Abstract
Background
A high rate of COVID-19 vaccination is critical to reduce morbidity and mortality related to infection and to control the COVID-19 pandemic. Understanding the factors that influence vaccine confidence can inform policies and programs aimed at vaccine promotion. We examined the impact of health literacy on COVID-19 vaccine confidence among a diverse sample of adults living in two major metropolitan areas.
Methods
Questionnaire data from adults participating in an observational study conducted in Boston and Chicago from September 2018 through March 2021 were examined using path analyses to determine whether health literacy mediates the relationship between demographic variables and vaccine confidence, as measured by an adapted Vaccine Confidence Index (aVCI).
Results
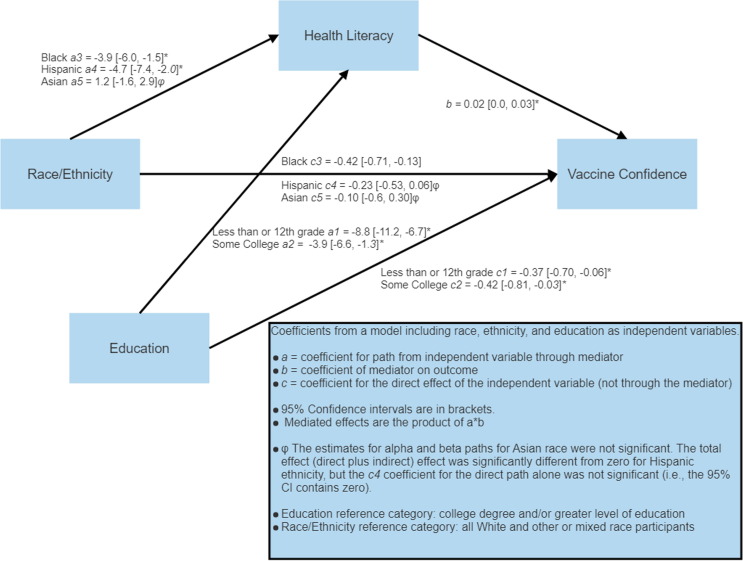
Participants (N = 273) were on average 49 years old, 63 % female, 4 % non-Hispanic Asian, 25 % Hispanic, 30 % non-Hispanic white, and 40 % non-Hispanic Black. Using non-Hispanic white and other race as the reference category, Black race and Hispanic ethnicity were associated with lower aVCI (−0.76, 95 % CI −1.00 to −0.50; −0.52, 95 % CI −0.80 to −0.27, total effects from a model excluding other covariates). Lower education was also associated with lower aVCI (using college or more as the reference, −0.73 for 12th grade or less, 95 % CI −0.93 to −0.47; −0.73 for some college/associate's/technical degree, 95 % CI −1.05 to −0.39). Health literacy partially mediated these effects for Black and Hispanic participants and those with lower education (indirect effects −0.19 and −0.19 for Black race and Hispanic ethnicity; 0.27 for 12th grade or less; −0.15 for some college/associate's/technical degree).
Conclusions
Lower levels of education, Black race, and Hispanic ethnicity were associated with lower scores on health literacy, which in turn were associated with lower vaccine confidence. Our findings suggest that efforts to improve health literacy may improve vaccine confidence, which in turn may improve vaccination rates and vaccine equity.
Clinical Trials Number: NCT03584490.
Keywords: Vaccine acceptance, SARS-CoV-2, COVID-19, Health disparities, Vaccine hesitancy, Health literacy
1. Introduction
The COVID-19 pandemic is the worst global pandemic in over 100 years. Mass vaccination campaigns are underway globally, yet lack of vaccine acceptance impedes potential benefits, including reducing COVID-19 transmission, morbidity, and mortality. Lower confidence in vaccines is associated with lower vaccine acceptance and inadequate control of infectious diseases [1], [2]. A person’s perception of the risks of natural infection for which the vaccine is designed, balanced against the potential risks of the vaccine, and the feasibility of obtaining a vaccine influences their acceptance of vaccination [3], [4]. The World Health Organization’s SAGE Working Group defines vaccine hesitancy as a delay in acceptance or refusal of a vaccine despite its availability, describing a “3 Cs” model of vaccine hesitancy, which includes confidence (beliefs around safety and efficacy of the vaccine), complacency (perception of personal risk of a bad outcome from infection), and convenience (the presence or absence of barriers to vaccination such as time, availability, and insurance) [4].
The Centers for Disease Control and Prevention (CDC) defines vaccine confidence as the degree of trust that patients, providers, and their families have in recommended vaccines [5]. Vaccine confidence encompasses a conceptual framework including 1) belief in the effectiveness and safety of the specific vaccine; 2) trust in the system delivering the vaccine, including the development of the vaccine; and 3) impressions of the motivation of policy-makers, industries, and the political system that encourages vaccination [4]. It is generally accepted that the greater an individual’s confidence is in a particular vaccine, the less likely they are to experience vaccine hesitancy, and the more likely they are to accept vaccination [6]. We use the term vaccine acceptance, a determinate of vaccine uptake, as “the degree to which individuals accept, question, or refuse vaccination,” labeling those who have chosen to pursue vaccination as “vaccine acceptors [7].”
Vaccine confidence and vaccine hesitancy are context- and vaccine-specific, existing on a continuum ranging from accepting a vaccine to delaying or declining vaccination [4], [8]. This may be particularly relevant for SARS-CoV-2, wherein vaccines were developed during a public health emergency with a sense of urgency, tremendous media attention, and involve mRNA technology that is unique among other available vaccines. Furthermore, COVID-19 vaccine protocols require multiple injections and evolving public health recommendations regarding booster shots. Certain demographic groups are more likely to have lower vaccine confidence, but proposed explanations for these differences are varied [9], [10], [11], [12]. The COVID-19 pandemic has amplified the urgency of improving our understanding of the factors that underlie vaccine confidence in order to inform the design and implementation of systems that improve vaccination rates and equity [1], [9], [10].
Public confidence in the approved COVID-19 vaccines is evolving [13], [14], [15], [16]. During the spring of 2020, 40–50% of Americans described themselves as either unsure or unlikely to get a COVID-19 vaccine, with a higher proportion of Black and Hispanic adults reporting hesitancy around vaccination [17], [18]. A Gallup poll conducted during July and August 2020 identified a decreasing proportion of vaccine-hesitant individuals (32%) but found higher rates of vaccine hesitancy among non-White respondents compared to White respondents in the United States [19]. Online surveys in the United States indicated decreasing vaccine hesitancy through January 2021 [20], but Black and Hispanic individuals were persistently less likely to accept vaccination [21], [22]. A subsequent meta-analysis described higher rates of vaccine hesitancy among Black Americans compared to other demographic groups but a likely decrease in vaccine hesitancy over time [23], [24]. Vaccine hesitancy estimates vary within low-, medium-, and high-income countries [25], [26], but socio-demographic differences in vaccine attitudes have also been documented globally [14]. Higher rates of vaccine hesitancy were noted in participants identifying as ethnic and racial minorities in the United States and United Kingdom, but decreased vaccine acceptance in these groups was only observed in the United States [27].
