Abstract
Purpose:
The authors aim to describe the visual outcomes and postoperative complications of concurrent pars plana vitrectomy and scleral-fixated intraocular lens (IOL) placement using Gore-Tex suture.
Methods:
A retrospective review of medical records was performed on 27 eyes of 27 patients undergoing concurrent pars plana vitrectomy and scleral-fixated IOL with Gore-Tex suture. Outcome measures were change in preoperative and postoperative visual acuity, final manifest refraction, and incidence of intraoperative and postoperative complications.
Results:
The mean age was 69.2 ± 11.3 years; there were 16 male patients (59%). The duration of follow-up ranged from 33 to 576 days with a mean of 200 ± 143 days. All patients received Bausch + Lomb Akreos AO60 IOL. The overall mean best-corrected visual acuity in Snellen equivalent improved from 20/276 preoperatively to 20/44 postoperatively (P < .001). The mean postoperative manifest spherical equivalent refraction was –0.35 ± 1.34 diopters (D). Seventy-five percent of eyes were ± 1.0 D of target refraction. Postoperative complications included corneal edema (26.0%), ocular hypertension (25.9%), hypotony (7.4%), cystoid macular edema (7.4%), vitreous hemorrhage (7.4%), and hyphema (3.7%). No cases of suture breakage, IOL dislocation, retinal detachment, or uveitis–glaucoma–hyphema syndrome were identified.
Conclusions:
The use of Gore-Tex suture for posterior chamber IOL fixation resulted in favorable outcomes. No suture-related complications occurred during the follow-up period. Final refraction in this setting is typically within ± 1.0 D of target.
Keywords: refractive outcomes, secondary IOL, sutured IOL
Introduction
With the aging population and the growing number of individuals who have undergone cataract surgery, intraocular lens (IOL) dislocation is becoming a broader public health concern. 1 The IOL-capsular bag complex may lose stability from many causes. In this setting, secondary IOL placement can be accomplished with anterior chamber IOLs, iris-fixated lenses, and scleral-fixated posterior chamber IOLs.
Without capsular support, scleral-fixated IOL placement is effective when pars plana vitrectomy (PPV) is also necessary to resolve additional complications such as retained lens material, dislocated IOL, or posteriorly subluxated crystalline lens. 2 During long-term follow-up of scleral-fixated IOLs, polypropylene suture (Prolene, Ethicon) has demonstrated the potential to erode and break, often requiring reoperation. 3 -5 As an alternative, ab externo scleral fixation using Gore-Tex (Gore Medical), a nonabsorbable polytetrafluoroethylene monofilament suture, has recently been described. 6 Gore-Tex has been shown to remain intact postoperatively for decades after cardiothoracic procedures. 7
Although ophthalmologists routinely use Gore-Tex suture in surgery, there are few reports that have detailed its use and long-term postoperative outcomes. Data from 2 institutions 8 -10 have shown low rates of complications, promising visual outcomes, and no cases of inflammation, suture erosion, or breakage when Gore-Tex is used. To the best of our knowledge, only 1 institution has previously documented the refractive outcomes of these patients in the postoperative period, an important marker of postsurgical success. 11,12 The aim of this study is to characterize the postsurgical refractive outcomes and complications of scleral-fixated IOLs using Gore-Tex suture at a single center.
Methods
A retrospective review was performed of all patients who underwent combined PPV and scleral fixation of an Akreos AO60 (Bausch + Lomb) IOL using 7-0 Gore-Tex suture (CV-8) at Vanderbilt University Medical Center, an academic level 1 trauma center, between July 1, 2016 and October 1, 2018. Patients were selected using current procedural terminology codes 66985 for secondary insertion of IOL prosthesis and 66986 for exchange of IOL prosthesis; only those cases inserting an Akreos AO60 IOL were included.
