Abstract
Study Objectives:
This review aims to assess the association between socioeconomic status (SES) and sleep health in the general population and the mediating effects of lifestyle and mental and physical health in this relationship.
Methods:
Observational studies testing the independent association between objective or subjective SES indicators and behavioral/physiological or clinical sleep health variables in the general population were included. PubMed/MEDLINE was searched for reports published from January 1990 to December 2019. The direction of effect was used as the primary effect measure, testing the hypothesis that low SES is associated with poor sleep health outcomes. Results are presented in the form of direction effect plots and synthesized as binomial proportions.
Results:
Overall, 336 studies were identified. A high proportion of effects at the expected direction was noted for measures of sleep continuity (100% for sleep latency, 50–100% for awakenings, 66.7–100% for sleep efficiency), symptoms of disturbed sleep (75–94.1% for insomnia, 66.7–100% for sleep-disordered breathing, 60–100% for hypersomnia), and general sleep satisfaction (62.5–100%), while the effect on sleep duration was inconsistent and depended on the specific SES variable (92.3% for subjective SES, 31.7% for employment status). Lifestyle habits, chronic illnesses, and psychological factors were identified as key mediators of the SES–sleep relationship.
Conclusions:
Unhealthy behaviors, increased stress levels, and limited access to health care in low-SES individuals may explain the SES–sleep health gradient. However, the cross-sectional design of most studies and the high heterogeneity in employed measures of SES and sleep limit the quality of evidence. Further research is warranted due to important implications for health issues and policy changes.
Citation:
Papadopoulos D, Etindele Sosso FA. Socioeconomic status and sleep health: a narrative synthesis of 3 decades of empirical research. J Clin Sleep Med. 2023;19(3):605–620.
Keywords: socioeconomic status, education, income, employment status, sleep health, sleep duration, insomnia, sleep quality
BRIEF SUMMARY
Current Knowledge/Study Rationale: A social gradient in sleep health has been observed in individual studies but its magnitude and the factors that mediate it have never been synthesized before.
Study Impact: Low socioeconomic status is significantly associated with poor sleep continuity and quality and increased symptoms of disturbed sleep in the context of multiple environmental, physical, and psychological stressful factors. A pathway model is proposed with implications for health care providers and public health policy makers.
INTRODUCTION
Physiological mechanisms of sleep disturbances were extensively documented in the last two decades,1,2 as well as their association with several other health outcomes, such as cardiovascular diseases and mental health.3 Since sleep health is a well-known health determinant,3 it is a matter of utmost importance to public health globally.4,5 It is commonly recognized that good sleep is necessary for optimal health and a poor sleep health may affect hormone levels, mood, and weight.5,6 Current clinical recommendations to improve sleep health include advice like establishing a regular sleep schedule, limiting or reducing stressors, limiting exposure to blue light in the hours before sleep, not using bed for any activities keeping the brain awake, and avoiding hormonal disruptors, such as alcohol, nicotine, caffeine, and other stimulants, in the hours before bedtime.7,8 However, people often fall under these situations because of a recurrent exposure to stressors produced by their social environment and their socioeconomic status (SES).
SES is a marker of living conditions and habits that influence health by way of different processes, including stress-related mechanisms.9 Even though measurement of SES has several methodological issues across research in health disparities,9 there is no doubt that low SES and its related chronic stress accumulated over time has major implications in health behaviors, environmental exposures, and health care utilization, resulting in increased morbidity and mortality.10–14 There is a vast amount of evidence across countries that health status is positively associated with socioeconomic indicators such as income, education, and other markers of socioeconomic position.10,11,13,14 In some analyses, lower SES is associated with greater physician and hospital use, although it appears that these findings are primarily driven by higher rates of poor health status or medical need in socioeconomically disadvantaged populations.10,11,13,14 Findings from a review in US child and adult populations with data on multiple health indicators revealed a clear gradient pattern in health disparities, in a way that even groups with intermediate SES levels were consistently less healthy than those of high SES.15 Among health outcomes influenced by variations of SES, the empirical literature also revealed that the same socioeconomic markers are often associated with sleep disturbances.
While in recent years there has been an increase in the interest in SES in sleep-related studies,5,16–21 there is a lack of reviews synthesizing the influence of SES on sleep health, leading to a general misunderstanding of the situation. There is no consensus on a positive or a negative association between SES and sleep health or sleep disturbances. Some studies reported different associations and trends between employment,22 education,23–26 or living conditions14,18,27 and individual sleep health. Furthermore, there is not enough information to understand potential pathways linking SES and sleep in general.
By studying the SES–sleep relation across the age span and also by considering the influence of socioeconomic indicators, such as education, household income, and occupation, we will be able to better understand how SES and the sleep health gradient associated with it contribute to the emergence of social inequalities and health disparities in the general population. It is important to synthesize the current literature on the SES–sleep relation and to move knowledge forward. The aims of this review are (1) to assess the association between SES and sleep health in the general population and (2) to explore the mediating effect of lifestyle and physical/mental health factors on the relationship between SES and sleep in the general population.
METHODS
Literature search
We performed a search in the PubMed/MEDLINE database to identify relevant studies testing the association between SES and various sleep indices. The search strategy included the following terms: socioeconomic* OR socio-economic* OR “social status” OR “social position*” OR “social class*” OR “social rank*” OR education* OR income* OR occupation* OR employment OR *employed OR asset* AND sleep* OR insomnia* OR circadian OR parasomnia* OR “restless leg*” OR “periodic leg movement*”. The search was restricted to published articles from January 1990 to December 2019 and excluded articles identified as reviews or meta-analyses.
Inclusion criteria
We considered observational studies of any design (cross-sectional, prospective, or retrospective cohort) that evaluated human participants of any age, gender, or race/ethnicity from the general population.
We considered multiple objective measures of SES, such as education, income, occupation, employment status, assets, and composite scores, as well as subjective SES, self-assessed by participants. In the composite category, we also included such variables as access to health insurance or recipiency of public benefits, since they are objective but may relate to more than one core SES measure (income, employment, or assets). In the subjective category, we included those variables that were measured based on participants’ own judgement of their social class (usually relatively to others) or their economic situation (financial difficulties, food security, etc). Proxy measures of SES (neighborhood or residence area deprivation indexes) were included when individual data were not available. For studies examining children or adolescents, parental SES measures (parental education and occupation, household income/assets) were used instead.
We evaluated sleep health on both a behavioral/physiological and a clinical (absence of complaints) basis.28,29 In the first instance, variables were grouped in the following categories: sleep duration, sleep latency, number of awakenings/wake after sleep onset, and sleep efficiency. Sleep timing was not evaluated due to difficulty in defining normal ranges. Variables should be presented numerically and derived either from objective tests, such as wrist actigraphy/accelerometry or polysomnography (PSG), or subjective reports in the form of questionnaires or sleep diaries. Clinical sleep variables were grouped as follows:
(1) insomnia/sleep difficulty, including complaints of difficulty in initiating sleep, difficulty in maintaining sleep, early morning awakening, or nonrestorative sleep, with or without daytime consequences, obtained from validated or nonvalidated questionnaires,
(2) sleep-disordered breathing, including complaints of snoring and sleep apnea symptoms (breathing stops, gasping, etc) from questionnaires or objective measurement of respiratory events during sleep (polygraphy or PSG),
(3) hypersomnia, including measurements of daytime sleepiness/hypersomnolence or long sleep duration, either by questionnaires or by objective tests (actigraphy, PSG, multiple sleep latency test),
(4) abnormal movements/behaviors during sleep, including complaints of restless legs, leg cramps, bruxism, rhythmic movements, parasomnias, nightmares, and enuresis, evaluated by questionnaires or PSG.
A final category was labeled as composite sleep disturbance, which included either composite measures of the above-mentioned physiological or clinical variables, usually in the form of validated scales, or variables that generally measure the overall satisfaction and quality of sleep, self-assessed in questionnaires. Sleep variables could be either continuous or categorical with cut-offs that were already defined in each article. Parental reports of children’s sleep health and sleep problems were also eligible.
Exclusion criteria
Reports were excluded based on the following criteria: (1) they were interventional trials, reviews or meta-analyses, case series or case reports, and not presenting original research; (2) they were in a non-English language; (3) the full text was not accessible; (4) they recruited participants that already presented specific conditions at baseline (namely, pregnant women, shift workers, caregivers, sleep disorders, or other chronic diseases); (5) they did not provide full effects or statistical significance in cases where either SES or sleep were evaluated as covariates or mediators of other comparisons; or (6) they reported univariate associations and unadjusted estimates of the variables of interest. The latter criterion was implemented to avoid biases in the assessment of true relationships.
Data extraction and quality assessment
We extracted the following data from included studies:
(1) study design (based on the SES–sleep analyses and not necessarily on the whole study),
(2) setting, time period of recruitment, participation rate, and sample size justification,
(3) characteristics of participants (numbers, age range, derived population, attrition),
(4) timing of SES and sleep measurement and range of follow-up (for cohort studies),
(5) SES measures (variables, measurement details, levels/categories if grouped),
(6) sleep measures (variables, measurement details/instruments, cut-off thresholds if categorical, assessors),
(7) covariates included in the analyses that tested the SES–sleep association,
(8) main results (statistical significance and direction of the association between SES and sleep),
(9) significant interaction/mediation effects of the SES–sleep association by other variables.
We used the National Heart, Lung, and Blood Institute’s Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies30 to rate the quality of included studies. SES was considered the exposure and sleep measures the outcome variable, respectively. Rating of the exposure and outcome assessment in each article was influenced by objectivity; studies employing subjective or area SES measures, self-reported physiological sleep parameters, or nondiagnostic symptoms/signs of sleep disorders (according to the International Classification of Sleep Disorders, third edition or the Diagnostic and Statistical Manual of Mental Disorders, fifth edition diagnostic criteria) were downgraded. Blinding of outcome assessors was nonapplicable in self-reported outcomes. Age, gender, and race were considered essential confounders in statistical analyses, while body mass index or obesity were also required in studies assessing sleep-disordered breathing. Regarding overall quality rating, we calculated the proportion of positive rating on the sum of applicable criteria. Studies with < 50% positive rating were judged as poor quality, ≥ 65% as good quality, and the rest as fair quality.
Effect measures and synthesis of results
Due to the high heterogeneity in the measurement and categorization of SES and sleep indices between studies, a meta-analysis was deemed nonfeasible, and outcomes are presented narratively with emphasis on direction rather than magnitude of effects. For each comparison between a SES and a sleep indicator in each study, a vote counting method31 was applied based on the direction of the effect of the SES predictor on the sleep outcome. The direction effect could be classified as expected, conflicting/unclear, or opposite, in respect to the expectance that lower SES predicts poorer sleep outcomes, which was guided by the widely acknowledged conceptual framework of the SES–health gradient.32 When studies presented analyses with multiple levels of covariate adjustment, direction effect was extracted from the least adjusted model (including age, gender, and race) to minimize heterogeneity. When studies reported data for more than one sleep outcome in a specific outcome category and the direction of effects was not similar in at least 70% of them, the overall direction was categorized as conflicting/unclear. The same classification was used when the statistical tests for the SES–sleep association literally showed absence of an effect (eg, P values > 0.9). In studies where outcome data were only presented stratified according to participants’ characteristics or recruiting sites, we summarized them, using fixed or random effects estimates, respectively, before deciding on the effect direction. When both continuous and categorical sleep outcome data were presented for the same outcome category, we preferred the categorical ones, while when outcome data were reported for more than two exposure SES levels without a clear trend in the effect direction we based the voting only on the association between the lowest and highest SES category.
Effect direction plots were drawn for each SES predictor to visualize the direction of the associations with each outcome category. In these plots, information presented for each study include its design, its quality rating, its sample size, and the direction effect vote for the applicable outcome categories.33 A binomial test was used to synthesize the direction of effects for each SES–sleep association. Studies that have not tested the association of interest or showed conflicting/unclear effect direction were excluded from the calculation. For each comparison, we present proportion of studies with expected direction of effect, the corresponding 95% Jeffreys confidence interval (CI) of the proportion, and the two-sided P value at the alpha level of 0.05 from the binomial test. A sensitivity analysis was undertaken, eliminating studies of poor quality. We also sought to investigate if the proportion of expected effects was influenced by certain study characteristics, such as the outcome measurement (only for the behavioral/physiological sleep outcomes) or the number of covariates included in the respective models from where the effect directions were drawn. We did this by fitting binomial regression models with effect direction as the dependent variable (1 = expected effect, 0 = opposite effect) and outcome measurement (objective vs subjective) or covariate amount (on continuous scale) as independent variables. A two-sided P value of < 0.05 indicated the statistical significance of the association.
Significant mediators of the association between SES and sleep are discussed separately with the aim to propose a theoretical model explaining socioeconomic inequalities in sleep health, while interaction effects between SES and demographic characteristics (age, gender, and race) in predicting sleep measures were also recognized and put under consideration. Mediators were identified either by hierarchical regression analysis (entering in the last step and reducing the effect of the main predictors) or by mediation analysis (showing significant indirect effects accounting for the variance between dependent and independent variables). Due to the limited number of studies that have tested these effects, the results are only presented narratively and were not synthesized.
RESULTS
Study selection
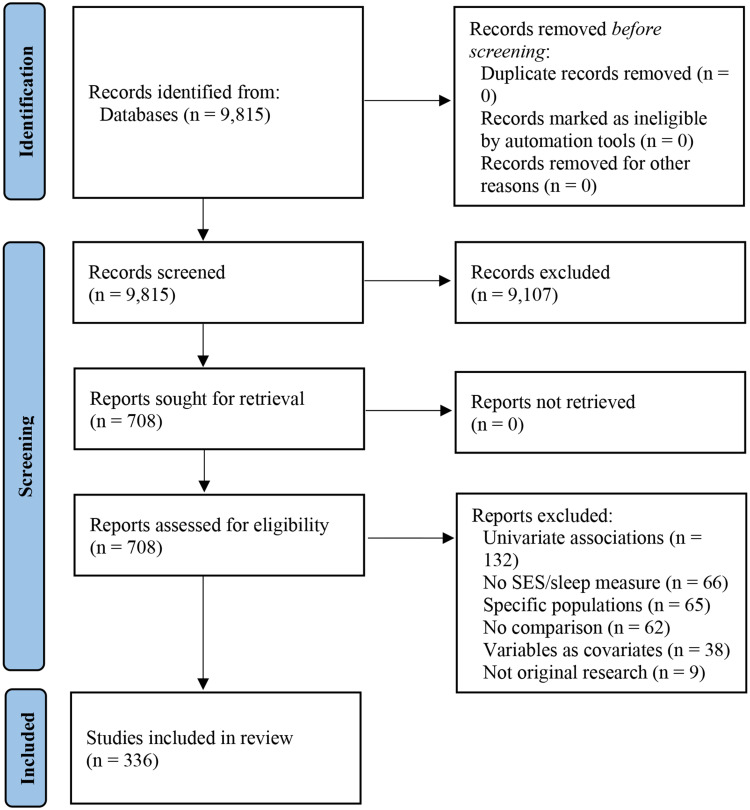
We identified a total of 9,815 articles. After title and abstract screening, we were able to exclude 9,107 reports for clearly not meeting our inclusion criteria and evaluated 708 full texts for eligibility. At this step, we further excluded 372 articles for reporting univariate associations between variables of interest (n = 132), not evaluating either of the key variables (n = 66), including samples from specific populations (n = 65), not presenting any comparison between variables of interest (n = 62), assessing variables of interest as covariates (n = 38), and not presenting original research or including duplicate samples (n = 9), and ended up with 336 studies13,16,18,19,23–27,34–360 for inclusion (Figure 1).
Figure 1. Review flow diagram.
Characteristics of included studies
Most studies were published between the years 2010 and 2019 (n = 247). Considering specific SES–sleep analyses for assessment of study design, 28 studies had a prospective cohort design (median follow-up: 5 years, range: 1–34 years), 2 had a retrospective cohort design (median follow-up: 3 years, range: 1–5 years) and the rest were cross-sectional (n = 306). Study settings were mostly in Asian (n = 105) and North American (n = 103) countries, followed by Europe (n = 71), South America (n = 21), Oceania (n = 21), and Africa (n = 7), while 8 reports came from countries of different continents. Ninety studies evaluated children and adolescents. Twenty-eight studies focused only on women and 4 on men. Six studies enrolled only ethnic minorities, while participants were employees in 17 and students in 7 studies, respectively.