A growing body of literature explores possible explanations for differences in vaccine confidence and acceptance observed among different sociodemographic groups. Higher levels of concern about vaccine safety explained some of the racial/ethnic differences in pediatric vaccine uptake in the United States [28]. In another U.S. study, access challenges may have explained lower H1N1 vaccination rates for Black Americans [29]. In the United Kingdom, investigators found higher levels of vaccine mistrust among racial/ethnic minorities, but the strongest predictors of having negative vaccine views were lower socioeconomic status and educational levels [30]. The relationship between educational attainment and vaccine hesitancy is complex; some studies find greater vaccine hesitancy among groups with lower educational attainment [31], [32], but others have not [33]. National U.S. surveys conducted before the widespread availability of COVID-19 vaccines found that higher education, income, and Democratic political party affiliation predicted COVID-19 vaccination intent [18], [34]. Studies conducted in other countries have also found associations between lower education levels and COVID-19 vaccine hesitancy [35], [36], [37].
Health literacy is a multi-dimensional concept comprised of individual domains, including individual-level skills, such as information-seeking, decision-making, problem-solving, critical appraisal, and communication, and organizational domains, such as the demands that the health system places on individuals [38]. Health literacy is defined as the degree to which an individual has the ability to find, understand and use information and services to inform health decisions [39] and is a potentially modifiable factor related to health outcomes [40], [41], [42]. Health literacy may explain some of the differences in vaccine confidence observed among unique demographic groups [43], [44], [45]. However, the relationship between vaccine confidence and health literacy is uncertain and may differ for unique demographic groups [46], [47]. Veldwijk et al. found that parents with lower health literacy may have been more willing to vaccinate their children against rotavirus compared with parents with higher education and health literacy who were only willing to vaccinate when it was offered as part of the National Immunization Program [48]. Casigliani et al. found that health literacy level was not associated with vaccine confidence for various vaccinations [49].
The relationship between health literacy and COVID-19 preventative behaviors, including vaccination, is still in a period of early exploration. In Australia, McCaffery et al. found that individuals with lower health literacy demonstrated less knowledge of COVID-19 symptoms and measures to prevent transmission and were more likely to express agreement with statements that contained COVID-19 vaccine misinformation [50]. Other studies have reported similar findings where individuals with indicators of lower health literacy were less likely to accept vaccination, but these studies used varying definitions of health literacy based on knowledge tests or surveys [51], [52], [53], [54]. In comparison, Turhan et al. found that health literacy, measured with the European Health Literacy Survey Questionnaire (HLS-EU-Q), was a significant mediator of the relationship between health system distrust and COVID-19 vaccine hesitancy in Turkey [55]. More recently, Zhang et al. found that individuals with higher health literacy, also measured with the HLS-EU-Q, had lower levels of COVID-19 vaccine hesitancy, but the relationship effect between hesitancy and health literacy disappeared when individuals had high-stress levels [56].
Thus, health literacy may be a modifiable factor associated with COVID-19 vaccine confidence. We sought to explore the relationship between demographic factors, health literacy, and COVID-19 vaccine confidence in a diverse sample of urban adults using a validated measure of health literacy (Health LiTT). In accordance with the Paasche-Orlow and Wolf model [57], which views health literacy as a mediating factor on the relational pathway between demographic factors and health outcomes, we hypothesize that health literacy is a mediator of the relationship between race and ethnicity and COVID-19 vaccine confidence. This hypothesis was pre-registered on clinicaltrials.gov as part of our Statistical Analysis Plan (NCT# STU00202907). We also explored how age, gender, and education predicted vaccine confidence, also using health literacy as a mediator.
2. Methods
2.1. Setting and recruitment
We recruited participants in Boston and Chicago as part of a parent study designed to determine if health literacy influences the psychometric properties of commonly used health questionnaires using research teams with expertise in recruiting diverse urban participants and evaluating patient-reported outcomes. Potential participants were recruited through community-based outreach methods, including digital and print advertisements (e.g., flyers, postcards, email outreach, web postings, advertisements in newspapers, on transit lines, and public buildings such as libraries) in Boston and Chicago. The study was also promoted on Research Match (https://www.researchmatch.org), a secure online national recruitment tool maintained by Vanderbilt University. Research team members conducted outreach to eligible patients who had previously indicated a willingness to learn about new studies at both medical centers. Recruitment materials were available in both English and Spanish. Bilingual research staff performed eligibility screening and obtained informed consent from potential participants.
2.2. Study protocol and sample
Participants had been characterized on health literacy, demographics, and other health variables at a baseline in-person visit of the parent study [9/18/2018–2/26/2020], which was put on hold after the onset of the COVID-19 pandemic. Participants subsequently completed a phone-based protocol from November 2020 through March 2021. Eligibility criteria for enrollment in the parent study and the phone-based protocol were: age 18 years or older; ability to speak Spanish or English; and ability to consent to study procedures. Exclusion criteria included significant cognitive or neurologic impairment. Participants with hearing or visual impairments that would prevent completion of survey questionnaires were also excluded. Only participants previously enrolled in the in-person protocol could enroll in the phone-based protocol, which was initiated after in-person visits of the parent study were put on hold due to the pandemic.
After completing informed consent, study participants were interviewed at baseline, 3, and 6 months. Participants were remunerated on an increasing schedule ($40, $50, $60) for participation. This analysis presents demographic data and health literacy measures that were collected at an in-person baseline interview for 304 individuals. We administered an adapted Vaccine Confidence Index (aVCI) during the phone-based protocol to a subset of participants who could be contacted. We required completion of at least 7 of the 8 items on aVCI (i.e., 80 % or more of the items) for inclusion in statistical analyses. Two hundred and seventy-three (273/304, 90 %) participants were included in the sample. Phone visits lasted approximately 60–90 min and involved the administration of multiple questionnaires. The study protocols and procedures were approved by Northwestern and Boston University Medical Center’s Internal Review Boards.
2.3. Measures
At the baseline in-person interview, investigators collected self-reported demographic data, including age, gender, race and ethnicity, preferred language, and education level. For the purposes of the analysis, we divided race and ethnicity into four categories: White Non-Hispanic and other (including participants designating themselves as other or more than one race), Asian Non-Hispanic, Black Non-Hispanic, and Hispanic participants. We collected race and ethnicity data from participants, given the aims of the study to explore potential health disparities related to health literacy, COVID-19, and other health issues.
