Abstract
Objectives
Small area analysis is a health services research technique that facilitates geographical comparison of services supply and utilization rates between health service areas (HSAs). HSAs are functionally relevant regions around medical facilities within which most residents undergo treatment. We aimed to identify HSAs for psychiatric outpatient care (HSA‐PSY) in Switzerland.
Methods
We used HSAr, a new and automated methodological approach, and comprehensive psychiatric service use data from insurances to identify HSA‐PSY based on travel patterns between patients' residences and service sites. Resulting HSA‐PSY were compared geographically, demographically and regarding the use of inpatient and outpatient psychiatric services.
Results
We identified 68 HSA‐PSY, which were reviewed and validated by local mental health services experts. The population‐based rate of inpatient and outpatient service utilization varied considerably between HSA‐PSY. Utilization of inpatient and outpatient services tended to be positively associated across HSA‐PSY.
Conclusions
Wide variation of service use between HSA‐PSY can hardly be fully explained by underlying differences in the prevalence or incidence of disorders. Whether other factors such as the amount of services supply did add to the high variation should be addressed in further studies, for which our functional mapping on a small‐scale regional level provides a good analytical framework.
Keywords: geography, psychiatry, service use, small area analysis
1. INTRODUCTION
Mental health services are highly complex systems with different treatment settings (e.g., inpatient and outpatient), and they often have geographically varying structures and configurations of psychiatric care (hospitals, outpatient clinics, practitioners in private practice, home treatment, etc.). This complexity makes the analysis and comparison of mental health service systems highly demanding. In Switzerland, for instance, the responsibility of 26 Cantons (Federal States) for local health services planning and a dual remuneration system with a strict distinction between outpatient and inpatient services lead to regionally diverse psychiatric care systems. Data on service use are stored in various sources (databases) and on various levels of aggregation at public federal and cantonal institutions and at private insurance companies.
Small area analysis (SAA) is a health services research technique that facilitates geographical comparison of population‐based health services expenditures and utilization rates between hospital service areas or health service areas (HSAs) (Goodman & Green, 1996; Paul‐Shaheen et al., 1987; Wennberg & Gittelsohn, 1973). HSAs are geographical regions around medical facilities (e.g., hospitals, outpatient clinics or physicians in private practice) within which most residents undergo treatment. In contrast to administrative units, which are typically bound to geopolitical entities (Kilaru et al., 2015), HSAs reflect the actual travel patterns of patients (patient‐flows) between residence and service sites (Klauss et al., 2005) and therefore represent spatial units that are more relevant with respect to health care use and planning (functional relevance).
Comparisons of small areas have repeatedly demonstrated wide variations in health care expenditures and utilization rates—both in medical and surgical (Ashton et al., 1999; Birkmeyer et al., 1998; Chassin et al., 1986; Coyte et al., 1996; Gittelsohn & Powe, 1995; Keller et al., 1990; Knickman & Foltz, 1984; Lewis, 1969; McPherson et al., 1982; Wennberg & Gittelsohn, 1973) as well as in psychiatric services (Almog et al., 2004; Ashton et al., 1999; Curtis et al., 2009; Gottlieb et al., 2021; Hendryx & Rohland, 1994; Hendryx et al., 1995; Okumura et al., 2019; Watts et al., 2011). Such‐wide variations cannot be fully explained by underlying differences in the prevalence or incidence of conditions. Whereas some areas may suffer from insufficient supply of medical care, research using SAA has repeatedly suggested the existence of supplier‐induced demand for health services (Watts et al., 2011; Wennberg, 1985, 1993; Wennberg et al., 1982). Rates of medical procedures (Wennberg & Gittelsohn, 1973) and of hospitalizations for general medical illnesses (Wennberg et al., 1987) have been shown to be related more strongly to the supply of a service than to the need for that service. This raises concerns that, once the true need for a health service has been served, excess supply must be consumed by those who do not actually need the services and are therefore exposed to risks without the potential for benefit (Fisher et al., 2003; Thornicroft & Tansella, 2009). Even though the concept of supplier‐induced effects was critically discussed in more recent literature (Leonard et al., 2009; Mercuri & Gafni, 2011, 2018), there is little debate that a better understanding of (geographical) variation in medical care and of its drivers may help to improve health care systems and their cost‐effectiveness (Drake et al., 2008; Harrison et al., 2019).
The techniques of SAA have been underused to comprehend psychiatric services provision and use (Drake et al., 2008; Watts et al., 2011). Previous attempts to map mental health services predominately stem from the USA (Almog et al., 2004; Ashton et al., 1999; Curtis et al., 2009; Gottlieb et al., 2021; Hendryx et al., 1995; Hendryx & Rohland, 1994; Watts et al., 2011), they were often limited to specific subpopulations (e.g., insurees of the Department of Veterans Affairs) (Ashton et al., 1999; Gottlieb et al., 2021) or they predominately focused on inpatient care (Almog et al., 2004; Hendryx et al., 1995; Stocker et al., 2016; Watts et al., 2011). However, if the inpatient and the outpatient mental health care settings are considered complementary, the comprehensive study of both treatment settings is necessary to better understand mental health services systems. In many high‐income countries there has been a shift from inpatient to community and outpatient care over recent decades (Thornicroft et al., 2016). Outpatient care is usually organized on a much smaller spatial scale than inpatient care (Gottlieb et al., 2021) and traveling times to service sites seems to be much more important in outpatient care (Stulz et al., 2018), making the relatively large hospital referral areas too crude a measure to capture the fine‐grained regional differences in outpatient service supply and use (Eveland et al., 1998).
In this study, we therefore aimed at using SAA and health insurance data on use of outpatient services to identify HSAs across Switzerland. In a subsequent step, we combined data on inpatient service use from a different source (databases) to better understand the relationship between utilization of inpatient and outpatient services in Switzerland. The aim of this paper was to describe the application of a new and automated methodological approach (Haynes et al., 2020) to identify psychiatric HSAs for outpatient treatment (HSA‐PSY) in Switzerland based on detailed and comprehensive psychiatric service use data. The resulting HSA‐PSY were described and compared geographically, demographically and with respect to the use of inpatient and outpatient psychiatric services. These HSA‐PSY, and forthcoming analyses based on them, may serve as a health care planning tool for regional authorities and foster supra‐regional coordination regarding health care planning activities.
