Abstract
Introduction:
Prepared (ready-to-eat) foods are sold in >90% of U.S. supermarkets, but little is known about their nutritional quality. This study examined trends in purchases of supermarket prepared foods and compared their nutritional profile to that of supermarket packaged foods and restaurant foods.
Methods:
Nutrition data were obtained on prepared foods sold from 2015–2019 in 2 supermarket chains (~1,200 stores). One chain (193 stores) provided transaction-level sales data from 2015–2017. Analyses (conducted in 2021–2022) examined trends in the number of different prepared foods offered by the chains, and trends in purchases of calories, total sugar, saturated fat, and sodium from prepared foods. Calorie and nutrient densities (i.e., per 100g of food) and prevalence of being “high in” calories or nutrients (based on Chilean standards) were analyzed among supermarket prepared foods, supermarket packaged foods, and restaurant foods consumed in the National Health and Nutrition Examination Surveys 2015–2018.
Results:
The number of different prepared foods offered at the supermarket chains increased from 1,930 in 2015 to 4,113 in 2019. Calories-per-transaction purchased from supermarket prepared foods increased by 1.0 calorie/month (95% CI=0.8, 1.1), a ~3% annual increase, with similar trends for other nutrients. At supermarkets, >90% of prepared bakery and deli items and 61% of prepared entrees/sides were high in calories or another nutrient of concern, similar to supermarket packaged foods and restaurant foods.
Conclusions:
Supply of and demand for supermarket prepared foods have grown substantially over time. These trends are concerning given these foods’ overall poor nutritional quality.
INTRODUCTION
Poor nutrition is a leading modifiable cause of death in the U.S.1 “Prepared foods” are an important contributor to the U.S. diet, comprising one-third of daily calorie intake.2 Prepared foods are ready-to-eat foods that are made away from home and are usually eaten on site or soon after purchasing.3 Sales of prepared foods have increased over the last several decades and now comprise the majority of food sales in the U.S.2 Prepared foods are a public health concern because compared to homemade foods, they are typically higher in calories, saturated fat, and sodium; contain fewer fruits and vegetables; and are served in larger portions.2,4
Although restaurants are the primary source of prepared foods in the U.S. (e.g., entrees, sides, desserts), nearly all U.S. supermarkets also sell prepared foods, including bulk bakery items, sandwiches, deli items, sushi, and pizza.5 According to food industry reports, supermarket prepared foods are already a multi-billion dollar market, with rapid growth expected over the next several years.6–9 Supermarket prepared foods often mimic restaurant foods,10,11 which is concerning given the overall low nutritional quality of restaurant foods.12–14 However, limited research has examined supermarket prepared foods. One study from 2011–2012 found that most supermarkets offered prepared foods,5 but examined only a small number of food categories (pizza, tacos, salads, and burgers/hotdogs) and did not report on sales or nutritional quality of these foods. To determine the importance of targeting supermarket prepared foods in future interventions, research characterizing the availability, sales, and nutritional profile of the full range of supermarket prepared foods is needed.
To address these gaps, this study had the following objectives: (1) examine changes in the availability of prepared foods at 2 large supermarket chains over time; (2) analyze time trends in sales of calories and nutrients of interest (saturated fat, sugar, and sodium) from prepared foods purchased in one of the supermarket chains; and (3) compare the nutritional profile (i.e., calorie and nutrient densities) of supermarket prepared foods with that of supermarket packaged foods and restaurant foods.
METHODS
Prepared Food Availability
To determine the availability of prepared foods over time, this study examined the number of different prepared foods sold by 2 supermarket chains from 2015–2019. The chains comprised ~1,200 stores in the Northeastern, Mid-Atlantic, and Southeastern U.S. The chains are traditional supermarkets (not specialty or discount stores) located in rural, suburban, and urban areas that are demographically similar to the U.S. overall.15 The chains participate in Guiding Stars, a shelf-tag nutrition labeling program.16,17
Data for this objective came from Guiding Stars, which tracked nutrition information for all foods sold in the 2 chains from July 2015–January 2019 (n=94,718 unique items) to implement their labeling system.16–18 Guiding Stars provided updated databases in 6-month intervals. Non-food items (n=1,405) were excluded. Guiding Stars provided products’ Universal Product Code (UPC), product description, serving size, servings-per-container, nutritional content per serving, and whether products were subject to U.S. calorie labeling requirements for prepared foods.3 Prepared foods were identified based on this calorie labeling indicator; prepared status and nutrition information were confirmed through an extensive data review process that used product websites and guidance from Guiding Stars personnel (see Grummon et al.15). All other foods were classified as packaged foods (i.e., prepackaged foods not prepared on site). Foods were further classified into 3 categories: (1) bakery items (e.g., muffins), (2) entrees/sides (e.g., pizza), and (3) deli meats and cheeses (e.g., sliced turkey). Categorization drew on a previously developed food grouping system19,20 and is described elsewhere.15 Appendix Tables 1–2 provide additional details on food categorization.
Prepared food availability was determined by calculating the number of different prepared foods (i.e., UPCs) sold at the 2 supermarket chains and the proportion of total foods sold that were prepared foods. These outcomes were calculated in 6-month intervals to provide information on availability over time.
Trends in Prepared Food Sales
To analyze time trends in sales of prepared foods, transaction-level purchasing data were obtained from 1 of the 2 supermarket chains (comprising 193 stores in Maine, Massachusetts, New Hampshire, New York, and Vermont) from April 1, 2015–March 31, 2017. The data included information on items’ UPC, product description, date of purchase, price, and quantity purchased. Sales from 175 stores that were continuously open throughout the study period were included. Analyses excluded 497,914,097 non-food items (15.3% of purchased items) and 246,191,725 items (7.6%) that were missing a product description and could not be identified, yielding an analytic sample of 2,501,428,658 items purchased across 273,106,246 transactions.
