Abstract
Purpose:
This work analyzes data from a series of surveys developed by the American Society of Retina Specialists (ASRS) that assesses the impact of COVID-19 on physicians, their practices, and their patients.
Methods:
Five surveys were sent by the ASRS between March and July 2020 to more than 2600 US and international retina specialists. Data and trends from these surveys were analyzed.
Results:
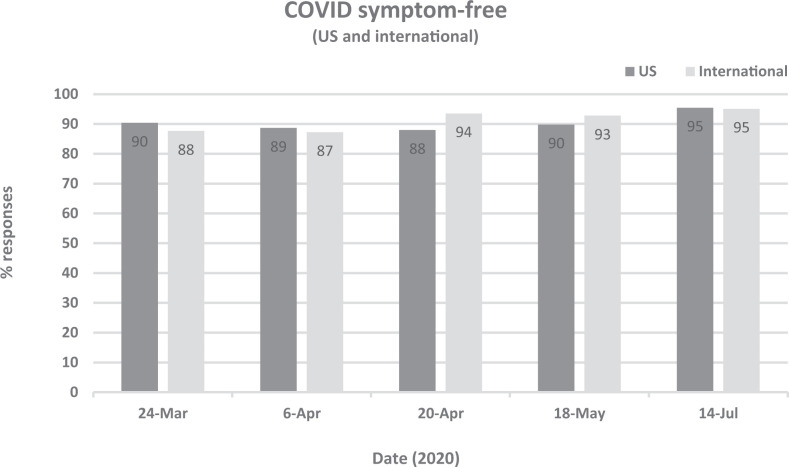
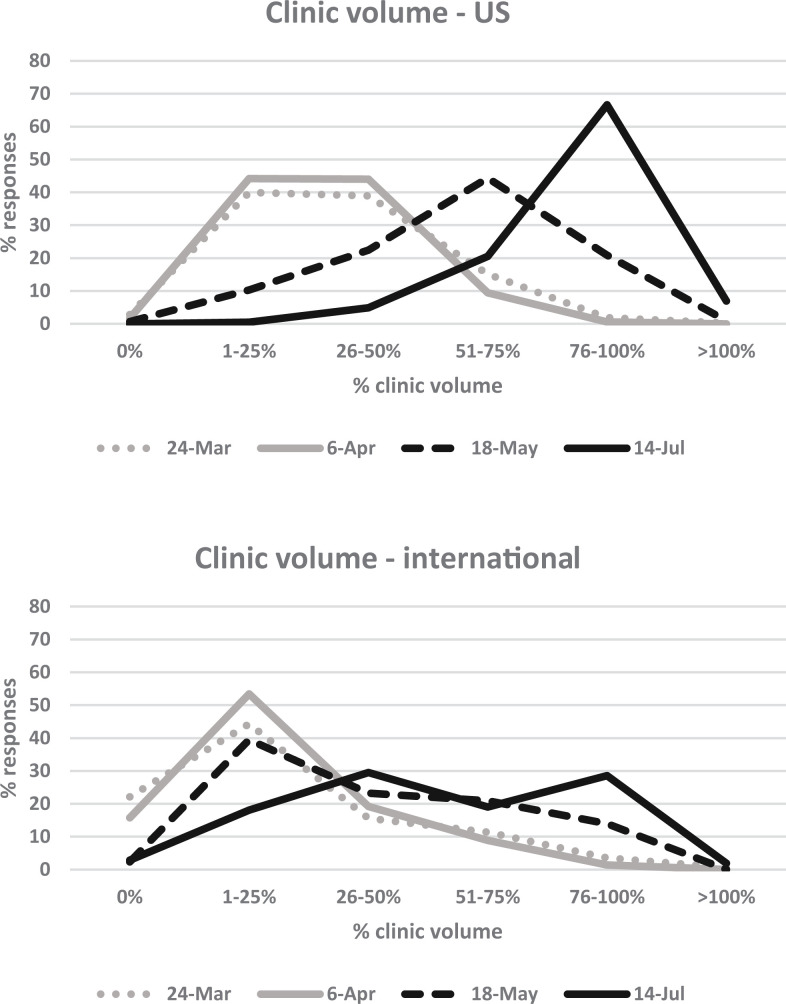
Most responding retina specialists (87%-95% in the United States and internationally) reported having no known COVID-related symptoms despite reported limitations in personal protective equipment. Clinic volumes globally were drastically reduced in March 2020 with only partial recovery through July 2020, which was slower internationally than in the United States. Practices were compelled to reduce staff and physician employment levels. Most respondents estimated some degree of delay in patient treatment with corresponding declines in vision and/or anatomy that were attributed most frequently to patients’ fears of the pandemic and least frequently to office unavailability.