The most frequent SES indicator was educational attainment (n = 246), followed by income (n = 142), employment status (n = 110), occupational class (n = 40), assets (n = 32), composite or other objective measures (n = 36), and subjective ratings (n = 36).
The number of studies that evaluated each sleep outcome was 139 for sleep duration, 22 for sleep latency, 18 for awakenings/wake after sleep onset, 21 for sleep efficiency, 94 for insomnia, 27 for sleep-disordered breathing, 64 for hypersomnia, 19 for abnormal movements/behaviors, and 90 for the composite sleep disturbance category. For objective evaluation of sleep, studies employed wrist actigraphy/accelerometry (n = 25) or PSG (n = 9). The most frequently used validated questionnaires for subjective sleep reports were the Pittsburgh Sleep Quality Index (n = 41), the Epworth Sleepiness Scale (n = 14), the Children’s Sleep Habits Questionnaire (n = 8), the Insomnia Severity Index (n = 7), the Athens Insomnia Scale (n = 4), and the Berlin Questionnaire (n = 4). All articles of this review are detailed in Table S1 (2.4MB, pdf) in the supplemental material.
Quality rating
Most articles were rated of fair overall quality (n = 234), followed by 54 of poor and 48 of good quality. All reports (n = 336) clearly stated their objectives and most of them (n = 330) recruited participants from the same population with uniform eligibility criteria. The population under assessment was clearly defined in 297 articles (88.4%) and the participation rate exceeded 50% in 229 studies (71.8% of applicable). Only 35 studies (10.4%) provided sample size justification, 18 studies (5.4%) measured the exposure prior to outcome, and 27 studies (8.0%) allowed sufficient time for the exposure to have an impact on outcome. Most reports assessed multiple levels of exposure (n = 238, 70.8%), with objective measures (n = 317, 94.3%); however only 13 articles (3.9%) mentioned repeated exposure measurements. Sixty-six studies (19.6%) used objective outcome measures and 54.5% of applicable reports (n = 18) referred to blinding of outcome assessors. From 28 prospective studies, only 7 (25.0%) were able to maintain a follow-up rate over 80%. Finally, 90.2% of reports (n = 303) adjusted for key confounding variables in their statistical analyses (Table S2 (2.4MB, pdf) ).
Synthesis of results
Direction of effects
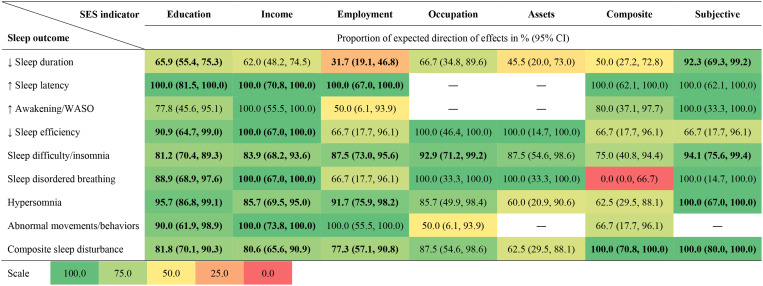
Proportion and 95% CIs of reports with expected SES–sleep associations are presented in Figure 2 in the form of a heat map. In the heat map cells, green shading indicates a high proportion of expected directions of effects, yellow shading represents an equal proportion of expected and opposite directions of effects, and red shading corresponds to a high proportion of opposite directions of effects. The complete effect direction plots for all comparisons are presented in Figure S1 (2.4MB, pdf) , Figure S2 (2.4MB, pdf) , Figure S3 (2.4MB, pdf) , Figure S4 (2.4MB, pdf) , Figure S5 (2.4MB, pdf) , Figure S6 (2.4MB, pdf) , and Figure S7 (2.4MB, pdf) .
Figure 2. Heat map presentation for the synthesis of effects direction for the associations between each socioeconomic indicator and sleep outcome category.
Shades of green indicate a high proportion of expected direction of effects, shades of yellow an equal proportion of expected and opposite direction of effects, and shades of red a high proportion of opposite direction of effects. Values in bold indicate statistically significant proportions (P < .05) from the binomial test. CI = confidence interval, SES = socioeconomic status, WASO = wake after sleep onset.
Regarding the behavioral/physiological sleep outcomes, the direction of effects on sleep duration was inconsistent for the different SES indicators. The estimated effects of education, income, occupation, and subjective SES were on the expected direction (range of proportions: 62.0–92.3%), while the estimated effects of employment status, assets, and composite SES were in the opposite direction or were unclear (range of proportions: 31.7–50.0%). The significance tests showed that short sleep duration was associated with low levels of education (P = .005), low subjective SES (P = .003), and being employed (P = .029). On the other hand, the direction of effects on measures of sleep continuity was consistently expected (proportions: 100.0% for sleep latency, 50.0–100.0% for awakenings/wake after sleep onset, and 66.7–100.0% for sleep efficiency). The significance tests revealed that increased sleep latency was associated with low levels of education (P < .001) or income (P = .016) and with unemployment (P = .031), while reduced sleep efficiency was related to low levels of education (P = .012) or income (P = .031).
Regarding the clinical sleep outcomes, estimated effects of SES on sleep were in the expected direction for insomnia (75.0–94.1%), hypersomnia (60.0–100.0%), abnormal movements/behaviors (50.0–100.0%), and composite sleep disturbances (62.5–100.0%). The same was true for sleep-disordered breathing (66.7–100.0%), except for its association with composite SES measures (0.0% of expected effects). Binomial probabilities were statistically significant for the effects of low educational attainment and low levels of income in all categories of sleep complaints and also for the effects of unemployment (P < .001), low occupational class (P = .002), and low subjective SES (P < .001) on insomnia, the effects of unemployment (P < .001) and low subjective SES (P = .031) on hypersomnia, and the effects of unemployment (P = .017), low composite SES (P = .016), and low subjective SES (P = .001) on composite sleep disturbance.
Eliminating the studies that were rated at poor quality did not change the summary direction of effects in any of the SES–sleep associations. However, the effect of employment status on sleep duration in favor of unemployment was no longer significant (binomial proportion of expected direction 34.2% [95% CI: 20.7%, 50.0%], P = .074). The method of outcome measurement had a significant impact only on the relationship between education and sleep duration. Studies that employed subjective sleep duration measures (binomial proportion of expected direction 70.3% [95% CI: 59.2%, 79.8%], P = .001) had 4 times higher probability (odds ratio 4.14 [95% CI: 1.10, 15.57], P = .036) of presenting effects on the expected direction compared to studies using objective ones (binomial proportion of expected direction 36.4% [95% CI: 13.7%, 65.2%], P = .549). The number of covariates tested in each study did not have a significant influence on the effect directions for any of the SES–sleep associations.
Interaction and mediation effects
Gender (n = 11) and race/ethnicity (n = 10) were the most common variables significantly moderating the association between SES and sleep outcomes. The interaction effect, however, was not in the same direction in all studies. Four studies showed nonsignificant results in one gender compared to the other (2137,303 in men and 261,318 in women), 3 articles45,128,307 reported worse outcome for men compared to women for each respective SES level, and 2 reports77,138 showed an inverse SES/sleep association in women compared to men. Regarding race, 4 studies92,124,125,176 found poorer and 2 studies136,294 better sleep in low-SES ethnic minorities compared to Whites for each respective SES level, while 2 reports212,215 showed opposite effects of SES on sleep measures in racial groups opposed to Caucasian populations. Advancing age predicted poorer sleep in low- as opposed to high-SES individuals in 3 studies,13,84,307 while the opposite effect was also demonstrated in 1 study.307 A 3-way interaction between race, gender, and SES was found in 1 study,247 where African American men had less pronounced and nonsignificant impacts of SES on sleep. Finally, 1 study84 reported a significant 4-way interaction between race, gender, age, and SES, with older minority women of low SES exerting significantly more negative effects on sleep.
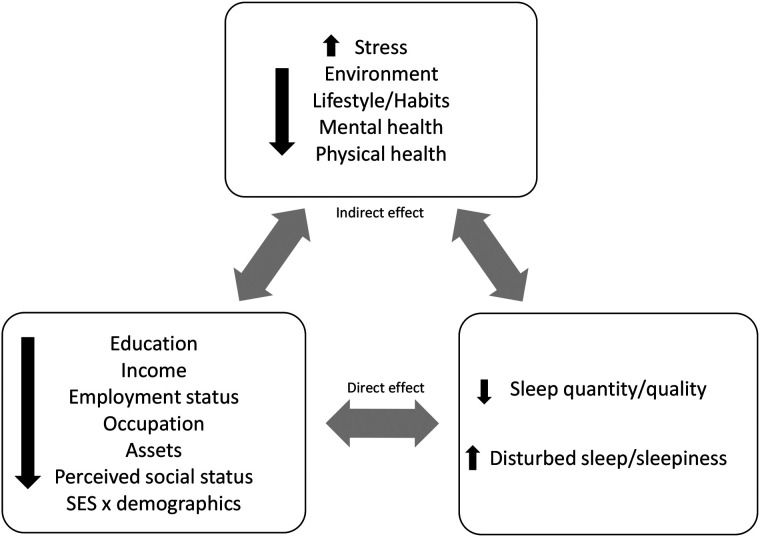
Behavioral, environmental, and sleep hygiene factors (smoking, alcohol consumption, physical activity, home environment, family status, screen time) were the most frequently encountered mediators (n = 24), while psychological/mental (anxiety, depression, worries) and physical health factors (obesity, presence of chronic illnesses, perceived health) each accounted for attenuation effects in 22 studies. Work-related characteristics (working hours, job demands, support, reward, or commitment) and perceived levels of stress showed mediation effects in 8 and 6 studies, respectively. All the above associations worked in the same way: low SES was linked to adverse and unfavorable environmental, lifestyle, physical, and psychological outcomes, which in turn were associated with poorer sleep.
DISCUSSION
Summary of findings
We aimed to synthesize the evidence from the existing literature on the association between SES and sleep health. Our findings support the hypothesis that lower SES is linked to poorer outcomes for nearly all the domains of sleep health evaluated, both in adults and children/adolescents. The association between SES and sleep duration is the least clear and requires further research. With the exception of subjective SES, which showed a very high proportion of expected directions of effects on sleep duration, the other more objective SES indicators presented only modest proportions of expected effects, ranging from 31.7 to 66.7%. The proportion of expected effects was statistically significant for the education–sleep duration relation, but in the subset of studies using objective sleep duration measurements (actigraphy or PSG) the effect was in the opposite direction. The only statistically significant effect in the opposite direction than expected is the association between sleep duration and employment status, where employed individuals exhibited higher odds of having short sleep duration. A very logical explanation is that employment is usually linked to increased work commitments early in the morning, forcing employed individuals to curtail their sleep schedule. The fact that unemployed individuals usually have lower levels of education, income, or assets than employed ones, but appear to sleep longer than them, could also explain the nonsignificant effects of the other SES indicators on sleep duration. Another possible reason behind this opposite effect is that unemployed individuals may also represent economically inactive populations, such as housewives or students, whose SES could vary depending on the other members of the household. Subjective SES ratings may better reflect the social structure and class, especially in developing societies or minorities, where individual SES could differ from household SES or neighborhood/community SES. In pediatric populations, children from high-SES families may spend less time sleeping at the expense of screen-playing time, academic commitments, or extracurricular activities. Despite these inconsistencies, there was evidence for a SES gradient in measures of sleep continuity and efficiency, meaning that low-SES individuals spend more time in bed to obtain the same amount of sleep as high-SES individuals. Finally, the only SES predictor that failed to reach statistical significance in its direction effect on sleep outcomes was assets, possibly owing to the small number of studies that employed this measure.
Correlation with previous literature
Our results are in accordance with previous reviews examining the impact of SES on a variety of health habits (diet,361 physical activity,362 smoking,363 or alcohol use364), biomarkers (blood pressure,365 obesity,366 cortisol secretion and allostatic load367), and diseases (cardiovascular diseases,368 diabetes mellitus,369 mental health disorders370), while chronic exposure to low SES from childhood leads to higher risk for overall and cause-specific mortality.371 This review adds to the growing body of literature about the detrimental effects of low social position on health and quality of life and is highly relevant for health care providers and policy makers alike; the former must acknowledge SES as an independent risk factor for poor sleep health and the latter need to implement targeted screening programs and accessible interventions tailored to these populations.
Sleep disparities in the context of socioeconomic disadvantage
We further tried to highlight the mechanisms responsible for the observed relations by identifying factors that mediate or attenuate the association between SES and sleep. Figure 3 depicts the theoretical model for the observed complex interactions between SES and sleep. Environmental, physical, and psychological health factors are possibly located in the pathway that links low SES and poor sleep. Our findings are in agreement with the previously described social-ecological model of sleep health,12 according to which sleep is influenced by individual-level factors (behavior, psychology, health), but these are embedded in the context of social factors (work, neighborhood), and the latter are also embedded within the context of societal factors (environment, technology). This model reveals the complexity of sleep, since it is conceptualized as the result of different processes acting on macrolevel (sociopolitical context) and microlevel (local living conditions). At the individual level, low-SES individuals are more prone to unhealthy behaviors, including those that relate to sleep health, due to being less educated, having higher stress levels in the context of financial or employment insecurity, and having limited access to health care resources and programs.372 As a result, their physical and mental health is worse than that of individuals of higher SES strata, and that is also reflected in their sleep.373 At the social and societal level, working long hours374 and in unhealthy environments,375 engaging in shift work,376 and living in crowded houses377 or in noisy, unpleasant, and dangerous neighborhoods14,378 might adversely impact sleep, while the influence of cultural and ethnic/racial beliefs and attitudes about sleep and health in general could be stronger in socioeconomically deprived individuals.379
Figure 3. Proposed pathways linking socioeconomic status and sleep outcomes.
The bidirectional arrows imply a possible reciprocal relationship between the two variables.
On the other hand, the effect of nonmodifiable characteristics, such as gender and race, seems conflicting between studies and warrants more attention in future research designs. Regarding ethnicity, several studies have shown that, particularly in developed countries, African American, Hispanic, and Latin American communities report more difficulty falling asleep, have poorer sleep quality, and sleep less than their Caucasian counterparts.17,24,146,215,234,236,274,294 There appears to be an association between the “social stress” experienced by people from certain ethnic groups and the development of sleep disturbances among their members.
Limitations
Limitations of this review also exist. The variety of SES measures and the different levels for each SES indicator in the included studies led to substantial heterogeneity and prevented the performance of a meta-analysis. Although vote counting is an acceptable synthesis method, it is limited by the fact that each study contributes equally in the synthesis, regardless of the size of its sample. Only the PubMed/MEDLINE database was searched, which could result in some low-impact manuscripts’ being missed. Several studies assessed sleep outcomes using a single question, an approach that may not capture the multidimensionality and day-to-day variability of sleep. Use of validated composite SES scores, validated sleep questionnaires, sleep diaries, and objective sleep assessments (actigraphy or PSG) is strongly encouraged in future research. Moreover, the cross-sectional design most studies employed cannot be safely used to infer causality. The establishment of cohorts free of sleep disorders at baseline and their prospective follow-up for long time periods across multiple trajectories of SES will provide more reliable evidence.
CONCLUSIONS
There exists a social gradient in sleep health in individuals both in developed and developing societies and across all ages. Socioeconomic deprivation is associated with poorer sleep continuity/efficiency, higher frequency of sleep complaints and daytime sleepiness, and lower overall sleep satisfaction, while the effect of social position on sleep duration varies depending on the way SES is assessed. Individual- and social-level factors that influence this relationship are behavioral traits, physical and mental health problems, work-related issues, and environmental characteristics. Future research should identify the combined effect of psychological factors, stress, and lifestyle on the development and progression of sleep disturbances, so that behavioral and pharmacological interventions can be implemented to reduce the incidence of sleep disturbances.
ACKNOWLEDGMENTS
The authors acknowledge Dr. Aarti Jagannath from the University of Oxford for her assistance in manuscript proof editing and Dr. Fabricio Ferreira de Oliveira from the Universidade Federal de São Paulo for his valuable comments and instructions after reviewing a previous version of the manuscript.
