Abstract
Purpose:
This study compares visual acuity (VA), anatomic outcomes, and complications in eyes that underwent complex retinal detachment (RD) repair in which silicone oil (SO) was retained vs removed.
Methods:
A retrospective chart review of patients undergoing vitrectomy with SO tamponade. The eyes were divided into 2 groups based upon SO removal or retention. Main outcome measures were corrected VA, anatomic outcomes, and the presence of SO-related complications.
Results:
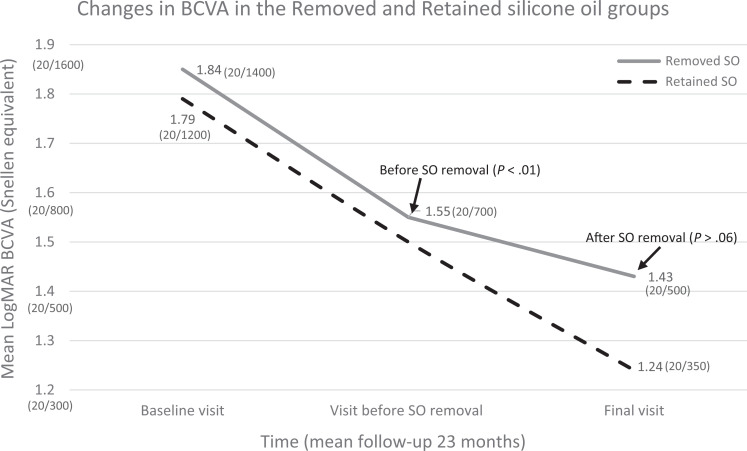
Fifty-seven eyes with removed SO and 53 eyes with retained SO were identified. In both groups, the mean best-corrected VA (BCVA) at the final visit was significantly better than at baseline. In the retained-SO group, vision improved from 1.79 ± 0.6 to 1.2 ± 0.7 logarithm of the minimum angle of resolution (logMAR) (Snellen, 20/1200 to 20/350) at the final visit (P < .001). In the removed-SO group, mean BCVA improved from 1.84 ± 0.5 at baseline to 1.55 ± 0.6 logMAR units (Snellen, 20/1400 to 20/700) at the visit preceding SO removal (P < .002) and to 1.43 ± 0.6 logMAR units (Snellen, 20/500) at the final visit (P < .001). Complication rates were similar in both groups, apart from RD, which occurred more frequently in the removed-SO group (P = .03).
Conclusions:
There was similarity in VA and complications among patients with removed or retained SO. Removal of SO may benefit eyes with SO-related complications, but SO retention may decrease the chance of RD and may be indicated in selected cases.
Keywords: retinal detachment, silicone oil, silicone oil removal, silicone oil retention, vitreoretinal surgery
Introduction
For decades, silicone oil (SO) has been successfully used by retina surgeons in the management of retinal detachment (RD). 1 SO tamponade is a standard technique for complex rhegmatogenous RD with proliferative vitreoretinopathy (PVR), diabetic tractional RD, and RD associated with giant retinal tears and penetrating trauma. 2
However, the use of SO in retinal surgery is known to have complications. Glaucoma, cataract, and keratopathy as well as other, less-common side effects have been described. 3,4 For these reasons, many surgeons plan for SO removal, usually within 6 months. However, if complications are noted, removal of SO may be carried out sooner. 2 Potential improvement of visual acuity (VA) may also serve as an additional motivation for early or routine SO removal. 5 Nevertheless, removal of SO from eyes with complex RD may result in complications such as retinal redetachment, hypotony, and intraocular hemorrhage. In addition, some complications attributed to the presence of the SO, including keratopathy and glaucoma, may still develop even after SO is removed. 5,6
There is no clear consensus among surgeons regarding the continued management of these high-risk eyes. The controversy regarding the decision and the timing of SO removal in complex RD patients prompted us to study the clinical outcomes associated with SO tamponade. This study of patients with complex RD with SO tamponade was undertaken to compare VA, anatomical outcomes, and complications in eyes with retained SO to outcomes for eyes from which SO was removed.