Conclusions:
The reported impact of COVID-19 on retina specialists, their practices, and their patients has been substantial. Although retina specialists were quickly resilient in optimizing delivery of patient care in a manner safe for patients and providers, the reduction in clinic volume has been devastating in the United States and internationally, with negative impacts on patient outcomes, reductions in practices’ volume and employment, and risk to practices’ financial health. Future studies will be required to quantify losses associated with these unprecedented and ongoing circumstances caused by the pandemic.
Keywords: practice management, retina, socioeconomics
Introduction
In December 2019, a cluster of cases of “viral pneumonia…of unknown cause” was reported in Wuhan, China and was subsequently determined on January 9, 2020 to have been caused by a novel coronavirus. 1 Cases of COVID-19 quickly spread in Asia, then Europe, and then the United States with differential regional impact particularly early in the pandemic’s course. As COVID-19 cases continued to spread around the world, shifting regional hot spots characterized a waxing and waning but unremitting course still occurring through the present. The World Health Organization declared COVID-19 a pandemic March 11, 2020, and the United States declared COVID-19 a national emergency March 13, 2020. Stay-at-home orders, travel bans, closure of nonessential businesses and even medical services, pop-up field hospitals, forced triaging of limited hospital resources, and other measures quickly swept the world in an effort to slow the impact of the pandemic, but by the end of 2020, the World Health Organization reported more than 79 million cases and more than 1.7 million deaths worldwide, 2 including approximately 20 million cases and 345 000 deaths reported in the United States by the Centers for Disease Control and Prevention. 3
The profound global impact caused by this pandemic had not been seen in more than a century. Shortly after the onset of the pandemic in the United States, the American Society of Retina Specialists (ASRS) developed a series of online surveys that was sent to retina specialists in the United States and internationally. These surveys were not designed for research purposes but rather as a means to share experiences and practice patterns among ASRS members in a time of rapid change and uncertainty. Nonetheless, these surveys serve as a gauge of the impact of COVID-19 on providers, practices, and patients and document behavior and attitude changes. In an effort to memorialize these unique circumstances, this report highlights some of the key findings extracted from these surveys.
Methods
A series of 5 COVID-19–related surveys were developed by the ASRS and emailed to all 2684 to 2822 ASRS members, consisting of 2085 to 2213 US and 599 to 609 international retina specialists (there was a slight fluctuation in membership during the survey period). Each survey had an open window for voluntary submission of responses ranging from 5 to 7 days. Survey 1 was open from March 23, 2020, through March 29, 2020; survey 2 was open from April 6, 2020, through April 11, 2020; survey 3 was open from April 20, 2020, through April 25, 2020; survey 4 was open from May 18, 2020, through May 25, 2020; and survey 5 was open from July 14, 2020, through July 20, 2020. In the design of these serial surveys, key questions were repeated to assess for trends in responses.
Deidentified survey results were shared with the ASRS membership shortly after the closing of each survey (www.asrs.org; Supplemental Material 1-5). Responses were divided into US and international responses based on self-reporting of practice location. For surveys 2 and 3, an additional subdivision of US members’ responses was created based on self-identification of a practice location in a “hot spot” of COVID-19 activity, and survey results were communicated to ASRS members with this subdivision (see Supplemental Material 2-3).
For the purposes of this analysis, US and international responses were presented separately. Except when indicated, US hot spot and US non–hot spot divisions have been removed, and the 2 groups have been aggregated into total US responses. Some of the key findings felt to be of interest by the authors were extracted from the surveys for analysis. Trending data across time were plotted using Excel (version 16.46, Microsoft).
Results
Survey Responses
Each survey was sent to all US and international ASRS members. In survey 1, there were 1037 total respondents (39% overall response rate); 83% of responses were from the United States (41% response rate), and 17% were international (29% response rate). In survey 2, there were 811 total respondents (30% overall response rate); 82% of responses were from the United States (32% response rate), and 18% were international (25% response rate). In survey 3, there were 661 respondents (24% overall response rate); 86% of responses were from the United States (26% response rate), and 14% were international (16% response rate). In survey 4, there were 533 respondents (20% overall response rate); 83% of responses were from the United States (21% response rate), and 17% were international (14% response rate). In survey 5, there were 534 respondents (20% response rate); 80% of responses were from the United States (20% response rate), and 20% were international (17% response rate).