ABBREVIATIONS
- CI
confidence interval
- PSG
polysomnography
- SES
socioeconomic status
DISCLOSURE STATEMENT
All authors have seen and approved the manuscript. Work for this study was performed at the Army Share Fund Hospital, Greece and the Redavi Institute, Canada. The authors report no conflicts of interest.
REFERENCES
- 1. Tobaldini E , Costantino G , Solbiati M , et al . Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases . Neurosci Biobehav Rev. 2017. ; 74 ( Pt B ): 321 – 329 . [DOI] [PubMed] [Google Scholar]
- 2. Chahine LM , Amara AW , Videnovic A . A systematic review of the literature on disorders of sleep and wakefulness in Parkinson’s disease from 2005 to 2015 . Sleep Med Rev. 2017. ; 35 : 33 – 50 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Itani O , Jike M , Watanabe N , Kaneita Y . Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression . Sleep Med. 2017. ; 32 : 246 – 256 . [DOI] [PubMed] [Google Scholar]
- 4. Kolla BP , He JP , Mansukhani MP , Frye MA , Merikangas K . Excessive sleepiness and associated symptoms in the U.S. adult population: prevalence, correlates, and comorbidity . Sleep Health. 2020. ; 6 ( 1 ): 79 – 87 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Papadopoulos D , Sosso FAE , Khoury T , Surani SR . Sleep disturbances are mediators between socioeconomic status and health: a scoping review . Int J Ment Health Addict. 2020. ; 20 ( 1 ): 480 – 504 . [Google Scholar]
- 6. Lo Martire V , Caruso D , Palagini L , Zoccoli G , Bastianini S . Stress & sleep: a relationship lasting a lifetime . Neurosci Biobehav Rev. 2020. ; 117 : 65 – 77 . [DOI] [PubMed] [Google Scholar]
- 7. Ohayon M , Wickwire EM , Hirshkowitz M , et al . National Sleep Foundation’s sleep quality recommendations: first report . Sleep Health. 2017. ; 3 ( 1 ): 6 – 19 . [DOI] [PubMed] [Google Scholar]
- 8. Hirshkowitz M , Whiton K , Albert SM , et al . National Sleep Foundation’s sleep time duration recommendations: methodology and results summary . Sleep Health. 2015. ; 1 ( 1 ): 40 – 43 . [DOI] [PubMed] [Google Scholar]
- 9. Phelan JC , Link BG , Tehranifar P . Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications . J Health Soc Behav. 2010. ; 51 ( Suppl ): S28 – S40 . [DOI] [PubMed] [Google Scholar]
- 10. Wong K , Chan AHS , Ngan SC . The effect of long working hours and overtime on occupational health: a meta-analysis of evidence from 1998 to 2018 . Int J Environ Res Public Health. 2019. ; 16 ( 12 ): E2102 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rodriguez JM , Karlamangla AS , Gruenewald TL , Miller-Martinez D , Merkin SS , Seeman TE . Social stratification and allostatic load: shapes of health differences in the MIDUS study in the United States . J Biosoc Sci. 2019. ; 51 ( 5 ): 627 – 644 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Grandner MA . Social-Ecological Model of Sleep Health . In: Grandner MA , ed. Sleep and Health. New York: : Academic Press; ; 2019. : 45 – 53 . [Google Scholar]
- 13. Vermeiren AP , Willeboordse M , Oosterhoff M , Bartelink N , Muris P , Bosma H . Socioeconomic multi-domain health inequalities in Dutch primary school children . Eur J Public Health. 2018. ; 28 ( 4 ): 610 – 616 . [DOI] [PubMed] [Google Scholar]
- 14. Ribeiro AI , Amaro J , Lisi C , Fraga S . Neighborhood socioeconomic deprivation and allostatic load: a scoping review . Int J Environ Res Public Health. 2018. ; 15 ( 6 ): E1092 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Braveman PA , Cubbin C , Egerter S , Williams DR , Pamuk E . Socioeconomic disparities in health in the United States: what the patterns tell us . Am J Public Health. 2010. ; 100 ( Suppl 1 ): S186 – S196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Counts CJ , Grubin FC , John-Henderson NA . Childhood socioeconomic status and risk in early family environments: predictors of global sleep quality in college students . Sleep Health. 2018. ; 4 ( 3 ): 301 – 306 . [DOI] [PubMed] [Google Scholar]
- 17. Hoggard LS , Hill LK . Examining how racial discrimination impacts sleep quality in African Americans: is perseveration the answer? Behav Sleep Med. 2018. ; 16 ( 5 ): 471 – 481 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Doane LD , Breitenstein RS , Beekman C , Clifford S , Smith TJ , Lemery-Chalfant K . Early life socioeconomic disparities in children’s sleep: the mediating role of the current home environment . J Youth Adolesc. 2019. ; 48 ( 1 ): 56 – 70 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Petrovic D , Haba-Rubio J , Carmeli C , Vollenweider P , Heinzer R , Stringhini S . Social inequalities in sleep-disordered breathing: evidence from the CoLaus|HypnoLaus study . J Sleep Res. 2019. ; 28 ( 5 ): e12799 . [DOI] [PubMed] [Google Scholar]
- 20. Etindele-Sosso FA . Insomnia, excessive daytime sleepiness, anxiety, depression and socioeconomic status among customer service employees in Canada . Sleep Sci. 2020. ; 13 ( 1 ): 54 – 64 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mokarami H , Gharibi V , Kalteh HO , Faraji Kujerdi M , Kazemi R . Multiple environmental and psychosocial work risk factors and sleep disturbances . Int Arch Occup Environ Health. 2020. ; 93 ( 5 ): 623 – 633 . [DOI] [PubMed] [Google Scholar]
- 22. Mai QD , Hill TD , Vila-Henninger L , Grandner MA . Employment insecurity and sleep disturbance: evidence from 31 European countries . J Sleep Res. 2019. ; 28 ( 1 ): e12763 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bøe T , Hysing M , Stormark KM , Lundervold AJ , Sivertsen B . Sleep problems as a mediator of the association between parental education levels, perceived family economy and poor mental health in children . J Psychosom Res. 2012. ; 73 ( 6 ): 430 – 436 . [DOI] [PubMed] [Google Scholar]
- 24. Biggs SN , Lushington K , James Martin A , van den Heuvel C , Declan Kennedy J . Gender, socioeconomic, and ethnic differences in sleep patterns in school-aged children . Sleep Med. 2013. ; 14 ( 12 ): 1304 – 1309 . [DOI] [PubMed] [Google Scholar]
- 25. Peltzer K , Pengpid S . Nocturnal sleep problems among university students from 26 countries . Sleep Breath. 2015. ; 19 ( 2 ): 499 – 508 . [DOI] [PubMed] [Google Scholar]
- 26. Perlus JG , O’Brien F , Haynie DL , Simons-Morton BG . Adolescent sleep insufficiency one year after high school . J Adolesc. 2018. ; 68 ( 1 ): 165 – 170 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Peltzer K , Pengpid S . Self-reported sleep duration and its correlates with sociodemographics, health behaviours, poor mental health, and chronic conditions in rural persons 40 years and older in South Africa . Int J Environ Res Public Health. 2018. ; 15 ( 7 ): 1357 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Buysse DJ . Sleep health: can we define it? Does it matter? Sleep. 2014. ; 37 ( 1 ): 9 – 17 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Knutson KL , Phelan J , Paskow MJ , et al . The National Sleep Foundation’s Sleep Health Index . Sleep Health. 2017. ; 3 ( 4 ): 234 – 240 . [DOI] [PubMed] [Google Scholar]
- 30. National Heart, Blood, and Lung Institute . Study quality assessment tools. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools . Accessed June 18, 2020. .
- 31. McKenzie JE , Brennan SE . Synthesizing and Presenting Findings Using Other Methods . In: Higgins JPT Thomas J , Chandler J , Cumpston M , Li T , Page MJ , Welch VA , eds. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3. London: : Cochrane; ; 2022. . [Google Scholar]
- 32. Galama TJ , van Kippersluis H . A theory of socio-economic disparities in health over the life cycle . Econ J (Lond). 2019. ; 129 ( 617 ): 338 – 374 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Boon MH , Thomson H . The effect direction plot revisited: application of the 2019 Cochrane Handbook guidance on alternative synthesis methods . Res Synth Methods. 2021. ; 12 ( 1 ): 29 – 33 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Habte-Gabr E , Wallace RB , Colsher PL , Hulbert JR , White LR , Smith IM . Sleep patterns in rural elders: demographic, health, and psychobehavioral correlates . J Clin Epidemiol. 1991. ; 44 ( 1 ): 5 – 13 . [DOI] [PubMed] [Google Scholar]
- 35. Moffitt PF , Kalucy EC , Kalucy RS , Baum FE , Cooke RD . Sleep difficulties, pain and other correlates . J Intern Med. 1991. ; 230 ( 3 ): 245 – 249 . [DOI] [PubMed] [Google Scholar]
- 36. Weyerer S , Dilling H . Prevalence and treatment of insomnia in the community: results from the Upper Bavarian Field Study . Sleep. 1991. ; 14 ( 5 ): 392 – 398 . [PubMed] [Google Scholar]
- 37. Hopton JL , Howie JG , Porter AM . Social indicators of health needs for general practice: a simpler approach . Br J Gen Pract . 1992. ; 42 ( 359 ): 236 – 240 . [PMC free article] [PubMed] [Google Scholar]
- 38. Kim KH , Shin HR , Nakama H . Health consciousness in relation to education in Korea–focusing on seven preventable health risk factors . Asia Pac J Public Health. 1994. ; 7 ( 1 ): 3 – 9 . [DOI] [PubMed] [Google Scholar]
- 39. Blazer DG , Hays JC , Foley DJ . Sleep complaints in older adults: a racial comparison . J Gerontol A Biol Sci Med Sci. 1995. ; 50 ( 5 ): M280 – M284 . [DOI] [PubMed] [Google Scholar]
- 40. Geroldi C , Frisoni GB , Rozzini R , De Leo D , Trabucchi M . Principal lifetime occupation and sleep quality in the elderly . Gerontology. 1996. ; 42 ( 3 ): 163 – 169 . [DOI] [PubMed] [Google Scholar]
- 41. Ohayon M . Epidemiological study on insomnia in the general population . Sleep. 1996. 19 ( Suppl 3 ): S7 – S15 . [DOI] [PubMed] [Google Scholar]
- 42. Rásky E , Stronegger WJ , Freidl W . Employment status and its health-related effects in rural Styria, Austria . Prev Med. 1996. ; 25 ( 6 ): 757 – 763 . [DOI] [PubMed] [Google Scholar]
- 43. Breslau N , Roth T , Rosenthal L , Andreski P . Daytime sleepiness: an epidemiological study of young adults . Am J Public Health. 1997. ; 87 ( 10 ): 1649 – 1653 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Fabsitz RR , Sholinsky P , Goldberg J . Correlates of sleep problems among men: the Vietnam Era Twin Registry . J Sleep Res. 1997. ; 6 ( 1 ): 50 – 56 . [DOI] [PubMed] [Google Scholar]
- 45. Rona RJ , Li L , Chinn S . Determinants of nocturnal enuresis in England and Scotland in the ’90s . Dev Med Child Neurol. 1997. ; 39 ( 10 ): 677 – 681 . [DOI] [PubMed] [Google Scholar]
- 46. Schechtman KB , Kutner NG , Wallace RB , Buchner DM , Ory MG . Gender, self-reported depressive symptoms, and sleep disturbance among older community-dwelling persons. FICSIT group. Frailty and injuries: cooperative studies of intervention techniques . J Psychosom Res. 1997. ; 43 ( 5 ): 513 – 527 . [DOI] [PubMed] [Google Scholar]
- 47. Rona RJ , Li L , Gulliford MC , Chinn S . Disturbed sleep: effects of sociocultural factors and illness . Arch Dis Child. 1998. ; 78 ( 1 ): 20 – 25 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Talvi AI , Järvisalo JO , Knuts LR , Kaitaniemi PR . Life-style related health promotion needs in oil refinery employees . Occup Med (Lond). 1998. ; 48 ( 1 ): 45 – 53 . [DOI] [PubMed] [Google Scholar]
- 49. Hall M , Bromberger J , Matthews K . Socioeconomic status as a correlate of sleep in African-American and Caucasian women . Ann N Y Acad Sci. 1999. ; 896 ( 1 ): 427 – 430 . [DOI] [PubMed] [Google Scholar]
- 50. Roberts RE , Shema SJ , Kaplan GA . Prospective data on sleep complaints and associated risk factors in an older cohort . Psychosom Med. 1999. ; 61 ( 2 ): 188 – 196 . [DOI] [PubMed] [Google Scholar]
- 51. Adler NE , Epel ES , Castellazzo G , Ickovics JR . Relationship of subjective and objective social status with psychological and physiological functioning: preliminary data in healthy white women . Health Psychol . 2000. ; 19 ( 6 ): 586 – 592 . [DOI] [PubMed] [Google Scholar]
- 52. Ito Y , Tamakoshi A , Yamaki K , et al . Sleep disturbance and its correlates among elderly Japanese . Arch Gerontol Geriatr. 2000. ; 30 ( 2 ): 85 – 100 . [DOI] [PubMed] [Google Scholar]
- 53. Phillips B , Young T , Finn L , Asher K , Hening WA , Purvis C . Epidemiology of restless legs symptoms in adults . Arch Intern Med. 2000. ; 160 ( 14 ): 2137 – 2141 . [DOI] [PubMed] [Google Scholar]
- 54. Sadeh A , Raviv A , Gruber R . Sleep patterns and sleep disruptions in school-age children . Dev Psychol. 2000. ; 36 ( 3 ): 291 – 301 . [DOI] [PubMed] [Google Scholar]
- 55. Gallant MP , Dorn GP . Gender and race differences in the predictors of daily health practices among older adults . Health Educ Res. 2001. ; 16 ( 1 ): 21 – 31 . [DOI] [PubMed] [Google Scholar]
- 56. Hublin C , Kaprio J , Partinen M , Koskenvuo M . Insufficient sleep–a population-based study in adults . Sleep. 2001. ; 24 ( 4 ): 392 – 400 . [DOI] [PubMed] [Google Scholar]
- 57. Ohida T , Kamal AM , Uchiyama M , et al . The influence of lifestyle and health status factors on sleep loss among the Japanese general population . Sleep. 2001. ; 24 ( 3 ): 333 – 338 . [DOI] [PubMed] [Google Scholar]
- 58. Pallesen S , Nordhus IH , Nielsen GH , et al . Prevalence of insomnia in the adult Norwegian population . Sleep. 2001. ; 24 ( 7 ): 771 – 779 . [PubMed] [Google Scholar]
- 59. Sutton DA , Moldofsky H , Badley EM . Insomnia and health problems in Canadians . Sleep. 2001. ; 24 ( 6 ): 665 – 670 . [DOI] [PubMed] [Google Scholar]
- 60. Akerstedt T , Knutsson A , Westerholm P , Theorell T , Alfredsson L , Kecklund G . Sleep disturbances, work stress and work hours: a cross-sectional study . J Psychosom Res. 2002. ; 53 ( 3 ): 741 – 748 . [DOI] [PubMed] [Google Scholar]
- 61. Li RH , Wing YK , Ho SC , Fong SY . Gender differences in insomnia–a study in the Hong Kong Chinese population . J Psychosom Res. 2002. ; 53 ( 1 ): 601 – 609 . [DOI] [PubMed] [Google Scholar]
- 62. Moore PJ , Adler NE , Williams DR , Jackson JS . Socioeconomic status and health: the role of sleep . Psychosom Med. 2002. ; 64 ( 2 ): 337 – 344 . [DOI] [PubMed] [Google Scholar]
- 63. Ohayon MM , Hong SC . Prevalence of insomnia and associated factors in South Korea . J Psychosom Res. 2002. ; 53 ( 1 ): 593 – 600 . [DOI] [PubMed] [Google Scholar]
- 64. Rocha FL , Guerra HL , Lima-Costa MF . Prevalence of insomnia and associated socio-demographic factors in a Brazilian community: the Bambuí study . Sleep Med. 2002. ; 3 ( 2 ): 121 – 126 . [DOI] [PubMed] [Google Scholar]
- 65. Chervin RD , Clarke DF , Huffman JL , et al . School performance, race, and other correlates of sleep-disordered breathing in children . Sleep Med. 2003. ; 4 ( 1 ): 21 – 27 . [DOI] [PubMed] [Google Scholar]
- 66. Doi Y , Minowa M . Gender differences in excessive daytime sleepiness among Japanese workers . Soc Sci Med. 2003. ; 56 ( 4 ): 883 – 894 . [DOI] [PubMed] [Google Scholar]
- 67. Doi Y , Minowa M , Tango T . Impact and correlates of poor sleep quality in Japanese white-collar employees . Sleep. 2003. ; 26 ( 4 ): 467 – 471 . [DOI] [PubMed] [Google Scholar]