Each identified case involved a concurrent PPV with 23- or 25-gauge instrumentation using the Constellation vitrectomy system (Alcon) and scleral fixation of an Akreos AO60 IOL using Gore-Tex suture and a modified technique. 6 Two localized conjunctival peritomies were created at the 3 and 9 o’clock positions. An infusion cannula was then placed inferotemporally 3 mm posterior to the limbus. Two sclerotomies were made both at the 3 and 9 o’clock positions, 2 mm posterior to the limbus and 4 mm apart. A complete PPV was performed. A 3.5-mm clear-corneal shelved incision was made using the keratome blade. Externally, a single 7-0 Gore-Tex suture (CV-8) was looped through the ipsilateral eyelets of an Akreos AO60 IOL in an anterior-posterior, posterior-anterior fashion. In a similar manner, a 7-0 Gore-Tex suture was looped though the other ipsilateral side. The ends of the Gore-Tex sutures were then passed through the keratome incision and out the sclerotomies in a hand-over-hand fashion. The lens was folded and passed through the corneal incision into the sulcus space after injection of viscoelastic. The lens was centered before the Gore-Tex sutures were tied down and buried. The sclerotomies were closed with 7-0 Vicryl (Ethicon, Inc) sutures. The corneal incision was typically closed with 1 or 2 10-0 nylon sutures. The conjunctival peritomies were closed with 7-0 Vicryl sutures. No intraocular gas or air was introduced to minimize the risk of IOL opacification. Each patient was examined on postoperative day 1, week 1, and month 1. Corneal sutures were all removed before final postoperative manifest refraction. Further follow-up continued as needed.
IOL calculations were performed using the Holladay 2 formula with HIC.SOAP Professional Edition software (Holladay Consulting), with optical biometry measurements obtained from the IOLMaster 500 (Carl Zeiss Meditec AG). Age, sex, laterality, surgical indication(s), relevant ophthalmic history, preoperative and postoperative best-available Snellen visual acuity (VA) using the last line that was read completely, preoperative and postoperative intraocular pressure (IOP), spherical equivalent refraction, manifest spherical equivalent refraction at last follow-up, and the duration and treatment of intraoperative and postoperative complications were recorded.
Counting fingers at a given distance was recorded in Snellen equivalent assuming fingers are approximately the size of a 200 letter. 13 Snellen VA was converted to logarithm of the minimum angle of resolution (logMAR) for statistical analysis. Hand motion vision corresponded to a logMAR of 3.00. 13 IOP was measured with a Tono-pen (Medtronic), with hypotony defined as an IOP of 5 mm Hg or less and ocular hypertension defined as an IOP of 25 mm Hg or more at any postoperative visit. Postoperative corneal edema, superficial punctate keratitis, and cystoid macular edema (CME) were recorded if lasting longer than 30 days postoperatively. CME was confirmed with spectral-domain optical coherence tomography.
The outcome measures were change in VA, final refraction, and the incidence of intraoperative and postoperative complications. Statistical analyses were performed with a paired sample t test or Fisher exact test when appropriate.
Results
Twenty-seven eyes of 27 patients (15 right eyes and 12 left eyes) received a combined PPV and scleral-fixated Akreos A060 IOL with Gore-Tex suture. Patient characteristics are outlined in Table 1. The mean age at the time of surgery was 69.2 ± 11.3 years (range, 45-86 years). Ophthalmic history was remarkable for ocular trauma in 5 eyes (18.5%), retinal detachment repair in 3 eyes (11.1%), age-related macular degeneration in 2 eyes (7.4%), proliferative diabetic retinopathy in 1 eye (3.7%), and corneal edema prior to surgery in 1 eye (3.7%). The mean duration of postoperative follow-up was 200 ± 143 days (range, 33-576 days).
Table 1.
| Demographic Information | No. (%) (N = 27) |
|---|---|
| Age, y | |
| Mean ± SD | 69.2 ± 11.3 |
| Range | 45-86 |
| Sex | |
| Male | 16 (59.3) |
| Female | 11 (40.7) |
| Eyes | |
| Left | 12 (44.4) |
| Right | 15 (55.6) |
| Relevant ophthalmic history | |
| Ocular trauma | 5 (18.5) |
| Retinal detachment repair | 3 (11.1) |
| Age-related macular degeneration | 2 (7.4) |
| Duration of follow-up, d | |
| Mean ± SD | 200 ± 143 |
| Range | 33-576 |
| Proliferative diabetic retinopathy | 1 (3.7) |
| Corneal edema prior to surgery | 1 (3.7) |
Indications for the placement of a scleral-sutured IOL included dislocated IOL in 18 eyes (66.7%), subluxated crystalline lens in 5 eyes (18.5%), visually significant inflammatory deposits on IOL in 2 eyes (7.4%), aphakia after complex cataract extraction in 1 eye (3.7%), and malpositioned anterior chamber IOL in 1 eye (3.7%). Table 2 outlines the clinical outcomes. Whereas the mean preoperative logMAR VA was 1.14 ± 0.89 (20/276 Snellen equivalent), the mean postoperative logMAR VA for all eyes improved by 0.80 (95% confidence interval, 0.47-1.13; P < .001) to 0.34 ± 0.36 (20/44 Snellen equivalent) at last follow-up. Improvement in VA was documented for all surgical indications, with dislocated IOL achieving statistical significance (P < .001). Figure 1 demonstrates the proportion of eyes within specified VA ranges before and after surgery. The number of eyes with VA 20/40 or better increased from 4 eyes (14.8%) preoperatively to 16 eyes (59.3%) postoperatively (P < .01).
