 11 Therefore, a clinical trial that shows the association of arrhythmia recurrence with the administration of isoproterenol after ablation may help better decide on the selection of strategy for the treatment with fewer side effects and a shorter duration of action. This randomized controlled study aimed to evaluate the impact of isoproterenol on arrhythmia recurrence in patients with AVNRT treated with ablation.
2. MATERIALS AND METHODS
2.1. Ethical statements
This study was confirmed by the ethics committee of Mashhad University of Medical Sciences (approval code. IR.MUMS.fm.REC.1395.364). Furthermore, this trial was registered at https://www.irct.ir/ (IRCT2016110630756N1). All participants received and signed written informed consent before enrollment.
2.2. Study design and randomization
The present randomized controlled clinical trial was conducted on all (303) patients with AVNRT who had had inducible arrhythmia and were candidates for RFA referred to the Cardiology Department of Imam Reza and Ghaem Hospitals affiliated to Mashhad University of Medical Sciences, Mashhad, Khorasan Razavi province, Iran, between 2016–2018.
After enrollment, 206 patients were randomly assigned using the simple randomization method and sealed envelope to receive isoproterenol (103 patients, doses of 0.5–4 μg/min) or control (without administration of isoproterenol, 103 patients). In both groups, patients had reproducibly inducible AVNRT without applying any provocative agent before ablation. After successful ablation, the arrhythmia induction was evaluated in the basal state and during isoproterenol infusion in the isoproterenol group and only in the basal state without any provocative agent in the control group. Isoproterenol was administered with doses of 0.5–4 μg/min to increase the rate of sinus rhythm by 25% compared to pre‐administration. The administration of isoproterenol was ended if arrhythmia was not induced.
2.3. Inclusion and exclusion criteria
The inclusion criteria were: (1) confirmation of AVNRT detection, (2) AVNRT induction without isoproterenol administration before ablation, and (3) no arrhythmia recurrence after standard ablation treatment. Furthermore, the exclusion criteria were (1) failure to perform ablation, (2) isoproterenol contraindication, and (3) non‐reproducibility of the induction of early arrhythmia.
2.4. Evaluation of outcomes
The baseline demographic characteristics of patients were documented, including age and gender. In addition, AVNRT type (typical or atypical), the total procedure time, fluoroscopy time, RF ablation time, and RFA frequency were also recorded. Moreover, follow‐up duration, complications during follow‐up, the frequency of Junctional rhythm, slow‐pathway elimination, DAVN, jump phenomenon, echo signal, and arrhythmia recurrence during the follow‐up period were documented.
2.5. Electrophysiological study
All antiarrhythmic drugs were discontinued before surgery for five half‐lives. The patients underwent local anesthesia with lidocaine, and three catheters of quadrupole electrodes were inserted through the femoral vein and placed in the upper right atrium, right ventricular apex, and the hiss bundle region. We performed a basic EP study to determine the retrograde conduction time through the AV node (Wenckebach point through the atrial and ventricular incremental pacing). We measured and documented the EP data. In the case of non‐inducible arrhythmia during the basic study, arrhythmia induction using programmed atrial stimulation with two or more drive trains (cycle lengths of 600 or 500 ms and 400 ms) with up to 3 extra‐stimuli or atrial burst pacing with descending cycle length was performed to induce the arrhythmia.
