INTRODUCTION
Ritonavir-boosted nirmatrelvir (Paxlovid) is an antiviral drug indicated for the treatment of coronavirus disease 2019 (COVID-19) among nonhospitalized adults and children aged ≥12 years at high risk of disease progression. In the original trial, Paxlovid reduced the risk of hospitalization or death by 88% among high-risk, unvaccinated adults.1
Paxlovid is authorized for use within 5 days of symptom onset.2 This limited window for initiating treatment makes rapid access critical. In March 2022, the Biden−Harris administration established Test-to-Treat programs that provide tests, prescriptions, and medication in 1 visit.3 Patients without access to Test-to-Treat programs are advised to contact their primary care provider (PCP) or visit a community health center. However, 1 in 4 Americans is without a PCP.4 Data through May 2022 show that antiviral prescriptions lagged in areas of high social vulnerability.5 Subsequently, additional Test-to-Treat facilities were established in high-vulnerability areas beginning in May 2022.3 The objective of this study was to map the location of and identify disparities in access to Test-to-Treat programs in the U.S.
METHODS
Location data for Test-to-Treat programs in the contiguous U.S. were obtained from HHS on July 18, 2022. The distribution of programs was examined at the ZIP-code tabulation area level. ZIP codes were defined as underserved if there was no Test-to-Treat program located within 20 miles of its boundaries. This analysis uses data on population, urbanicity, race and ethnicity, and poverty for each ZIP code (see Appendix Methods Material, available online), stratified on the basis of cut offs from the Centers for Disease Control and Prevention COVID Data Tracker.6 A 20-mile distance is a conservative definition, particularly in metropolitan areas, so sensitivity analyses included 15-mile, 10-mile, and 5-mile radii.
RESULTS
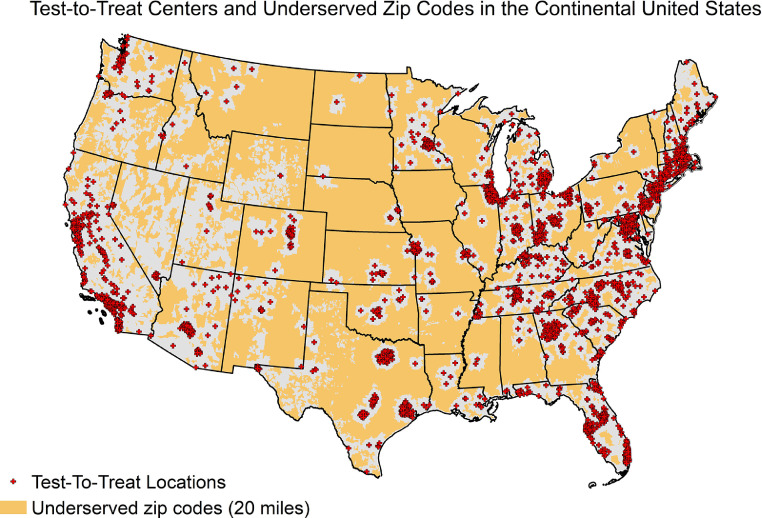
In July 2022, there were 2,642 Test-to-Treat programs in the continental U.S. There was an unequal geographic distribution of programs across the U.S. (Figure 1 ). More than 52,000,000 people in 14,812 ZIP codes—16% of the population—do not have access to a Test-to-Treat program in their ZIP code or within 20 miles.
Figure 1.
Distribution of Test-to-Treat centers and underserved ZIP codes in the continental U.S., July 18, 2022.
Most ZIP codes representing metropolitan areas have a Test-to-Treat program within 20 miles (77%), and 49% have a program within 5 miles (Table 1 and Appendix Table 1, available online). In contrast, only 30% of small towns and 23% of rural areas have nearby access. Most ZIP codes with a high proportion of Hispanic and Black residents have access to nearby Test-to-Treat programs (72%, 65%). ZIP codes with a high proportion of American Indian/Alaska Native residents were likely to be underserved (70%). About half of high-poverty ZIP codes do not have access to a Test-to-Treat program within 20 miles, compared with 41% of low-poverty ZIP codes. Trends were similar when the analysis used smaller radii (15, 10, or 5 miles), although disparities increased for some subpopulations as radius size decreased (Appendix Table 1, available online, and Appendix Figure 1, available online).
Table 1.