- 68. Kravitz HM , Ganz PA , Bromberger J , Powell LH , Sutton-Tyrrell K , Meyer PM . Sleep difficulty in women at midlife: a community survey of sleep and the menopausal transition . Menopause. 2003. ; 10 ( 1 ): 19 – 28 . [DOI] [PubMed] [Google Scholar]
- 69. Larsson L-G , Lindberg A , Franklin KA , Lundbäck B . Gender differences in symptoms related to sleep apnea in a general population and in relation to referral to sleep clinic . Chest. 2003. ; 124 ( 1 ): 204 – 211 . [DOI] [PubMed] [Google Scholar]
- 70. Hara C , Lopes Rocha F , Lima-Costa MF . Prevalence of excessive daytime sleepiness and associated factors in a Brazilian community: the Bambuí study . Sleep Med. 2004. ; 5 ( 1 ): 31 – 36 . [DOI] [PubMed] [Google Scholar]
- 71. Paine SJ , Gander PH , Harris R , Reid P . Who reports insomnia? Relationships with age, sex, ethnicity, and socioeconomic deprivation . Sleep. 2004. ; 27 ( 6 ): 1163 – 1169 . [DOI] [PubMed] [Google Scholar]
- 72. Roberts RE , Lee ES , Hemandez M , Solari AC . Symptoms of insomnia among adolescents in the lower Rio Grande Valley of Texas . Sleep. 2004. ; 27 ( 4 ): 751 – 760 . [DOI] [PubMed] [Google Scholar]
- 73. Su TP , Huang SR , Chou P . Prevalence and risk factors of insomnia in community-dwelling Chinese elderly: a Taiwanese urban area survey . Aust N Z J Psychiatry. 2004. ; 38 ( 9 ): 706 – 713 . [DOI] [PubMed] [Google Scholar]
- 74. Terzano MG , Parrino L , Cirignotta F , et al. Studio Morfeo Committee . Studio Morfeo: insomnia in primary care, a survey conducted on the Italian population . Sleep Med. 2004. ; 5 ( 1 ): 67 – 75 . [DOI] [PubMed] [Google Scholar]
- 75. Acebo C , Sadeh A , Seifer R , Tzischinsky O , Hafer A , Carskadon MA . Sleep/wake patterns derived from activity monitoring and maternal report for healthy 1- to 5-year-old children . Sleep. 2005. ; 28 ( 12 ): 1568 – 1577 . [DOI] [PubMed] [Google Scholar]
- 76. Averina M , Nilssen O , Brenn T , Brox J , Arkhipovsky VL , Kalinin AG . Social and lifestyle determinants of depression, anxiety, sleeping disorders and self-evaluated quality of life in Russia–a population-based study in Arkhangelsk . Soc Psychiatry Psychiatr Epidemiol. 2005. ; 40 ( 7 ): 511 – 518 . [DOI] [PubMed] [Google Scholar]
- 77. Chen YY , Kawachi I , Subramanian SV , Acevedo-Garcia D , Lee YJ . Can social factors explain sex differences in insomnia? Findings from a national survey in Taiwan . J Epidemiol Community Health. 2005. ; 59 ( 6 ): 488 – 494 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Fass R , Quan SF , O’Connor GT , Ervin A , Iber C . Predictors of heartburn during sleep in a large prospective cohort study . Chest. 2005. ; 127 ( 5 ): 1658 – 1666 . [DOI] [PubMed] [Google Scholar]
- 79. Gander PH , Marshall NS , Harris R , Reid P . The Epworth Sleepiness Scale: influence of age, ethnicity, and socioeconomic deprivation. Epworth Sleepiness scores of adults in New Zealand . Sleep. 2005. ; 28 ( 2 ): 249 – 253 . [DOI] [PubMed] [Google Scholar]
- 80. Gellis LA , Lichstein KL , Scarinci IC , et al . Socioeconomic status and insomnia . J Abnorm Psychol. 2005. ; 114 ( 1 ): 111 – 118 . [DOI] [PubMed] [Google Scholar]
- 81. Hale L . Who has time to sleep? J Public Health (Oxf). 2005. ; 27 ( 2 ): 205 – 211 . [DOI] [PubMed] [Google Scholar]
- 82. Hsu HC , Lin MH . Exploring quality of sleep and its related factors among menopausal women . J Nurs Res. 2005. ; 13 ( 2 ): 153 – 164 . [DOI] [PubMed] [Google Scholar]
- 83. Kim H , Young T . Subjective daytime sleepiness: dimensions and correlates in the general population . Sleep. 2005. ; 28 ( 5 ): 625 – 634 . [DOI] [PubMed] [Google Scholar]
- 84. McLaughlin Crabtree V , Beal Korhonen J , Montgomery-Downs HE , Faye Jones V , O’Brien LM , Gozal D . Cultural influences on the bedtime behaviors of young children . Sleep Med. 2005. ; 6 ( 4 ): 319 – 324 . [DOI] [PubMed] [Google Scholar]
- 85. Ohayon MM , Vecchierini MF . Normative sleep data, cognitive function and daily living activities in older adults in the community . Sleep. 2005. ; 28 ( 8 ): 981 – 989 . [PubMed] [Google Scholar]
- 86. Phillips B , Mannino D . Correlates of sleep complaints in adults: the ARIC study . J Clin Sleep Med. 2005. ; 1 ( 3 ): 277 – 283 . [PubMed] [Google Scholar]
- 87. Tjepkema M . Insomnia . Health Rep. 2005. ; 17 ( 1 ): 9 – 25 . [PubMed] [Google Scholar]
- 88. Tworoger SS , Davis S , Vitiello MV , Lentz MJ , McTiernan A . Factors associated with objective (actigraphic) and subjective sleep quality in young adult women . J Psychosom Res. 2005. ; 59 ( 1 ): 11 – 19 . [DOI] [PubMed] [Google Scholar]
- 89. Ursin R , Bjorvatn B , Holsten F . Sleep duration, subjective sleep need, and sleep habits of 40- to 45-year-olds in the Hordaland Health Study . Sleep. 2005. ; 28 ( 10 ): 1260 – 1269 . [DOI] [PubMed] [Google Scholar]
- 90. BaHammam A , Bin Saeed A , Al-Faris E , Shaikh S . Sleep duration and its correlates in a sample of Saudi elementary school children . Singapore Med J. 2006. ; 47 ( 10 ): 875 – 881 . [PubMed] [Google Scholar]
- 91. Kronholm E , Härmä M , Hublin C , Aro AR , Partonen T . Self-reported sleep duration in Finnish general population . J Sleep Res. 2006. ; 15 ( 3 ): 276 – 290 . [DOI] [PubMed] [Google Scholar]
- 92. Lauderdale DS , Knutson KL , Yan LL , et al . Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study . Am J Epidemiol. 2006. ; 164 ( 1 ): 5 – 16 . [DOI] [PubMed] [Google Scholar]
- 93. Sekine M , Chandola T , Martikainen P , Marmot M , Kagamimori S . Work and family characteristics as determinants of socioeconomic and sex inequalities in sleep: the Japanese Civil Servants Study . Sleep. 2006. ; 29 ( 2 ): 206 – 216 . [DOI] [PubMed] [Google Scholar]
- 94. Adam EK , Snell EK , Pendry P . Sleep timing and quantity in ecological and family context: a nationally representative time-diary study . J Fam Psychol. 2007. ; 21 ( 1 ): 4 – 19 . [DOI] [PubMed] [Google Scholar]
- 95. Friedman EM , Love GD , Rosenkranz MA , et al . Socioeconomic status predicts objective and subjective sleep quality in aging women . Psychosom Med. 2007. ; 69 ( 7 ): 682 – 691 . [DOI] [PubMed] [Google Scholar]
- 96. Ozden C , Ozdal OL , Altinova S , Oguzulgen I , Urgancioglu G , Memis A . Prevalence and associated factors of enuresis in Turkish children . Int Braz J Urol. 2007. ; 33 ( 2 ): 216 – 222 . [DOI] [PubMed] [Google Scholar]
- 97. Rangarajan S , Rangarajan S , D’Souza GA . Restless legs syndrome in an Indian urban population . Sleep Med. 2007. ; 9 ( 1 ): 88 – 93 . [DOI] [PubMed] [Google Scholar]
- 98. Stamatakis KA , Kaplan GA , Roberts RE . Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up . Ann Epidemiol. 2007. ; 17 ( 12 ): 948 – 955 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Baigi A , Lindgren EC , Starrin B , Bergh H . In the shadow of the welfare society ill-health and symptoms, psychological exposure and lifestyle habits among social security recipients: a national survey study . Biopsychosoc Med. 2008. ; 2 ( 1 ): 15 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Blay SL , Andreoli SB , Gastal FL . Prevalence of self-reported sleep disturbance among older adults and the association of disturbed sleep with service demand and medical conditions . Int Psychogeriatr. 2008. ; 20 ( 3 ): 582 – 595 . [DOI] [PubMed] [Google Scholar]
- 101. Ekici M , Ekici A , Keles H , Akin A , Karlidag A , Tunckol M , Kocyigit P . Risk factors and correlates of snoring and observed apnea . Sleep Med. 2008. ; 9 ( 3 ): 290 – 296 . [DOI] [PubMed] [Google Scholar]
- 102. Inan M , Tokuc B , Aydiner CY , Aksu B , Oner N , Basaran UN . Personal characteristics of enuretic children: an epidemiological study from South-East Europe . Urol Int. 2008. ; 81 ( 1 ): 47 – 53 . [DOI] [PubMed] [Google Scholar]
- 103. Jean-Louis G , Magai C , Casimir GJ , et al . Insomnia symptoms in a multiethnic sample of American women . J Women’s Health. 2008. ; 17 ( 1 ): 15 – 25 . [DOI] [PubMed] [Google Scholar]
- 104. Kuehni CE , Strippoli MP , Chauliac ES , Silverman M . Snoring in preschool children: prevalence, severity and risk factors . Eur Respir J. 2008. ; 31 ( 2 ): 326 – 333 . [DOI] [PubMed] [Google Scholar]
- 105. Li X , Sundquist K , Sundquist J . Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study . Sleep Med. 2008. ; 9 ( 2 ): 129 – 136 . [DOI] [PubMed] [Google Scholar]
- 106. Mezick EJ , Matthews KA , Hall M , et al . Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project . Psychosom Med. 2008. ; 70 ( 4 ): 410 – 416 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Roberts RE , Roberts CR , Chan W . Persistence and change in symptoms of insomnia among adolescents . Sleep. 2008. ; 31 ( 2 ): 177 – 184 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Virtanen P , Vahtera J , Broms U , Sillanmäki L , Kivimäki M , Koskenvuo M . Employment trajectory as determinant of change in health-related lifestyle: the prospective HeSSup study . Eur J Public Health. 2008. ; 18 ( 5 ): 504 – 508 . [DOI] [PubMed] [Google Scholar]
- 109. Xiang YT , Ma X , Cai ZJ , et al . The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey . Sleep. 2008. ; 31 ( 12 ): 1655 – 1662 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Yao KW , Yu S , Cheng SP , Chen IJ . Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults . J Nurs Res. 2008. ; 16 ( 2 ): 131 – 139 . [DOI] [PubMed] [Google Scholar]
- 111. Arber S , Bote M , Meadows R . Gender and socio-economic patterning of self-reported sleep problems in Britain . Soc Sci Med. 2009. ; 68 ( 2 ): 281 – 289 . [DOI] [PubMed] [Google Scholar]
- 112. Baker FC , Wolfson AR , Lee KA . Association of sociodemographic, lifestyle, and health factors with sleep quality and daytime sleepiness in women: findings from the 2007 National Sleep Foundation “Sleep in America Poll” . J Women’s Health. 2009. ; 18 ( 6 ): 841 – 849 . [DOI] [PubMed] [Google Scholar]
- 113. Cho YW , Shin WC , Yun CH , Hong SB , Kim J , Earley CJ . Epidemiology of insomnia in Korean adults: prevalence and associated factors . J Clin Neurol. 2009. ; 5 ( 1 ): 20 – 23 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Hall MH , Matthews KA , Kravitz HM , et al . Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study . Sleep. 2009. ; 32 ( 1 ): 73 – 82 . [PMC free article] [PubMed] [Google Scholar]
- 115. Jiang F , Zhu S , Yan C , Jin X , Bandla H , Shen X . Sleep and obesity in preschool children . J Pediatr. 2009. ; 154 ( 6 ): 814 – 818 . [DOI] [PubMed] [Google Scholar]
- 116. Joo S , Baik I , Yi H , Jung K , Kim J , Shin C . Prevalence of excessive daytime sleepiness and associated factors in the adult population of Korea . Sleep Med. 2009. ; 10 ( 2 ): 182 – 188 . [DOI] [PubMed] [Google Scholar]
- 117. Kim JM , Stewart R , Kim SW , Yang SJ , Shin IS , Yoon JS . Insomnia, depression, and physical disorders in late life: a 2-year longitudinal community study in Koreans . Sleep. 2009. ; 32 ( 9 ): 1221 – 1228 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Krueger PM , Friedman EM . Sleep duration in the United States: a cross-sectional population-based study . Am J Epidemiol. 2009. ; 169 ( 9 ): 1052 – 1063 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Reddy EV , Kadhiravan T , Mishra HK , et al . Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study . Sleep Med. 2009. ; 10 ( 8 ): 913 – 918 . [DOI] [PubMed] [Google Scholar]
- 120. Sivertsen B , Krokstad S , Øverland S , Mykletun A . The epidemiology of insomnia: associations with physical and mental health. The HUNT-2 study . J Psychosom Res. 2009. ; 67 ( 2 ): 109 – 116 . [DOI] [PubMed] [Google Scholar]
- 121. Vincent N , Cox B , Clara I . Are personality dimensions associated with sleep length in a large nationally representative sample? Compr Psychiatry. 2009. ; 50 ( 2 ): 158 – 163 . [DOI] [PubMed] [Google Scholar]
- 122. Yang QZ , Bu YQ , Dong SY , Fan SS , Wang LX . A comparison of sleeping problems in school-age children between rural and urban communities in China . J Paediatr Child Health. 2009. ; 45 ( 7-8 ): 414 – 418 . [DOI] [PubMed] [Google Scholar]
- 123. Fritsch Montero R , Lahsen Martínez P , Romeo Gómez R , Araya Baltra R , Rojas Castillo G . Sleep disorders in the adult population of Santiago of Chile and its association with common psychiatric disorders . Actas Esp Psiquiatr. 2010. ; 38 ( 6 ): 358 – 364 . [PubMed] [Google Scholar]
- 124. Goodin BR , McGuire L , Smith MT . Ethnicity moderates the influence of perceived social status on subjective sleep quality . Behav Sleep Med. 2010. ; 8 ( 4 ): 194 – 206 . [DOI] [PubMed] [Google Scholar]
- 125. Grandner MA , Patel NP , Gehrman PR , et al . Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints . Sleep Med. 2010. ; 11 ( 5 ): 470 – 478 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Gu D , Sautter J , Pipkin R , Zeng Y . Sociodemographic and health correlates of sleep quality and duration among very old Chinese . Sleep. 2010. ; 33 ( 5 ): 601 – 610 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Knutson KL , Van Cauter E , Rathouz PJ , DeLeire T , Lauderdale DS . Trends in the prevalence of short sleepers in the USA: 1975-2006 . Sleep. 2010. ; 33 ( 1 ): 37 – 45 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Lallukka T , Arber S , Rahkonen O , Lahelma E . Complaints of insomnia among midlife employed people: the contribution of childhood and present socioeconomic circumstances . Sleep Med. 2010. ; 11 ( 9 ): 828 – 836 . [DOI] [PubMed] [Google Scholar]
- 129. Li S , Jin X , Yan C , Wu S , Jiang F , Shen X . Habitual snoring in school-aged children: environmental and biological predictors . Respir Res. 2010. ; 11 ( 1 ): 144 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Li SX , Zhang B , Li AM , Wing YK . Prevalence and correlates of frequent nightmares: a community-based 2-phase study . Sleep. 2010. ; 33 ( 6 ): 774 – 780 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. Meltzer LJ , Johnson C , Crosette J , Ramos M , Mindell JA . Prevalence of diagnosed sleep disorders in pediatric primary care practices . Pediatrics. 2010. ; 125 ( 6 ): e1410 – e1418 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Mittelmark MB , Bull T . Social determinants of rest deprivation amongst Ghanaian women: national and urban-rural comparisons with data from a cross-sectional nationally representative survey . BMC Public Health. 2010. ; 10 ( 1 ): 580 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Nomura K , Yamaoka K , Nakao M , Yano E . Social determinants of self-reported sleep problems in South Korea and Taiwan . J Psychosom Res. 2010. ; 69 ( 5 ): 435 – 440 . [DOI] [PubMed] [Google Scholar]
- 134. Paparrigopoulos T , Tzavara C , Theleritis C , Psarros C , Soldatos C , Tountas Y . Insomnia and its correlates in a representative sample of the Greek population . BMC Public Health. 2010. ; 10 ( 1 ): 531 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Park S , Cho MJ , Chang SM , et al . Relationships of sleep duration with sociodemographic and health-related factors, psychiatric disorders and sleep disturbances in a community sample of Korean adults . J Sleep Res. 2010. ; 19 ( 4 ): 567 – 577 . [DOI] [PubMed] [Google Scholar]