2.6. Radiofrequency ablation
After confirming the detection of AVNRT, an ablation catheter (Stinger, 7‐French, 4‐mm, solid‐tip) was embedded into the right atrium through the femoral vein in the septal tricuspid annulus and the anterior coronary sinus opening to regulate the slow pathway potential. The low‐power, scattered, slow pathway with an AV electrogram ratio of 0.1–0.15 (40) was generated during a sinus rhythm using a heart ablation generator IBI‐1500 T11 (St. Jude Medical, Inc.). Additionally, the temperature was controlled and limited to 60°C, and the power was titrated from 30 to 50 W of energy. In each RFA program, we moved the catheter to a new point if no junctional rhythm appeared for 20 s and repeated the ablation. If the junctional rhythm was observed, RFA lasted for up to 60 s unless there was a catheter dislocation or AV or ventriculoatrial (VA) block. The arrhythmia induction was assessed in the case of recurrent junctional rhythm or AV/VA block during RFA. The arrhythmia re‐induction protocols included the programmed atrial stimulation using 1–3 extra‐stimuli, a single ventricular extra‐stimuli, atrial and ventricular incremental pacing up to the Wenckebach cycle length, and atrial burst pacing. If the electrical stimulation failed to induce arrhythmia again, we deduced that the AVNRT was no longer inducible. In both isoprenaline and control groups, an acceptable endpoint was considered the persistence of single atrial echo signals or 50‐ms or more increment of the atrium‐to‐His (A–H) interval in response to a 10‐ms decrement of the coupling interval of an atrial extra‐stimulus (A–H jump) after ablation. We identified this as the slow pathway modification. Otherwise, we concluded that the slow pathway had been eliminated.
2.7. Follow‐up
All patients were visited and underwent 12‐lead electrocardiography (ECG) by a cardiac electrophysiologist on the day after the ablation and before discharge from the hospital. Moreover, all patients were discharged from the hospital without antiarrhythmic drugs and again performed 12‐lead ECG at 1 and 6 months of follow‐up. If symptoms of short‐duration supraventricular tachycardia (SVT) occur, 24‐ to 48‐h Holter monitoring was performed in patients that cannot tolerate standard 12‐lead ECG during the symptomatic period. Eventually, the incidence rate of arrhythmia recurrence and the time elapsed from ablation to arrhythmia recurrence were recorded. In case of developing symptoms similar to those before ablation or evidence of tachycardia recurrence in the ECG or Holter monitoring, the EP studies and, if necessary, the catheter ablation were repeated.
2.8. Statistical analysis
Data were analyzed using the SPSS version 22 statistical software (SPSS Inc.) and expressed according to the nature of parametric and non‐parametric as means ± SD or number with percentage, respectively. 12 , 13 , 14 First, the normal distribution of data was investigated using a one‐sample Kolmogorov–Smirnov test. Then, as appropriate, comparing continuous variables was performed using Student's t test for parametric data, or Mann–Whitney U and Wilcoxon tests for non‐parametric data. Next, the comparison between categorical variables was made using the Chi‐square test. Additionally, Kaplan‐Meyer analysis and log‐rank testing were used for event analysis. Finally, the hazard ratio (HR) was measured by means of Cox regression analysis. The p ≤ 0.05 were considered statistically significant.
3. RESULTS
3.1. Baseline characteristics
Overall, 206 patients (53 males and 153 females) with a mean age of 49.87 ± 15.5 years were included in the study and allocated to two groups, including those treated with isoproterenol (n = 103) and control (n = 103, Figure 1.). As presented in Table 1, the demographic characteristics of patients were well distributed between the two groups, including age (p = .41) and gender (p = .477).
FIGURE 1.
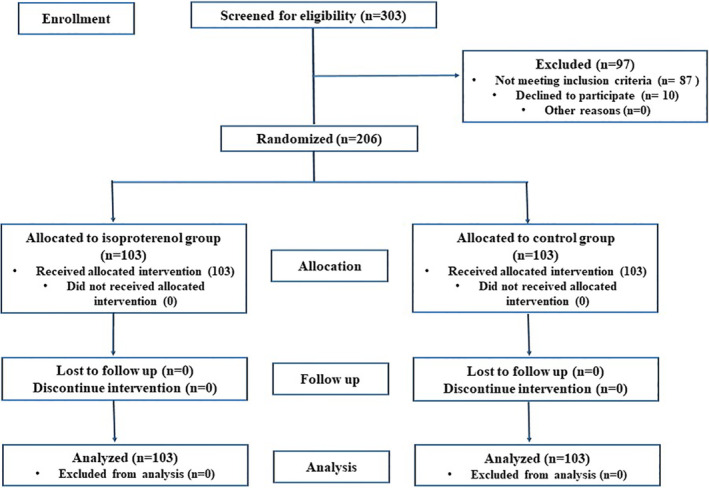
The flowchart of the study.
