Abstract
Background: Adverse sequelae are common in survivors of critical illness. Physical, psychological and cognitive impairments can affect quality of life for years after the original insult. Driving is an advanced task reliant on complex physical and cognitive functioning. Driving represents a positive recovery milestone. Little is currently known about the driving habits of critical care survivors. The aim of this study was to explore the driving practices of individuals after critical illness.
Methods: A purpose-designed questionnaire was distributed to driving licence holders attending critical care recovery clinic. Results: A response rate of 90% was achieved. 43 respondents declared their intention to resume driving. Two respondents had surrendered their licence on medical grounds. 68% had resumed driving by 3 months, 77% by 6 months, and 84% by 1 year. The median interval (range) between critical care discharge and resumption of driving was 8 weeks (1–52 weeks). Psychological, physical and cognitive barriers were cited by respondents as barriers to driving resumption. Eight themes regarding driving resumption were identified from the framework analysis under three core domains and included: psychological/cognitive impact on ability to drive (Emotional readiness and anxiety; Confidence; Intrinsic motivation; Concentration), physical ability to drive (Weakness and fatigue; Physical recovery), and supportive care and information needs to resume driving (Information/advice; Timescales).
Conclusion: This study demonstrates that resumption of driving following critical illness is substantially delayed. Qualitative analysis identified potentially modifiable barriers to driving resumption.
Keywords: driving, critical illness, critical care, recovery, intensive care
Introduction
Physical, psychological and cognitive impairments are common in survivors of critical illness. 1 These impairments, collectively known as Post-Intensive Care Syndrome (PICS), diminish quality of life and are burdensome for patients, carers and society.2,3 An increasing awareness and recognition of PICS has prompted commitments to enhance multidisciplinary aftercare with the overall goal of improving patient-centred outcomes and health-related quality of life.
Resumption of driving represents a crucial recovery milestone. For those patients who are licence holders, return to driving may promote independence and enable other determinants of recovery such as social activity and return to employment. Driving is, however, a complex task necessitating intact cognition (executive skills, visual perception, attention, memory and comprehension), physical ability (strength, sensation, coordination and reaction speed) as well as emotional preparedness. 4 These elements may all be affected after critical illness. 5
National and international guidance regarding fitness to drive covers neurological, cardiovascular and respiratory conditions.4,6,7 Although specific components of PICS such as cognitive impairment and limb dysfunction are discussed in the guidance, with a legal requirement to notify DVLA of cognitive defects, the combined impact of an individual’s interacting PICS domains on driving suitability is not addressed. Thus, healthcare professionals and individuals lack consistent advice as to when driving resumption can occur. Individuals may self-determine suitability to drive without professional guidance. Premature resumption carries risks to both self and other road users. Conversely, return to driving should not be arbitrarily prohibited or unduly prolonged. Enabling return to driving is important as it allows independence and return to everyday activities. Very little evidence exists to guide clinicians and patients following critical illness. Wolfe and Lehockey (2016) suggest clinicians should take into account functional ability and medical history, including conditions that may impair ability to drive and react, and correlate these factors with the risk for driving accidents. 8 Presently, little is known about when, or if, patients return to driving after critical illness and what barriers patients experience in relation to this activity. The aim of this study was to explore and gain insight into driving practices of individuals following critical illness.
Methods
Design
An anonymised, cross-sectional, questionnaire was used to ascertain both quantitative (age, gender, driving status, time course of driving resumption) and qualitative experiential aspects of driving resumption (via open-ended questions). The primary outcome was the prevalence of driving resumption at 3 months following ICU discharge.
Setting
This study was undertaken in the adult critical care department of a large UK District General Hospital with 18 beds, approximately 800 admissions per year, ICU mortality of 18.9%, and mixed medical/surgical case mix.
Respondents
Driving licence-holding adults having undergone four or more days mechanical ventilation attending the Rehabilitation After Critical Illness outpatient clinic between 3 and 12 months after hospital discharge were eligible to participate.