Following completion of the 5 surveys, the responses were reviewed by the authors who identified questions related to impact on physicians, practices, and patients. The full survey results are included for review (see Supplemental Material 1-5), and the following summarizes the findings of select questions relevant to these categories.
Impact on Physicians
Disease exposure
In each of the 5 surveys, a question assessing COVID-19–related personal exposure (“Which best describes your personal experience with COVID-19?”) was repeated. Responding retina specialists remained generally symptom free during the pandemic, with a range across each of the 5 surveys of 88% to 95% US and 87% to 95% international respondents indicating that they did not have any known COVID-19–related symptoms (Figure 1). In the first 4 surveys, the answer choices assessed symptoms (see Figure 1), positive contacts, quarantining, and hospitalization over the preceding 2-week interval (see Supplemental Material 1-4), while the fifth survey removed the time stipulation (see Supplemental Material 5). In July 2020 at the time of survey 5, 0.48% of responding retina specialists in the United States and 0% internationally reported being hospitalized because of COVID-19.
Figure 1.
Responding retina specialists in the United States and internationally remained largely symptom free during the pandemic across all 5 surveys.
Physician risk assessment
A single question in survey 2 in early April 2020 assessed whether responding retina specialists were in a “higher-risk group,” which was defined within the survey question as “age >60 [years] and/or with immune suppression, diabetes or other comorbidities.” Of the responding retina specialists, 29% US and 26% international respondents indicated they were in a higher-risk group. Of these higher-risk respondents, 90% in the United States (84% internationally) reported continuation of patient care at that time. The remaining group of non–higher-risk retina specialists consisted of 71% US and 74% international respondents. Of these non–higher-risk respondents, 97% US and 78% international pollees reported continuation of patient care at the time of survey 2.
Personal protective equipment
A series of different questions throughout the surveys assessed availability and use of personal protective equipment (PPE). At the time of survey 1 at the end of March 2020, US and international respondents reported incomplete availability of appropriate PPE to examine “one high-risk patient in your office,” including “N95 (or comparable tight-fitting) masks” (available for only 52% of either the US or international group); “surgical (or similar loose-fitting) masks” (available for 56% US, 51% international); “goggles (or face shield, etc)” (available for 43% US, 64% international); “gown” (available for 27% US, 48% international); and “gloves” (available for 80% US, 82% international).
By survey 4 in July 2020, a modified question assessed the availability of “an adequate supply of appropriate PPE” and identified improved availability, with “an adequate supply” reported in 86% US and 87% international respondents; this survey 4 question did not query the specific PPE elements as in survey 1. However, a substantial percentage of respondents (14% US and 13% international) reported not having an adequate supply of PPE in July 2020.
Face mask use by retina specialists and patients increased during the pandemic. Mask uptake by retina specialists was swift. At the time of survey 1 at the end of March 2020, 77% of US and 89% international respondents reported wearing a mask for routine patient care (ie, for “most asymptomatic [non–high-risk patients]”). When the same question was repeated just 2 weeks later in early April 2020 during survey 2, 96% of US and 95% international respondents reported wearing a mask for routine patient care.
Regarding masks for asymptomatic patients, at the time of survey 1 at the end of March 2020, only 8% US but 39% international respondents reported that all patients were asked to wear masks. Four weeks later, at the end of April 2020 in survey 3, 79% US and 77% international respondents reported that all patients were asked to wear masks. Of note, analysis of responses in survey 3 by self-reported hot spot locations in the United States identified that 84% of US hot spot respondents mandated patient mask use in contrast to 68% of US non–hot spot respondents. At the time of survey 5 in July 2020, a variation of this survey question was posed, inquiring about mask use for patients undergoing intravitreal injection, and 95% US and 94% international respondents reported masking all patients given an injection (these response rates were extrapolated by counting only those who responded whether “all” or “not all” patients administered an injection were masked).