Health literacy was measured using Health Literacy Assessment Using Talking Touchscreen Technology (Health LiTT), a computerized assessment that does not require an interviewer. Health LiTT assesses three types of performance-based health literacy skills: prose, document, and quantitative by self-administration. The measure has been validated in English and Spanish and is scored on a T-score scale [58], [59], [60]. Higher scores indicate a higher level of health literacy. Participants also provided information about their educational attainment, which we collapsed into three categories 1) 12th grade equivalent or less, 2) some college-level education or an associate or technical degree, or 3) a college degree or greater level of educational attainment.
We used an adapted, eight-item Vaccine Confidence Index (aVCI) from Lorini et al. [47], which itself was inspired by the Global Vaccine Confidence Index, an evolving survey-based measure of confidence in immunizations developed through a systematic review of the literature and survey implementation in low and high-income countries [61], [62], [63]. Related indices have been used in global samples to measure confidence around vaccination [61], [62], [64]. An eight-item survey was used in a study assessing vaccine confidence in healthcare workers in Italy [47], containing Likert-style items related to influenza infection and vaccination. We adapted these items to be relevant to the COVID-19 virus and vaccination (e.g., “COVID-19 is a serious disease”, “COVID-19 vaccines are effective”; “COVID-19 vaccines have serious side effects”) [47]. Respondents chose their level of agreement with a particular statement with a range of responses from “totally agree” to “totally disagree” (Refer to Supplemental Materials for adapted VCI questions and scoring, based on the work of Lorini et al.). Higher scores on the aVCI reflect a higher ratio of vaccine confidence to vaccine skepticism, with a maximum score of 4.0 and a minimum score of 0.25. We selected the Lorini et al. [47] adapted VCI because of its relevance to vaccination against an infectious viral illness and its simple wording. The adapted VCI is available in English and Italian. Two Spanish-speaking research team members (PM and MM), who speak different dialectical forms of Spanish (Mexico, Chile) translated the tool into Spanish for this study. After the items were translated, they were checked by an additional native Spanish speaker (ES, Mexican American descent). In order to evaluate the psychometric properties of the aVCI, we completed a parallel analysis comparing eigenvalues from our data to eigenvalues generated from a Monte-Carlo simulation that supported a unidimensional structure (i.e., one component) [65]. We found Cronbach’s alpha of 0.73 and 0.69 for English and Spanish versions of the aVCI, respectively.
2.4. Statistical analysis
The primary hypotheses and analysis plan for this study were registered at clinicaltrials.gov prior to data analysis. Analyses were guided by the Paasche-Orlow and Wolf model (2007) of health literacy, which posits that demographic variables, including race, ethnicity, education, and age are antecedents of health literacy, and health literacy, in turn, is an antecedent of individual differences in health-related beliefs, knowledge, and decision making [57]. We used the lavaan package in R for statistical analyses [66], [67]. For each covariate of interest, we determined total, direct, and indirect effects using maximum likelihood estimation and 95% bootstrapped confidence intervals (CI) for all effects. Any estimate for which the 95% confidence interval did not contain zero was regarded as significant. Direct and indirect effects were only interpreted if the total effect was significant. First, using Health LiTT as the mediator and the adapted VCI as the dependent variable, we conducted four separate demographic analyses using the following covariates: 1) Race and ethnicity (four categories), 2) education (three categories), 3) age, and 4) gender. We used binary (0/1) variables for Black, Asian, and Hispanic ethnicity with all other participants as the reference category (White and other or mixed race participants). Seven participants endorsed both Black race and Hispanic ethnicity and were coded appropriately (i.e., a value of “1″ for both binary variables). Next, we repeated analyses combining any covariate with a significant total effect (i.e., the combined indirect and direct effect) into a single model.
3. Results
3.1. Descriptive statistics
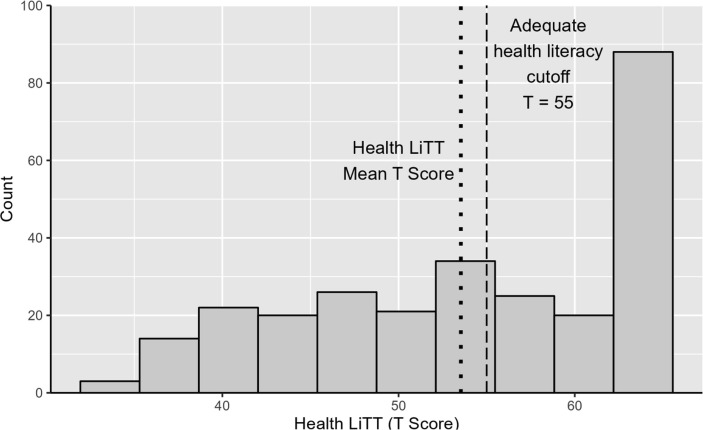
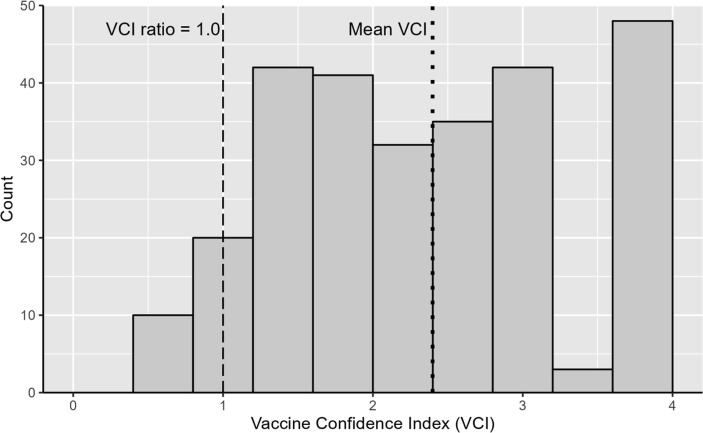
Table 1 presents demographics and descriptive statistics for the sample (N = 273). No participants identified as transgender or gender non-binary in this sample. We had a wide distribution of health literacy in our sample. Fig. 1 is a histogram of the Health LiTT scores, showing the range of scores with many participants showing high scores and a long left tail. Fig. 2 is a histogram of the distribution of the aVCI, which also had a wide range, with most participants having a ratio score above 1.0 in the direction of greater vaccine confidence.
Table 1.
