Abstract
Introduction
Cost is a major barrier to medication accessibility. While a minority of adults experience problems affording their medications, older adults are particularly vulnerable due to increased polypharmacy and fixed incomes.
Clinicians can help reduce cost-related non-adherence and improve medication affordability; however, opportunities to improve affordability are often missed due to failure of the patient or clinician to discuss the issue.
Objective
Identify the incidence and resolution of cost-related conversations between patients and clinicians during primary care visits.
Methods
We conducted this quality improvement project at a primary care office. Student pharmacists observed in-person encounters with patients ≥65 years of age and documented the incidence of cost-related conversations and who initiated the conversation. After the visit, they asked if the patient had affordability issues. Patients and clinicians were blinded to the study purpose and hypothesis.
Results
Students observed 79 primary care visits. Cost conversations (medication or non-medication related) occurred in 37% (29/79) of visits. Having concerns about affordability did not impact the likelihood of conversation about non-medication related healthcare costs (RR = 1.21 95% CI 0.35–4.19, p = 0.67) or medication related costs (RR = 0.86 95% CI 0.13–5.65, p = 1.0).
Conclusion
Our results indicated that cost conversations did not routinely occur at our site. Failure to discuss costs, especially for patients with underlying cost concerns, may lead to cost related non-adherence and worse outcomes.
Keywords: Primary care, Elderly, Cost, Conversation, Medication
Abbreviations: CI, Confidence Interval; COPD, Chronic Obstructive Pulmonary Disease; RR, Relative Risk; SD, Standard Deviation
1. Introduction
Medication non-adherence is responsible for nearly $100 billion in yearly excess healthcare costs due to hospitalizations.1 Cost is one cause of non-adherence with 6.8% of adults experiencing cost-related medication non-adherence.2 Cost related non-adherence is prevalent in older adults as many are living on a fixed income and taking multiple medications. Clinicians can help reduce cost related non-adherence and improve medication affordability.3 However, opportunities to improve affordability are often missed due to failure of either the patient or clinician to discuss the issue. Clinicians may fail to discuss costs due to lack of awareness of, or difficulty calculating, medication costs,4,5 while patients may not feel comfortable discussing costs with their healthcare team.6,7 The incidence of conversations around cost varies from study to study and may be affected by factors such as method of reporting (e.g. observation vs survey), setting (e.g. specialty vs primary care), and disease state.6, 7, 8 Yet, a common finding is that there is a discordance between patients' desire to discuss costs and the prevalence of cost conversations.7
The goal of this project was to identify the incidence and resolution of cost-related conversations between patients and clinicians during primary care visits.
2. Methods
This quality improvement project was conducted at a primary care office located in Pittsburgh, Pennsylvania. The project was reviewed by the health system's institutional review board and determined to not be human subject research. The office consisted of eight clinicians, one clinician was unavailable, leaving five physicians and two nurse practitioners available for observation. Each participating clinician had multiple visits observed. Four pharmacy students conducted the observations over a two week period, from May 31, 2022 until June 13, 2022. Visits were included if the patient was 65 years or older presenting for a primary care-related reason. Patients were excluded if the visit was conducted via video or phone, or if the patient was on Medicaid, had documented cognitive impairment, or declined observation. Physicians were also able to opt out of observation, and those visits were also excluded.
Patients were identified by reviewing the clinic schedule using our inclusion and exclusion criteria. After a patient checked in and gave consent, their visit with both the medical assistant and clinician (physician or nurse practitioner) was observed. During the visit, observers used a standardized data collection form (Appendix 1). This form was used to organize collection of data from the electronic health record (e.g., demographics), the visit observation (e.g., occurrence of a cost conversation), and the post visit discussion with the patient (e.g., affordability concerns). All clinic staff were blinded to the purpose of the project. Medication-cost conversations were defined as any direct mention of cost as it pertained to medication. Non-medication related cost conversations consisted of mention of any costs associated with health care, such as coverage of referrals, cost of copays for office visits, or cost of labs. After the clinician finished the visit and left the room, but before the patient was checked out, the student asked the patient three questions. The questions were “What insurance do you use?”, “Do you use any of the following to pay for medications?” and “Does the cost of your medication affect your ability to take them, and if so, how often?” and then the patient was provided a corresponding list that included PACE (a state funded program in Pennsylvania for those 65 and older based on income thresholds), manufacturer copay cards, 340B pricing, patient assistance programs, and GoodRx© (a discount card for cash paying customers). If patients reported affordability concerns, the observers provided resources, including the clinic pharmacist's phone number.
The primary outcome was the incidence of cost-related conversations. Secondary outcomes included which person initiated the conversation, the number of patients who identified having medication affordability issues, and describing the resources utilized to address affordability.