TABLE 1.
The demographic characteristics and the results of EP study and ablation parameters in AVNRT patients.
| Variable (mean ± SD) | Isoproterenol (n = 103) | Control (n = 103) | p‐value |
|---|---|---|---|
| Age (mean ± SD, years) | 52.2 ± 16 | 47.5 ± 15 | .41 a |
| Gender n (%) | |||
| Male | 22 (21.4%) | 31 (30.0%) | .477 b |
| Female | 81 (78.6%) | 72 (70.0%) | |
| AVNRT arrhythmia n (%) | |||
| Typical | 100 (97.0%) | 100 (97.0%) | .28 b |
| Typical and atypical | 1 (1.0%) | 3 (3.0%) | |
| Atypical | 2 (2.0%) | 0 (0.0%) | |
| Total procedure time (mean ± SD, min) | 50.4 ± 17.0 | 42.4 ± 18.8 | .01 a |
| Total procedure time without isoproterenol injection (mean ± SD, min) | 39.8 ± 16.1 | 42.2 ± 18.7 | .16 c |
| Fluoroscopy time (mean ± SD, s) | 698.76 ± 525.95 | 745.33 ± 559.81 | .569 |
| Diagnostic fluoroscopy time (mean ± SD, s) | 106.91 ± 57.98 | 116.61 ± 164.45 | .699 c |
| RF ablation time (mean ± SD, s) | 202.56 ± 187.79 | 190.69 ± 173.01 | .579 c |
| RF applications (mean ± SD, n) | 5.2 ± 4.9 | 5.4 ± 5.5 | .910 c |
| Slow‐pathway elimination n (%) | 36 (71.3) | 34 (66.3) | .56 b |
| Junctional rhythm n (%) | |||
| Yes | 101 (98.0%) | 103 (100%) | .502 b |
| No | 2 (2.0%) | 0 (0%) | |
Abbreviations: AVNRT, atrioventricular nodal re‐entrant tachycardia; RF, radiofrequency.
Comparing between the isoproterenol and control groups using T test.
Comparing the isoproterenol and control groups using Chi‐square test.
Comparing between the isoproterenol and control groups using Mann–Whitney test.
3.2. The results of the EP study and ablation parameters in AVNRT patients
Most patients showed the typical AVNRT arrhythmia in both isoproterenol and control groups (97.0% for both cases), and there were no significant differences in the type of arrhythmia between the two groups (p = .28, Table 1). The mean total procedural time, measured as the time from insertion to the removal of venous sheaths, was longer in the isoproterenol group than in the control group (50.4 ± 17 and 42.2 ± 18.7 min, respectively; p = .01). As presented in Table 1, no significant differences were observed in the total procedure time without isoproterenol injection (p = .160), fluoroscopy time (p = .16), diagnostic fluoroscopy duration (p = .699), RF ablation duration (0.567), and the number of RF ablations (0.91) between the isoproterenol and control groups (Table 2). Additionally, the success rate of ablation was reported to be 100% in both groups, in which 133 patients (65.5%) with slow‐pathway modification and 70 patients (34.5%) with slow‐pathway elimination. No significant differences were observed in the slow pathway modification or elimination between the two studied groups (p = .56). Furthermore, the junctional rhythm was observed in 204 of 206 patients (99%) during RF application, and no significant differences were reported between the two studied groups (0.502).
TABLE 2.