Baseline Characteristics of Study Sample by Race and Ethnicity.
| Total | Hispanic | Non-Hispanic Black | Non-Hispanic White | Non-Hispanic Asian | Other or More Than One Race | |
|---|---|---|---|---|---|---|
| n | 273 | 67 | 109 | 81 | 10 | 6 |
| Age (years) | ||||||
| Mean (SD) | 49.3 (16.2) | 47.2 (15.6) | 52.5 (12.7) | 49.8 (19.5) | 30.6 (11.1) | 39.8 (14.0) |
| Gender | ||||||
| Female ( %) | 173 (63.4) | 47 (70.1) | 72 (66.1) | 46 (56.8) | 5 (50.0) | 3 (50.0) |
| Male ( %) | 100 (36.6) | 20 (29.9) | 37 (33.9) | 35 (43.2) | 5 (50.0) | 3 (50.0) |
| Language | ||||||
| English ( %) | 217 (79.5) | 11 (16.4) | 109 (100.0) | 81 (100.0) | 10 (100.0) | 6 (100.0) |
| Spanish ( %) | 56 (20.5) | 56 (83.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Education | ||||||
| ≤12th grade ( %) | 105 (38.5) | 31 (46.3) | 59 (54.1) | 13 (16.0) | 0 (0.0) | 2 (33.3) |
| Some college ( %) | 51 (18.7) | 17 (25.4) | 29 (26.6) | 4 (4.9) | 0 (0.0) | 1 (16.7) |
| College and above ( %) | 117 (42.9) | 19 (28.4) | 21 (19.3) | 64 (79.0) | 10 (100.0) | 3 (50.0) |
| Health LiTT T Score | ||||||
| Mean (SD) | 53.5 (8.6) | 50.4 (8.7) | 50.4 (7.8) | 59.3 (5.6) | 61.6 (3.2) | 53.3 (13.2) |
| aVCI | ||||||
| Mean (SD) | 2.4 (1.0) | 2.3 (0.9) | 2.1 (0.9) | 2.9 (0.9) | 2.9 (0.69) | 2.5 (1.4) |
Note: No participants identified as non-binary or transgender in this sample. Some college includes an incomplete bachelor’s degree or an associate’s degree, or technical school.
Fig. 1.
Baseline Distribution of Health Literacy (Health LiTT) in Sample Note. Histogram of health literacy as measured by Health LiTT. By definition, T scores have a mean of 50 and standard deviation of 10, relative to the reference sample. A T score of 55 is the cutoff for adequate health literacy. There is wide range of scores in this sample, although a ceiling effect is apparent at the top end of the scale.
Fig. 2.
Baseline Distribution of Scores on Adapted Vaccine Confidence Index (VCI) Note. Histogram of adapted VCI scores in our sample. Most participants have a ratio greater than 1.0, in the direction of greater vaccine confidence.
3.2. Mediation analyses in lavaan
Mediation analyses are presented in Table 2 . All values are unstandardized. One participant did not report their ethnicity and was excluded from any analysis involving this variable. Compared with White and other race (reference category), Black and Hispanic participants had lower levels of health literacy as measured by Health LiTT, which in turn was associated with lower levels of aVCI. Asian participants had higher levels of health literacy. Although the binary variable for Asian race suggested a positive effect on vaccine confidence mediated by health literacy, this was no longer significant in the model that included race, ethnicity, and education. Participants who had a 12th grade or lower education level and those with less than a college degree (some college or associates or technical degree) also had lower health literacy compared to participants with a college education or greater (the reference category) and this in turn was associated with lower levels of aVCI. Neither age nor gender had an effect on aVCI (i.e., total effects were not significant).
Table 2.
Mediation Model Estimates Including Direct, Indirect, and Total Effects.
| Model | Path | Estimate | 95 % Bootstrapped Confidence Intervals |
|---|---|---|---|
| 1. Race and ethnicity | Direct effects on aVCI | ||
| Reference category: all non-Black, non-Asian, non-Hispanic participants (White and Other or Mixed Race) | Black Race ==> aVCI | −0.6* | −0.8, −0.3 |
| Hispanic Ethnicity ==> aVCI | −0.3* | −0.6, −0.1 | |
| Asian Race ==> aVCI | −0.03 | −0.5, 0.4 | |
| Covariate ==> Health Literacy | |||
| Black Race ==> Health literacy | −7.6* | −9.5, −5.4 | |
| Hispanic Ethnicity ==> Health literacy | −7.4* | −10.0, −5.0 | |
| Asian Race ==> Health literacy | 3.1* | 0.2, 5.0 | |
| VCI regressed on Health Literacy | |||
| Health literacy ==> aVCI | 0.03* | 0.01, 0.04 | |
| Indirect effects on aVCI | |||
| Black Race ==> Health literacy ==> aVCI | −0.2* | −0.3, −0.1 | |
| Hispanic ==> Health literacy ==>aVCI | −0.2* | −0.4, −0.1 | |
| Asian Race ==> Health literacy ==> aVCI | 0.08* | 0.02, 0.2 | |
| Total effects on aVCI | |||
| Black Race - Total effect on aVCI | −0.8* | −1.0, −0.5 | |
| Hispanic Ethnicity - Total effect on aVCI | −0.5* | −0.8, −0.3 | |
| Asian Race - Total effect on aVCI | 0.05 | −0.4, 0.5 | |
| 2. Education Level | Direct effects on aVCI | ||
| Reference: College education or greater | 12th grade or less ==> aVCI | −0.5 * | −0.8, −0.2 |
| Some college ==> aVCI | −0.6 * | −0.9, −0.2 | |
| Covariate ==> Mediator (Health Literacy) | |||
| 12th grade or less ==> Health literacy | −10.9* | −12.8, −8.9 | |
| Some college ==> Health literacy | −6.3 * | −8.7, −3.9 | |
| aVCI regressed on Mediator (Health Literacy) | |||
| Health literacy ==>aVCI | 0.03* | 0.01, 0.04 | |
| Indirect effects on aVCI | |||
| 12th grade or less ==> Health literacy ==> aVCI | −0.3* | −0.5, −0.1 | |
| Some college ==> Health literacy ==>aVCI | −0.2* | −0.3, −0.1 | |
| Total effects on aVCI | |||
| 12th grade or less - Total effect on aVCI | −0.7* | −0.9, −0.5 | |
| Some college-Total effect on aVCI | −0.7* | −1.1, −0.4 | |
| 3. Gender | Direct effects on aVCI | ||
| Female = 1; Male = 0 | Female gender ==> aVCI | −0.01 | −0.2, 0.2 |
| Covariate ==> Health Literacy | |||
| Female gender ==> Health literacy | 0.3 | −1.7, 2.3 | |
| aVCI regressed on Health Literacy | |||
| Health literacy ==> aVCI | 0.04* | 0.03, 0.05 | |
| Indirect effects on aVCI | |||
| Female gender ==> Health literacy ==> aVCI | 0.01 | −0.07, 0.09 | |
| Total effects on aVCI | |||
| Female gender-Total effect on aVCI | 0 | −0.2, 0.2 | |
| 4. Age continuous in years | Direct effects on aVCI | ||
| Age ==> aVCI | 0 | −0.0, 0.01 | |
| Covariate ==> Health Literacy | |||
| Age ==> Health literacy | −0.2* | −0.3, −0.1 | |
| aVCI regressed on Health Literacy | |||
| Health literacy ==> aVCI | 0.04* | 0.03, 0.06 | |
| Indirect effects on aVCI | |||
| Age ==> Health literacy ==> aVCI | −0.01* | −0.01, −0.01 | |
| Total effects on aVCI | |||
| Age-Total effect on aVCI | −0.01 | −0.01, 0.00 |
Note. aVCI = Adapted Vaccine Confidence Index; Estimates are unstandardized and starred (*) if the 95 % confidence interval does not contain zero; Health Literacy is the mediator.