2. METHOD
2.1. Data sources
To delineate HSA for psychiatric outpatient services (HSA‐PSY) in Switzerland, we used the pooled data of all health insurance companies in Switzerland for the most recently available years 2014–2017. Swiss health insurance data is gathered at the SASIS AG (SASIS AG, 2021) and includes information on all health services (diagnostics, therapies, and other procedures) covered by mandatory basic health insurance. For the current study, we used the following information on all outpatient mental health services recorded in the central database of the SASIS AG: Community of residence of the patient, postcode of the service provider, number of outpatient visits, year of outpatient visit, and number of service providers per postcode. The number of psychiatric outpatient visits is defined as the number of calendar days with utilization of ambulatory psychiatric services covered basic health insurance. Basic health insurance is compulsory for all residents in Switzerland and covers the costs for inpatient and outpatient medical care detailed in the Swiss Federal Law on Health Insurance (Federal Office of Public Health, 2021). Health insurers in Switzerland must ensure equal enrolment, range of services and treatment for everyone, making no distinctions on the basis of health status or other indicators. The health insurance companies in Switzerland provide detailed data on health services covered by basic insurance to the SASIS database (coverage almost 100% in 2014–2017; Schuler et al., 2020).
Whereas the SASIS database was used to delineate the HSA‐PSY and to calculate outpatient service use within these HSA‐PSY, the medical statistics dataset of the Federal Statistical Office (Bundesamt für Statistik, 2021a) was used to calculate hospital use (e.g., bed days per capita) per HSA‐PSY. This national database includes socio‐demographic, administrative and medical information (e.g., diagnoses) on all inpatient treatments provided by Swiss hospitals.
To calculate utilization rates, number of residents living in the identified area was obtained from the Federal Statistical Office for the census year 2017 (Bundesamt für Statistik, 2020).
2.2. Delineation of HSA for psychiatric outpatient services (HSA‐PSY) in Switzerland
There were two conflicting requirements when defining the HSA‐PSY: On the one hand, the HSA‐PSY should be as small as possible (SAA) because smaller regions tend to be more homogeneous and enable identification of differences, which are not recognizable on a more aggregated level (Tobler's first law of geography; Tobler, 1970). On the other hand, the resulting HSA‐PSY should be as self‐containing as possible; that is, most residents of an HSA‐PSY should undergo outpatient treatment at a service site in the HSA‐PSY where they live to enable comparisons between largely independent neighbouring HSA‐PSY.
We delineated HSA‐PSY based on outpatient data in this study. Outpatient services are usually organized on a smaller spatial scale than inpatient services and the resulting HSA‐PSY therefore provide a better basis for future analyses of health services provision and use in the tradition of SAA, which calls for small and homogeneous regions. We delineated HSA‐PSY based on travel flows between patients' residences and outpatient service sites using the R‐Package by Haynes et al. (2020) based on the methodological approach developed by Wennberg and Gittelsohn (1973). Each patient‐flow was defined by an origin (the residential political community of the patient), a destination (the postcode area of the service provider), and the size of the flow (the number of outpatient visits). To delineate HSA‐PSY, we considered all psychiatric services recorded in the SASIS database, which had been provided in an outpatient setting (either in private practices or by institutional outpatient service providers).
To enable comprehensive analyses of in‐ and outpatient services in a later stage, we started delineation of HSA‐PSY with the 706 Swiss MedStat regions, which are used within the context of governmental health data collection and which are the smallest common regional level on which Swiss inpatient data are recorded. The Swiss MedStat regions are based on aggregated postcodes and are of sufficient size to warrant anonymity of patients but they are still small enough to provide an appropriate starting point for HSA delineation (Bundesamt für Statistik, 2021b). In a first step of analysis, outpatient‐flows were aggregated on the level of these MedStat regions. While service providers (destinations of patient flows) could be easily allocated to these MedStat regions based on their postcode, for patients the community of residence (but no postcode) was recorded in the SASIS database. Therefore, patients living in larger communities (i.e., cities), which comprised multiple MedStat regions, could not be unequivocally allocated to one specific MedStat region. We therefore merged MedStat regions within the same community into one overarching, synthetic MedStat region (MedStatSyn regions). Like‐wise, in cases where the boarders of the communities were not congruent with the boarders of postcode areas (i.e., MedStat regions), neighbouring MedStat regions were merged into overarching MedStatSyn regions if such merging increased the “congruency of the external boarder” (the fraction of buildings in a community, which could be allocated to one MedStat or MedStatSyn region, respectively, was used as measure to judge the “congruence of the external boarder”). This‐step of pre‐processing resulted in 563 MedStatSyn regions.
To delineate population‐based HSA‐PSY from patient‐flows between these MedStatSyn regions, we then used the automated, reproducible and objective method developed by Haynes et al. (2020). In contrast to other approaches to delineate HSAs (Delamater et al., 2013; Franconi et al., 2017; Hu et al., 2018; Jia, 2016; Jia et al., 2017; Wang et al., 2020), this approach can also deal with regions where no interventions were performed, it allows for spatial contiguity of HSAs, and is implemented in a readily available open access program, the R package HSAr (Haynes, 2020). The iterative process to delineate HSA‐PSY for Swiss outpatient psychiatric care providers with HSAr encompassed the following steps:
Step 1: Identify destinations of patient flows, that is, MedStatSyn regions with service sites (outpatient clinics or physicians in private practice).
Step 2: For each of these destinations (representing a potential HSA), identify all neighbouring MedStatSyn regions, which are sharing a common border with the destination region.
Step 3: Merge the neighbouring MedStatSyn regions with the destination region, if most patients living in the neighbouring (origin) MedStatSyn region travel to service providers in the destination region.
Step 4: Iterate steps 2 and 3 until all patient origin MedStatSyn regions are allocated to the neighbouring destination region (HSA) with most significant flow.
Step 5: Check if all MedStatSyn regions are allocated to a destination. For unallocated regions (either regions without any interventions or regions with primarily long distance flows), identify the neighbouring regions and allocate the unassigned origin region to the neighbouring HSA‐PSY receiving most inflow, that is, outpatient visits (information borrowed from neighbours where necessary).
Step 6: Check if all HSA‐PSY have a localization index (LI) greater than 50%. The LI is the fraction of all outpatient visits which the patients living in an HSA‐PSY use at local psychiatric outpatient services; thus a LI > 50% reflects that patients use the majority of their psychiatric consultations in the HSA‐PSY where they live. Merge HSA‐PSY with an LI below this pre‐defined threshold with the neighbouring HSA‐PSY with the highest patient flow.
Step 7: Check if all HSA‐PSY contain at least 6 service providers to fulfil the data owner's data protection terms. Merge HSA‐PSY with less than 6 service providers with the neighbouring HSA‐PSY receiving most flow.
Step 8: Repeat steps 5–7 until no new changes are made to the HSA‐PSY allocations.
2.3. Validation of HSA‐PSY by experts
These automatically and empirically derived HSA‐PSY were reviewed by a board of local mental health services experts from various parts of Switzerland. Each of these experts (including medical directors of large psychiatric institutions and other experts in mental health services research) reviewed the validity of the HSA‐PSY in his or her part of Switzerland qualitatively based on the following criteria, which are not or only partly covered by the HSAr method:
-
‐
Functional relevance: Patient‐flows between HSA‐PSY should be minimized. While setting the LI > 0.5 in HSAr warranted that most patients undergo treatment in the HSA‐PSY where they live, experts were asked to suggest merging MedStatSyn regions if, due to their experience, the automatically delineated HSA‐PSY were not sufficiently self‐containing (cf. criterion “relevance for health services planning").