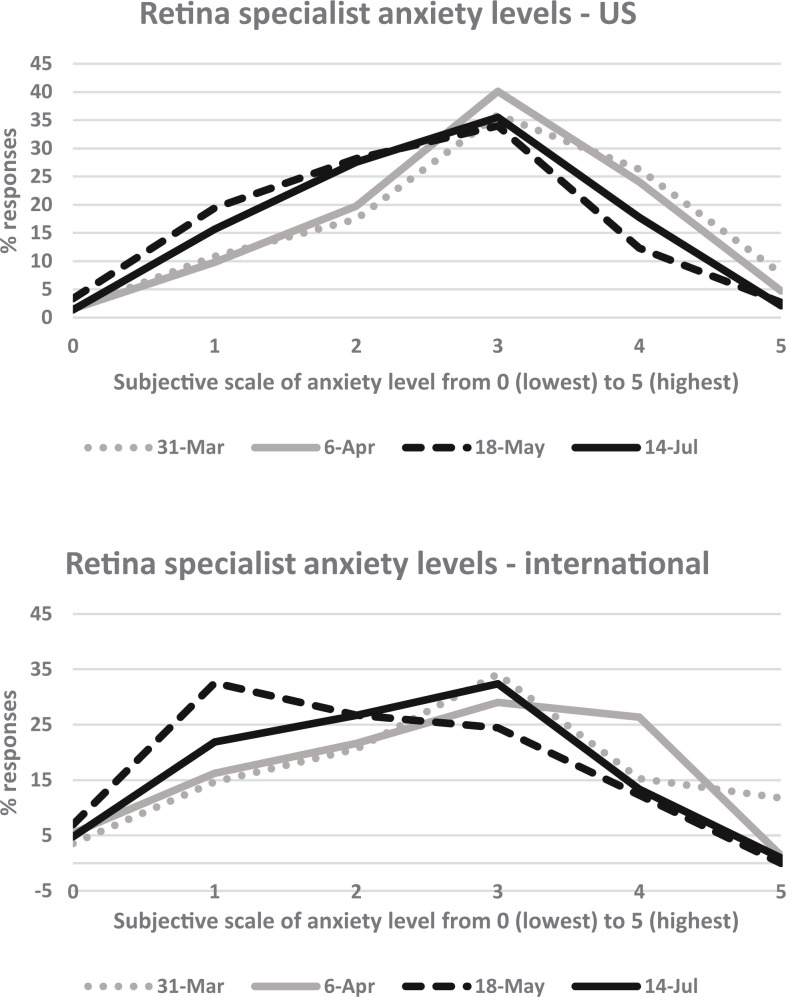
Well-being/anxiety
Anxiety levels during the pandemic in responding retina specialists were assessed with a question repeated in surveys 1, 2, 4, and 5 (“On a scale of 0 [no anxiety] to 5 [extremely anxious], how would you rate your current overall concern/psyche as it relates to the pandemic?”). Anxiety remained consistently elevated in the United States and internationally (Figure 2). In the United States, anxiety levels were highest at the time of survey 1 at the end of March 2020, with only slight improvement in consistently elevated levels by July 2020 at the time of survey 5. Internationally, anxiety levels were also elevated by the end of March 2020 according to survey 1; unlike in the United States, there appears to have been a significant but transient improvement internationally seen in May 2020 (survey 4) but with a worsening return to elevated anxiety levels by July 2020 (survey 5).
Figure 2.
Self-reported subjective anxiety levels in US and international retina specialists remained elevated. In the United States, there was a slight improvement in anxiety over time. Internationally, elevated anxiety appeared to transiently relax in mid-May with a return to elevated levels by July.
Impact on Practices
Clinic volume
A question assessing clinic volume was repeated in surveys 1, 2, 4, and 5 (“What percent of your normal [pre–COVID-19] patient volume is your practice [in its entirety] currently seeing?”). Both in the United States and internationally, significant reductions in clinic volume were reported (Figure 3). In the United States at the end of March 2020 (survey 1), 82% of respondents reported 50% volume or less compared with “normal (pre-COVID)” levels, and only 2% of US respondents reported clinic volumes at 76% to 100%. Similar findings were reported 2 weeks later in early April 2020 (survey 2). There was a steady recovery in US clinic volume in May 2020 (survey 4) into July 2020 (survey 5). By July 2020 (survey 5), US clinic volumes had returned to 76% to 100% in 67% of respondents and more than 100% for 7%, although 26% of US respondents still reported 75% volume or less by July 2020.
Figure 3.
Clinic volumes globally were drastically reduced in March 2020, with gradual but incomplete recovery through July 2020 that was slower internationally than in the United States.
