Abstract
Study Design
A retrospective study at a single academic institution.
Purpose
We aimed to understand the pathogenesis of cervical spondylolisthesis by analyzing whether narrowing of the disc height stabilizes the slipped disc level according to the degenerative cascade.
Overview of Literature
According to Kirkaldy-Willis’ degenerative cascade, the narrowing of the disc height at slipped level contributes to intervertebral stability in lumbar spondylolisthesis. Conversely, the pathogenesis of cervical spondylolisthesis is unknown due to a scarcity of reports on the condition.
Methods
The images of 83 patients with cervical single-level spondylolisthesis were studied. We looked at 52 slipped levels for anterior slippage and 31 for posterior slippage. The imaging parameters included slippage in the neutral, flexed, and extended positions, axial facet joint orientation, sagittal facet slope, global cervical alignment, C2–C7 angle, C2–C7 sagittal vertical axis, range of motion (ROM), and slipped disc angle ROM.
Results
With the narrowing of the intervertebral disc height, slippage in the flexed position of both anterior and posterior spondylolisthesis increased. However, in both anterior and posterior spondylolisthesis, disc height narrowing did not show stability. The narrowing of the intervertebral disc height was found to be a risk factor for a translation of slippage of 1.8 mm or more in flexion-extension motion in anterior spondylolisthesis in multivariate regression analysis.
Conclusions
Narrowing the intervertebral disc height did not stabilize the translation of slippage in flexion-extension motion in cervical spondylolisthesis. Instead, narrowing of the disc height was associated with a translation of slippage of 1.8 mm or more in flexion-extension motion in cases of anterior slippage. Therefore, we discovered that degenerative cascade stabilization for cervical spondylolisthesis was difficult to achieve.
Keywords: Spondylolisthesis, Degenerative cascade, Disc narrowing, Cervical, Instability
Introduction
Lumbar spondylolisthesis has been studied in many cases, and various studies have been conducted [1–3]. The degenerative cascade proposed by Kirkaldy-Willis in the lumbar spine is well known [4,5]. In the lumbar spine, degeneration of the intervertebral discs causes dysfunction, which is followed by instability caused by degeneration of the intervertebral joints. Furthermore, this is followed by a period of lumbar spine restabilization due to the appearance of osteophytes and disc height narrowing [4,5]. This is thought to be the case with lumbar spondylolisthesis as well. After degeneration progressed, osteophytes around the disc and intervertebral joints are thought to stabilize the slipped vertebrae. A disc height narrowing stabilizes the slipped vertebrae [1–3].
Cervical spondylolisthesis has not been well studied due to the limited number of cases and the relatively small number of studies conducted [6–12]. There was a time when cervical spondylolisthesis was considered a rare condition [8], and several recent reports reported that it is relatively common in the elderly [6,9]. In a single-center study, we looked at the imaging characteristics of a large number of cases of cervical spondylolisthesis. We discovered that anterior slippage was more common in the intervertebral spaces when disc height was still present. In contrast, posterior slippage tended to occur in the intervertebral spaces with markedly reduced disc height [6]. Although studies of cervical spine slippage have also examined its relationship to surgical outcomes [7,11], its pathogenesis is still not well understood. To date, no report exists that considers cervical spondylolisthesis to be stabilized by narrowing the disc height, similar to lumbar spondylolisthesis.
We hypothesized that similar to the lumbar spine, if a degenerative cascade exists in the cervical spine, more options may exist for decompression in cervical spondylolisthesis with narrowing of the intervertebral space. To test this theory, we looked at the images of a large number of patients with cervical spondylolisthesis.
Materials and Methods
1. Design
We conducted a retrospective study at a single academic institution.
2. Ethical approval
We conducted this research in accordance with the principles of the Helsinki Declaration. The Institutional Review Board of Tokyo Dental College Ichikawa General Hospital reviewed and approved the study’s protocol (IRB no., 254). All patients signed a written informed consent form.
3. Subjects
Between 2008 and 2013, 731 patients underwent surgeries for cervical spinal disorders at the Tokyo Dental College Ichikawa General Hospital. Preoperatively, all patients received standard radiographic examinations of the cervical spine, which included lateral imaging in flexion and extension. Additionally, each patient received a plain computed tomography (CT) or myelogram-CT. We defined cervical spondylolisthesis as anteroposterior vertebral slipping of more than 2 mm, identified on lateral standing X-ray images in a neutral position or on sagittal CT images, according to the criteria described in previous papers [10,12]. Spondylolisthesis was recognized in 101 cases at 124 levels. In 68 and 40 cases, respectively, anterior and posterior spondylolisthesis was found. Cases with more than two intervertebral slippages were thought to present with unique pathology. Therefore, in this study, only single intervertebral slippage cases were examined. The analysis of this study was performed on 52 patients with anterior single-level spondylolisthesis and 31 patients with posterior single-level spondylolisthesis.