-
‐
Small‐scale areas: The HSA‐PSY should be small and homogeneous to identify differences in health utilization, which are not identifiable on a more aggregated level.
-
‐
Congruence with mobility spaces: If the allocation of MedStatSyn regions to HSA‐PSY was ambiguous, the resulting HSA‐PSY should be in accordance with the general mobility patterns of the population as represented by the Swiss Labour Market regions (Bundesamt für Statistik, 2018).
-
‐
Relevance for health services planning: If the allocation of MedStatSyn regions to HSA‐PSY was ambiguous, the HSA‐PSY should facilitate effective health care planning.
The authors then optimized the empirically derived HSA‐PSY manually in an iterative process with the expert panel based on the aforementioned criteria until all experts approved the resulting HSA‐PSY. When manually optimizing the HSY‐PSY, the data protection requirement of at least 6 service providers per HSA‐PSY had to be taken into account. While this requirement was promoted by setting the number of outpatient visits per HSA‐PSY in HSAr to be at least 10,000, in some cases the automatically derived HSA‐PSY had nevertheless to be manually merged into overarching HSA‐PSY to be in accordance with the data owner's data protection terms. Like‐wise, some suggestions of experts to further split‐up HSA‐PSY could not be realized because resulting HSA‐PSY would then have included less than 6 service providers (e.g., HSA‐PSY 25 or 68 in Figure 1).
FIGURE 1.
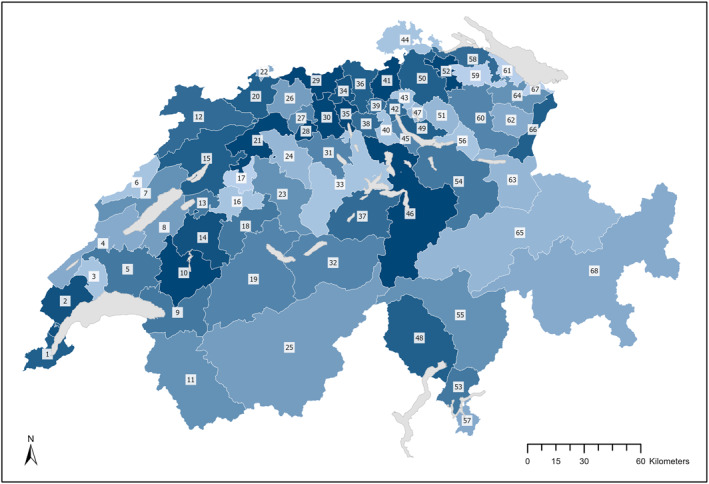
Swiss map with the 68 health service areas for psychiatric outpatient care (HSA‐PSY)
2.4. Service use in the HSA‐PSY
Finally, we calculated utilization rates of inpatient and outpatient services per 1000 population in the empirically derived HAS‐PSY for the year 2017. The population‐based rate of outpatient visits was then correlated with the rate of hospitalizations and with the rate of hospital bed days, respectively.
3. RESULTS
In total, there were 5,568,261 outpatient visits in the final dataset. These outpatients visits were provided at 3871 different service sites (there was at least one outpatient service provider in 382 out of the totally 563 MedStatSyn regions). On the aggregated level of these 563 MedStatSyn regions, there were 23,947 distinct flow patterns between patients' residences and outpatient service providers' sites. The size of these patient flows was indicated by the number of outpatient visits per flow. In MedStatSyn regions with less than 1000 outpatient visits in 2017, data were enriched with the number of outpatient visits in the years 2014–2016, resulting in the aforementioned 5,568,261 outpatient visits. This data enrichment step aimed at getting more reliable estimates of the magnitude of patient flows and hence spatial patterns.
3.1. Psychiatric health services areas in Switzerland
Figure 1 depicts the 68 HSA‐PSY for outpatient treatment in Switzerland (see also Table 1 for further details). These 68 HSA‐PSY resulted after the 61 regions, which had been automatically delineated by HSAr, were manually modified in a post‐processing step based on the inputs of the expert panel and under consideration of data protection requirements (at least 6 service providers per HSA‐PSY).
TABLE 1.
Description of the 68 health service areas for psychiatric outpatient care (HSA‐PSY) in Switzerland
| No | Name | Area (km2) | Population (2017) | Hospitalizations (2017) | Hospital bed days (2017) | Outpatient visits (2017) | |||
|---|---|---|---|---|---|---|---|---|---|
| N | Rate | N | Rate | N | Rate | ||||
| 1 | Genève | 246 | 496,229 | 3874 | 7.8 | 127,921 | 257.8 | 601,372 | 1212 |
| 2 | Nyon | 424 | 114,989 | 805 | 7.0 | 20,367 | 177.1 | 98,471 | 856 |
| 3 | Morges | 217 | 48,183 | 359 | 7.5 | 8909 | 184.9 | 38,592 | 801 |
| 4 | Yverdon | 615 | 82,726 | 721 | 8.7 | 17,591 | 212.6 | 60,315 | 729 |
| 5 | Lausanne | 692 | 386,061 | 2974 | 7.7 | 84,049 | 217.7 | 392,885 | 1018 |
| 6 | La Chaux‐de‐Fonds | 246 | 54,253 | 465 | 8.6 | 13,887 | 256.0 | 29,007 | 535 |
| 7 | Neuchâtel | 471 | 123,768 | 995 | 8.0 | 30,780 | 248.7 | 68,582 | 554 |
| 8 | Payerne | 367 | 64,576 | 399 | 6.2 | 10,418 | 161.3 | 35,639 | 552 |
| 9 | Montreux | 646 | 135,001 | 1251 | 9.3 | 28,259 | 209.3 | 131,202 | 972 |
| 10 | Bulle | 668 | 81,127 | 759 | 9.4 | 17,967 | 221.5 | 43,948 | 542 |
| 11 | Monthey—Martigny | 1483 | 131,488 | 1022 | 7.8 | 28,869 | 219.6 | 62,268 | 474 |
| 12 | Jura | 839 | 73,351 | 665 | 9.1 | 19,215 | 262.0 | 29,405 | 401 |
| 13 | Murten | 163 | 35,927 | 221 | 6.2 | 5968 | 166.1 | 13,347 | 372 |