Characteristics of Underserved ZIP Codes (Compared With Those of Served Codes) in the Continental U.S.
| Characteristics | Underserved ZIP codes(No Test-to-Treat program within 20 miles of ZIP code) (n=14,812) | Served ZIP codes(Test-to-Treat program[s] within 20 miles of ZIP code) (n=18,488) |
|---|---|---|
| Urbanicitya | ||
| Metropolitan (urban centers with 50,000+ population and surrounding ZIP codes) | 4,083 (22.89) | 13,751 (77.1) |
| Micropolitan (urban clusters with a 10,000–49,999 population and surrounding ZIP codes) | 3,046 (63.6) | 1,741 (36.4) |
| Small town (urban clusters with a 2,500–9,999 population and surrounding ZIP codes) | 2,492 (69.8) | 1,076 (30.2) |
| Rural (clusters <2,500 population and primary flow of commuting is local) | 4,798 (76.6) | 1,469 (23.4) |
| Race/ethnicityb,c | ||
| Percentage Black | ||
| High (>37%) | 710 (35.1) | 1,310 (64.9) |
| Medium (>2.5% to 37%) | 2,690 (26.4) | 7,509 (73.6) |
| Low (≤2.5%) | 10,900 (54.7) | 9,041 (45.3) |
| Percentage Hispanic | ||
| High (>45.5%) | 449 (28.1) | 1,149 (71.9) |
| Medium (>18.3% to 45.5%) | 896 (27.6) | 2,349 (72.4) |
| Low (≤18.3%) | 12,955 (47.4) | 14,362 (52.6) |
| Percentage American Indian/Alaska Native | ||
| High (>30.1%) | 255 (70.4) | 107 (29.6) |
| Medium (>0.7% to 30.1%) | 9,020 (61.2) | 5,725 (38.8) |
| Low (≤0.7%) | 4,966 (29.3) | 12,003 (70.7) |
| Povertyb,c | ||
| High (>17.3%) | 3,974 (49.4) | 4,069 (50.6) |
| Medium (>12.3% to 17.3%) | 2,730 (49.3) | 2,806 (50.7) |
| Low (≤12.3%) | 7,521 (40.9) | 10,872 (59.1) |
Note: All values are n (%).
Urbanicity status was drawn from the USDA data set on rural−urban commuting area codes; in this data set, ZIP codes are considered metropolitan if located within an urban center of >50,000 people, along with the surrounding ZIP codes where the primary commuting flow of the ZIP code is into the urban center. Micropolitan ZIP codes are located within urban clusters with a population of 10,000 to 50,000 people and/or if the primary commuting flow of the ZIP code is into such a micropolitan area. Small-town ZIP codes are located within urban clusters with a population of 2,500 to 9,000, including surrounding ZIP codes with primary commuting flow into the urban cluster. Rural ZIP codes are those with a local primary commuting flow (i.e., little commuting to urban areas or urban clusters). Urbanicity status was unavailable for 844 ZIP codes in the continental U.S. (including 451 served ZIP codes and 393 underserved ZIP codes).
Information on race/ethnicity and poverty status was drawn from the American Community Survey (2020 5-year estimates). Poverty status information was unavailable for 1,328 ZIP codes in the continental U.S. (including 741 served and 587 underserved ZIP codes). Information on the percentage of Black and Hispanic residents was unavailable for 1,140 ZIP codes (including 628 served and 512 underserved ZIP codes). Information on the percentage of American Indian/Alaska Native residents was unavailable for 1,224 ZIP codes (including 653 served and 571 underserved ZIP codes).
Thresholds for the percentage of racial/ethnic subgroups and percent of the population in poverty are drawn from CDC's COVID Data Tracker, which creates thresholds on the basis of terciles of population characteristics by county.
CDC, Centers for Disease Control and Prevention; USDA, U.S. Department of Agriculture.