Table 2.
Visual Outcomes.
| Mean Preoperative VA, LogMAR ± SD (Snellen) |
Mean Postoperative VA, LogMAR ± SD (Snellen) |
Difference, LogMAR (95% CI) | P | |
|---|---|---|---|---|
| Overall (n = 27) | 1.14 ± 0.89 (20/276) | 0.34 ± 0.36 (20/44) | 0.80 (0.47 to 1.13) | <.001 |
| Indication | ||||
| Dislocated IOL (n = 18) | 1.21 ± 0.96 (20/324) | 0.30 ± 0.35 (20/40) | 0.91 (0.47 to 1.35) | <.001 |
| Subluxed crystalline lens (n = 5) | 1.22 ± 0.90 (20/332) | 0.33 ± 0.14 (20/43) | 0.89 (–0.21 to 1.99) | .09 |
| Inflammatory deposits on IOL (n = 2) | 0.53 ± 0.49 (20/68) | 0.40 ± 0.43 (20/50) | 0.13 (–0.49 to 0.74) | .23 |
Abbreviations: IOL, intraocular lens; LogMAR, logarithm of the minimum angle of resolution; VA, visual acuity.
Figure 1.
Preoperative and postoperative visual acuity (VA) of patients receiving a scleral-fixated intraocular lens using Gore-Tex suture. The percentage of eyes with the same VA or better at each benchmark (20/30, 20/40, 20/50, 20/70, 20/100, 20/200, counting fingers at 5 feet) was significantly higher postoperatively than preoperatively (with P < .05 denoting significance).
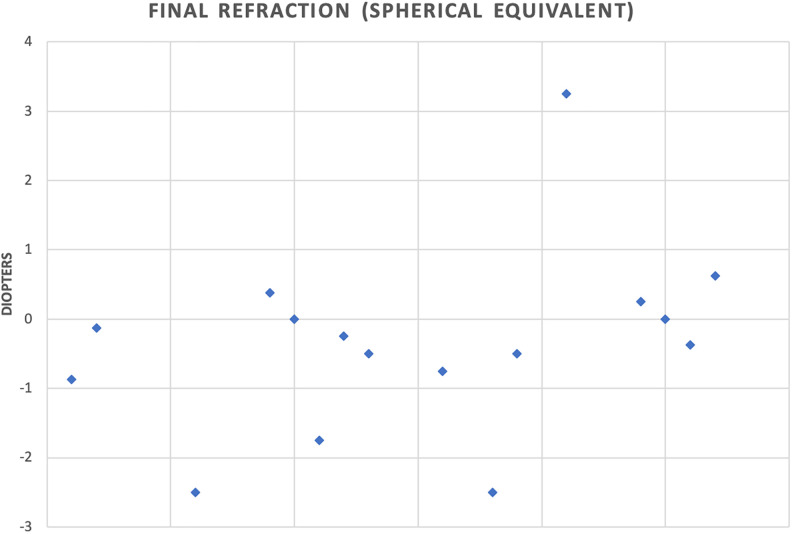
Out of the 16 eyes with postoperative refractive data available, 12 eyes (75.0%) had a final manifest spherical equivalent refraction within ± 1.0 diopter (D) of target (Figure 2). Eleven eyes (68.8%) had an average myopic shift of –1.27 D from target refraction, and the remaining 5 eyes (31.3%) had an average hyperopic shift of +1.0 D. All 3 eyes with final refractions differing more than ±2.0 D from target were due to a myopic shift. The mean postoperative manifest spherical equivalent refraction was –0.35 ± 1.34 D. Twelve of 16 eyes (75.0%) were myopic or plano at final correction. Three of 4 hyperopic patients were less than +1.0 D spherical equivalent. Average astigmatic correction was 1.52 ± 1.21 D. Astigmatism occurred at 86 ± 66° on average.
Figure 2.
Final postoperative refractive outcomes in spherical equivalent. Twelve of the 16 patients had final refraction within 1.0 D of target refraction.