| 14 | Fribourg | 557 | 156,372 | 1293 | 8.3 | 33,935 | 217.0 | 99,745 | 638 |
| 15 | Biel | 912 | 217,694 | 2051 | 9.4 | 67,526 | 310.2 | 136,549 | 627 |
| 16 | Bern | 281 | 272,476 | 2986 | 11.0 | 98,664 | 362.1 | 191,091 | 701 |
| 17 | Münchenbuchsee | 171 | 58,255 | 547 | 9.4 | 17,600 | 302.1 | 27,303 | 469 |
| 18 | Münsingen | 464 | 83,219 | 779 | 9.4 | 28,944 | 347.8 | 35,257 | 424 |
| 19 | Thun | 1702 | 169,907 | 1444 | 8.5 | 49,812 | 293.1 | 70,020 | 412 |
| 20 | Binningen | 374 | 227,825 | 2214 | 9.7 | 81,923 | 359.6 | 175,386 | 770 |
| 21 | Solothurn | 445 | 150,083 | 1774 | 11.8 | 50,412 | 335.9 | 67,926 | 453 |
| 22 | Basel | 37 | 193,921 | 3273 | 16.9 | 108,876 | 561.4 | 233,536 | 1204 |
| 23 | Burgdorf | 682 | 93,035 | 965 | 10.4 | 27,376 | 294.3 | 41,710 | 448 |
| 24 | Langenthal | 434 | 89,108 | 844 | 9.5 | 30,732 | 344.9 | 41,388 | 464 |
| 25 | Sion—Sierre—Brig | 3851 | 218,403 | 1520 | 7.0 | 46,339 | 212.2 | 62,613 | 287 |
| 26 | Liestal | 320 | 94,225 | 1059 | 11.2 | 38,935 | 413.2 | 69,257 | 735 |
| 27 | Olten | 122 | 66,854 | 712 | 10.7 | 23,187 | 346.8 | 32,354 | 484 |
| 28 | Zofingen | 89 | 55,797 | 492 | 8.8 | 17,807 | 319.1 | 22,791 | 408 |
| 29 | Rheinfelden | 283 | 81,638 | 643 | 7.9 | 22,967 | 281.3 | 49,549 | 607 |
| 30 | Aarau | 269 | 131,059 | 1244 | 9.5 | 46,372 | 353.8 | 73,492 | 561 |
| 31 | Sursee | 380 | 98,463 | 623 | 6.3 | 27,941 | 283.8 | 26,574 | 270 |
| 32 | Interlaken | 1229 | 47,542 | 436 | 9.2 | 16,516 | 347.4 | 23,966 | 504 |
| 33 | Luzern—Entlebuch | 1010 | 332,985 | 2727 | 8.2 | 109,587 | 329.1 | 119,224 | 358 |
| 34 | Brugg | 126 | 49,359 | 586 | 11.9 | 32,768 | 663.9 | 27,329 | 554 |
| 35 | Lenzburg | 122 | 71,437 | 572 | 8.0 | 20,456 | 286.4 | 34,982 | 490 |
| 36 | Baden | 285 | 168,401 | 1442 | 8.6 | 50,438 | 299.5 | 82,896 | 492 |
| 37 | Ob‐ und Nidwalden | 722 | 80,498 | 458 | 5.7 | 17,794 | 221.0 | 23,665 | 294 |
| 38 | Wohlen‐Bremgarten | 154 | 76,564 | 581 | 7.6 | 21,229 | 277.3 | 33,056 | 432 |
| 39 | Spreitenbach‐Schlieren | 66 | 102,564 | 897 | 8.7 | 28,161 | 274.6 | 55,689 | 543 |
| 40 | Affoltern am Albis | 135 | 65,775 | 601 | 9.1 | 22,109 | 336.1 | 37,834 | 575 |
| 41 | Bülach | 242 | 134,289 | 1039 | 7.7 | 34,589 | 257.6 | 73,511 | 547 |
| 42 | Zürich | 90 | 411,356 | 4692 | 11.4 | 156,728 | 381.0 | 373,404 | 908 |
| 43 | Wallisellen | 86 | 122,152 | 1134 | 9.3 | 37,283 | 305.2 | 67,398 | 552 |
| 44 | Schaffhausen | 342 | 95,810 | 928 | 9.7 | 34,452 | 359.6 | 53,510 | 559 |
| 45 | Thalwil | 104 | 124,118 | 1064 | 8.6 | 33,870 | 272.9 | 74,237 | 598 |
| 46 | Zug—Schwyz—Altdorf | 1708 | 225,914 | 1578 | 7.0 | 59,622 | 263.9 | 67,488 | 299 |
| 47 | Uster | 63 | 78,821 | 858 | 10.9 | 29,042 | 368.5 | 50,975 | 647 |
| 48 | Locarno | 1118 | 69,076 | 649 | 9.4 | 19,160 | 277.4 | 46,282 | 670 |
| 49 | Meilen | 170 | 159,289 | 1359 | 8.5 | 48,716 | 305.8 | 106,395 | 668 |
| 50 | Winterthur | 502 | 234,192 | 2930 | 12.5 | 96,931 | 413.9 | 175,824 | 751 |
| 51 | Wetzikon | 233 | 89,009 | 873 | 9.8 | 29,237 | 328.5 | 49,561 | 557 |
| 52 | Frauenfeld | 175 | 61,211 | 672 | 11.0 | 22,324 | 364.7 | 40,700 | 665 |
| 53 | Lugano | 291 | 146,651 | 1049 | 7.2 | 36,330 | 247.7 | 92,995 | 634 |
| 54 | Lachen—Einsiedeln—Glarus | 1127 | 133,779 | 987 | 7.4 | 34,646 | 259.9 | 32,419 | 242 |
| 55 | Bellinzona—Misox | 1699 | 90,014 | 752 | 8.4 | 26,230 | 291.4 | 55,268 | 614 |
| 56 | Rapperswil‐Jona | 199 | 63,470 | 413 | 6.5 | 14,658 | 229.3 | 26,913 | 424 |
| 57 | Mendrisio | 131 | 56,503 | 483 | 8.5 | 14,550 | 257.5 | 36,946 | 654 |
| 58 | Kreuzlingen | 252 | 65,117 | 717 | 11.0 | 22,222 | 341.3 | 43,965 | 675 |
| 59 | Weinfelden | 217 | 52,103 | 536 | 10.3 | 18,027 | 346.0 | 32,484 | 623 |
| 60 | Wil | 679 | 142,123 | 1387 | 9.7 | 49,960 | 348.6 | 73,811 | 519 |
| 61 | Münsterlingen | 112 | 65,356 | 908 | 13.9 | 29,843 | 456.6 | 44,392 | 679 |
| 62 | Herisau | 294 | 39,092 | 466 | 12.3 | 13,427 | 354.4 | 19,566 | 501 |
| 63 | Sargans | 628 | 53,988 | 399 | 7.4 | 13,809 | 255.8 | 21,567 | 399 |
| 64 | St. Gallen | 305 | 163,184 | 1713 | 10.5 | 62,869 | 385.3 | 98,273 | 602 |
| 65 | Chur—Surselva—Prättigau | 3038 | 144,916 | 1452 | 10.0 | 48,754 | 336.4 | 68,164 | 470 |
| 66 | Rheintal—Werdenberg | 275 | 92,199 | 693 | 7.5 | 26,422 | 286.6 | 47,009 | 510 |
| 67 | Rorschach | 48 | 44,824 | 530 | 11.8 | 19,380 | 432.4 | 26,686 | 595 |
| 68 | Engadin—Bergell—Puschlav—Münstertal | 3571 | 44,436 | 293 | 6.6 | 10,618 | 239.0 | 19,107 | 430 |
Note: Figures relate to the year 2017 and rates are per 1000 inhabitants.