Fifty consecutive clinic attendees between 2014 and 2015 were invited to complete a short, anonymised questionnaire to solicit quantitative (timing) and qualitative data (open-ended textual responses) about driving resumption. Informed consent was sought from all respondents and completion of the survey was considered indicative of consent. Royal Berkshire NHS Foundation Trust R&D approved this work as a service evaluation.
Materials and procedure
Survey questions were devised by an iterative process and were considered for content and face validity by two researchers (JM and CW). Five questions were included in the final questionnaire (listed in Supplemental Table 1). Respondents could opt to complete the handwritten paper survey whilst in clinic or alternatively in their own time by postal return. Respondents received assurance that any ongoing treatment or care would not be affected by participating in the survey.
Data Analysis
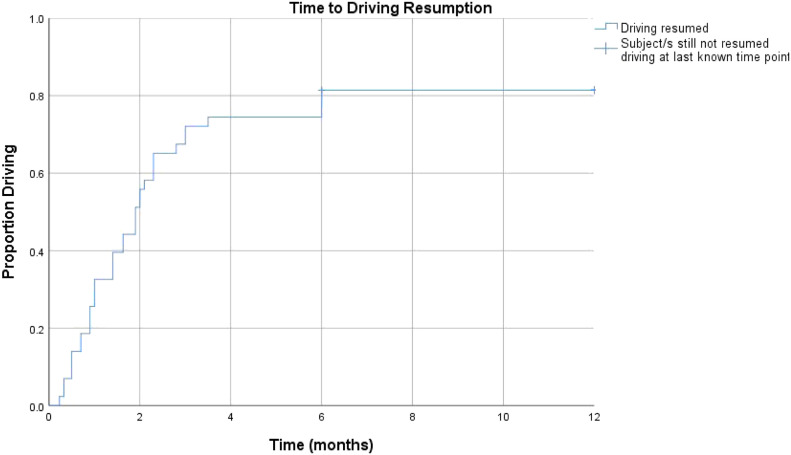
Quantitative data were of the nominal/ordinal form and analysed using SPSS Version 25 using descriptive frequency analyses (percentages). Continuous data were reported as a median and range. The Kaplan-Meier method was used to analyse time-to-event i.e. days from ICU discharge to driving resumption.
Qualitative textual data from the open-ended questions were analysed into themes using framework analysis. 9 This is an established approach used in numerous health research studies, and it is not uncommon to use open-ended survey text as a qualitative data source.10,11 Themes for the framework were derived from the data, with the framework refined as data analysis took place. Data were examined by two researchers to ensure consensus was reached across each theme and how comments were attributed under those themes. These two researchers transcribed and analysed the handwritten survey data independently before agreeing the key themes for the framework analysis. This was then applied across all the data. A third researcher independently reviewed the raw data and choice of themes in the framework to increase robustness and reduce potential bias.
Results
45 out of 50 respondents completed the questionnaire (90% response rate). The median age of respondents was 60 years (range 27–82), and 50% female. 43 respondents possessed a valid driving licence and declared an intention to resume driving. Two respondents had surrendered their licence on medical grounds. The surveyed population was reflective of the diverse critical care unit admission source: emergency admission 39%, post-operative admission 25%, medical inpatient ward admission 29%, other 7%.
43 out of 45 respondents provided information about driving resumption timeframes. The primary outcome, the proportion of respondents who had resumed driving by the 3 months time-point after ICU discharge, was 68% (n = 31). By the 6 months time-point the proportion was 77% (n = 35).
The median interval between ICU discharge and resumption of driving was 8 weeks. The time period for resumption was markedly variable ranging from 1 to 52 weeks post ICU discharge (Figure 1). 16% had not resumed driving by the 1 year time-point.
Figure 1.
Kaplan-Meier curve time to driving resumption after ICU discharge.