The results of follow‐up variables in AVNRT patients.
| Variable | Isoproterenol (n = 103) | Control (n = 103) | p‐value |
|---|---|---|---|
| Follow‐up duration (mean ± SD, months) | 17.85 ± 7.8 | 14.89 ± 4.2 | .9 a |
| Complication n (%) | |||
| No complication | 103 (100%) | 102 (99.03%) | .454 b |
| Transient AV block | 0 (0.0%) | 1 (0.97%) | |
| Complete AV block | 0 (0.0%) | 0 (0.0) | |
| Jump phenomenon n (%) | |||
| Yes | 54 (54.0%) | 55 (56.3%) | .894 b |
| No | 48 (46.0%) | 45 (43.7%) | |
| Presence of echo signal n (%) | |||
| Yes | 62 (60.0%) | 48 (57.3%) | 0.5 b |
| No | 40 (40.0%) | 55 (42.7%) | |
| DAVN n (%) | |||
| Yes | 71 (70.0%) | 69 (33.7%) | .56 b |
| No | 32 (30.0%) | 34 (66.3%) | |
| Recurrence of arrhythmia n (%) | |||
| Yes | 1 (1.0%) | 4 (3.8%) | .179 b |
| No | 102 (99.0%) | 99 (96.2%) | |
Abbreviation: AV, atrioventricular.
Comparing the isoproterenol and control groups using the Mann–Whitney test.
Comparing the isoproterenol and control groups using the Chi‐square test.
3.3. Follow‐up results in AVNRT patients
The mean follow‐up period was 17.85 ± 7.8 months in the isoproterenol group and 14.89 ± 4.2 months in the control group (p = .9, Table 2). Most patients (99.5%) reported no complications during the follow‐up period, and only one patient in the control group experienced a transient AV block (p = .454, Table 2). Furthermore, there were no significant differences in the frequency of junctional rhythm (p = .502), jump phenomenon (p = .894), presence of echo signal (0.5), and DAVN (p = .56) after ablation in ANVRT patients between the two studied groups (Table 2).
Our results also determined that one patient in the isoproterenol group and four in the control group experienced AVNRT recurrence during the follow‐up period (HR = 0.245; 95% confidence interval [CI], 0.043–1.418; p = .173). The experimental event rate (EER) was 0.01, and the control event rate (CER) was 0.04. The Number Needed to Treat (NNT) index was also obtained to be 34.3 for isoproterenol intervention. However, based on the Kaplan–Meier curve, there was no significant difference in the incidence rate of arrhythmia recurrence during the follow‐up period between the two studied groups (p = .129, Figure 2). Additionally, all five patients who encountered recurrent arrhythmia were female with accelerated junctional rhythm during ablation and typical AVNRT arrhythmia. However, there were no significant differences between the arrhythmia's recurrence according to age (p = .23), gender (p = .18), junctional rhythm (p = .89), and type of AVNRT arrhythmia (p = .92) based on the Kaplan–Meier curve. Similarly, the prevalence of arrhythmia recurrence among patients with DAVN and those without DAVN were 4 (2.6%) and 1 (1.4%), respectively, and no significant difference was observed using the Kaplan–Meier curve (p = .7).
FIGURE 2.