Descriptive statistics were calculated for patient baseline characteristics, the presence of cost related (medication and non-medication) conversations, and the initiator of each conversation. The incidence of cost conversations were compared between patients who had affordability concerns and those that did not using a Fisher's exact test. In addition, Fisher's exact tests were used to examine whether other potential factors impacting cost related non-adherence were associated with the occurrence of a cost conversation.3,9
3. Results
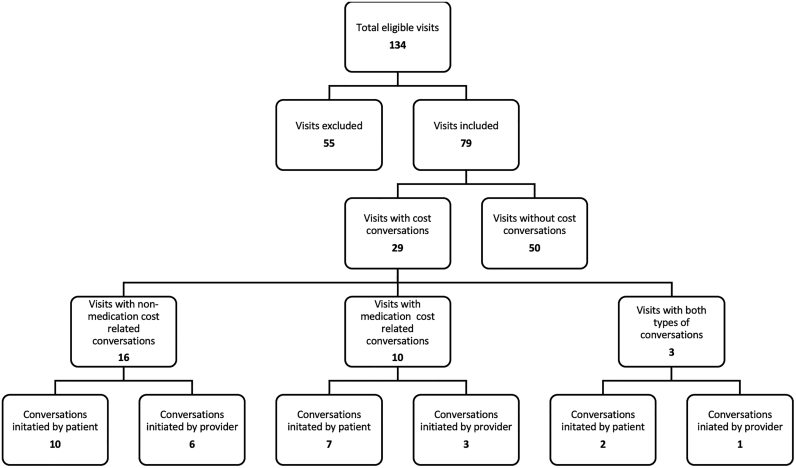
Of 134 potential patient visits, 79 visits were observed (Fig. 1). Patients observed were mostly white (92.4%), female (78.5%), and on Medicare (87.3%) with an average age of 73. In addition, the majority were established patients (94.9%), had heart disease (93.7%), presented for a routine physical or follow-up (43.1%), and were on an average of 5.78 prescription medications with an average of 0.51 branded medications (Table 1). Out of 79 observed visits, there were 29 visits (37%) where a cost conversation occurred between the clinician and patient. Of these, 16 visits had a conversation about non-medication healthcare costs, ten had a conversation about medication related costs, and three had a conversation about both; thus there were 32 total conversations (19 non-medication healthcare cost conversations and 13 medication related cost conversations) about cost in 29 visits. Patients initiated 53% (17/32) of the conversations about cost (Fig. 1). Each clinician initiated a cost conversation at least once, with two clinicians initiating two cost conversations, and two initiating four. Of the 29 visits with a cost conversation, clinicians offered cost-related resources in 28% (8/29) of visits. These resources included: referral to a specialty provider (1), referral to a local pharmacy for a covered vaccination (1), change in therapy to a less cost-prohibitive medication (1), referral to office staff for a prior authorization (2), referral to the hospital systems 340B program (2), and referral to a manufacturer coupon (1). Patients reported using various cost-saving measures when asked after their visit: 15 patients used GoodRx©, eight used PACE, two used manufacturer coupons, one patient used the hospital systems 340B program, and one patient used a patient assistance program from a manufacturer (Table 2).
Fig. 1.
Breakdown of cost conversation occurrence and conversation initiation.
Table 1.
Baseline characteristics of the total patients included for observation (n = 79).
| Baseline Characteristics (n = 79) | |
|---|---|
| Sex, N (%) | |
| Male | 17 (21.5) |
| Female | 62 (78.5) |
| Age, Years | |
| Average (SD) | 73.38 (±6.04) |
| Median | 72 |
| Race, N (%) | |
| White/Caucasian | 73 (92.4) |
| Black/African American | 4 (5.1) |
| Asian | 0 (0) |
| American Indian/Alaskan Native | 0 (0) |
| Native Hawaiian/Pacific Islander | 0 (0) |
| Other | 2 (2.5) |
| Chronic Disease States, N (%) | |
| Asthma/COPD | 12 (15.2) |
| Heart Disease | 74 (93.7) |
| Diabetes | 21 (26.6) |
| Cancer | 4 (5.1) |
| Vascular Disease | 9 (11.4) |
| Rheumatoid Arthritis | 3 (3.8) |
| Chronic Pain | 34 (43.0) |
| Anxiety/Depression | 20 (25.3) |
| Prescription Insurance Type, N (%) | |
| Medicare | 69 (87.3) |
| Commercial Insurance | 10 (12.7) |
| No Insurance | 0 (0) |
| Reason for Patient Visit, N (%) | |
| Annual Wellness Visit | 28 (35.4) |
| Physical Routine/Follow Up | 34 (43.0) |
| Sick Visit/Acute Need | 15 (19.0) |
| Transitions of Care | 1 (1.3) |
| New Patient Visit, N (%) | |
| New Patient | 4 (5.1) |
| Established Patient | 75 (94.9) |
| Number of Prescription Medications per Patient | |
| Average (SD) | 5.78 (±3.80) |
| Median | 5 |
| Total Number of Branded Prescription Medications per Patient | |
| Average (SD) | 0.51 (±0.92) |
| Median | 0 |
Table 2.