28 out of the 45 respondents provided information about the advice they received regarding driving resumption (Table 1). One respondent had undertaken a ‘return to driving’ course. Seven (16%) of respondents reported that ability to perform an emergency stop was a key factor determining whether, or not, to resume driving.
Table 1.
Sources of advice received by respondents.
| Sources of advice | No: of respondents n (%) |
|---|---|
| Did not seek or receive advice | 17 (38) |
| Did seek or receive advice | 28 (62) |
| • GP | 8 (29) |
| • DVLA a | 4 (14) |
| • Specialist b | 4 (14) |
| • Nurse | 2 (7) |
| • Recovery after critical illness clinic | 1 (4) |
| • Insurance company | 1 (4) |
aDVLA = Driver and Vehicle Licensing Agency.
bSpecialist = two cardiologists, one surgeon, one ward doctor.
Qualitative analysis
Eight themes regarding driving resumption were identified from the framework analysis under three core domains (Table 2). These included: psychological/cognitive impact on ability to drive (Emotional readiness and anxiety; Confidence; Intrinsic motivation; Concentration), physical ability to drive (Weakness and fatigue; Physical recovery), and supportive care and information needs to resume driving (Information/advice; Timescales). These themes were coexistent; for example, where there was diminished physical ability, confidence was commonly affected. Cognitive deficits, such as spatial awareness and information processing were considered under the psychological domain as respondents did not link these to physical issues and placed these within the context of psychological recovery.
Table 2.
Evidence of themes.
| Domain | Themes | No: Of comments | Sample comments |
|---|---|---|---|
| Psychological/cognitive impact on ability to drive | Confidence in relation to driving ability | 27 | Respondent 21 – Male, 76: “Confidence an important factor (lack of) after long hospital stay” |
| Respondent 42 - Male, 64: “Apprehensive at first; start/ed when confident in self” | |||
| Ability to drive – intrinsic motivation | 25 | Respondent 16 – Male, 66: “Important for ‘return to normal” | |
| Respondent 19 – Female, 55: “Wanted to return to being the person I was before all this trauma” | |||
| Concentration | 10 | Respondent 12 – Female, 75: “Extremely muddled after discharge; more alert now” | |
| Respondent 36 - Male, 61: “It’s your mental ability that’s the problem; unable to deal with all the information around you, difficult to process it; things move too fast after a prolonged period of not driving” | |||
| Emotional readiness | 9 | Respondent 31 – Female, 74: “Nerve wracking at first” | |
| Respondent 41 – Male, 76: “Emotional rollercoaster” | |||
| Anxiety | 7 | Respondent 5 – Male, 34: “Didn’t want to rush and put family in danger” | |
| Respondent 15 – Female, 72: “Felt so vulnerable (so waited longer than advised)” | |||
| Physical ability | Physical recovery | 20 | Respondent 5 - Male, 34: “Not strong enough at first; waited until gained some weight” |
| Respondent 9 – Female, 31: “Hard work in arms; waited until I could do an emergency stop; had an open wound (covered) – waited until it didn’t hurt” | |||
| Weakness/Fatigue | 7 | Respondent 2 – Female, 56: “Too tired initially; body so utterly weakened; Strength began to return after a few weeks. Even after 2 months still to tiring to drive more than 1h; Motorway driving tiring” | |
| Respondent 37 – Male, 71: “Felt weak and listless with no energy and not until 5/6 weeks that felt able” | |||
| Supportive care and information needs | Timescales | 41 | Respondent 1 - female, 68: “Approx. 3 months (1st time)” |
| Respondent 29 – Male, 60: “At least 10 weeks” | |||
| Information from ICU/Recovery clinic/GP | 34 | Respondent 8 - Male, 75: “Asked ward doctor (concerned re: medication side effects); advised if could brake, okay” | |
| Respondent 23 - female, 36: “Discussed with work and GP; GP advised against it at first. Course arranged via work. No information given from hospital (how/when/legalities).” | |||
| Guidance/other (distance) | 26 | Respondent 16 – Male, 66: “Initially, short journeys only; should be part of post-ICU debriefing process” | |
| Respondent 12 – Female, 75: “Try to drive in quiet area with company” | |||
| Suggestions | 9 | Respondent 8 – Male, 75: “Short trips at first; not unduly limited now. Should seek advice, especially if long period of not driving; short trips to be advised at first for others” | |
| Respondent 12 – Female, 75: “Driving instructor session would be useful before deciding to drive” |
Psychological and cognitive impact on ability to drive
The psychological and cognitive aspects of resuming driving was strongly influenced by confidence, a prominent theme that was raised by many respondents (n = 27). It was reported both negatively and positively, with a lack of confidence an important factor in returning to driving, and on extent of driving. Some respondents, however, reported no issues in returning to driving, Confidence determined how, when, and how much people returned to driving. Various strategies were used to mitigate against this, including having accompanied practice. Some respondents suggested ‘driving buddies’ and with many advocating local drives first. Self-confidence was reported to increase once driving had been attempted.