In the densely populated Swiss midlands including most of the urban areas, the area of the HSA‐PSY tended to be smaller, particularly in the metropolitan area around Zurich, Switzerland's biggest city (HSA‐PSY 42 in Figure 1). In the sparsely populated mountainous regions around the massive Alps, the HSA‐PSY were much larger‐scaled (e.g., HSA‐PSY 11, 19, 25, 32, 65 and 68).
3.2. Outpatient service use
The rate of outpatient visits varied between 242.3 and 1211.9 per 1000 population in the 68 HSA‐PSY (Table 1 and Figure 2a). The median rate of the 68 HSA‐PSY was 552.8 visits per 1000 population (IQR = 746.1–935.5).
FIGURE 2.
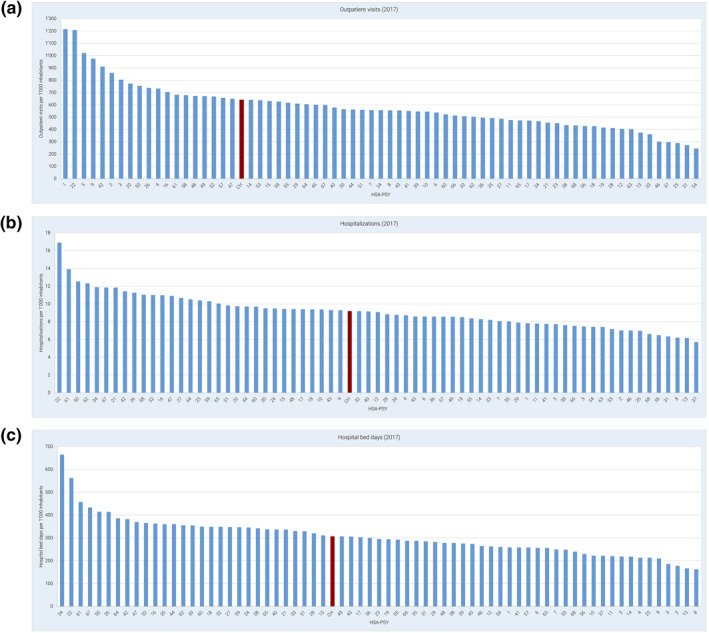
Number of (a) outpatient visits, (b) hospitalizations, and (c) hospital bed days per 1000 inhabitants and year in the 68 health service areas for psychiatric outpatient care (HSA‐PSY). CH, Switzerland
3.3. Inpatient service use
The rates of hospitalizations (Figure 2b) and hospital bed days (Figure 2c) per 1000 population again varied massively between HSA‐PSY. The median rates of the 68 HAS‐PSY were 8.9 (IQR = 10.0–12.2) for hospitalizations and 293.7 (IQR = 352.6–444.0) for hospital bed days.
3.4. Association between inpatient and outpatient service use
The population‐based utilization rate of outpatient services by the residents of an HSA‐PSY was positively associated with the rate of hospitalizations per capita in that HSY‐PSY (p < 0.001) and it tended to be positively associated with the utilization of hospital bed days per capita (p = 0.119). However, despite these overall trends, some HSA‐PSY were characterized by high outpatient and low inpatient utilization or vice versa (Figures 3a and 3b).
FIGURE 3.
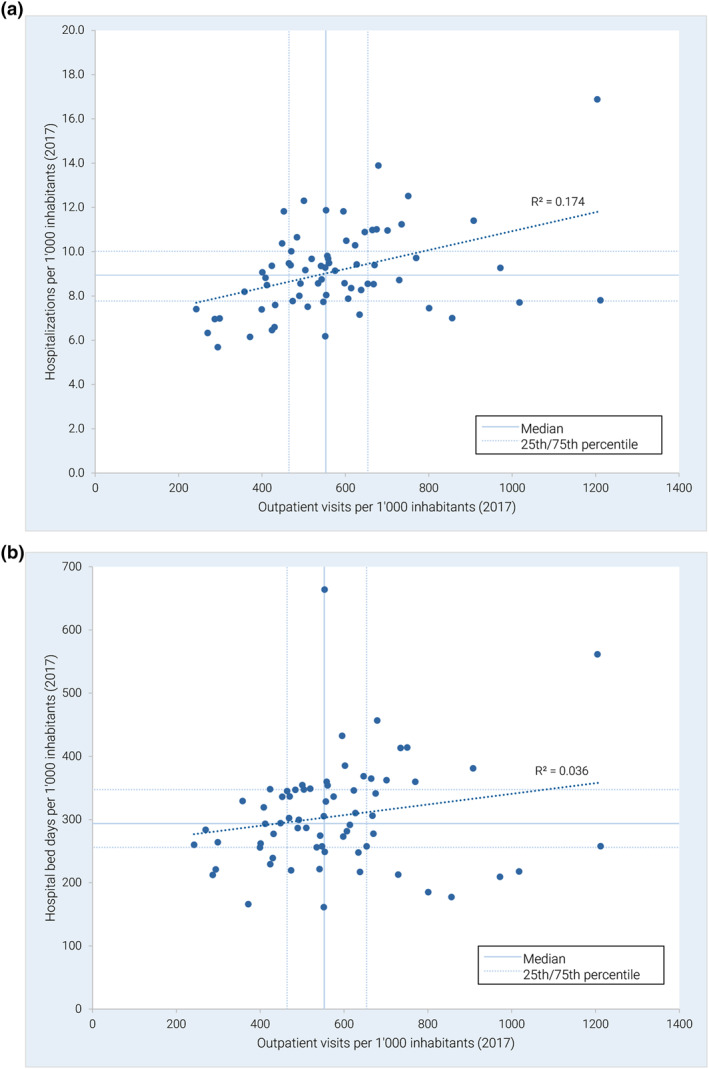
(a) Rate of hospitalizations and rate of outpatient visits per 1000 inhabitants and year in the 68 health service areas for psychiatric outpatient care (HSA‐PSY). (b) Rate of hospital bed days and rate of outpatient visits per 1000 inhabitants and year in the 68 health service areas for psychiatric outpatient care (HSA‐PSY)
4. DISCUSSION
We used SAA to delineate HSA‐PSY based on flows between patients' residences and outpatient service sites in Switzerland. The resulting 68 HSA‐PSY vary considerably regarding their size (area and population) but they represent functionally relevant spatial units for the comprehensive analysis of supply and use of inpatient and outpatient mental health services and for future service planning. So far, empirically derived and therefore functionally relevant HSA have been rarely used internationally (and never in Switzerland) to comprehensively study both inpatient and outpatient mental health services (Gottlieb et al., 2021).