Fig. 3 shows a graphical example of the hypothesized mediation model with binary covariates for Black and Asian race and Hispanic ethnicity, educational level, health literacy as the mediator, and vaccine confidence as the outcome. The model including race, ethnicity, and education accounted for 20 % of the variance in vaccine confidence (R2 = 0.2).
Fig. 3.
Path Analysis Model from a lavaan Latent Variable Analysis Note. Model illustrating the mediation of Race and Ethnicity and Education on vaccine confidence through health literacy. All path lines are significant with p < 0.05, except for the direct and indirect effects of Asian Race and the direct effect of Hispanic ethnicity on aVCI. Estimates are standardized path coefficients. Mediated effects are the product of a and b coefficients (a*b).
4. Discussion
We found that a performance-based measure of health literacy is associated with vaccine confidence for a diverse group of adults. Our results are consistent with several studies reporting that higher health literacy is associated with more favorable attitudes toward COVID-19 preventative strategies, such as wearing masks, social distancing, and hand-washing [50], [68], [69]. We also found that demographic differences in COVID-19 vaccine confidence by race, ethnicity, and education are significantly mediated by health literacy, which suggests that improving health literacy should be one component of strategies seeking to improve vaccination rates and to potentially ameliorate disparities in vaccination rates.
It is the responsibility of the healthcare and public health systems to communicate clearly to all people about their health choices, including treatment and prevention options, and to create a welcoming environment to promote health and well-being. Confidence in evidence-based sources of information can be easily undermined. COVID-19 has spawned an infodemic [70], [71], [72] given the tremendous volume of unverified, misleading, or false information about the COVID-19 virus and vaccination [73], [74], [75]. Indeed, the torrent of information on COVID-19 is itself a major health literacy challenge. People who have experienced discrimination in healthcare settings and in interactions with the government and its proxies may be particularly inclined to mistrust clinicians or government sources. In turn, they may use alternative channels for information. Health literacy has been identified as one essential component of strategies to reduce individual or community-level susceptibility to health-related misinformation [76], [77], [78].
Thus, designing educational campaigns to promote COVID-19 vaccination should not only focus on specific vaccine details (e.g., how the vaccine works, possible side effects, the timing of the vaccination schedule) but also include information about sources of relevant and reliable information, stakeholders in the process, and involve trusted community members from a broad range of stakeholder groups [26]. More importantly, this information should be presented in plain and clear language and using a non-judgmental approach that demonstrates respect for individual autonomy. In an era of increased use of digital health services and digital health information, efforts to reduce disparities in digital access and to increase the skills necessary to use these resources are also essential [79]. Interventions that improve critical appraisal skills, one component of health literacy, should be evaluated for their effectiveness in communities of varying literacy levels. While health literacy interventions have been shown to improve health-related knowledge on various health issues, more research is needed on the impact of these interventions on low literacy populations and specifically on interventions that are interactive and/or involve digital technology [80].
Racial and ethnic minorities and individuals with lower educational attainment are more likely to have low health literacy [40], [81]. Racial and ethnic minorities are also at higher risk for morbidity, mortality, and disproportionate impacts related to COVID-19 [82], [83], [84], [85]. These disparities in COVID-19 infections and outcomes are related to demographic factors that underlie social vulnerability (poverty, systemic racism, violence), including lower education or socioeconomic status [85], [86], [87]. Identifying modifiable factors that contribute to racial disparities in the COVID-19 pandemic is essential not only to determine interventions to reduce disparities and improve health equity but also to avoid propagating harmful misconceptions about minority racial and ethnic demographic groups that increase the odds of discrimination or neglect [88]. Health literacy is one modifiable factor that can be explicitly targeted in public health promotion programs to reduce disparities. Okan and Sorensen have described health literacy as a social vaccine, a key element of non-pharmaceutical interventions (NPIs) interventions to reduce the spread of COVID-19 (hand hygiene, social distancing) because health literacy may allow individuals and communities to develop social and economic structures to improve their health and to respond to the complexities of an ongoing pandemic [70].
Empowering people to develop the skills necessary to obtain and evaluate health information is critical to efforts aimed at improving health literacy. Substantial investment in patient-focused and public health education has long been needed to improve health outcomes [89]. The data presented in the current analysis suggest that such efforts to promote health literacy would also be in the public interest as part of successful COVID-19 vaccine campaigns.
4.1. Limitations
Our methods have specific limitations. First, our sample may not be generalizable as it was restricted to urban English- or Spanish-speaking participants who consented to participation in a research study. Second, this analysis does not account for changing views on vaccination in the setting of an evolving pandemic with ongoing public health education campaigns. We are aware that disparities in vaccination rates have evolved; for example, more recent data exhibit declining disparities in vaccination rates for people of Hispanic ethnicity and Black Americans [22], [24]. Third, although we have hypothesized a causal pathway that includes race, and ethnicity with health literacy as a mediator, we were unable to evaluate alternative pathways for factors that were not measured as part of this study, such as experiences of racial or ethnic discrimination, specific health conditions, and health access factors. Fourth, our sample lacked adequate numbers of individuals with self-reported Asian, Pacific Islander, and Native American race and ethnicity, and therefore we were unable to evaluate the relationships between health literacy, vaccine confidence, and these demographic groups individually. In our mediation analysis, we included a small number of Asian participants (N = 11) and may not have detected a mediation effect due this small sample size. Fifth, we adapted an existing tool to measure vaccine confidence in our sample; however, there are other available tools with substantial application in global populations and it is theoretically possible use of an alternative tool would lead to different results than those observed here. Sixth, we completed a mediation analysis using a single measure for both health literacy (at baseline) and vaccine confidence (collected at a subsequent date). It is possible that repeated measures of these variables would have led to different results in our mediation analysis.