Methods
This was a retrospective comparative study. We were granted permission by the institutional review board at the University of Louisville to review existing medical records of patients who had pars plana vitrectomy and SO injection between October 2014 and June 2017. Exclusion criteria included follow-up of less than 6 months after SO-injection surgery and follow-up of less than 3 months after SO-removal surgery. Eyes that underwent previous glaucoma surgery were also excluded. Eyes were separated into 2 groups: eyes with retained SO and eyes with removed SO. The two groups were compared.
Demographic information collected included age, sex, and ethnicity. The indication for SO injection, duration of SO tamponade, best-corrected Snellen VA (BCVA), intraocular pressure (IOP), status of intraocular SO (eg, emulsification of the oil or its migration to the anterior chamber), corneal clarity, lens status, and findings of the dilated fundus examination were recorded.
Measurements of IOP by Goldman tonometry at the first visit and at the last visit were considered the patient’s baseline IOP and final IOP, respectively. High or elevated IOP was defined as IOP greater than 25 mm Hg, and hypotony was defined as IOP less than or equal to 5 mm Hg. We used the term keratopathy to encompass band keratopathy, epithelial or stromal edema, or localized corneal opacities. Glaucoma was diagnosed if characteristic optic nerve or visual field abnormalities were documented. Values of BCVA were converted to logarithm of the minimum angle of resolution equivalent units (logMAR) for the purpose of statistical calculations. Based on the Freiburg Visual Acuity Test, logMAR equivalent values for “counting fingers” and “hand motion” acuities were assumed to be +1.85 and +2.3, respectively. 7 Eyes with light perception or no light perception vision were not included in VA calculations. BCVA was achieved using refraction.
All patients had undergone a complete vitrectomy using a wide-angle viewing system followed by SO injection. Shaving of the vitreous base was attempted in all eyes. Detachment of the posterior hyaloid face was performed if it was not already detached. In some cases, triamcinolone acetonide was used to improve visualization of the vitreous. Viscosities for SO of 5000 and 1000 centistokes were used according to the surgeon’s preference, and all eyes received 360° of prophylactic laser retinopexy. Some eyes had cataract extraction at the time of the primary vitrectomy surgery whether by phacoemulsification or by pars plana lensectomy and were considered pseudophakic or aphakic in the data analysis. Anatomical success was defined as complete retinal attachment throughout the follow-up period. SO removal included air–fluid exchange in all cases.
Statistics
Statistical evaluations were performed using Microsoft Excel 2013 (Microsoft). Fisher exact test was used to compare categorical data. The two-tailed Student t test was used for the analysis of the continuous variables. A P value less than .05 was considered statistically significant.
Results
A total of 136 patients who had undergone PPV with SO tamponade were identified. Seventy-three patients had also undergone SO-removal surgery and 63 patients retained their SO. Sixteen patients from the removed-SO group and 10 patients from the retained-SO group were excluded (P = .53) because they met the exclusion criteria or had incomplete medical records. Fifty-seven (52%) eyes remained in the removed-SO group, and there were 53 (48%) eyes in the retained-SO group.
The demographic characteristics of the patients are shown in Table 1. There were no statistically significant differences between the groups with respect to any of the demographic features. The mean time for SO removal was 10 ± 10 months (range, 10 days-72 months). The follow-up post-SO removal was 12.1 ± 11.7 months (range, 3-60 months), and the mean follow-up time for all eyes was 23 ± 20 months (range, 6-126 months). The indications for the use of SO included rhegmatogenous RD with PVR (56 eyes, 51%); tractional RD with proliferative diabetic retinopathy (PDR) (31 eyes, 28%); penetrating ocular injury with RD (11 eyes, 10%); RD associated with giant retinal tears (4 eyes, 4%); tractional RD associated with retinopathy of prematurity (2 eyes, 2%); and conditions such as chorioretinal coloboma, choroidal effusion, and keratoprosthesis groups in the frequency of SO removal vs SO retention with respect to any of these groups (Table 2).