International clinic volumes also saw profound declines. At the end of March 2020 (survey 1), 82% of international respondents reported 50% volume or less compared with “normal (pre-COVID)” levels, and only 4% of international respondents indicated clinic volumes at 76% to 100%. Similar findings were reported 2 weeks later in early April 2020 (survey 2). International recovery appears to have been slower than in the United States, and by July 2020 (survey 5), international clinic volumes had returned to 76% to 100% in only 29% and more than 100% for only 2%; the majority (70%) of international respondents still experienced 75% clinic volume or less in July 2020.
Staff reductions
A single question in survey 3 at the end of April 2020 assessed reductions in staff employment. Among respondents, 39% US and 39% international retina specialists reported their practices “have or are about to reduce staff (eg, layoffs, furloughs, etc).” In the same survey question, 40% US and 40% international respondents reported they have “not reduced number of staff, but we have reduced employee hours.”
Physician reductions
A question in survey 4 in May 2020 assessed reductions in physician employment. Among respondents, 11% US and 15% international retina specialists indicated they “have or are about to reduce the number of current physicians (eg, layoffs, furloughs, etc),” and 2% US and 4% international respondents indicated they “have or are about to rescind job offers for incoming physicians.” In the same survey question, 6% US and 11% international respondents “have not reduced physician employment but are considering it.” The remaining respondents (82% US, 72% international) in survey 4 reported no plans for physician employment reductions at that time.
US federal relief program participation
A question in survey 4 in May 2020 assessed participation in US federal relief programs. US respondents reported applying for multiple federal relief programs including the Payroll Protection Program (74% of US respondents), the Medicare Advanced Payment Program (27%), and the Emergency Disaster Loan (9%). Of the US respondents who knew about their practices’ plans to attest to Provider Relief Funds (64% knew and 36% did not know), 93% reported their practice would attest. Because these programs are US specific, international responses are not reported here.
Practices’ financial health predictions
A question in survey 3 at the end of April 2020 assessed retina specialists’ predictions for their practice’s financial health “in the absence of substantive federal grants or loans.” Among respondents, 36% US and 58% international retina specialists predicted their practices would be “financially unhealthy” by year end of 2020 under those circumstances. In the same survey question, 60% US and 58% international respondents predicted their practices would be “smaller than pre-COVID size and volume” by year-end of 2020.
Telemedicine participation
Participation in telemedicine was assessed in survey 4 in May 2020. Among respondents, 72% US and 69% international retina specialists reported they “have not recently videoconferenced with any patients to discuss their ocular health.” Fewer respondents (23% US, 25% international) reported “videoconferencing with some patients,” and a smaller number (5% US, 6% international) reported “offering hybrid visits (in-office imaging followed by a remote videoconferencing visit).”
Impact on Patients
Delay in treatment
Retina specialists were surveyed with a question in July 2020 (survey 5) to estimate the length of COVID-19–related delays in patient treatment “despite your office’s recommendation to be seen.” A small number of respondents (2% US, 5% international) reported that no patients experienced such delays. For the remaining patients who were delayed, the average “delay from original scheduled visit until actual visit” for these “patients requiring treatment” was estimated as 1 to 2 months by 46% US and 38% international respondents and 2 to 3 months by 33% US and 37% international respondents. A few reported longer average delays of more than 3 months (6% US, 8% international), and some reported shorter delays of less than 1 month (13% US, 12% international).
Reasons for treatment delay
A question in survey 5 in July 2020 also surveyed reasons, in rank order, for delay of the previously mentioned patients requiring treatment. The highest ranked reason for delay was “patients scared to come/were fearful of contracting COVID-19,” with 86% US and 78% international respondents indicating this was the most significant factor. In the United States and internationally, the remaining responses in rank order were: “patients reside in nursing homes and unable to leave”; “patients did not have transportation”; “patients urged not to by other physicians”; “my office did not have availability”; and “no patients experienced a delay in treatment.”
Vision/anatomy impact
A question in survey 5 in July 2020 surveyed retina specialists to estimate the rate of “a significant decline in visual acuity and/or anatomical function” in patients whose treatment was delayed. Only 3% US and 4% international respondents indicated “no patients experienced a delay in treatment.” The majority of respondents (44% US, 53% international) estimated a significant decline in visual acuity or anatomy to be found in the lowest percentage quartile (1%-25%) of patients whose treatment was delayed. The rate of such significant decline was estimated to be 26% to 50% of patients by 37% US and 30% international respondents; a significant decline was estimated in 51% to 75% of patients by 12% US and 10% international respondents; and a significant decline was estimated in 76% to 100% of patients by 4% US and 3% international respondents.