“… started with short trips of less than 1 mile, which gradually got longer. Accompanied practice, a ‘driving buddy’ was useful for confidence” (Respondent 3)
Distinct from confidence, emotional readiness related to respondents reporting being ready to drive again, as opposed to being confident in their ability. They cited confidence and emotions as different, and that emotional problems might be at the root of recovery and ability to drive:
“This was an emotional and confidence thing rather than a physical.” (Respondent 41)
“I found it a bit stressful at first – but I needed to drive again. But I now get a bit angry at drivers” (Respondent 10)
Intrinsic motivation to drive as part of motivation to resume normal activities with driving a marker of recovery was identified by respondents.
“… (driving is) important for ‘returning to normal’” (Respondent 16)
“Stubbornness, determination and denial. A desire to get my independence back” (Respondent 23)
Reduced ability to concentrate, feeling muddled and being mentally unprepared, with slower response times and decreased mental alertness were reported. This theme also related to spatial awareness, and one driver reported having a minor accident (described as a ‘scrape’) on their first drive since discharge and directly attributed this to being unable to concentrate post-ICU. Respondents varied in their self-awareness of their mental capacity to drive.
“… things move too fast after a long period of not driving” (Respondent 36)
“(I needed to) be mentally ready; I can’t do long journeys – am tired and have no concentration” (Respondent 13)
“I did a test drive to check spatial awareness etc..” (Respondent 8)
Physical ability
Features of physical ability to drive included: weakness and fatigue, and physical recovery. Individual physical recovery and the ability to perform key driving functions, such as emergency stops, were a determining factor in driving resumption. For some respondents this aspect prevented driving for several months.
“I was physically exhausted at first. I had no shoulder or ankle flexibility” (Respondent 23)
Weakness and fatigue were also cited by respondents.
“Accompaniment was helpful if I got too tired… (or I was) concerned about fatigue” (Respondent 3)
“A stay in ICU is such a shock, your body is so utterly weakened. When recovering you take one step at a time and meet the challenges. Certainly, driving was not my first concern. . . As a few weeks passed, my strength began to return . . . Even after 2 months I’m still too tired to drive for an hour, especially motorway driving.” (Respondent 2)
The connection with mental and psychological readiness was also outlined:
“I wanted to wait until my legs felt strong to use the footbrake in an emergency and my brain was quick to respond” (Respondent 6)
Supportive care and information needs
Sources of information accessed by individuals about driving following critical illness was highly variable. Respondents reported that advice from GPs or medical teams often focused on physical function; ability to undertake an emergency stop was commonly used as a proxy for readiness to drive. This was not always regarded as helpful, with some respondents suggesting a driving test, or some sort of cognitive check prior to driving resumption was needed. Mental and cognitive ability were not interrogated, other than subjective ‘readiness’.