Nutrition information was obtained for each item purchased by linking the sales data to the Guiding Stars database on UPC at each 6-month interval for which Guiding Stars data were provided. Items sold at the hot bar were excluded because transaction information did not specify which items were selected. Initial linking of the sales data to the Guiding Stars data yielded complete nutrition data for 81.4% of purchased items. After completing several steps to fill in the missing data, 91.2% of purchased items had complete calorie data and 88.6% had complete data for other nutrients. Values for the remaining missing data were imputed to avoid detecting trends that were solely due to missingness (Appendix provides details).
Prepared foods were identified using information in the Guiding Stars database and classified as bakery items, entrees/sides, and deli items (as for objective 1). Outcome measures were sales of calories and unhealthy nutrients (i.e., sugar, saturated fat, and sodium) from prepared foods, derived by multiplying nutrients-per-serving by servings-per-container in each product. Mean calories- and nutrients-per-transaction were calculated by summing calories or nutrients purchased across all prepared foods in a 4-week period and dividing by the number of transactions in that 4-week period. Purchases were aggregated to 4-week periods (hereafter “month”) to reduce the influence of short-term fluctuations in purchases. The percent of total purchases of each nutrient that came from prepared foods was also calculated.
Monthly time trends in mean calories- and nutrients-per-transaction purchased from prepared foods were estimated using generalized estimating equations, regressing the outcome of interest on month. Observations were weighted by the total number of transactions in each store (to reflect between-store differences in sales) and clustered at the store-level. Models were estimated with robust SEs. Monthly trends in percent of total calories and nutrients purchased from prepared foods were estimated similarly. Analyses were conducted overall, by food category, and by poverty status of supermarkets’ census tracts (> versus ≤median poverty level [9.8%], from the 2015–2019 American Community Survey21) to examine trends by neighborhood SES.
Nutritional Profiles of Supermarket Prepared Foods, Supermarket Packaged Foods, and Restaurant Foods
This study additionally compared the nutritional profile of supermarket prepared foods to that of similar supermarket packaged foods and restaurant prepared foods. Data on the nutritional profile of supermarket foods came from Guiding Stars (described above) for the chain with sales data available. Data on restaurant foods came from the National Health and Nutrition Examination Surveys (NHANES), a nationally representative survey of the civilian, non-institutionalized U.S. population. This study examined foods consumed in NHANES rather than a restaurant foods database (e.g., MenuStat) to reflect the frequency with which different restaurant foods are consumed. Data were obtained from the 2015–2016 and 2017–2018 NHANES cycles (n=19,225) to mirror the periods covered by the supermarket data. This study analyzed the first day of dietary recalls collected by NHANES, consistent with recommendations for estimating mean usual intake.22 Dietary intake data included information on the types, amounts, and sources (e.g., restaurant vs store) of foods consumed. Participants reporting consumption of restaurant foods (n=2,701) were demographically similar to NHANES participants overall (Appendix Table 3).
Supermarket foods were classified as prepared foods or packaged foods as described above and elsewhere.15 Supermarket foods were additionally categorized as bakery items, entrees/sides, or deli items, as above. Foods consumed by NHANES participants were classified as restaurant foods if they were obtained from any restaurant (full-service or quick service), including: restaurants with wait staff; fast food or pizza restaurants; bars, taverns, or lounges; or other types of restaurants. Restaurant foods were classified as bakery items, entrees/sides, or deli items using food codes and combination food types (Appendix Table 2).
Outcome measures were calorie density (calories per 100g of food, calculated as [calories-per-serving/serving size in grams]*100), sugar density (grams per 100g), saturated fat density (grams per 100g), and sodium density (milligrams per 100g) from each source (i.e., supermarket prepared foods, similar supermarket packaged foods, and restaurant foods). These density measures allowed for assessment of nutritional composition independent of product size. For supermarket prepared and packaged foods, densities were calculated by dividing nutrients-per-serving by serving size (grams) for the 88.6% of items with complete data before imputation (n=277 prepared bakery UPCs, 456 prepared entrees/sides, 159 prepared deli, 2,220 packaged bakery, 3,389 packaged entrees/sides, and 1,337 packaged deli). For restaurant foods, densities were calculated by dividing nutrients consumed by the amount of food (grams) for each item consumed on the dietary recall day (1,249 bakery items; 25,704 entrees/sides; 163 deli items). Supermarket and restaurant foods were classified as “high in” calories (>300kcal/100g food), sugar (>15g/100g food), saturated fat (>5g/100g food) and sodium (>500mg/100g food), based on 2018 thresholds of the Chilean Law of Food Labeling and Advertising.23
Statistical Analysis
To characterize the nutritional profiles of supermarket prepared foods, supermarket packaged foods, and restaurant foods, the median and IQR of nutrient densities were calculated, as was the percent of foods that were “high in” each nutrient. Analyses of supermarket foods were weighted by the total number of servings sold of each UPC to reflect customer demand. Primary analyses of restaurant foods included all prepared foods consumed as separate observations without applying survey weights, which gave more weight to more commonly consumed foods but did not reflect NHANES’s complex sampling design. Sensitivity analyses calculated nutrient outcomes among participants, then estimated survey-adjusted outcomes among consumers of restaurant foods after applying sampling weights. All nutrient density analyses were stratified by food category. The nutritional profile of supermarket prepared foods was examined over time by plotting the percent of items that were high in calories and each nutrient of interest at each 6-month interval with Guiding Stars data.
Analyses were conducted in 2021–2022 using SAS version 9.4 (Cary, NC) and Stata MP version 17. This study was approved by the Harvard Pilgrim Health Care IRB.
RESULTS
The number of different prepared foods offered (i.e., available for purchase) at the supermarkets more than doubled from 1,930 foods in July 2015 to 4,113 in January 2019, though the rate of growth slowed in later years (Figure 1). The percent of different food offerings that were prepared foods also approximately doubled, from 3.1% of all food items in 2015 to 6.4% in 2019.
