Abstract
Study Design
Retrospective cohort study.
Purpose
This study aimed to evaluate the relationship between C7 plumb line (C7PL) decompensation and the Scoliosis Research Society (SRS) 22-item patient questionnaire scores, including those related to self-image, preoperatively and 2 years after surgery.
Overview of Literature
In the surgical treatment of adolescent idiopathic scoliosis (AIS), inferior trunk balance caused by C7PL decompensation can negatively affect patients’ quality of life. However, there are few reports in the literature that describe or clarify how postoperative trunk imbalance affects each SRS-22 domain, including self-image domain scores.
Methods
A total of 120 patients with AIS who underwent posterior spinal fusion from August 2006 to March 2017 at our facility and were followed up for 2 years or more were included. Radiological parameters were measured on whole-spine anteroposterior and lateral radiographs. Revised SRS-22 (SRS-22r) values were also recorded. Coronal trunk imbalance was defined as a deviation of ≥2.0 cm between the C7PL and the central sacral vertical line. Patients with and without coronal trunk imbalance at 2 years after surgery were defined as D (+) (decompensation type) and D (−), respectively. Mean SRS-22r values, including function, pain, self-image, mental health, and subtotal were compared between the D (+) and D (−) groups. Logistic regression analysis was performed to detect the preoperative factors related to D (+) using predictors, including curve type, maximum Cobb angle, and coronal trunk imbalance.
Results
At 2 years after surgery, the D (+) group had a significantly lower self-image in the domain of SRS-22r scores compared with the D (−) group. Preoperative coronal trunk imbalance was significantly related to D (+) but not to significant changes in the postoperative SRS-22 score in any of the SRS-22 domains.
Conclusions
Postoperative C7PL deviation lowers the self-image in patients with AIS. Patients with preoperative coronal trunk imbalance were significantly more likely to be D (+).
Keywords: Scoliosis, Postural balance, Adolescent, Postoperative complications, Patient outcome assessment
Introduction
An ideal standing trunk balance in the treatment of adolescent idiopathic scoliosis (AIS) is defined by the alignment of the C7 plumb line (C7PL) and central sacral vertical line (CSVL) on the coronal plane and C7PL located at the posterosuperior edge of the first sacral vertebrae in the sagittal view [1,2]. Despite achieving a good postoperative correction of scoliosis, residual decompensation of the coronal trunk balance is occasionally observed due to coronal decompensation. In such cases, inferior trunk balance caused by C7PL decompensation, which is not directly related to the functional disorder, can negatively affect patients’ quality of life. Given that AIS commonly presents in sensitive adolescent patients who are prone to be affected by psychological stress, the mental health of patients with residual decompensation should be carefully considered [3]. The the Scoliosis Research Society (SRS) 22-item patient questionnaire is a widely adopted method for evaluating AIS. The questionnaire’s self-image domain score—which includes the patient’s impression of their appearance while clothed, the presence of depressed mood, and treatment satisfaction—accurately reflects the patient’s psychological traits [3]. Although good trunk balance (i.e., an ability to maintain postural control without coronal trunk deviation as measured with a plumb line from C7 to S1) was associated with little pain [4], there are few reports in the literature that describe or clarify how postoperative trunk imbalance affects each SRS-22 domain, including self-image domain scores.
In this study, we evaluated the relationship between C7PL decompensation and SRS-22 scores, including those relating to self-image, before and 2 years after surgery.
Materials and Methods
We conducted this study in compliance with the principles of the Declaration of Helsinki. The study’s protocol was reviewed and approved by the Institutional Review Board of Shinshu University (IRB approval no., 3716). After obtaining written informed consent, 120 patients with AIS (12 males and 108 females; mean±standard deviation age, 14.9±2.1 years) who underwent posterior spinal fusion between August 2006 and March 2017 at our facility and were followed up for ≥2 years were enrolled in the study.
In terms of the frontal trunk balance, the SRS defines “compensation” as having a C7PL decompensation of less than 1.5 cm from the CSVL. Although there are some variations in how “decompensation” is defined, in the context of poor trunk balance, most patients exhibit a deviation of 2.0 cm or more [5,6]. Therefore, patients in this study with a C7PL deviation of ≥2.0 cm from the CSVL at 2 years after surgery were defined as having decompensation type and denoted as D (+), and patients with <2.0 cm deviation were denoted as D (−). Clinical outcomes were assessed and compared between the D (+)/D (−) groups. For clinical evaluations, the results of the SRS-22 questionnaire for function, pain, self-image, mental health, subtotal, and satisfaction were compared. Scoring was performed using the Japanese version of the original SRS-22 questionnaire [7,8]. Measurements were performed 3 times by the first author, who had not attended the surgery, and the mean value was calculated.