4. Analysis of radiological findings
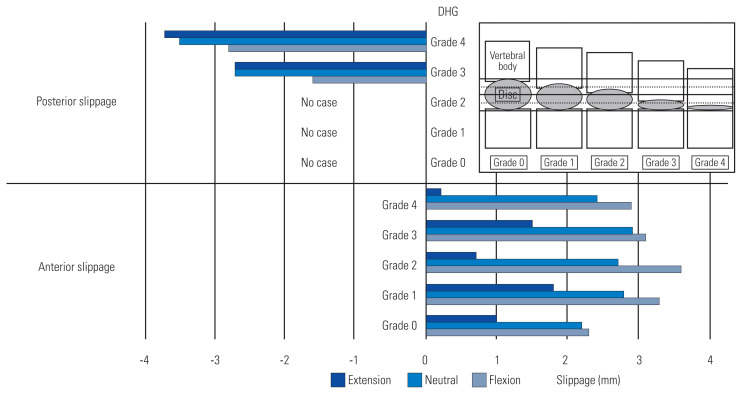
Two spinal surgeons independently performed the radiological evaluation using a DICOM viewer (Synapse version 4.1.0; FUJIFILM Medical, Tokyo, Japan). We evaluated the intervertebral disc height according to the revised Matsumoto method [6,13]. We defined disc height grade (DHG) as the percentage of height reduction compared with the most adjacent normal disc on sagittal CT images, graded from 0 to 4: grade 0, no narrowing of the disc space; grade 1, less than 25% loss of height; grade 2, 25%–50% loss of height; grade 3, 50%–75% loss of height; and grade 4, more than 75% loss of height (Fig. 1).
Fig. 1.
Slippage in the neutral, flexed, and extended positions examined in five groups by disc height grade (DHG). DHG: grade 0, no narrowing of the disc space; grade 1, less than 25% loss of height; grade 2, 25%–50% loss of height; grade 3, 50%–75% loss of height; and grade 4, more than 75% loss of height.
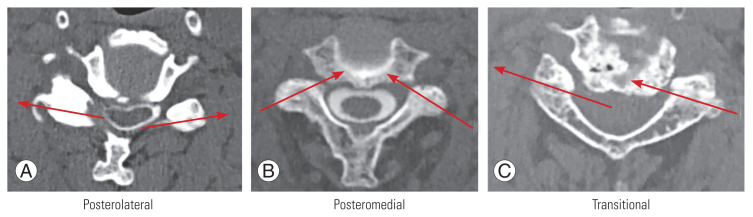
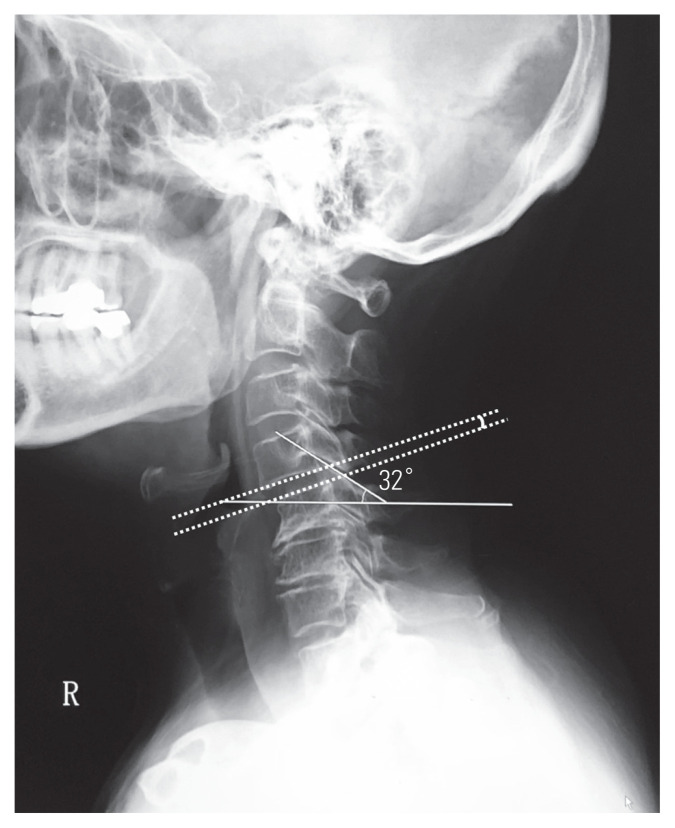
The slippage was measured in the flexed and extended positions, as well as in the neutral position, using simple radiographic lateral views. Anterior slippage was considered positive in this study. For example, an anterior slippage of 2 mm exhibits a slip distance of +2 mm, and a posterior slippage of 2 mm exhibits a slip distance of −2 mm. The facet joint type was determined using Pal’s method, which used axial CT slices to determine the orientation of the superior articular process at a slipped level [6,12] (Fig. 2). Sagittal facet slope was measured as the angle between the line of the facet joint and a horizontal line using simple X-ray lateral images (Fig. 3). According to Takeshima’s method, alignment type was decided by simple X-ray lateral images [14]: group A, lordosis; group B, straight; group C, kyphosis; group D, sigmoid with cranial lordosis; and group E, sigmoid with cranial kyphosis. Sagittal alignment of the cervical spine was measured at C2–C7, using the Cobb method, on lateral radiographs of patients who stood in a neutral position. The C2–C7 sagittal vertical axis (SVA) was measured, with positive sagittal alignment defined as an anterior deviation of the C2 plumb line (extending from the centroid of the C2 vertebra) from the superior posterior corner of the C7 vertebral body. Neck range of motion (ROM) was assessed based on the differences in C2–C7 angles from flexion to extension. Slipped disc angle was defined as a Cobb angle at the slipped intervertebral space (Fig. 3). Slipped disc ROM was assessed based on the differences in slipped disc angles from flexion to extension.