Table 1.
Demographic Characteristics of Patients.
| Parameter | Removed SO | Retained SO | P Value (Removed vs Retained) |
|---|---|---|---|
| No. (%) | 57 (52) | 53 (48) | |
| Follow-up range (mean, SD), mo | 6-77 (22, 16) | 6-126 (23, 23) | .796 |
| Age range (mean, SD), y | 9-87 (54, 17) | 11-88 (57, 17) | .429 |
| Sex, n (%) | 31 male (54) | 25 male (48) | .349 |
| Ethnicity | |||
| White, n (%) | 32 (56) | 21 (40) | .090 |
| Middle Eastern, n (%) | 17 (32) | 23 (43) | .167 |
| African American, n (%) | 8 (12) | 9 (17) | .793 |
Abbreviation: SO, silicone oil.
Table 2.
Baseline Characteristics of Retinal Detachment.
| Diagnosis | Removed SO n = 57 (%) | Retained SO n = 53 (%) | P Value (Removed vs. Retained) |
|---|---|---|---|
| RRD with PVR | 32 (56.1) | 24 (45.2) | .34 |
| TRD associated with PDR | 13 (22.8) | 18 (34) | .21 |
| RRD associated with penetrating injury | 7 (12.2) | 4 (7.5) | .53 |
| RRD associated with GRT | 1 (1.8) | 3 (5.6) | .35 |
| TRD associated with ROP | 1 (1.8) | 1 (1.9) | 1.0 |
| Other indications | 3 (5.2) | 3 (5.6) | 1.0 |
Abbreviations: GRT, giant retinal tear; PDR, proliferative diabetic retinopathy; PVR, proliferative vitreoretinopathy; ROP, retinopathy of prematurity; RRD, rhegmatogenous retinal detachment; SO, silicone oil; TRD, tractional retinal detachment.
The main results are presented in Table 3. Twenty of 53 patients in the retained-SO group (37.7%) and 25 of 57 (43.8%) of patients in the removed-SO group had undergone one or more previous surgeries, including vitrectomy or globe repair (P = .7). In the retained-SO group, 18 of the 53 patients had undergone a scleral buckle (33%) vs 23 of the 57 patients (40.3%) in the removed-SO group (P = .56).
Table 3.
Main Results.
| Removed SO | Retained SO | P Value | |
|---|---|---|---|
| VA baseline, logMAR, (Snellen) | 1.84 ± 0.5, (20/1400) | 1.79 ± 0.6 (20/1200) | .44 |
| VA final visit, logMAR, (Snellen) | 1.4 ± 0.6, (20/500) | 1.2 ± 0.7 (20/350) | .18 |
| Previous ocular surgery (PPV, globe repair), (%) | 25 (43.8) | 20 (37.7) | .7 |
| Retinal redetachment rate, (%) | 10 (18) | 2 (4) | .03 |
| Total complication rate, (%) | 34 (60) | 24 (45) | .18 |
Abbreviations: logMAR, logarithm of the minimum angle of resolution; PPV, pars plana vitrectomy; SO, silicone oil; VA, visual acuity.