DISCUSSION
The Test-to-Treat program was designed to reduce barriers to accessing treatment, and the Centers for Disease Control and Prevention found that nearly half of the sites were located in high-social-vulnerability ZIP codes by May 2022.5 However, this new analysis shows that some populations remain without access. Most ZIP codes with the highest proportion of American Indian/Alaska Native residents and almost half of those with a high-poverty rate remain underserved as of July 2022. People in rural locations had lower access to Test-to-Treat programs (23% of ZIP codes) than those in metropolitan areas (77%). This parallels trends in the cumulative COVID-19 death rate, which is increasingly higher among people living in rural and micropolitan areas.6
Limitations
These findings have several limitations. First, the analysis does not address whether underserved populations successfully access Paxlovid through PCPs and community pharmacies. Second, geographic access is only one aspect of ensuring treatment access; previous work found that Paxlovid was underprescribed in high-social-vulnerability ZIP codes despite hosting a high proportion of Test-to-Treat programs.5
In an effort to reduce barriers to antivirals, the U.S. Food and Drug Administration authorized state-licensed pharmacists to directly prescribe Paxlovid on July 6, 2022.7 Although this is intended to expand treatment access, community pharmacies not participating in the Test-to-Treat program may not offer this service to patients, and little data exist on the implementation and impact of this policy. Furthermore, recent publications suggest multifaceted barriers to the uptake of antivirals and that expanded access must be coupled with increased outreach to patients and providers.5 , 8 Finally, pharmacy deserts persist in the U.S., and many communities will continue to have limited access to antivirals even if pharmacy-based programs expand.9 , 10
CONCLUSIONS
Achieving pharmacoequity is an important goal, especially in the context of an ongoing pandemic with major disparities in health outcomes. Policy efforts and transparent data are key to addressing these disparities.
Acknowledgments
ACKNOWLEDGMENTS
This manuscript was originally published as a preprint in the COVID-19 SARS-CoV-2 preprints collection from medRxiv and bioRxiv (https://doi.org/10.1101/2022.08.02.22278349).
No financial disclosures were reported by the authors of this paper.
CRediT AUTHOR STATEMENT
Emily R. Smith: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. Erin M. Oakley: Data curation, Formal analysis, Methodology, Visualization, Writing – original draft.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2023.01.022.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Hammond J, Leister-Tebbe H, Gardner A, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with COVID-19. N Engl J Med. 2022;386(15):1397–1408. doi: 10.1056/NEJMoa2118542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ritonavir-boosted nirmatrelvir (Paxlovid). NIH.https://www.covid19treatmentguidelines.nih.gov/therapies/antiviral-therapy/ritonavir-boosted-nirmatrelvir–paxlovid-/. Updated December 1, 2022. Accessed July 22, 2022.
- 3.Office of the Assistant Secretary for Preparedness & Response, HHS. Fact sheet: federally-supported test to treat sites. Washington, DC: Office of the Assistant Secretary for Preparedness & Response, HHS.https://aspr.hhs.gov/TestToTreat/Documents/ASPR-Fact-Sheet-Federally-Supported-Test-to-Treat-Sites.pdf. Published May 2022. Accessed July 22, 2022.
- 4.Levine DM, Linder JA, Landon BE. Characteristics of Americans with primary care and changes over time, 2002–2015. JAMA Intern Med. 2020;180(3):463–466. doi: 10.1001/jamainternmed.2019.6282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gold JAW, Kelleher J, Magid J, et al. Dispensing of oral antiviral drugs for treatment of COVID-19 by ZIP code-level social vulnerability - United States, December 23, 2021–May 21, 2022. MMWR Morb Mortal Wkly Rep. 2022;71(25):825–829. doi: 10.15585/mmwr.mm7125e1. [DOI] [PubMed] [Google Scholar]
- 6.COVID Data Tracker. Centers for Disease Control and Prevention.https://covid.cdc.gov/covid-data-tracker/#pop-factors_7daynewdeaths. Accessed July 22, 2022.
- 7.Tanne JH. COVID-19: FDA authorises pharmacists to prescribe Paxlovid. BMJ. 2022;378:o1695. doi: 10.1136/bmj.o1695. [DOI] [PubMed] [Google Scholar]
- 8.Leonhardt D. The power of Paxlovid. The New York Times. October 7, 2022. https://www.nytimes.com/2022/10/07/briefing/covid-treatment-paxlovid.html. Accessed October 10, 2022.
- 9.Ying X, Kahn P, Mathis WS. Pharmacy deserts: more than where pharmacies are. J Am Pharm Assoc (2003) 2022;62(6):1875–1879. doi: 10.1016/j.japh.2022.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Wittenauer R, Shah PD, Bacci JL, Stergachis A. Pharmacy deserts and COVID-19 risk at the census tract level in the State of Washington. Vaccine X. 2022;12 doi: 10.1016/j.jvacx.2022.100227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.