Fig. 2.
(A–C) Type of facet joint in axial section of computed tomography (CT). Using CT axial images, the facet joints are classified into three categories based on the direction of the superior articular process (arrows). The orientation is divided into posterior lateral orientation (A), posterior medial orientation (B), and transitional (C) where the orientation changes from side to side.
Fig. 3.
Sagittal facet slope and slipped disc angle. We measured the facet slope, which combines both the disc slope and facet angle of the slipped vertebrae. The facet slope was defined as the angle between the line drawn on the facet joint and the horizontal line in the lateral view of a simple X-ray (solid line). Slipped disc angle was defined as Cobb angle at slipped intervertebral space (dotted line).
5. Statistical analysis
Statistical analysis was performed using software (IBM SPSS ver. 25.0; IBM Corp., Armonk, NY, USA). All values are expressed as the mean±standard deviation and were considered significant when p<0.05. Comparing each independent variable among the five groups was performed using one-way analysis of variance (ANOVA) for continuous variables and Kruskal-Wallis test for discrete variables. Tukey’s post-hoc test was used to examine statistical differences after these analyses. The risk factor analysis was carried out using logistic regression analysis. First, a univariate analysis was used to determine the significance of various parameters. Factors with p<0.05 in the univariate analysis for anterior slippage and factors with p<0.15 in the univariate analysis for posterior slippage were then included in the multivariate analysis. The t-test for continuous variables and the Mann-Whitney U test for discrete variables were used to compare each independent variable between the two groups. A receiver operating characteristic (ROC) curve analysis was performed to investigate a cutoff value for the translation of slippage more than 1.8 mm in the flexion-extension motion of anterior slippage using parameters detected as a risk factor in regression analysis. Youden index was used to determine the cutoff value of each parameter and to determine its sensitivity and specificity.
Results
1. Demographics of patients
Anterior slippage was observed in 52 levels. When divided by DHG, DHG 1 was narrowed by 25% or less in 25 levels, the largest number of DHG, accounting for about half of the cases. From DHG 0 to 4, the remaining disc heights were nearly evenly distributed. The five groups were divided by DHG, and no significant differences were found in age, sex ratios, disease type, or level of slippage.
Posterior slippage was found in 31 levels. When divided by DHG, there were no cases of DHG 0 to DHG 2, only DHG 3 and 4 with more than 50% narrowing, and most of them were classified as DHG 4 with the largest narrowing. The two groups divided by DHG presented with no significant differences in age, sex ratios, disease type, or level of slippage (Table 1).
Table 1.