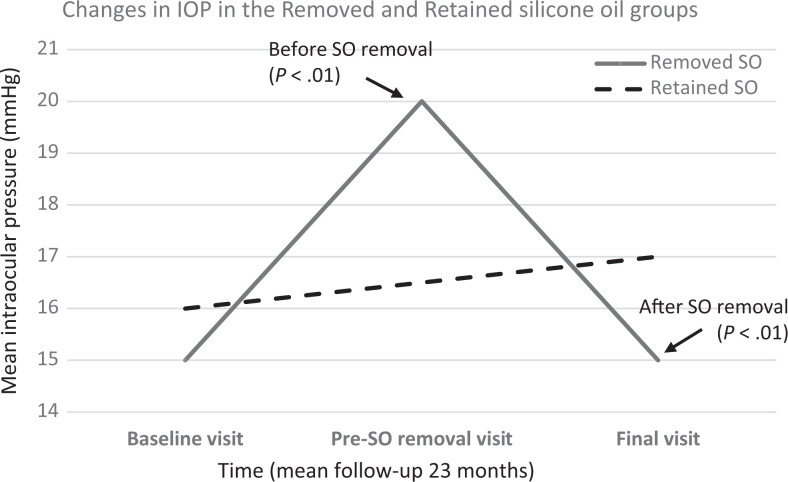
No difference was found between groups regarding baseline and final VA (P = .44, P = .18), and in both groups mean BCVA at the final visit was significantly better than at baseline (P < .001, P < .0001 for the retained-SO and removed-SO groups, respectively). In the retained-SO group, mean BCVA improved from 1.79 ± 0.6 logMAR units at the baseline visit to 1.2 ± 0.7 logMAR units at the final visit (P < .001). In the removed-SO group, mean BCVA improved from 1.84 ± 0.5 logMAR units at baseline to 1.55 ± 0.6 units at the visit preceding SO removal (P < .002) then to 1.4 ± 0.6 units at the final visit (P < .0001) (Figure 1). However, the VA was not statistically significant when comparing pre-SO removal to post-SO removal (P > .065). In the retained-SO group, 26% of eyes had a BCVA greater than or equal to 5/200 at baseline, which increased to 66% of eyes at the final visit (P < .001). In the removed-SO group, 23% of eyes had a BCVA greater than or equal to 5/200 at baseline, and 53% of eyes had a BCVA greater than or equal to 5/200 at the visit before SO removal (P = .002). After removal of the oil, 60% of eyes had a BCVA greater than or equal to 5/200 (P < .001). In both groups, changes in the mean IOP between the baseline and at the final visits did not differ significantly. In the removed-SO group, mean IOP increased significantly from a baseline value of 15 ± 5 mm Hg to 20 ± 11 mm Hg at the visit preceding SO removal (P < .001). After removal of SO, the mean IOP in this group decreased significantly to 15 ± 6 mm Hg at the last visit (P < .001) (Figure 2).
Figure 1.
Changes in best-corrected visual acuity (BCVA) in eyes in both the Removed and Retained silicone oil (SO) groups over the time of follow-up.
Figure 2.
Changes in intraocular pressure (IOP) in eyes in both the Removed and Retained silicone oil (SO) groups over the time of follow-up.
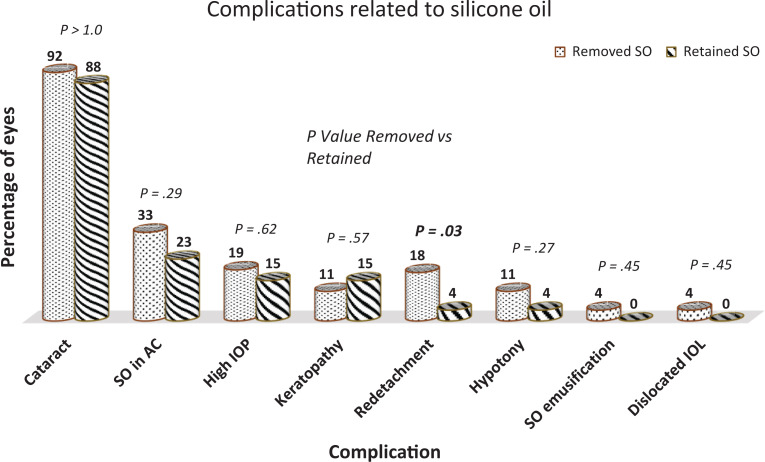
Anatomical success was achieved in 98 patients (89%) after the primary vitrectomy with SO tamponade. After SO was removed, 10 patients (18%) had a retinal redetachment, with a mean interval of 69 days after removal. Only 2 eyes (4%) had a retinal redetachment in the retained-SO group (P = .03). In the 12 eyes that had retinal redetachment, the diagnoses were RD associated with PVR in 9 eyes (75%) and penetrating eye trauma in 3 (25%) eyes. In all these eyes, PPV with SO reinjection or exchange was performed. The anatomical success rate after the second RD repair surgery was 94%.