Patient reported information about insurance, resources, and cost concerns.
| Prescription Insurance Type, N(%) | |
| Medicare | 69 (87.3) |
| Commercial Insurance | 10 (12.7) |
| No insurance | 0 (0) |
| Resources Used By Patients To Pay For Medication, N (%) | |
| GoodRx | 15 (19.0) |
| PACE | 8 (10.1) |
| Manufacturer Coupons | 2 (2.5) |
| Hospital System's 340b Program | 1 (1.3) |
| Manufacturer Patient Assistance Program | 1 (1.3) |
| None Reported | 58 (73.4) |
| Patients Who Reported Cost Affected Adherence, N (%) | |
| Yes | 7 (8.9) |
| No | 72 (91.1) |
Out of the 79 patients included in the project, seven patients indicated affordability issues affected their ability to adhere to medications. Only one patient who expressed concern had a medication-related cost conversation with their clinician, while two out of the seven discussed non-medication healthcare costs with their clinician. Having concerns about affordability did not impact the likelihood of having either a conversation about non-medication related healthcare costs (RR = 1.21 95% CI 0.35–4.19, p = 0.67) or a conversation about medication related costs (RR = 0.86 95% CI 0.13–5.65, p = 1.0). Several variables were examined for association with cost conversations and we found no significant results (Table 3).
Table 3.
Association between selected variables and the occurrence of cost conversations.
| Secondary Outcomes | RR (95% CI) | p-value |
|---|---|---|
| Taking 5 or more medications AND having a cost-related conversation | 1.59 (0.83–3.05) | 0.16 |
| Taking at least 1 brand name medication AND having a cost-related conversation | 0.97 (0.52–1.82) | 1 |
| Having a chronic visit AND a cost conversation (as compared to having an acute visit) | 1.46 (0.60–3.58) | 0.55 |
| Having affordability concerns AND a cost-related conversation | 1.19 (0.48–2.95) | 0.7 |
4. Discussion
The findings from this quality improvement project show that discussions around cost, medication related or non-medication related, occurred in less than half of the visits observed. These findings align with existing literature which found that cost conversations occur in 4.5%–65% of visits depending on the location and patient population with an average of 30%.5,8 This project's rate of 38% falls near the middle of this range. Compared to clinicians, more patients brought up the discussion about affordability and insurance coverage. Similarly aligned with the literature,8 there was a discordance between patients reporting cost concerns and raising these cost concerns with the clinician. This discrepancy indicates an opportunity for clinicians to be proactive in asking patients about affordability as patients may not bring forward these concerns.
The incidence of cost conversations may reflect the nature of the patient population and visits observed. Observed visits discussed a wide variety of medical conditions, most of which were for routine follow-up, but 19% of observed visits were for acute care focused visits. One acute care focused visit included a cost related conversation, which may suggest clinicians have a differently focused workflow when conducting acute care or sick visits. Additionally, most patients were already established with these clinicians so previous conversations could have occurred. All patients had insurance and these patients were on mostly generic medications, so the perceived burden that medication costs have on these patients may be low.
Of patients with cost concerns, 28% were offered some sort of assistance from the clinician to mitigate costs. The rates and type of assistance offered may indicate a further opportunity to improve medication affordability by optimizing what resources are offered. Many patients may be attempting to address affordability independently through resources like GoodRx©, but this resource may not be the best patient-specific choice. Using discount cards, high cost medications may remain unaffordable and the patient's out-of-pocket spending will not contribute to reaching a high deductible or catastrophic coverage for Medicare Part D thresholds. Conversely, information and referral to enrollment in PACE, a state medication assistance program for those 65 and older, was not offered in the observed visits. Eight patients were already using PACE, so it is unclear whether PACE was not discussed in visits due to previous discussions, patients were previously identified as ineligible, or a lack of knowledge by clinicians or patients regarding PACE. Follow up studies could identify clinician decision making and knowledge regarding affordability resources. Each patient's specific medications and eligibility for various programs varies and the results from this project suggest a larger role for pharmacy and social work in optimizing the resources selected. These allied team members could aid in addressing affordability either directly with patients or through a systematic process to support and guide prescribers.