Demographics of patients and radiological findings among the five groups divided by the DHG
| Characteristic | DHG 0 | DHG 1 | DHG 2 | DHG 3 | DHG 4 | p-value |
|---|---|---|---|---|---|---|
| Anterior slippage | ||||||
| No. of disc level | 6 | 25 | 11 | 6 | 4 | |
| Age (yr) | 71.7±4.1 | 71.6±9.8 | 76.9±7.4 | 71.2±9.2 | 68.5±10.9 | 0.509 |
| Sex | ||||||
| Male | 2 | 20 | 7 | 2 | 2 | 0.093 |
| Female | 4 | 5 | 4 | 4 | 2 | |
| Disesase | 0.426 | |||||
| CSM | 4 | 24 | 9 | 5 | 3 | |
| OPLL | 2 | 1 | 1 | 0 | 1 | |
| Others | 0 | 0 | 1 | 1 | 0 | |
| Slipped levela) | 4.2±1.6 | 5.0±1.9 | 4.2±1.5 | 4.2±1.2 | 4.5±1.7 | 0.597 |
| Slippage in Flex (mm) | 2.3±0.3 | 3.3±0.6 | 3.6±0.7 | 3.1±0.9 | 2.9±0.9 | 0.023 |
| Slippage in neutral (mm) | 2.2±0.4 | 2.8±0.6 | 2.7±0.5 | 2.9±1.0 | 2.4±0.6 | 0.515 |
| Slippage in Ext (mm) | 1.0±0.8 | 1.8±1.0 | 0.7±0.8 | 1.5±1.4 | 0.2±0.3 | 0.046 |
| Translation of slippage (mm) | 1.2±0.8 | 1.4±0.7 | 2.8±1.1 | 1.6±1.5 | 2.8±0.7 | 0.007 |
| Type of facet joint | 0.170 | |||||
| Posteromedial | 4 | 8 | 6 | 4 | 1 | |
| Transitional | 1 | 7 | 3 | 1 | 0 | |
| Posterolateral | 1 | 10 | 2 | 1 | 3 | |
| Saggital facet slope (°) | 31.3±6.8 | 19.8±11.1 | 21.8±10.2 | 20.5±10.3 | 25.3±22.1 | 0.275 |
| Alignment type | 0.697 | |||||
| A: lordosis | 1 | 7 | 3 | 1 | 1 | |
| B: straight | 1 | 8 | 3 | 2 | 1 | |
| C: kyphosis | 0 | 3 | 2 | 0 | 0 | |
| D: sigmoid cranial lordosis | 2 | 3 | 0 | 1 | 1 | |
| E: sigmoid cranial kyphosis | 2 | 4 | 3 | 2 | 1 | |
| C2–C7 angle (°) | 7.0±8.5 | 5.6±15.7 | 6.9±10.4 | 12.8±11.0 | 9.5±8.1 | 0.123 |
| C2–C7 SVA (mm) | 20.7±10.5 | 36.1±17.9 | 27.5±13.7 | 29.2±15.3 | 17.5±25.4 | 0.123 |
| Flex C2–C7 angle (°) | −14.8±9.9 | −13.9±16.6 | −13.4±10.4 | −2.2±11.4 | −12.0±6.7 | 0.439 |
| Ext C2–C7 angle (°) | 24.7±9.0 | 19.5±12.2 | 17.6±12.0 | 30.8±8.7 | 18.0±12.1 | 0.175 |
| ROM (°) | 39.5±10.5 | 33.4±14.2 | 30.9±12.0 | 33.0±11.7 | 30.0±11.9 | 0.736 |
| Slipped disc angle (°) | 0.7±5.4 | 0.3±5.8 | 0.1±2.9 | −0.5±4.4 | −0.3±2.5 | 0.994 |
| Slipped disc ROM (°) | 8.3±7.5 | 7.8±5.3 | 9.1±3.8 | 8.0±7.0 | 8.0±2.6 | 0.983 |
| Posterior slippage | ||||||
| No. of disc level | 0 | 0 | 0 | 8 | 23 | |
| Age (yr) | 66.0±11.4 | 66.4±9.2 | 0.915 | |||
| Sex | 0.445 | |||||
| Male | 7 | 17 | ||||
| Female | 1 | 6 | ||||
| Disesase | 0.173 | |||||
| CSM | 8 | 18 | ||||
| OPLL | 0 | 1 | ||||
| Others | 0 | 4 | ||||
| Slipped levela) | 4.4±1.2 | 4.3±1.0 | 0.872 | |||
| Slippage in Flex (mm) | −1.6±1.0 | −2.8±1.2 | 0.022 | |||
| Slippage in neutral (mm) | −2.7±0.7 | −3.5±1.2 | 0.068 | |||
| Slippage in Ext (mm) | −2.7±0.7 | −3.7±1.2 | 0.050 | |||
| Translation of slippage (mm) | 1.1±1.6 | 0.9±0.9 | 0.638 | |||
| Type of facet joint | 0.826 | |||||
| Posteromedial | 1 | 9 | ||||
| Transitional | 4 | 0 | ||||
| Posterolateral | 3 | 14 | ||||
| Saggital facet slope (°) | 26.9±9.3 | 30.0±11.5 | 0.499 | |||
| Alignment type | 0.661 | |||||
| A: lordosis | 5 | 7 | ||||
| B: straight | 0 | 6 | ||||
| C: kyphosis | 0 | 1 | ||||
| D: sigmoid cranial lordosis | 0 | 2 | ||||
| E: sigmoid cranial kyphosis | 3 | 7 | ||||
| C2–C7 angle (°) | 15.9±21.2 | 8.8±14.4 | 0.298 | |||
| C2–C7 SVA (mm) | 25.0±15.5 | 21.8±17.0 | 0.646 | |||
| Flex C2–C7 angle (°) | −13.1±20.1 | −10.9±14.9 | 0.745 | |||
| Ext C2–C7 angle (°) | 27.4±21.9 | 24.7±12.7 | 0.683 | |||
| ROM (°) | 40.5±11.0 | 35.6±12.2 | 0.331 | |||
| Slipped disc angle (°) | 6.5±4.0 | 1.7±8.1 | 0.123 | |||
| Slipped disc ROM (°) | 9.0±4.1 | 7.7±4.5 | 0.474 | |||
Values are presented as number or mean±standard deviation. The bold type is considered statistically significant.
