Abstract
Background
The latest wave of the coronavirus disease 2019 (COVID-19) pandemic in Macau began on 18 June 2022 and was more serious than previous waves. Ensuing disruption from the wave is likely to have had a variety of negative mental health consequences for Macau residents including increased risk for insomnia. This study investigated the prevalence and correlates of insomnia among Macau residents during this wave as well as its association with quality of life (QoL) from a network analysis perspective.
Methods
A cross-sectional study was conducted between 26 July and 9 September 2022. Univariate and multivariate analyses explored correlates of insomnia. Analysis of covariance (ANCOVA) examined the relationship between insomnia and QoL. Network analysis assessed the structure of insomnia including “Expected influence” to identify central symptoms in the network, and the flow function to identify specific symptoms that were directly associated with QoL. Network stability was examined using a case-dropping bootstrap procedure.
Results
A total of 1,008 Macau residents were included in this study. The overall prevalence of insomnia was 49.0% (n = 494; 95% CI = 45.9–52.1%). A binary logistic regression analysis indicated people with insomnia were more likely to report depression (OR = 1.237; P < 0.001) and anxiety symptoms (OR = 1.119; P < 0.001), as well as being quarantined during the COVID-19 pandemic (OR = 1.172; P = 0.034). An ANCOVA found people with insomnia had lower QoL (F(1,1,008) = 17.45, P < 0.001). “Sleep maintenance” (ISI2), “Distress caused by the sleep difficulties” (ISI7) and “Interference with daytime functioning” (ISI5) were the most central symptoms in the insomnia network model, while “Sleep dissatisfaction” (ISI4), “Interference with daytime functioning” (ISI5), and “Distress caused by the sleep difficulties” (ISI7) had the strongest negative associations with QoL.
Conclusion
The high prevalence of insomnia among Macau residents during the COVID-19 pandemic warrants attention. Being quarantined during the pandemic and having psychiatric problems were correlates of insomnia. Future research should target central symptoms and symptoms linked to QoL observed in our network models to improve insomnia and QoL.
Keywords: insomnia, quality of life, COVID-19 outbreak, prevalence, network analysis
1. Introduction
Since 2019, Coronavirus Disease 2019 (COVID-19) has been a constant threat that affects daily lives. Repeated and sporadic outbreaks of COVID-19 have brought unprecedented challenges worldwide. The Macau Special Administrative Region of China (Macao SAR) has had a unique geo-political position in the context of COVID-19 due to its heavy reliance upon mainland Chinese visitation and gambling revenues to support the local economy (1, 2). The latest wave of the COVID-19 pandemic in Macau occurred from 18 June to 7 August 2022. Labeled as the “618” pandemic, this wave resulted in the largest number of confirmed cases in the history of Macau, with 705 (38.7%) new confirmed cases and 1,116 (61.3%) asymptomatic infection cases (3). In response, the Macau SAR government took immediate, active, progressive measures that included temporary shut-down of entry/exit to mainland China, suspension of business and public institution operations (e.g., casinos, schools, construction sites), and self-isolation to maintain “relative static management” for 12 days from 11 July 2022 (3). The estimated number of visitors from mainland China decreased sharply from 336,488 in June, 2022 to 7,321 in July 2022 (4). A high perceived contagion risk during the wave increased negative emotions and curtailed willingness to travel (5). Additionally, ongoing border restrictions during the entire COVID-19 pandemic have restricted the flow of domestic and foreign tourists with devastating effects on the economy of Macau (6). Macau SAR has followed the “dynamic zero-COVID” prevention policy of mainland China that had been remarkably effective in minimizing the spread of COVID-19 (7, 8) but was accompanied by increases in potentially chronic psychological problems (9), such as depression, anxiety, and insomnia (10, 11).
One of the most common behavioral health consequences of COVID-19 and the dynamic zero policy has been insomnia, which is the most common sleep disorder and is characterized by difficulty initiating or maintaining sleep, accompanied by daytime impairments in functioning (12, 13). Insomnia is a risk factor for progression to or exacerbations of other physical and psychiatric disorders in addition to broader costs to social life and healthcare (13). Insomnia has also been a widespread health that poses significant challenges for prevention and treatment during the COVID-19 pandemic (14). A previous insomnia study revealed a pooled prevalence of 11.3% with significant differences across 13 countries before the COVID-19 pandemic (15). However, the rate of insomnia symptoms was up to 36.7% in a large multi-center survey conducted during the COVID-19 pandemic (16). During the initial COVID-19 outbreak, the insomnia rate among Macau residents was as high as 27.6% (17). However, given the increased severity of the most recent wave, the prevalence of insomnia in Macau should be re-estimated.
A variety of factors can contribute to insomnia amid pandemic conditions including concerns about infection and the rapidly increasing number of cases (18), social isolation or lockdown (19), and stress from economic hardships (14). Insomnia has been described as both a symptom and a sign of increased psychiatric morbidity, especially in relation to depression and anxiety disorders (15, 20). Sociodemographic correlates of insomnia have also been documented, though results are sometimes discrepant. For example, some studies suggested younger adults have more severe insomnia symptoms (21, 22) while other research has found insomnia is more common among older adults (15, 23). In addition, due to its potential chronicity, insomnia is associated with substantial impairments in quality of life (QoL) (15, 20, 24) and such losses are often an impetus for seeking treatment (25). However, to date, there has been an absence of studies on relevant correlates of insomnia among Macau residents or the nature of its links with QoL during this latest serious COVID-19 wave.
Network analysis (NA) provides a new perspective for exploring psychiatric problems that are conceptualized as causally linked symptom systems (26). A network is comprised of nodes that represent symptoms of a particular syndrome and edges that represent intercorrelations between symptoms (27). NA offers insight into how symptoms of a syndrome are interconnected and can be used to identify the most central or influential symptoms of a syndrome that can be prioritized as specific targets for interventions (28). NA has been applied widely to multiple psychiatric disorders among various subpopulations during the COVID-19 pandemic (29–31). A previous network model of insomnia symptoms among mental health professionals suggested that “interference with daytime functioning” was the most influential symptom (29). However, to date, no studies have focused on insomnia symptoms or their links with QoL among Macau residents during the recent 618 COVID-19 wave.
To address these gaps, this study (1) investigated the prevalence and correlates of insomnia among Macau residents during the “618” COVID-19 waves, (2) examined the most central symptoms within the network model of insomnia, and (3) evaluated relations between particular insomnia symptoms and QoL in the sample. We hypothesized that insomnia would be common and negatively associated with QoL among Macau residents in this wave.