5. Conclusions
These analyses add to the available knowledge on vaccine confidence during the COVID-19 pandemic and can inform efforts to improve uptake of vaccination through targeted campaigns and community-based interventions, with a focus on health literacy. At the time of this writing, COVID-19 infection is highly prevalent and rising in many parts of the world, particularly in those geographic areas and communities with low vaccine uptake. In order to reduce COVID-19 transmission, morbidity and mortality, and to improve health equity, researchers and clinicians need to improve their understanding of the complex factors that influence these epidemiologic patterns. Health literacy is one important factor that may inform the response to current and future pandemics by increasing the skills necessary for people to appraise health information and to engend trust in people interacting with public health systems. Health literacy interventions are particularly essential for patients experiencing or at risk for health disparities [40]. Vaccine education and promotion programs that incorporate principles of health literacy in their design and implementation have the potential to improve vaccine equity and reduce COVID-19 morbidity and mortality.
Authors contributions
JWG and MPO initiated and designed the original study. E Hahn was involved in the design of the original study and provided expertise around the use of the Health LiTT assessment tool. ES, MT and LH helped with study setup and led the recruitment and survey administration teams in Chicago and Boston respectively. ES, CW, MM, and JT were involved in study implementation, participant recruitment, survey administration, and data management. E. Hurstak, MPO, and JWG designed the primary analysis approach for this manuscript. JWG performed the statistical analysis. E. Hurstak prepared the first and second drafts of the manuscript. PM provided expertise on data analysis, interpretation of findings, and manuscript preparation. All authors were involved in the interpretation of findings and participated in manuscript preparation and approval.
Ethical approval
The Institutional Review Boards at Northwestern Feinberg School of Medicine and Boston University School of Medicine approved this study.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: JWG declares that he and his lab have received a research grant from Pfizer to create a patient decision aid for children with atopic dermatitis (unrelated to this manuscript and unrelated to vaccines, vaccine confidence, and COVID-19); Pfizer is a maker of one common COVID-19 vaccine (Pfizer-BioNTech). He and his lab also have funding for research from the National Institutes of Health and the National Eczema Association. He has no other interests to declare. MPO is a primary investigator on multiple National Institute of Health funded research projects. Otherwise, the authors whose names are listed immediately certify that they have no other affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Acknowledgments
Acknowledgments
We would like to thank the participants in this study, as well as the extended study teams at Northwestern University and Boston University School of Medicine.
Funding
The research was funded by the National Institute of Health’s, National Institute on Minority Health and Health Disparities (NIMHD) 5R01MD010440-05.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2023.02.059.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Supplementary Data and Statistical Code
Data availability
The authors have made the data, code in R, and a detailed document describing analyses available in supplemental materials.
References
- 1.Butler R., MacDonald N.E. Diagnosing the determinants of vaccine hesitancy in specific subgroups: The Guide to Tailoring Immunization Programmes (TIP) Vaccine. 2015;33:4176–4179. doi: 10.1016/j.vaccine.2015.04.038. [DOI] [PubMed] [Google Scholar]
- 2.Doherty M., Buchy P., Standaert B., Giaquinto C., Prado-Cohrs D. Vaccine impact: benefits for human health. Vaccine. 2016;34:6707–6714. doi: 10.1016/j.vaccine.2016.10.025. [DOI] [PubMed] [Google Scholar]
- 3.Smith L.E., Amlôt R., Weinman J., Yiend J., Rubin G.J. A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017;35:6059–6069. doi: 10.1016/j.vaccine.2017.09.046. [DOI] [PubMed] [Google Scholar]
- 4.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Vaccinate with confidence: strategy to reinforce in Covid-19 vaccines. CDC; 2021. https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence.html.
- 6.Schmitzberger F.F., Scott K.W., Nham W., Mathews K., Schulson L., Fouche S., et al. Identifying strategies to boost COVID-19 vaccine acceptance in the United States. Rand Health Quarterly. 2022;9:3. [PMC free article] [PubMed] [Google Scholar]
- 7.Thomson A., Robinson K., Vallée-Tourangeau G. The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34:1018–1024. doi: 10.1016/j.vaccine.2015.11.065. [DOI] [PubMed] [Google Scholar]
- 8.Dudley M.Z., Privor-Dumm L., Dubé È., MacDonald N.E. Words matter: vaccine hesitancy, vaccine demand, vaccine confidence, herd immunity and mandatory vaccination. Vaccine. 2020;38:709–711. doi: 10.1016/j.vaccine.2019.11.056. [DOI] [PubMed] [Google Scholar]
- 9.Prins W., Butcher E., Hall L.L., Puckrein G., Rosof B. Improving adult immunization equity: where do the published research literature and existing resources lead? Vaccine. 2017;35:3020–3025. doi: 10.1016/j.vaccine.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 10.Grohskopf L.A., Liburd L.C., Redfield R.R. Addressing influenza vaccination disparities during the COVID-19 pandemic. JAMA. 2020;324:1029–1030. doi: 10.1001/jama.2020.15845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crouse Quinn S., Jamison A.M., Freimuth V.S., An J., Hancock G.R. Determinants of influenza vaccination among high-risk Black and White adults. Vaccine. 2017;35:7154–7159. doi: 10.1016/j.vaccine.2017.10.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burger A.E., Reither E.N., Mamelund S.E., Lim S. Black-white disparities in 2009 H1N1 vaccination among adults in the United States: a cautionary tale for the COVID-19 pandemic. Vaccine. 2021;39:943–951. doi: 10.1016/j.vaccine.2020.12.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fridman A., Gershon R., Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS One. 2021;16:e0250123. doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cascini F., Pantovic A., Al-Ajlouni Y., Failla G., Ricciardi W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. EClinicalMedicine. 2021;40 doi: 10.1016/j.eclinm.2021.101113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J., Lu X., Lai X., Lyu Y., Zhang H., Fenghuang Y., et al. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: a longitudinal study. Vaccines (Basel) 2021:9. doi: 10.3390/vaccines9030191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hyland P., Vallières F., Shevlin M., Bentall R.P., McKay R., Hartman T.K., et al. Resistance to COVID-19 vaccination has increased in Ireland and the United Kingdom during the pandemic. Public Health. 2021;195:54–56. doi: 10.1016/j.puhe.2021.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Neergaard L, Fingerhut H. AP-NORC poll: half of Americans would get a Covid-19 vaccine. Associated Press; 2020. May 28.
- 18.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann Intern Med. 2020;173:964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Keefe S. One in three Americans would not get the Covid-19 vaccine. Gallup: Gallup; 2020. August 7.
- 20.Carnegie Mellon University Delphi Group. COVID-19 trends and impact survey: vaccine acceptance summary. Delphi Group at Carnegie Mellon University; 2021. https://delphi.cmu.edu/covidcast/indicator/?sensor=fb-survey-smoothed_wcovid_vaccinated_appointment_or_accept.