Figure 1.
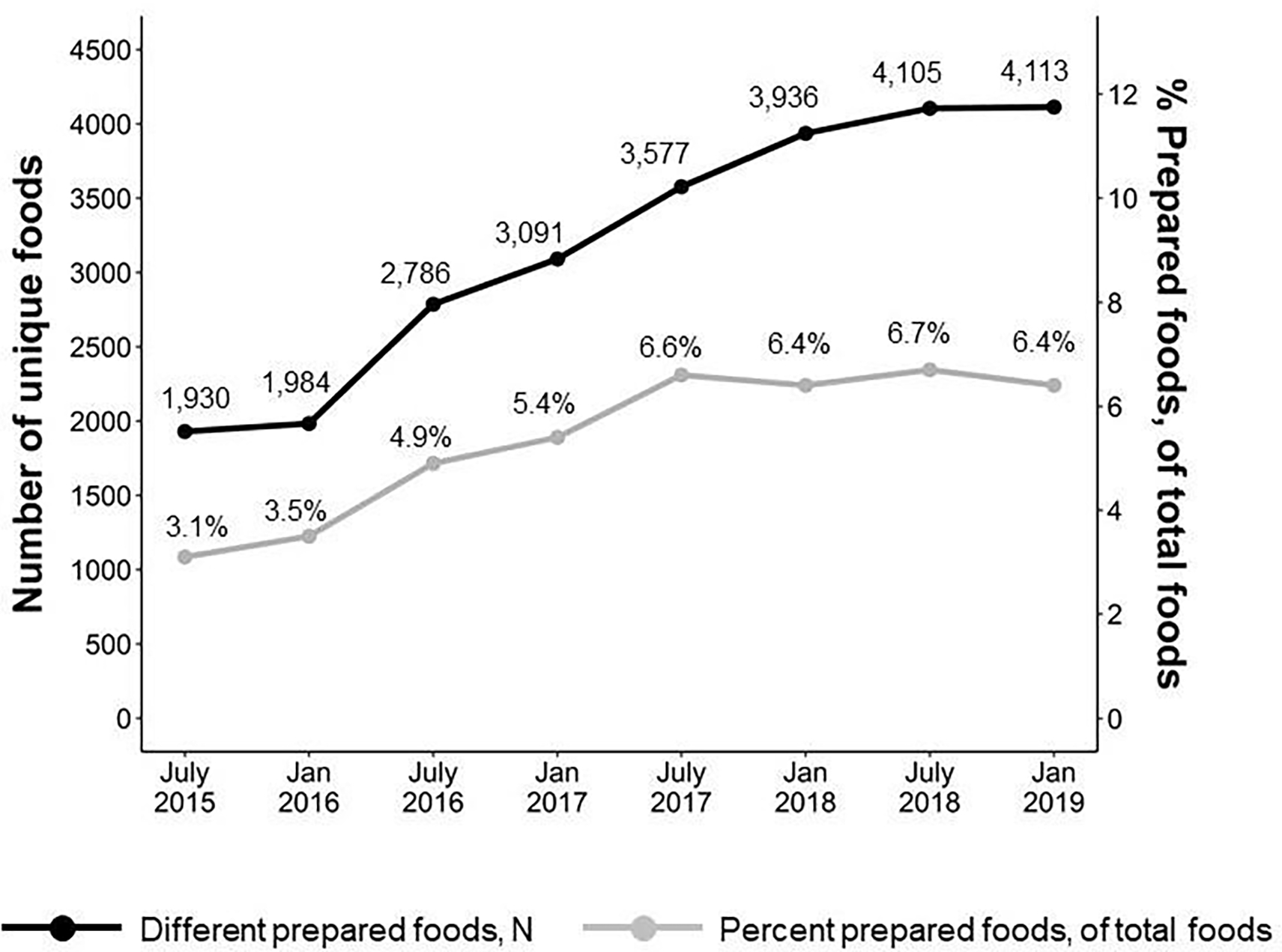
Increasing availability of prepared foods over time.
Notes: The graph shows the number of different prepared foods (black) and percent of total different foods that are prepared foods (grey) offered in supermarkets over time.
There were small increases in nutrients-per-transaction purchased from supermarket prepared foods from April 2015–March 2017 (Figure 2). In April 2015, transactions included a mean (SD) of 404.2 calories (68.2), 14.6g sugar (2.7), 9.2g saturated fat (1.7), and 1,287.2mg sodium (236.0) purchased from prepared foods. Over the following 2 years, there was a monthly increase of 1.0 calories (95% CI=0.8, 1.1), 0.08g sugar (95% CI=0.07, 0.08), 0.01g saturated fat (95% CI=0.01, 0.02), and 3.6mg sodium (95% CI=3.0, 4.1) purchased per transaction from prepared foods. The percent of total nutrients (i.e., from all items sold) that were purchased from prepared foods was stable over time except for a small decrease in percent of saturated fat from prepared foods (trend= −0.02%/month, 95% CI= −0.02, −0.02).
Figure 2.