2. Materials and methods
2.1. Participants and procedure
This cross-sectional study was conducted between 26 July and 9 September 2022 in Macau, China using a snowball sampling method. Due to lockdowns and the potential risk of infection during the wave, face-to-face interviews could not be performed. Following previous studies (17, 31–33), the study was conducted online using snowball convenience sampling and participants were invited to participate in this survey on reactions to COVID-19 using a Quick Response code (QR code) through advertisements in major social network platforms (specifically: WeChat, Facebook, and Instagram). The QR linked to an invitation and questionnaires. Inclusion criteria were as follows: (1) Residents who lived in Macau during the recent 618 COVID-19 wave; (2) aged 18 years or above; (3) able to understand the purposes and content of the survey. There were no specific exclusion criteria for this study. All participants provided electronic written informed consent on a voluntary and confidential basis. This study protocol was approved by the Institutional Review Board (IRB) of the University of Macau.
2.2. Measures
Basic socio-demographic information was collected including age, gender, marital status, living status, education level, and employment status during the COVID-19 pandemic. Additionally, several variables related to COVID-19 were measured, including concern about COVID-19, status as being quarantined during the COVID-19 pandemic, worry about COVID-19 infection, level of economic loss due to the COVID-19 pandemic, monthly income, regular physical exercise during the pandemic, presence of chronic physical illnesses, history of psychiatric disorders, and suicidality during the COVID-19 outbreak.
Insomnia symptoms were assessed with the validated Chinese version of the Insomnia Severity Index (ISI) questionnaire (34, 35), which consisted of seven items that assessed (1) severity of sleep onset problem; (2) sleep maintenance problem; (3) early morning wakening problem; (4) sleep dissatisfaction; (5) interference of sleep difficulties with daytime functioning; (6) noticeability of sleep problems by others, and (7) distress caused by sleep difficulties. Each item was rated on a 5-point Likert scale from “0” (no problem) to “4”(very severe problem). Total ISI scores ranged from 0 to 28, with a higher score indicating more severe insomnia symptoms. Following previous studies, a total score of ≥ 8 was considered as “having insomnia symptoms.” More specifically, a score between 8 and 14 was defined as “subthreshold insomnia,” a score between 15 and 21 was defined as clinical insomnia (moderate severity), and a score between 22 and 28 was defined as clinical insomnia (severe) (36, 37). The Chinese version of ISI had good reliability and validity in Chinese populations (38, 39).
Depressive symptoms were measured with the validated Chinese version of the nine-item Patient Health Questionnaire (PHQ-9) (40, 41). Each item was rated on a 4-point frequency scale from “0” (not at all) to “3”(nearly every day); total scores ranged from 0 to 27, with higher values indicating more severe depressive symptoms. Anxiety symptoms were measured with the validated Chinese version of the seven-item Generalized Anxiety Disorder scale (GAD-7) (42, 43). Each item was scored on a 4-point frequency scale from “0” (not at all) to “3”(nearly every day). Total scores ranged from 0 to 21 with higher overall scores indicating more severe anxiety symptoms. Global quality of life (QoL) was assessed by summing scores on the first two items on the Chinese version of the World Health Organization Quality of Life-Brief Version (WHOQOL-BREF) (44–46); a higher total score reflected better QoL.
2.3. Statistical analysis
2.3.1. Univariate and multivariate analyses
Univariate and multivariate analyses were performed using SPSS version 26.0 (SPSS Inc., Chicago, Illinois, USA). Normality distributions of continuous variables were assessed using one-sample Kolmogorov-Smirnov tests and P-P plots. Comparisons of demographic and clinical variables including COVID-19-related variables between subgroups with and without insomnia symptoms were conducted using independent sample t-tests or Mann-Whitney U tests for continuous variables and Chi-square tests for categorical variables, as appropriate. Analysis of covariance (ANCOVA) was used to compare QoL between subgroups with and without insomnia symptoms after controlling for variables that had significant differences in univariate analyses. A standard binary logistic regression analysis was performed to examine independent correlates of insomnia status. Having insomnia symptoms was the dependent variable; measures on which there were significant group differences in univariate analyses were entered as independent variables. Significant statistical differences were set at P < 0.05 (two-tailed).
2.3.2. Network structure
A network analysis was conducted using R software (47). In the insomnia network structure, nodes represented individual insomnia symptoms and edges represented the correlations between symptoms. Thicker edges represented stronger correlations, with green edges indicating positive correlations and red indicating negative correlations. To assess associations between different insomnia symptoms in the network model, a Graphical Gaussian Model (GGM) with graphic least absolute shrinkage and selection operator (LASSO) and an Extended Bayesian Information Criterion (EBIC) model were applied (48) to improve the accuracy of prediction, simplicity and interpretability of the network model (49). Network estimation was assessed using the “estimateNetwork” function in R “bootnet” with “EBICglasso” as the default method and the “qgraph” package for visualization (48). The “ggplot2” package was used for optimize visualization of the network (48, 50). Expected Influence (EI) was used to determine central symptoms in the network model in light of its reliability as a centrality index (51). Predictability was assessed using the “mgm” package (52) to calculate the variance in a node that could be explained by neighboring nodes in the network model (31). In addition, the “flow” function in R package “qgraph” was adopted to identify particular insomnia symptoms that were directly associated with QoL (53).
Stability and accuracy of the network model were evaluated using the R-package, “bootnet” (Version 1.4.3) (48). Stability was examined using the correlation stability coefficient (CS-coefficient), which calculates the maximum proportion of dropped cases to maintain a correlation above 0.7 between the centrality indices of the original sample and those of subset samples with a 95% probability (48). Following previous studies (17, 49), a CS-coefficient value above 0.25 was viewed as an acceptable stable network model, though 0.5 was preferable. Edge accuracy was estimated using bootstrapped 95% confidence intervals (CIs), with a narrower CI suggesting a more trustworthy network (48). A non-parametric bootstrapped difference test was performed to evaluate differences between edges pairs (48).
3. Results
3.1. Participant characteristics
A total of 1,020 Macau residents were invited to participate in this study, of whom 1,008 met entry criteria and completed the assessment for a participation rate of 98.82%. Demographic and clinical characteristics of the sample are shown in Table 1. The mean age of participants was 34.8 years (SD = 11.5 years) and 26.7% (n = 269) were male. Most participants had an education of college level or above (n = 831; 82.4%) and lived with other people (n = 935; 92.8%).
TABLE 1.
