Abstract
Rationale:
Phleboliths are idiopathic calcifications resulting from mineralised structures inside veins, venules or blood vessels.
Patient Concerns:
A 48-year-old woman presented with multiple hard bodies on palpation.
Diagnosis:
Imaging studies revealed multiple, round, well-defined radiopaque lesions, extending from the coronoid process region down to the base of the mandible. The diagnosis was vascular malformation with multiple phleboliths.
Treatment and Outcome:
No treatment was proposed and the patient is under follow-up.
Take-Away Lessons:
Asymptomatic phleboliths of the head and neck region in an adult woman have been under surveillance.
Keywords: Case report, intramuscular haemangiomas, phlebolith, vascular malformations
INTRODUCTION
Deposition of calcium salts is a common outcome that may take place in the human body. Disordered deposition in soft tissues has been regarded as heterotopic calcification. There are three types of heterotopic calcifications: dystrophic, idiopathic and metastatic.[1] Phleboliths are idiopathic calcifications (occurring even when the levels of calcium and phosphate are normal) that arise from mineralised structures inside veins, venules or blood vessels.[1] In several cases, phleboliths are associated with vascular anomalies.[2] Amongst adults, phleboliths may represent remnants of this lesion that had taken place in the individual during his/her childhood.[2,3] Usually, phleboliths occur in the pelvic and in the head and neck region.[4,5]
The diagnosis of phleboliths is important because it allows the practitioner to identify vascular anomalies that may complicate surgical procedures in the region.[5] The diagnosis may be carried out by means of ultrasonography (USG) or other advanced imaging techniques, such as computed tomography (CT) with contrast and magnetic resonance imaging (MRI). These diagnostic tools can provide images that show the location and the extent of the lesions. Differential diagnosis of phleboliths in the head and neck includes conditions such as sialoliths, tonsilloliths, calcified lymph nodes, atherosclerotic plaques in the carotid artery, cured acne lesions, cysticercosis and miliary osteomas of the skin.[1]
In this context, the objective of this study was to report a case of a patient with phleboliths in the right masseter region. Data on this condition may be helpful to head and neck surgeons, general practitioners and oral & maxillofacial surgeons during the management of this condition.
CASE REPORT
A 48-year-old woman was referred by her general dentist to the Oral Medicine Clinic of the Federal University of Minas Gerais with a chief complaint of ‘pain and swelling on the cheek’ with more than 20 years of evolution. Her previous history was unremarkable. On examination, a slight swelling on the right side of her face without alterations on the skin and buccal mucosa was observed. On palpation, multiple hard bodies not attached to the tissues were detected [Figure 1]. Periapical and panoramic radiographic examinations revealed multiple, round, variable-size, well-defined radiopaque lesions with radiolucent edges, located from the angle of the mandible up to the coronoid process region [Figure 2]. In addition, USG was conducted and showed a lesion corresponding to a low flow vascular anomaly in the right buccal mucosa region. The final diagnosis was venous malformation with multiple phleboliths. No treatment was performed, but the patient was enlightened about the condition and has been under follow-up ever since.
Figure 1.
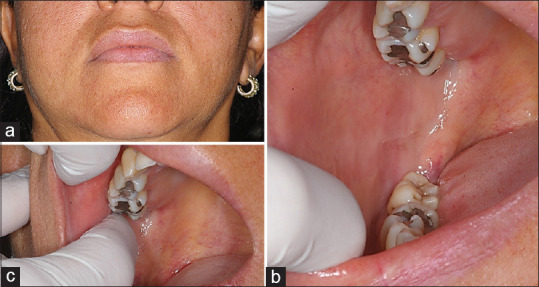
Clinical aspects (a) Extraoral examination demonstrating a slight swelling on her right side face without alterations on the skin, (b) Intraoral examination demonstrating a slight volume increase on anterior portion of right buccal mucosa with normal colour and surface, (c) On palpation, the presence of multiple hard bodies not attached to the tissues were detected (pointing out the submerged nodule)
Figure 2.
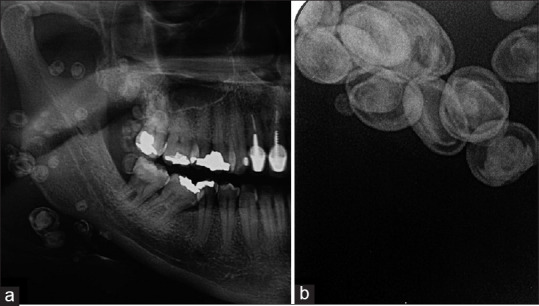
Radiographic aspects (a) Cropped panoramic radiograph demonstrates multiple, round well-defined radiopaque lesions with radiolucent edges of variable sizes along buccal region, extending from coronoid process region up to the base of the mandible, (b) Periapical radiograph of right buccal mucosa demonstrating multiple radiopaque lesions with radiolucent edges, variable sizes, rounded and oval shapes
DISCUSSION AND CONCLUSION
In this article, the case of a venous malformation with multiple phleboliths in the head and neck region of a 42-year-old woman was reported. Almost all patients complained or only noticed the lesion due to the clinical swelling of the affected area.