DHG, disc height grade; CSM, cervical spondylotic myelopathy; OPLL, ossification of posterior longitudinal ligament; Flex, flexion; Ext, extension; SVA, sagittal vertical axis; ROM, range of motion.
If it was a C4 spondylolisthesis, it was evaluated as 4.
The slipped vertebra was excluded in the surgical site in 13.5% (7/52) of anterior slippage and 6.5% (2/31) of the posterior slippage. The fixation surgery was performed on the slipped vertebrae in 17.3% (9/52) of anterior slippage and 12.9% (4/31) of the posterior slippage.
2. Slippage in neutral, flexed, and extended positions
No significant difference was found in sliding distance in the neutral and extended positions when anterior slippage was examined in five groups by DHG. Although the ANOVA showed a significant difference in the distance of slippage in the extended position, the post-hoc tests showed no difference. However, the distance of slippage was significantly smaller in cases with no disc height narrowing at DHG 0 in the flexed position. When the subject extended the neck from the neutral position, the distance of slippage shortened, and when the subject flexed the neck, the distance of slippage increased in all DHG groups. When the subject extended his neck, the distance of slippage changed more than when he flexed his neck.
In posterior slippage, when sliding was examined in two groups by DHG, the distance of slippage was significantly greater in cases with strong narrowing of the disc height at DHG 4 in a flexed position. In the neutral and extended positions, the distance of slippage was greater in the DHG 4 group, but not statistically significant. When the subject flexed the neck from the neutral position, the distance of slippage was shorter in all groups, and the distance of slippage was slightly larger in the extended position. In posterior slippage, unlike anterior slippage, the distance of slippage changed more when the subject flexed the neck than when the subject extended the neck (Table 1, Fig. 1).
3. Other radiological findings
In either anterior or posterior slippage, no significant difference was found in the distribution of facet type at axial, facet slope at sagittal, or overall cervical alignment. Similarly, no significant difference was found in C2–C7 angle, C2–C7 SVA, ROM, slipped disc angle, and slipped disc ROM (Table 1).
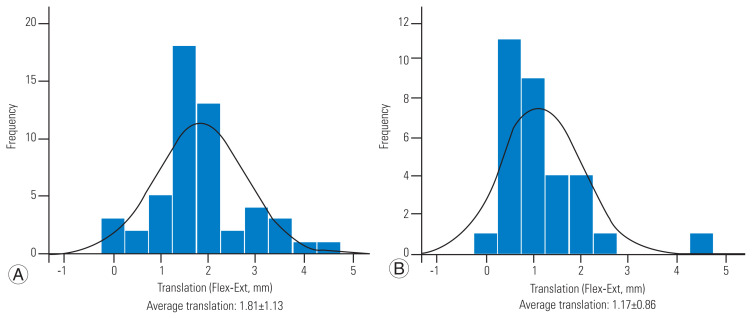
4. Translation of slippage
The translation of anterior slippage in flexion-extension motion is evenly spread around the mean value in the case of anterior slippage. Conversely, in the case of posterior slippage, the change in translation is smaller, and the distribution around the mean value is steeper. The anterior slippage exhibited a mean translation of 1.8 mm, and the posterior slippage exhibited a mean translation of 1.2 mm in flexion-extension motion. Using this average value as a threshold, we analyzed the risk factors for the larger translation as follows (Fig. 4).
Fig. 4.
Histogram of the translation of the slippage in flexion (Flex)-extension (Ext) motion of anterior (A) and posterior (B) slippage. The histogram of anterior slippage is gentle and has a larger change of value in translation. The histogram of posterior slippage is steeper and the change of value in translation is smaller. Values are presented as mean±standard deviation.
-
Risk factor analysis for a translation of slippage more than 1.8 mm in flexion-extension motion of anterior slippage
Univariate logistic regression analysis was performed for age, sex ratios, the type of disease, level of slippage, slippage in a neutral position, DHG, type of facet joint in axial, sagittal facet joint slope, a type of global cervical alignment, C2–C7 angle, C2–C7 SVA, C2–C7 angle in flexion and extension, ROM, slipped disc angle, and slipped disc ROM. In a univariate logistic regression analysis, sex ratios, level of slippage, DHG, ROM, and slipped disc ROM were all found to be significant risk factors for anterior slippage translation greater than 1.8 mm in flexion-extension motion. Multivariate logistic regression analysis showed that DHG, ROM, and slipped disc ROM was the significant risk factor. The present results show that every 1-grade increase in DHG is 10.4 times more at risk of a translation of slippage more than 1.8 mm in flexion-extension motion, 1.1 times for every 1° increase in ROM, and 1.5 times for every 1° increase in slipped disc ROM (Tables 2, 3).