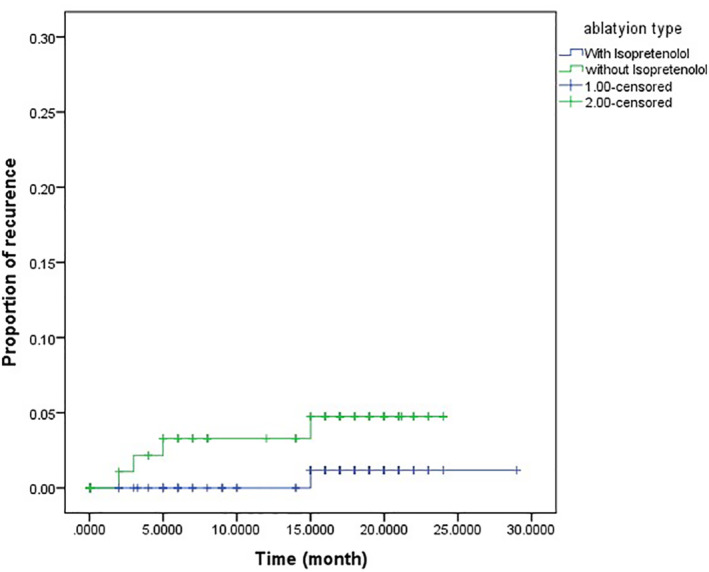
Kaplan‐Mayer curve showing arrhythmia recurrence in AVNRT patients in isoproterenol and control groups.
4. DISCUSSION
To the best of our knowledge, this study was the first randomized controlled clinical trial determining the efficacy of isoproterenol in preventing arrhythmia recurrence after ablation in patients with AVNRT. Our results showed that the presence or absence of isoproterenol administration to evaluate post‐ablation inducibility did not significantly ameliorate the incidence of arrhythmia recurrence during the follow‐up period of about 16.5 months. In our study, the incidence rate of arrhythmia recurrence after ablation was 1.0% in the isoproterenol group and 3.8% in the control group. Additionally, there was no significant difference in the incidence rate of arrhythmia recurrence during the follow‐up period between the two studied groups based on the Kaplan–Meier curve (p = .129). Inconsistent with our results, Frey and coworkers demonstrated that AVNRT recurrence occurred in 9 of 534 patients (2.7%) during the 15.5 years follow‐up after ablation. 15 In another study, the recurrence rate was reported as about 1% during the 26 months of follow‐up. 16 Wang et al. supported that seven patients (6.14%) had AVNRT recurrence following 5 years of follow‐up. 17
In line with our results, Heydari and coworkers conducted a retrospective observational study on AVNRT patients who underwent radiofrequency ablation and divided them into two groups of receiving isoproterenol for arrhythmia re‐induction after ablation (90 patients) and not receiving isoproterenol as the control group (85 patients). During about 18 months of follow‐up, they determined that four patients (4.4%) in the isoproterenol group and three patients (3.4%) in the control group experienced arrhythmia recurrence after ablation and the total incidence rate of arrhythmia recurrence was 4%. Similarly, there were no significant differences in the recurrence rate between the isoproterenol and control group (p = .723). 10 Consistently, Chin and coworkers studied 3311 patients who underwent catheter ablation for AVNRT for about 130 months and divided them according to the presence or absence of arrhythmia recurrence. In line with our results, most of the patients were female and with typical AVNRT arrhythmia, and AVNRT recurrence was observed in 65 patients (2%). Interestingly, there were no significant differences in the administration of isoproterenol for re‐induction of AVNRT between the no‐recurrence and recurrence groups (41.2%, and 43.1%, respectively, p = .76). 18 These studies may confirm our results regarding no relationship between the administration of isoproterenol and the recurrence rate of arrhythmia.