An unpaired t-test and Fisher’s exact test were used to compare D (+)/(−). Logistic regression analysis was performed to detect the associated factors of D (+) by using the preoperative curve type, preoperative maximum Cobb angle, and preoperative coronal trunk imbalance (C7PL deviation of ≥2.0 cm from the CSVL) as candidate factors. All p-values of <0.05 were considered statistically significant. Statistical analysis was performed using IBM SPSS Statistics ver. 21.0 (IBM Corp., Armonk, NY, USA).
Results
Among the 120 cases, there were 18 cases of D (+) and 102 cases of D (−) (Table 1). The mean±standard deviation postoperative C7PL deviation was 1.1±0.1 cm, and 15 of 18 D (+) patients exhibited a trunk imbalance with C7PL >2.0 cm immediately after surgery. The remaining three patients showed a C7PL <2.0 cm at 3 months postoperatively but subsequently became D (+). There were no significant differences in age, sex, height, weight, body mass index, Lenke curve type, number of fused vertebrae, or surgical time between the two groups.
Table 1.
Baseline patient characteristics
| Characteristic | Total | D (+) | D (−) | D (+) vs. D (−) p-value |
|---|---|---|---|---|
| No. of patients | 120 | 18 | 102 | |
| Age (yr) | 14.8±2.1 | 14.2±2.0 | 14.9±2.1 | 0.33 |
| Sex | 0.97 | |||
| Male | 12 | 2 | 10 | |
| Female | 108 | 16 | 92 | |
| Height (cm) | 154.4±7.5 | 160.9±1.8 | 153.7±7.5 | 0.12 |
| Weight (kg) | 45.0±7.3 | 48.2±4.6 | 44.7±7.4 | 0.44 |
| Body mass index (kg/m2) | 19.0±2.5 | 18.6±1.7 | 19.1±2.6 | 0.77 |
| Lenke curve type | 0.55 | |||
| 1 | 53 | 8 | 45 | |
| 2 | 15 | 1 | 14 | |
| 3 | 2 | 1 | 1 | |
| 4 | 3 | 0 | 3 | |
| 5 | 29 | 4 | 25 | |
| 6 | 18 | 4 | 14 | |
| No. of fused vertebrae | 8.9±2.8 | 10.1±2.7 | 8.7±2.7 | 0.16 |
| Surgical time (min) | 203±75 | 242±93 | 196±70 | 0.08 |
| Amount of bleeding (mL) | 833±695 | 1,235±851 | 768±644 | 0.05 |
Values are presented as number for categorical variables or mean±standard deviation for continuous variables.
D (+), decompensation group at 2 years after the operation; D (−), compensation group at 2 years after the operation.
1. Clinical performance evaluation (SRS-22r)
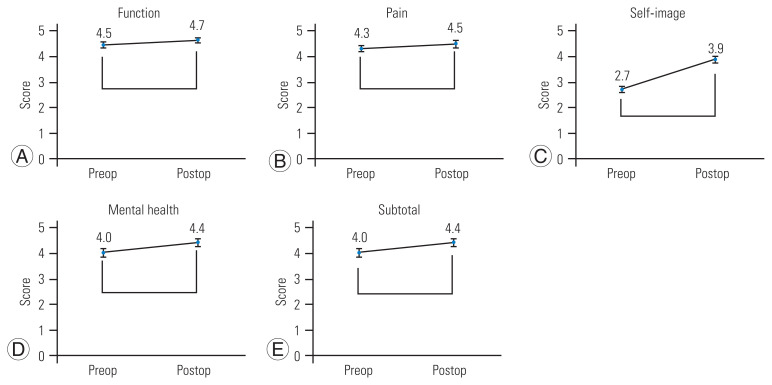
When all the data were analyzed, improvements in the postoperative SRS-22 scores were observed. All domains achieved statistically significant improvements except for the pain domain (Fig. 1). Function improved from 4.5 points to 4.7 points (difference, 0.2 points; 95% confidence interval [CI], 0.1–0.3; p<0.01); pain, 4.3 to 4.5 (difference, 0.2; 95% CI, 0.0–0.3; p=0.12); self-image, 2.7 to 3.9 (difference, 1.2; 95% CI, 1.1–1.5; p<0.01); mental health, 4.0 to 4.4 (difference 0.5; 95% CI, 0.3–0.6; p<0.01); and subtotal, 4.0 to 4.4 (difference, 0.4; 95% CI, 0.4–0.6; p<0.01).