-
Analysis for the cutoff value of DHG, ROM, and slipped disc ROM for the translation of slippage more than 1.8 mm in flexion-extension motion of anterior slippage
The ROC curve was drawn for the translation of slippage more than 1.8 mm in flexion-extension motion of anterior slippage. Next, the cutoff value was examined using the Youden index. Area under the ROC curve was 0.620 for DHG, 0.617 for ROM, and 0.701 for slipped disc ROM. The cutoff value for DHG was 1.5, with a sensitivity of 0.542 and specificity of 0.714. The cutoff value for ROM was 33.5, with a sensitivity of 0.625 and specificity of 0.643. The cutoff value for slipped disc ROM was 5, with a sensitivity of 0.900 and specificity of 0.714.
-
Risk factor analysis for a translation of slippage more than 1.2 mm in flexion-extension motion of posterior slippage
The level of slippage was found to be a significant risk factor for a translation of slippage greater than 1.2 mm in the flexion-extension motion of posterior slippage in univariate logistic regression analysis. Multivariate logistic regression analysis showed no statistically significant risk factor for a translation of slippage more than 1.2 mm (Tables 4, 5).
Table 2.
Risk factor analysis for translation of slippage more than 1.8 mm in flexion-extension motion of anterior slippage
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
|
|
|
|||
| p-value | OR (95% CI) | p-value | OR (95% CI) | |
| Age | 0.137 | |||
|
| ||||
| Male/female | 0.001 | 0.100 (0.025–0.401) | 0.192 | |
|
| ||||
| Disease | 0.792 | |||
|
| ||||
| Slipped level | 0.028 | 0.594 (0.374–0.945) | 0.694 | |
|
| ||||
| Slippage in neutral | 0.905 | |||
|
| ||||
| Disc height grade | 0.021 | 2.000 (1.109–3.608) | 0.004 | 10.401 (2.082–51.954) |
|
| ||||
| Type of facet joint | 0.924 | |||
|
| ||||
| Sagittal facet slope | 0.783 | |||
|
| ||||
| Alignment type | 0.670 | |||
|
| ||||
| C2–C7 angle | 0.165 | |||
|
| ||||
| C2–C7 sagittal vertical axis | 0.125 | |||
|
| ||||
| Flexion C2–C7 angle | 0.053 | |||
|
| ||||
| Extension C2–C7 angle | 0.264 | |||
|
| ||||
| ROM | 0.006 | 1.096 (1.026–1.171) | 0.025 | 1.148 (1.017–1.295) |
|
| ||||
| Slipped disc angle | 0.617 | |||
|
| ||||
| Slipped disc ROM | 0.003 | 1.300 (1.091–1.550) | 0.023 | 1.491 (1.058–2.102) |
The bold type is considered statistically significant.
OR, odds ratio; CI, confidence interval; ROM, range of motion.
Table 3.
A number of disc levels and the mean values of factors that were significant risks in the multivariate logistic regression analysis for translation of slippage more than 1.8 mm in flexion-extension motion of anterior slippage
| Translation of slippage | Anterior slippage | p-value | |
|---|---|---|---|
| ≥1.8 mm | <1.8 mm | ||
| No. of disc level | 22 | 30 | |
| Disc height grade | 2.1±1.2 | 1.3±0.9 | 0.014 |
| ROM | 41.9±14.4 | 29.8±10.3 | 0.001 |
| Slipped disc ROM | 11.9±4.4 | 6.2±4.7 | 0.000 |
Values are presented as number of mean±standard deviation. The bold type is considered statistically significant.
ROM, range of motion.
Table 4.
Risk factor analysis for translation of slippage more than 1.2 mm in flexion-extension motion of posterior slippage
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
|
|
|
|||
| p-value | OR (95% CI) | p-value | OR (95% CI) | |
| Age | 0.872 | |||
|
| ||||
| Male/female | 0.955 | |||
|
| ||||
| Disease | 0.904 | |||
|
| ||||
| Slipped level | 0.036 | 0.430 (0.196–0.946) | 0.057 | |
|
| ||||
| Slippage in neutral | 0.983 | |||
|
| ||||
| Disc height grade | 0.768 | |||
|
| ||||
| Type of facet joint | 0.458 | |||
|
| ||||
| Sagittal facet slope | 0.894 | |||
|
| ||||
| Alignment type | 0.165 | |||
|
| ||||
| C2–C7 angle | 0.651 | |||
|
| ||||
| C2–C7 sagittal vertical axis | 0.194 | |||
|
| ||||
| Flexion C2–C7 angle | 0.572 | |||
|
| ||||
| Extension C2–C7 angle | 0.770 | |||
|
| ||||
| ROM | 0.254 | |||
|
| ||||
| Slipped disc angle | 1.000 | |||
|
| ||||
| Slipped disc ROM | 0.146 | 0.287 | ||
The bold type is considered statistically significant.
OR, odds ratio; CI, confidence interval; ROM, range of motion.
Table 5.