“Asked doctor as wanted to be sure; doctor advised it was okay if I could do an emergency stop” (Respondent 9)
“No guidance, our doctor said that I should start when I felt ready” (Respondent 16)
Timescales for those who returned to driving varied significantly, with feelings of being ‘ready’ most commonly cited by respondents, thus suggesting this subjective notion of readiness was important for mental preparedness with many respondents articulating that they did not feeling ready to tackle long drives.
“(it has) taken 18 months to feel I could drive safely” (Respondent 14)
“To begin with I just sat in the car without actually driving, 6 weeks on I’m only driving short distances.” (Respondent 21)
Respondent-generated ideas to assist with driving resumption included driving re-tests, time with driving instructors to build confidence and motorway driving courses. Graded exposure to driving was a recurring theme, with many people initially ‘testing’ their ability to drive safely by undertaking short distance journeys. Clear accessible guidance after critical illness was advocated by respondents.
Discussion
This single centre study elicited the incidence, time-course and experience of driving resumption among 45 adult critical illness survivors who had undergone four or more days of mechanical ventilation in a mixed general UK NHS intensive care. We showed that driving resumption was frequently delayed or not achieved; 32% of driving licence holders had not resumed driving by 3 months following ICU discharge and 16% had not resumed driving by 1 year.
Numerous barriers to driving resumption were cited by respondents. Lack of confidence was a highlighted factor. Respondents in this study often cited accompanied and local drives to rebuild confidence and enable return to driving. Intrinsic motivation was also key. Respondents wished to resume normal activities as soon as possible, with driving being a defining activity in people’s recovery and sense of self-worth. This echoes findings from previous research highlighting the desire to regain independence following critical illness. 12
Ability to perform an emergency stop is not included in any guidance or standards, however from our survey it appears to be used as a proxy by healthcare professionals and patients in determining readiness to resume driving. Only one respondent underwent a return to driving course, but this may be an avenue for survivors to explore to enable safe and timely resumption of this activity.
There is a clinical responsibility too that needs to be considered. As shown in our study, from whom, and how, these survivors gain their information about driving resumption is highly variable. Clinicians need to consider cognition, and especially the executive component of cognition, alongside the patient’s physical function which is often the primary focus. Medications may impair ability to drive. Current DVLA guidance acknowledges there is no single marker of impaired cognitive function relevant to driving and a comprehensive approach to assessment is required. 4 In cases where cognitive ability is difficult to determine, a further neuropsychiatric/psychological assessment may be needed or an in-car, on-road assessment.4,8 Recovery after critical illness clinics provide an suitable forum for return to driving discussions.
An unnecessary delay in driving resumption could impact the mental health of critical illness survivors, further impeding recovery. Isolation and depression have been noted in older adults who have experienced a similar loss of independence.13–16 Commentary from individuals in the public domain describe how in old age the car begins to represent life with feelings of freedom and normality being restored, even if only temporarily. 17 The nature of not being able to drive represents an unwelcome agonising change. 18 Frailty associated with critical care survivorship may mean that individuals of a lower age demographic may entertain similar thoughts and feelings.
Many individuals rely on driving as a means of accessing work and social support, especially in rural areas and communities. Approximately one million people in the UK and over three million people in the US are primarily employed as drivers or are required to drive as part of their job, reflecting the importance of driving after critical illness to the economy as well as individual financial stability.19,20
Driving enables resumption of other important activities alongside work. Critical illness survivors often have on-going health requirements and for ease of access a vehicle is frequently required. Accessing hobbies and leisure pursuits is vital for enhancing quality of life. 21 Driving enables parental and carer responsibilities often required of individuals in this demographic.
To our knowledge this is the first published study to explore the principal themes and metrics specific to driving after critical illness. Limitations of our study include the single-centre methodology which may not reflect the UK-wide or global picture. The qualitative data reflect only written textual responses and was gathered from open-ended questionnaires in a small, self-selected sample, and interviews may have yielded more in-depth data. However, similar studies using textual analysis have still yielded important implications for practice,11,22,23 as in our study. Clinical data about type/severity of critical illness or hospital length of stay following critical illness were not collected, nor was any involvement in trauma related to driving or road traffic accidents. It is recognised that varying lengths of hospital stay may have impacted on the results obtained. The questionnaire was not pilot tested or validated prior to use which would have helped improve design, clarity of the questions and reduced the risk of bias. Data from non-responders would have added insight into this topic and potentially influenced results. Strengths of our study include the high response rate and the wealth of qualitative data ascertained relative to survey length.