Conclusions
In a time of rapid, unprecedented, and unpredictable change caused by a sweeping global pandemic, these serial surveys developed by the ASRS help assess the impact of these changes on the retina community. Analysis of these survey data highlights several key themes. First, physicians’ well-being was adversely affected by elevated anxiety levels throughout the survey period. Although not surprising given the pandemic’s circumstances that undoubtedly affected every individual, there are good reasons to predict that anxiety levels of retina specialists might have been particularly increased. Early in the pandemic, evidence emerged indicating transmission of disease through ocular fluids, 4 and the COVID-19–related death in February 2020 of Dr Wenliang Li, a Chinese ophthalmologist who was one of the first to recognize the outbreak of COVID-19, was publicly mourned worldwide. 5
In the setting of these exposure risks, PPE availability remained limited universally, including for retina specialists as demonstrated by the surveys. At the end of March 2020, early in the pandemic, many retina specialists in the United States and internationally reported not having adequate PPE to see a single high-risk patient, and even months later, by July 2020, more than 10% in the United States and internationally reported not having an adequate supply of appropriate PPE.
A second and related key theme is that despite this heightened anxiety, retina specialists globally prioritized the well-being of their patients and their patients’ vision. Despite more than 1 in 4 respondents being in a higher-risk group, the majority of retina specialists—higher risk as well as non-higher risk—reported continuing to see patients during very uncertain times in an early peak of the pandemic.
Telemedicine options were developed for continuation of health care delivery in these pandemic circumstances, and in the second quarter (April-June) of 2020, telemedicine visits for primary care consisted of 35.3% of visits. 6 However, given the nature of diagnosis, care, and treatment of retinal diseases, in-office and in-person management was likely required. Approximately 70% of US and international respondents did not participate in telemedicine, and although the volume of telemedicine visits by the remaining retina specialists was not specifically queried, we assume that telemedicine was a minor component of their overall practices. Consistent with this, a study of US insurance claims data revealed that telehealth visits accounted for only 1.6% of ophthalmic encounters from March 15, 2020, through September 1, 2020, and even at its peak during the week from April 5, 2020, through April 11, 2020, telehealth accounted for only 17.0% of ophthalmic encounters, the majority of which were related to cornea and external disease diagnoses. 7
Third, in the setting of continued dedication to patient care despite increased anxiety, increased exposure risk, and limited PPE and resources, most responding retina specialists remained largely symptom free. In the United States and internationally, 87% to 95% of respondents did not report having any known COVID-19–related symptoms in each of the 5 surveys from March through July 2020. In the final survey in July 2020, less than 1% of US respondents and 0% international respondents reported being hospitalized from COVID-19. Maintaining safety among retina specialists themselves and their patients highlights the resilience and resourcefulness of a collaborative retina community. Despite limited PPE availability, mask use for physicians and patients was high. Novel adaptations, such as shields for a slitlamp or indirect ophthalmoscope, were developed to increase the safety of patient encounters. An international dialog quickly commenced to define best practices through various institutions and organizations, including the ASRS, to optimize patient care and safety. 8 -10
Fourth, despite the resourcefulness and resilience of retina specialists, the negative impact of the pandemic has unquestionably been high. The toll on physicians' well-being was discussed earlier. Although the majority of responding retina specialists did not report any known COVID-19 symptoms, the remaining 5% to 13% in the United States and internationally may have been afflicted by COVID-19. It is not clear based on the survey results what proportion of illness by retina specialists could have been attributed to exposure during patient care.
Clinic volumes were drastically reduced with more than 80% of US and international respondents reporting 50% volume or less at the end of March 2020. Persistent reductions were seen through the last survey in July 2020, particularly internationally, where recovery was markedly slower. In contrast to, for example, primary care, where a 50.2% reduction in in-office visits was offset by an increase in telemedicine visits to a net decrease of only 21.4% of encounters in the second quarter of 2020, 6 it is likely that the impact on retina practice volume was higher in the absence of a significant telemedicine contribution. Consistent with this loss in clinic volume and therefore revenue, retina practices have been forced to make reductions in staff employment and even unprecedented reductions in physician employment. A large number of respondents predicted their practices would be financially unhealthy and/or smaller in size by the end of 2020 in the absence of substantive federal support.