This project had several strengths including observation of clinical encounters in their entirety. Data collection started when vitals were collected by the medical assistants and observed through the entire encounter with the clinician. Observing the full visit makes it unlikely that we missed any potential conversations about cost. Several past studies have utilized recordings and surveys, which may not accurately capture all cost conversations due to recall bias.8 Additionally, access to the patient's electronic health record allowed for contextualizing the conversations by determining whether the patient was new or existing as well as any other relevant background. Another strength of our project is that the clinicians were blinded to the purpose of the study. Blinding the clinicians encouraged an accurate representation of the likelihood of cost conversations occurring. If clinicians were told the purpose was to evaluate cost conversations, they may have been more inclined to have those conversations. Administering the patient surveys after the visit rather than before also prevented the patient from feeling compelled to discuss cost if they had not planned to before the survey.
The findings of this project may be limited in that the majority of visits were with returning patients, so it is unknown if medication affordability was discussed during a prior visit. Visits were also observed in the first half of the year, so patient affordability concerns may occur later in the year if patients enter the Medicare coverage gap their total medication costs (including costs paid by insurance and patient out-of-pocket costs) exceed a threshold. Workflow challenges caused us to miss the beginning of a few encounters where medical assistants roomed the patient, thus a few cost conversations could have been missed. However, the risk of missing a conversation during this time is unlikely as no cost conversations occurred in this portion of the appointment during the remaining visits and all interactions with the prescribers were captured in their entirety. Due to the single-center setting and homogeneous population analyzed in this project, the results may not be widely applicable; however, they may be useful for clinics with a similar census and workflow. Finally, this project is limited in that few patients expressed affordability concerns limiting the ability (and statistical power) to understand the relationships between cost conversations and the presence of affordability concerns. The patient survey was designed to link affordability to a tangible outcome of reduced adherence. However, this question is based on a patient reported outcome and a patient could desire further discussion on affordability despite taking their medications regularly. Patient reported cost-related nonadherence may also be influenced by social desirability bias, or the patient's desire to respond in a favorable, socially acceptable nature.10,11 Given the context of the medical office setting, patient's may have underreported nonadherence due to embarrassment around their financial status.11
5. Conclusions
Our results indicate that cost conversations do occur in primary care settings, but these discussions may occur inconsistently and patients that report non-adherence due to cost may not be consistently engaged in conversations regarding cost. Failure to discuss costs, especially with patients with underlying cost concerns may lead to cost related non-adherence and worse health outcomes. Future studies could examine why cost is not consistently discussed as well as explore ways to better identify and intervene with optimized resources for patients with affordability concerns.
Funding
This project did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Osterberg L., Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 2.Chung G.C., Marottoli R.A., Cooney L.M., Jr., Rhee T.G. Cost-related medication nonadherence among older adults: findings from a nationally representative sample. J Am Geriatr Soc. 2019;67(12):2463–2473. doi: 10.1111/jgs.16141. [DOI] [PubMed] [Google Scholar]
- 3.Choudhry N.K., Denberg T.D., Qaseem A. Clinical Guidelines Committee of American College of Physicians. Improving adherence to therapy and clinical outcomes while containing costs: opportunities from the greater use of generic medications: best practice advice from the clinical guidelines committee of the american college of physicians. Ann Intern Med. 2016;164(1):41–49. doi: 10.7326/M14-2427. [DOI] [PubMed] [Google Scholar]
- 4.Sloan C.E., Millo L., Gutterman S., Ubel P.A. Accuracy of physician estimates of out-of-pocket costs for medication filling. JAMA Netw Open. 2021;4(11) doi: 10.1001/jamanetworkopen.2021.33188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allan G.M., Lexchin J., Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9) doi: 10.1371/journal.pmed.0040283. (PMID: 17896856; PMCID: PMC1989748) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harrington N.G., Scott A.M., Spencer E.A. Working toward evidence-based guidelines for cost-of-care conversations between patients and physicians: a systematic review of the literature. Soc Sci Med. 2020;258 doi: 10.1016/j.socscimed.2020.113084. [DOI] [PubMed] [Google Scholar]
- 7.Everson J., Henderson S.C., Cheng A., Senft N., Whitmore C., Dusetzina S.B. Demand for and occurrence of medication cost conversations: A narrative review. Med Care Res Rev. 2022 doi: 10.1177/10775587221108042. 10775587221108042. [DOI] [PubMed] [Google Scholar]
- 8.Hunter W.G., Hesson A., Davis J.K., et al. Patient-physician discussions about costs: definitions and impact on cost conversation incidence estimates. BMC Health Serv Res. 2016;31(16):108. doi: 10.1186/s12913-016-s1353-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Briesacher B.A., Gurwitz J.H., Soumerai S.B. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22(6):864–871. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bergen N., Labonté R. “Everything is perfect, and we have no problems”: detecting and limiting social desirability bias in qualitative research. Qual Health Res. 2020;30(5):783–792. doi: 10.1177/1049732319889354. [DOI] [PubMed] [Google Scholar]
- 11.Piette J.D., Heisler M., Wagner T.H. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164(16):1749–1755. doi: 10.1001/archinte.164.16.1749. [DOI] [PubMed] [Google Scholar]