Demographic characteristics of the study sample (N = 1,008).
| Measure | Total (N = 1,008) | Without insomnia (N = 514) | With insomnia (N = 494) | Univariable analysis | |||||
| n | % | n | % | n | % | χ2 | df | p | |
| Male | 269 | 26.7 | 131 | 25.5 | 138 | 27.9 | 0.772 | 1 | 0.380 |
| Married | 471 | 46.7 | 254 | 49.4 | 217 | 43.9 | 3.049 | 1 | 0.081 |
| Living with others | 935 | 92.8 | 478 | 93.0 | 457 | 92.5 | 0.089 | 1 | 0.766 |
| College and above education | 831 | 82.4 | 433 | 84.2 | 398 | 80.6 | 2.349 | 1 | 0.125 |
| Employed during the COVID-19 pandemic | 687 | 68.2 | 349 | 67.9 | 338 | 68.4 | 0.032 | 1 | 0.859 |
| Very concern about the COVID-19 pandemic | 764 | 75.8 | 377 | 73.3 | 387 | 78.3 | 3.424 | 1 | 0.064 |
| Being quarantined during the COVID-19 pandemic | 109 | 10.8 | 41 | 8.0 | 68 | 13.8 | 8.752 | 1 | 0.003 |
| Worried about COVID-19 infection | 12.843 | 2 | 0.002 | ||||||
| No worry | 396 | 39.3 | 218 | 42.4 | 178 | 36.0 | |||
| Worried | 462 | 45.8 | 239 | 46.5 | 223 | 45.1 | |||
| Very worried | 150 | 14.9 | 57 | 11.1 | 93 | 18.8 | |||
| Economic loss | 70.528 | 2 | <0.001 | ||||||
| Noor minimal | 370 | 36.7 | 236 | 45.9 | 134 | 27.1 | |||
| Fair | 405 | 40.2 | 211 | 41.1 | 194 | 39.3 | |||
| Very much | 233 | 23.1 | 67 | 13.0 | 166 | 33.6 | |||
| Monthly income (≥MOP 30,000) | 381 | 37.8 | 213 | 41.4 | 168 | 34.0 | 5.917 | 1 | 0.015 |
| Physical exercise during the pandemic (≥30 min/day) | 471 | 46.7 | 256 | 49.8 | 215 | 43.5 | 3.995 | 1 | 0.046 |
| Presence of chronic physical diseases | 34 | 3.4 | 14 | 2.7 | 20 | 4.0 | 1.357 | 1 | 0.244 |
| Having a history of psychiatric disorders | 58 | 5.8 | 11 | 2.1 | 47 | 9.5 | 25.259 | 1 | 0.001 |
| Any suicidality during the latest COVID-19 outbreak | 90 | 8.9 | 13 | 2.5 | 77 | 15.6 | 52.821 | 1 | <0.001 |
| Mean | SD | Mean | SD | Mean | SD | Z | df | p | |
| Age (years) | 34.85 | 11.517 | 35.54 | 12.027 | 34.13 | 10.927 | −1.428 | —* | 0.153 |
| PHQ-9 total | 7.32 | 6.058 | 4.15 | 3.843 | 10.61 | 6.187 | −18.204 | —* | <0.001 |
| GAD-7 total | 5.33 | 5.189 | 2.82 | 3.33 | 7.94 | 5.48 | −16.534 | —* | <0.001 |
| Global quality of life | 6.07 | 1.47 | 6.66 | 1.324 | 5.46 | 1.367 | −13.462 | —* | <0.001 |
Bolded values: <0.05. df, degree of freedom; PHQ-9, Patient Health Questionnaire-9 items; GAD-7, Generalized Anxiety Disorder-7 items; SD, standard deviation. 1 USD = 8.078 MOP; *Mann-Whitney U test.
3.2. Prevalence and correlates of insomnia
The overall prevalence of insomnia (ISI-7 total score ≥ 8) was 49.0% (n = 494; 95% CI = 45.9–52.1%). With respect to severity levels, 303 (30.1%) reported subthreshold insomnia, 147 (14.6%) reported moderate insomnia, and 44 (4.4%) reported severe insomnia. Table 1 summarizes differences between subgroups with and without insomnia. People with insomnia were more likely to be quarantined during the COVID-19 pandemic (P = 0.003), more worried about COVID-19 infection (P = 0.002), experienced economic losses during the COVID-19 pandemic (P < 0.001), have history of psychiatric disorders (P < 0.001), experience suicidality during the COVID-19 outbreak (P < 0.001), more likely to report having a lower monthly income (MOP < 30,000) (P = 0.015) and report less than 30 min of physical exercise every day during the pandemic (P = 0.046) when compared to people without insomnia. Additionally, those with insomnia reported higher mean levels of depression (PHQ-9) (P < 0.001) and anxiety (GAD-7) (P < 0.001) as well as a lower mean QoL score (P < 0.001).
After controlling for variables on which there were significant group differences in univariate analyses, the insomnia subgroup still had a lower QoL score (F(1,1,008) = 17.450, P < 0.001) than did the no insomnia subgroup. The logistic regression analysis revealed that people with insomnia were comparatively more likely to report depression (OR = 1.237; P < 0.001), anxiety symptoms (OR = 1.119; P < 0.001), and being quarantined during the COVID-19 pandemic (OR = 1.172; P = 0.034) (see Table 2).
TABLE 2.
Independent correlates of insomnia among Macau residents during the COVID-19 pandemic (N = 1,008).
| Measure | Multiple logistic regression analysis | ||
| p | OR | 95% CI | |
| Being quarantined during the COVID-19 pandemic | 0.034 | 1.172 | 1.043–2.811 |
| Worried about COVID-19 infection | |||
| No worry | - | – | – |
| Worried | 0.161 | 1.269 | 0.910–1.769 |
| Very worried | 0.739 | 0.918 | 0.556–1.517 |
| Economic loss | |||
| No or minimal | - | – | – |
| Fair | 0.300 | 1.199 | 0.851–1.690 |
| Very much | 0.065 | 1.537 | 0.973–2.428 |
| Monthly income (≥MOP 30,000) | 0.594 | 1.092 | 0.789–1.512 |
| Physical exercise during the pandemic (≥30 min/day) | 0.460 | 1.124 | 0.825–1.532 |
| Having a history of psychiatric disorders | 0.753 | 1.142 | 0.499–2.612 |
| Any suidality during the latest COVID-19 outbreak | 0.952 | 1.024 | 0.468–2.242 |
| PHQ-9 total | <0.001 | 1.237 | 1.174–1.303 |
| GAD-7 total | <0.001 | 1.119 | 1.059–1.184 |
Bolded values: <0.05. CI, confidence interval; OR, odds ratio.