- 136. Patel NP , Grandner MA , Xie D , Branas CC , Gooneratne N . “Sleep disparity” in the population: poor sleep quality is strongly associated with poverty and ethnicity . BMC Public Health. 2010. ; 10 ( 1 ): 475 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Tomfohr LM , Ancoli-Israel S , Dimsdale JE . Childhood socioeconomic status and race are associated with adult sleep . Behav Sleep Med. 2010. ; 8 ( 4 ): 219 – 230 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Tufik S , Santos-Silva R , Taddei JA , Bittencourt LR . Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study . Sleep Med. 2010. ; 11 ( 5 ): 441 – 446 . [DOI] [PubMed] [Google Scholar]
- 139. Amra B , Farajzadegan Z , Golshan M , Fietze I , Penzel T . Prevalence of sleep apnea-related symptoms in a Persian population . Sleep Breath. 2011. ; 15 ( 3 ): 425 – 429 . [DOI] [PubMed] [Google Scholar]
- 140. Arakane M , Castillo C , Rosero MF , Peñafiel R , Pérez-López FR , Chedraui P . Factors relating to insomnia during the menopausal transition as evaluated by the Insomnia Severity Index . Maturitas. 2011. ; 69 ( 2 ): 157 – 161 . [DOI] [PubMed] [Google Scholar]
- 141. Arman AR , Ay P , Fis NP , et al . Association of sleep duration with socio-economic status and behavioural problems among schoolchildren . Acta Paediatr. 2011. ; 100 ( 3 ): 420 – 424 . [DOI] [PubMed] [Google Scholar]
- 142. Bonuck KA , Chervin RD , Cole TJ , Emond A , Henderson J , Xu L , Freeman K . Prevalence and persistence of sleep disordered breathing symptoms in young children: a 6-year population-based cohort study . Sleep. 2011. ; 34 ( 7 ): 875 – 884 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Eder DN , Zou D , Grote L , Hedner J . Self-reported features of sleep, utilization of medical resources, and socioeconomic position: a Swedish population survey . Behav Sleep Med. 2011. ; 9 ( 3 ): 162 – 172 . [DOI] [PubMed] [Google Scholar]
- 144. Hense S , Barba G , Pohlabeln H , et al . Factors that influence weekday sleep duration in European children . Sleep. 2011. ; 34 ( 5 ): 633 – 639 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Li SX , Yu MWM , Lam SP , et al . Frequent nightmares in children: familial aggregation and associations with parent-reported behavioral and mood problems . Sleep. 2011. ; 34 ( 4 ): 487 – 493 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. McHale SM , Kim JY , Kan M , Updegraff KA . Sleep in Mexican-American adolescents: social ecological and well-being correlates . J Youth Adolesc. 2011. ; 40 ( 6 ): 666 – 679 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Moore M , Kirchner HL , Drotar D , Johnson N , Rosen C , Redline S . Correlates of adolescent sleep time and variability in sleep time: the role of individual and health related characteristics . Sleep Med. 2011. ; 12 ( 3 ): 239 – 245 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Pallesen S , Saxvig IW , Molde H , Sørensen E , Wilhelmsen-Langeland A , Bjorvatn B . Brief report: behaviorally induced insufficient sleep syndrome in older adolescents: prevalence and correlates . J Adolesc. 2011. ; 34 ( 2 ): 391 – 395 . [DOI] [PubMed] [Google Scholar]
- 149. Pigeon WR , Heffner K , Duberstein P , Fiscella K , Moynihan J , Chapman BP . Elevated sleep disturbance among blacks in an urban family medicine practice . J Am Board Fam Med. 2011. ; 24 ( 2 ): 161 – 168 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Ryu SY , Kim KS , Han MA . Factors associated with sleep duration in Korean adults: results of a 2008 community health survey in Gwangju metropolitan city, Korea . J Korean Med Sci. 2011. ; 26 ( 9 ): 1124 – 1131 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Wong WS , Fielding R . Prevalence of insomnia among Chinese adults in Hong Kong: a population-based study . J Sleep Res. 2011. ; 20 ( 1 Pt 1 ): 117 – 126 . [DOI] [PubMed] [Google Scholar]
- 152. Zhang J , Lam SP , Li SX , Li AM , Lai KY , Wing YK . Longitudinal course and outcome of chronic insomnia in Hong Kong Chinese children: a 5-year follow-up study of a community-based cohort . Sleep. 2011. ; 34 ( 10 ): 1395 – 1402 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Adams RJ , Piantadosi C , Appleton SL , et al . Investigating obstructive sleep apnoea: will the health system have the capacity to cope? A population study . Aust Health Rev. 2012. ; 36 ( 4 ): 424 – 429 . [DOI] [PubMed] [Google Scholar]
- 154. Blümel JE , Cano A , Mezones-Holguín E , et al . A multinational study of sleep disorders during female mid-life . Maturitas. 2012. ; 72 ( 4 ): 359 – 366 . [DOI] [PubMed] [Google Scholar]
- 155. Brug J , van Stralen MM , Te Velde SJ , et al . Differences in weight status and energy-balance related behaviors among schoolchildren across Europe: the ENERGY-project . PLoS One. 2012. ; 7 ( 4 ): e34742 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Calem M , Bisla J , Begum A , et al . Increased prevalence of insomnia and changes in hypnotics use in England over 15 years: analysis of the 1993, 2000, and 2007 National Psychiatric Morbidity Surveys . Sleep. 2012. ; 35 ( 3 ): 377 – 384 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Green MJ , Espie CA , Hunt K , Benzeval M . The longitudinal course of insomnia symptoms: inequalities by sex and occupational class among two different age cohorts followed for 20 years in the west of Scotland . Sleep. 2012. ; 35 ( 6 ): 815 – 823 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Guo X , Zhang X , Li Y , et al . Differences in healthy lifestyles between prehypertensive and normotensive children and adolescents in Northern China . Pediatr Cardiol. 2012. ; 33 ( 2 ): 222 – 228 . [DOI] [PubMed] [Google Scholar]
- 159. Heilemann MV , Choudhury SM , Kury FS , Lee KA . Factors associated with sleep disturbance in women of Mexican descent . J Adv Nurs. 2012. ; 68 ( 10 ): 2256 – 2266 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Kachikis AB , Breitkopf CR . Predictors of sleep characteristics among women in southeast Texas . Women’s Health Issues. 2012. ; 22 ( 1 ): e99 – 109 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Lallukka T , Sares-Jäske L , Kronholm E , et al . Sociodemographic and socioeconomic differences in sleep duration and insomnia-related symptoms in Finnish adults . BMC Public Health. 2012. ; 12 ( 1 ): 565 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Lima MG , Bergamo Francisco PM , de Azevedo Barros MB . Sleep duration pattern and chronic diseases in Brazilian adults (ISACAMP, 2008/09) . Sleep Med. 2012. ; 13 ( 2 ): 139 – 144 . [DOI] [PubMed] [Google Scholar]
- 163. Marco CA , Wolfson AR , Sparling M , Azuaje A . Family socioeconomic status and sleep patterns of young adolescents . Behav Sleep Med. 2011. ; 10 ( 1 ): 70 – 80 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Mazzotti DR , Guindalini C , Sosa AL , Ferri CP , Tufik S . Prevalence and correlates for sleep complaints in older adults in low and middle income countries: a 10/66 Dementia Research Group study . Sleep Med. 2012. ; 13 ( 6 ): 697 – 702 . [DOI] [PubMed] [Google Scholar]
- 165. Nicholson JM , Lucas N , Berthelsen D , Wake M . Socioeconomic inequality profiles in physical and developmental health from 0-7 years: Australian National Study . J Epidemiol Community Health. 2012. ; 66 ( 1 ): 81 – 87 . [DOI] [PubMed] [Google Scholar]
- 166. Nishikitani M , Nakao M , Tsurugano S , Yano E . The possible absence of a healthy-worker effect: a cross-sectional survey among educated Japanese women . BMJ Open. 2012. ; 2 ( 5 ): e000958 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Rosenbaum J . Degrees of health disparities: health status disparities between young adults with high school diplomas, sub-baccalaureate degrees, and baccalaureate degrees . Health Serv Outcomes Res Methodol. 2012. ; 12 ( 2-3 ): 156 – 168 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Soltani M , Haytabakhsh MR , Najman JM , et al . Sleepless nights: the effect of socioeconomic status, physical activity, and lifestyle factors on sleep quality in a large cohort of Australian women . Arch Women Ment Health. 2012. ; 15 ( 4 ): 237 – 247 . [DOI] [PubMed] [Google Scholar]
- 169. Stranges S , Tigbe W , Gómez-Olivé FX , Thorogood M , Kandala NB . Sleep problems: an emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia . Sleep. 2012. ; 35 ( 8 ): 1173 – 1181 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Talala KM , Martelin TP , Haukkala AH , Härkänen TT , Prättälä RS . Socio-economic differences in self-reported insomnia and stress in Finland from 1979 to 2002: a population-based repeated cross-sectional survey . BMC Public Health. 2012. ; 12 ( 1 ): 650 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Tu X , Cai H , Gao YT , et al . Sleep duration and its correlates in middle-aged and elderly Chinese women: the Shanghai Women’s Health Study . Sleep Med. 2012. ; 13 ( 9 ): 1138 – 1145 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Wall H , Smith C , Hubbard R . Body mass index and obstructive sleep apnoea in the UK: a cross-sectional study of the over-50s . Prim Care Resp J. 2012. ; 21 ( 4 ): 371 – 376 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Zhang J , Lam SP , Li SX , et al . Long-term outcomes and predictors of chronic insomnia: a prospective study in Hong Kong Chinese adults . Sleep Med. 2012. ; 13 ( 5 ): 455 – 462 . [DOI] [PubMed] [Google Scholar]
- 174. Ansarin K , Sahebi L , Sabur S . Obstructive sleep apnea syndrome: complaints and housing characteristics in a population in the United States . Sao Paulo Med J. 2013. ; 131 ( 4 ): 220 – 227 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Chen DR , Truong KD , Tsai MJ . Prevalence of poor sleep quality and its relationship with body mass index among teenagers: evidence from Taiwan . J Sch Health. 2013. ; 83 ( 8 ): 582 – 588 . [DOI] [PubMed] [Google Scholar]
- 176. El-Sheikh M , Bagley EJ , Keiley M , Elmore-Staton L , Chen E , Buckhalt JA . Economic adversity and children’s sleep problems: multiple indicators and moderation of effects . Health Psychol. 2013. ; 32 ( 8 ): 849 – 859 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Grandner MA , Petrov ME , Rattanaumpawan P , Jackson N , Platt A , Patel NP . Sleep symptoms, race/ethnicity, and socioeconomic position . J Clin Sleep Med. 2013. ; 9 ( 9 ): 897 – 905 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Hartz A , Ross JJ , Noyes R , Williams P . Somatic symptoms and psychological characteristics associated with insomnia in postmenopausal women . Sleep Med. 2013. ; 14 ( 1 ): 71 – 78 . [DOI] [PubMed] [Google Scholar]
- 179. Hoefelmann LP , Lopes AS , da Silva KS , Moritz P , Nahas MV . Sociodemographic factors associated with sleep quality and sleep duration in adolescents from Santa Catarina, Brazil: what changed between 2001 and 2011? Sleep Med. 2013. ; 14 ( 10 ): 1017 – 1023 . [DOI] [PubMed] [Google Scholar]
- 180. Hsu YW , Ho CH , Wang JJ , Hsieh KY , Weng SF , Wu MP . Longitudinal trends of the healthcare-seeking prevalence and incidence of insomnia in Taiwan: an 8-year nationally representative study . Sleep Med. 2013. ; 14 ( 9 ): 843 – 849 . [DOI] [PubMed] [Google Scholar]
- 181. Innes KE , Flack KL , Selfe TK , Kandati S , Agarwal P . Restless legs syndrome in an Appalachian primary care population: prevalence, demographic and lifestyle correlates, and burden . J Clin Sleep Med. 2013. ; 9 ( 10 ): 1065 – 1075 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Jarrin DC , McGrath JJ , Silverstein JE , Drake C . Objective and subjective socioeconomic gradients exist for sleep quality, sleep latency, sleep duration, weekend oversleep, and daytime sleepiness in adults . Behav Sleep Med. 2013. ; 11 ( 2 ): 144 – 158 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Kidwai R , Ahmed SH . Prevalence of insomnia and use of sleep medicines in urban communities of Karachi, Pakistan . J Pak Med Assoc. 2013. ; 63 ( 11 ): 1358 – 1363 . [PubMed] [Google Scholar]
- 184. Kim WH , Kim BS , Kim SK , Chang SM , Lee DW , Cho MJ , Bae JN . Prevalence of insomnia and associated factors in a community sample of elderly individuals in South Korea . Int Psychogeriatr. 2013. ; 25 ( 10 ): 1729 – 1737 . [DOI] [PubMed] [Google Scholar]
- 185. Luo J , Zhu G , Zhao Q , Guo Q , Meng H , Hong Z , Ding D . Prevalence and risk factors of poor sleep quality among Chinese elderly in an urban community: results from the Shanghai aging study . PLoS One. 2013. ; 8 ( 11 ): e81261 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Mindell JA , Sadeh A , Kwon R , Goh DY . Cross-cultural comparison of maternal sleep . Sleep. 2013. ; 36 ( 11 ): 1699 – 1706 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Yoshioka E , Saijo Y , Kita T , Satoh H , Kawaharada M , Kishi R . Effect of the interaction between employment level and psychosocial work environment on insomnia in male Japanese public service workers . Int J Behav Med. 2013. ; 20 ( 3 ): 355 – 364 . [DOI] [PubMed] [Google Scholar]
- 188. Anders MP , Breckenkamp J , Blettner M , Schlehofer B , Berg-Beckhoff G . Association between socioeconomic factors and sleep quality in an urban population-based sample in Germany . Eur J Public Health. 2014. ; 24 ( 6 ): 968 – 973 . [DOI] [PubMed] [Google Scholar]
- 189. Basner M , Spaeth AM , Dinges DF . Sociodemographic characteristics and waking activities and their role in the timing and duration of sleep . Sleep. 2014. ; 37 ( 12 ): 1889 – 1906 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Carrillo-Larco RM , Bernabé-Ortiz A , Miranda JJ , Rey de Castro J . Peruvians’ sleep duration: analysis of a population-based survey on adolescents and adults . PeerJ. 2014. ; 2 : e345 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Gjevre JA , Pahwa P , Karunanayake C , et al. Saskatchewan Rural Health Study Team . Excessive daytime sleepiness among rural residents in Saskatchewan . Can Respir J. 2014. ; 21 ( 4 ): 227 – 233 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Gubelmann C , Guessous I , Theler JM , Haba-Rubio J , Gaspoz JM , Marques-Vidal P . Trends and determinants of time in bed in Geneva, Switzerland . J Clin Sleep Med. 2014. ; 10 ( 10 ): 1129 – 1135 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Jarrin DC , McGrath JJ , Quon EC . Objective and subjective socioeconomic gradients exist for sleep in children and adolescents . Health Psychol. 2014. ; 33 ( 3 ): 301 – 305 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Kang K , Seo JG , Seo SH , Park KS , Lee HW . Prevalence and related factors for high-risk of obstructive sleep apnea in a large korean population: results of a questionnaire-based study . J Clin Neurol. 2014. ; 10 ( 1 ): 42 – 49 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Karaman S , Karaman T , Dogru S , et al . Prevalence of sleep disturbance in chronic pain . Eur Rev Med Pharmacol Sci. 2014. ; 18 ( 17 ): 2475 – 2481 . [PubMed] [Google Scholar]