No intraoperative complications were noted. Table 3 outlines the postoperative complications, including persistent corneal edema in 7 eyes (26.0%), ocular hypertension in 7 eyes (26.0%), superficial punctate keratitis in 7 eyes (26.0%), anterior uveitis in 2 eyes (7.4%), CME in 2 eyes (7.4%), vitreous hemorrhage in 2 eyes (7.4%), hypotony in 2 eyes (7.4%), hyphema in 1 eye (3.7%), and endophthalmitis in 1 eye (3.7%). All complications were managed with medical therapy or observation. The case of postoperative endophthalmitis (culture-negative) resolved in 18 days after receiving intravitreal injection of ceftazidime, vancomycin, and moxifloxacin. No additional surgical intervention was performed. All cases of hypotony, hyphema, and vitreous hemorrhage resolved within 30 days. All cases of CME and ocular hypertension resolved within 90 days. There were no cases of postoperative suture breakdown, persistent postoperative inflammation, dislocated IOL, retinal detachment, or uveitis–glaucoma–hyphema syndrome in the follow-up period.
Table 3.
Postoperative Complications.
| No. of Eyes, % | Mean Duration (Range), d | |
|---|---|---|
| Corneal edema | 7 (26.0) | 84 (40-264) |
| Ocular hypertension | 7 (26.0) | 18 (2-44) |
| Superficial punctate keratitis | 7 (26.0) | 129 (38-247) |
| Anterior uveitis | 2 (7.4) | 186 (28-344) |
| Cystoid macular edema | 2 (7.4) | 63 (49-77) |
| Vitreous hemorrhage | 2 (7.4) | 12 (8-16) |
| Hypotony | 2 (7.4) | 20 (20-20) |
| Hyphema | 1 (3.7) | 7 |
| Endophthalmitis | 1 (3.7) | 18 |
| Suture breakdown | 0 | – |
| Intraocular lens dislocation | 0 | – |
| Retinal detachment | 0 | – |
Conclusions
The durability of suture material is thought to be correlated with the success of a scleral-sutured IOL, which is often performed alongside PPV. Prolene (Ethicon, Inc) has historically been favored because it is proven to be well tolerated for intraocular use. However, its tendency to break down over time has led many to reexamine its benefits. One report found that 10-0 Prolene breakage occurred in 27% of eyes that underwent scleral-sutured IOL, and approximately half (49%) of eyes required additional procedures to resolve postoperative complications. 5 For this reason, Gore-Tex has gained interest for replacement of Prolene in scleral-sutured IOLs because of its documented success in nonophthalmic procedures. 7
Recent studies 8 -10 on IOLs fixated with Gore-Tex have found few complications and favorable outcomes. However, previous studies often included older poly(methyl methacrylate) lenses that, because of their rigid structure, can prolong surgical time and increase risk of complications compared with modern foldable lenses. Additionally, refractive outcomes in this setting have only recently been described in small case series involving a variety of IOLs and surgical techniques. 11,12 Our study is the first to our knowledge to report the postoperative refraction among eyes exclusively receiving an Akreos A060 IOL fixated 2 mm posterior to the limbus with Gore-Tex suture.
The largest review of scleral-fixated IOLs using Gore-Tex suture with concurrent PPV included 85 cases with a minimum follow-up period of 365 days (mean, 598 ± 183 days). 9 Postoperative complications in that study included vitreous hemorrhage (7.1%), CME (4.8%), ocular hypertension (3.6%), hyphema (2.4%), and corneal edema (2.4%). A smaller series of 49 cases with mean follow-up of 6.9 months found a higher incidence of postoperative ocular hypertension (16.3%), hypotony (12.2%), corneal edema (8.2%), CME (6.1%), IOL tilt (4.1%), and hyphema (4.1%). 10 No cases of postoperative endophthalmitis, choroidal detachment, uveitis–glaucoma–hyphema syndrome, or persistent postoperative inflammation have been reported in previous studies.
The profile of complications in our case series was similar to previous reports. Perhaps most important, no case of suture breakdown or erosion was found. Only 1 case of Gore-Tex suture erosion after a scleral-sutured IOL has been previously reported in the literature. 10 Gore-Tex has demonstrated superior tensile strength compared with other materials, 14 which has led to increased interest for ophthalmic use. We also found no scleritis or inflammation associated with suture placement. In vivo analysis has shown that Gore-Tex demonstrates excellent biocompatibility with minimal inflammatory response. 15 In addition, no cases of IOL tilt were noted, and no additional procedures were required to reposition the IOL after initial placement. A previous report 10 recommended a 3-1-1 knot-tying technique, tightening the nasal and temporal suture until optimal anatomical placement is achieved. We prefer an adjustable 1-1-1 slipknot to ensure centration without overtightening.