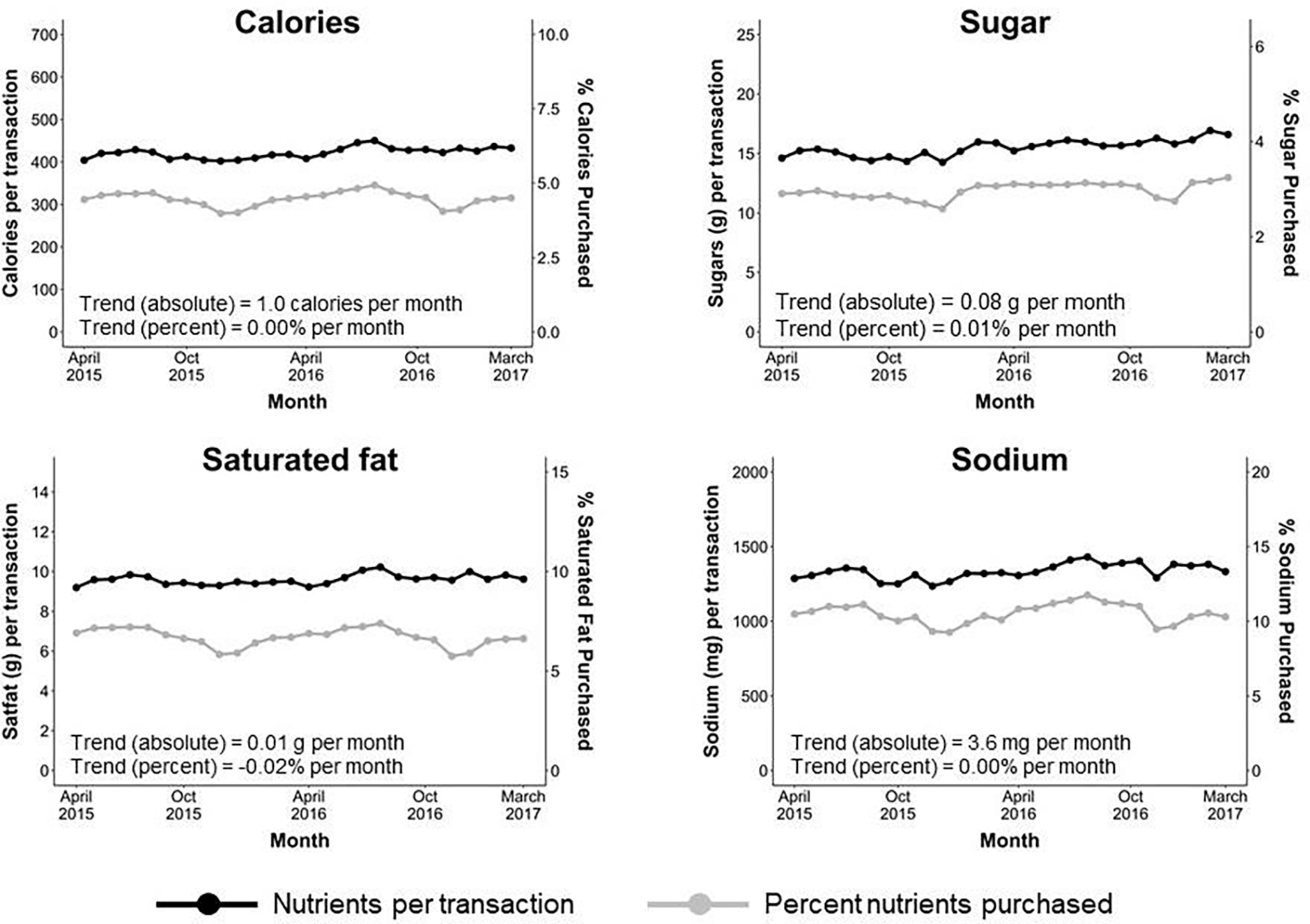
Trends in purchased nutrient content from supermarket prepared foods.
Notes: The graph shows the mean calories- and nutrients-per-transaction (black) and mean percent of calories and nutrients purchased (grey) from prepared foods across all supermarkets over time. Trends represent the absolute change in mean calories- and nutrients-per-transaction per month from generalized estimating equations (calories: trend=1.0 [95% CI=0.8, 1.1]; sugars: 0.08 [95% CI=0.07, 0.08]; saturated fat: 0.01 [95% CI=0.01, 0.02]; sodium: 3.6 [95% CI=3.0, 4.1]), as well as change in percent of calories- and nutrients-per-transaction per month that came from prepared foods (calories: trend=0.00% [95% CI=0.00, 0.00]; sugars: 0.01% [95% CI=0.00, 0.01]; saturated fat: −0.02% [95% CI= −0.02, −0.02]; sodium: 0.00% [95% CI=0.00, 0.01]).
Increases in purchases of calories from prepared foods were driven by prepared bakery items (1.2 calories/month, 95% CI=1.1, 1.2). Conversely, trends were negative for purchases of prepared deli items (−0.2 calories/month, 95% CI= −0.3, −0.2) and flat for prepared entrees/sides (0.1 calories/month, 95% CI= 0.0, 0.1) (Appendix Figure 1). The results were similar by poverty level of supermarkets’ census tracts (Appendix Figure 2).
Supermarket prepared foods had generally high calorie and nutrient densities in all food categories (Table 1). The proportion of prepared foods high in ≥1 nutritional outcome was 97% for bakery items, 61% for entrees/sides, and 92% for deli items. The proportion of prepared foods for sale that were high in calories or other nutrients was generally constant over time (Appendix Figure 3). Supermarket packaged foods followed an overall similar pattern to supermarket prepared foods, with some exceptions (e.g., 94% of purchased packaged deli items were high in saturated fat versus only 62% for prepared foods). Restaurant foods consumed by NHANES participants were similarly high in calories and unhealthy nutrients (Table 1). For example, like supermarket prepared foods, the majority of restaurant bakery items, entrees/sides, and deli items were high in ≥1 nutritional outcome (90%, 59%, and 100%, respectively). These results were very similar when examining person-level outcomes (Appendix Table 4).
Table 1.