The most used examinations to identify phleboliths are MRI and conventional radiograph. The radiograph is the examination mostly used by health professionals in daily routine for diagnosis purposes due to easier access and low cost. Despite these advantages, conventional radiographs have limitations, such as the two-dimensional characteristic, poor information about lesions’ size and involvement with adjacent structures as well as image distortion. Thus, practitioners may request CT, which provides a three-dimensional image, but also has drawbacks, such as impaired soft-tissue analysis and exposure of the patients to a higher dose of radiation compared to conventional radiographs.[6]
Alternatively, USG and MRI may also be requested. MRI is the gold standard for soft-tissue analyses and does not use radiation, but is more expensive, time-consuming and generally requires contrast. The USG, on the other hand, can also provide soft-tissue analyses, does not use ionising radiation, is cheaper and contrast is unnecessary.[7] Advanced USG techniques, such as Doppler, also offer real-time visualisation of vessels and can be used for the diagnosis of vascular anomalies. Nevertheless, some studies comparing USG and MRI images have shown that MRI images provide better visualisation of changes.[8]
Regarding management and treatment, in general, most cases of vascular anomalies are submitted to a follow-up due to the lack of symptomatology, as for the patient whose case has been reported herein. In cases of vascular anomalies that achieve increased proportions or any concern for the patient, interventions, such as sclerotherapy or surgical excision, are usually carried out.[9] Sclerotherapy has been largely used due to its low morbidity and good results.[10] The main reason for treatment was the presence of swelling or pain. As regards phleboliths more specifically, from the moment that calcifications have already taken place, they do not disappear spontaneously or with sclerotherapy.
In the reported case, the patient had multiple phleboliths. The longer the evolution of the lesion, the higher the chance of multiple phleboliths within the lesion, since phleboliths are the outcome of a haemodynamic change in the blood vessels that calcified over time.[11]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES, Finance Code 001), Brazil. Leni Verônica Oliveira Silva is recipient of fellowship. We would like to thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, #305493/2018-3, #435644/2018-1, #404710/2018-2, #310797/2019-5).
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
Ricardo Alves Mesquita and Lucas Guimarães Abreu are research fellows of CNPq.
REFERENCES
- 1.Keberle M, Robinson S. Physiologic and pathologic calcifications and ossifications in the face and neck. Eur Radiol. 2007;17:2103–11. doi: 10.1007/s00330-006-0525-6. [DOI] [PubMed] [Google Scholar]
- 2.Eivazi B, Fasunla AJ, Güldner C, Masberg P, Werner JA, Teymoortash A. Phleboliths from venous malformations of the head and neck. Phlebology. 2013;28:86–92. doi: 10.1258/phleb.2011.011029. [DOI] [PubMed] [Google Scholar]
- 3.Park JW, Kim CH, Moon CW. Intramuscular hemangioma in buccal cheek: A case report. J Korean Assoc Oral Maxillofac Surg. 2017;43:262–6. doi: 10.5125/jkaoms.2017.43.4.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zachariades N, Rallis G, Papademetriou J, Konsolaki E, Markaki S, Mezitis M. Phleboliths. A report of three unusual cases. Br J Oral Maxillofac Surg. 1991;29:117–9. doi: 10.1016/0266-4356(91)90097-o. [DOI] [PubMed] [Google Scholar]
- 5.Banks KP, Bui-Mansfield LT, Chew FS, Collinson F. A compartmental approach to the radiographic evaluation of soft-tissue calcifications. Semin Roentgenol. 2005;40:391–407. doi: 10.1053/j.ro.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 6.Markic G, Müller L, Patcas R, Roos M, Lochbühler N, Peltomäki T, et al. Assessing the length of the mandibular ramus and the condylar process: A comparison of OPG, CBCT, CT, MRI, and lateral cephalometric measurements. Eur J Orthod. 2015;37:13–21. doi: 10.1093/ejo/cju008. [DOI] [PubMed] [Google Scholar]
- 7.Hechler BL, Phero JA, Van Mater H, Matthews NS. Ultrasound versus magnetic resonance imaging of the temporomandibular joint in juvenile idiopathic arthritis: A systematic review. Int J Oral Maxillofac Surg. 2018;47:83–9. doi: 10.1016/j.ijom.2017.07.014. [DOI] [PubMed] [Google Scholar]
- 8.Hwang M, Piskunowicz M, Darge K. Advanced Ultrasound techniques for pediatric imaging. Pediatrics. 2019;143:e20182609. doi: 10.1542/peds.2018-2609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balaji SM, Balaji P. Unusual number of phleboliths in a lip vascular malformation – A case report. Indian J Dent Res. 2022;33:110–2. doi: 10.4103/ijdr.ijdr_397_22. [DOI] [PubMed] [Google Scholar]
- 10.Rosbe KW, Hess CP, Dowd CF, Frieden IJ. Masseteric venous malformations: Diagnosis, treatment, and outcomes. Otolaryngol Head Neck Surg. 2010;143:779–83. doi: 10.1016/j.otohns.2010.08.053. [DOI] [PubMed] [Google Scholar]
- 11.Mandel L, Perrino MA. Phleboliths and the vascular maxillofacial lesion. J Oral Maxillofac Surg. 2010;68:1973–6. doi: 10.1016/j.joms.2010.04.002. [DOI] [PubMed] [Google Scholar]