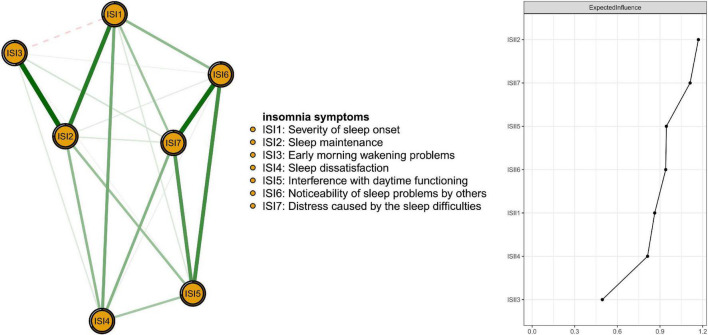
3.3. Network structure of insomnia symptoms
Figure 1 presents the network structure of insomnia symptoms as measured by ISI items. The three nodes with the highest centrality were ISI2 (“Sleep maintenance problems”), ISI7 (“Distress caused by the sleep difficulties”), and ISI5 (“Interference with daytime functioning”). The mean predictability was 0.696, indicating an average of 69.6% of the variance in each node could be accounted for by its neighboring nodes in the model. Descriptive information and network centrality indices of each insomnia symptom are shown in Supplementary Table 1.
FIGURE 1.
Network structure of insomnia symptoms among Macau residents during the COVID-19 pandemic.
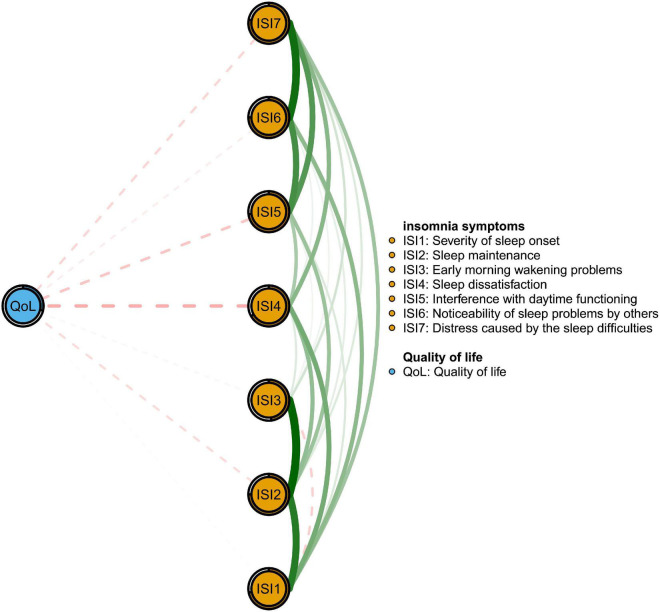
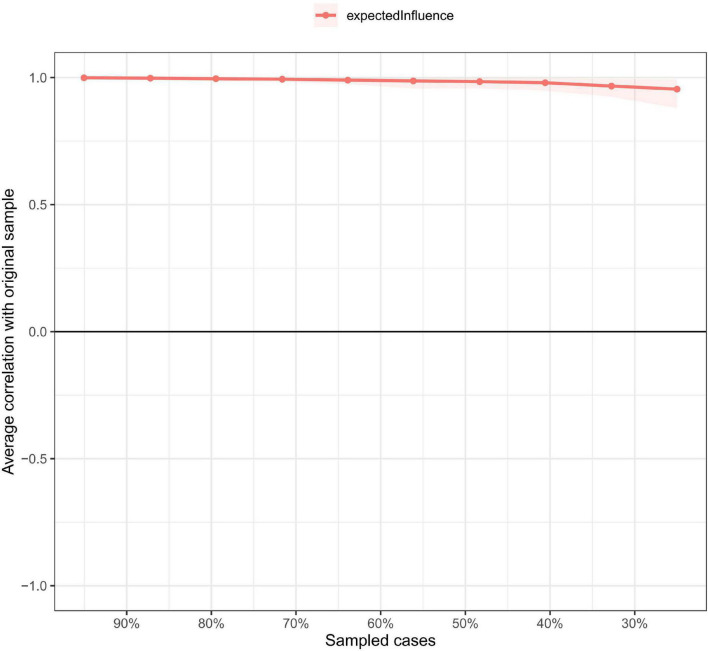
Figure 2 shows that ISI4 (“Sleep dissatisfaction”; average edge weight = −0.13) had the strongest negative association with QoL, followed by ISI5 (“Interference with daytime functioning”; average edge weight = −0.09) and ISI7 (“Distress caused by the sleep difficulties”; average edge weight = −0.06). Figure 3 presents network stability results. The CS-C of EI was 0.75 based on the case-dropping bootstrap procedure, indicating that the network model was stable. For the accuracy of the network, bootstrap 95% CIs for estimated edge weights showed a narrow range (see Supplementary Figure 1); most of the edge weights were non-zero, suggesting that a majority of edges were stable and accurate. Bootstrapped difference tests for edge weights showed that most comparisons among edge weights were statistically significant, underscoring how the network model was reliable (Supplementary Figure 2).
FIGURE 2.
Flow network of quality of life and insomnia symptoms.
FIGURE 3.
Network stability of insomnia symptoms among Macau residents during the COVID-19 pandemic.
4. Discussion
This was the first study to explore the epidemiology, correlates, and network structure of insomnia and its links with QoL among Macau residents shortly after the 618 COVID-19 wave.
Overall, the prevalence of insomnia was 49% (95% CI: 45.9–52.1%). Notably, this was much higher than the previous rate (27.6%; 95% CI: 24.8–30.4%) found among Macau residents during the first wave of the COVID-19 pandemic (17); as such, this finding suggests there may have been an exacerbation of sleep disturbances in this community. In addition, this rate exceeds rates reported in studies on the general population of mainland China (24.7%) (54), healthcare workers (34⋅3%; 95% CI: 27.5–41.5%) (55) and COVID-19 survivors (26.5%) (56). The high current rate in Macau may be due, in part, to the rapid and extensive transmission of the virus during this wave, the associated lockdown of most residents for the first time in over 2 years since the pandemic onset, and the suspension of daily activities. Together, these influences likely contributed to increased stress responses and disturbances in the sleep habits of many residents (57). One previous study has also found the severity of the pandemic and lockdown policies in Chinese cities are related to significant increases in rates of insomnia (58).