Nutrient Profile (Median [IQR] or %) of Prepared and Packaged Foods in Supermarkets and Restaurants
| Outcome | Supermarketsa | NHANES restaurantsb | |
|---|---|---|---|
| Prepared foods | Packaged foods | ||
|
| |||
| Bakery items | |||
| Calorie density (kcal/100g) | 366.3 (322.2, 398.2) | 421.1 (372.1, 470.6) | 375.0 (330.9, 428.2) |
| Sugar density (g/100g) | 24.8 (21.2, 32.5) | 34.5 (20.5, 41.9) | 22.8 (7.2, 32.9) |
| Saturated fat density (g/100g) | 4.7 (3.5, 9.4) | 5.8 (2.9, 9.3) | 5.9 (3.0, 9.5) |
| Sodium density (mg/100g) | 318.6 (309.7, 411.8) | 357.1 (300.0, 482.1) | 347.6 (304.4, 511.6) |
| High in calories (>300kcal/100g) | 79% | 90% | 82% |
| High in sugar (>15g/100g) | 85% | 80% | 65% |
| High in saturated fat (>5g/100g) | 84% | 74% | 57% |
| High in sodium (>500mg/100g) | 8% | 23% | 26% |
| High in any nutrientc | 97% | 94% | 90% |
| Entrees/sides | |||
| Calorie density (kcal/100g) | 141.7 (100.0, 143.4) | 238.1 (152.9, 328.9) | 219.3 (102.2, 293.0) |
| Sugar density (g/100g) | 0.1 (0.0, 2.0) | 2.1 (0.6, 4.4) | 2.0 (0.4, 3.8) |
| Saturated fat density (g/100g) | 3.3 (0.6, 3.4) | 1.8 (0.0, 3.5) | 2.3 (0.3, 4.7) |
| Sodium density (mg/100g) | 511.1 (191.2, 2965.2) | 526.7 (350.0, 814.3) | 451.2 (243.0, 665.1) |
| High in calories (>300kcal/100g) | 4% | 30% | 23% |
| High in sugar (>15g/100g) | 0% | 1% | 7% |
| High in saturated fat (>5g/100g) | 53% | 31% | 23% |
| High in sodium (>500mg/100g) | 56% | 54% | 46% |
| High in any nutrientc | 61% | 64% | 59% |
| Deli items | |||
| Calorie density (kcal/100g) | 333.3 (125.0, 388.0) | 357.1 (300.0, 392.9) | 325.7 (325.0, 327.5) |
| Sugar density (g/100g) | 0.0 (0.0, 2.4) | 0.0 (0.0, 0.0) | 1.1 (1.0, 1.1) |
| Saturated fat density (g/100g) | 10.7 (1.8, 17.9) | 16.7 (10.7, 20.0) | 8.8 (8.8, 11.3) |
| Sodium density (mg/100g) | 928.6 (642.9, 1392.9) | 803.6 (642.9, 1238.1) | 814.3 (811.4, 821.4) |
| High in calories (>300kcal/100g) | 54% | 75% | 87% |
| High in sugar (>15g/100g) | 0% | 0% | 0% |
| High in saturated fat (>5g/100g) | 62% | 94% | 94% |
| High in sodium (>500mg/100g) | 83% | 94% | 98% |
| High in any nutrientc | 92% | 99% | 100% |
The supermarket sample included 277 prepared bakery items, 2,200 packaged bakery items, 456 prepared entrees and sides, 3,389 packaged entrees and sides, 159 prepared deli items, and 1,337 packaged deli items sold at 1 of supermarket chains between April 1, 2015 and March 31, 2017.
The NHANES sample included 1,249 bakery items, 25,704 entrees and sides, and 163 deli items from restaurants consumed by NHANES participants in survey cycles 2015–2016 or 2017–2018.
Percent of foods that were high in calories, sugar, saturated fat, and/or sodium.
NHANES, National Health and Nutrition Examination Survey.
DISCUSSION
This study of prepared foods sold across 2 large U.S. supermarket chains found substantial increases in prepared foods available for sale over time, coupled with small increases in calories and nutrients purchased from these foods. Prepared foods purchased from supermarkets had generally unhealthy nutritional profiles, with 61% of prepared entrees and >90% of prepared bakery and deli items high in calories or at least 1 nutrient of concern. The nutritional profile of supermarket prepared foods was similar to that of comparable packaged items sold in supermarkets and restaurant foods consumed by a nationally representative sample.
The large increase in the number of prepared foods offered by the supermarket chains from 2015–2019 suggests increasing retailer investment in prepared foods, a trend also documented in industry publications.24,25 There were also small increases in nutrients purchased from prepared foods from 2015–2017: calories purchased from prepared foods increased on average by 1.0 calories/month, a ~3% annual increase, driven by prepared bakery items (1.2-calorie/month increase, ~9% annually). Although this is among the first studies to examine purchases of supermarket prepared foods, prior studies have documented increasing sales of similar packaged foods.26,27 Notably, the percent of total calories and nutrients purchased from prepared foods did not change over time, suggesting that customers did not substitute prepared foods for packaged foods but instead may have increased overall food purchases during the study period. The addition of supermarket prepared foods to customers’ baskets could have negative health implications given their overall low nutritional quality.
Prior studies have documented that both restaurant foods12–14,28,29 and ready-to-heat/ready-to-eat supermarket packaged foods26,30–38 are typically high in calories, saturated fat, sodium, and/or sugar. This study finds a comparably unhealthy nutritional profile of supermarket prepared foods. Although median nutrient densities varied between bakery items, entrees, and deli items, the majority were high in calories or at least 1 nutrient of concern (sugar, saturated fat, sodium). Overconsumption of these nutrients has been linked to chronic disease risk and mortality.39–42 The overall similar nutritional quality of supermarket prepared foods to restaurant foods observed in this study may contradict customers’ perceptions that supermarkets are healthy retail establishments.43,44 These results also have implications for research studies on the neighborhood food environment, which typically consider supermarkets healthy and restaurants unhealthy.45 This study demonstrates that supermarkets’ prepared food options are generally as unhealthy as restaurant foods, indicating that greater nuance is needed when determining supermarkets’ contributions to the neighborhood food environments.