The rates of all complications, except for retinal redetachment, were similar in eyes with removed SO compared to eyes with retained SO (Figure 3). One-third (36 or 32.7%) of all eyes had elevated IOP. Before SO removal, 22 eyes (39%) developed high IOP. After SO removal, IOP remained elevated in 50% of these eyes, which necessitated continuous medical control in 9 eyes (15.8%) and valve surgery in 2 eyes (3.5%). In the retained SO group, 14 eyes (26%) developed high IOP and were managed medically. The IOP normalized in all these eyes; however, 8 (57%) required continuous medical therapy.
Figure 3.
Complications related to silicone oil among eyes after their SO was removed and eyes with retained SO. All complications occurred at similar frequency among groups except for retinal re-detachment which occurred more frequently in the Removed SO group (P = .03). Boldface indicates significance of P < .05. SO: silicone oil, AC: anterior chamber, IOP: intraocular pressure, IOL: intraocular lens.
The majority of our patients were pseudophakic (78 eyes, 71%) or aphakic (4 eyes, 4%) at the time of the primary vitrectomy. Of the remaining 28 phakic eyes, 25 (89%) developed cataract during follow-up.
Keratopathy was noted in 23 eyes (21%) of all patients. Before SO removal in the removed-SO group, 15 eyes (26%) had keratopathy, with 11 eyes showing a nonspecific pattern that included stromal or epithelial edema or localized opacification, and the remaining 4 eyes showing a classic band keratopathy. After SO was removed in these eyes, 9 corneas (60%) became clear again but in 6 eyes (40%) the keratopathy remained. In the retained-SO group, 8 eyes (15%) developed a keratopathy (4 eyes with band keratopathy and 4 eyes with nonspecific keratopathy) that persisted throughout the follow-up. No difference in hypotony was observed between the 2 groups (P = .27).
Migration of the SO into the anterior chamber occurred in 19 eyes (33%) from the removed-SO group and in 12 eyes (23%) from the retained-SO group (P = .29). The presence of SO in the anterior chamber appeared to have no effect on the rate of elevated IOP (P = .11). In contrast, 15 eyes (65%) with keratopathy had SO in their anterior chambers and the association was significant (P < .001).
SO was removed routinely without the presence of SO-related complications in 23 eyes (40% of the removed-SO group, 21% of all eyes). However, removal of SO was deemed necessary in 34 eyes (60% of the removed-SO group, 31% of all eyes) because of the development of complications during follow-up, including high IOP (9 eyes), cataract (7 eyes), SO in the anterior chamber (4 eyes), keratopathy (3 eyes), dislocation of the intraocular lens (2 eyes), retinal redetachment (2 eyes), or a combination of the mentioned complications (7 eyes).
In eyes that retained their SO throughout the time of the follow up, 29 eyes (55% of the retained SO group, 26% of all eyes) had no complications. In 24 eyes (45% of the retained SO group, 22% of all eyes), SO-related complications were observed but did not necessitate SO removal. These complications were either visually insignificant media opacities including cataract and keratopathy or were successfully managed by medical therapy.
Conclusions
The usefulness of SO in complex RD in comparison with other available tamponading agents was established in the Silicone Study. 8,9 The necessity and timing of SO removal from eyes with these complex detachments remain less certain. Although it was strongly recommended in the Silicone Study that the oil be removed whenever possible, there was no established consensus among surgeons in the study regarding the selection of eyes and the timing for oil removal: the percentage of eyes with removed SO varied from 20% to 75% and the timing of removal varied from 1 month to almost 40 months. 5
Regarding the effect of SO removal on vision, the Silicone Study reported a significant improvement in VA at the final visit only in eyes that had an attached retina before SO removal. This result is not surprising considering the recommendation in the study to remove SO as soon as possible, which created a tendency for eyes selected for SO removal to have milder grades of PVR and a decreased likelihood of complications after removal. 5
Other groups have reported improvement in VA with SO removal in retrospective reviews; however, SO-removed eyes were not compared with SO-retained eyes. 6,10 -13 Interestingly, improvement in visual function after SO removal in some of these reviews was associated with better VA at initial visits and before SO removal. This suggests that eyes with significant visual improvement may have had less-aggressive disease or may have shown substantial improvement in response to the primary vitrectomy even before the SO was removed. 6,12 In our cohort, VA improved significantly from baseline after the primary vitrectomy in both groups. There was an additional modest yet not statistically significant improvement in vision in eyes that later underwent SO removal, indicating that visual improvement may have occurred in response to the primary vitrectomy surgery and retinal reattachment.