Corneal edema and ocular hypertension appear to be common complications in the postoperative period, but most cases in our series were transient, and none required additional surgical intervention. No abnormal increases in IOP lasted longer than 45 days.
In regard to possible inflammatory reactions to Gore-Tex, 2 patients presented with anterior uveitis in the postoperative period but had histories of intraocular inflammation. Another patient had a transient recurrence of anterior chamber inflammation 6 months after a previous IOL was exchanged because of multiple persistent inflammatory deposits that created a film over the patient’s vision. Importantly, no patient had evidence of conjunctivitis, scleritis, or local suture reaction.
The incidence of postoperative CME, vitreous hemorrhage, hypotony, and hyphema were similar to previous reports, 9,10 and none of these complications were persistent. Consistent with previous reports, scleral fixation of an IOL using Gore-Tex suture resulted in significant improvement in VA. Patients with a dislocated IOL had significant improvement in vision, but this did not hold true for other indications. Studies with larger sample sizes are needed to better quantify the visual improvement when patients are subdivided based on surgical indication. All patients received an Akreos AO60 IOL, although various IOLs can be used. One advantage of the Akreos AO60 is its ability to be folded, allowing for a smaller corneal incision. We also did not observe any cases of IOL opacification. A previous study found that scleral-sutured Akreos IOLs can opacify when exposed to air or gas tamponade, 16 which was not used in our case series.
Our study is among the first to document the refractive outcomes of patients who received a scleral-sutured IOL using Gore-Tex. Only 18.8% of patients in our study had a final refraction that was 2.0 D or more off target of the predicted refraction, a slightly higher rate compared with a previous study. 12 All these cases were myopic shifts, likely due to anterior placement of the IOL.
A more posterior positioning of the haptics represents an attempt to align with in-the-bag measurements obtained from optical biometry. 6 The overall postoperative refractive outcomes from our study appear to be superior to those previously reported for sulcus-fixated IOLs using Prolene. 17 Furthermore, the mean postoperative manifest refraction was also similar to previous literature reports. 17,18 The final refraction tends to be more myopic because sulcus-fixated IOLs are more anterior compared with in-the-bag placement. However, because a hyperopic shift was found in a few cases, we suggest that a target refraction of –0.5 to –1.0 D is optimal. Additionally, careful attention should be paid to the tension placed on the sutures, because excessive tightening can induce anterior shift of the IOL with resultant diffraction. The scleral penetrating point may also affect the refractive outcome. Postoperative astigmatism in this setting tended to be with-the-rule astigmatism, an important point to consider in preoperative discussions with patients.
Limitations of this study include its retrospective design and limited sample size. However, this is balanced by the uniformity in the surgical procedure performed among all patients. Importantly, our findings underscore the value of preoperative patient education, which may be tailored based on presenting etiology. Patients should also be counseled extensively on postoperative expectations of uncorrected VA and potential complications. Prospective studies with longer duration of follow-up are needed to establish the risk of complications and visual outcomes of Gore-Tex–sutured IOLs compared with other frequently used techniques.
Footnotes
Ethical Approval: Institutional review board approval for this study was obtained from the Vanderbilt University Medical Center (VUMC IRB No. 181802). This study was conducted in compliance with HIPAA (Health Insurance Portability and Accountability Act).
Statement of Informed Consent: Informed consent was not required.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported in part by an unrestricted grant to the Vanderbilt Eye Institute by Research to Prevent Blindness.