Fig. 1.
(A–E) Scoliosis Research Society 22-item patient questionnaire score changes of all subjects. Error bars represent 95% confidence intervals. Preop, preoperation; Postop, 2 years after the operation. *p<0.05.
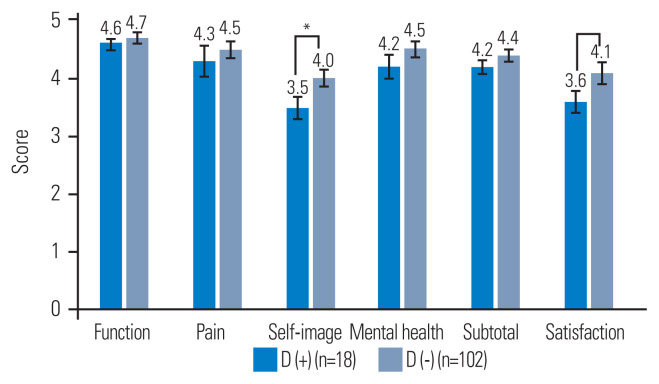
At 2 years after surgery, the D (+) was significantly lower compared with the D (−) in self-image and satisfaction in the revised SRS-22 (SRS-22r) domain scores (Fig. 2). The results were as follows: mean function: D (+), 4.6 points (95% CI, 4.5–4.7) and D (−), 4.7 (95% CI, 4.6–4.8), p=0.14; pain: D (+), 4.3 (95% CI, 4.1–4.5) and D (−) 4.5 (95% CI, 4.3–4.6), p=0.62; self-image: D (+), 3.5 (95% CI, 3.3–3.7) and D (−), 4.0 (95% CI, 3.9–4.2), p<0.01; mental health: D (+), 4.2 (95% CI, 4.0–4.4) and D (−), 4.5 (95% CI, 4.3–4.6), p=0.50; subtotal: D (+), 4.2 (95% CI, 4.1–4.3) and D (−), 4.4 (95% CI, 4.3–4.5), p=0.54; and satisfaction, D (+), 3.6 (95% CI, 3.3–3.8) and D (−), 4.1 (95% CI, 3.9–4.3), p=0.01. According to stratification by the degree of coronal deviation, the mean self-image score was 4.1 in the group with postoperative C7PL deviation <1 cm and 4.0 in the group with postoperative C7PL deviation >1 cm to <2 cm, with no significant difference between the groups (p=0.50). Similarly, the respective mean satisfaction scores were comparable at 4.2 and 4.0 (p=0.26).
Fig. 2.
Comparison of the Scoliosis Research Society 22-item patient questionnaire scores at 2 years after the operation between D (+) and D (−). Error bars represent 95% confidence intervals. D (+), decompensation group at 2 years after the operation; D (−), compensation group at 2 years after the operation. *p<0.05.
The minimal clinically important difference (MCID) for self-image is reported to be 0.98 [9]. In terms of postoperative self-image, the D (−) showed better mean improvement than 0.98, whereas the D (+) did not, and there was a significant difference in the improvement score (p=0.03). The improvement in D (−) was 1.4 (95% CI, 1.2–1.6), and that of D (+) was 0.9 (95% CI, 0.7–1.2). The number of patients who achieved MCID in the D (−) and D (+) groups were 68 (67%) of 102 patients and 9 (50%) of 18 patients, respectively, with no significant differences in the rate of MCID achievement between the groups (p=0.17).
2. Preoperative curve profile associated with postoperative decompensation
We examined the curve type, maximum Cobb angle, and coronal trunk imbalance, and only the coronal trunk imbalance showed a significant association with D (+) (Table 2). Although the thoracolumbar/lumbar curve was significantly associated with preoperative trunk imbalance (Table 3), no clear association was observed with postoperative coronal balance (Table 2). There was no clear association between the maximum Cobb angle and preoperative and postoperative coronal trunk imbalance (Tables 2, 3).