Together, this study’s findings underscore the importance of designing policy and behavioral interventions to encourage healthier prepared food choices in supermarkets. One possible strategy is labeling requirements. For example, the Affordable Care Act mandates calorie labeling of prepared foods in large U.S. retailers as a strategy for encouraging healthy prepared food choice and spurring product reformulation.3 Implementation of these labels was associated with small declines in prepared food purchases from restaurants46–49 and supermarkets,50 as well as the introduction of lower-calorie prepared bakery options in supermarkets.15 Calorie labels might therefore mitigate the increase in calories purchased from prepared foods observed in the present study, which examined sales prior to labeling. Other countries mandate nutrient warning labels,23 which have been found to reduce availability51,52 and purchases53,54 of unhealthy packaged foods in supermarkets; these labels could potentially also be applied to supermarket prepared foods. Another way to improve prepared food selection could be through choice architecture interventions, which target product placement and promotion (e.g., making healthy items most visible to customers). These interventions can lead to healthier food choices for both packaged55 and prepared foods.56
Limitations
Limitations of this study included that data were not available on consumption of supermarket prepared foods or on the number of people who intended to share each item. This made it difficult to contextualize the absolute amount of nutrients purchased and to examine how people consume these foods as part of their overall diet, including potential replacement of homemade or restaurant meals. Furthermore, the data did not contain information on customer demographic characteristics, precluding investigation among populations that may have different purchasing patterns, such as households with lower-income or who shop online.19,57,58 Third, data on calories and nutrients purchased from items at the supermarket hot bar were unavailable. The estimated trends of purchases from and nutritional profile of entrees/sides could be incorrect if either the popularity of hot bar items or their nutrient content changed over time. Fourth, because the purchasing data were limited to a Northeast supermarket chain, the observed trends in nutrient purchases over time and nutritional composition of supermarket prepared foods may not generalize to other regions. The chain also participates in Guiding Stars and may be more health-focused than non-participating chains. Future studies using data from other regions of the U.S. and from other supermarkets (including those not participating in nutrition labeling programs) could address these limitations. Finally, nutrient profile analyses compared foods purchased from supermarkets in the Northeast to foods consumed by a nationally representative sample; given these differences, comparisons should be interpreted with caution.
CONCLUSIONS
This study found a substantial increase in supermarket prepared food offerings over time coupled with small increases in unhealthy nutrients purchases from supermarket prepared foods. Supermarket prepared foods had generally poor nutritional quality, with a similar profile to restaurant foods. Interventions that encourage healthy prepared food choice in supermarkets are warranted.
Supplementary Material
ACKNOWLEDGMENTS
This study was supported by R01 DK115492 from NIDDK (PI: JPB). AHG was supported by T32 HL098048 and K01 HL158608 from NHLBI. The funders did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. No financial disclosures were reported by the authors of this paper.
Footnotes
CREDIT STATEMENT
Nutritional composition and purchasing patterns of supermarket prepared foods over time (Petimar et al.)
Joshua Petimar: methodology, software, formal analysis, data curation, writing – original draft, writing – review & editing, visualization; Anna H. Grummon: methodology, software, formal analysis, data curation, writing – original draft, writing – review & editing, visualization; Denise Simon: project administration, writing – review & editing; Jason P. Block: conceptualization, methodology, supervision, funding acquisition, writing – review & editing
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Mokdad AH, Ballestros K, Echko M, et al. The state of US health, 1990–2016: Burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472. 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saksena MJ, Okrent AM, Anekwe TD, et al. America’s Eating Habits: Food Away From Home. U.S. Department of Agriculture, Economic Research Service; 2018. [Google Scholar]
- 3.Food and Drug Administration. Food Labeling; Nutrition Labeling of Standard Menu Items in Restaurants and Similar Retail Food Establishments; Extension of Compliance Date. Federal Register. 2017:20825–20829. [PubMed] [Google Scholar]
- 4.Lin BH, Guthrie J, Frazao E. Nutrient contribution of food away from home. America’s eating habits: Changes and consequences. 1999;750. [Google Scholar]
- 5.Zenk SN, Powell LM, Isgor Z, Rimkus L, Barker DC, Chaloupka FJ. Prepared food availability in US food stores: a national study. Am J Prev Med. 2015;49(4):553–562. 10.1016/j.amepre.2015.02.025. [DOI] [PubMed] [Google Scholar]
- 6.Wilson R, Weber J, McKone D. Capitalizing on Opportunities in Fresh Prepared Foods. L.E.K. Consulting; 2017. https://docs.google.com/viewer?url=https%3A%2F%2Fwww.lek.com%2Fsites%2Fdefault%2Ffiles%2Finsights%2Fpdf-attachments%2FLEK_Analysis_2_Fresh_Prepared_Foods.pdf. Accessed March 17, 2022. [Google Scholar]
- 7.FMI. FMI and Nielsen Release Consumer Research on Fresh Prepared/Deli in Grocery. https://www.fmi.org/newsroom/news-archive/view/2016/11/30/fmi-and-nielsen-release-consumer-research-on-fresh-prepared-deli-in-grocery. Accessed March 17, 2022.
- 8.Manning L. Grocers look to grab-and-go as a differentiator. Grocery Dive. https://www.grocerydive.com/news/grocers-look-to-grab-and-go-as-a-differentiator/559375/. Published August 13, 2019. Accessed March 17, 2022.
- 9.Hobson K. Supermarket Prepared Meals: What to Watch Out For. Consumer Reports. 2016. https://www.consumerreports.org/food-shopping/supermarket-prepared-meals-what-to-watch-out-for/. Accessed March 17, 2022.
- 10.Meyersohn N. The rise of ‘grocerants’: Grocery stores that cook you dinner. CNN Business. https://www.cnn.com/2019/12/20/business/grocery-stores-restaurants/index.html. Published online 2019. Accessed March 28, 2022.
- 11.Juntti M. How can retail foodservice compete with fast-casual restaurants? New Hope Network. https://www.newhope.com/business-resources/how-can-retail-foodservice-compete-fast-casual-restaurants. Published online 2018. Accessed March 28, 2022.