Our results also revealed that 74.2% of AVNRT patients included in our study were female. This finding is in line with previous results regarding the more prevalent AVNRT in the female gender. 19 , 20 Moreover, we also figured out that the success rate of ablation in AVNRT patients was 100% in both isoproterenol and control groups. In accordance with our results, Katritsis et al. compared the catheter ablation vs. antiarrhythmic drug therapy for AVNRT patients. They emphasized that all patients who underwent catheter ablation were free of arrhythmia or conduction disturbances during the 5‐year follow‐up. In contrast, 75% of patients in the antiarrhythmic drug therapy group required hospital admission for cardioversion. In addition, survival‐free hospital admission for persistent tachycardia cardioversion was significantly higher in the ablation group than in the antiarrhythmic drug group. 21
We also showed that all five patients who encountered recurrent arrhythmia were female with junctional rhythm and typical AVNRT arrhythmia. However, there was no significant relationship between the recurrence of arrhythmia and gender, junctional rhythm, and type of AVNRT arrhythmia. In line with our results, Heidari et al. noticed that age, gender, time of fluoroscopy and radiofrequency, type of ablation, and the presence of junctional rhythm did not significantly affect the treatment outcomes of AVNRT. 10 Additionally, Feldman and coworkers investigated 1419 patients with AVNRT who underwent slow pathway ablation and reported 98.1% success in the ablation process. Similar to our results, the mean age of patients was 48.6 years old, and 66.2% of patients were female. Moreover, the atypical AVNRT was only diagnosed in 5.1% of patients, 76.1% received isoproterenol, and 1.41% encountered transient AV block. Following the 63 months of follow‐up, 22 patients (1.5%) had recurrent AVNRT, and they found that age <20 years and female gender were significant predictors of recurrent AVNRT. Interestingly, the usage of isoproterenol could not be a significant predictor of AVNRT recurrence. 22 Accordantly, Katritsis and coworkers evaluated 1007 patients with typical AVNRT and 77 with atypical AVNRT who underwent slow pathway ablation. Similar to our results, they reported that 96% of patients had junctional rhythm during RF, and only one case (0.1%) of transient AV block was observed in the typical AVNRT group. They found 21 cases (2.1%) of arrhythmia recurrence in the typical and three cases (3.9%) in the atypical group after 3 months of follow‐up, and the total recurrence rate was 2.2%. Furthermore, they noticed that the patients with recurrence arrhythmia were mostly female, with typical AVNRT, longer fluoroscopy time, and junctional rhythm. However, only the female gender had the predictive value for arrhythmia recurrence. 23
This study also had several limitations. The most important one was the lack of cooperation of patients in the follow‐up study; however, in cases where the patients did not refer to the clinic during the determined appointments, we tried to call them to ask about their condition and check the clinical symptoms related to arrhythmia recurrence. The second limitation was the sample size due to the low arrhythmia recurrence rate. Although our study was conducted on more than 200 patients, based on the incidence of recurrence after ablation in an interventional group (1%) and the incidence of recurrence after ablation in the control group (3.8%) and regarding type one error of 0.05, we found study power <80%. Therefore, the non‐statistically significant difference between the isoproterenol and control group may be due to the inadequate sample size, and the results might be significant in a higher sample size. However, this was the largest sample size we could reach during our study period. Therefore, it seems that the effect of isoproterenol on clinical outcomes should be investigated in other studies with statistically larger sample sizes.
5. CONCLUSIONS
According to the findings, the presence or absence of isoproterenol administration for arrhythmia re‐induction after ablation did not ameliorate the treatment outcomes and arrhythmia recurrence following RFA in AVNRT patients. However, further clinical trials with larger sample sizes and longer duration of follow‐up are necessary to confirm our findings.
AUTHOR CONTRIBUTIONS
Neda Vahid Lotfabadi: Investigation, Data Curation; Saeed Mehrabi: Investigation, Data Curation; Alireza Heidari‐Bakavoli: Conceptualization, Methodology; Negar Morovatdar: Formal Analysis, Methodology, Software; Mohammad Tayyebi: Conceptualization, Methodology, Supervision, Funding Acquisition; Vafa Baradaran Rahimi: Formal Analysis, Writing – Original Draft, Writing – review & editing.
FUNDING INFORMATION
This study was financially supported by grant number: 950133 from Mashhad University of Medical Sciences.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ETHICS APPROVAL
This study was confirmed by the ethics committee of Mashhad University of Medical Sciences (approval code. IR.MUMS.fm.REC.1395.364). Furthermore, this trial was registered at https://www.irct.ir/ (IRCT2016110630756N1).
CONSENT TO PARTICIPATE
All participants received and signed written informed consent before their inclusion in the study.