We also explored the network structure of insomnia at the symptom level in the sample. The node, “Sleep maintenance problems” (ISI2) was the most central symptom in the insomnia network model and indicated difficulties maintaining sleep (e.g., not sleeping well at night and waking up frequently) had the strongest connections with other symptoms in the insomnia network. Other influential nodes included “Distress caused by sleep difficulties” (ISI7), tapping residents’ worry/distress about current sleep problems, and “Interference with daytime functioning” (ISI5) due to insomnia. These findings align with a previous insomnia network model study in which “Interference with daytime functioning” (ISI5), “sleep maintenance” (ISI2), and “Distress caused by the sleep difficulties” (ISI7) were the most central symptoms of mental health professionals in China (29). Across both samples, these symptoms were most influential within insomnia network models and were more likely to predict insomnia than more peripheral symptoms (59). As such, concerns with sleep maintenance, distress caused by sleep problems and inference with daily functioning should be targeted for insomnia interventions while reductions of these symptoms may be key markers of treatment success. Furthermore, much of the variance of individual insomnia symptoms could be explained by this network model with an average predictability of 69.6%. This finding underscores strong inter-correlations between insomnia symptoms in this sample. The remaining variance may be attributed, in part, to other psychiatric disturbances related to insomnia, such as depression and anxiety (17).
Several correlates of insomnia among Macau residents also emerged in the study. Notably, people who were quarantined during this COVID-19 pandemic were more likely to suffer from insomnia, consistent with previous studies (57, 60). Although quarantine is an effective strategy for controlling transmission of the virus (61), it also limits resident zones of activity, usual routines and autonomy; such losses are related to negative mental health outcomes including depression, anxiety, insomnia, and suicidality (62). Previous studies have contended that stress induced by COVID-19 may lead to elevated levels of inflammation in socially isolated populations and result in mood and sleep disturbances (57). Long-time exposure to social media during isolation or quarantine could also disrupt the circadian rhythms of quarantined persons (63).
In addition, insomnia had significant positive correlations with depressive and anxiety symptoms in the sample. Previous evidence suggests that people with mood disorders and anxiety disorders have 3.3-fold and 2.6-fold risks, respectively, for developing insomnia compared to non-diagnosed controls (15). In another cross-sectional study, depression was more strongly related to sleep initiation difficulties while anxiety was more strongly linked to difficulty maintaining sleep (64). Close relations between these psychiatric disorders and insomnia may be due to overlapping neurobiology (65, 66) and psychosocial stressors that affect both sleep and emotional status (67). During this COVID-19 wave, the rising number of confirmed cases, continual dissemination in the daily news and mandated daily nucleic acid testing and/or rapid antigen self-testing might have exacerbated depression, anxiety symptoms, and insomnia (68).
In one recent depression-anxiety-insomnia network model study conducted during the pandemic, “sleep problems” emerged as a bridge symptom (17) linking these three psychiatric disorders. Indeed, possible bidirectional relations of anxiety and depression with insomnia are widely accepted and negative spirals in one or more of these disturbances could contribute to exacerbations in symptoms of other syndromes (15, 69, 70). From this perspective, interventions to alleviate insomnia problems such as cognitive behavioral therapy may help to address both sleep disturbances and comorbid disorders (71).
Concerning sociodemographic correlates of insomnia, neither age nor gender was significant. Previous studies reported women (15) and younger adults (72) were more likely to have insomnia symptoms. The discrepancy with past work may have reflected similar responses to the COVID-19 wave among different demographic groups or the larger proportion of women (73.3%) and young age (mean age = 34.8 years) of this sample. Insomnia was not significantly associated with regular physical exercise in the multivariate model for this sample in contrast to pre-pandemic evidence of a negative association (73). The null association in this study may have been a partial function of confinement and reduced opportunities for exercise among most residents during the “618” COVID-19 waves.
Economic losses and lower-income levels were associated with insomnia symptoms in univariate analyses but did not make unique contributions within the multivariate prediction model. Although previous studies have reported significant links between financial burdens and the severity of insomnia (74, 75), the relatively high level of economic security in Macau SAR may have had buffering effects. Despite significant economic losses from the COVID-19 pandemic, the gross domestic product (GDP) per capita in Macau versus mainland China (US$ 45,421.6 versus US$12,556.3) remained relatively high in the region and ranked 31st in the world (76). The Macau SAR government also launched targeted financial support programs to promote economic recovery and guarantee free distribution of anti-epidemic supplies (e.g., KN95 masks and self-test COVID-19 antigen kits) for residents (8). These measures may have provided some relief from economic pressure. In addition, associations between economic factors and other correlates of insomnia status (depressive and anxiety symptoms) may have attenuated unique contributions of economic correlates in the multivariate prediction model.
The negative relationship between insomnia and QoL observed here has been found in other studies (77–79). In the flow network model, insomnia symptoms of “Sleep dissatisfaction” (ISI4), “Interference with daytime functioning” (ISI5) and “Distress caused by sleep difficulties” (ISI7) had the strongest, most direct negative associations with QoL and are plausible targets for reducing insomnia and improving QoL. Previous research suggests that sleep dissatisfaction is a significant predictor of sleep disorder severity among people with insomnia (80) and is regarded as a key indicator of sleep quality (81). Poor sleep quality (e.g., insufficient sleep) corresponds to poor physical or mental health outcomes including high blood pressure (82), cardiovascular diseases (83), depression (84) and suicidal behavior (85). In addition, poor sleep can deplete energy during the daytime and interfere with the daily functioning of samples assessed during the pandemic (77, 86). Maintaining a daily routine (e.g., work or studying) may play an important role in maintaining QoL (87). Furthermore, distress caused by insomnia such as nervousness or negative mood, and fatigue could affect perceived QoL (79). Once again, interventions to increase satisfaction with sleep also provide a viable pathway for improving QoL among insomnia sufferers.
The merits of this study included its large sample size and use of network analysis to pinpoint central symptoms of insomnia and those having stronger links to QOL. The main limitations should be acknowledged as well. First, this was a non-experimental, cross-sectional study, so causal relations between insomnia and other factors could not be drawn. Second, this study was conducted in Macau SAR, so results may be not representative of other regions due to different COVID-19 trajectories and policies. Third, to reduce the possibility of COVID-19 infection, an online survey based on snowball sampling was conducted; as a result, the representativeness and generalizability of results may have been reduced due to selection biases. Thus, the random sampling method should be used in future studies. Fourth, some factors related to insomnia, such as occupation and social support, were not recorded. More relevant variables should be included in future studies. Finally, because the assessment was based on self-reports, biases in recall and social desirability could not be controlled.
In conclusion, the comparatively high prevalence of insomnia among Macau residents during the recent COVID-19 wave and its association with poor QoL warrant attention. Being quarantined during the wave and concurrent elevations in symptoms of depression and anxiety were significant, unique correlates of insomnia. “Sleep maintenance” (ISI2) was the most central symptom in the network model of insomnia, while “Sleep dissatisfaction” (ISI4) had the strongest relationship with poor QoL. Future interventions should prioritize reducing problems in sleep maintenance as a means of improving insomnia and QoL.