- 21.The Delphi Group at Carnegie Mellon University in Partnership with Facebook. Topline Report on COVID-19 Vaccination in the United States Survey Waves 6-8 January 10-February 27 2021. 2021. https://www.cmu.edu/delphi-web/surveys/CMU_Topline_Vaccine_Report_20210312.pdf.
- 22.Ndugga N. Latest data on COVID-19 vaccinations by race/ethnicity. Kaiser Family Foundation; 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/.
- 23.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38:6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dhanani L.Y., Franz B. A meta-analysis of COVID-19 vaccine attitudes and demographic characteristics in the United States. Public Health. 2022;207:31–38. doi: 10.1016/j.puhe.2022.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solís Arce J.S., Warren S.S., Meriggi N.F., Scacco A., McMurry N., Voors M., et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med. 2021;27:1385–1394. doi: 10.1038/s41591-021-01454-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wouters O.J., Shadlen K.C., Salcher-Konrad M., Pollard A.J., Larson H.J., Teerawattananon Y., et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021;397:1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nguyen L.H., Joshi A.D., Drew D.A., Merino J., Ma W., Lo C.-H., et al. Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nat Commun. 2022;13:636. doi: 10.1038/s41467-022-28200-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shui I.M., Weintraub E.S., Gust D.A. Parents concerned about vaccine safety: differences in race/ethnicity and attitudes. Am J Prev Med. 2006;31:244–251. doi: 10.1016/j.amepre.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Galarce E.M., Minsky S., Viswanath K. Socioeconomic status, demographics, beliefs and A(H1N1) vaccine uptake in the United States. Vaccine. 2011;29:5284–5289. doi: 10.1016/j.vaccine.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 30.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg Health Eur. 2021;1 doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Facciolà A., Visalli G., Orlando A., Bertuccio M.P., Spataro P., Squeri R., et al. Vaccine hesitancy: an overview on parents' opinions about vaccination and possible reasons of vaccine refusal. J Public Health Res. 2019;8:1436. doi: 10.4081/jphr.2019.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wagner A.L., Shotwell A.R., Boulton M.L., Carlson B.F., Mathew J.L. Demographics of vaccine hesitancy in Chandigarh, India. Front Med (Lausanne) 2020;7 doi: 10.3389/fmed.2020.585579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wagner A.L., Masters N.B., Domek G.J., Mathew J.L., Sun X., Asturias E.J., et al. Comparisons of vaccine hesitancy across five low- and middle-income countries. Vaccines (Basel) 2019;7 doi: 10.3390/vaccines7040155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39:1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sallam M., Dababseh D., Eid H., Al-Mahzoum K., Al-Haidar A., Taim D., et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a Study in Jordan and Kuwait among Other Arab Countries. Vaccines (Basel) 2021;9 doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Mohaithef M., Padhi B.K. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. 2020;13:1657–1663. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sørensen K., Van den Broucke S., Fullam J., Doyle G., Pelikan J., Slonska Z., et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12:80. doi: 10.1186/1471-2458-12-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. What is health literacy? CDC; 2021. https://www.cdc.gov/healthliteracy/learn/index.html.
- 40.Berkman N.D., Sheridan S.L., Donahue K.E., Halpern D.J., Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 41.Tavakoly Sany S.B., Behzhad F., Ferns G., Peyman N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Serv Res. 2020;20:60. doi: 10.1186/s12913-020-4901-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muscat D.M., Shepherd H.L., Nutbeam D., Morony S., Smith S.K., Dhillon H.M., et al. Developing verbal health literacy with adult learners through training in shared decision-making. Health Lit Res Pract. 2017;1:e257–e268. doi: 10.3928/24748307-20171208-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Castro-Sánchez E., Chang P.W.S., Vila-Candel R., Escobedo A.A., Holmes A.H. Health literacy and infectious diseases: why does it matter? Int J Infect Dis. 2016;43:103–110. doi: 10.1016/j.ijid.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 44.Biasio L.R. Vaccine literacy is undervalued. Hum Vaccin Immunother. 2019;15:2552–2553. doi: 10.1080/21645515.2019.1609850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Biasio L.R. Vaccine hesitancy and health literacy. Hum Vaccin Immunother. 2017;13:701–702. doi: 10.1080/21645515.2016.1243633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lorini C., Santomauro F., Donzellini M., Capecchi L., Bechini A., Boccalini S., et al. Health literacy and vaccination: a systematic review. Hum Vaccin Immunother. 2018;14:478–488. doi: 10.1080/21645515.2017.1392423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lorini C., Collini F., Gasparini F., Paolini D., Grazzini M., Ierardi F., et al. Health literacy, vaccine confidence and influenza vaccination uptake among nursing home staff: a cross-sectional study conducted in Tuscany. Vaccines (Basel) 2020;8 doi: 10.3390/vaccines8020154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Veldwijk J., van der Heide I., Rademakers J., Schuit A.J., de Wit G.A., Uiters E., et al. Preferences for vaccination: does health literacy make a difference? Med Decis Making. 2015;35:948–958. doi: 10.1177/0272989X15597225. [DOI] [PubMed] [Google Scholar]
- 49.Casigliani V., Arzilli G., Menicagli D., Scardina G., Lopalco P.L. Vaccine hesitancy and health literacy: we need to change our paradigm. Eur J Public Health. 2020;30 [Google Scholar]
- 50.McCaffery K.J., Dodd R.H., Cvejic E., Ayrek J., Batcup C., Isautier J.M., et al. Health literacy and disparities in COVID-19-related knowledge, attitudes, beliefs and behaviours in Australia. Public Health Res Pract. 2020;30 doi: 10.17061/phrp30342012. [DOI] [PubMed] [Google Scholar]
- 51.Kricorian K., Civen R., Equils O. COVID-19 vaccine hesitancy: misinformation and perceptions of vaccine safety. Hum Vaccin Immunother. 2021:1–8. doi: 10.1080/21645515.2021.1950504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Montagni I., Ouazzani-Touhami K., Mebarki A., Texier N., Schück S., Tzourio C. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health (Oxf) 2021;3(4):695–702. doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Duong T.V., Lin C.Y., Chen S.C., Huang Y.K., Okan O., Dadaczynski K., et al. Oxford COVID-19 vaccine hesitancy in school principals: impacts of gender, well-being, and coronavirus-related health literacy. Vaccines (Basel) 2021;9 doi: 10.3390/vaccines9090985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Biasio L.R., Bonaccorsi G., Lorini C., Pecorelli S. Assessing COVID-19 vaccine literacy: a preliminary online survey. Hum Vaccin Immunother. 2021;17:1304–1312. doi: 10.1080/21645515.2020.1829315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Turhan Z., Dilcen H.Y., Dolu İ. The mediating role of health literacy on the relationship between health care system distrust and vaccine hesitancy during COVID-19 pandemic. Curr Psychol. 2021:1–10. doi: 10.1007/s12144-021-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zhang H., Li Y., Peng S., Jiang Y., Jin H., Zhang F. The effect of health literacy on COVID-19 vaccine hesitancy among community population in China: the moderating role of stress. Vaccine. 2022;40:4473–4478. doi: 10.1016/j.vaccine.2022.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Paasche-Orlow M.K., Wolf M.S. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31(Suppl. 1):S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 58.Hahn E.A., Choi S.W., Griffith J.W., Yost K.J., Baker D.W. Health literacy assessment using talking touchscreen technology (Health LiTT): a new item response theory-based measure of health literacy. J Health Commun. 2011;16:150–162. doi: 10.1080/10810730.2011.605434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yost K.J., Webster K., Baker D.W., Jacobs E.A., Anderson A., Hahn E.A. Acceptability of the talking touchscreen for health literacy assessment. J Health Commun. 2010;15(Suppl. 2):80–92. doi: 10.1080/10810730.2010.500713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yost K.J., Webster K., Baker D.W., Choi S.W., Bode R.K., Hahn E.A. Bilingual health literacy assessment using the Talking Touchscreen/la Pantalla Parlanchina: development and pilot testing. Patient Educ Couns. 2009;75:295–301. doi: 10.1016/j.pec.2009.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Larson H.J., de Figueiredo A., Xiahong Z., Schulz W.S., Verger P., Johnston I.G., et al. The state of vaccine confidence 2016: global insights through a 67-country survey. EBioMedicine. 2016;12:295–301. doi: 10.1016/j.ebiom.2016.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Larson H.J., Schulz W.S., Tucker J.D., Smith D.M. Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. 2015:7. doi: 10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.The Vaccine Confidence Project, London School of Hygiene and Tropical Medicine. The State of Vaccine Confidence. London School of Hygiene and Tropical Medicine; 2015:32.