These surveys only briefly explored impact on patients. Most responding retina specialists estimated some form of delay in treatment for patients, although there was variability in responses predicting the extent of associated visual or anatomic decline. Notably, the most reported reason for delay was patients’ fear of the pandemic, and the least reported reason was availability of the retina specialist.
The full impact of this ongoing pandemic will not be realized in the near future. Further studies defining COVID-19–related shifts to physicians, practices, and patients with analysis of objective data will clearly be important. Early studies have already begun to define visual and anatomic loss in patients who were delayed in receiving intravitreal injections because of the pandemic. 11 -14
This study is limited by inherent weaknesses of survey data. These surveys were not formulated for research purposes but rather for communication of experiences and practice patterns among the ASRS membership during rapidly changing and uncertain times. Responses for this survey were anonymous, which limits longitudinal analysis of individual responses. This study examined responses to questions that were felt by the authors to be of interest to the retina community. These questions were selected post hoc and do not represent the extensive information captured by the surveys in their entirety.
This analysis was divided by location to identify differences in responses in the United States and internationally. Different regions in the United States and internationally have maintained different tempos of pandemic activity with likely significant variability in different international and even intra-US locations. In surveys 2 and 3, US responses were analyzed by self-reporting of location as a “hot spot” or “non–hot spot” (see Supplemental Material 2 and 3). Beyond this, further specificity regarding the location and extent of local COVID-19 activity was not captured by the survey and therefore could not be reflected in this analysis. Similarly, other demographic data, such as practice type, were not queried in these surveys and therefore could not be included in this analysis. The impact of COVID-19 may have been differentially affected by location and practice type, 15 among other reasons, and generalization of results simply by US vs internationally likely underestimates more profound effects that may have been seen locally or in different practice settings.
Surveys are also limited by biases. Our surveys captured self-reported perceptions at the time of each response and are subject to such response bias. Although the ASRS is an open society and therefore the largest and most representative society of retina specialists in the world, sampling bias may exist, as surveys were sent only to retina specialists who were ASRS members at the time of the survey. Along the same lines, the surveys were drafted by the ASRS, and the questions and answer choices may reflect associated wording bias. Similarly, in this report, the selection of questions to be included in the analysis may reflect biases of the authors.
Despite a high overall response rate across all surveys, nonresponse bias in which the population of those responding vs not responding may be systematically different is unavoidable, and the decreasing numbers of respondents for successive surveys in this series may suggest progressive nonresponse bias. For example, although the survey results indicate that most responding retina specialists remained symptom free and that very few were hospitalized, it is possible that those with symptoms, particularly those more severely affected, may not have been in a position to respond to the surveys.
Despite these limitations, such survey data effectively memorialize the reported impact of the COVID-19 pandemic on retina specialists, their practices, and their patients. Health care workers have been among the true heroes in these crisis times, and retina specialists have continually served on the front line to maintain their patients’ vision. The impact of the COVID-19 pandemic on patient outcomes is currently being explored, and the toll on retina specialists and their practices appears to have been disproportionately high. Ongoing support by communities and governments will be important to maintain the ability of retina specialists, and all health care workers, to serve their patients as the world develops strategies to cope with these unprecedented circumstances.
Supplemental Material
Supplemental Material, sj-docx-1-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-2-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-3-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-4-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-5-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Footnotes
Ethical Approval: Ethical approval or institutional review board oversight was not sought for the present study because this study did not involve human participants.
Statement of Informed Consent: This study did not involve human participants, and informed consent was not obtained.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: P.H.: ASRS (board of directors), Alimera (consultant, honoraria), DORC International (consultant, lecture fees), and Genentech (consultant, honoraria, lecture fees), J.F.B.: ASRS (executive vice president; employee); K.P.: none; J.M.J.: ASRS (board of directors) and DORC International (consultant, lecture fees); T.M.: ASRS (board of directors) and Alcon Surgical (FDA Committee); and C.C.A.: ASRS (board of directors), Adverum Biotechnologies Inc (investigator, grants), Allergan (advisory board, honoraria), Apellis Pharmaceuticals (investigator, grants), ArcticDX (consultant, stockholder, stock), Bausch + Lomb (consultant, honoraria), Chengdu Kanghong Biotechnology Co (consultant, honoraria), Genentech (consultant, investigator, grants, honoraria), Glaxo Smith Kline (investigator, grants), Hoffman-La Roche (investigator, grants), Katalyst Surgical (consultant, stockholder, royalty, stock), Kodiak Sciences (investigator, grants), Merck & Co (investigator, grants), Ophthotech/Iveric Bio (investigator, grants), Panoptica (investigator, grants), Regeneron (investigator, grants), Stealth Biotherapeutics (investigator, grants), and Volk Optical (consultant, honoraria).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The surveys that form the basis for the research were funded by the ASRS.