Table 2.
Preoperative associated factors for postoperative coronal decompensation
| Candidate | Odds ratio (95% CI) | p-value |
|---|---|---|
| Preoperative coronal imbalance (more than 2 cm) | 5.1 (1.3–20.8) | 0.02* |
| Main curve site (TL/L curve) | 1.7 (0.4–6.5) | 0.44 |
| Cobb angle (+10°) | 1.3 (0.8–2.2) | 0.30 |
CI, confidence interval; TL/L, thoracolumbar or lumbar.
p<0.05.
Table 3.
Preoperative associated factors for preoperative coronal decompensation
| Candidate | Odds ratio (95% CI) | p-value |
|---|---|---|
| Main curve site (TL/L curve) | 3.4 (1.2–9.9) | 0.03* |
| Cobb angle (+10°) | 1.1 (0.7–1.7) | 0.77 |
CI, confidence interval; TL/L, thoracolumbar or lumbar.
p<0.05.
It was unclear how the curve profile changed by surgery affected the decompensation type. The correction rate of the thoracic curve for D (+) and D (−) was 59% and 52%, respectively, with no significant difference between the groups (p=0.45). Comparable findings were observed for the correction rate of the TL/L curve (58% and 60%, respectively; p=0.84).
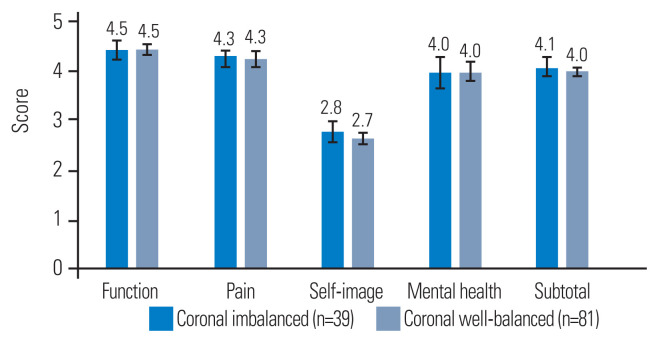
3. Influence of preoperative coronal trunk imbalance on the clinical outcome
There were no significant differences in the SRS-22 score in any domains between patients with and without preoperative coronal trunk imbalance (Fig. 3). The SRS-22 scores were as follows: mean function of those with preoperative decompensation of coronal balance, 4.5 points (95% CI, 4.3–4.7), and those with preoperative non-decompensation of coronal balance, 4.5 (95% CI, 4.3–4.6), showing no significant difference (p=0.99); pain, 4.3 (95% CI, 4.2–4.4) and 4.3 (95% CI, 4.1–4.4), p=0.08; self-image, 2.8 (95% CI, 2.6–2.9) and 2.7 (95% CI, 2.5–2.8), p=0.10; mental health, 4.0 (95% CI, 4.3–4.7) and 4.0 (95% CI, 3.8–4.2), p=0.70; and subtotal, 4.1 (95% CI, 3.9–4.2) and 3.9 (95% CI, 3.9–4.1), p=0.42.
Fig. 3.
Comparison of the Scoliosis Research Society 22-item patient questionnaire scores at 2 years after the operation between coronal imbalanced cases and well-balanced cases preoperatively. Error bars represent 95% confidence intervals.
In the D (+) group, five patients exhibited C7PL <2.0 cm preoperatively. These cases revealed no distinctive features in terms of the position of the major curve and the size of the Cobb angle (Table 4).
Table 4.
Clinical features of patients who switched from non-imbalance to D (+)
| Case no. | Age (yr) | Sex | Lenke type | Preoperative | Postoperative | Satisfaction | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||
| Cobb angle (°) | C7PL (cm) | Self-image | C7PL (cm) | Self-image | |||||
| 1 | 11 | Female | 6 | 51 | Lt. 1.1 | 2.4 | Lt. 2.4 | 3.8 | 5 |
|
| |||||||||
| 2 | 17 | Female | 2 | 43 | Rt. 0.6 | 2.6 | Lt. 2.0 | 3.4 | 4 |
|
| |||||||||
| 3 | 12 | Female | 1 | 48 | Rt. 0.8 | 2.4 | Lt. 2.3 | 3.4 | 4 |
|
| |||||||||
| 4 | 15 | Female | 3 | 87 | Lt. 1.2 | 2.6 | Lt. 3.5 | 4.2 | 4 |
|
| |||||||||
| 5 | 12 | Female | 1 | 52 | Rt. 1.1 | 1.8 | Lt. 3.5 | 3.6 | 4 |
D (+), decompensation group at 2 years after the operation; C7PL, C7 plumb line; Rt, right; Lt, left.