Several factors may explain visual improvement after SO removal, including reduced optical effects of the silicone bubble, continued recovery of retinal function after successful reattachment, and ancillary procedures such as excision of media opacities or epiretinal membrane that may have been performed at the time of SO removal. 11 Notably, 50% of patients in the Silicone Study, compared to 14% in our cohort, had such a secondary procedure, which may have contributed to improvement in VA.
The most feared consequence of SO removal is retinal redetachment, which has been reported in rates as high as 38%. 14 -16 In our cohort, the overall rate was 11% and found in significantly higher rates in eyes with removed SO compared to eyes with retained SO, with most redetachments documented within 2 months of the SO-removal procedure. This finding is consistent with that of many other reports. In the Silicone Study, 14% of eyes redetached after SO removal, the majority within 3 months of the procedure. 2,5,11,17 Different mechanisms have been postulated to underlie retinal redetachment after SO removal, including reopening of preexisting retinal breaks that were tamponaded by the surface tension of the oil bubble, formation of new breaks, insufficient retinopexy, residual traction, and progression of PVR. 5,11
SO retention may also lead to visually significant complications such as cataract, high IOP, and keratopathy. The rates of SO-related complications observed in our cohort fall within the range of those previously reported. Elevated IOP was documented in one-third of our patients. Some authors have reported rates of glaucoma that reach 70% with SO tamponade in advanced PDR 18 ; however, in most studies, including the Silicone Study, the documented rates were lower (1.5%-28%). 2,6,10,11,17,19 Although the rate of high IOP in our series was not significantly different among eyes that retained their SO and those from which the oil was removed, it decreased significantly after SO removal, from 39% to 19%. Similarly, most authors have reported decreased rates of elevated IOP post-SO removal. 2,11 Evidently, more effective control of this complication is an advantage of SO removal. It is important to note, however, that even if removal of SO is deferred, elevated IOP may be a temporary problem and acceptable control of IOP may be achieved by medical and rarely surgical management. Indeed, out of all 110 eyes in our series, 36 eyes (33%) developed elevated IOP, but the condition progressed to glaucoma with optic nerve damage in only about half of such eyes. (19 eyes).
Cataract was seen in 25 (89%) of our phakic eyes. In many studies with long follow-up, cataract eventually developed in all phakic eyes, 2,3 and most cases are recorded within the first year after SO injection. 6,11,18 Although it has been shown that cataract formation may be delayed by early SO removal, the majority of cases develop cataract or undergo cataract surgery. 20
In about one-fifth of our patients, keratopathy of some type was documented. In 9 out of 15 eyes (60%) eyes from the removed-SO group, the keratopathy disappeared post-SO removal. Similarly, varying rates of keratopathy ranging from 4% to 63% and improvement of corneal disease following SO removal have been reported. 5,6,10,11,15,21 We also found an association between the presence of SO in the anterior chamber and the development of keratopathy, which is consistent with findings of cytotoxicity of SO on the corneal endothelium. 22 Similar to cataract, keratopathy may still develop even after SO removal. In the Silicone Study, almost 30% of eyes demonstrated late-onset corneal changes after SO removal. 5
Hypotony is an important complication seen in patients who undergo vitrectomy and SO tamponade. In the Silicone Study, hypotony was recorded in 18% of eyes with SO tamponade and was correlated with anatomic failure and RD, anterior contraction of PVR membranes, poor VA, and corneal opacification. 19 Many retrospective reviews with different patient cohorts reported varying rates of hypotony ranging from 4% to 51%. 6,10,11 In our cohort, 8 eyes (7%) developed hypotony, most of them from the removed-SO group. Of these hypotonic eyes, 4 eyes also had retinal redetachment and poor vision, 3 eyes had keratopathy, and 2 eyes eventually developed phthisis bulbi.