Data availability statement
The datasets presented in this article are not readily available because the Institutional Review Board (IRB) of the University of Macau that approved the study prohibits the authors from making publicly available the research dataset of clinical studies. Requests to access the datasets should be directed to Y-TX, xyutly@gmail.com.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board (IRB) of the University of Macau. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LZ, SS, YF, and Y-TX: study design. PC, ML, K-IL, IC, TS, ZS, and TC: data collection, analysis, and interpretation. PC and Y-TX: drafting of the manuscript. TJ: critical revision of the manuscript. All authors approved the final version for publication.
Acknowledgments
The authors are grateful to all participants and clinicians involved in this study.
Funding Statement
This study was supported by the University of Macau (MYRG2019-00066-FHS and MYRG2022-00187-FHS), Sci-Tech Innovation 2030 – Major Project of Brain Science and Brain-Inspired Intelligence Technology (2021ZD0200600), Beijing Scholar 2021 (No. 063), and Beijing Hospitals Authority Clinical Medicine Development of Special Funding Support (XMLX202128).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1113122/full#supplementary-material
References
- 1.McCartney G. The impact of the coronavirus outbreak on Macao. From tourism lockdown to tourism recovery. Curr Issues Tour. (2021) 24:2683–92. 10.1080/13683500.2020.1762549 [DOI] [Google Scholar]
- 2.Blaschke B. Macau Raises 2019 Gaming Tax Budget by 12.9% to Almost mop $100 Billion. London: International Airlines Group; (2019). [Google Scholar]
- 3.Portal do Governo da Região Administrativa Especial de Macau da República Popular da China. Report on the Macao SAR Government’s Response to the “618” Pandemic. Washington, DC: Portal do Governo da Região Administrativa Especial de Macau da República Popular da China; (2022). [Google Scholar]
- 4.Macao Statistics and Census Department. Visitor arrivals. Washington, D.C: Macao Statistics and Census Department; (2022). [Google Scholar]
- 5.Agyeiwaah E, Adam I, Dayour F, Badu Baiden F. Perceived impacts of COVID-19 on risk perceptions, emotions, and travel intentions: evidence from Macau higher educational institutions. Tour Recreat Res. (2021) 46:195–211. 10.1080/02508281.2021.1872263 [DOI] [Google Scholar]
- 6.Lai I, Wong J. Comparing crisis management practices in the hotel industry between initial and pandemic stages of COVID-19. Int J Contemp Hosp Manage. (2020) 32:3135–56. 10.1108/IJCHM-04-2020-0325 [DOI] [Google Scholar]
- 7.Liu J, Liu M, Liang W. The dynamic COVID-Zero strategy in China. China CDC Wkly. (2022) 4:74–5. 10.46234/ccdcw2022.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao Y, Xu J, Bai W, Sun H, Shui B, Yang Z, et al. COVID-19 prevention and control strategies: learning from the Macau model. Int J Biol Sci. (2022) 18:5317–28. 10.7150/ijbs.70177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bai W, Sha S, Cheung T, Su Z, Jackson T, Xiang Y. Optimizing the dynamic zero-COVID policy in China. Int J Biol Sci. (2022) 18:5314–6. 10.7150/ijbs.75699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vindegaard N, Benros M. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immunity. (2020) 89:531–42. 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar A, Nayar K. COVID 19 and its mental health consequences. J Ment Health. (2021) 30:1–2. 10.1080/09638237.2020.1757052 [DOI] [PubMed] [Google Scholar]
- 12.Burman D. Sleep disorders: insomnia. FP Essent. (2017) 460:22–8. [PubMed] [Google Scholar]
- 13.Buysse D. Insomnia. JAMA. (2013) 309:706–16. 10.1001/jama.2013.193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheshmehzangi A, Chen H, Su Z, Zou T, Xiang Y, Dawodu A. How does the COVID-19 fuel insomnia? Brain Behav Immun Health. (2022) 21:100426. 10.1016/j.bbih.2022.100426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aernout E, Benradia I, Hazo J, Sy A, Askevis-Leherpeux F, Sebbane D, et al. International study of the prevalence and factors associated with insomnia in the general population. Sleep Med. (2021) 82:186–92. 10.1016/j.sleep.2021.03.028 [DOI] [PubMed] [Google Scholar]
- 16.Morin C, Bjorvatn B, Chung F, Holzinger B, Partinen M, Penzel T, et al. Insomnia, anxiety, and depression during the COVID-19 pandemic: an international collaborative study. Sleep Med. (2021) 87:38–45. 10.1016/j.sleep.2021.07.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bai W, Zhao Y, Cai H, Sha S, Zhang Q, Lei S, et al. Network analysis of depression, anxiety, insomnia and quality of life among Macau residents during the COVID-19 pandemic. J Affect Disord. (2022) 311:181–8. 10.1016/j.jad.2022.05.061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Y, Qin Q, Sun Q, Sanford L, Vgontzas A, Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. (2020) 16:1417–8. 10.5664/jcsm.8524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen W, Chen S, Zhong B. Sense of alienation and its associations with depressive symptoms and poor sleep quality in older adults who experienced the lockdown in Wuhan, China, during the COVID-19 pandemic. J Geriatr Psychiatry Neurol. (2022) 35:215–22. 10.1177/08919887221078564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. (2007) 3(5 Suppl.):S7–10. 10.5664/jcsm.26929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang Y, Zhu L, Ma Y, Bo H, Deng H, Cao J, et al. Association of insomnia disorder with sociodemographic factors and poor mental health in COVID-19 inpatients in China. Sleep Med. (2020) 75:282–6. 10.1016/j.sleep.2020.06.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bajaj S, Blair K, Schwartz A, Dobbertin M, Blair R. Worry and insomnia as risk factors for depression during initial stages of COVID-19 pandemic in India. PLoS One. (2020) 15:e0243527. 10.1371/journal.pone.0243527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ding K, Wang S, Xu W, Lin L, Liao D, Chen H, et al. Low mental health literacy and its association with depression, anxiety and poor sleep quality in Chinese elderly. Asia Pac Psychiatry. (2022) 14:e12520. 10.1111/appy.12520 [DOI] [PubMed] [Google Scholar]
- 24.Mai E, Buysse D. Insomnia: prevalence, impact, pathogenesis, differential diagnosis, and evaluation. Sleep Med Clin. (2008) 3:167–74. 10.1016/j.jsmc.2008.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morin C, LeBlanc M, Daley M, Gregoire J, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. (2006) 7:123–30. 10.1016/j.sleep.2005.08.008 [DOI] [PubMed] [Google Scholar]