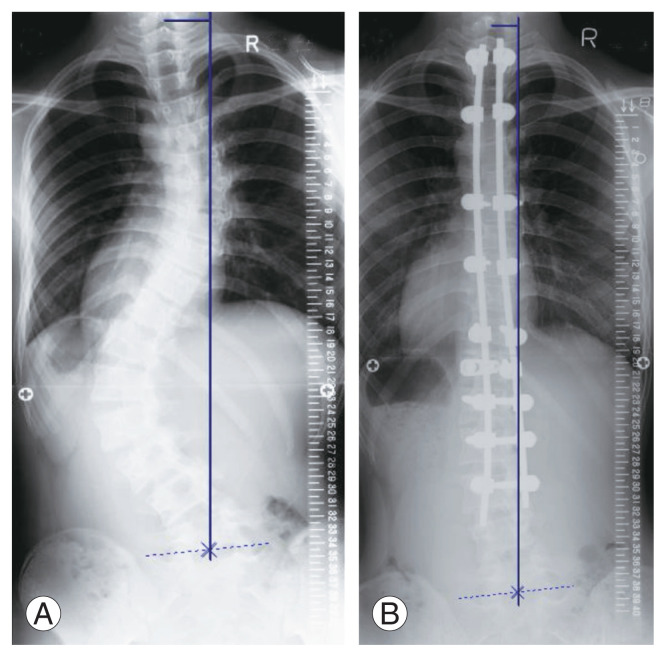
4. Report of a typical case
A 14-year-old female was diagnosed with AIS by a nearby hospital and visited our department. Her condition was Lenke type 6C (main thoracic curve=45°, thoracolumbar curve=74°) (Fig. 4A). C7PL decompensation was 3.5 cm to the left. Her SRS-22 scores were as follows: pain, 4.0; function, 3.8; self-image, 3.0; mental health, 3.4; and subtotal, 3.55. Posterior correction and fusion (Th2–L3) were performed. At 2 years postoperatively, the Cobb angle at the thoracic and thoracolumbar curves were 14° and 19°, respectively (Fig. 4B); C7PL deviation was 2.1 cm to the left; and SRS-22 scores were pain 4.8, function 3.8, self-image 3.4, mental health 4.8, subtotal 4.2, and satisfaction 2.0.
Fig. 4.
Posteroanterior radiograph of a typical case. (A) Before surgery. (B) 2 Years postoperatively.
Discussion
Our study showed that postoperative C7PL deviation is a factor that worsens the self-image in patients with AIS. Interestingly, there was no apparent association between C7PL deviation and self-image preoperatively. At 2 years after surgery, however, the self-image of patients with a C7PL deviation of 2 cm or more from CSVL was significantly poorer than patients with a deviation of 2 cm or less.
There have been some reports on the relationship between trunk balance and SRS score in patients with AIS. Fortin et al. [4] reported no relationship between trunk balance failure and either function, pain, self-image, or mental health, in 55 patients with AIS who did not undergo surgery. Watanabe et al. [10] suggested a ≥40° Cobb angle and a ≥20° of rotation angle in surgically untreated AIS to be factors that worsen patients’ self-image; on the other hand, inferior trunk balance with C7PL decompensation of 20 to 30 mm was found to not affect self-image. Thus, Fortin et al. [4] and Watanabe et al. [10] both concluded that trunk balance was not remarkably associated with the self-image of patients with unoperated scoliosis. These results are consistent with our study, which showed no significant differences in SRS-22 score between the patients with or without preoperative coronal trunk imbalance.