Limitations of our study include the use of SO of different viscosities and the performance of surgery by different surgeons. Although the sample size in our study is adequate and larger than that of other studies, the study’s retrospective nature and the variable follow-up may limit the power to provide standardized data and firm conclusions about anatomic and visual outcomes. In this study, SO removal was performed for a variety of reasons; in some cases there were predisposing indications for its removal. We recognize that there may be a selection bias in this retrospective study that may influence outcomes.
In summary, equally good anatomic and visual results were attained both in the SO-retained and SO-removed groups. Removal of SO was associated with a higher likelihood of retinal redetachment, yet its retention in the eye may be associated with a higher chance for keratopathy and elevated IOP. Both situations may necessitate further management in eyes that are already compromised by prior surgeries, trauma, or complex pathology. Our data show that there is little difference in VA or complication profiles if SO is removed or retained. The management plan in these difficult cases must be tailored to the individual patient. In selected cases, it may be appropriate to leave SO in the eye, and in other cases SO removal may be deferred until SO-related complications arise and fail medical therapy.
Footnotes
Authors’ Notes: Data from this study were presented in part at the American Society of Retina Specialists’ 33rd Annual Meeting in Vienna, Austria, July 12, 2015.
Ethical Approval: This study was conducted in accordance with the Declaration of Helsinki and was approved by the institutional review board comity of the University of Louisville, and the Jordan University of Science and Technology.
Statement of Informed Consent: Informed consent was not required because of the retrospective nature of the study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Cibis PA, Becker B, Okun E, Canaan S. The use of liquid silicone in retinal detachment surgery. Arch Ophthalmol. 1962;68:590–599. doi:10.1001/archopht.1962.00960030594005 [DOI] [PubMed] [Google Scholar]
- 2. Al-Wadani SF, Abouammoh MA, Abu El-Asrar AM. Visual and anatomical outcomes after silicone oil removal in patients with complex retinal detachment. Int Ophthalmol. 2014;34(3):549–556. doi:10.1007/s10792-013-9857-9 [DOI] [PubMed] [Google Scholar]
- 3. Federman JL, Schubert HD. Complications associated with the use of silicone oil in 150 eyes after retina-vitreous surgery. Ophthalmology. 1988;95(7):870–876. doi:10.1016/s0161-6420(88)33080-0 [DOI] [PubMed] [Google Scholar]
- 4. Young TA, D’Amico DJ. Controversies in proliferative vitreoretinopathy tamponade and pharmacologic adjuvants. Int Ophthalmol Clin. 2005;45(4):163–171. doi:10.1097/01.iio.0000176368.93887.2c [DOI] [PubMed] [Google Scholar]
- 5. Hutton WL, Azen SP, Blumenkranze MS, et al. The effect of silicone oil removal. Silicone Study Report 6. Arch Ophthalmol. 1994;112(6):778–785. doi:10.1001/archopht.1994.01090180076038 [DOI] [PubMed] [Google Scholar]
- 6. Abu El-Asrar AM, Al-Bishi SM, Kangave D. Outcome of temporary silicone oil tamponade in complex rhegmatogenous retinal detachment. Eur J Ophthalmol. 2003;13(5):474–481. doi:10.1177/112067210301300509 [DOI] [PubMed] [Google Scholar]