References
- 1. Mönestam E. Frequency of intraocular lens dislocation and pseudophacodonesis, 20 years after cataract surgery—a prospective study. Am J Ophthalmol. 2019;198:215–222. doi:10.1016/j.ajo.2018.10.020 [DOI] [PubMed] [Google Scholar]
- 2. Wagoner MD, Cox TA, Ariyasu RG, Jacobs DS, Karp CL. Intraocular lens implantation in the absence of capsular support: a report by the American Academy of Ophthalmology. Ophthalmology. 2003;110(4):840–859. doi:10.1016/s0161-6420(02)02000-6 [DOI] [PubMed] [Google Scholar]
- 3. Kokame GT, Yanagihara RT, Shantha JG, Kaneko KN. Long-term outcome of pars plana vitrectomy and sutured scleral-fixated posterior chamber intraocular lens implantation or repositioning. Am J Ophthalmol. 2018;189:10–16. doi:10.1016/j.ajo.2018.01.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bading G, Hillenkamp J, Sachs HG, Gabel VP, Framme C. Long-term safety and functional outcome of combined pars plana vitrectomy and scleral-fixated sutured posterior chamber lens implantation. Am J Ophthalmol. 2007;144(3):371–377. doi:10.1016/j.ajo.2007.05.014 [DOI] [PubMed] [Google Scholar]
- 5. Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141(2):308–312. doi:10.1016/j.ajo.2005.09.012 [DOI] [PubMed] [Google Scholar]
- 6. Khan MA, Gerstenblith AT, Dollin ML, Gupta OP, Spirn MJ. Scleral fixation of posterior chamber intraocular lenses using Gore-Tex suture with concurrent 23-gauge pars plana vitrectomy. Retina. 2014;34(7):1477–1480. doi:10.1097/IAE.0000000000000233 [DOI] [PubMed] [Google Scholar]
- 7. Sakamoto T, Nagase Y, Takiguchi M, Umehara N. A successful case of external stenting for bronchomalacia lasting over 20 years. Ann Thorac Surg. 2019;108(2):e103–e104. doi:10.1016/j.athoracsur.2018.12.055 [DOI] [PubMed] [Google Scholar]
- 8. Khan MA, Gupta OP, Smith RG, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638–643. doi:10.1136/bjophthalmol-2015-306839 [DOI] [PubMed] [Google Scholar]
- 9. Khan MA, Samara WA, Gerstenblith AT, et al. Combined pars plana vitrectomy and scleral fixation of an intraocular lens using Gore-Tex suture: one-year outcomes. Retina. 2018;38(7):1377–1384. doi:10.1097/IAE.0000000000001692 [DOI] [PubMed] [Google Scholar]
- 10. Patel NA, Shah P, Yannuzzi NA, et al. Clinical outcomes of 4-point scleral fixated 1-piece hydrophobic acrylic equiconvex intraocular lens using polytetrafluoroethylene suture. Clin Ophthalmol. 2018;12:2145–2148. doi:10.2147/OPTH.S174211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Su D, Stephens JD, Obeid A, et al. Refractive outcomes after pars plana vitrectomy and scleral fixated intraocular lens with Gore-Tex suture. Ophthalmol Retina. 2019;3(7):548–552. doi:10.1016/j.oret.2019.02.012 [DOI] [PubMed] [Google Scholar]
- 12. Botsford BW, Williams AM, Conner IP, Martel JN, Eller AW. Scleral fixation of intraocular lenses with Gore-Tex suture: refractive outcomes and comparison of lens power formulas. Ophthalmol Retina. 2019;3(6):468–472. doi:10.1016/j.oret.2019.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Holladay JT. Visual acuity measurements. J Cataract Refract Surg. 2004;30(2):287–290. doi:10.1016/j.jcrs.2004.01.014 [DOI] [PubMed] [Google Scholar]
- 14. González-Barnadas A, Camps-Font O, Espanya-Grifoll D, España-Tost A, Figueiredo R, Valmaseda-Castellón E. In vitro tensile strength study on suturing technique and material. J Oral Implantol. 2017;43(3):169–174. doi:10.1563/aaid-joi-D-16-00164 [DOI] [PubMed] [Google Scholar]
- 15. Korzinskas T, Jung O, Smeets R, et al. In vivo analysis of the biocompatibility and macrophage response of a non-resorbable PTFE membrane for guided bone regeneration. Int J Mol Sci. 2018;19(10). doi:10.3390/ijms19102952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kalevar A, Dollin M, Gupta RR. Opacification of scleral-sutured Akreos AO60 intraocular lens after vitrectomy with gas tamponade: case series [published online September 27, 2017]. Retin Cases Brief Rep. doi:10.1097/ICB.0000000000000634 [DOI] [PubMed] [Google Scholar]
- 17. Yang CS, Chao YJ. Long-term outcome of combined vitrectomy and transscleral suture fixation of posterior chamber intraocular lenses in the management of posteriorly dislocated lenses. J Chin Med Assoc. 2016;79(8):450–455. doi:10.1016/j.jcma.2016.01.016 [DOI] [PubMed] [Google Scholar]
- 18. Donaldson KE, Gorscak JJ, Budenz DL, Feuer WJ, Benz MS, Forster RK. Anterior chamber and sutured posterior chamber intraocular lenses in eyes with poor capsular support. J Cataract Refract Surg. 2005;31(5):903–909. doi:10.1016/j.jcrs.2004.10.061 [DOI] [PubMed] [Google Scholar]