A number of disc levels and the mean values of factors that were the risks in the univariate logistic regression analysis for translation of slippage more than 1.2 mm in the posterior slippage
| Translation of slippage | Posterior slippage | p-value | |
|---|---|---|---|
| ≥1.2 mm | <1.2 mm | ||
| No. of disc level | 13 | 18 | |
| Slipped level | 3.9±0.9 | 4.7±1.0 | 0.028 |
Values are presented as number of mean±standard deviation. The bold type is considered statistically significant.
Discussion
Because the pathologies were different between the two conditions, we divided cervical spondylolisthesis into anterior and posterior slippage in this study. According to our reports, anterior cervical slippage often manifests itself in the cephalad intervertebral space above the level where the disc height decreased, whereas slipped intervertebral space often persists and can still slip in flexion. Alternatively, posterior slippage of the cervical spine appears in the intervertebral space where the disc height is markedly reduced for advanced disc degeneration [6]. In fact, in this study, various DHGs (from 0 to 4) existed in the anteriorly slipped intervertebral space. DHGs are only 3 and 4 in the posteriorly slipped intervertebral space, and the disc height is significantly reduced.
In the results of anterior cervical slippage, only two radiological parameters were significantly different among the five groups divided by DHG. First, in the flexed position, the distance of slippage was smaller in the group without disc height narrowing. Second, in the group without disc height narrowing, the translation of slippage in flexion-extension motion was the smallest. Because of the proper elasticity of healthy discs, the slippage in the flexed position is less likely to be larger if the disc height remains constant. The appearance of instability after disc degeneration in the first stage of the degenerative cascade in the lumbar spine is consistent with these results [4,5].
Alternatively, multivariate logistic regression analysis showed that the factors associated with a translation in anterior slippage of more than 1.8 mm in flexion-extension motion were narrowing of disc height, greater ROM, and greater slipped disc ROM. The easier it is to move and thus the greater the amount of slip movement, the larger the ROM and slipped disc ROM. When the disc height was narrowed, it was discovered that the mobility at the slipped level was not stabilized. Rather, the possibility of moving more than 1.8 mm in the flexion-extension motion increased with stronger disc narrowing. In an analysis using the ROC curve, we found that this instability appeared after the middle stage of disc space narrowing when disc space narrowing appeared more than 25%. This is the first report that describes this result. In lumbar spondylolisthesis, some studies suggest that a decrease in disc height cannot be involved in the stability of the slipped intervertebral space, and researchers pointed out that controversy is still needed [15]. The mobility of the slipped intervertebral space was not stabilized in the cervical spondylolisthesis when the disc height narrowed at a slipped level. The cervical spine, which is supposed to move, appears to exhibit a built-in structure that allows it to move even after degeneration.
In the results of posterior slippage, we found that the distance of slippage in flexion was significantly greater in the DHG 4 group, which exhibited a narrower disc height. In the DHG 4 group, the distance of slippage in neutral and extension was also significantly greater. After the disc space narrows, it is understandable that mobility between vertebrae in the cephalocaudal direction shifts to mobility in the anterior-posterior direction. Therefore, the narrower the intervertebral space, the greater the slippage. Univariate logistic regression analysis showed that the factors associated with a translation in the posterior slippage of more than 1.2 mm in flexion-extension motion were cephalad intervertebral space slippage. The univariate analysis for anterior spondylolisthesis included this risk factor as well. These study results could indicate that the cephalad vertebra is a risk factor for cervical spondylolisthesis instability. Because the cephalic vertebrae exhibit a longer distance to travel in flexion-extension motion, it makes sense that they would move more in the anterior-posterior direction. However, we think that further investigation is necessary, especially for posterior cervical spondylolisthesis, since there are few cases in this study, and statistical power was low as it was the same in previous reports [7,10–12].
We, for the first time, described in this study that a difference was found in the distribution of translation of the slippage in flexion-extension motion between anterior and posterior slippage. In the flexion-extension motion, the variation in translation of anterior slippage is large, whereas the variation in translation of posterior slippage is small. In the anterior-posterior direction, this result could also indicate that anterior slippage is more mobile than posterior slippage. From the result of translation of slippage divided by the DHG, we suggested that the translation of slippage in flexion-extension motion of anterior slippage did not decrease when the intervertebral disc was narrowed. In the case of posterior slippage, the movement of the slippage in flexion-extension motion was not related to disc space narrowing, even though the slippage itself progressed, according to disc space narrowing.
The results of this study did not support the degenerative cascade theory, that is, disc narrowing contributes to the stability of slippage [4,5]. Our findings suggest that the cervical spine is an organ that innately tends to move. When we consider the results of this study, the indication for decompression surgery for cervical spondylolisthesis should be carefully considered. It should be kept in mind that even if the intervertebral disc space is narrowed, fixation surgery should be considered. However, since this study did not include clinical symptoms, future studies including clinical information are needed.