Conclusion
Significant time delay to driving resumption and numerous barriers associated with driving resumption were evident within this cohort of critical care survivors. Inconsistency of information received by respondents about driving resumption after critical illness in this study reflects lack of published guidance. Although the deleterious effects of a critical care stay are well documented 24 research about the impact these have on subsequent driving ability is lacking. The balance between avoiding unnecessary delay to driving resumption whilst averting premature return warrants further investigation. Reducing avoidable delay to driving where appropriate should be viewed as a low-cost high impact intervention to enhance health related quality of life. Further research is needed to understand the epidemiology, enablers and barriers to driving in this population.
Appendix
List of abbreviations
- DVLA –
Driver and Vehicle Licensing Agency
- GP –
General Practitioner
- ICU –
Intensive Care Unit
- NHS –
National Health Service
- PICS –
Post-intensive care syndrome
- UK –
United Kingdom
- US –
United States
Footnotes
Availability of data and material: The survey data that support the findings of this study are available from the corresponding author, (CA), upon reasonable request.
Authors contributions: JM, CW, NP and MG were responsible for study conception and design.
CA and JM were responsible for quantitative data analysis and interpretation.
NP and JM were responsible for qualitative data analysis and interpretation.
JM and CA prepared the manuscript.
All authors contributed to manuscript revision and approved the final version for submission.
JM acts as the guarantor for the intellectual integrity of the data.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval: The study was confirmed as service improvement that did not require ethical approval
Consent to participate: Informed consent was obtained from all individual respondents included in the study.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Chloe Apps https://orcid.org/0000-0002-4855-4243
References
- 1.Connolly B, O’Neill B, Salisbury L, et al. Physical rehabilitation interventions for adult patients during critical illness: an overview of systematic reviews. Thorax 2016; 71: 881–890. DOI: 10.1136/thoraxjnl-2015-208273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cuthbertson BH, Roughton S, Jenkinson D, et al. Quality of life in the five years after intensive care: a cohort study, 14. London, England: Critical care, 2010, pp. R6–R6. DOI: 10.1186/cc8848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herridge MS, Tansey CM, Matté A, et al. Functional disability 5 years after acute respiratory distress syndrome. New Engl J Med 2011; 364: 1293–1304. DOI: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 4.Driver and Vehicle Licensing Agency . Assessing Fitness to Drive: Guide for Medical Professionals, 2021, https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/965900/MIS828_interactive_020321_Final.pdf (accessed 22 March 2021). [Google Scholar]
- 5.Harvey MA, Davidson JE. Postintensive care syndrome: right care, right now…and laterand later. Crit Care Med 2016; 44: 381–385. [DOI] [PubMed] [Google Scholar]
- 6.National Highway Traffic Safety Administration and American Association of Motor Vehicles Administrators . Driver Fitness Medical Guidelines, 2009, https://www.aamva.org/At-Risk-Drivers/(accessed 25 April 2021). [Google Scholar]
- 7.Canadian Medical Association . Determining Medical Fitness to Operate Motor Vehicles. CMA Driver’s Guide, 2017, https://www.schulich.uwo.ca/geriatrics/docs/CMA_Drivers_Guide_9th_edition.pdf (accessed 22 April 2021). [Google Scholar]