Our analyses of data compiled from various sources showed a significant variation between HSA‐PSY with regard to the population‐based use of both psychiatric inpatient and outpatient services. It is unlikely that such wide variation in (inpatient and outpatient) service use is solely caused by different prevalence rates of mental disorders in the HSA‐PSY. Whether other factors such as the amount of services supply, the population structure (e.g. age and sex) or the degree of urbanization may add to the explanation of the high variation in the population‐based service use rates between the HSA‐PSY should be addressed in further studies, for which our functional mapping provides a good basis.
If one considers inpatient and outpatient mental health care to be substitutable to some degree, our findings of no or even positive associations between utilization rates of inpatient and of outpatient services appears rather counterintuitive. That is, one might expect lower use of inpatient services in HSA‐PSY with higher use of outpatient services and vice versa. Even though Switzerland has one of the highest numbers of psychiatrists and one of the highest numbers of psychiatric hospital beds per capita when compared to other OECD countries (OECD, 2014), there seems still to be a gap in mental health care—particularly those patients with the most urgent need for treatment and patients in rural areas often lack access to mental health care (Stocker et al., 2016). Such treatment gap despite relatively high resources may raise the question whether psychiatric resources are appropriately allocated to patients and regions in Switzerland. While our findings suggest that there might be an under‐supply in some regions, psychiatric services might be sufficient or even overfunded in other regions. Even though the concept of supplier‐induced effects was more critically discussed in more recent literature (Leonard et al., 2009; Mercuri & Gafni, 2011, 2018) and quantifying the objective need for mental health care supply remains difficult, our findings may foster further research and the discussion for optimal allocation of resources.
As in many high income countries, a shift from inpatient to outpatient mental health care was also proclaimed by policy makers in Switzerland (Schweizerische Gesundheitsdirektorenkonferenz, 2008). However, the dual Swiss remuneration system with a strict discrimination between outpatient and inpatient health care hinders the enforcement of outpatient and intermediate (e.g., day hospital or home treatment) services. Health insurances are currently obliged to fully refund outpatient treatments whereas inpatient treatment is partly financed by both Cantons (55%) and health insurances (45%). Obviously, health insurances are therefore sparsely motivated in the strengthening of outpatient services. In addition, the current financial incentives in Switzerland often make the provision of inpatient mental health care more attractive for psychiatric institutions from an economically point of view because the actual costs of more intensive institutional outpatient services are usually not fully covered by current tariffs (which were developed to cover costs of physicians in private practice). The qualitative and/or quantitative in‐depth study of those HSA‐PSY with a strong focus of outpatient care (while providing relatively little inpatient care) might be an interesting endeavour for future research to learn more about the drivers and outcomes of deinstitutionalization.
4.1. Limitations
Some limitations of the study warrant attention. In Switzerland, treatment for mental health issues is covered by basic health insurance if it is provided by psychiatric hospitals, outpatient clinics, psychiatrists in private practice or general practitioners. If costs for health services were payed out of pocket (e.g. due to deductibles) or by private health insurance models (e.g. treatment at psychologists in private practice), they were not recorded in the SASIS database and hence omitted in our analyses. Psychotherapy by psychologist was only reimbursed by basic health insurances if they were employed at psychiatric hospitals, outpatient clinics or at psychiatrists in private practice. However, out of pocket payments for psychological psychotherapy were estimated to account for less than 10% of the total costs in outpatient psychiatry (Kaiser et al., 2019) and treatment of more severe mental health issues might be covered by basic health insurance in the vast majority of cases. In addition, the data protection requirement of at least 6 service providers per HSA‐PSY did sometimes prohibit delineation of small‐scaled functional areas. However, this merely applied to some sparsely populated mountainous regions.
5. CONCLUSIONS
In this study, we applied a new and automated methodological approach (HSAr) to identify HSA‐PSY in Switzerland based on detailed and comprehensive psychiatric service use data from health insurance claims. From a policy making perspective, this new approach provides an analytical framework to examine the effects of financial incentives and of regional (e.g. cantonal) mental health programs on service use by enabling comprehensive analysis of inpatient and outpatient service use on a small‐scale regional level. As of midyear, psychotherapy by psychologists in private practice will also be covered by basic health insurance in Switzerland. Our HSA‐PSY provide a basis for future examination of the local effects of this new national legislation. As aforementioned, further research should examine service use in patient subgroups (e.g., diagnostic and age groups) and at identifying factors, which are associated with the substantially varying amount of mental health care use between the HSA‐PSY (such as services supply, degree of urbanization, socioeconomic indicators or the role of stigmatization).
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to the conception or design of the research or the acquisition, analysis, or interpretation of the data for the work; to drafting the work; to revising it critically with respect to important intellectual content; and to approving the version to be published.
CONFLICT OF INTEREST
All other authors received no specific grant related to this study from any funding agency, commercial or not‐for‐profit sectors.
ACKNOWLEDGEMENTS
GT is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration South London at King's College London NHS Foundation Trust, and by the NIHR Asset Global Health Unit award. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. GT is also supported by the Guy's and St Thomas' Charity for the On Trac project (EFT151101), and by the UK Medical Research Council (UKRI) in relation to the Emilia (MR/S001255/1) and Indigo Partnership (MR/R023697/1) awards.
Stulz, N. , Jörg, R. , Reim‐Gautier, C. , Bonsack, C. , Conus, P. , Evans‐Lacko, S. , Gabriel‐Felleiter, K. , Heim, E. , Jäger, M. , Knapp, M. , Richter, D. , Schneeberger, A. , Thornicroft, G. , Traber, R. , Wieser, S. , Tuch, A. , & Hepp, U. (2023). Mental health service areas in Switzerland. International Journal of Methods in Psychiatric Research, 32(1), e1937. 10.1002/mpr.1937
DATA AVAILABILITY STATEMENT
Research data are not shared.