- 196. Leng Y , Wainwright NW , Cappuccio FP , et al . Self-reported sleep patterns in a British population cohort . Sleep Med. 2014. ; 15 ( 3 ): 295 – 302 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Liviya Ng W , Freak-Poli R , Peeters A . The prevalence and characteristics associated with excessive daytime sleepiness among Australian workers . J Occup Environ Med. 2014. ; 56 ( 9 ): 935 – 945 . [DOI] [PubMed] [Google Scholar]
- 198. McDonald L , Wardle J , Llewellyn CH , van Jaarsveld CHM , Fisher A . Predictors of shorter sleep in early childhood . Sleep Med. 2014. ; 15 ( 5 ): 536 – 540 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Paine SJ , Fink J , Gander PH , Warman GR . Identifying advanced and delayed sleep phase disorders in the general population: a national survey of New Zealand adults . Chronobiol Int. 2014. ; 31 ( 5 ): 627 – 636 . [DOI] [PubMed] [Google Scholar]
- 200. Pallesen S , Sivertsen B , Nordhus IH , Bjorvatn B . A 10-year trend of insomnia prevalence in the adult Norwegian population . Sleep Med. 2014. ; 15 ( 2 ): 173 – 179 . [DOI] [PubMed] [Google Scholar]
- 201. Pan Y , Wang W , Wang KS . Associations of alcohol consumption and chronic diseases with sleep apnea among US adults . Int J High Risk Behav Addict. 2014. ; 3 ( 2 ): e19088 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Seib C , Anderson D , Lee K . Prevalence and correlates of sleep disturbance in postmenopausal women: the Australian Healthy Aging of Women (HOW) Study . J Women’s Health. 2014. ; 23 ( 2 ): 151 – 158 . [DOI] [PubMed] [Google Scholar]
- 203. Speirs KE , Liechty JM , Wu CF ; Strong Kids Research Team . Sleep, but not other daily routines, mediates the association between maternal employment and BMI for preschool children . Sleep Med. 2014. ; 15 ( 12 ): 1590 – 1593 . [DOI] [PubMed] [Google Scholar]
- 204. Takahashi M , Tsutsumi A , Kurioka S , et al . Occupational and socioeconomic differences in actigraphically measured sleep . J Sleep Res. 2014. ; 23 ( 4 ): 458 – 462 . [DOI] [PubMed] [Google Scholar]
- 205. Uhlig BL , Sand T , Odegård SS , Hagen K . Prevalence and associated factors of DSM-V insomnia in Norway: the Nord-Trøndelag Health Study (HUNT 3) . Sleep Med. 2014. ; 15 ( 6 ): 708 – 713 . [DOI] [PubMed] [Google Scholar]
- 206. Whinnery J , Jackson N , Rattanaumpawan P , Grandner MA . Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position . Sleep. 2014. ; 37 ( 3 ): 601 – 611 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Bagley EJ , Kelly RJ , Buckhalt JA , El-Sheikh M . What keeps low-SES children from sleeping well: the role of presleep worries and sleep environment . Sleep Med. 2015. ; 16 ( 4 ): 496 – 502 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Baiden P , Fallon B , den Dunnen W , Boateng GO . The enduring effects of early-childhood adversities and troubled sleep among Canadian adults: a population-based study . Sleep Med. 2015. ; 16 ( 6 ): 760 – 767 . [DOI] [PubMed] [Google Scholar]
- 209. Benbir G , Demir AU , Aksu M , et al . Prevalence of insomnia and its clinical correlates in a general population in Turkey . Psychiatry Clin Neurosci. 2015. ; 69 ( 9 ): 543 – 552 . [DOI] [PubMed] [Google Scholar]
- 210. Bonke J . Trends in short and long sleep in Denmark from 1964 to 2009, and the associations with employment, SES (socioeconomic status) and BMI . Sleep Med. 2015. ; 16 ( 3 ): 385 – 390 . [DOI] [PubMed] [Google Scholar]
- 211. Buxton OM , Chang AM , Spilsbury JC , Bos T , Emsellem H , Knutson KL . Sleep in the modern family: protective family routines for child and adolescent sleep . Sleep Health. 2015. ; 1 ( 1 ): 15 – 27 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Cunningham TJ , Ford ES , Chapman DP , Liu Y , Croft JB . Independent and joint associations of race/ethnicity and educational attainment with sleep-related symptoms in a population-based US sample . Prev Med. 2015. ; 77 : 99 – 105 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Ding M , Keiley MK , Garza KB , Duffy PA , Zizza CA . Food insecurity is associated with poor sleep outcomes among US adults . J Nutr. 2015. ; 145 ( 3 ): 615 – 621 . [DOI] [PubMed] [Google Scholar]
- 214. El-Sheikh M , Keiley M , Bagley EJ , Chen E . Socioeconomic adversity and women’s sleep: stress and chaos as mediators . Behav Sleep Med. 2015. ; 13 ( 6 ): 506 – 523 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Gamaldo AA , McNeely JM , Shah MT , Evans MK , Zonderman AB . Racial differences in self-reports of short sleep duration in an urban-dwelling environment . J Gerontol B Psychol Sci Soc Sci. 2015. ; 70 ( 4 ): 568 – 575 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Katainen RE , Siirtola TJ , Engblom JR , Erkkola RU , Polo-Kantola P . A population-based survey of quality of life in middle-aged Finnish women . Menopause. 2015. ; 22 ( 4 ): 402 – 413 . [DOI] [PubMed] [Google Scholar]
- 217. Kim WH , Kim BS , Kim SK , et al . Sleep duration and associated factors in a community sample of elderly individuals in Korea . Psychogeriatrics. 2015. ; 15 ( 2 ): 87 – 94 . [DOI] [PubMed] [Google Scholar]
- 218. Kurina LM , Thisted RA , Chen JH , McClintock MK , Waite LJ , Lauderdale DS . Actigraphic sleep characteristics among older Americans . Sleep Health. 2015. ; 1 ( 4 ): 285 – 292 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Nisar N , Sikandar R , Sohoo NA . Menopausal symptoms: prevalence, severity and correlation with sociodemographic and reproductive characteristics. A cross sectional community based survey from rural Sindh Pakistan . J Pak Med Assoc. 2015. ; 65 ( 4 ): 409 – 413 . [PubMed] [Google Scholar]
- 220. Patel SR , Sotres-Alvarez D , Castañeda SF , et al . Social and health correlates of sleep duration in a US Hispanic population: results from the Hispanic Community Health Study/Study of Latinos . Sleep. 2015. ; 38 ( 10 ): 1515 – 1522 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Schwartz NG , Rattner A , Schwartz AR , et al. CRONICAS Cohort Study Group . Sleep disordered breathing in four resource-limited settings in Peru: prevalence, risk factors, and association with chronic diseases . Sleep. 2015. ; 38 ( 9 ): 1451 – 1459 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Sivertsen B , Harvey AG , Pallesen S , Hysing M . Mental health problems in adolescents with delayed sleep phase: results from a large population-based study in Norway . J Sleep Res. 2015. ; 24 ( 1 ): 11 – 18 . [DOI] [PubMed] [Google Scholar]
- 223. Stringhini S , Haba-Rubio J , Marques-Vidal P , et al . Association of socioeconomic status with sleep disturbances in the Swiss population-based CoLaus study . Sleep Med. 2015. ; 16 ( 4 ): 469 – 476 . [DOI] [PubMed] [Google Scholar]
- 224. Suarez E , Fang SC , Bliwise D , Yaggi HK , Araujo A . Disentangling racial/ethnic and socioeconomic differences in self-reported sleep measures: the Boston Area Community Health Survey . Sleep Health. 2015. ; 1 ( 2 ): 90 – 97 . [DOI] [PubMed] [Google Scholar]
- 225. van de Straat V , Bracke P . How well does Europe sleep? A cross-national study of sleep problems in European older adults . Int J Public Health. 2015. ; 60 ( 6 ): 643 – 650 . [DOI] [PubMed] [Google Scholar]
- 226. Yoon H-S , Yang JJ , Song M , et al . Correlates of self-reported sleep duration in middle-aged and elderly Koreans: from the Health Examinees Study . PLoS One. 2015. ; 10 ( 5 ): e0123510 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Zapata Roblyer MI , Grzywacz JG . Demographic and parenting correlates of adolescent sleep functioning . J Child Fam Stud. 2015. ; 24 ( 11 ): 3331 – 3340 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Danielsson K , Markström A , Broman JE , von Knorring L , Jansson-Fröjmark M . Delayed sleep phase disorder in a Swedish cohort of adolescents and young adults: prevalence and associated factors . Chronobiol Int. 2016. ; 33 ( 10 ): 1331 – 1339 . [DOI] [PubMed] [Google Scholar]
- 229. de Jong DM , Cremone A , Kurdziel LB , et al . Maternal depressive symptoms and household income in relation to sleep in early childhood . J Pediatr Psychol. 2016. ; 41 ( 9 ): 961 – 970 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. de Ruiter I , Olmedo-Requena R , Sánchez-Cruz JJ , Jiménez-Moleón JJ . Changes in sleep duration in Spanish children aged 2-14 years from 1987 to 2011 . Sleep Med. 2016. ; 21 : 145 – 150 . [DOI] [PubMed] [Google Scholar]
- 231. Hawkins SS , Takeuchi DT . Social determinants of inadequate sleep in US children and adolescents . Public Health. 2016. ; 138 : 119 – 126 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Heshmat R , Qorbani M , Ghoreshi B , et al . Association of socioeconomic status with psychiatric problems and violent behaviours in a nationally representative sample of Iranian children and adolescents: the CASPIAN-IV study . BMJ Open. 2016. ; 6 ( 8 ): e011615 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Johnson DA , Lisabeth L , Hickson D , et al . The social patterning of sleep in African Americans: associations of socioeconomic position and neighborhood characteristics with sleep in the Jackson Heart Study . Sleep. 2016. ; 39 ( 9 ): 1749 – 1759 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Malone SK , Patterson F , Lu Y , Lozano A , Hanlon A . Ethnic differences in sleep duration and morning-evening type in a population sample . Chronobiol Int. 2016. ; 33 ( 1 ): 10 – 21 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Paine SJ , Gander PH . Explaining ethnic inequities in sleep duration: a cross-sectional survey of Māori and non-Māori adults in New Zealand . Sleep Health. 2016. ; 2 ( 2 ): 109 – 115 . [DOI] [PubMed] [Google Scholar]
- 236. Paine SJ , Harris R , Cormack D , Stanley J . Racial discrimination and ethnic disparities in sleep disturbance: the 2002/03 New Zealand Health Survey . Sleep. 2016. ; 39 ( 2 ): 477 – 485 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Peltzer K , Pengpid S . Sleep duration and health correlates among university students in 26 countries . Psychol Health Med. 2016. ; 21 ( 2 ): 208 – 220 . [DOI] [PubMed] [Google Scholar]
- 238. Peña MM , Rifas-Shiman SL , Gillman MW , Redline S , Taveras EM . Racial/ethnic and socio-contextual correlates of chronic sleep curtailment in childhood . Sleep. 2016. ; 39 ( 9 ): 1653 – 1661 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Safak ED , Gocer S , Mucuk S , et al . The prevalence and related factors of restless leg syndrome in the community dwelling elderly; in Kayseri, Turkey: a cross-sectional study . Arch Gerontol Geriatr. 2016. ; 65 : 29 – 35 . [DOI] [PubMed] [Google Scholar]
- 240. Schäfer AA , Domingues MR , Dahly DL , et al . Correlates of self-reported weekday sleep duration in adolescents: the 18-year follow-up of the 1993 Pelotas (Brazil) Birth Cohort Study . Sleep Med. 2016. ; 23 : 81 – 88 . [DOI] [PubMed] [Google Scholar]
- 241. Seyedmehdi SM , Rahnama N , Yazdanparast T , et al . Prevalence of snoring and the risk of sleep apnea in hospital staff . Work. 2016. ; 55 ( 4 ): 765 – 772 . [DOI] [PubMed] [Google Scholar]
- 242. Smagula SF , Koh WP , Wang R , Yuan JM . Chronic disease and lifestyle factors associated with change in sleep duration among older adults in the Singapore Chinese Health Study . J Sleep Res. 2016. ; 25 ( 1 ): 57 – 61 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Tareque MI , Ikeda N , Koshio A , Hasegawa T . Is adjustment for reporting heterogeneity necessary in sleep disorders? Results from the Japanese World Health Survey . BMC Psychiatry. 2016. ; 16 ( 1 ): 25 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Wong JC , Li J , Pavlova M , et al . Risk factors for probable REM sleep behavior disorder: a community-based study . Neurology. 2016. ; 86 ( 14 ): 1306 – 1312 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Abraham O , Pu J , Schleiden LJ , Albert SM . Factors contributing to poor satisfaction with sleep and healthcare seeking behavior in older adults . Sleep Health. 2017. ; 3 ( 1 ): 43 – 48 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Ahmed AE , Al-Jahdali H , Fatani A , et al . The effects of age and gender on the prevalence of insomnia in a sample of the Saudi population . Ethn Health. 2017. ; 22 ( 3 ): 285 – 294 . [DOI] [PubMed] [Google Scholar]
- 247. Assari S , Nikahd A , Malekahmadi MR , Lankarani MM , Zamanian H . Race by gender group differences in the protective effects of socioeconomic factors against sustained health problems across five domains . J Racial Ethn Health Disparities. 2016. ; 4 ( 5 ): 884 – 894 . [DOI] [PubMed] [Google Scholar]
- 248. Bapat R , van Geel M , Vedder P . Socio-economic status, time spending, and sleep duration in Indian children and adolescents . J Child Fam Stud. 2017. ; 26 ( 1 ): 80 – 87 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Barazzetta M , Ghislandi S . Family income and material deprivation: do they matter for sleep quality and quantity in early life? Evidence from a longitudinal study . Sleep. 2017. ; 40 ( 3 ): zsw066 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Brambilla P , Giussani M , Pasinato A , et al. “Ci piace sognare” Study Group . Sleep habits and pattern in 1–14 years old children and relationship with video devices use and evening and night child activities . Ital J Pediatr. 2017. ; 43 ( 1 ): 7 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Cheng GH , Chan A , Lo JC . Factors of nocturnal sleep and daytime nap durations in community-dwelling elderly: a longitudinal population-based study . Int Psychogeriatr. 2017. ; 29 ( 8 ): 1335 – 1344 . [DOI] [PubMed] [Google Scholar]
- 252. Clark BK , Kolbe-Alexander TL , Duncan MJ , Brown W . Sitting time, physical activity and sleep by work type and pattern-the Australian Longitudinal Study on Women’s Health . Int J Environ Res Public Health. 2017. ; 14 ( 3 ): E290 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253. Costanian C , Abdullah P , Sawh N , Nagapatan A , Tamim H . Factors associated with shorter night-time sleep in toddlers: the Survey of Young Canadians . Can J Public Health. 2018. ; 108 ( 5-6 ): e571 – e577 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Didriksen M , Rigas AS , Allen RP , et al . Prevalence of restless legs syndrome and associated factors in an otherwise healthy population: results from the Danish Blood Donor Study . Sleep Med. 2017. ; 36 : 55 – 61 . [DOI] [PubMed] [Google Scholar]
- 255. Foroughi M , Malekmohammad M , Sharafkhaneh A , Emami H , Adimi P , Khoundabi B . Prevalence of obstructive sleep apnea in a high-risk population using the Stop-Bang Questionnaire in Tehran, Iran . Tanaffos. 2017. ; 16 ( 3 ): 217 – 224 . [PMC free article] [PubMed] [Google Scholar]
- 256. Fulgencio LB , Corrêa-Faria P , Lage CF , Paiva SM , Pordeus IA , Serra-Negra JM . Diagnosis of sleep bruxism can assist in the detection of cases of verbal school bullying and measure the life satisfaction of adolescents . Int J Paediatr Dent. 2017. ; 27 ( 4 ): 293 – 301 . [DOI] [PubMed] [Google Scholar]