Although this study exhibits a larger sample size than the cervical spondylolisthesis study, it is still a retrospective study with a small number of cases. This reduces the precision of logistic regression analysis and the ability to set appropriate thresholds for slippage translation. A selection bias was not excluded because healthy subjects were not included as controls in this study. Precisely knowing whether narrowing of disc height itself contributes to intervertebral instability is impossible because this study was not a longitudinal one. It is desirable to perform a longitudinal study with a larger sample size including healthy subjects as controls.
Conclusions
In anterior slippage, narrowing the disc space did not reduce slippage translation in flexion-extension motion. Conversely, the narrowing of the disc space was a risk factor for 1.8 mm or more translation. Furthermore, anterior slippage exhibited a larger variety of translation in flexion-extension motion than posterior slippage. Next, the narrowing of the disc space in the posterior slippage did not increase the translation of slippage as in the anterior slippage. With the narrowing of the disc space, the posterior slippage progressed as well. The findings of this study show that the cervical spine is not affected by the degenerative cascade.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by all authors. The first draft of the manuscript was written by Ryoma Aoyama, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
References
- 1.Friberg O. Instability in spondylolisthesis. Orthopedics. 1991;14:463–5. doi: 10.3928/0147-7447-19910401-11. [DOI] [PubMed] [Google Scholar]
- 2.Lattig F, Fekete TF, Grob D, Kleinstuck FS, Jeszenszky D, Mannion AF. Lumbar facet joint effusion in MRI: a sign of instability in degenerative spondylolisthesis? Eur Spine J. 2012;21:276–81. doi: 10.1007/s00586-011-1993-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matsunaga S, Sakou T, Morizono Y, Masuda A, Demirtas AM. Natural history of degenerative spondylolisthesis: pathogenesis and natural course of the slippage. Spine (Phila Pa 1976) 1990;15:1204–10. doi: 10.1097/00007632-199011010-00021. [DOI] [PubMed] [Google Scholar]
- 4.Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976) 1978;3:319–28. doi: 10.1097/00007632-197812000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Kirkaldy-Willis WH, Farfan HF. Instability of the lumbar spine. Clin Orthop Relat Res. 1982;(165):110–23. [PubMed] [Google Scholar]
- 6.Aoyama R, Shiraishi T, Kato M, et al. Characteristic findings on imaging of cervical spondylolisthesis: analysis of computed tomography and X-ray photography in 101 spondylolisthesis patients. Spine Surg Relat Res. 2018;2:30–6. doi: 10.22603/ssrr.2017-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dean CL, Gabriel JP, Cassinelli EH, Bolesta MJ, Bohlman HH. Degenerative spondylolisthesis of the cervical spine: analysis of 58 patients treated with anterior cervical decompression and fusion. Spine J. 2009;9:439–46. doi: 10.1016/j.spinee.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 8.Jiang SD, Jiang LS, Dai LY. Degenerative cervical spondylolisthesis: a systematic review. Int Orthop. 2011;35:869–75. doi: 10.1007/s00264-010-1203-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kawasaki M, Tani T, Ushida T, Ishida K. Anterolisthesis and retrolisthesis of the cervical spine in cervical spondylotic myelopathy in the elderly. J Orthop Sci. 2007;12:207–13. doi: 10.1007/s00776-007-1122-5. [DOI] [PubMed] [Google Scholar]
- 10.Lee C, Woodring JH, Rogers LF, Kim KS. The radiographic distinction of degenerative slippage (spondylolisthesis and retrolisthesis) from traumatic slippage of the cervical spine. Skeletal Radiol. 1986;15:439–43. doi: 10.1007/BF00355101. [DOI] [PubMed] [Google Scholar]
- 11.Ninomiya K, Yamane J, Aoyama R, et al. Clinical effects of anterior cervical spondylolisthesis on cervical spondylotic myelopathy after posterior decompression surgery: a retrospective multicenter study of 732 cases. Global Spine J. 2020. Nov 18, [Epub]. [DOI] [PMC free article] [PubMed]
- 12.Park MS, Moon SH, Oh JK, Lee HW, Riew KD. Natural history of cervical degenerative spondylolisthesis. Spine (Phila Pa 1976) 2019;44:E7–12. doi: 10.1097/BRS.0000000000002764. [DOI] [PubMed] [Google Scholar]
- 13.Matsumoto M, Fujimura Y, Suzuki N, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19–24. doi: 10.1302/0301-620x.80b1.7929. [DOI] [PubMed] [Google Scholar]
- 14.Takeshima T, Omokawa S, Takaoka T, Araki M, Ueda Y, Takakura Y. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine (Phila Pa 1976) 2002;27:E348–55. doi: 10.1097/00007632-200208010-00014. [DOI] [PubMed] [Google Scholar]
- 15.Simmonds AM, Rampersaud YR, Dvorak MF, Dea N, Melnyk AD, Fisher CG. Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine. 2015;23:178–89. doi: 10.3171/2014.11.SPINE1426. [DOI] [PubMed] [Google Scholar]