ORCID iD: Timothy Murray, MD, MBA  https://orcid.org/0000-0002-1974-2536
https://orcid.org/0000-0002-1974-2536
Supplemental Material: Supplemental material is available online with this article.
References
- 1. World Health Organization. Listing of WHO’s response to COVID-19. June 29, 2020. Updated December 28, 2020. Accessed August 2, 2021. https://www.who.int/news/item/29-06-2020-covidtimeline
- 2. World Health Organization. Weekly epidemiological update. December 29, 2020. Accessed August 2, 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update- - -29-december-2020
- 3. Centers for Disease Control and Prevention. COVID Data Tracker. December 31, 2020. Accessed August 2, 2021. https://covid.cdc.gov/covid-data-tracker/#trends_totalandratecasestotalrate
- 4. Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138(5):575–578. doi:10.1001/jamaophthalmol.2020.1291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Parrish RK II, Stewart MW, Duncan Powers SL. Ophthalmologists are more than eye doctors—in memoriam Li Wenliang. Am J Ophthalmol. 2020;213:A1–A2. doi:10.1016/j.ajo.2020.02.014 32169251 [Google Scholar]
- 6. Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and content of primary care office-based vs telemedicine care visits during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(10):e2021476. doi:10.1001/jamanetworkopen.2020.21476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Portney DS, Zhu Z, Chen EM, et al. COVID-19 and utilization of teleophthalmology: trends and diagnoses (CUT Group). Ophthalmology. 2021;S0161-6420(21)00118-4. doi:10.1016/j.ophtha.2021.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schultheis WG, Sharpe JE, Zhang Q, et al. Effect of taping face masks on quantitative particle counts near the eye: implications for intravitreal injections in the COVID-19 era. Am J Ophthalmol. 2021;225:166–171. doi:10.1016/j.ajo.2021.01.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Korobelnik JF, Loewenstein A, Eldem B, et al. Anti-VEGF intravitreal injections in the era of COVID-19: responding to different levels of epidemic pressure. Graefes Arch Clin Exp Ophthalmol. 2021;259(3):567–574. doi:10.1007/s00417-021-05097-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chao DL, Sridhar J, Kuriyan AE, et al. Rationale for American Society of Retina Specialists best practice recommendations for conducting vitreoretinal surgery during the coronavirus disease-19 era. J Vitreoretin Dis. 2020;4(5):420–429. doi:10.1177/2474126420941707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Song W, Singh RP, Rachitskaya AV. The effect of delay in care among patients requiring intravitreal injections. Ophthalmol Retina. 2021;S2468-6530(20)30507-8. doi:10.1016/j.oret.2020.12.020 [DOI] [PubMed] [Google Scholar]
- 12. Ashkenazy N, Goduni L, Smiddy WE. Short-term effects of COVID-19-related deferral of intravitreal injection visits. Clin Ophthalmol. 2021;315:413–417. doi:10.2147/OPTH.S296345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Naravane AV, Mundae R, Zhou Y, et al. Short term visual and structural outcomes of anti-vascular endothelial growth factor (anti-VEGF) treatment delay during the first COVID-19 wave: a pilot study. PLoS One. 2021;16(2):e0247161. doi:10.1371/journal.pone.0247161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kovacs KD, Gonzales LA, Mahrous MA, et al. Choroidal neovascularization and macular hemorrhage: real-world experience during the New York City COVID-19 lockdown. J Vitreoretin Dis. Published online February 24, 2021. doi:10.1177/2474126421993664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. El Hamichi S, Gold A, Heier J, Kiss S, Murray TG. Impact of the COVID-19 pandemic on essential vitreoretinal care with three epicenters in the United States. Clin Ophthalmol. 2020;14:2593–2598. doi:10.2147/OPTH.S267950 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-2-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-3-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-4-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases
Supplemental Material, sj-docx-5-vrd-10.1177_24741264211034112 for The Impact of COVID-19 on US and International Retina Specialists, Their Practices, and Their Patients by Paul Hahn, Jill F. Blim, Kirk Packo, J. Michael Jumper, Timothy Murray and Carl C. Awh in Journal of VitreoRetinal Diseases