REFERENCES
- Almog, M. , Curtis, S. , Copeland, A. , & Congdon, P. (2004). Geographical variation in acute psychiatric admissions within New York city 1990–2000: Growing inequalities in service use? Social Science & Medicine, 59(2), 361–376. 10.1016/j.socscimed.2003.10.019 [DOI] [PubMed] [Google Scholar]
- Ashton, C. M. , Petersen, N. J. , Souchek, J. , Menke, T. J. , Yu, H. J. , Pietz, K. , Eigenbrodt, M. L. , Barbour, G. , Kizer, K. W. , & Wray, N. P. (1999). Geographic variations in utilization rates in Veterans Affairs hospitals and clinics. New England Journal of Medicine, 340(1), 32–39. 10.1056/NEJM199901073400106 [DOI] [PubMed] [Google Scholar]
- Birkmeyer, J. D. , Sharp, S. M. , Finlayson, S. R. , Fisher, E. S. , & Wennberg, J. E. (1998). Variation profiles of common surgical procedures. Surgery, 124(5), 917–923. 10.1016/s0039-6060(98)70017-0 [DOI] [PubMed] [Google Scholar]
- Bundesamt für Statistik . (2018). Arbeitsmarktregionen 2018. Retrieved from https://www.bfs.admin.ch/bfs/de/home/statistiken/querschnittsthemen/raeumliche‐analysen/raeumliche‐gliederungen/analyseregionen.assetdetail.8948840.html
- Bundesamt für Statistik . (2020). Ständige Wohnbevölkerung nach Alter, Kanton, Bezirk und Gemeinde, 2010–2019. Retrieved from https://www.bfs.admin.ch/bfs/de/home/statistiken/bevoelkerung/stand‐entwicklung/bevoelkerung.assetdetail.13707291.html
- Bundesamt für Statistik . (2021a). Medizinische Statistik der Krankenhäuser (MS). Retrieved from https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/erhebungen/ms.assetdetail.7369.html
- Bundesamt für Statistik . (2021b). Medstat‐regionen. Retrieved from https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/nomenklaturen/medsreg.html
- Chassin, M. R. , Brook, R. H. , Park, R. E. , Keesey, J. , Fink, A. , Kosecoff, J. , Kahn, K. , Merrick, N. , & Solomon, D. H. (1986). Variations in the use of medical and surgical services by the Medicare population. New England Journal of Medicine, 314(5), 285–290. 10.1056/NEJM198601303140505 [DOI] [PubMed] [Google Scholar]
- Coyte, P. C. , Hawker, G. , & Wright, J. G. (1996). Variations in knee replacement utilization rates and the supply of health professionals in Ontario, Canada. Journal of Rheumatology, 23(7), 1214–1220. [PubMed] [Google Scholar]
- Curtis, S. , Congdon, P. , Almog, M. , & Ellermann, R. (2009). County variation in use of inpatient and ambulatory psychiatric care in New York state 1999–2001: Need and supply influences in a structural model. Health & Place, 15(2), 568–577. 10.1016/j.healthplace.2008.09.009 [DOI] [PubMed] [Google Scholar]
- Delamater, P. L. , Shortridge, A. M. , & Messina, J. P. (2013). Regional health care planning: A methodology to cluster facilities using community utilization patterns. BMC Health Services Research, 13(1), 333. 10.1186/1472-6963-13-333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake, R. , Skinner, J. , & Goldman, H. H. (2008). What explains the diffusion of treatments for mental illness? American Journal of Psychiatry, 165(11), 1385–1392. 10.1176/appi.ajp.2008.08030334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eveland, A. P. , Dever, G. E. , Schafer, E. , Sprinkel, C. , Davis, S. , & Rumpf, M. (1998). Analysis of health service areas: Another piece of the psychiatric workforce puzzle. Psychiatric Services, 49(7), 956–960. 10.1176/ps.49.7.956 [DOI] [PubMed] [Google Scholar]
- Federal Office of Public Health . (2021). Health insurance. Swiss Confederation. [Google Scholar]
- Fisher, E. S. , Wennberg, D. E. , Stukel, T. A. , Gottlieb, D. J. , Lucas, F. L. , & Pinder, E. L. (2003). The implications of regional variations in medicare spending. Part 2: Health outcomes and satisfaction with care. Annals of Internal Medicine, 138(4), 288–298. 10.7326/0003-4819-138-4-200302180-00007 [DOI] [PubMed] [Google Scholar]
- Franconi, L. , Ichim, D. , & D’Aló, M. (2017). Labour Market areas for territorial policies: Tools for a European approach. Statistical Journal of the IAOS, 33(3), 585–591. 10.3233/sji-160343 [DOI] [Google Scholar]
- Gittelsohn, A. , & Powe, N. R. (1995). Small area variations in health care delivery in Maryland. Health Services Research, 30(2), 295–317. [PMC free article] [PubMed] [Google Scholar]
- Goodman, D. C. , & Green, G. R. (1996). Assessment tools: Small area analysis. American Journal of Medical Quality, 11(1), S12–S14. [PubMed] [Google Scholar]
- Gottlieb, D. J. , Watts, B. V. , Peltzman, T. , Riblet, N. B. V. , Cornelius, S. , Forehand, J. A. , & Shiner, B. (2021). Small area analysis of Veterans Affairs mental health services data. Psychiatric Services. 10.1176/appi.ps.202000130 [DOI] [PubMed] [Google Scholar]
- Harrison, R. , Manias, E. , Mears, S. , Heslop, D. , Hinchcliff, R. , & Hay, L. (2019). Addressing unwarranted clinical variation: A rapid review of current evidence. Journal of Evaluation in Clinical Practice, 25(1), 53–65. 10.1111/jep.12930 [DOI] [PubMed] [Google Scholar]
- Haynes, A. G. (2020). HSAr ‐Automated HSA delineation through R. Retrieved from https://github.com/aghaynes/HSAr
- Haynes, A. G. , Wertli, M. M. , & Aujesky, D. (2020). Automated delineation of hospital service areas as a new tool for health care planning. Health Services Research, 55(3), 469–475. 10.1111/1475-6773.13275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendryx, M. S. , & Rohland, B. M. (1994). A small area analysis of psychiatric hospitalizations to general hospitals. Effects of community mental health centers. General Hospital Psychiatry, 16(5), 313–318. 10.1016/0163-8343(94)90017-5 [DOI] [PubMed] [Google Scholar]
- Hendryx, M. S. , Urdaneta, M. E. , & Borders, T. (1995). The relationship between supply and hospitalization rates for mental illness and substance use disorders. Journal of Mental Health Administration, 22(2), 167–176. 10.1007/BF02518756 [DOI] [PubMed] [Google Scholar]
- Hu, Y. , Wang, F. , & Xierali, I. M. (2018). Automated delineation of hospital service areas and hospital referral regions by modularity optimization. Health Services Research, 53(1), 236–255. 10.1111/1475-6773.12616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jia, P. (2016). Developing a flow‐based spatial algorithm to delineate hospital service areas. Applied Geography, 75, 137–143. 10.1016/j.apgeog.2016.08.008 [DOI] [Google Scholar]
- Jia, P. , Wang, F. , & Xierali, I. M. (2017). Using a huff‐based model to delineate hospital service areas. The Professional Geographer, 69(4), 522–530. 10.1080/00330124.2016.1266950 [DOI] [Google Scholar]