- 257. Grandner MA , Winkelman JW . Nocturnal leg cramps: prevalence and associations with demographics, sleep disturbance symptoms, medical conditions, and cardiometabolic risk factors . PLoS One. 2017. ; 12 ( 6 ): e0178465 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Ham OK , Kim J , Lee BG , Choi E . Behavioral characteristics and cardiovascular disease risks associated with insomnia and sleep quality among middle-aged women in South Korea . Res Nurs Health. 2017. ; 40 ( 3 ): 206 – 217 . [DOI] [PubMed] [Google Scholar]
- 259. Hardy LL , Mihrshahi S , Bellew W , Bauman A , Ding D . Children’s adherence to health behavior recommendations associated with reducing risk of non-communicable disease . Prev Med Rep. 2017. ; 8 : 279 – 285 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Kim WJ , Joo W-T , Baek J , et al . Factors associated with insomnia among the elderly in a Korean rural community . Psychiatry Investig. 2017. ; 14 ( 4 ): 400 – 406 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Koolhaas CM , van Rooij FJA , Schoufour JD , et al . Objective measures of activity in the elderly: distribution and associations with demographic and health factors . J Am Med Dir Assoc. 2017. ; 18 ( 10 ): 838 – 847 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262. Ma JF , Qiao Y , Gao X , et al . A community-based study of risk factors for probable rapid eye movement sleep behavior disorder . Sleep Med. 2017. ; 30 : 71 – 76 . [DOI] [PubMed] [Google Scholar]
- 263. Ma Y , Peng L , Kou C , Hua S , Yuan H . Associations of overweight, obesity and related factors with sleep-related breathing disorders and snoring in adolescents: a cross-sectional survey . Int J Environ Res Public Health. 2017. ; 14 ( 2 ): E194 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Maume DJ . Social relationships and the sleep-health nexus in adolescence: evidence from a comprehensive model with bi-directional effects . Sleep Health. 2017. ; 3 ( 4 ): 284 – 289 . [DOI] [PubMed] [Google Scholar]
- 265. McDowall PS , Elder DE , Campbell AJ . Relationship between parent knowledge of child sleep, and child sleep practices and problems: a pilot study in a children’s hospital cohort . J Paediatr Child Health. 2017. ; 53 ( 8 ): 788 – 793 . [DOI] [PubMed] [Google Scholar]
- 266. Mota-Veloso I , Celeste RK , Fonseca CP , et al . Effects of attention deficit hyperactivity disorder signs and socio-economic status on sleep bruxism and tooth wear among schoolchildren: structural equation modelling approach . Int J Paediatr Dent. 2017. ; 27 ( 6 ): 523 – 531 . [DOI] [PubMed] [Google Scholar]
- 267. Netsi E , Santos IS , Stein A , Barros FC , Barros AJD , Matijasevich A . A different rhythm of life: sleep patterns in the first 4 years of life and associated sociodemographic characteristics in a large Brazilian birth cohort . Sleep Med. 2017. ; 37 : 77 – 87 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Palmer KT , D’Angelo S , Harris EC , et al . Sleep disturbance and the older worker: findings from the Health and Employment after Fifty study . Scand J Work Environ Health. 2017. ; 43 ( 2 ): 136 – 145 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Patte KA , Qian W , Leatherdale ST . Sleep duration trends and trajectories among youth in the COMPASS study . Sleep Health. 2017. ; 3 ( 5 ): 309 – 316 . [DOI] [PubMed] [Google Scholar]
- 270. Perales F , Plage S . Losing ground, losing sleep: local economic conditions, economic vulnerability, and sleep . Soc Sci Res. 2017. ; 62 : 189 – 203 . [DOI] [PubMed] [Google Scholar]
- 271. Seo WH , Kwon JH , Eun SH , Kim G , Han K , Choi BM . Effect of socio-economic status on sleep . J Paediatr Child Health. 2017. ; 53 ( 6 ): 592 – 597 . [DOI] [PubMed] [Google Scholar]
- 272. Sivertsen B , Bøe T , Skogen JC , Petrie KJ , Hysing M . Moving into poverty during childhood is associated with later sleep problems . Sleep Med. 2017. ; 37 : 54 – 59 . [DOI] [PubMed] [Google Scholar]
- 273. Tang J , Liao Y , Kelly BC , et al . Gender and regional differences in sleep quality and insomnia: a general population-based study in Hunan Province of China . Sci Rep. 2017. ; 7 ( 1 ): 43690 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Walsemann KM , Ailshire JA , Fisk CE , Brown LL . Do gender and racial/ethnic disparities in sleep duration emerge in early adulthood? Evidence from a longitudinal study of U.S. adults . Sleep Med. 2017. ; 36 : 133 – 140 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275. Wang S , Li B , Wu Y , et al . Relationship of sleep duration with sociodemographic characteristics, lifestyle, mental health, and chronic diseases in a large Chinese adult population . J Clin Sleep Med. 2017. ; 13 ( 3 ): 377 – 384 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Yu XT , Sadeh A , Lam HS , Mindell JA , Li AM . Parental behaviors and sleep/wake patterns of infants and toddlers in Hong Kong, China . World J Pediatr. 2017. ; 13 ( 5 ): 496 – 502 . [DOI] [PubMed] [Google Scholar]
- 277. Yunus RM , Wazid SW , Hairi NN , et al . Association between elder abuse and poor sleep: a cross-sectional study among rural older Malaysians . PLoS One. 2017. ; 12 ( 7 ): e0180222 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Zhang HS , Li Y , Mo HY , et al . A community-based cross-sectional study of sleep quality in middle-aged and older adults . Qual Life Res. 2017. ; 26 ( 4 ): 923 – 933 . [DOI] [PubMed] [Google Scholar]
- 279. Berhanu H , Mossie A , Tadesse S , Geleta D . Prevalence and associated factors of sleep quality among adults in Jimma Town, Southwest Ethiopia: a community-based cross-sectional study . Sleep Disord. 2018. ; 2018 : 8342328 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Cha S-E , Eun K-S . Convergence in sleep time accomplished? Gender gap in sleep time for middle-aged adults in Korea . Int J Environ Res Public Health. 2018. ; 15 ( 4 ): 803 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Chang VC , Chaput JP , Roberts KC , Jayaraman G , Do MT . Factors associated with sleep duration across life stages: results from the Canadian Health Measures Survey . Health Promot Chronic Dis Prev Can. 2018. ; 38 ( 11 ): 404 – 418 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. de Jonge J , Shimazu A , Dollard M . Short-term and long-term effects of off-job activities on recovery and sleep: a two-wave panel study among health care employees . Int J Environ Res Public Health. 2018. ; 15 ( 9 ): 2044 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. de Lima TR , Silva DAS . Association of sleep quality with sociodemographic factors and lifestyle in adolescents from southern Brazil . World J Pediatr. 2018. ; 14 ( 4 ): 383 – 391 . [DOI] [PubMed] [Google Scholar]
- 284. Dong X , Wang Y , Chen Y , et al . Poor sleep quality and influencing factors among rural adults in Deqing, China . Sleep Breath. 2018. ; 22 ( 4 ): 1213 – 1220 . [DOI] [PubMed] [Google Scholar]
- 285. Gómez-Olivé FX , Rohr JK , Roden LC , Rae DE , von Schantz M . Associations between sleep parameters, non-communicable diseases, HIV status and medications in older, rural South Africans . Sci Rep. 2018. ; 8 ( 1 ): 17321 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286. Goyal A , Pakhare AP , Bhatt GC , Choudhary B , Patil R . Association of pediatric obstructive sleep apnea with poor academic performance: a school-based study from India . Lung India. 2018. ; 35 ( 2 ): 132 – 136 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287. Jaisoorya TS , Dahale AB , Sunil KG , Manoj L , Gokul GR , Thennarassu K . Insomnia in primary care-a study from India . Sleep Health. 2018. ; 4 ( 1 ): 63 – 67 . [DOI] [PubMed] [Google Scholar]
- 288. Khan IW , Juyal R , Shikha D , Gupta R . Generalized Anxiety disorder but not depression is associated with insomnia: a population based study . Sleep Sci. 2018. ; 11 ( 3 ): 166 – 173 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Lima MG , Barros MBA , Ceolim MF , Zancanella E , Cardoso TAMO . Sleep duration, health status, and subjective well-being: a population-based study . Rev Saude Publica. 2018. ; 52 : 82 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Lin LN , Chang LY , Hurng BS , Wu CC , Yen LL , Chang HY . Sex differences in sleep patterns and changes in 7th to 12th graders: a longitudinal follow-up study in Taiwan . Sleep. 2018. ; 41 ( 3 ): zsx211 . [DOI] [PubMed] [Google Scholar]
- 291. Ma J , Li C , Kwan MP , Chai Y . A multilevel analysis of perceived noise pollution, geographic contexts and mental health in Beijing . Int J Environ Res Public Health. 2018. ; 15 ( 7 ): E1479 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292. Ma Y , Hu Z , Qin X , Chen R , Zhou Y . Prevalence and socio-economic correlates of insomnia among older people in Anhui, China . Australas J Ageing. 2018. ; 37 ( 3 ): E91 – E96 . [DOI] [PubMed] [Google Scholar]
- 293. Manyanga T , Barnes JD , Tremblay MS , et al. ISCOLE Research Group . No evidence for an epidemiological transition in sleep patterns among children: a 12-country study . Sleep Health. 2018. ; 4 ( 1 ): 87 – 95 . [DOI] [PubMed] [Google Scholar]
- 294. Matthews KA , Jennings JR , Lee L . Socioeconomic status in childhood predicts sleep continuity in adult Black and White men . Sleep Health. 2018. ; 4 ( 1 ): 49 – 55 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295. Meneton P , Hoertel N , Wiernik E , et al . Work environment mediates a large part of social inequalities in the incidence of several common cardiovascular risk factors: findings from the Gazel cohort . Soc Sci Med. 2018. ; 216 : 59 – 66 . [DOI] [PubMed] [Google Scholar]
- 296. Miner B , Gill TM , Yaggi HK , et al . Insomnia in community-living persons with advanced age . J Am Geriatr Soc. 2018. ; 66 ( 8 ): 1592 – 1597 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297. Olorunmoteni OE , Fatusi AO , Komolafe MA , Omisore A . Sleep pattern, socioenvironmental factors, and use of electronic devices among Nigerian school-attending adolescents . Sleep Health. 2018. ; 4 ( 6 ): 551 – 557 . [DOI] [PubMed] [Google Scholar]
- 298. Park C , Sim CS , Sung JH , et al . Low income as a vulnerable factor to the effect of noise on insomnia . Psychiatry Investig. 2018. ; 15 ( 6 ): 602 – 612 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299. Pepin JR , Sayer LC , Casper LM . Marital status and mothers’ time use: childcare, housework, leisure, and sleep . Demography. 2018. ; 55 ( 1 ): 107 – 133 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Plancoulaine S , Reynaud E , Forhan A , Lioret S , Heude B , Charles MA ; EDEN Mother−Child Cohort Study Group . Night sleep duration trajectories and associated factors among preschool children from the EDEN cohort . Sleep Med. 2018. ; 48 : 194 – 201 . [DOI] [PubMed] [Google Scholar]
- 301. Schlieber M , Han J . The sleeping patterns of Head Start children and the influence on developmental outcomes . Child Care Health Dev. 2018. ; 44 ( 3 ): 462 – 469 . [DOI] [PubMed] [Google Scholar]
- 302. Thichumpa W , Howteerakul N , Suwannapong N , Tantrakul V . Sleep quality and associated factors among the elderly living in rural Chiang Rai, northern Thailand . Epidemiol Health. 2018. ; 40 : e2018018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303. Wu W , Wang W , Dong Z , et al . Sleep quality and its associated factors among low-income adults in a rural area of China: a population-based study . Int J Environ Res Public Health. 2018. ; 15 ( 9 ): E2055 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304. Yang T , Peng S , Barnett R , Zhang C . Regional contextual influences on short sleep duration: a 50 universities population-based multilevel study in China . Glob Health Action. 2018. ; 11 ( 1 ): 1442684 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Zheng W , Luo X-N , Li H-Y , et al . Prevalence of insomnia symptoms and their associated factors in patients treated in outpatient clinics of four general hospitals in Guangzhou, China . BMC Psychiatry. 2018. ; 18 ( 1 ): 232 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306. Zheng W , Luo X-N , Li H-Y , et al . Association of sleep duration with sleep disturbances, quality of life, and sociodemographic factors in general hospital outpatients . Perspect Psychiatr Care. 2018. ; 54 ( 3 ): 422 – 427 . [DOI] [PubMed] [Google Scholar]
- 307. Akay A , Martinsson P , Ralsmark H . Relative concerns and sleep behavior . Econ Hum Biol. 2019. ; 33 : 1 – 14 . [DOI] [PubMed] [Google Scholar]
- 308. Åkerstedt T , Discacciati A , Häbel H , Westerlund H . Psychosocial work demands and physical workload decrease with ageing in blue-collar and white-collar workers: a prospective study based on the SLOSH cohort . BMJ Open. 2019. ; 9 ( 9 ): e030918 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Al-Hazzaa HM , Alhussain MH , Alhowikan AM , Obeid OA . insufficient sleep duration and its association with breakfast intake, overweight/obesity, socio-demographics and selected lifestyle behaviors among Saudi school children . Nat Sci Sleep. 2019. ; 11 : 253 – 263 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310. Althakafi KA , Alrashed AA , Aljammaz KI , et al . Prevalence of short sleep duration and effect of co-morbid medical conditions - a cross-sectional study in Saudi Arabia . J Family Med Prim Care. 2019. ; 8 ( 10 ): 3334 – 3339 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311. Barros MBA , Lima MG , Ceolim MF , Zancanella E , Cardoso TAMO . Quality of sleep, health and well-being in a population-based study . Rev Saude Publica. 2019. ; 53 : 82 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Bazargan M , Mian N , Cobb S , Vargas R , Assari S . Insomnia symptoms among African-American older adults in economically disadvantaged areas of South Los Angeles . Brain Sci. 2019. ; 9 ( 11 ): E306 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Carneiro IM , Fonseca P , Ferreira R . Children’s Sleep Habits Questionnaire in two subpopulations from Cape Verde and Mozambique: exploratory and regression analysis . Acta Med Port. 2019. ; 32 ( 10 ): 628 – 634 . [DOI] [PubMed] [Google Scholar]
- 314. Chami HA , Bechnak A , Isma'eel H , et al . Sleepless in Beirut: sleep difficulties in an urban environment with chronic psychosocial stress . J Clin Sleep Med. 2019. ; 15 ( 4 ): 603 – 614 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315. Chen JH . Experience of poverty and problem sleep in later life . Res Aging. 2019. ; 41 ( 7 ): 697 – 722 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Gordon S , Vandelanotte C , Rayward AT , Murawski B , Duncan MJ . Sociodemographic and behavioral correlates of insufficient sleep in Australian adults . Sleep Health. 2019. ; 5 ( 1 ): 12 – 17 . [DOI] [PubMed] [Google Scholar]