- 12.Jarlenski MP, Wolfson JA, Bleich SN. Macronutrient Composition of Menu Offerings in Fast Food Restaurants in the U.S. Am J Prev Med. 2016;51(4):e91–e97. 10.1016/j.amepre.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 13.Wolfson JA, Moran AJ, Jarlenski MP, Bleich SN. Trends in Sodium Content of Menu Items in Large Chain Restaurants in the U.S. Am J Prev Med. 2018;54(1):28–36. 10.1016/j.amepre.2017.08.018. [DOI] [PubMed] [Google Scholar]
- 14.An R. Fast-food and full-service restaurant consumption and daily energy and nutrient intakes in US adults. Eur J Clin Nutr. 2016;70(1):97–103. 10.1038/ejcn.2015.104. [DOI] [PubMed] [Google Scholar]
- 15.Grummon AH, Petimar J, Zhang F, et al. Calorie labeling and product reformulation: A longitudinal analysis of supermarket prepared foods. Am J Prev Med. 2021;61(3):377–385. 10.1016/j.amepre.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guilding Stars Licensing Company. Guiding Stars: Nutritious Choices Made Simple. https://guidingstars.com/. Accessed September 6, 2020.
- 17.Fischer LM, Sutherland LA, Kaley LA, et al. Development and implementation of the Guiding Stars nutrition guidance program. Am J Health Promot. 2011;26(2):E55–E63. 10.4278/ajhp.100709-QUAL-238. [DOI] [PubMed] [Google Scholar]
- 18.Guiding Stars. Data and the Stars. https://guidingstars.com/data-and-the-stars/. Published online 2022. Accessed July 21, 2022. [Google Scholar]
- 19.Franckle RL, Moran A, Hou T, et al. Transactions at a northeastern supermarket chain: Differences by Supplemental Nutrition Assistance Program use. Am J Prev Med. 2017;53(4):e131–e138. 10.1016/j.amepre.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moran A, Thorndike A, Franckle R, et al. Financial Incentives Increase Purchases Of Fruit And Vegetables Among Lower-Income Households With Children. Health Aff (Millwood). 2019;38(9):1557–1566. 10.1377/hlthaff.2018.05420. [DOI] [PubMed] [Google Scholar]
- 21.Manson S, Schroeder J, Van Riper D, Kugler T, Ruggles S. IPUMS National Historical Geographic Information System: Version 16.0 [dataset]. Published online 2021. 10.18128/D050.V13.0. [DOI]
- 22.National Cancer Institute. Summary Tables: Recommendations on Potential Approaches to Dietary Assessment for Different Research Objectives Requiring Group-level Estimates. National Cancer Institute Dietary Assessment Primer. https://dietassessmentprimer.cancer.gov/approach/table.html. Accessed December 3, 2019. [Google Scholar]
- 23.Corvalan C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: Update on the Chilean law of food labelling and advertising. Obes Rev. 2019;20(3):367–374. 10.1111/obr.12802. [DOI] [PubMed] [Google Scholar]
- 24.Miller RK. Restaurant, Food & Beverage Market Research Handbook 2018–2019.
- 25.Parker J Pathways to continued growth of retail foodservice. Grocery Business. https://digitalmag.grocerybusiness.com/winsightgrocerybusiness/january_2019?pg=54#pg54. Published January 2019. [Google Scholar]
- 26.Poti JM, Mendez MA, Ng SW, Popkin BM. Is the degree of food processing and convenience linked with the nutritional quality of foods purchased by US households? Am J Clin Nutr. 2015;101(6):1251–1262. 10.3945/ajcn.114.100925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baker P, Machado P, Santos T, et al. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes Rev. 2020;21(12):e13126. 10.1111/obr.13126. [DOI] [PubMed] [Google Scholar]
- 28.Huang Y, Theis DRZ, Burgoine T, Adams J. Trends in energy and nutrient content of menu items served by large UK chain restaurants from 2018 to 2020: an observational study. BMJ Open. 2021;11(12):e054804. 10.1136/bmjopen-2021-054804. [DOI] [Google Scholar]
- 29.Dunford E, Webster J, Barzi F, Neal B. Nutrient content of products served by leading Australian fast food chains. Appetite. 2010;55(3):484–489. 10.1016/j.appet.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 30.Eyles H, Neal B, Jiang Y, Ni Mhurchu C. Estimating population food and nutrient exposure: a comparison of store survey data with household panel food purchases. Br J Nutr. 2016;115(10):1835–1842. 10.1017/S000711451600088X. [DOI] [PubMed] [Google Scholar]
- 31.Choi E, Kim BH. A comparison of the fat, sugar, and sodium contents in ready-to-heat type home meal replacements and restaurant foods in Korea. J Food Compost Anal. 2020;92:103524. 10.1016/j.jfca.2020.103524. [DOI] [Google Scholar]
- 32.Choi I, Kim WG, Yoon J. Energy intake from commercially-prepared meals by food source in Korean adults: Analysis of the 2001 and 2011 Korea National Health and Nutrition Examination Surveys. Nutr Res Pract. 2017;11(2):155. 10.4162/nrp.2017.11.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Remnant J, Adams J. The nutritional content and cost of supermarket ready-meals. Cross-sectional analysis. Appetite. 2015;92:36–42. 10.1016/j.appet.2015.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hillier SE, Nunn O, Lorrain-Smith K. An analysis of the nutritional value of UK supermarket ready meals. Proc Nutr Soc. 2020;79(OCE3):E794. 10.1017/S0029665120007806. [DOI] [Google Scholar]
- 35.Pulker CE, Farquhar HR, Pollard CM, Scott JA. The nutritional quality of supermarket own brand chilled convenience foods: an Australian cross-sectional study reveals limitations of the Health Star Rating. Public Health Nutr. 2020;23(12):2068–2077. 10.1017/S1368980020000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.AlOudat M, Magyar N, Simon-Sarkadi L, Lugasi A. Nutritional content of ready-to-eat meals sold in groceries in Hungary. Int J Gastron Food Sci. 2021;24:100318. 10.1016/j.ijgfs.2021.100318. [DOI] [Google Scholar]