It has been reported that the improvement in self-image after AIS is associated with the correction of breast asymmetry and shoulder balance [11]. However, few reports in the literature have examined the relationship between C7PL and self-image. D’Andrea et al. [12] investigated the association between preoperative and 2-year postoperative radiographic imaging scores from the Harms Study Group and SRS scores in 78 patients with AIS. The radiographic scoring system of the Harms Study Group was measured on a 100-point scale, and a C7PL deviation of <2.0 from CSVL was defined as 5 points, with 1 point deducted for every 1.0-cm increase in deviation. Therefore, the overall effect of C7PL on this scoring method is underestimated. In a study on 890 patients with AIS, Gomez et al. [13] found no difference in SRS-22 scores between those with and without residual decompensation of coronal trunk balance at 2 years postoperatively; however, there is no mention of self-image in the study. Our study revealed that postoperative C7PL decompensation adversely affected self-image. Although preoperative C7PL decompensation had a small effect on self-image in patients with AIS, the surgical correction of scoliosis enabled a greater effect of C7PL decompensation on self-image, and we speculate that D (+) cases thus tend to result in poor self-image.
The patients with preoperative coronal imbalance in our study showed a significantly higher possibility of D (+). This result was consistent with that of a study by Karami et al. [5] that included 120 patients with AIS and showed that preoperative coronal trunk imbalance was a risk factor for trunk imbalance at 2 years postoperatively. In our study, early postoperative radiographs showed that cases with C7PL >2.0 cm tended to become D (+), and there were several cases in which trunk imbalance had subsequently progressed at 3 months to 2 years postoperatively. Munakata et al. [14] proposed the modified S-line as a method to prevent postoperative D (+). In surgery for Lenke 1 type cases, it might be possible to keep the postoperative C7PL deviation within 1 cm by determining the upper instrumented vertebra based on the modified S-line.
In this study, the preoperative major curve was thoracolumbar/lumbar, which was a risk factor for imbalance before the operation. There are similar reports in the literature. Gauchard et al. [15] studied the position of the major curve and Cobb angle in 102 patients with AIS who underwent conservative treatment and compared patients with either a thoracic or thoracolumbar/lumbar major curve, reporting that those with a thoracic curve showed smaller trunk balance decompensation. Fortin et al. [4] studied 55 patients with AIS who underwent conservative treatment and found that having a thoracolumbar/lumbar curve as a major curve was mildly associated with the decompensation of trunk balance. However, the position of the curve did not affect postoperative imbalance in this study. In addition, the size of the preoperative major curve was not related to the postoperative imbalance. Gomez et al. [13] reported no association between the residual cases of trunk imbalance and the size of the major curve before surgery, which was a similar finding to that in our study.
In this study, the satisfaction in the D (−) group was significantly higher than in the D (+) group. As a factor to improve satisfaction, Watanabe et al. [16] suggested the importance of self-image, because the improvement in self-image is related to improved treatment satisfaction, regardless of major curve pattern or pain. Together with the results of this study, it appears that C7PL correction can result in improved self-image, and subsequently, improved satisfaction.
There are two notable limitations in this study. First, the number of D (+) patients (n=18) was small, which made it difficult to conduct a multivariate analysis. Factors that affect self-image can include those other than C7PL deviation (e.g., Cobb angle correction, waist line, and shoulder balance). Further analysis might be warranted, with a larger sample size. Next, we were unable to find any remarkable characteristics in the five patients in whom the well-balanced coronal trunk became D (+). The mean postoperative self-image of these five patients was 3.7, which was higher than the mean of 3.6 for all those D (+), and we believe that it was unlikely that these five patients posed any substantial effect on our overall results. However, the cause of deterioration in balance warrants further investigation.
In patients with AIS, the value of self-image was significantly lower in decompensation cases with a C7PL deviation of 2.0 cm or more at 2 years after surgery compared with patients with less than a 2.0 cm deviation. The patients with preoperative coronal trunk imbalance showed a greater tendency to have postoperative decompensation; thus, special attention should be paid in the correction of C7PL deviation.
Footnotes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
SH and SI wrote the report. HO, MU, SK, TT, RM, TH, TK, YM, MK, and TM provided advice for improving the report. JT gave the plan of the study prior to write the report. All authors have approved the contents of the report.