CONSENT FOR PUBLICATION
All the authors consented to this study's publication in the journal.
ACKNOWLEDGMENTS
This study was financially supported by the research council of Mashhad University of Medical Sciences (grant number: 950133).
Vahid Lotfabadi N, Mehrabi S, Heidari‐Bakavoli A, Morovatdar N, Tayyebi M, Baradaran Rahimi V. Evaluation of the effects of isoproterenol on arrhythmia recurrence following catheter ablation in patients with atrioventricular nodal re‐entrant tachycardia: A randomized controlled clinical trial. Pharmacol Res Perspect. 2023;11:e01068. doi: 10.1002/prp2.1068
Neda Vahid Lotfabadi and Saeed Mehrabi shared the first co‐authorship.
Contributor Information
Mohammad Tayyebi, Email: tayyebim@mums.ac.ir.
Vafa Baradaran Rahimi, Email: baradaranrv@mums.ac.ir, Email: vafa_br@yahoo.com.
DATA AVAILABILITY STATEMENT
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Katritsis DG, Camm AJ. Atrioventricular nodal reentrant tachycardia. Circulation. 2010;122(8):831‐840. [DOI] [PubMed] [Google Scholar]
- 2. Shafiee‐Nick R, Afshari AR, Mousavi SH, et al. A comprehensive review on the potential therapeutic benefits of phosphodiesterase inhibitors on cardiovascular diseases. Biomed Pharmacother. 2017;94:541‐556. [DOI] [PubMed] [Google Scholar]
- 3. Katritsis DG. Catheter ablation of atrioventricular nodal re‐entrant tachycardia: facts and fiction. Arrhythm Electrophysiol Rev. 2018;7(4):230‐231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sugumar H, Tung M, Leather R, Lane C, Sterns LD, Novak PG. Atrioventricular nodal non Re‐entrant tachycardia (AVNNT). Heart Lung Circ. 2017;26(5):524‐525. [DOI] [PubMed] [Google Scholar]
- 5. Sohinki D, Obel OA. Current trends in supraventricular tachycardia management. Ochsner J. 2014;14(4):586‐595. [PMC free article] [PubMed] [Google Scholar]
- 6. Chun HM, Sung RJ. Supraventricular tachyarrhythmias. Pharmacologic versus nonpharmacologic approaches. Med Clin North Am. 1995;79(5):1121‐1134. [DOI] [PubMed] [Google Scholar]
- 7. Weismüller P, Kuly S, Brandts B, Kattenbeck K, Ranke C, Trappe HJ. Is electrical stimulation during administration of catecholamines required for the evaluation of success after ablation of atrioventricular node re‐entrant tachycardias? J Am Coll Cardiol. 2002;39(4):689‐694. [DOI] [PubMed] [Google Scholar]
- 8. Liberman L, Hordof AJ, Fishberger SB, Pass RH. The role of isoproterenol testing following radiofrequency catheter ablation of accessory pathways in children. Pacing Clin Electrophysiol. 2003;26(2 Pt 1):559‐561. [DOI] [PubMed] [Google Scholar]
- 9. Stern JD, Rolnitzky L, Goldberg JD, et al. Meta‐analysis to assess the appropriate endpoint for slow pathway ablation of atrioventricular nodal reentrant tachycardia. Pacing Clin Electrophysiol. 2011;34(3):269‐277. [DOI] [PubMed] [Google Scholar]
- 10. Heydari A, Tayyebi M, Jami RD, Amiri A. Role of isoproterenol in predicting the success of catheter ablation in patients with reproducibly inducible atrioventricular nodal reentrant tachycardia. Tex Heart Inst J. 2014;41(3):280‐285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Matsushita T, Chun S, Sung RJ. Influence of isoproterenol on the accelerated junctional rhythm observed during radiofrequency catheter ablation of atrioventricular nodal slow pathway conduction. Am Heart J. 2001;142(4):664‐668. [DOI] [PubMed] [Google Scholar]