- 37.Howard S, Adams J, White M. Nutritional content of supermarket ready meals and recipes by television chefs in the United Kingdom: cross sectional study. BMJ. 2012;345(dec14 14):e7607. 10.1136/bmj.e7607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kanzler S, Hartmann C, Gruber A, Lammer G, Wagner KH. Salt as a public health challenge in continental European convenience and ready meals. Public Health Nutr. 2014;17(11):2459–2466. 10.1017/S1368980014000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. Added sugar intake and cardiovascular diseases mortality among US adults. JAMA Intern Med. 2014;174(4):516–524. 10.1001/jamainternmed.2013.13563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Debras C, Chazelas E, Srour B, et al. Total and added sugar intakes, sugar types, and cancer risk: results from the prospective NutriNet-Santé cohort. Am J Clin Nutr. 2020;112(5):1267–1279. 10.1093/ajcn/nqaa246. [DOI] [PubMed] [Google Scholar]
- 41.Sacks FM, Lichtenstein AH, Wu JHY, et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory From the American Heart Association. Circulation. 2017;136(3):e1–e23. 10.1161/CIR.0000000000000510. [DOI] [PubMed] [Google Scholar]
- 42.Ma Y, He FJ, Sun Q, et al. 24-Hour Urinary Sodium and Potassium Excretion and Cardiovascular Risk. N Engl J Med. 2022;386(3):252–263. 10.1056/NEJMoa2109794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Barnes TL, Freedman DA, Bell BA, Colabianchi N, Liese AD. Geographic measures of retail food outlets and perceived availability of healthy foods in neighbourhoods. Public Health Nutr. 2016;19(8):1368–1374. 10.1017/S1368980015002864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dubowitz T, Ghosh-Dastidar M, Cohen DA, et al. Diet And Perceptions Change With Supermarket Introduction In A Food Desert, But Not Because Of Supermarket Use. Health Aff (Millwood). 2015;34(11):1858–1868. 10.1377/hlthaff.2015.0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Block J, Seward M, James P. Food, environment, and health. In: Duncan DT, Kawachi I, eds. Neighborhoods and Health. Oxford University Press; 2018:247–278. 10.1093/oso/9780190843496.003.0009. [DOI] [Google Scholar]
- 46.Cawley J, Susskind A, Willage B. The Impact of Information Disclosure on Consumer Behavior: Evidence from a Randomized Field Experiment of Calorie Labels on Restaurant Menus. J Policy Anal Manage. 2020;39(4):1020–1042. 10.1002/pam.22219. [DOI] [Google Scholar]
- 47.Petimar J, Zhang F, Cleveland LP, et al. Estimating the effect of calorie menu labeling on calories purchased in a large restaurant franchise in the southern United States: quasi-experimental study. BMJ. 2019;367:l5837. 10.1136/bmj.l5837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Petimar J, Zhang F, Rimm EB, et al. Changes in the calorie and nutrient content of purchased fast food meals after calorie menu labeling: A natural experiment. PLOS Med. 2021;18(7):e1003714. 10.1371/journal.pmed.1003714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bollinger B, Leslie P, Sorensen A. Calorie Posting in Chain Restaurants. Am Econ J Econ Policy. 2011;3(1):91–128. 10.1257/pol.3.1.91. [DOI] [Google Scholar]
- 50.Petimar J, Grummon AH, Zhang F, et al. Assessment of Calories Purchased After Calorie Labeling of Prepared Foods in a Large Supermarket Chain. JAMA Intern Med. 2022;182(9):965–973. 10.1001/jamainternmed.2022.3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Reyes M, Taillie LS, Popkin B, Kanter R, Vandevijvere S, Corvalan C. Changes in the amount of nutrient of packaged foods and beverages after the initial implementation of the Chilean Law of Food Labelling and Advertising: A nonexperimental prospective study. PLoS Med. 2020;17(7):e1003220. 10.1371/journal.pmed.1003220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Barahona N, Otero C, Otero S, Kim J. Equilibrium effects of food labeling policies. SSRN Electronic Journal. Published online 2021. 10.2139/ssrn.3698473. [DOI] [Google Scholar]
- 53.Taillie LS, Reyes M, Colchero MA, Popkin B, Corvalan C. An evaluation of Chile’s Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: A before-and-after study. PLoS Med. 2020;17(2):e1003015. 10.1371/journal.pmed.1003015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taillie LS, Bercholz M, Popkin B, Reyes M, Colchero MA, Corvalan C. Changes in food purchases after the Chilean policies on food labelling, marketing, and sales in schools: a before and after study. Lancet Planet Health. 2021;5(8):e526–e533. 10.1016/S2542-5196(21)00172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Foster GD, Karpyn A, Wojtanowski AC, et al. Placement and promotion strategies to increase sales of healthier products in supermarkets in low-income, ethnically diverse neighborhoods: a randomized controlled trial. Am J Clin Nutr. 2014;99(6):1359–1368. 10.3945/ajcn.113.075572. [DOI] [PubMed] [Google Scholar]
- 56.Thorndike AN, Gelsomin ED, McCurley JL, Levy DE. Calories Purchased by Hospital Employees After Implementation of a Cafeteria Traffic Light-Labeling and Choice Architecture Program. JAMA Netw Open. 2019;2(7):e196789. 10.1001/jamanetworkopen.2019.6789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mancino L, Guthrie J, Ver Ploeg M, Lin BH. Nutritional Quality of Foods Acquired by Americans: Findings from USDA’s National Household Food Acquisition and Purchase Survey. Economic Research Service; 2018. [Google Scholar]
- 58.Zatz LY, Moran AJ, Franckle RL, et al. Comparing Online and In-Store Grocery Purchases. J Nutr Educ Behav. 2021;53(6):471–479. 10.1016/j.jneb.2021.03.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