- Kaiser, B. , Frey, M. , & Huddleston, C. (2019). Kostenfolgen eines Wechsels vom Delegations‐zu einem Anordnungsmodell für Leistungen der psychologischen Psychotherapie für die OKP. BSS Volkswirtschaftliche Beratung. [Google Scholar]
- Keller, R. B. , Soule, D. N. , Wennberg, J. E. , & Hanley, D. F. (1990). Dealing with geographic variations in the use of hospitals. The experience of the Maine medical assessment foundation orthopaedic study group. Journal of Bone and Joint Surgery American, 72(9), 1286–1293. 10.2106/00004623-199072090-00002 [DOI] [PubMed] [Google Scholar]
- Kilaru, A. S. , Wiebe, D. J. , Karp, D. N. , Love, J. , Kallan, M. J. , & Carr, B. G. (2015). Do hospital service areas and hospital referral regions define discrete health care populations? Medical Care, 53(6), 510–516. 10.1097/MLR.0000000000000356 [DOI] [PubMed] [Google Scholar]
- Klauss, G. , Staub, L. , Widmer, M. , & Busato, A. (2005). Hospital service areas ‐‐ a new tool for health care planning in Switzerland. BMC Health Services Research, 5(1), 33. 10.1186/1472-6963-5-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knickman, J. R. , & Foltz, A. M. (1984). Regional differences in hospital utilization. How much can be traced to population differences? Medical Care, 22(11), 971–986. 10.1097/00005650-198411000-00001 [DOI] [PubMed] [Google Scholar]
- Leonard, C. , Stordeur, S. , & Roberfroid, D. (2009). Association between physician density and health care consumption: A systematic review of the evidence. Health Policy, 91(2), 121–134. 10.1016/j.healthpol.2008.11.013 [DOI] [PubMed] [Google Scholar]
- Lewis, C. E. (1969). Variations in the incidence of surgery. New England Journal of Medicine, 281(16), 880–884. 10.1056/NEJM196910162811606 [DOI] [PubMed] [Google Scholar]
- McPherson, K. , Wennberg, J. E. , Hovind, O. B. , & Clifford, P. (1982). Small‐area variations in the use of common surgical procedures: An international comparison of New England, England, and Norway. New England Journal of Medicine, 307(21), 1310–1314. 10.1056/NEJM198211183072104 [DOI] [PubMed] [Google Scholar]
- Mercuri, M. , & Gafni, A. (2011). Medical practice variations: What the literature tells us (or does not) about what are warranted and unwarranted variations. Journal of Evaluation in Clinical Practice, 17(4), 671–677. 10.1111/j.1365-2753.2011.01689.x [DOI] [PubMed] [Google Scholar]
- Mercuri, M. , & Gafni, A. (2018). Examining the role of the physician as a source of variation: Are physician‐related variations necessarily unwarranted? Journal of Evaluation in Clinical Practice, 24(1), 145–151. 10.1111/jep.12770 [DOI] [PubMed] [Google Scholar]
- OECD . (2014). Making mental health count: The social and economic costs of neglecting mental health care. OECD Publishing. [Google Scholar]
- Okumura, Y. , Sakata, N. , Tachimori, H. , & Takeshima, T. (2019). Geographical variation in psychiatric admissions among recipients of public assistance. Journal of Epidemiology, 29(7), 264–271. 10.2188/jea.JE20180066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul‐Shaheen, P. , Clark, J. D. , & Williams, D. (1987). Small area analysis: A review and analysis of the North American literature. Journal of Health Politics, Policy and Law, 12(4), 741–809. 10.1215/03616878-12-4-741 [DOI] [PubMed] [Google Scholar]
- SASIS, AG. (2021). Datenpool (DP). Retrieved from https://www.sasis.ch/
- Schuler, D. , Tuch, A. , & Peter, C. (2020). Psychische Gesundheit in der Schweiz. Monitoring 2020. (Obsan Bericht 15/2020). Schweizerisches Gesundheitsobservatorium. [Google Scholar]
- Schweizerische Gesundheitsdirektorenkonferenz . (2008). Leitfaden zur Psychiatrieplanung, Bericht der Arbeitsgruppe Spitalplanung. GDK. [Google Scholar]
- Stocker, D. , Stettler, P. , Jäggi, J. , Bischof, S. , Guggenbühl, T. , Abrassart, A. , & Künzi, K. (2016). Versorgungssituation psychisch erkrankter Personen in der Schweiz. Bundesamt für Gesundheit. [Google Scholar]
- Stulz, N. , Pichler, E. M. , Kawohl, W. , & Hepp, U. (2018). The gravitational force of mental health services: Distance decay effects in a rural Swiss service area. BMC Health Services Research, 18(1), 81. 10.1186/s12913-018-2888-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft, G. , Deb, T. , & Henderson, C. (2016). Community mental health care worldwide: Current status und further developments. World Psychiatry, 15(3), 276–286. 10.1002/wps.20349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornicroft, G. , & Tansella, M. (2009). Better mental health care. Cambridge University Press. [Google Scholar]
- Tobler, W. (1970). A computer movie simulating urban growth in the Detroit region. Economic Geography, 46(Supplement), 234–240. 10.2307/143141 [DOI] [Google Scholar]
- Wang, C. , Wang, F. , & Onega, T. (2020). Network optimization approach to delineating health care service areas: Spatially constrained Louvain and Leiden algorithms. Transactions in GIS, 25(2), 1065–1081. 10.1111/tgis.12722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts, B. V. , Shiner, B. , Klauss, G. , & Weeks, W. B. (2011). Supplier‐induced demand for psychiatric admissions in Northern new England. BMC Psychiatry, 11(1), 146. 10.1186/1471-244X-11-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wennberg, J. E. (1985). On patient need, equity, supplier‐induced demand, and the need to assess the outcome of common medical practices. Medical Care, 23(5), 512–520. 10.1097/00005650-198505000-00012 [DOI] [PubMed] [Google Scholar]
- Wennberg, J. E. (1993). Future directions for small area variations. Medical Care, 31(5 Suppl), 75–80. 10.1097/00005650-199305001-00012 [DOI] [PubMed] [Google Scholar]
- Wennberg, J. E. , Barnes, B. A. , & Zubkoff, M. (1982). Professional uncertainty and the problem of supplier‐induced demand. Social Science & Medicine, 16(7), 811–824. 10.1016/0277-9536(82)90234-9 [DOI] [PubMed] [Google Scholar]
- Wennberg, J. E. , Freeman, J. L. , & Culp, W. J. (1987). Are hospital services rationed in new haven or over‐utilised in Boston? Lancet, 1(8543), 1185–1189. 10.1016/s0140-6736(87)92152-0 [DOI] [PubMed] [Google Scholar]
- Wennberg, J. E. , & Gittelsohn, A. (1973). Small area variations in health care delivery. Science, 182(4117), 1102–1108. 10.1126/science.182.4117.1102 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.