- 8.Wolfe PL, Lehockey KA. Neuropsychological assessment of driving capacity. Arch Clin Neuropsychol 2016; 31: 517–529. DOI: 10.1093/arclin/acw050. [DOI] [PubMed] [Google Scholar]
- 9.Ritchie J, Spencer L. Qualitative data analysis for applied policy research by Jane Ritchie and Liz Spencer. In: Bryman A, Burgess RG. (eds). Analysing qualitative data. London: Routledge; 1994, pp. 173–194. [Google Scholar]
- 10.Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013; 13: 117. DOI: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiseman T, Lucas G, Sangha A, et al. Insights into the experiences of patients with cancer in London: framework analysis of free-text data from the National Cancer Patient Experience Survey 2012/2013 from the two London Integrated Cancer Systems. BMJ Open 2015; 5: e007792. DOI: 10.1136/bmjopen-2015-007792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ågård AS, Egerod I, Tønnesen E, et al. Struggling for independence: A grounded theory study on convalescence of ICU survivors 12 months post ICU discharge. Intensive Crit Care Nurs 2012; 28: 105–113, DOI: 10.1016/j.iccn.2012.01.008 10.1016/j.iccn.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Marottoli RA, de Leon CFM, Glass TA, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. J Am Geriatr Soc 1997; 45: 202–206, DOI: 10.1111/j.1532-5415.1997.tb04508.x 10.1111/j.1532-5415.1997.tb04508.x. [DOI] [PubMed] [Google Scholar]
- 14.Windsor TD, Anstey KJ, Butterworth P, et al. The role of perceived control in explaining depressive symptoms associated with driving cessation in a longitudinal study. The Gerontologist 2007; 47: 215–223. DOI: 10.1093/geront/47.2.215. [DOI] [PubMed] [Google Scholar]
- 15.Marottoli RA, de Leon CFM, Glass TA, et al. Consequences of driving cessation: decreased out-of-home activity levels. Journals Gerontol Ser B: Psychol Sci Soc Sci 2000; 55: S334–S340. DOI: 10.1093/geronb/55.6.S334. [DOI] [PubMed] [Google Scholar]
- 16.Mezuk B, Rebok GW. Social integration and social support among older adults following driving cessation. Journals Gerontol Ser B: Psychol Sci Soc Sci 2008; 63: S298–S303. DOI: 10.1093/geronb/63.5.S298. [DOI] [PubMed] [Google Scholar]
- 17.Athill D. Somewhere towards the End. New York: W. W. Norton, 2009. [Google Scholar]
- 18.Aronson L. Don’t ruin my life-aging and driving in the 21st century. New Engl J Med 2019; 380: 705–707. DOI: 10.1056/NEJMp1613342. [DOI] [PubMed] [Google Scholar]
- 19.Department for Transport . GB Driving Licence Data, https://data.gov.uk/dataset/d0be1ed2-9907-4ec4-b552-c048f6aec16a/gb-driving-licence-data (2019, (accessed 02 October 2019). [Google Scholar]
- 20.U.S Census Bureau . American Community Survey 2017, https://www.census.gov/data/tables/2017/demo/industry-occupation/truckers-acs17.html 2019, (accessed 8 January 2020). [Google Scholar]
- 21.Hashem MD, Nallagangula A, Nalamalapu S, et al. Patient outcomes after critical illness: a systematic review of qualitative studies following hospital discharge. Crit Care 2016; 20: 345. DOI: 10.1186/s13054-016-1516-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pattison N, O’Gara G, Wigmore T. Negotiating transitions: involvement of critical care outreach teams in end-of-life decision making. Am J Crit Care 2015; 24: 232–240. DOI: 10.4037/ajcc2015715. [DOI] [PubMed] [Google Scholar]
- 23.Miller SJ, Desai N, Pattison N, et al. Quality of transition to end-of-life care for cancer patients in the intensive care unit. Ann Intensive Care 2015; 5: 18. DOI: 10.1186/s13613-015-0059-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azoulay E, Vincent J-L, Angus DC, et al. Recovery after critical illness: putting the puzzle together-a consensus of 29. Crit Care 2017; 21: 296. DOI: 10.1186/s13054-017-1887-7dsm. [DOI] [PMC free article] [PubMed] [Google Scholar]