- 317. Hartescu I , Morgan K . Regular physical activity and insomnia: an international perspective . J Sleep Res. 2019. ; 28 ( 2 ): e12745 . [DOI] [PubMed] [Google Scholar]
- 318. Kobel S , Wartha O , Dreyhaupt J , Kettner S , Steinacker JM . Cross-sectional associations of objectively assessed sleep duration with physical activity, BMI and television viewing in German primary school children . BMC Pediatr. 2019. ; 19 ( 1 ): 54 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319. Laganière C , Gaudreau H , Pokhvisneva I , Atkinson L , Meaney M , Pennestri MH . Maternal characteristics and behavioural/emotional problems in preschoolers: how they relate to sleep rhythmic movements at sleep onset . J Sleep Res. 2019. ; 28 ( 3 ): e12707 . [DOI] [PubMed] [Google Scholar]
- 320. Lee ES , Park S . Patterns of change in employment status and their association with self-rated health, perceived daily stress, and sleep among young adults in South Korea . Int J Environ Res Public Health. 2019. ; 16 ( 22 ): E4491 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Lee EY , Carson V , Jeon JY , Spence JC , Tremblay MS . Levels and correlates of 24-hour movement behaviors among South Koreans: results from the Korea National Health and Nutrition Examination Surveys, 2014 and 2015 . J Sport Health Sci. 2019. ; 8 ( 4 ): 376 – 385 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322. Lei WY , Chang WC , Wong MW , et al . Sleep disturbance and its association with gastrointestinal symptoms/diseases and psychological comorbidity . Digestion. 2019. ; 99 ( 3 ): 205 – 212 . [DOI] [PubMed] [Google Scholar]
- 323. Maeda M , Filomeno R , Kawata Y , et al . Association between unemployment and insomnia-related symptoms based on the Comprehensive Survey of Living Conditions: a large cross-sectional Japanese population survey . Ind Health. 2019. ; 57 ( 6 ): 701 – 710 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Manyanga T , Barnes JD , Chaput JP , Katzmarzyk PT , Prista A , Tremblay MS . Prevalence and correlates of adherence to movement guidelines among urban and rural children in Mozambique: a cross-sectional study . Int J Behav Nutr Phys Act. 2019. ; 16 ( 1 ): 94 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325. Matenchuk BA , Tamana SK , Lou WYW , et al. CHILD Study Investigators . Prenatal depression and birth mode sequentially mediate maternal education’s influence on infant sleep duration . Sleep Med. 2019. ; 59 : 24 – 32 . [DOI] [PubMed] [Google Scholar]
- 326. Miner B , Gill TM , Yaggi HK , et al . The epidemiology of patient-reported hypersomnia in persons with advanced age . J Am Geriatr Soc. 2019. ; 67 ( 12 ): 2545 – 2552 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327. Muller D , Paine SJ , Wu LJ , Signal TL . How long do preschoolers in Aotearoa/New Zealand sleep? Associations with ethnicity and socioeconomic position . Sleep Health. 2019. ; 5 ( 5 ): 452 – 458 . [DOI] [PubMed] [Google Scholar]
- 328. Nagata JM , Palar K , Gooding HC , et al . Food insecurity is associated with poorer mental health and sleep outcomes in young adults . J Adolesc Health. 2019. ; 65 ( 6 ): 805 – 811 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Nasim M , Saade M , AlBuhairan F . Sleep deprivation: prevalence and associated factors among adolescents in Saudi Arabia . Sleep Med. 2019. ; 53 : 165 – 171 . [DOI] [PubMed] [Google Scholar]
- 330. Peltzer K , Pengpid S . Prevalence, social and health correlates of insomnia among persons 15 years and older in Indonesia . Psychol Health Med. 2019. ; 24 ( 6 ): 757 – 768 . [DOI] [PubMed] [Google Scholar]
- 331. Pontes LDS , Prietsch SOM . Sleep bruxism: population based study in people with 18 years or more in the city of Rio Grande, Brazil . Rev Bras Epidemiol. 2019. ; 22 : e190038 . [DOI] [PubMed] [Google Scholar]
- 332. Poulain T , Vogel M , Sobek C , Hilbert A , Körner A , Kiess W . Associations between socio-economic status and child health: findings of a large German cohort study . Int J Environ Res Public Health. 2019. ; 16 ( 5 ): E677 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333. Redondo-Bravo L , Fernández-Alvira JM , Górriz J , et al . Does socioeconomic status influence the risk of subclinical atherosclerosis?: a mediation model . J Am Coll Cardiol. 2019. ; 74 ( 4 ): 526 – 535 . [DOI] [PubMed] [Google Scholar]
- 334. Ren Y , Liu Y , Meng T , et al . Social-biological influences on sleep duration among adult residents of Northeastern China . Health Qual Life Outcomes. 2019. ; 17 ( 1 ): 47 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335. Sheehan CM , Frochen SE , Walsemann KM , Ailshire JA . Are U.S. adults reporting less sleep?: findings from sleep duration trends in the National Health Interview Survey, 2004-2017 . Sleep. 2019. ; 42 ( 2 ): zsy221 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Singh EI , Vitzthum VJ . Community, household, and individual correlates of sleep behaviors in Guyanese female youth . Am J Hum Biol. 2019. ; 31 ( 5 ): e23291 . [DOI] [PubMed] [Google Scholar]
- 337. Sun J , Chen M , Cai W , et al . Chronotype: implications for sleep quality in medical students . Chronobiol Int. 2019. ; 36 ( 8 ): 1115 – 1123 . [DOI] [PubMed] [Google Scholar]
- 338. Talvitie E , Hintsanen M , Pulkki-Råback L , et al . Adverse childhood environment and self-reported sleep in adulthood: the Young Finns Study . Health psychol. 2019. ; 38 ( 8 ): 705 – 715 . [DOI] [PubMed] [Google Scholar]
- 339. Teo JX , Davila S , Yang C , et al . Digital phenotyping by consumer wearables identifies sleep-associated markers of cardiovascular disease risk and biological aging . Commun Biol. 2019. ; 2 ( 1 ): 361 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340. Vézina-Im LA , Lebel A , Gagnon P , Nicklas TA , Baranowski T . Individual correlates of sleep among childbearing age women in Canada . Behav Sleep Med. 2019. ; 17 ( 5 ): 634 – 645 . [DOI] [PubMed] [Google Scholar]
- 341. Wang Y , Li Y , Liu X , et al . Gender-specific prevalence of poor sleep quality and related factors in a Chinese rural population: the Henan Rural Cohort Study . Sleep Med. 2019. ; 54 : 134 – 141 . [DOI] [PubMed] [Google Scholar]
- 342. Wendt A , Costa CS , Machado AKF , et al . Sleep disturbances and daytime fatigue: data from the Brazilian National Health Survey, 2013 . Cad Saude Publica. 2019. ; 35 ( 3 ): e00086918 . [DOI] [PubMed] [Google Scholar]
- 343. Williamson AA , Mindell JA , Hiscock H , Quach J . Sleep problem trajectories and cumulative socio-ecological risks: birth to school-age . J Pediatr. 2019. ; 215 : 229 – 237.e4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344. Yao C , Fereshtehnejad S-M , Keezer MR , Wolfson C , Pelletier A , Postuma RB . Risk factors for possible REM sleep behavior disorder: a CLSA population-based cohort study . Neurology. 2018. ; 92 ( 5 ): e475 – e485 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345. Zhu G , Catt M , Cassidy S , et al . Objective sleep assessment in >80,000 UK mid-life adults: associations with sociodemographic characteristics, physical activity and caffeine . PLoS One. 2019. ; 14 ( 12 ): e0226220 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346. Chami HA , Ghandour B , Isma’eel H , Nasreddine L , Nasrallah M , Tamim H . Sleepless in Beirut: sleep duration and associated subjective sleep insufficiency, daytime fatigue, and sleep debt in an urban environment . Sleep Breath. 2020. ; 24 ( 1 ): 357 – 367 . [DOI] [PubMed] [Google Scholar]
- 347. Harding R , Haszard JJ , Schaughency E , Drummond B , Galland B . Parent report of children’s sleep disordered breathing symptoms and limited academic progress in reading, writing, and math . Sleep Med. 2020. ; 65 : 105 – 112 . [DOI] [PubMed] [Google Scholar]
- 348. Holstein BE , Ammitzbøll J , Damsgaard MT , Pant SW , Pedersen TP , Skovgaard AM . Difficulties falling asleep among adolescents: social inequality and time trends 1991-2018 . J Sleep Res. 2020. ; 29 ( 1 ): e12941 . [DOI] [PubMed] [Google Scholar]
- 349. Li N , Xu G , Chen G , Zheng X . Sleep quality among Chinese elderly people: a population-based study . Arch Gerontol Geriatr. 2020. ; 87 : 103968 . [DOI] [PubMed] [Google Scholar]
- 350. Metse AP , Bowman JA . Prevalence of self-reported suboptimal sleep in Australia and receipt of sleep care: results from the 2017 National Social Survey . Sleep Health. 2020. ; 6 ( 1 ): 100 – 109 . [DOI] [PubMed] [Google Scholar]
- 351. Seaton CL , Bottorff JL , Caperchione CM , Johnson ST , Oliffe JL . The association between men’s heath behaviors and interest in workplace health promotion . Workplace Health Saf. 2020. ; 68 ( 5 ): 226 – 235 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352. Sundbom F , Malinovschi A , Lindberg E , Almqvist C , Janson C . Insomnia symptoms and asthma control—interrelations and importance of comorbidities . Clin Exp Allergy. 2020. ; 50 ( 2 ): 170 – 177 . [DOI] [PubMed] [Google Scholar]
- 353. Tomaso CC , Nelson JM , Espy KA , Nelson TD . Associations between different components of executive control in childhood and sleep problems in early adolescence: a longitudinal study . J Health Psychol. 2020. ; 25 ( 13-14 ): 2440 – 2452 . [DOI] [PubMed] [Google Scholar]
- 354. Troxel WM , Haas A , Ghosh-Dastidar B , et al . Food insecurity is associated with objectively measured sleep problems . Behav Sleep Med. 2020. ; 18 ( 6 ): 719 – 729 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355. van de Straat V , Cheval B , Schmidt RE , et al . Early predictors of impaired sleep: a study on life course socioeconomic conditions and sleeping problems in older adults . Aging Ment Health. 2020. ; 24 ( 2 ): 322 – 332 . [DOI] [PubMed] [Google Scholar]
- 356. Visvalingam N , Sathish T , Soljak M , et al . Prevalence of and factors associated with poor sleep quality and short sleep in a working population in Singapore . Sleep Health. 2020. ; 6 ( 3 ): 277 – 287 . [DOI] [PubMed] [Google Scholar]
- 357. Wendt A , da Silva ICM , Gonçalves H , Assunção MCF , Menezes AMB , Wehrmeister FC . Sleep parameters measured by accelerometry: descriptive analyses from the 22-year follow-up of the Pelotas 1993 birth cohort . Sleep Med. 2020. ; 67 : 83 – 90 . [DOI] [PubMed] [Google Scholar]
- 358. Wu W , Jiang Y , Wang N , et al . Sleep quality of Shanghai residents: population-based cross-sectional study . Qual Life Res. 2020. ; 29 ( 4 ): 1055 – 1064 . [DOI] [PubMed] [Google Scholar]
- 359. Sarveswaran G , Arikrishnan K , Krishnamoorthy Y , Sakthivel M , Majella MG , Lakshminarayanan S . Prevalence and determinants of poor quality of sleep among adolescents in rural Puducherry, South India . Int J Adolesc Med Health. 2019. ; 33 ( 2 ): 20180101 . [DOI] [PubMed] [Google Scholar]
- 360. Zvolensky MJ , Kauffman BY , Bogiaizian D , Viana AG , Bakhshaie J , Peraza N . Worry among Latinx college students: relations to anxious arousal, social anxiety, general depression, and insomnia . J Am Coll Health. 2021. ; 69 ( 5 ): 529 – 536 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361. Irala-Estévez JD , Groth M , Johansson L , Oltersdorf U , Prättälä R , Martínez-González MA . A systematic review of socio-economic differences in food habits in Europe: consumption of fruit and vegetables . Eur J Clin Nutr. 2000. ; 54 ( 9 ): 706 – 714 . [DOI] [PubMed] [Google Scholar]
- 362. Stalsberg R , Pedersen AV . Effects of socioeconomic status on the physical activity in adolescents: a systematic review of the evidence . Scand J Med Sci Sports. 2010. ; 20 ( 3 ): 368 – 383 . [DOI] [PubMed] [Google Scholar]
- 363. Hiscock R , Bauld L , Amos A , Fidler JA , Munafò M . Socioeconomic status and smoking: a review . Ann N Y Acad Sci. 2012. ; 1248 ( 1 ): 107 – 123 . [DOI] [PubMed] [Google Scholar]
- 364. Wiles NJ , Lingford-Hughes A , Daniel J , et al . Socio-economic status in childhood and later alcohol use: a systematic review . Addiction. 2007. ; 102 ( 10 ): 1546 – 1563 . [DOI] [PubMed] [Google Scholar]
- 365. Colhoun HM , Hemingway H , Poulter NR . Socio-economic status and blood pressure: an overview analysis . J Hum Hypertens. 1998. ; 12 ( 2 ): 91 – 110 . [DOI] [PubMed] [Google Scholar]
- 366. McLaren L . Socioeconomic status and obesity . Epidemiol Rev. 2007. ; 29 ( 1 ): 29 – 48 . [DOI] [PubMed] [Google Scholar]
- 367. Dowd JB , Simanek AM , Aiello AE . Socio-economic status, cortisol and allostatic load: a review of the literature . Int J Epidemiol. 2009. ; 38 ( 5 ): 1297 – 1309 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368. Clark AM , DesMeules M , Luo W , Duncan AS , Wielgosz A . Socioeconomic status and cardiovascular disease: risks and implications for care . Nat Rev Cardiol. 2009. ; 6 ( 11 ): 712 – 722 . [DOI] [PubMed] [Google Scholar]
- 369. Agardh E , Allebeck P , Hallqvist J , Moradi T , Sidorchuk A . Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis . Int J Epidemiol. 2011. ; 40 ( 3 ): 804 – 818 . [DOI] [PubMed] [Google Scholar]
- 370. Reiss F . Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review . Soc Sci Med. 2013. ; 90 ( 90 ): 24 – 31 . [DOI] [PubMed] [Google Scholar]
- 371. Galobardes B , Lynch JW , Smith GD . Is the association between childhood socioeconomic circumstances and cause-specific mortality established? Update of a systematic review . J Epidemiol Community Health. 2008. ; 62 ( 5 ): 387 – 390 . [DOI] [PubMed] [Google Scholar]
- 372. Pampel FC , Krueger PM , Denney JT . Socioeconomic disparities in health behaviors . Annu Rev Sociol. 2010. ; 36 ( 1 ): 349 – 370 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373. Grandner MA . Sleep, health, and society . Sleep Med Clin. 2020. ; 15 ( 2 ): 319 – 340 . [DOI] [PubMed] [Google Scholar]
- 374. Linton SJ , Kecklund G , Franklin KA , et al . The effect of the work environment on future sleep disturbances: a systematic review . Sleep Med Rev. 2015. ; 23 : 10 – 19 . [DOI] [PubMed] [Google Scholar]
- 375. Magee C , Gopaldasani V , Bakand S , Coman R . The physical work environment and sleep: a latent class analysis . J Occup Environ Med. 2019. ; 61 ( 12 ): 1011 – 1018 . [DOI] [PubMed] [Google Scholar]
- 376. Boivin DB , Boudreau P . Impacts of shift work on sleep and circadian rhythms . Pathol Biol (Paris). 2014. ; 62 ( 5 ): 292 – 301 . [DOI] [PubMed] [Google Scholar]
- 377. Johnson DA , Billings ME , Hale L . Environmental determinants of insufficient sleep and sleep disorders: implications for population health . Curr Epidemiol Rep. 2018. ; 5 ( 2 ): 61 – 69 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378. Troxel WM , DeSantis A , Richardson AS , et al . Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration . Sleep. 2018. ; 41 ( 10 ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379. Ruggiero AR , Peach HD , Gaultney JF . Association of sleep attitudes with sleep hygiene, duration, and quality: a survey exploration of the moderating effect of age, gender, race, and perceived socioeconomic status . Health Psychol Behav Med. 2019. ; 7 ( 1 ): 19 – 44 . [DOI] [PMC free article] [PubMed] [Google Scholar]