- 12. Abbasi S, Kamalinejad M, Babaie D, et al. A new topical treatment of atopic dermatitis in pediatric patients based on Ficus carica L. (Fig): a randomized, placebo‐controlled clinical trial. Complement Ther Med. 2017;35:85‐91. [DOI] [PubMed] [Google Scholar]
- 13. Askari VR, Baradaran Rahimi V, Tabatabaee SA, Shafiee‐Nick R. Combination of imipramine, a sphingomyelinase inhibitor, and beta‐caryophyllene improve their therapeutic effects on experimental autoimmune encephalomyelitis (EAE). Int Immunopharmacol. 2019;77:105923. [DOI] [PubMed] [Google Scholar]
- 14. Baradaran Rahimi V, Askari VR, Mousavi SH. Ellagic acid dose and time‐dependently abrogates d‐galactose‐induced animal model of aging: investigating the role of PPAR‐gamma. Life Sci. 2019;232:116595. [DOI] [PubMed] [Google Scholar]
- 15. Frey MK, Richter B, Gwechenberger M, et al. High incidence of atrial fibrillation after successful catheter ablation of atrioventricular nodal reentrant tachycardia: a 15.5‐year follow‐up. Sci Rep. 2019;9(1):11784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Manolis AS, Maounis T, Vassilikos V, Chiladakis J, Cokkinos DV. Arrhythmia recurrences are rare when the site of radiofrequency ablation of the slow pathway is medial or anterior to the coronary sinus os. Europace. 2002;4(2):193‐199. [DOI] [PubMed] [Google Scholar]
- 17. Wang L, Wu T. Predictors of long‐term success in catheter ablation of atrioventricular nodal reentrant tachycardia: a multivariate regression analysis. Int J Cardiol. 2002;86(2):289‐294. [DOI] [PubMed] [Google Scholar]
- 18. Chin CG, Chung FP, Lin YJ, et al. Extremely late recurrences (≥3 years) of atrioventricular nodal reentrant tachycardia: electrophysiological characteristics of the index and repeat ablation procedures. Int J Cardiol. 2020;305:70‐75. [DOI] [PubMed] [Google Scholar]
- 19. Farkowski MM, Pytkowski M, Maciag A, et al. Gender‐related differences in outcomes and resource utilization in patients undergoing radiofrequency ablation of supraventricular tachycardia: results from Patients' Perspective on Radiofrequency Catheter Ablation of AVRT and AVNRT study. Europace. 2014;16(12):1821‐1827. [DOI] [PubMed] [Google Scholar]
- 20. Wasmer K, Dechering DG, Köbe J, et al. Patients' and procedural characteristics of AV‐block during slow pathway modulation for AVNRT‐single center 10 year experience. Int J Cardiol. 2017;244:158‐162. [DOI] [PubMed] [Google Scholar]
- 21. Katritsis DG, Zografos T, Katritsis GD, et al. Catheter ablation vs. antiarrhythmic drug therapy in patients with symptomatic atrioventricular nodal re‐entrant tachycardia: a randomized, controlled trial. Europace. 2017;19(4):602‐606. [DOI] [PubMed] [Google Scholar]
- 22. Feldman A, Voskoboinik A, Kumar S, et al. Predictors of acute and long‐term success of slow pathway ablation for atrioventricular nodal reentrant tachycardia: a single center series of 1,419 consecutive patients. Pacing Clin Electrophysiol. 2011;34(8):927‐933. [DOI] [PubMed] [Google Scholar]
- 23. Katritsis DG, Zografos T, Siontis KC, et al. Endpoints for successful slow pathway catheter ablation in typical and atypical atrioventricular nodal Re‐entrant tachycardia: a contemporary, multicenter study. JACC Clin Electrophysiol. 2019;5(1):113‐119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon reasonable request.