- 26.Borsboom D, Cramer A. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. (2013) 9:91–121. 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- 27.Hofmann S, Curtiss J, McNally R. A complex network perspective on clinical science. Perspect Psychol Sci. (2016) 11:597–605. 10.1177/1745691616639283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borsboom D. A network theory of mental disorders. World Psychiatry. (2017) 16:5–13. 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bai W, Zhao Y, An F, Zhang Q, Sha S, Cheung T, et al. Network analysis of insomnia in chinese mental health professionals during the covid-19 pandemic: a cross-sectional study. Nat Sci Sleep. (2021) 13:1921. 10.2147/NSS.S326880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li W, Zhao N, Yan X, Xu X, Zou S, Wang H, et al. Network analysis of depression, anxiety, posttraumatic stress symptoms, insomnia, pain, and fatigue in clinically stable older patients with psychiatric disorders during the COVID-19 outbreak. J Geriatr Psychiatry Neurol. (2022) 35:196–205. 10.1177/08919887221078559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cai H, Bai W, Sha S, Zhang L, Chow I, Lei S, et al. Identification of central symptoms in Internet addictions and depression among adolescents in Macau: a network analysis. J Affect Disord. (2022) 302:415–23. 10.1016/j.jad.2022.01.068 [DOI] [PubMed] [Google Scholar]
- 32.Liu S, Yang L, Zhang C, Xiang Y, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e17–8. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hlatshwako T, Shah S, Kosana P, Adebayo E, Hendriks J, Larsson E, et al. Online health survey research during COVID-19. Lancet Digit Health. (2021) 3:e76–7. 10.1016/S2589-7500(21)00002-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morin C. Insomnia: Psychological assessment and management. New York, NY: Guilford press; (1993). [Google Scholar]
- 35.Yu D. Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. (2010) 66:2350–9. 10.1111/j.1365-2648.2010.05394.x [DOI] [PubMed] [Google Scholar]
- 36.Morin C, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schulte T, Hofmeister D, Mehnert-Theuerkauf A, Hartung T, Hinz A. Assessment of sleep problems with the Insomnia Severity Index (ISI) and the sleep item of the Patient Health Questionnaire (PHQ-9) in cancer patients. Support Care Cancer. (2021) 29:7377–84. 10.1007/s00520-021-06282-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baghyahi S, Torabi S, Gao Y, Cao K, Baghsyahi H. Relaibility and validity of the Chinese translation of insomnia severity index (C-ISI) in Chinese patients with insomnia. Eur Psychiatry. (2011) 26:1556. 10.1016/S0924-9338(11)73260-6 [DOI] [Google Scholar]
- 39.Bai C, Ji D, Chen L, Li L, Wang C. Reliability and validity of Insomnia Severity Index in clinical insomnia patients. Chin J Pract Nurs. (2018) 2018:2182–6. [Google Scholar]
- 40.Chen M, Sheng L, Qu S. Diagnostic test of screening depressive disorders in general hospital with the Patient Health Questionnaire. Chin Ment Health J. (2015) 2015:241–5. [Google Scholar]
- 41.Kroenke K, Spitzer R, Williams J. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.He X, Li C, Qian J, Cui H, Wu W. A study on the reliability and validity of generalized Anxiety Scale in general hospitals. Shanghai Psychiatry. (2010) 22:200–3. [Google Scholar]
- 43.Spitzer R, Kroenke K, Williams J, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 44.Cheung Y, Yeo K, Chong K, Khoo E, Wee H. Measurement equivalence of the English, Chinese and Malay versions of the World Health Organization quality of life (WHOQOL-BREF) questionnaires. Health Qual Life Outcomes. (2019) 17:1–6. 10.1186/s12955-019-1130-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xia P, Li N, Hau K, Liu C, Lu Y. Quality of life of Chinese urban community residents: a psychometric study of the mainland Chinese version of the WHOQOL-BREF. BMC Med Res Methodol. (2012) 12:37. 10.1186/1471-2288-12-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. (1998) 28:551–8. 10.1017/S0033291798006667 [DOI] [PubMed] [Google Scholar]
- 47.R Core Team. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; (2020). [Google Scholar]
- 48.Epskamp S, Borsboom D, Fried E. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. (2018) 50:195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yang Y, Zhang D, Li Y, Zhang M, Wang P, Liu X, et al. Prevalence, correlates, and network analysis of Internet addiction symptoms among Chinese pregnant and postpartum women. J Affect Disord. (2022) 298:126–33. 10.1016/j.jad.2021.10.092 [DOI] [PubMed] [Google Scholar]
- 50.Gómez-Rubio V. ggplot2-elegant graphics for data analysis. J Stat Softw. (2017) 77:1–3. 10.18637/jss.v077.b02 [DOI] [Google Scholar]
- 51.Robinaugh D, Millner A, McNally R. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. (2016) 125:747–57. 10.1037/abn0000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Haslbeck J, Waldorp L. How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods. (2018) 50:853–61. 10.3758/s13428-017-0910-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Epskamp S, Cramer A, Waldorp L, Schmittmann V, Borsboom D. qgraph: Network visualizations of relationships in psychometric data. J Stat Softw. (2012) 48:1–18. 10.18637/jss.v048.i04 [DOI] [Google Scholar]
- 54.Huang Y, Wang Y, Zeng L, Yang J, Song X, Rao W, et al. Prevalence and correlation of anxiety, insomnia and somatic symptoms in a Chinese population during the COVID-19 epidemic. Front Psychiatry. (2020) 11:568329. 10.3389/fpsyt.2020.568329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pappa S, Ntella V, Giannakas T, Giannakoulis V, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. 10.1016/j.bbi.2020.05.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu F, Wang X, Yang Y, Zhang K, Shi Y, Xia L, et al. Depression and insomnia in COVID-19 survivors: a cross-sectional survey from Chinese rehabilitation centers in Anhui province. Sleep Med. (2022) 91:161–5. 10.1016/j.sleep.2021.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang C, Song W, Hu X, Yan S, Zhang X, Wang X, et al. Depressive, anxiety, and insomnia symptoms between population in quarantine and general population during the COVID-19 pandemic: a case-controlled study. BMC Psychiatry. (2021) 21:99. 10.1186/s12888-021-03108-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kong G, Kong D, Shi L. Sleeplessness in COVID-19 pandemic: lockdown and anxiety. J Asian Econ. (2022) 80:101460. 10.1016/j.asieco.2022.101460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mullarkey M, Marchetti I, Beevers C. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. (2019) 48:656–68. 10.1080/15374416.2018.1437735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liu C, Liu D, Huang N, Fu M, Ahmed J, Zhang Y, et al. The combined impact of gender and age on post-traumatic stress symptoms, depression, and insomnia during COVID-19 outbreak in China. Front Public Health. (2021) 8:620023. 10.3389/fpubh.2020.620023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nussbaumer-Streit B, Mayr V, Dobrescu A, Chapman A, Persad E, Klerings I, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev. (2020) 4:CD013574. 10.1002/14651858.CD013574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. (2020) 70:124. 10.1016/j.sleep.2020.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan S, Siddique R, Li H, Ali A, Shereen M, Bashir N, et al. Impact of coronavirus outbreak on psychological health. J Glob Health. (2020) 10:010331. 10.7189/jogh.10.010331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jansson M, Linton S. The role of anxiety and depression in the development of insomnia: Cross-sectional and prospective analyses. Psychol Health. (2006) 21:383–97. 10.1080/14768320500129015 [DOI] [Google Scholar]