- 64.Frew P.M., Holloway I.W., Goldbeck C., Tan D., Wu E., Jauregui J., et al. Development of a measure to assess vaccine confidence among men who have sex with men. Expert Rev Vaccines. 2018;17:1053–1061. doi: 10.1080/14760584.2018.1541405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lubbe D. Parallel analysis with categorical variables: Impact of category probability proportions on dimensionality assessment accuracy. Psychol Methods. 2019;24:339–351. doi: 10.1037/met0000171. [DOI] [PubMed] [Google Scholar]
- 66.Rosseel Y. lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48:1–36. [Google Scholar]
- 67.R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2021. R: a language and environment for statistical computing. [Google Scholar]
- 68.Silva M.J., Santos P. The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: a cross-sectional study. Int J Environ Res Public Health. 2021;18 doi: 10.3390/ijerph18105421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Riiser K., Helseth S., Haraldstad K., Torbjørnsen A., Richardsen K.R. Adolescents' health literacy, health protective measures, and health-related quality of life during the Covid-19 pandemic. PLoS One. 2020;15:e0238161. doi: 10.1371/journal.pone.0238161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Okan O., Messer M., Levin-Zamir D., Paakkari L., Sørensen K. Health literacy as a social vaccine in the COVID-19 pandemic. Health Promot Int. 2022 doi: 10.1093/heapro/daab197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dib F., Mayaud P., Chauvin P., Launay O. Online mis/disinformation and vaccine hesitancy in the era of COVID-19: Why we need an eHealth literacy revolution. Hum Vaccin Immunother. 2021:1–3. doi: 10.1080/21645515.2021.1874218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Eysenbach G. How to fight an infodemic: the four pillars of infodemic management. J Med Internet Res. 2020;22:e21820. doi: 10.2196/21820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Puri N., Coomes E.A., Haghbayan H., Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16:2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mheidly N., Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020;41:410–420. doi: 10.1057/s41271-020-00247-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Islam M.S., Sarkar T., Khan S.H., Mostofa Kamal A.H., Hasan S.M.M., Kabir A., et al. COVID-19-related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg. 2020;103:1621–1629. doi: 10.4269/ajtmh.20-0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sell T.K., Hosangadi D., Smith E., Trotochaud M., Vasudevan P., Gronvall G., et al. Johns Hopkins Center for Health Security; Baltimore, MD: 2021. National priorities to combat misinformation and disinformation for COVID-19 and future public health threats: a call for a national strategy. [Google Scholar]
- 77.Merkley E., Loewen P. Public Policy Forum; 2021. Science and health misinformation in the digital age. [Google Scholar]
- 78.Wojtowicz A. National Academies of Sciences Engineering Medicine. Addressing Health Misinformation with Health Literacy Strategies. Roundtable on Health Literacy. Washington (DC): National Academies Press (US); 2020. [PubMed]
- 79.Lyles C.R., Wachter R.M., Sarkar U. Focusing on digital health equity. JAMA. 2021;326:1795–1796. doi: 10.1001/jama.2021.18459. [DOI] [PubMed] [Google Scholar]
- 80.Meherali S., Punjani N.S., Mevawala A. Health literacy interventions to improve health outcomes in low-and middle-income countries. HLRP: Health Literacy Res Pract. 2020;4:e251–e266. doi: 10.3928/24748307-20201118-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wolf M.S., Gazmararian J.A., Baker D.W. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165:1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 82.Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C., et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alcendor D.J. Racial disparities-associated COVID-19 mortality among minority populations in the US. J Clin Med. 2020:9. doi: 10.3390/jcm9082442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garg S., Kim L., Whitaker M., O'Halloran A., Cummings C., Holstein R., et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 - COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:458–464. doi: 10.15585/mmwr.mm6915e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Perry BL, Aronson B, Pescosolido BA. Pandemic precarity: COVID-19 is exposing and exacerbating inequalities in the American heartland. Proc Natl Acad Sci 2021;118:e2020685118. [DOI] [PMC free article] [PubMed]
- 86.Hawkins R.B., Charles E.J., Mehaffey J.H. Socio-economic status and COVID-19-related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Selden T.M., Berdahl T.A. COVID-19 and racial/ethnic disparities in health risk, employment, and household composition. Health Aff (Millwood) 2020;39:1624–1632. doi: 10.1377/hlthaff.2020.00897. [DOI] [PubMed] [Google Scholar]
- 88.Chowkwanyun M., Reed A.L., Jr. Racial health disparities and Covid-19 - caution and context. N Engl J Med. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 89.Paasche-Orlow M.K., Schillinger D., Greene S.M., Wagner E.H. How health care systems can begin to address the challenge of limited literacy. J Gen Intern Med. 2006;21:884–887. doi: 10.1111/j.1525-1497.2006.00544.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Data and Statistical Code
Data Availability Statement
The authors have made the data, code in R, and a detailed document describing analyses available in supplemental materials.