- 7. Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg Visual Acuity Test. Invest Ophthalmol Vis Sci. 2006;47(3):1236–1240. doi:10.1167/iovs.05-0981 [DOI] [PubMed] [Google Scholar]
- 8. Silicone Study Report 2. Vitrectomy with silicone oil or perfluoropropane gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Arch Ophthalmol. 1992;110(6):780–792. doi:10.1001/archopht.1992.01080180052028 [DOI] [PubMed] [Google Scholar]
- 9. Schwartz SG, Flynn HW, Jr, Lee WH, Wang X. Tamponade in surgery for retinal detachment associated with proliferative vitreoretinopathy. Cochrane Database Syst Rev. 2014;14(2):CD006126. doi:10.1002/14651858.CD006126.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. La Heij EC, Hendrikse F, Kessels AG. Results and complications of temporary silicone oil tamponade in patients with complicated retinal detachments. Retina. 2001;21(2):107–114. doi:10.1097/00006982-200104000-00002 [DOI] [PubMed] [Google Scholar]
- 11. Falkner CI, Binder S, Kruger A. Outcome after silicone oil removal. Br J Ophthalmol. 2001;85(11):1324–1327. doi:10.1136/bjo.85.11.1324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Falkner-Radler CI, Smretschnig E, Graf A, Binder S. Outcome after silicone oil removal and simultaneous 360° endolaser treatment. Acta Ophthalmol. 2011;89(1):46–51. doi:10.1111/j.1755-3768.2010.02059.x [DOI] [PubMed] [Google Scholar]
- 13. Goezinne F, La Heij EC, Berendschot TT, Liem AT, Hendrikse F. Risk factors for redetachment and worse visual outcome after silicone oil removal in eyes with complicated retinal detachment. Eur J Ophthalmol. 2007;17(4):627–637. doi:10.1177/112067210701700423 [DOI] [PubMed] [Google Scholar]
- 14. Cox MS, Trese MT, Murphy PL. Silicone oil for advanced proliferative vitreoretinopathy. Ophthalmology. 1986;93(5):646–650. doi:10.1016/s0161-6420(86)33686-8 [DOI] [PubMed] [Google Scholar]
- 15. Gonvers M. Temporary silicone oil tamponade in the management of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1985;100(2):239–245. doi:10.1016/0002-9394(85)90788-3 [DOI] [PubMed] [Google Scholar]
- 16. Casswell AG, Gregor ZJ. Silicone oil removal. II. Operative and postoperative complications. Br J Ophthalmol. 1987;71(12):898–902. doi:10.1136/bjo.71.12.898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Scholda C, Egger S, Lakits A, Haddad R. Silicone oil removal: results, risks and complications. Acta Ophthalmol Scand. 1997;75(6):695–699. doi:10.1111/j.1600-0420.1997.tb00633.x [DOI] [PubMed] [Google Scholar]
- 18. Janco L, Tkácová Villemová K, Ondrejková M, Vida R, Bartoš M, Mesárošová M. Retinal tamponade with silicone oil—long term results [in Czech]. Cesk Slov Oftalmol. 2014;70(5):178–182. [PubMed] [Google Scholar]
- 19. Barr CC, Lai MY, Lean JS, et al. Postoperative intraocular pressure abnormalities in the Silicone Study. Silicone Study Report 4. Ophthalmology. 1993;100(11):1629–1635. doi:10.1016/s0161-6420(93)31425-9 [DOI] [PubMed] [Google Scholar]
- 20. Franks WA, Leaver PK. Removal of silicone oil—rewards and penalties. Eye (Lond). 1991;5(3):333–337. doi:10.1038/eye.1991.53 [DOI] [PubMed] [Google Scholar]
- 21. Casswell AG, Gregor ZJ. Silicone oil removal. I. The effect on the complications of silicone oil. Br J Ophthalmol. 1987;71(12):893–897. doi:10.1038/eye.1991.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yang CS, Chen KH, Hsu WM, Li YS. Cytotoxicity of silicone oil on cultivated human corneal endothelium. Eye (Lond). 2008;22(2):282–288. doi:10.1038/sj.eye.6702962 [DOI] [PubMed] [Google Scholar]