- 65.Benca R, Peterson M. Insomnia and depression. Sleep Med. (2008) 9:S3–9. 10.1016/S1389-9457(08)70010-8 [DOI] [PubMed] [Google Scholar]
- 66.O’Connell K, Frei O, Bahrami S, Smeland O, Bettella F, Cheng W, et al. Characterizing the genetic overlap between psychiatric disorders and sleep-related phenotypes. Biol Psychiatry. (2021) 90:621–31. 10.1016/j.biopsych.2021.07.007 [DOI] [PubMed] [Google Scholar]
- 67.Riemann D, Krone L, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. (2020) 45:74–89. 10.1038/s41386-019-0411-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sun Q, Qin Q, Basta M, Chen B, Li Y. Psychological reactions and insomnia in adults with mental health disorders during the COVID-19 outbreak. BMC Psychiatry. (2021) 21:19. 10.1186/s12888-020-03036-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jansson-Fröjmark M, Lindblom K. A bidirectional relationship between anxiety and depression, and insomnia? A prospective study in the general population. J Psychosom Res. (2008) 64:443–9. 10.1016/j.jpsychores.2007.10.016 [DOI] [PubMed] [Google Scholar]
- 70.Franzen P, Buysse D. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialog Clin Neurosci. (2008) 10:473–81. 10.31887/DCNS.2008.10.4/plfranzen [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jansson-Fröjmark M, Norell-Clarke A. Cognitive behavioural therapy for insomnia in psychiatric disorders. Curr Sleep Med Rep. (2016) 2:233–40. 10.1007/s40675-016-0055-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cao X, Wang S, Zhong B, Zhang L, Ungvari G, Ng C, et al. The prevalence of insomnia in the general population in China: a meta-analysis. PLoS One. (2017) 12:e0170772. 10.1371/journal.pone.0170772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hartescu I, Morgan K, Stevinson C. Increased physical activity improves sleep and mood outcomes in inactive people with insomnia: a randomized controlled trial. J Sleep Res. (2015) 24:526–34. 10.1111/jsr.12297 [DOI] [PubMed] [Google Scholar]
- 74.Mahmud S, Mohsin M, Dewan M, Muyeed A. The global prevalence of depression, anxiety, stress, and insomnia among general population during COVID-19 Pandemic: a systematic review and meta-analysis. Trends Psychol. (2022) 10.1007/s43076-021-00116-9 [Epub ahead of print]. [DOI] [Google Scholar]
- 75.Morin C, Vézina-Im L, Ivers H, Micoulaud-Franchi J, Philip P, Lamy M, et al. Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020). Sleep. (2021) 45:zsab258. 10.1093/sleep/zsab258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.The World Bank. GDP per capita (current US$). Washington, D.C: The World Bank; (2022). [Google Scholar]
- 77.Tsaras K, Tsiantoula M, Papagiannis D, Papathanasiou I, Chatzi M, Kelesi M, et al. The Effect of Depressive and Insomnia Symptoms in Quality of Life among Community-Dwelling Older Adults. Int J Environ Res Public Health. (2022) 19:13704. 10.3390/ijerph192013704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bowen A, Staggs S, Kaar J, Nokoff N, Simon S. Short sleep, insomnia symptoms, and evening chronotype are correlated with poorer mood and quality of life in adolescent transgender males. Sleep Health. (2021) 7:445–50. 10.1016/j.sleh.2021.03.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang J, Lin R, Sun K, Gao L. Incidence and correlates of insomnia and its impact on health-related quality of life among Chinese pregnant women: a cross-sectional study. J Reprod Infant Psychol. (2022) 10.1080/02646838.2021.2020228 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 80.Ohayon M, Paiva T. Global sleep dissatisfaction for the assessment of insomnia severity in the general population of Portugal. Sleep Med. (2005) 6:435–41. [DOI] [PubMed] [Google Scholar]
- 81.Ohayon M, Wickwire E, Hirshkowitz M, Albert S, Avidan A, Daly F, et al. National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health. (2017) 3:6–19. 10.1016/j.sleh.2016.11.006 [DOI] [PubMed] [Google Scholar]
- 82.Gangwisch J, Malaspina D, Babiss L, Opler M, Posner K, Shen S, et al. Short sleep duration as a risk factor for hypercholesterolemia: analyses of the National Longitudinal Study of Adolescent Health. Sleep. (2010) 33:956–61. 10.1093/sleep/33.7.956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cespedes Feliciano E, Quante M, Rifas-Shiman S, Redline S, Oken E, Taveras E. Objective sleep characteristics and cardiometabolic health in young adolescents. Pediatrics. (2018) 142:e20174085. 10.1542/peds.2017-4085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Scott A, Webb T, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. (2021) 60:101556. 10.1016/j.smrv.2021.101556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Supartini A, Honda T, Basri N, Haeuchi Y, Chen S, Ichimiya A, et al. The impact of sleep timing, sleep duration, and sleep quality on depressive symptoms and suicidal ideation amongst Japanese freshmen: The EQUSITE study. Sleep Disord. (2016) 2016:8737654. 10.1155/2016/8737654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Babicki M, Piotrowski P, Mastalerz-Migas A. Assessment of insomnia symptoms, quality of life, daytime sleepiness, and psychoactive substance use among polish students: a Cross-Sectional Online Survey for Years 2016–2021 before and during COVID-19 Pandemic. J Clin Med. (2022) 11:2106. 10.3390/jcm11082106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Eklund M. Work status, daily activities and quality of life among people with severe mental illness. Qual Life Res. (2009) 18:163–70. 10.1007/s11136-008-9431-5 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this article are not readily available because the Institutional Review Board (IRB) of the University of Macau that approved the study prohibits the authors from making publicly available the research dataset of clinical studies. Requests to access the datasets should be directed to Y-TX, xyutly@gmail.com.