References
- 1.Mac-Thiong JM, Transfeldt EE, Mehbod AA, et al. Can c7 plumbline and gravity line predict health related quality of life in adult scoliosis? Spine (Phila Pa 1976) 2009;34:E519–27. doi: 10.1097/BRS.0b013e3181a9c7ad. [DOI] [PubMed] [Google Scholar]
- 2.Richards BS, Scaduto A, Vanderhave K, Browne R. Assessment of trunk balance in thoracic scoliosis. Spine (Phila Pa 1976) 2005;30:1621–6. doi: 10.1097/01.brs.0000170298.89145.b4. [DOI] [PubMed] [Google Scholar]
- 3.Kotwicki T, Chowanska J, Kinel E, Czaprowski D, Tomaszewski M, Janusz P. Optimal management of idiopathic scoliosis in adolescence. Adolesc Health Med Ther. 2013;4:59–73. doi: 10.2147/AHMT.S32088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fortin C, Grunstein E, Labelle H, Parent S, Ehrmann Feldman D. Trunk imbalance in adolescent idiopathic scoliosis. Spine J. 2016;16:687–93. doi: 10.1016/j.spinee.2016.02.033. [DOI] [PubMed] [Google Scholar]
- 5.Karami M, Maleki A, Mazda K. Assessment of coronal radiographic parameters of the spine in the treatment of adolescent idiopathic scoliosis. Arch Bone Jt Surg. 2016;4:376–80. [PMC free article] [PubMed] [Google Scholar]
- 6.Lenke CL. Revised glossary of terms: SRS Terminology Committee and Working Group on Spinal Classification. Milwaukee (WI): Scoliosis Research Society; 2000. [Google Scholar]
- 7.Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the Scoliosis Research Society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:63–9. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- 8.Hashimoto H, Sase T, Arai Y, Maruyama T, Isobe K, Shouno Y. Validation of a Japanese version of the Scoliosis Research Society-22 Patient Questionnaire among idiopathic scoliosis patients in Japan. Spine (Phila Pa 1976) 2007;32:E141–6. doi: 10.1097/01.brs.0000255220.47077.33. [DOI] [PubMed] [Google Scholar]
- 9.Carreon LY, Sanders JO, Diab M, et al. The minimum clinically important difference in Scoliosis Research Society-22 appearance, activity, and pain domains after surgical correction of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:2079–83. doi: 10.1097/BRS.0b013e3181c61fd7. [DOI] [PubMed] [Google Scholar]
- 10.Watanabe K, Hasegawa K, Hirano T, Uchiyama S, Endo N. Use of the scoliosis research society outcomes instrument to evaluate patient outcome in untreated idiopathic scoliosis patients in Japan: part II. Relation between spinal deformity and patient outcomes. Spine (Phila Pa 1976) 2005;30:1202–5. doi: 10.1097/01.brs.0000162285.12045.81. [DOI] [PubMed] [Google Scholar]
- 11.Smith PL, Donaldson S, Hedden D, et al. Parents’ and patients’ perceptions of postoperative appearance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:2367–74. doi: 10.1097/01.brs.0000240204.98960.dd. [DOI] [PubMed] [Google Scholar]
- 12.D’Andrea LP, Betz RR, Lenke LG, et al. Do radiographic parameters correlate with clinical outcomes in adolescent idiopathic scoliosis? Spine (Phila Pa 1976) 2000;25:1795–802. doi: 10.1097/00007632-200007150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Gomez JA, Matsumoto H, Colacchio ND, et al. Risk factors for coronal decompensation after posterior spinal instrumentation and fusion in adolescent idiopathic scoliosis. Spine Deform. 2014;2:380–5. doi: 10.1016/j.jspd.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 14.Munakata R, Koseki M, Oba H, et al. Selecting the C7-LIV line vertebra as the upper instrumented vertebra for adolescent idiopathic scoliosis Lenke type 1A curves: multicenter and a minimum 2-year follow-up study. Spine (Phila Pa 1976) 2020;45:1239–45. doi: 10.1097/BRS.0000000000003509. [DOI] [PubMed] [Google Scholar]
- 15.Gauchard GC, Lascombes P, Kuhnast M, Perrin PP. Influence of different types of progressive idiopathic scoliosis on static and dynamic postural control. Spine (Phila Pa 1976) 2001;26:1052–8. doi: 10.1097/00007632-200105010-00014. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe H, Kikkawa I, Amamiya M. SRS-22 for evaluating pre- and post-operative idiopathic scoliosis. J Jpn Ped Orthop Ass. 2013;22:39–42. [Google Scholar]